Background:
The chronic inflammatory skin condition hidradenitis suppurativa (acne inversa), characterized by hair follicle or apocrine gland infection, causes recurrent superficial nodules and abscesses in axillary, mammary, and perianal regions. Chronic reoccurrence results in fistula formation, causing scarring and fibrosis. Surgical excision of affected skin tissue with adequate free margins is the gold standard treatment to prevent recurrence. This case series describes 6 cases of radical excision of localized axillary hidradenitis suppurativa, with immediate or delayed perforator-based propeller flap defect closure.
Methods:
All patients presenting for surgical treatment of hidradenitis suppurativa between 2016 and 2018 were identified from the hospital database. Only patients with hidradenitis suppurativa confined to the axilla were included. Patients with simple abscess incisions, recurrence after previous grafting/flap surgery, and extension of the disease outside the axilla region were excluded. Patient demographics, size of defect, complications, time of follow-up, recurrences, and level of patient satisfaction were documented.
Results:
Six patients with localized axillary hidradenitis suppurativa were identified, with 8 propeller flap surgeries performed. Defect size was assessed by pathologic examination of excised specimens, ranging from 11–18 cm × 6–14 cm × 0.5–2 cm (length × width × depth). Seven of the eight wounds healed primarily. Functional and aesthetic results were satisfactory and there were no recurrences. The only observed complication was venous congestion following 1 flap procedure.
Conclusion:
These findings confirm that the propeller flap procedure can be effective for immediate or delayed defect closure after radical excision of localized axillary hidradenitis suppurativa, providing that no perifocal signs of infection are present after debridement.
INTRODUCTION
The chronic skin condition hidradenitis suppurativa (HS), also referred to as acne inversa, was first described by Velpeau in 1839 as inflammation of the skin with the formation of superficial abscesses in the axillary, mammary, and perianal areas.1 HS is characterized by infection and inflammation of hair follicles or apocrine glands, causing recurrent nodules and abscesses under the skin, painful induration, and requiring sloughing and pus drainage. Reoccurrence in cases of refractory and chronic disease can result in lesions progressing to form sinus tracts and fistulae, which when healed can lead to severe scarring and fibrosis. HS may affect any area of the body surface where apocrine glandular tissue is found, but infections typically occur in the skin of the inframammary, inguinal, perineal, and axillary regions.2
Local incision and drainage of purulent lesions are often required in the acute phase of HS and although these conservative procedures provide adequate short-term relief, they are not effective as a long-term treatment and insufficient debridement is a major factor in episodes of recurrence.3,4 When the disease is chronic and extensive, surgical excision of the affected skin tissue and the adjacent apocrine glandular zone (with adequate free margins) is considered the gold standard treatment for prevention of recurrence.5–7
Historically, extensive and severe HS is treated with excision of the affected tissue and the surgical defect is either left to heal by secondary intention or grafted with a split-thickness skin graft.3,4 Higher rates of postoperative morbidity, secondary scar contractures, prolonged recovery time, and shoulder stiffness with objectively reduced range of movement have also been reported in this group.5,8
Most of the described flap procedures for the coverage of soft-tissue defects following the resection of HS are technically demanding and associated with disfiguring scars and donor site morbidity.9,10 However, recently the use of local, regional, and free flaps have been applied to reconstruction of the axilla after excision of HS, such as the fasciocutaneous V-Y flap, Limberg flap, and musculocutaneous flap.11
In particular, perforator flaps such as the thoracodorsal artery perforator (TDAP) flap have been reported to be effective for the reconstruction of soft-tissue defects following excision of severe extensive axillary HS.8 The propeller flap is a local island fasciocutaneous flap, based on a single dissected perforator. It is designed like a propeller with 2 blades of unequal length with the perforator forming the pivot point so that when the blades are switched, the long arm comfortably fills in the defect.12
Radical surgical excision is the treatment of choice in severe and extensive HS, and while many methods have been applied for treatment, most of them do not provide satisfactory results for patients. Therefore, the purpose of this case series is to highlight the effective use of the perforator-based propeller flap, as an immediate or delayed covering technique for defects in the axillary area resulting from excision of severe and extensive HS, with optimal functional and aesthetic results observed.
