Supplemental Digital Content is available in the text.
Background:
As social media’s applications continue to evolve, the pitfalls and dangers associated with misuse have been accentuated in the literature. Consequently, academic institutions across the nation have implemented social media policies. This study is aimed to evaluate the state of social media literature examining postgraduate trainees (residents/fellows).
Methods:
A systematic search was performed identifying peer-reviewed publications presenting original research. Studies published through December 8, 2018, focusing on social media use among postgraduate trainees were considered for inclusion.
Results:
Fifty-three studies were categorized into 4 domains: (1) resident recruitment, (2) graduate medical education, (3) professional development, and (4) academic scholarship. Thirty-four (64.15%) investigated social media’s impact on professional development, of which 16 (47.05%) highlighted the detrimental potential on trainee professionalism. The remaining 18 (52.94%) focused on promoting social media training during residency, and/or enhancing social media competency to benefit professional development. Fourteen (26.42%) rationalized social media use in augmenting graduate medical education. Ten (18.87%) assessed social media’s influence on resident recruitment, of which 7 (70%) depicted use as a screening instrument for program directors on resident applicants. Two (3.77%) of the studies introduced social media as a platform for academic scholarship with indicators as altmetrics.
Conclusions:
The well-established disadvantages of social media use by the postgraduate trainee continue to persist in the literature. However, there is recognition of social media as a valuable resource in influencing resident recruitment, graduate medical education, professional development, and academic scholarship, representing a paradigm shift—from cautiously avoidant to thoughtful capitalization on its immense potential.
INTRODUCTION
With over 3 billion estimated users worldwide, social media’s application is seemingly limitless in today’s society.1 Their use has been increasingly adopted in healthcare, as the ability for cost-effective and rapid dissemination of information can be used as a tool for education, networking, and collaboration. However, the attributes which make social media a powerful tool for communication also facilitate user vulnerability to abuse and unprofessionalism. This is particularly true for trainees in graduate medical education who maintain social media profiles.
There are large bodies of literature investigating professional social media use by attending plastic surgeons.2–4 Recently, studies specific to trainees in plastic surgery have begun to emerge.5 To better understand the nature of the literature discussing professional social media use in plastic surgery training, we undertook a systematic review of the available body of research. Our objective was to assess the state of social media use within the trainee population with regards to resident recruitment, education, professional development, and academic scholarship. We sought to investigate how social media have been incorporated in graduate medical education in general, and how that pertains to plastic surgery.
METHODS
Literature Search Methodology
A systematic review of the scientific literature was conducted in December 2018 for English-language peer-reviewed publications using the following 6 electronic databases: Cochrane Library, EBSCO Host CINAHL, OvidSP Embase, OvidSP MEDLINE, OVIDSP PsycINFO, and PubMed. The following terms and Boolean operators were incorporated into each database search: social media [AND] resident [OR] resident physician [OR] trainee [OR] graduate medical education [OR] residency education. Mapped terms were included when possible. There were no time limitations applied to the search.
For study purposes, social media were defined as web-based or mobile-based applications that enable individuals to construct a profile, publish user-generated content, facilitate multiuser interactive communication, and promote development of social networks. For this study, podcasts and blogs were included for analysis. However, Wiki platforms were excluded, as this platform allows content to be created without explicit authorship though it is a form of collaborative editing. In addition, Wiki platforms do not facilitate interuser exchanges, making them inherently different from blogging and other social media platforms.6,7 “Trainee” was defined as a resident physician, intern, or fellow. Thus, studies pertaining to medical students, undergraduate medical education, continuing medical education, and practicing physicians were excluded. Trainees in ancillary fields of medicine including pharmacy, nursing, and dietetics were excluded.
Selection Criteria
All titles and abstracts of the retrieved studies from the above database query were independently screened, and relevant publications were selected for potential inclusion. The full-text remaining articles were retrieved and assessed further for the presence of all of the following inclusion criteria: study focused on postgraduate trainees, main focus of study pertained to social media use, study presents original research data, and article word count excluding abstract, references, figure legends, or table captions exceeds 500 words. The following publication types were excluded: perspective, commentary, letters to the editor, conference abstracts, and case reports.
Data Extraction
The following variables were recorded from each study: study authors, publication year, study aim(s), study design, study time/duration, participant description, number of institutions involved in sampling, intervention description, social media platform used, evaluation method, type of data collected, internal structure validity, complexity of data analysis, outcomes, and study quality.
Quality Assessment
The quality of quantitative studies was appraised using the Medical Education Research Study Quality Instrument (MERSQI) (See table, Supplemental Digital Content 1, which displays quality reporting of the 42 quantitative studies according to the Medical Education Research Study Quality Instrument [MERSQI], http://links.lww.com/PRSGO/B145). MERSQI is an instrument designed to evaluate the quality of medical education research and has been shown to have substantial interrater reliability with reproducible results when utilized independently.8 Qualitative studies were appraised using the Consolidated criteria for Reporting Qualitative studies: 32-item checklist. (See table, Supplemental Digital Content 2, which displays quality reporting of the 11 qualitative studies according to consolidated criteria for reporting qualitative research criteria, http://links.lww.com/PRSGO/B146.)
This checklist was developed to promote explicit and comprehensive reporting of qualitative studies.9 Criterion validity of the above tools was evidenced by publication impact factors, citation rates, and expert ratings.8–10
RESULTS
The initial search of the 6 aforementioned online databases identified 667 potential studies. Ten additional records were identified through a manual search of reference lists from the initial set of retrieved studies. After duplicates were removed from the initial search pool, 612 studies remained. After these studies were screened by title, a further 448 irrelevant studies were excluded. The remaining 164 studies were selected for full-text review, and after application of inclusion and exclusion criteria, 53 studies were included for final study analysis (Fig. 1).
Fig. 1.
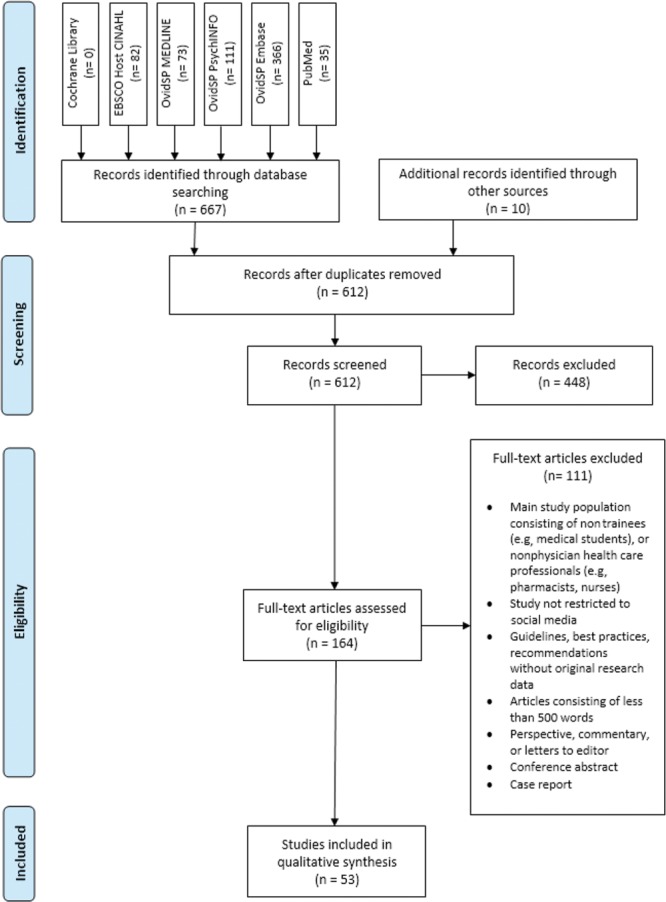
Study attrition diagram showing the study selection and attrition process.
