Supplemental Digital Content is available in the text
Keywords: community-acquired pneumonia, meta-analysis, pneumonia, vitamin D
Abstract
Emerging evidence has shown that vitamin D deficiency may be related with community-acquired pneumonia (CAP), but individually published studies showed inconclusive results. The aim of this study was to quantitatively summarize the association between vitamin D and the CAP.
We conducted this meta-analysis though a systematic literature search of PubMed, Medline, and EMBASE up to 31 September 2018 with the following keywords ‘vitamin D’ or ‘cholecalciferol’ or ‘25-hydroxyvitamin D’ or ‘25(OH)D’ in combination with ‘community-acquired pneumonia’ or ‘CAP’ or ‘pneumonia’ with no limitations. This meta-analysis was performed following the guidelines of Meta-analysis of Observational Studies in Epidemiology. The association between vitamin D levels and CAP were measured as odds ratio (OR) and weighted mean difference (WMD). Results were combined using a random-effect or a fix-effect meta-analysis, and sensitivity analyses were conducted to explore potential factors.
Eight observational studies involving 20,966 subjects were included. In this meta-analysis, CAP patients with vitamin D deficiency (serum 25(OH)D levels <20 ng/mL) experienced a significantly increased risk of CAP (odds ratio (OR) = 1.64, 95% confidence intervals (CI): 1.00, 2.67), and an obvious decrease of −5.63 ng/mL (95% CI: −9.11, −2.14) in serum vitamin D was demonstrated in CAP patients. Sensitivity analysis showed that exclusion of any single study did not materially alter the overall combined effect.
The evidence from this meta-analysis indicates an association between vitamin D deficiency and an increased risk of CAP patients. However, well-designed trails are required to determine the explicit effect of vitamin D supplementation.
1. Introduction
Community-acquired pneumonia (CAP) is an infectious inflammation of lung parenchyma (including lung interstitium) occurring outside hospitals, which is one of the common infectious diseases threatening human health and is a non-negligible problem during prevention and control of public health emergencies. The prevalence and incidence rates of CAP are linked to increasing age, especially among the elderly above age 65. The patients of CAP in the US was estimated to be 5.6 million every year, among which about 1.1 million patients that needed hospitalization.[1] The average in-hospital duration of CAP patients was 1 week in the US, the 30-day mortality rate was above 20%, and the mortality rate within 1 year of CAP patients after discharge was about 30%.[2–4] Besides, the clinical and economic burden of CAP is high over the world. For example, the costs of CAP in the Europe exceeded 10 billion Euro annually, with inpatient care accounting 5.7 billion, outpatient care 0.5 billion and drugs 0.2 billion.[5–7] About 60% of CAP patients were treated outpatient and the costs were low, however, the 40% of CAP patients admitted were faced with high mortality rate and medical costs, and the death rates of CAP patients during in-hospital treatment were far higher than other causes of death and ranked second among all in-hospital patients[8] With the developing of aging population recent decades, the hospitalization rate and death rate of CAP patients above age 65 are rising.[9]
Recently, much attention has been paid to the role of vitamin D in host defense against infection. Apart from its classic function in calcium-phosphate homeostasis, vitamin D has pleiotropic immunomodulatory properties. It is reported that the vitamin D plays an important role in the innate immune response, particularly by increasing the production of antimicrobial peptides (B–defensing, cathelicidin).10 Furthermore, vitamin D has been found to be of great effect on the activity of the adaptive immune system.[10] And several studies have shown an association between vitamin D deficiency (VDD) and increased the susceptibility to respiratory tract infections.[11–15] One study has investigated the relationship between 25-hydroxyvitamin D (25-(OH) D) levels and clinical outcome in CAP adults.[16] Berry et al found that vitamin D levels were associated with the incidence rate of respiratory tract infections, or namely the incidence rate of respiratory tract infections dropped by 7% when the serum 25-(OH) D3 level increased by 10 nmol/L.[12] Another retrospective study showed the possibility of hospitalization due to CAP rose when the serum 25-(OH) D3 level was < 37 nmol/L.[17] These studies all imply VDD may be the potent cause of CAP. However, Remmelts et al found an opposite conclusion that vitamin D did not reduce the incidence rate of pneumonia, and vitamin D supplementation even would raise the incidence of pneumonia without the medication of steroid hormones.[18] When 162 respiratory tract infection (RTI) adults were randomly given 12 weeks of vitamin D (2000U/d) or placebo, the serum vitamin D levels in the test group significantly rose, but the RTI was not significantly improved.[19] Another study in Canada showed the vitamin D level was not significantly related with the hospitalization of RTI children.[20]
Up to present, there is more and more evidence indicating the association between vitamin D deficiency with community-acquired pneumonia. But these studies researching on the relationship of vitamin D and community-acquired pneumonia showed inconclusive results. Hence, we performed this meta-analysis to quantitatively summarize the association between vitamin D and the CAP, in order to provide some scientific suggestions for prevention of CAP.