PATIENTS AND METHODS
Inclusion Criteria
A case series study was performed on all consecutive patients undergoing surgical treatment for axillary HS at the department of plastic and reconstructive surgery at the Al-Babtain Centre at the Ibn Sina Hospital, Kuwait. All patients presenting for operative treatment of HS between January 2016 and June 2018 were identified from the hospital database. Only patients presenting with extensive and severe HS confined to the axilla were included in the study, whereas patients who presented with HS of other areas of the body (such as the groin) were excluded. The severity of disease was classified using the Hurley classification criteria.13 Patients who were eligible for primary closure of the defect after surgical excision of the axilla were excluded from this study (Hurley stage I and II). In addition, patients presenting with moderate lesions with a good response to medical treatment were also excluded. Other exclusion criteria were cases of peripheral vascular disease and the presence of any signs of clinical infection upon admission. Those patients classified as Hurley stage III with extensive disease or recurrent disease were divided into 2 groups according to their timing of reconstruction, with either immediate or delayed construction performed depending on the conditions after excision. Both verbal and written consent were obtained from the patients, including consent of use of photographic images (Fig. 1).
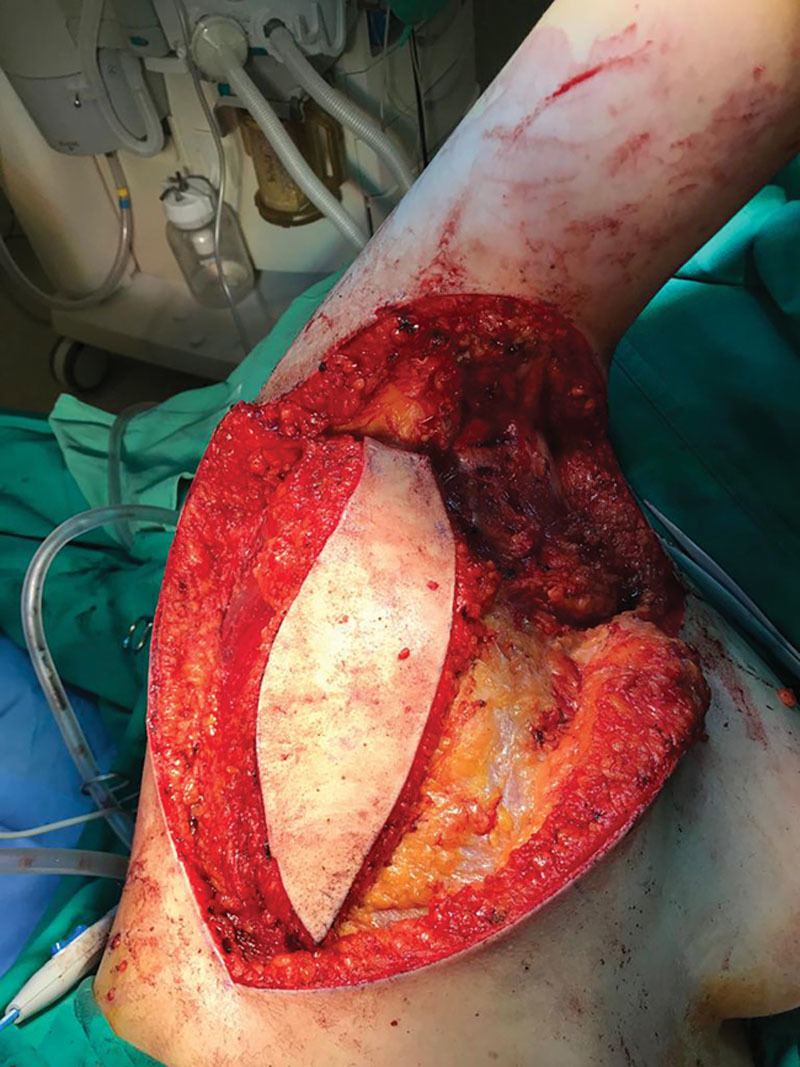
Fig. 1.

Grade 111 hidradenitis suppurativa in the right axilla region, graded according to the Hurley classification criteria.
Analyzed Parameters
Demographic data were extracted (Table 1) on patient smoking, obesity, duration of disease, drug history, previous HS treatment (medical and surgical), complications after surgery (wound infection, wound breakdown, hematoma, lymphocutaneous fistula, lymphocele, lymphedema), time of follow-up, and episodes of recurrences. Sizes of the defects were assessed retrospectively by macroscopic measurement of the pathology specimens. Finally, patients were asked if they would undergo the procedure again considering their postoperative result.
Table 1.