Key study characteristics are described in Tables 1–4 for each of the 4 common areas of trainee education identified during the literature review: (1) resident recruitment, (2) education, (3) professional development, and (4) academic scholarship. Several studies focused on multiple areas. Ten (18.87%) studies investigated resident recruitment, whereas 14 (26.42%) studies investigated education. The majority of the studies (64.15%, n = 34) investigated professional development. The fewest studies (3.77%, n = 2) investigated academic scholarship. The social media platforms most frequently identified were Facebook (n = 34; 33.33%), Twitter (n = 24; 23.53%), YouTube (n = 7; 6.89%), and blogs (n = 7; 6.89%).
Table 1.
Studies Regarding SoMe Influence on Graduate Medical Education.
| Studies Regarding SoMe Influence on Graduate Medical Education | ||||
|---|---|---|---|---|
| Study Authors and Date | Aim(s) | Participants | Evaluation Method(s) | Major Findings |
| Bensalem-Owen et al (2011)11 | Assess efficacy of using podcasts to provide resident EEG education | n = 10 anesthesiology residents | • Test scores between podcast and nonpodcast users | No statistically significant difference in mean test scores between podcast learners and conventional (lecture-based) learners |
| Bergl et al (2015)12 | Advance internal medicine residency program’s educational mission via Twitter | n = 61 internal medicine residents | • Survey to measure resident satisfaction of educational contribution per twitter feed, number of tweets generated | 68.9% agreed Twitter feed enhanced education, over 1,000 tweets generated |
| Bogoch et al (2012)13 | Assess efficacy of posting morning report session blog as an educational tool | n = 93 internal medicine residents and medical students | • Survey of reported helpfulness, detailed blog analytics | 74% reported blog was helpful |
| Calderon et al (2011)14 | Implement innovative teaching tools in nephrology such as blogs, concept maps, interactive cases, and role play | n = 220 students, residents, fellows, and other physicians | • Postintervention survey regarding opinions of study’s tools versus traditional methods | 63% agreed study’s tools would increase interest in nephrology as a career for students and residents, 45% agreed blogs would enhance nephrology education |
| Desai et al (2012)15 | In-depth analysis of Twitter activity at Kidney Week 2011 | n = 132 internal medicine faculty, PDs, chief residents, and residents | • Analyze conference participants Twitter authorship and retweet activity | 132 participants authored 867 tweets. 19% of participants were faculty and authored 49% of tweets. 14% of participants were residents and authored 16% of tweets. 52% of 261 retweets were authored by faculty |
| Galiatsatos et al (2016)16 | Assess impact of academic institute’s Twitter page on attitude and behavior of residents toward SoMe use for medical education | n = 35 internal medicine residents | • Pre- and postintervention surveys to assess resident views and frequency of use of SoMe for educational purposes | 97.1% preintervention residents use SoMe. 77% of respondents used SoMe for medical education at baseline. 25.7% preintervention Twitter use increased to 57.5% postintervention |
| Jalali et al (2015)17 | Analyze educational content value of tweets from an academic conference | n = 373 conference participants that generated 4,958 tweets utilizing #ICRE2013 | • Categorize tweets into 3 cognitive themes and assess educational utility • Identify top 10 influencers or promoters of knowledge |
Analysis of Twitter transcript revealed evidence of 3 cognitive themes as related to how people learn. Twitter appears to be most effective at stimulating individuals’ preconceptions, thus engaging them with new material acquired during a medical education conference |
| Koontz et al (2018)18 | Investigate SoMe use trends within an academic radiology department, highlighting generation gaps between trainees and faculty | n = 112 consisting radiology trainees and faculty | • Survey regarding SoMe utilization and SoMe-based educational curriculum | 83% of respondents use SoMe. Faculty are more likely than trainees to avoid SoMe use (30% versus 9%). Trainees are more likely than faculty to find electronic case-based curriculum useful (95% versus 83%). Baby Boomers are less interested in using SoMe for educational activities compared with Generation X and Millenials (24% versus 73%) |
| Liu et al (2017)19 | Assess efficacy of an interactive SoMe (Facebook, Twitter)-based ECG interpretation curriculum for residents | n = 39 emergency, family, and internal medicine residents participated in the study, of which 15 completed the poststudy assessment | • Pre- and postintervention assessments of ECG interpretation competency | ECG scores were 66% preintervention and increased to 76% postintervention |
| Loeb et al (2013)20 | Characterize SoMe use among members of the American Urological Association | n = 382 consisting of urology attendings and trainees | • Survey regarding SoMe use including motives | 74% reported having a SoMe account, of which 28% reported SoMe utilization partly or entirely for professional purposes. 89% of attendings and 98% of trainees (residents/fellows) have Facebook accounts. Urologists who were <40 years old were more likely to have SoMe accounts versus their older counterparts |
| Matava et al (2013)21 | Delineate the content needs, format, preferences, and usage patterns of podcasts | n = 169 anesthesia residents across 10 Canadian programs | • Survey regarding podcast use and preference practices | 60% report having used medical podcasts. 72% cited “ability to review materials whenever” as reasoning for finding podcasts valuable. Of the 40% that denied podcast use, 58% reported nonuse because they did not know they were available |
| Oyewumi et al (2017)22 | Assess SoMe use within Canadian ENT programs and gauge interest within these programs to integrate SoMe into networking, social, and educational programs | n = 101 including 19 residents, 1 fellow, and 80 staff physicians | • Survey regarding SoMe use and implications | 58.4% reported use of SoMe accounts for personal and professional use. <35% failed to separate their personal and professional accounts. Trainees and physicians identified potential benefits of SoMe in their specialty but most were unsure how to apply it to their practice |
| Ranschaert et al (2016)23 | Investigate how radiologists are using SoMe and attitude toward use | n = 477 radiologists and radiology trainees including 277 from Europe and 127 from North America | • The RANSOM survey assessing SoMe use practices | 85% use SoMe for personal and professional reasons. SoMe preference for personal use (USA 94%, Europe 91%) and professional use (USA 41%, Europe 35%). 75% ranked insufficient legislation, guidelines, and policies as the top disadvantage of using SoMe. 85% foresee a great future for SoMe in medicine. 73% believe radiologists should use SoMe more because it enhances professional and academic development |
| Salem et al (2017)24 | Assess professional SoMe use to determine the value of digital media for clinical practice and academic exchange | n = 228 consisting of 58 urology residents (Canada) and 170 urology residents (Germany) | • Survey to determine SoMe use, perceived usefulness of digital media for clinical practice, and educational utility | 46% use SoMe professionally. 34% of professional SoMe users and 20% of all respondents stated familiarity with SoMe guidelines. Professional use of SoMe was 65% in Canada and 39% in Germany. SoMe usefulness for clinical practice was 65% in Canada and 39% in Germany |
ECG, electrocardiography; EEG, electroencephalography; ENT, ear, nose, throat; PDs, program directors; RANSOM, radiologists and social media; SoMe, social media.