2. Methods
2.1. Search strategy and selection criteria
Literatures on PubMed, Medline, Medline, Cochrane and EMBASE were systematically searched up till 31 September 2018 for relevant articles using the following keywords ‘vitamin D’ or ‘cholecalciferol’ or ‘25-hydroxyvitamin D’ or ‘25(OH)D’ in combination with ‘community-acquired pneumonia’ or ‘CAP’ or ‘pneumonia’ with no limitations. We also manually searched all eligible original articles, reviews and other relevant articles. And we contacted relevant authors by emails if necessary. This meta-analysis was performed following the guidelines for Meta-analysis of Observational Studies in Epidemiology (MOOSE).[21] No ethical approval is needed, for the reason that this study is a meta-analysis.
2.2. Inclusion and exclusion criteria
Original articles exploring the association between serum vitamin D status and CAP were reviewed and selected following these inclusion criteria:
-
1.
the study population was human;
-
2.
serum was sampled for assays of vitamin D levels;
-
3.
CAP was the outcome and the control group consisted of people without CAP;
-
4.
the sample size, the odd ratios (ORs) and their corresponding 95% confidence intervals (CIs) of the study were available;
-
5.
vitamin D deficiency (VDD), vitamin D insufficiency (VDI) and severe vitamin D deficiency (SVDD) were defined as 10 to 20 ng/mL, 20 to 30 ng/mL, and <10 ng/mL 25(OH)D, respectively[22];
-
6.
studies published in English; Animal experiments, chemistry, cell-line studies and editorials, review studies, commentaries, opinions and case reports were excluded.
Two authors independently assessed all literature searches and obtained full articles for all citations meeting the selection criteria. Final inclusion or exclusion decisions were made after reading the full articles carefully. A third author was participated in the literature searches to get a consensus when disagreement disappeared.
2.3. Quality assessment
In order to assess the quality of studies in this meta-analysis, the predefined methodological quality assessment criteria for observational studies was used. We assessed the quality of these studies with a checklist, adapted from Taggart et al,[23] using participants selection, comparability of groups at baseline, and how the diagnosis of CAP was made and according to what definition (see Table S1, Supplemental Content, which illustrates the Quality assessment of observational studies). We excluded any study that did not score in any item or a total score <7 out of 10 maximal points.[24] We used the design and sample size of studies to score for heterogeneity. Two authors (LLQ and YFZ) were responsibility for the extraction data independently, and the third author (BAL) took part in to reach a consensus when any differences occurred.
2.4. Data extraction
Data were extracted independently by two authors, and cross-checked by a third author using a standardized data extraction form. This information of each study was extracted carefully: the name of first author, publication year, location, study design, sample size, vitamin D assay method, vitamin D concentration, prevalence of vitamin D deficiency, and potential confounding factors included in the adjustments. In case of relevant data missing, the main authors were contacted for more information.