Patient Demographic Data with a Summary of Analyzed Endpoints
| Patient Number | Age at Time of Surgery | Sex | Axilla Side | Follow-up (mo) | Complications | Defect Size (cm) | Comorbidities | Immediate or Delayed Reconstruction | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Length | Width | Depth | ||||||||
| 1 | 19 | M | Bilateral | 12 | Wound dehiscence | 15.9 | 8.5 | 1.3 | Psychosis | Both |
| 2 | 33 | M | Left unilateral | 8 | None | 16.5 | 12 | 0.5 | None | Delayed |
| 3 | 40 | F | Left unilateral | 14 | Necrosis at the distal end of the flap | 20 | 13 | 2 | Morbidly obese | Immediate |
| 4 | 32 | M | Bilateral | 6 | None | 12 | 8 | 0.5 | Heavy smoker | Immediate |
| 5 | 37 | F | Left unilateral | 7 | Venous congestion | 14 | 9 | 0.8 | None | Immediate |
| 6 | 30 | M | Right unilateral | 9 | None | 11 | 6 | 0.8 | Smoker | Delayed |
Operative Technique
Under general anesthesia, patients were placed in the right or left lateral position with an angle of 120 degrees maintained between the upper limb and trunk. Excision of the affected axilla (cutis and subcutis) (Fig. 1A) was performed radically, down to the muscle fascia. The resulting defect (Fig. 1B) was closed using a perforator-based propeller flap which relies on either thoracodorsal or intercostal system depends on the excision. The skin paddle was designed based on aesthetic considerations of the donor and recipient site.14.8 The perforator was selected at the nearest point of the defect, identified by Doppler ultrasound imaging. The flap was rotated from the trunk to close the defect at the axilla. (See Video [online], which displays how a flap is raised after detecting its perforator artery via a Doppler and is rotated to fill the axillary defect after the excision of the hidradenitis suppurativa.)
Video.
All procedures were performed by the same surgeon.
Postoperatively, all patients received antibiotic treatment with 1.5 g cefuroxime (second-generation cephalosporin) and 500 mg metronidazole, with 3 intravenous doses followed by oral antibiotics 3 times daily, for a total of 7 days. Patients were immobilized for 24 hours and thromboembolic prophylaxis with low molecular weight heparin was administered until full mobilization was achieved. The arm should be kept abducted at 90-degree angle for at least 24 hours postoperatively. Twenty-four to forty-eight hours postoperatively, suction drains were removed and compressive stockings were applied for a minimum 4-week period.
RESULTS
Between January 2016 and June 2018, a total of 6 patients with localized axillary HS were identified. Two patients had bilateral HS and therefore, in total, 8 propeller flap procedures were performed. Four patients were treated by radical excision and immediate reconstruction by propeller flap, the other 2 patients were treated with delayed reconstruction using the same flap, with axilla reconstructed after 2 weeks of excision.
The first patient was 19 years old and presented with stage 3 bilateral axillary HS based on the Hurley classification system. The left side was treated by radical excision with immediate reconstruction using the propeller flap procedure. Right side excision was also performed, although reconstruction was delayed for 2 weeks. Four of the total 6 patients were males and 2 were females, with a mean age of 30 years old. In all cases, multiple incisions of abscesses had been performed before the current surgery and all of the patients had tried conservative forms of treatment before surgery.
The average defect size was assessed by retrospective macroscopic measurements of the excised specimens during pathologic examination. Defect sizes ranged from 11–18 cm × 6–14 cm × 0.5–2 cm (length × width × depth). All wounds, except for 1, healed primarily and in all cases functional and aesthetic results were satisfactory. No major complications were observed and no episodes of recurrence were reported.
The postoperative courses were uneventful, with no occurrence of major complications such as flap necrosis, septicemia, or thromboembolic events. In 1 patient, there was a minor case of wound dehiscence, which healed following repeated dressing and follow-up. One patient developed a postoperative distal 0.5 cm flap necrosis. The mean postoperative duration of admittance was 4 days (ranging from 2 to 6 days) and the mean follow-up time was 10 months (ranging from 2 to 18 months). No cases of recurrence were observed within the follow-up period.
The patients reported being pleased with their postoperative results, both functionally and aesthetically. All of the patients stated that they would undergo the same procedure again if they had the choice. In addition, surgically the postoperative results were considered to be both functionally and aesthetically pleasing (Figs. 2–5).
Fig. 2.

Axilla region after excision of the lesion.
Fig. 5.

Flap placement and direct closure of the donor site.