Table 4.
Studies Regarding SoMe Influence on Academic Scholarship.
| Studies Regarding SoMe Influence on Academic Scholarship | ||||
|---|---|---|---|---|
| Study Authors and Date | Aim(s) | Participants | Evaluation Method(s) | Major Findings |
| Nikolian et al (2018)58 | Determine Twitter use across the USA by general surgery training programs and evaluate if educational content increases engagement | n = 32 departmental Twitter accounts out of the 272 departments | • Analyze Twitter activity between October 1, 2016, and December 31, 2016, and characterize each tweet as educational or promotional • Assess metrics related to SoMe presence |
Accounts posted a median 1.0 tweet per week. 81% of tweets were promotional. Accounts with generally promotional content generated low engagement (3.4 likes/tweet; 1.5 retweets/tweet) versus a more active account with 48% educational content and 19.6 unique tweets/wk averaging 11.4 likes/tweet; 5.9 retweets/tweet |
| Rivas et al (2018)59 | Assess the perceived role of SoMe in urologic knowledge acquisition among trainees | n = 316 residents and urologists consisting of members of the European Society of Residents in Urology, the German Society of Residents in Urology, and the Residents and Young Urologist Spanish Workgroup | • Survey to evaluate the influence of SoMe and urology education | 99% use SoMe professionally and/or personally. YouTube and LinkedIn were the most commonly used platforms for professional use. SoMe ranked in third place as a source for urologic news/updates, after journals and websites. 61% follow urologic associations, 44% follow urologic journals, and 39% follow urologic experts on SoMe. The perceived influence of SoMe on urology knowledge was rated as moderate to high by 63% and as low to none by 37% of young urologists |
SoMe, social media.
Table 2.
Studies Regarding SoMe Influence of Resident Recruitment.
| Studies Regarding SoMe Influence on Resident Recruitment | ||||
|---|---|---|---|---|
| Study Authors and Date | Aim(s) | Participants | Evaluation Method(s) | Major Findings |
| Deloney et al (2014)25 | Investigate use and perceived utility of information provided on radiology program websites, and preferences for interview day experience | n = 70 interviewees for a diagnostic radiology residency program | • Survey to elucidate online sources for gaining program-specific information | 85% of respondents used at least 1 SoMe platform to gain information about programs, 38% of which cited a blog (auntminnie.com). 59% found residency program websites to be most useful. 73% used institution’s website to discover more about program |
| Dulmage et al (2018)26 | Identify unstructured SoMe data submitted by residency applicants and categorize positive and negative statements to determine key themes to provide detailed insights into the motivations and desires of trainees | Anonymized medical trainees applying to residency in 9 specialties—dermatology, general surgery, internal medicine, OBGYN, plastic surgery, otolaryngology, physical medicine and rehabilitation, pediatrics, and radiology (2007–2017) | • Positive and negative comments broken down into major features, themes, and subthemes to determine frequency counts and percentages | 6,314 comments identified, of which 4,541 (72%) were positive and 1,773 (28%) were negative. Institution was most commonly cited as major feature in both positive (17%) and negative (47%) comments. Training (clinical more often than research) was the second most cited feature in both positive (22%) and negative (16%) comments. Geography was the most cited theme—city, cost of living, and commute were commonly cited subthemes |
| Go et al (2012)27 | Determine general surgery and subspecialty PDs’ use of SoMe during residency selection, recruitment, impact on applicant, and ethical opinions | n = 250 general surgery PDs | • Survey to assess frequency of SoMe use for screening applicants and reasoning behind its use | 17.3% PDs reported reviewing applicant SoMe to gain additional information, 37.5% of plastic surgery PDs reported this practice and was the highest reported of all specialties. Facebook was the most commonly used SoMe platform at 92.9%. 78.6% report interest in screening for unprofessional behavior as the most common reason for SoMe use |
| Go et al (2012)28 | Determine extent of SoMe screening of applicants by residency programs | n = 2,619 including 1,200 PDs, 179 AMG, 396 USIMG, and 844 non-USIMGs | • Survey to determine level of insight AMG, USIMG, non-USIMG have on use of SoMe screening by PDs for resident application • Survey PDs regarding SoMe practices for resident recruitment |
16.3% of PDs reported screening applicants’ SoMe, and 38.1% of which ranked the applicant lower as a result. More AMGs believed PDs used Facebook to screen applicants versus USIMGs and non-USIMGs |
| Golden et al (2012)29 | Assess otolaryngology (ENT) applicants’ Facebook profiles, including the presence of content in violation of ACGME professional standards | n = 119 ENT applicants with publicly searchable Facebook profiles | • Review content of ENT applicants’ Facebook profiles and screen for unprofessional content | 11% of ENT applicants had questionable content. One profile contained clear violations of professionalism. Professionalism scores from this study did not predict applicant’s success with the match |
| Langenfeld et al (2016)30 | Assess the rate and manner in which general surgery PDs use SoMe and experience with inappropriate SoMe use among students, residents, and faculty | n = 110 general surgery PDs | • Survey to evaluate PDs’ SoMe use and practices regarding resident applicant screening, and monitoring digital professionalism of current residents and faculty | 45% of PDs had visited resident SoMe profiles, with 10% resulting in formal disciplinary action. 18% PDs reported screening resident applicants, with 11% resulting in lowering the applicant’s rank or removal from rank list |
| Ponce et al (2013)31 | Determine number of Facebook profiles, amount of publicly available information, and screen for inappropriate content of orthopedic surgery applicants | n = 153 orthopedic surgery applicants at a single institution (USA) with publicly accessible Facebook profiles | • Review Facebook profiles, perform descriptive analysis, screen for unprofessional content using the ACGME’s description of professionalism as a guide | Mean professionalism score of 2.82 (3 = no professionalism issues; 2 = questionable content). 16% of Facebook profiles contained unprofessional content. No significant difference in professionalism scores between applicants that matched versus those who did not match |
| Schweitzer et al (2012)32 | Evaluate use of social networking websites as a means for medical students and trainees to interact with GME programs and the impact these relationships have on application decisions | n = 992 including 797 medical students and 195 trainees | • Survey regarding SOMe use and its impact on desired residency program | 35% report using SoMe sites to gather information about residency positions. 85% reported that their desired residency program did not have a SoMe presence. 10% reported that SoMe presence would influence their choice in residency |
| Sullivan et al (2017)33 | Evaluate utility of SoMe as a screening tool for (OBGYN) resident applicant professionalism | n = 87 OBGYN residency applicants | • Review Facebook accounts of applicants before and after Match day | No applicants met criteria for unprofessional SoMe content. Public profiles increased by 1.1%, limited profiles increased by 10.3%, and private profiles decreased by 11.5% after Match day |
ACGME, Accreditation Council for Graduate Medical Education; AMG, American medical graduates; ENT, ear, nose, throat; GME, graduate medical education; OBGYN, Obstetrics and Gynecology; PDs, program directors; SoMe, social media; USIMG, US international medical graduates.
Table 3.