2.5. Statistical analysis
This meta-analysis was performed on RevMan 5.3 (Cochrane Collaboration, London, UK). The relationship of vitamin D levels and CAP were evaluated as ORs and weighted mean difference (WMD). If the OR and 95% CI were not available, the 2 × 2 tables were used to obtain the value of OR and 95%CI. Data reported as median and range was converted to mean and standard deviation (SD).[25]
Forest plots were used to evaluate the pooled estimates and corresponding 95% CIs for each study. The I2 statistical test was performed to assess the heterogeneity in this meta-analysis. According to the I2 statistical test, there were low (I2 < 25%), moderate (near 50%) and high heterogeneity (> 75%). In case of heterogeneity (I2 > 50%), a random-effects model was used; otherwise, the fixed-effects model was used in this meta-analysis. The sensitivity analyses were conducted to explore potential factors that may introduce heterogeneity into the results, and to investigate the effect of a single article on the overall risk estimated by removing one article in each turn. In this study, the P < .05 was considered significant. Publication bias was also conducted to explore potential factors by the funnel plots.
3. Results
3.1. Description of studies
A total of 623 articles were initially identified through the systematic literature search, and 47 full articles were read after screening the abstracts. Of these, 7 reviews and 22 studies not meeting the inclusion criteria were excluded. In addition, 6 studies were excluded for the reason of insufficient data. Finally, 8 articles[26–33] were included after the strict screening. A flow chart showing the selecting process is summarized in Figure 1.
Figure 1.

Flow chart of literature search and study selection.
According to the predefined methodological quality assessment criteria for observational studies,[23–24] the quality scores of these studies ranged from 8 to 10, indicating all the included studies were of high quality (see Table S2, Supplementary Content, which illustrates the quality scores of included studies).
Characteristics of the included articles are summarized in Table 1. Among the 8 articles, there were 4 case-control studies, 2 retrospective studies, one cross-sectional study and one prospective study. And these studies were published from 2010 to 2018 and reflected 6 countries. Four assay techniques were used to measure vitamin D levels. Among these included studies, 6 studies explored the relationship between VDD and CAP,[27–30,32–33] 5 studies researched the relationship between VDI and CAP,[26,28–29,32–33] and 5 other studies discussed the relationship between SVDD and CAP.[28,30–33] Meanwhile, only 6 of the 8 studies explored the mean difference in serum vitamin D levels between CAP and non-CAP.[26,29–33]
Table 1.
Characteristics of observational studies included in this meta-analysis.
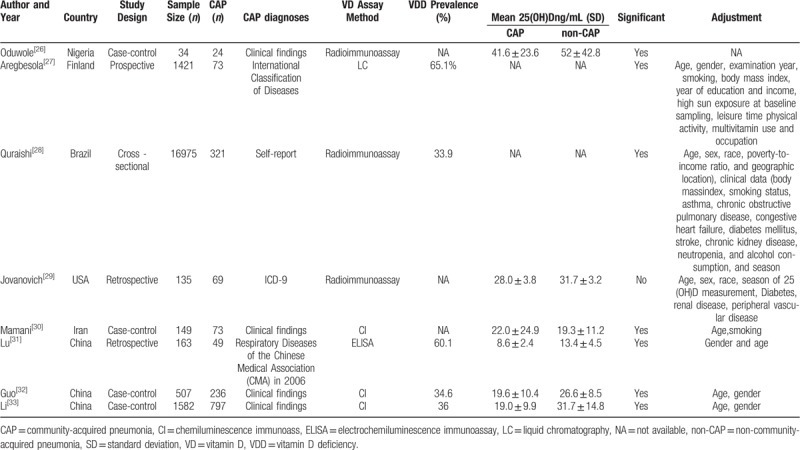
The diversities of participant characteristics were considerable in these studies. A total of 20,966 participants were consisted of various ethnicities. Age ranged from 3 days to 94 years old, and the prevalence of VDD, if provided by studies, ranged from 33.9% to 65.1%. Seven of the 8 studies were conducted in adjustments of age, BMI, gender, smoking and other factors. More detailed information of included studies was presented in Table 1.