DISCUSSION
The treatment of axillary HS can broadly be divided into medical and surgical approaches. Medical treatments include both topical and systemic therapies, such as antibiotics, steroids, and biological therapies.15 However, many of these interventions have significant side effects and are associated with a high rate of recurrence of disease.16 Historically, extensive severe HS is treated by excision of the affected tissue and the surgical defect is either left to heal by secondary intention or grafted with a split-thickness skin graft.3,4 Although surgical excision of the affected skin tissue is considered to be the gold standard treatment for prevention of recurrence,5 some negative implications have been reported in this treatment group, such as higher rates of postoperative morbidity, secondary scar contractures, prolonged recovery time, and shoulder stiffness with objectively reduced range of movement.5
Recent surgical advances in the reconstruction of the axilla after excision of HS have exhibited the successful use of local, regional, and free flaps, such as the fasciocutaneous V-Y flap, Limberg flap, and musculocutaneous flap. In particular, perforator flaps, such as the TDAP flap, have been reported to be advantageous for the reconstruction of soft-tissue defects following excision of severe extensive axillary HS. The use of perforator flaps overcome some of the technical difficulties and the tendency for scar formation and donor site morbidity associated with previously described flap reconstruction procedures.9–11 Although staged procedures for excision and coverage have been advocated to decrease the rate of postoperative infection,17 other studies have proposed that the rate of wound infections and recurrence rates are independent of the method used for reconstruction.18 Postoperative infection was not an issue in any of the cases assessed in this study.
Although studies on the vascular basis of the TDAP flap procedures have identified the expected perforator locations from the descending branch,19–21 the skin paddle is generally designed based on aesthetic considerations of both the donor and recipient site.8,14 In the axillary region, the thoracodorsal artery and the posterior intercostal artery perforators are particularly useful as basing flaps that can import inner tissues to defects on the lateral region. Hyakusoku et al22 described an island propeller flap procedure, based on a broad central subcutaneous pedicle that can be rotated to a maximum of 90-degree angle to release scar contractures around the flexure creases of joints.
Previously reported studies have postulated that any flap based on a single vascular perforator can sustain its own composite block of tissue (angiosome) and sufficiently sustaining the angiosome of the adjacent perforator and potentially up to half the territory of the perforator next to it.23,24 However, the rate of ischemic complications have been reported to reach 10% in procedures using propeller flap types.25
CONCLUSIONS
The results of this case series study support the use of perforator-based propeller flaps for effective postexcision reconstruction of severe axillary HS. Based on these cases and the currently available literature, the propeller flap procedure appears to be an ideal method for the treatment of extensive axillary HS, with short recovery times, low rates of postoperative complications, short follow-up periods, and therefore an improved postoperative quality of life.
Fig. 3.

Marking for flap formation and identification of the perforator.
Fig. 4.
Cutting the flap and dissection of the donor site.
Footnotes
Published online 14 August 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Balik E, Eren T, Bulut T, et al. Surgical approach to extensive hidradenitis suppurativa in the perineal/perianal and gluteal regions. World J Surg. 2009;33:481–487. [DOI] [PubMed] [Google Scholar]
- 2.Harrison BJ, Mudge M, Hughes LE. Recurrence after surgical treatment of hidradenitis suppurativa. Br Med J (Clin Res Ed). 1987;294:487–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bieniek A, Matusiak L, Okulewicz-Gojlik D, et al. Surgical treatment of hidradenitis suppurativa: experiences and recommendations. Dermatol Surg. 2010;36:1998–2004. [DOI] [PubMed] [Google Scholar]