Studies Regarding SoMe Influence on Professional Development.
| Studies Regarding SoMe Influence on Professional Development | ||||
|---|---|---|---|---|
| Study Authors and Date | Aim(s) | Participants | Evaluation Method(s) | Major Findings |
| Adilman et al (2016)34 | Assess SoMe use among oncologists as increased use will enhance physician communication, education, and mentorship | n = 207 consisting of 51% medical oncologists, 29% trainees, 6% radiation oncologists, 6% medical students, 6% other | • Survey to measure SoMe use to identify gaps between age-defined physician generations | 72% use SoMe. SoMe use highest at 93% in 25-34 yrs old. SoMe use lowest at 39% in 45-54 yrs old. |
| Barker et al (2012)35 | Determine SoMe practices of anesthesiology PDs | n = 66 anesthesiology PDs | • Survey regarding SoMe use practices by PDs and its influence on anesthesiology trainees | 30.3 % of program hospitals had SoMe policies. 81.8% denied reprimanding trainee for inappropriate SoMe use. 66.7% denied providing SoMe use education. 54.5% monitor SoMe habits of trainees if alerted of problem. 12.1% report frequent use of internet for screening resident applicant. 57.6% report never using internet to screen applicants. |
| Ben-Yakov et al (2015)36 | Determine ethical perspective and practices of using internet to search for patients | n = 530, including emergency physicians, residents, and medical students | • Survey to assess frequency of searching patient on internet | 12.1% used Google to search for patients, 1.9% used Facebook. 13% disclosed their actions to patient. 24.5% reported searching for patients on Facebook as “very unethical” |
| Black et al (2010)37 | Measure and compare use frequency and content on Facebook profiles of 2 cohorts of medical students and residents (2007 and 2009) | n = 1,023 consisting of 372 Facebook profiles of medical students and residents in 2007, and 651 in 2009 | • Evaluate Facebook profiles for privacy settings, personal information, affiliated social groups, and photographic content | 39.8% of residents and 69.5% of medical students maintained their Facebook accounts. 2009 cohort was less likely to post unprofessional content compared with 2007 cohort. 33% of public profiles depicted alcohol use, 12.6% had unprofessional “wall” postings including obscenities, racist remarks, and descriptions of unprofessional behavior. |
| Chandawarkar et al (2018)5 | Characterize trends and content of plastic surgery residency-associated Instagram accounts | n = 67 integrated plastic surgery programs | • Identify number of integrated plastic surgery programs with Instagram accounts, number of posts, follower count • Post content analysis |
21% of integrated plastic surgery programs have active Instagram accounts, with a total of 806 posts, 4,466 followers, 3.97% posts included intraoperative photos, one (0.12%) showed a patient image. |
| Colvin et al (2018)38 | Implement a pilot curriculum to address professionalism, social, and communication competencies in surgical residency | n = 16 surgical interns | • Pre- and postintervention surveys regarding perceived need for PSC training | Preintervention survey revealed 86% agreeing to additional PSC training, this increased to 94% postintervention. |
| Cook et al (2013)39 | Examine professionalism practices and policies, utilization of new resources, and professionalism concerns with SoMe use in pediatric training programs | n = 122 pediatric program PDs | • Survey regarding professionalism practices, including structure of curricula, methods of trainee assessment, use of nationally available resources, and SoMe policies | 70% provide instruction to trainees about professionalism on SoMe. 73% were unaware of the AMA policy on “Professionalism in the Use of Social Media.” 30% report prohibiting trainee from graduating or sitting for an exam secondary to ethical or professional misconduct. |
| Dawkins et al (2017)40 | Explore SoMe professionalism competency and frequency of exposure to postings that violate SoMe professionalism guidelines among pediatric residents | n = 1,628 pediatric residents | • Survey with vignettes that challenge published SoMe guidelines to test competency • Assess frequency of viewing similar postings • Assess knowledge of institutional SoMe policies, and experience with education on SoMe professionalism |
73.29% correctly determined the 5 vignettes as unprofessional. 53.93% endorsed frequently viewing posts that violated professionalism standards, including derogatory remarks about patients. 40% unaware of SoMe policy, and 12.5% reported no such policy exists. 22.85% have never received structured SoMe training. |
| Desai et al (2014)41 | Investigate novel use of private bidirectional direct messages via Twitter to provide resident feedback and evaluations | n = 13 emergency medicine residents | • Pre- and postintervention surveys regarding opinions on pre- and postintervention feedback and evaluation methods • Measurement of tweets and completed formal evaluations via Twitter |
13 residents received 8 formal evaluations. 220 tweets were provided by 7 faculty members. Postintervention survey demonstrated increased feedback volume and detail of evaluations via Twitter |
| Diller et al (2018)42 | Analyze Twitter use of EM residency programs and assess conformance of recommendations by CORD of emergency medicine | n = 88 EM programs | • Survey to determine CORD compliance • Assess program Twitter use motives |
58% of respondents had a program-level Twitter account. 61% were not compliant with CORD recommendations and were managed by residents versus faculty. Twitter was frequently used for educational and promotional purposes. |
| Farber et al (2017)43 | Assess Twitter use by academic urology programs | n = 38 academic urology residency programs | • Assess volume of tweets, followers, following, account age, and activity details • Repeat assessment in 6 months |
30% of urology residencies have Twitter accounts. Among the 5 most active accounts, median number of tweets, followers, following, and age of account was 58, 154, 107.5, and 20 mo, respectively. At 6-mo reassessment, there was average 161% increase in tweets and 148% increase in follower count. Twitter presence and U.S. News and world report ranking appear to be unrelated (p = 0.51) |
| George et al (2014)44 | Measure medical students’ insight regarding the magnitude their Facebook postings may have on residency admissions process | n = 2,109 medical students | • Survey to determine medical student opinions on residency admissions committees using Facebook to screen applicants for unprofessionalism | 63.5% believed unprofessional Facebook photos should not be grounds for automatic rejection. 33.7% believed photos should have no bearing on application and are irrelevant. 2.8% believed pictures should be grounds for automatic rejection. Over 50% of residency programs report inappropriate Facebook posting could adversely affect admission |
| Ginory et al (2012)45 | Determine need for SoMe training about digital professionalism during residency | n = 182 psychiatry residents | • Survey regarding Facebook use along with professionalism concerns | 12.3% respondents have Facebook account publicly available for viewing. 9.7% have received friend requests from a current patient—none accepted. 3.9% received friend requests from a former patient—one was accepted. 18.7% have searched for their patient’s SoMe profile. 2.7% report having discussed the use of SoMe with their training programs |
| Irfan et al (2018)46 | Assess utility of SoMe among family medicine residents and physicians in Saudi Arabia | n = 132 including 92 family medicine residents and 40 physicians | • Survey to determine SoMe use frequency, platform preference, and perceived benefits | 38% physicians reported professional SoMe use versus 21% of residents. Youtube was most frequently accessed at 68.2%. Generally, females use SoMe for education and professional development, whereas males use it more frequently for personal purposes |
| Jain et al (2018)47 | Assess Canadian-educated, graduating urology residents’ practices of and attitudes toward personal and professional SoMe use | n = 100 final-year residents in urology training programs | • Survey to measure personal and professional SoMe use • Determine awareness of existing professional guidelines for SoMe use |