3.2. The relationships between vitamin D status and the risk of CAP
The relationships between vitamin D status and CAP are shown in Figures 2–4. Random effect model showed that the association between vitamin D deficiency (VDD) and CAP was significant with high heterogeneity (OR = 1.64, 95%CI: 1.00, 2.67, I2 = 89%) (Fig. 2). Besides, random-effects meta-analysis revealed the association with CAP was not significant for vitamin D insufficiency (VDI), with high heterogeneity (OR = 1.37, 95% CI: 0.81, 2.32, I2 = 88%) (Fig. 3), and significant for severe vitamin D deficiency (SVDD), with high heterogeneity (OR = 6.65, 95%CI: 2.58, 17.15, I2 = 90%) (Fig. 4).
Figure 2.
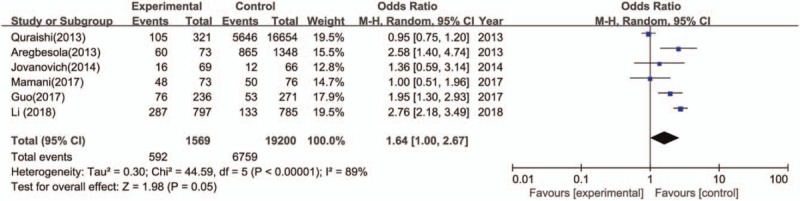
The meta-analysis of the association between VDD and CAP. CAP = community-acquired pneumonia, VDD = vitamin D deficiency.
Figure 4.

The meta-analysis of the association between SVDD and CAP. CAP = community-acquired pneumonia, SVDD = severe vitamin D deficiency.
Figure 3.
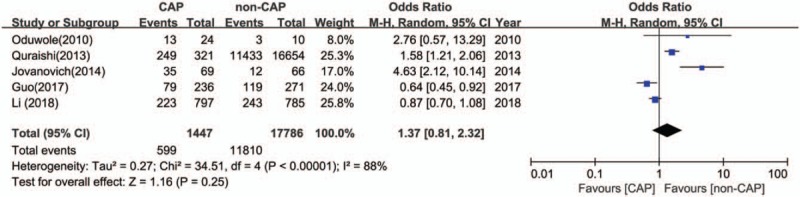
The meta-analysis of the association between VDI and CAP. CAP = community-acquired pneumonia, VDI = vitamin D insufficiency.
The comparison of mean difference between CAP group and non-CAP group is shown in Figure 5. Based on 6 studies, the pooled effect was −5.63 ng/mL (95% CI: −9.11, −2.14) with high heterogeneity (I2 = 95%, P < .01), which showed that there was statistically significant difference in vitamin D levels between CAP group and non-CAP group.
Figure 5.

The meta-analysis of the association between VD level and CAP. CAP = community-acquired pneumonia, VD = vitamin D.
3.3. Sensitivity analysis
Sensitivity analyses were conducted to examine the potential sources of heterogeneity in this meta-analysis. In the results of the WMD, Li‘s study conducted in China[33] was responsible for most of the heterogeneity in this meta-analysis. After excluding this study, the heterogeneity was down to 75% and the WMD was −4.56 (95% CI: −6.40, −2.71). Further exclusion of any single study did not alter the overall combined relative risk, and each outcome had statistical significance. And Quraishi study[28] conducted in Brazil was responsible for most of the heterogeneity in the result of the ORs in this meta-analysis (OR = 1.97, 95% CI: 1.38, 2.81, I2 = 61%). Besides, there were no obvious changes in the pooled ORs as the results of the exclusion of any other single study.
3.4. Publication bias
No obvious publication bias was observed in the funnel plots of this meta-analysis (see Figure S1, Supplementary Content, which illustrates the publication bias in this meta-analysis).
4. Discussion
This is the first meta-analysis on the relationship between serum vitamin D status and CAP among people. The results of 8 observational studies provide strong evidence that serum 25(OH)D level is associated with CAP. Both the results of the pooled ORs and the pooled effect of WMD showed that the serum 25(OH)D levels had a relationship with CAP. VDD experienced a significantly increased risk of CAP (OR = 1.64, 95%CI: 1.00, 2.67). People with CAP, compared to the control, were with the decreased level of vitamin D by 4.56 ng/mL. Considering the prevalence of vitamin D deficiency among humans, this result may provide some scientific suggestions for prevention of CAP.