- 4.Chen E, Friedman HI. Management of regional hidradenitis suppurativa with vacuum-assisted closure and split thickness skin grafts. Ann Plast Surg. 2011;67:397–401. [DOI] [PubMed] [Google Scholar]
- 5.Busnardo FF, Coltro PS, Olivan MV, et al. The thoracodorsal artery perforator flap in the treatment of axillary hidradenitis suppurativa: effect on preservation of arm abduction. Plast Reconstr Surg. 2011;128:949–953. [DOI] [PubMed] [Google Scholar]
- 6.Rieger UM, Erba P, Pierer G, et al. Hidradenitis suppurativa of the groin treated by radical excision and defect closure by medial thigh lift: aesthetic surgery meets reconstructive surgery. J Plast Reconstr Aesthet Surg. 2009;62:1355–1360. [DOI] [PubMed] [Google Scholar]
- 7.Wormald JC, Balzano A, Clibbon JJ, et al. Surgical treatment of severe hidradenitis suppurativa of the axilla: thoracodorsal artery perforator (TDAP) flap versus split skin graft. J Plast Reconstr Aesthet Surg. 2014;67:1118–1124. [DOI] [PubMed] [Google Scholar]
- 8.Ruetschi MS, LeWinn LR, Chaglassian TA. Variation of latissimus dorsi skin island design for postmastectomy reconstruction. Ann Plast Surg. 1981;6:171–178. [DOI] [PubMed] [Google Scholar]
- 9.Greenbaum AR. Modified abdominoplasty as a functional reconstruction for recurrent hydradenitis suppurativa of the lower abdomen and groin. Plastic and Reconstructive Surgery. 2007;119:764–766. [DOI] [PubMed] [Google Scholar]
- 10.Dagrégorio G, Darsonval V. A tailor-made flap for an extremely severe case of hidradenitis suppurativa in the genital area. Ann Chir Plast Esthet. 2005;50:242–246. [DOI] [PubMed] [Google Scholar]
- 11.Ortiz CL, Castillo VL, Pilarte FS, et al. Experience using the thoracodorsal artery perforator flap in axillary hidradentitis suppurativa cases. Aesthetic Plast Surg. 2010;34:785–792. [DOI] [PubMed] [Google Scholar]
- 12.Pontén B. The fasciocutaneous flap: its use in soft tissue defects of the lower leg. Br J Plast Surg. 1981;34:215–220. [DOI] [PubMed] [Google Scholar]
- 13.Hurley H. Dermatological Surgery: Principles and Practice. 19892nd ed New York, NY: Marcel Dekker. [Google Scholar]
- 14.Millard DR., Jr Variations in the design of the latissimus dorsi flap in breast reconstruction. Ann Plast Surg. 1981;7:269–271. [DOI] [PubMed] [Google Scholar]
- 15.Jemec GB. Clinical practice. Hidradenitis suppurativa. N Eng J Med. 2012;366:158–164. [DOI] [PubMed] [Google Scholar]
- 16.Soria A, Canoui-Poitrine F, Wolkenstein P, et al. Absence of efficacy of oral isotretinoin in hidradenitis suppurativa: a retrospective study based on patients’ outcome assessment. Dermatology. 2009;218:134–135. [DOI] [PubMed] [Google Scholar]
- 17.Lirón-Ruiz R, Torralba-Martinez JA, Pellicer-Franco E, et al. Treatment of long-standing extensive perianal hidradenitis suppurativa using double rotation plasty, V-Y plasty and free grafts. Int J Colorectal Dis. 2004;19:73–78. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka A, Hatoko M, Tada H, et al. Experience with surgical treatment of hidradenitis suppurativa. Ann Plast Surg. 2001;47:636–642. [DOI] [PubMed] [Google Scholar]
- 19.Angrigiani C, Grilli D, Siebert J. Latissimus dorsi musculocutaneous flap without muscle. Plast Reconstr Surg. 1995;96:1608–1614. [DOI] [PubMed] [Google Scholar]
- 20.Spinelli HM, Fink JA, Muzaffar AR. The latissimus dorsi perforator-based fasciocutaneous flap. Ann Plast Surg. 1996;37:500–506. [DOI] [PubMed] [Google Scholar]
- 21.Thomas BP, Geddes CR, Tang M, et al. The vascular basis of the thoracodorsal artery perforator flap. Plast Reconstr Surg. 2005;116:818–822. [DOI] [PubMed] [Google Scholar]
- 22.Hyakusoku H, Yamamoto T, Fumiiri M. The propeller flap method. Br J Plast Surg. 1991;44:53–54. [DOI] [PubMed] [Google Scholar]
- 23.Callegari PR, Taylor GI, Caddy CM, et al. An anatomic review of the delay phenomenon: I. experimental studies. Plast Reconstr Surg. 1992;89:397–407; discussion 417. [PubMed] [Google Scholar]
- 24.Taylor GI, Corlett RJ, Caddy CM, et al. An anatomic review of the delay phenomenon: II. clinical applications. Plast Reconstr Surg. 1992;89:408–16; discussion 417. [PubMed] [Google Scholar]
- 25.De Mey A, Lejour M, Declety A, et al. Late results and current indications of latissimus dorsi breast reconstructions. Br J Plast Surg. 1991;44:1–4. [DOI] [PubMed] [Google Scholar]