92% report SoMe use, of which 73% endorse personal SoMe use. 12% reported frequent professional SoMe. 59% objected to direct patient interaction online. 76% supported using SoMe to provide patients with static information, 65% supported using SoMe to collaborate with colleagues. 2%–8% had read guidelines and legislation for physician online use |
| Jent et al (2011)48 | Assess insight on SoMe and professionalism between faculty and trainees | n = 109 including 29 faculty members (pediatricians, psychologist, social workers), and 80 residents and medical students | • Survey regarding SoMe use and opinions on fictional SoMe vignettes | 93.8% trainees and students report SoMe use versus 72.4% of faculty. 17.5% of trainees and students and 11% of faculty reported searching patient’s SoMe. No significant differences in responses to vignettes between trainees, students, and faculty |
| Khandelwal et al (2015)49 | Successfully create a flipped classroom workshop to simulate settings focused on application of challenging professionalism principles, including SoMe use | n = 37 residents representing 19 different medical and surgical disciplines | • Pre and postintervention surveys evaluating various aspects regarding professionalism including competency and comfort. | Preintervention survey: 58.2% of trainees incorrectly believed physicians should “be available whenever their patients need them”. Postintervention trainees felt more comfortable defining professionalism, describing social contract between physicians and society, and applying principles of professionalism |
| Klee et al (2015)50 | Investigate SoMe use of younger physicians versus their predecessors, and evaluate whether or not training regarding appropriate SoMe use is adequate | n = 253 including 61 family medicine residents, and 192 family medicine physicians | • Survey to evaluate SoMe use and correlate this with age and level of medical experience | 90% of residents, 77% of junior physicians, and 70% of senior physicians reported having SoMe accounts. 66% of residents and 50% of practicing physicians believed it was unethical to be SoMe friends with patients. 26% junior physicians and 10% of residents or senior physicians report having had SoMe training. The majority agreed SoMe use should be addressed in medical school and residency |
| Koo et al (2018)37 | Characterize changes in the frequency and nature of unprofessional content on urologists’ Facebook accounts during a 1-y transition period from residency graduation to practice | n = 281 urologists, of which 198 had publicly identifiable Facebook accounts | • Screen publicly available posts for unprofessional or potentially objectionable content via a 65 category rubric based on published professionalism guidelines at completion of residency • Repeat screen 1-year postgraduation |
No significant improvements. 70% versus 71% 1-y later, had publicly available Facebook profiles. 43% versus 40% 1-y later, contained unprofessional or potentially objectionable content (i.e., apparent intoxication, profanity, and offensive comments about patients) |
| Koo et al (2017)51 | Characterize unprofessional content on public Facebook accounts of US urology residency graduates | n = 281 urologists, of which 201 had publicly identifiable Facebook accounts | • Screen publicly available posts for unprofessional or potentially objectionable content via a 65 category rubric based on published professionalism guidelines | 40% of Facebook profiles contained unprofessional or potentially objectionable content, including 13% portraying explicitly unprofessional behavior. 42% self-identified as a urologist on their Facebook profile |
| Landman et al (2010)52 | Examine SoMe use among surgical residents and faculty and continue the discourse about both the use of SoMe and the need for practical guidelines for surgical house staff and faculty | n = 215 including 88 residents, of which 25 have public profiles, and 127 faculty members, of which 17 have public profiles | • Screen publicly accessible Facebook accounts for inappropriate content | 64% of residents and 22% of faculty had Facebook profiles, of which 50% were publicly available. 31% of the publicly accessible Facebook profiles displayed work-related postings, of which 14% were patient-specific. |
| Langenfeld et al (2014)53 | Investigate Facebook profiles of general surgery residents in the Midwest (USA) for evidence of unprofessional conduct | n = 996 surgical residents, of which 32% had identifiable Facebook profiles | • Screen Facebook profiles for unprofessional content | 73.7% of residents had no unprofessional content. 14.1% had potentially unprofessional content. 12.2% had explicitly unprofessional content (i.e., Binge drinking, sexually suggestive photos, and HIPAA violations) |
| Lefebvre et al (2016)54 | Investigate existing perceptions and competencies regarding SoMe and professionalism among residents | n = 70 residents from 9 disciplines | • Survey testing competency regarding digital professionalism and SoMe use | 29% were familiar with current institutional policy on SoMe use, this was associated with a higher score by a mean of 2.2 correct responses to the survey. 67% reported instruction during medical school regarding appropriate SoMe use |
| Moubarak et al (2011)55 | Obtain insight on opinions of trainees at an academic institution in France regarding Facebook activity and its impact on the doctor–patient relationship | n = 202 consisting of 160 residents and 42 fellows in varied specialties | • Survey evaluating views on the doctor–patient relationship via hypothetical situations that could arise with Facebook | 85% would automatically decline patient friend request. 48% believed the doctor–patient relationship would be altered if the patient discovered their doctor had a Facebook account |
| Thompson et al (2011)56 | Document potential patient privacy violations on Facebook profiles of medical students and residents at a single institution in Gainesville, Fla. | n = 1,023 consisting of 372 Facebook profiles of medical students and residents in 2007, and 651 in 2009 | • Screen Facebook profiles for unprofessional content and assess publicly accessible information at two points in time (2007 and 2009) | 12 instances of potential patient privacy violations—1 in 2007, and 11 in 2009. Medical students were more likely to have these violations compared with residents (11 versus 1) |
| Thompson et al (2008)39 | Assess content on SoMe posted by medical students and residents at a single institution in Gainesville, Fla | n= 362 consisting of 322 medical students and 40 residents | • Screen Facebook profiles for unprofessional content and assess publicly accessible information | 64.3% of medical students and 12.8% of residents had Facebook accounts. 62.7% of profiles were public. 10 profiles were randomly selected for in-depth analysis—70% had photos with alcohol, of which 10%–50% portrayed excessive drinking. 30% had unprofessional content including drunkenness, overt sexuality, profanity, and patient privacy violations |
| Wagner et al (2018)57 | Characterize surgeons’ professional use and perceptions of SoMe across 4 academic institutions in the USA | n = 208 including 132 faculty and 76 trainees | • Survey regarding SoMe usage and attitudes. | 70% believe SoMe benefits professional development. Age <55 predicted positive attitude toward SoMe, whereas the rank of respondent as an associate professor predicted negative attitude toward SoMe. Lack of time and personal and patient privacy concerns were cited most commonly as the reasons for not using SoMe |
CORD, Council of Residency Directors; EM, emergency medicine; HIPAA, Health Insurance Portability and Accountability Act; PD, program directors; PSC, professionalism and social competencies; SoMe; Social Media.
Many specialties were represented throughout the literature (Fig. 2). The 2 most frequently cited specialties were urology and general surgery, each with 7 (13.21%) publications. This was followed by emergency medicine, with 4 (7.54%) publications. The following specialties were each cited in 3 (5.66%) publications: anesthesiology, internal medicine, pediatrics, and radiology. Only 1 study (1.9%) investigated social media use by plastic surgery trainees.
Fig. 2.

Publications by specialty/subspecialty. ENT indicates ear, nose, throat; OBGYN, Obstetrics and Gynecology. Studies included in our literature review categorized by specialty and subspecialty. Multidisciplinary publications incorporated trainees from more than 1 specialty.