According to the results of quality assessment, studies included in this meta-analysis were with high quality. Besides, there was no obvious publication bias after the analysis of funnel plots. The results of sensitivity analyses implied 2 studies probably contributed to the heterogeneity.[28,30] After these 2 studies were excluded, low heterogeneity was found. Other heterogeneity might result from different vitamin D measuring methods, different sample time, and the differences among the study populations. Hence, more studies are needed to give full proof.
Vitamin D plays an important role in the CAP. As we known, the cause of CAP is associated with both pathogen infection and immune dysfunction. Vitamin D could considerably exert immune functions, so the level of vitamin D may be a susceptible factor of CAP. So far, the relationship between VD and CAP has been extensively studied. As reported by the US Centers for Disease Control and Prevention (CDC), when newborns with low vitamin D in vivo grow up to 1 year old, they have 6 times higher risks of suffering lung infections than infants with normal vitamin D levels.[34] Another random control-case study showed when 1- to 36-month-old pneumonia infants orally took a single high-dose of vitamin D3 (100,000 IU), recurrence was basically not found within 3 months.[35]
Vitamin D may play two roles in the occurrence of CAP. 1) Vitamin D takes effect through the binding between its activated form 1, 25-(OH)2D3 and the vitamin D receptor (VDR). VDR can stimulate the expression of antibacterial peptides that resist bacterial and viral infections.[36] VDD causes the reduction of VDR level in vivo and thereby the denaturation, cornification and proliferation of respiratory tract mucous membrane epithelia, damaging their clearance function and the accumulation of non-neutralized proinflammatory media; consequently, the inflammatory reactions could not be controlled, leading to injured pulmonary tissues and blocked gas exchange. 2) Recent studies have confirmed the very important immunomodulatory functions that vitamin D could directly regulate the human inherent immunity and adaptive immunity, and which is closely related with respiratory infectious diseases, such as tuberculosis and CAP.[37] Vitamin D levels are significantly downregulated in critically ill patients with acute severe pneumonia or sepsis and are correlated with prognosis.[31,38] In case of pulmonary infection, the pulmonary endothelial cells can convert the inactive vitamin D into its active form, and stimulate the expression of antibacterial peptides, thereby resisting infection.[39] Moreover, vitamin D deficiency is directly correlated with lung function injuries and is one independent risk factor of pneumonia.[40] Thus, vitamin D level affects not only the occurrence of lung diseases, but also the severity of CAP. Supplement with vitamin D might be able to reduce the occurrence and the severity of CAP.
There have a few limitations in this study. First, different methods were used to assess vitamin D levels. Second, the relationships from this meta-analysis between vitamin D and CAP might be affected by confounding factors, such as race, age and body mass index. Third, only published articles were included. Finally, vitamin D levels are still affected by the unapproved immunomodulatory reference intervals, season, sunlight, and races. Thus, stricter and normalized double-blind large-size studies are still needed.
5. Conclusion
The evidence presented here indicates an association between VDD and an increased risk of CAP, as person with < 20 ng/mL serum vitamin D is under increased risk of CAP (OR = 1.64, 95%CI: 1.00, 2.67). However, more evidence is needed to better understand the effect of vitamin D on the CAP, and well-designed trails are required to determine the explicit effect of vitamin D supplementation. Therefore, people at risk of VDD and determining how to supplement vitamin D could be considered in the future.
Author contributions
Conceptualization: Yun-Fang Zhou.
Data curation: Yun-Fang Zhou, Lulu Qin, Bang-An Luo.
Formal analysis: Yun-Fang Zhou, Lulu Qin.
Investigation: Yun-Fang Zhou, Lulu Qin.
Methodology: Yun-Fang Zhou, Lulu Qin, Bang-An Luo.
Software: Yun-Fang Zhou, Lulu Qin.
Writing – original draft: Yun-Fang Zhou, Lulu Qin.
Writing – review & editing: Yun-Fang Zhou, Lulu Qin, Bang-An Luo.