Resident Recruitment
Of the studies investigating resident recruitment, 7 (70%) discussed social media as a screening instrument for program directors (PDs) during the resident interview process. These studies revealed that 12.1%–37.5% of PDs frequently screen social media profiles of applicants.27–31,33,35,44 Plastic surgery was the specialty most likely to utilize social media for screening applicants, and Facebook (Facebook, Inc., Menlo Park, Calif.) was the social media platform most frequently used for this practice.27 Of the PDs that screened applicants, 11%–38.1% reported lowering the applicant’s rank or removing the applicant from the program’s rank list.28,30
Two (20%) studies investigated the influence of social media on applicant residency preferences. The studies revealed 85% of interviewees utilized at least 1 social media platform to learn more about individual programs,25 and 10% of respondents to another study reported that the presence of a program’s social media profile would influence their residency choices.32 Overall, there is an apparent trend toward residency programs establishing social media profiles, and taking advantage of this largely cost-permissible opportunity.5,16,22,25,43
Education
Fourteen (26.42%) of the studies discussed social media as a platform for enhancing education. The majority of these studies (57.14%, n = 8) were observational, cross-sectional studies consisting of surveys without intervention, and were aimed at gaining insight as to how social media are used in the trainee population for enhancing their education. Unsurprisingly, the majority of trainees use social media personally, up to 97.1%.12 The familiarity and ease of use make social media an appealing educational platform for trainees, and up to 77% use social media for bolstering their medical education at baseline.12
Twitter was the most commonly used social media platform (35.71%; n = 5) identified in studies pertaining to education. Three of the studies utilized pre- and postintervention (Twitter feed) surveys to evaluate the participants’ opinions. One study revealed that 68.9% of respondents agreed their program’s Twitter feed enhanced their education.11 Other popular interventional social media platforms were blogs (n = 2) and podcasts (n = 2).13,14,19,21 Overall, the reported learner satisfaction from the incorporation of social media into trainee education was favorable. One study was able to measure this objectively through evaluation of quiz scores following the implementation of a Facebook and Twitter-based curriculum. The reported scores increased 10% points following the implementation of this curriculum.60
Professional Development
There were a total of thirty-four (64.15%) studies that investigated professional development. These studies included topics such as policing trainee digital professionalism (n = 10), observational studies investigating motivations for social media use (n = 8), studies investigating trainee professionalism competency (n = 6), Twitter analytics from conferences (n = 2), courses teaching trainees about social media and professionalism (n = 2), and studies investigating the existence of residency program social media accounts and related analytics (n = 3).
Of these studies, almost half (47.05%, n = 16) highlighted the potential negative impact of social media on trainee professionalism. For example, 10 (29.42%) studies investigated publicly available Facebook profiles of trainees for evidence of unprofessional conduct finding that up to 43% of publicly available Facebook accounts contained evidence of unprofessional conduct.37 Photographs with alcohol, apparent intoxication, and sexually suggestive content were the most common recurring offenses.39,51–53,61 The definition of unprofessional social media content differed from study to study. However, the majority of these studies advocated the urgent need for the establishment of standardized definitions regarding inappropriate social media content geared specifically for the trainee population. Four (11.76%) studies highlighted the need for professional and social competency training regarding social media use. Overt unfamiliarity with the existence of institutional social media policies was a recurring issue.30,39,40,54 Two studies demonstrated that the majority of trainees (73.29%) were able to provide correct responses to vignettes portraying issues with online professionalism.40,48 In addition, 94% of trainees agreed that a curriculum to address professionalism, social, and communication competencies should be implemented at their institution.38
Thirteen studies (38.24%) explored current social media use and promoted it as a tool for improving professional development through knowledge acquisition, specialty-specific news/updates, and connecting with colleagues.5,18,20,22,23,34,43,46,47,57–59 Social media platforms cited most often for professional development were Twitter, YouTube, and LinkedIn.34,46,59 One study successfully utilized Twitter to expedite the formal evaluation process between faculty and trainees through the use of private bidirectional direct messages.41 The trainees and faculty responded favorably to this novel method and postintervention surveys revealed increased feedback volume and detail of evaluations received by Twitter when compared with the traditional method.41 Overall, a substantial portion of the literature regarding social media and professionalism continue to focus on the dangers and apparent violations of professionalism. However, the number of studies investigating the use of social media to enhance professional development is growing.
Academic Scholarship
There were 2 studies (3.77%) promoting social media as a platform for academic scholarship. An approach described by Nikolian et al58 entails residents and faculty supplying infographics, slides, and abstracts to be presented at a future conference to their program’s Twitter account manager before the conference. This is followed by conference organizers assigning a specific hashtag for conference attendees to use. This method utilizes Twitter as a microblogging platform for academic scholarship and effectively disseminates research findings for the viewing of all of those interested.
The above approach does not address the issue of the lack of an existing peer-review process for verifying the credibility of scholarly articles published on social media platforms without an adjunctive conference. Rivas et al59 found that 59% of urology trainees agreed that impact factor/altmetrics in social media could be considered for inclusion in an academic profile. The establishment of a standardized approach to providing an analogous peer-reviewing process for articles published on social media platforms is a fairly novel proposition that warrants further investigation.
DISCUSSION
Today, 77% of Americans are on social media, spending 2 hours on content per day, and engaging 3 to 8 social media platforms.1 The large-scale adoption of social media by society and the resulting capacity for widespread and rapid content dissemination is undeniable. As social media use enters the medical field and plastic surgery in particular, much has been written for attending surgeons to incorporate it successfully into their practices.62 However, young adults, the demographic trainees fall in, particularly stand out in usage, with 88% of 18- to 29-year olds indicating they use some form of social media.58 Trainees must also learn how to navigate the complex relationship between their professional lives and social media persona. This relationship is a double-edged sword and should be discussed earnestly to allow for the development of a healthy social media presence beginning during a trainee’s residency. Our study demonstrates that there is a dearth of published studies in the plastic surgery literature regarding social media use by trainees. In fact, of the 53 studies identified in this review, only 1 addressed the use of social media by plastic surgery trainees. Of the published literature regarding this topic in all other specialties, 4 areas were commonly addressed: (1) resident recruitment, (2) education, (3) professional development, and (4) academic scholarship.
A social media presence may help or hinder a trainee. Beginning with the recruitment of medical students, programs turn to social media to find the ideal residency candidates. The current study demonstrates that residency PDs not only use their program’s social media profiles as an advertisement to attract applicants but also as a screening tool to eliminate those that may behave inappropriately online.
This surveillance may continue throughout residency with studies showing nearly half of trainee social media accounts demonstrating unprofessional behavior at some point in their residency, and over 90% of trainees advocating for more education on professionalism in the online arena. The potential for severe consequences resulting from unprofessional behavior and the blurring of professional and personal boundaries on social media propelled governing bodies to begin tackling the problem head-on.63–65 In 2013, the Accreditation Council for Graduate Medical Education initiated the implementation of a restructured accreditation system for trainees, including educational milestones (developmentally based, specialty-specific fundamental accomplishments). In plastic surgery, these milestones explicitly include professional and ethical use of social media as a requirement for training progression.66
Despite potential pitfalls, social media also have tremendous potential to enhance trainee education and scholarly activity. Notably, numerous studies have shown social media to be a powerful educational tool by engaging tech-savvy trainees with educational blogs, YouTube videos, podcasts, and Twitter feeds.12,21,33 The incorporation of social media into education is overwhelmingly well-received by the trainee population. There is also a great opportunity for encouraging professional development and increased scholarly activity of trainees by engaging in social media. Such examples include connecting with colleagues across the globe, following experts of various fields, conducting scholarly communication, or utilizing healthcare hashtags to follow topics of interest.