Supplementary Material
Footnotes
Abbreviations: CAP = community-acquired pneumonia, CI = confidence intervals, MOOSE = Meta-analysis of Observational Studies in Epidemiology, OR = odds ratio, RTI = respiratory tract infection, SVDD = severe vitamin D deficiency, VDD = vitamin D deficiency, VDI = vitamin D insufficiency, VDR = vitamin D Receptor, WMD = weighted mean difference.
How to cite this article: Zhou YF, Luo BA, Qin LL. The association between vitamin d deficiency and community-acquired pneumonia. Medicine. 2019;98:38(e17252).
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].American Thoracic Society. Guidelines for the management of the adults with community-acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med 2001;163:1730. [DOI] [PubMed] [Google Scholar]
- [2].File TM, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med 2010;122:130–41. [DOI] [PubMed] [Google Scholar]
- [3].Adamuz J, Viasus D, Jimenez-Martinez E, et al. Incidence, timing and risk factors associated with 1-year mortality after hospitalization for community-acquired pneumonia. I Infect 2014;68:534–41. [DOI] [PubMed] [Google Scholar]
- [4].Remington LT, Sligl WI. Community-acquired pneumonia. Cun Opin Pulm Med 2014;20:215–24. [DOI] [PubMed] [Google Scholar]
- [5].Welte T, Torres A, Nathwani D. Clinical and economic burden of community -acquired pneumonia among adults in Europe. Thorax 2012;67:71–9. [DOI] [PubMed] [Google Scholar]
- [6].Trotter CL, Stuart JM, George R, et al. Increasing hospital admissions for pneumonia, England. Emerg Infect Dis 2008;14:727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Thiem U, Heppner HJ, Pientka L. Elderly patients with community-acquired pneumonia: optimal treatment strategies. Drugs Aging 2011;28:519–37. [DOI] [PubMed] [Google Scholar]
- [8].Zilberberg MD, Shon AF, Huang H, et al. Hospital days, hospitalization costs, and inpatient mortality among patients with mucormycotic: a retrospective analysis of US hospital discharge data. BMC Infect Dis 2014;14:310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gonzalez-Castillo J, Martin-Sanchez FJ, Llinares P, et al. () Guidelines for the management of community-acquired pneumonia in the elderly patient. Rev Esp Quimioter 2014;27:69–86. [PubMed] [Google Scholar]
- [10].Aranow C. Vitamin D and the immune system. J Investig Med 2011;59:881–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Laaksi I, Ruohola JP, Tuohimaa P, et al. An association of serum vitamin D concentrations < 40nmol/L with acute respiratory tract infection in young Finnish men. Am J Clin Nutr 2007;86:714–7. [DOI] [PubMed] [Google Scholar]
- [12].Berry DJ, Hesketh K, Power C, et al. Vitamin D status has a linear association with seasonal infections and lung function in British adults. Br J Nutr 2011;106:1433–40. [DOI] [PubMed] [Google Scholar]
- [13].Ginde AA, Mansbach JM, Camargo CA. Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med 2009;169:384–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Sabetta JR, DePetrillo P, Cipriani RJ. Serum 25-hydroxyvitamin D and the incidence of acute viral respiratory tract infections in healthy adults. PLoS One 2010;5:e11088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Belderbos ME, Houben ML, Wilbrink B, et al. Cord blood vitamin D deficiency is associated with respiratory syncytial virus bronchiolitis. Pediatrics 2011;127:e1513–20. [DOI] [PubMed] [Google Scholar]
- [16].Leow L, Simpson T, Cursons R, et al. Vitamin D, innate immunity and outcomes in community acquired pneumonia. Respirology 2011;16:611–6. [DOI] [PubMed] [Google Scholar]
- [17].Jovanovich AJ, Ginde AA, Holmen J, et al. Vitamin D level and risk of community-acquired pneumonia and sepsis. Nutrients 2014;6:2196–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Remmelts H, Spoorenberg S, Oosterheert J, et al. The role of vitamin D supplementation in the risk of developing pneumonia: three independent case-control studies. Thorax 2013;68:990–6. [DOI] [PubMed] [Google Scholar]
- [19].Genuis SJ, Schwalfenberg GK. Picking a bone with contemporary osteoporosis management: nutrient strategies to enhance skeletal integrity. Clin Nutr 2007;26:193–207. [DOI] [PubMed] [Google Scholar]
- [20].Khoo AL, Chai L, Koenen H, et al. Translating the role of vitamin D3 in infectious disease. Crit Rev Microbiol 2012;38:122–35. [DOI] [PubMed] [Google Scholar]
- [21].2000;Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of observational studies in epidemiology (moose) group JT JAMA. 283:2008–12. [DOI] [PubMed] [Google Scholar]
- [22].Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2011;96:1930–1930. [DOI] [PubMed] [Google Scholar]
- [23].Taggart DP, D’Amico R, Altman DG. Effect of arterial revascularisation on survival: a systematic review of studies comparing bilateral and single internal mammary arteries. Lancet 2001;358:870–5. [DOI] [PubMed] [Google Scholar]
- [24].Duckitt K, Harrington D. Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ (Clin Res Ed ) 2005;330:565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005;20:5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Oduwole AO, Renner JK, Disu E, et al. Relationship between vitamin D levels and outcome of pneumonia in children. West Afr J Med 2010;29:373–8. [DOI] [PubMed] [Google Scholar]
- [27].Aregbesola A, Voutilainen S, Nurmi T, et al. Serum 25-hydroxyvitamin D3 and the risk of pneumonia in an ageing general population. J Epidemiol Community Health 2013;6:533–6. [DOI] [PubMed] [Google Scholar]
- [28].Quraishi SA, Bittner EA, Christopher KB, et al. Vitamin D status and community-acquired pneumonia: results from the third national health and nutrition examination survey. PLoS One 2013;8:e81120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Jovanovich A, Ginde A, Holmen J, et al. Vitamin D level and risk of community-acquired pneumonia and sepsis. Nutrients 2014;6:2196–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Mamani M, Muceli N, Basir H, et al. Association between serum concentration of 25-hydroxyvitamin D and community-acquired pneumonia: a case-control study. Int J Gen Med 2017;10:423–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Lu D, Zhang J, Ma C, et al. Link between community-acquired pneumonia and vitamin D levels in older patients. Z Gerontol Geriatr 2017;12:1–5. [DOI] [PubMed] [Google Scholar]
- [32].Guo LY, Li W, Cheng XF, et al. Relationship between vitamin D status and viral pneumonia in children. Pediatr Allerg Immunol Pulmonol 2017;44:86–91. [Google Scholar]
- [33].Li W, Cheng X, Guo L, et al. Association between serum 25-hydroxyvitamin D concentration and pulmonary infection in children. Medicine (Baltimore) 2018;97:e9060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Mandell LA, Whitney CG. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007;44:S27–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Manaseki-Holland S, Qader G, et al. Effects of vitamin D supplementation to children diagnosed with pneumonia in Kabul: a randomized controlled trial. Trop Med Int Health 2010;15:1148–55. [DOI] [PubMed] [Google Scholar]
- [36].White JH. Vitamin D as an inducer of cathelicidin antimicrobial peptide expression: past, present and future. J Steroid Biochem Mol Biol 2010;121:234–8. [DOI] [PubMed] [Google Scholar]
- [37].Williams B, Williams AJ, Anderson ST. Vitamin D deficiency and insufficiency in children with tuberculosis. Pediatr Infect Dis J 2008;27:941–2. [DOI] [PubMed] [Google Scholar]
- [38].Pascale GD, Vallecoccia MS, Schiattarella A, et al. Clinical and microbiological outcome in septic patients with extremely low 5-hydroxyvitamin D levels at initiation of critical care. Clin Microbiol Infect 2016;22:e7–13. [DOI] [PubMed] [Google Scholar]
- [39].Gunville CF, Mourani PM, Ginde AA. The role vitamin D in prevention and treatment of infection. Inflamm Allergy Drug Targets 2013;12:239–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Lambert AA, Kirk GD, Astemborski J, et al. A cross sectional analysis of the role of the antimicrobial peptide cathelicidin in lung function impairment within the A-LIVE cohort. PLoS One 2014;9:e95099. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