Given its potential for enhancing the residency experience, social media use by plastic surgery trainees will likely continue to rise over the coming years. Trainees must learn to navigate balancing an online social media presence with their professional responsibilities. Unfortunately, there presently are no universal social media guidelines specific to trainees in plastic surgery. Chandawarkar et al5 recently published proposed responsible guidelines for social media use for plastic surgery trainees, where an excellent attempt at bridging this gap while encouraging meaningful social media use was made. In their publication, they offer recommendations to trainees to first consider the purpose of their posts to encourage thoughtful content. They also outline areas of potential legal, ethnical, professional, and less obvious violations. Given the lack of published data on social media use by plastic surgery trainees, further discussion into social media use during the training period of a plastic surgeon’s career should be undertaken with an emphasis on nurturing responsible conduct early on. This is particularly poignant as responsible conduct during the trainee’s residency may have implications for future board certification and career prospects following graduation.
CONCLUSIONS
Social media’s ubiquity and novelty present challenges in defining their use for the physician in training. The majority of initial studies on the matter voiced caution and concern regarding the professionalism of house staff or applicants. The obvious uses of social media as a tool for PDs to screen applicants and monitor trainee’s online professionalism have been highlighted in the literature. In this study, we depict evolving perceptions, a paradigm shift, where a growing body of literature is now focusing on promoting responsible social media use, examining how social media training can enhance professional growth and academic scholarship. As the tone of dialogue transitions from trepidation to interest or even enthusiasm, it is clear that there is a need for formalized standards and education on social media use established within the trainee’s curriculum. Beyond responsible use, training in social media as a platform for professional development and scholarly pursuits can ultimately help house staff harness social media’s pervasiveness and reach in a positive manner.
Footnotes
Published online 19 August 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Pew Research Center. Social media fact sheet. Pew Research Center: Internet, Science & Tech. 2017. https://www.pewinternet.org/fact-sheet/social-media/. Accessed December 2018.
- 2.Fan KL, Economides JM, Song DH. To bot or not? Challenging the top social media influencers in #plasticsurgery. Plast Reconstr Surg. 2019;143:337–343. [DOI] [PubMed] [Google Scholar]
- 3.Branford OA, Kamali P, Rohrich RJ, et al. #Plasticsurgery. Plast Reconstr Surg. 2016;138:1354–1365. [DOI] [PubMed] [Google Scholar]
- 4.Mabvuure NT, Rodrigues J, Klimach S, et al. A cross-sectional study of the presence of United Kingdom (UK) plastic surgeons on social media. J Plast Reconstr Aesthet Surg. 2014;67:362–367. [DOI] [PubMed] [Google Scholar]
- 5.Chandawarkar AA, Gould DJ, Stevens WG. Insta-grated plastic surgery residencies: the rise of social media use by trainees and responsible guidelines for use. Aesthet Surg J. 2018;38:1145–1152. [DOI] [PubMed] [Google Scholar]
- 6.Alalwan AA, Rana NP, Dwivedi YK, et al. Social media in marketing: a review and analysis of the existing literature. Telemat Informat. 2017;34:1177–1190. [Google Scholar]
- 7.Grajales FJ, 3rd, Sheps S, Ho K, et al. Social media: a review and tutorial of applications in medicine and health care. J Med Internet Res. 2014;16:e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cook DA, Reed DA. Appraising the quality of medical education research methods: the medical education research study quality instrument and the newcastle-ottawa scale-education. Acad Med. 2015;90:1067–1076. [DOI] [PubMed] [Google Scholar]
- 9.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. [DOI] [PubMed] [Google Scholar]
- 10.Crowe M, Sheppard L. A general critical appraisal tool: an evaluation of construct validity. Int J Nurs Stud. 2011;48:1505–1516. [DOI] [PubMed] [Google Scholar]
- 11.Bensalem-Owen M, Chau DF, Sardam SC, et al. Education research: evaluating the use of podcasting for residents during EEG instruction: a pilot study. Neurology. 2011;77:e42–e44. [DOI] [PubMed] [Google Scholar]
- 12.Bergl PA, Narang A, Arora VM. Maintaining a twitter feed to advance an internal medicine residency program’s educational mission. JMIR Med Educ. 2015;1:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bogoch II, Frost DW, Bridge S, et al. Morning report blog: a web-based tool to enhance case-based learning. Teach Learn Med. 2012;24:238–241. [DOI] [PubMed] [Google Scholar]
- 14.Calderon KR, Vij RS, Mattana J, et al. Innovative teaching tools in nephrology. Kidney Int. 2011;79:797–799. [DOI] [PubMed] [Google Scholar]
- 15.Desai T, Shariff A, Shariff A, et al. Tweeting the meeting: an in-depth analysis of twitter activity at kidney week 2011. Plos One. 2012;7:e40253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Galiatsatos P, Porto-Carreiro F, Hayashi J, et al. The use of social media to supplement resident medical education - the SMART-ME initiative. Med Educ Online. 2016;21:29332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jalali A, Sherbino J, Frank J, et al. Social media and medical education: exploring the potential of twitter as a learning tool. Int Rev Psychiatry. 2015;27:140–146. [DOI] [PubMed] [Google Scholar]
- 18.Koontz NA, Kamer AP, Dodson SC, et al. Social media utilization at an academic radiology practice. Acad Radiol. 2018;25:111–117. [DOI] [PubMed] [Google Scholar]
- 19.Liu SS, Zakaria S, Vaidya D, et al. Electrocardiogram training for residents: a curriculum based on facebook and twitter. J Electrocardiol. 2017;50:646–651. [DOI] [PubMed] [Google Scholar]
- 20.Loeb S, Bayne CE, Frey C, et al. ; American Urological Association Social Media Work Group. Use of social media in urology: data from the American Urological Association (AUA). BJU Int. 2014;113:993–998. [DOI] [PubMed] [Google Scholar]
- 21.Matava CT, Rosen D, Siu E, et al. Elearning among canadian anesthesia residents: a survey of podcast use and content needs. BMC Med Educ. 2013;13:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oyewumi M, Lee J, Vescan A. Social media in otolaryngology–head and neck surgery. Ear Nose Throat J. 2017;96:E29–E33. [PubMed] [Google Scholar]
- 23.Ranschaert ER, Van Ooijen PM, McGinty GB, et al. Radiologists’ usage of social media: results of the RANSOM survey. J Digit Imaging. 2016;29:443–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salem J, Borgmann H, Baunacke M, et al. Widespread use of internet, applications, and social media in the professional life of urology residents. Can Urol Assoc J. 2017;11:E355–E366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deloney LA, Perrot LJ, Lensing SY, et al. Radiology resident recruitment: a study of the impact of web-based information and interview day activities. Acad Radiol. 2014;21:931–937. [DOI] [PubMed] [Google Scholar]
- 26.Dulmage BO, Akintilo L, Welty LJ, et al. A qualitative, cross-sectional study of positive and negative comments of residency programs across 9 medical and surgical specialties. Am J Med. 2018;131:1130–1134.e6. [DOI] [PubMed] [Google Scholar]
- 27.Go PH, Klaassen Z, Chamberlain RS. Attitudes and practices of surgery residency program directors toward the use of social networking profiles to select residency candidates: a nationwide survey analysis. J Surg Educ. 2012;69:292–300. [DOI] [PubMed] [Google Scholar]
- 28.Go PH, Klaassen Z, Chamberlain RS. Residency selection: do the perceptions of US programme directors and applicants match? Med Educ. 2012;46:491–500. [DOI] [PubMed] [Google Scholar]
- 29.Golden JB, Sweeny L, Bush B, et al. Social networking and professionalism in otolaryngology residency applicants. Laryngoscope. 2012;122:1493–1496. [DOI] [PubMed] [Google Scholar]
- 30.Langenfeld SJ, Vargo DJ, Schenarts PJ. Balancing privacy and professionalism: a survey of general surgery program directors on social media and surgical education. J Surg Educ. 2016;73:e28–e32. [DOI] [PubMed] [Google Scholar]
- 31.Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70:502–507. [DOI] [PubMed] [Google Scholar]
- 32.Schweitzer J, Hannan A, Coren J. The role of social networking web sites in influencing residency decisions. J Am Osteopath Assoc. 2012;112:673–679. [PubMed] [Google Scholar]
- 33.Sullivan ME, Frishman GN, Vrees RA. Showing your public face: does screening social media assess residency applicants’ professionalism? Am J Obstet Gynecol. 2017;217:619–620. [DOI] [PubMed] [Google Scholar]
- 34.Adilman R, Rajmohan Y, Brooks E, et al. Social media use among physicians and trainees: results of a national medical oncology physician survey. J Oncol Pract. 2016;12:79–80, e52. [DOI] [PubMed] [Google Scholar]
- 35.Barker AL, Wehbe-Janek H, Bhandari NS, et al. A national cross-sectional survey of social networking practices of U.S. Anesthesiology residency program directors. J Clin Anesth. 2012;24:618–624. [DOI] [PubMed] [Google Scholar]
- 36.Ben-Yakov M, Kayssi A, Bernardo JD, et al. Do emergency physicians and medical students find it unethical to ‘look up’ their patients on facebook or google? West J Emerg Med. 2015;16:234–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Black EW, Thompson LA, Duff WP, et al. Revisiting social network utilization by physicians-in-training. J Grad Med Educ. 2010;2:289–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Colvin J, French J, Siperstein A, et al. Addressing professionalism, social, and communication competencies in surgical residency via integrated humanities workshops: a pilot curriculum. J Surg Educ. 2018;75:589–593. [DOI] [PubMed] [Google Scholar]
- 39.Cook AF, Sobotka SA, Ross LF. Teaching and assessment of ethics and professionalism: a survey of pediatric program directors. Acad Pediatr. 2013;13:570–576. [DOI] [PubMed] [Google Scholar]
- 40.Dawkins R, King WD, Boateng B, et al. Pediatric residents’ perceptions of potential professionalism violations on social media: a US national survey. JMIR Med Educ. 2017;3:e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Desai B. A novel use of twitter to provide feedback and evaluations. Clin Teach. 2014;11:141–145. [DOI] [PubMed] [Google Scholar]
- 42.Diller D, Yarris LM. A descriptive analysis of the use of twitter by emergency medicine residency programs. J Grad Med Educ. 2018;10:51–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Farber NJ, Koprowski CJ, Modi PK, et al. Twitter use among academic urology programs. Urology Prac. 2017;4:269–274. [DOI] [PubMed] [Google Scholar]
- 44.George DR, Green MJ, Navarro AM, et al. Medical student views on the use of facebook profile screening by residency admissions committees. Postgrad Med J. 2014;90:251–253. [DOI] [PubMed] [Google Scholar]
- 45.Ginory A, Sabatier LM, Eth S. Addressing therapeutic boundaries in social networking. Psychiatry. 2012;75:40–48. [DOI] [PubMed] [Google Scholar]
- 46.Irfan KS, Farhana I, Eiad AF, et al. Family physicians’ utility of social media: a survey comparison among family medicine residents and physicians. Afr Health Sci. 2018;18:817–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jain K, Fuoco MB, Fervaha G, et al. A new wave of urologists? Graduating urology residents’ practices of and attitudes toward social media. Can Urol Assoc J. 2018;12:E298–E313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jent JF, Eaton CK, Merrick MT, et al. The decision to access patient information from a social media site: what would you do? J Adolesc Health. 2011;49:414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khandelwal A, Nugus P, Elkoushy MA, et al. How we made professionalism relevant to twenty-first century residents. Med Teach. 2015;37:538–542. [DOI] [PubMed] [Google Scholar]
- 50.Klee D, Covey C, Zhong L. Social media beliefs and usage among family medicine residents and practicing family physicians. Fam Med. 2015;47:222–226. [PubMed] [Google Scholar]
- 51.Landman MP, Shelton J, Kauffmann RM, et al. Guidelines for maintaining a professional compass in the era of social networking. J Surg Educ. 2010;67:381–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Langenfeld SJ, Cook G, Sudbeck C, et al. An assessment of unprofessional behavior among surgical residents on facebook: a warning of the dangers of social media. J Surg Educ. 2014;71:e28–e32. [DOI] [PubMed] [Google Scholar]
- 53.Thompson LA, Dawson K, Ferdig R, et al. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23:954–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lefebvre C, Mesner J, Stopyra J, et al. Social media in professional medicine: new resident perceptions and practices. J Med Internet Res. 2016;18:e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moubarak G, Guiot A, Benhamou Y, et al. Facebook activity of residents and fellows and its impact on the doctor-patient relationship. J Med Ethics. 2011;37:101–104. [DOI] [PubMed] [Google Scholar]
- 56.Thompson LA, Black E, Duff WP, et al. Protected health information on social networking sites: ethical and legal considerations. J Med Internet Res. 2011;13:e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wagner JP, Cochran AL, Jones C, et al. Professional use of social media among surgeons: results of a multi-institutional study. J Surg Educ. 2018;75:804–810. [DOI] [PubMed] [Google Scholar]
- 58.Nikolian VC, Barrett M, Valbuena VS, et al. Educational content and the use of social media at US departments of surgery. Surgery. 2018;163:467–471. [DOI] [PubMed] [Google Scholar]
- 59.Rivas JG, Socarras MR, Patruno G, et al. Perceived role of social media in urologic knowledge acquisition among young urologists: a european survey. Eur Urol Focus. 2018;4:768–773. [DOI] [PubMed] [Google Scholar]
- 60.Koo K, Bowman MS, Ficko Z, et al. Older and wiser? Changes in unprofessional content on urologists’ social media after transition from residency to practice. BJU Int. 2018;122:337–343. [DOI] [PubMed] [Google Scholar]
- 61.Koo K, Ficko Z, Gormley EA. Unprofessional content on facebook accounts of US urology residency graduates. BJU Int. 2017;119:955–960. [DOI] [PubMed] [Google Scholar]
- 62.Gould DJ, Nazarian S. Social media return on investment: how much is it worth to my practice? Aesthet Surg J. 2018;38:565–574. [DOI] [PubMed] [Google Scholar]
- 63.American Medical Association. (n.d.). Code Of Medical Ethics Of The American Medical Association (2016-2017 ed.). [Google Scholar]
- 64.Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. Jama. 2012;307:1141–1142. [DOI] [PubMed] [Google Scholar]
- 65.Shore R, Halsey J, Shah K, et al. ; AMA Council on Ethical and Judicial Affairs (CEJA). Report of the AMA council on ethical and judicial affairs: professionalism in the use of social media. J Clin Ethics. 2011;22:165–172. [PubMed] [Google Scholar]
- 66.Accreditation Council for Graduate Medical Education. 2017. http://www.acgme.org/What-We-Do/Accreditation/Milestones/Overview. Accessed December 12, 2018.


