Abstract
Background:
Bleeding modifies the surgeon's view of the field during transsphenoidal endoscopic pituitary surgery. Since ventilation can alter venous return, we compared the effect of volume-controlled ventilation (VCV) and pressure-controlled ventilation (PCV) on intraoperative bleeding.
Methods:
Eighty-six patients were randomized to VCV or PCV in this single blinded study; comparisons concerned 42 in the PCV group and 43 in the VCV group.
Results:
Intraoperative bleeding, the primary endpoint, did not differ between groups whether analysis focused on 7 levels of the score, from minimal bleeding to bleeding with significant change in the conduct of surgical procedure (P = .89) or on a stratification into 3 categories, mild, moderate, and major (P = .47). Median [interquartile range] peak airway pressure was lower in the PCV group (13.5 [12.5–15] vs 16.3 [14.4–19.1] cm H2O, P < .001) while mean airway pressures were similar (P = .08). Means ± SD of tidal volumes were lower in the VCV group when expressed as absolute values (470.6 ± 84 vs 434.7 ± 71.7 ml, P = .05) or as tidal volume/theoretical ideal weight ratio (6.7 [6.5–7] vs 7.2 [6.9–7.9], P < .001). The 2 groups were similar for postoperative complications and number of patients cured.
Conclusion:
In conclusion, ventilation mode does not influence intraoperative bleeding during transsphenoidal pituitary surgery.
Trial registration:
Clinicaltrials.gov identifier: NCT01891838; July 3, 2013
Keywords: hemorrhage, pituitary adenoma, positive-pressure respiration
1. Introduction
Pituitary tumors which are mainly adenomas represent 10% to 15% of all intracranial tumors. These tumors can be revealed either by an evolutionary endocrine syndrome (secreting tumor) or by a tumor syndrome including visual disorders (compression of the optic chiasm). The surgical access is now routinely transsphenoidal endonasal endoscopic surgery. Complete resection is possible in 76% to 98% of patients depending on the size of the adenoma, with hormonal control at 3 months obtained in 66% to 100% of cases and a perioperative mortality near to zero.[1] The restricted surgical area, 2 to 4 cm2, explains why bleeding can blur the surgeon's vision and consequently impede the result of the procedure. In the absence of a mucosal or vascular burglary due to the rhino access or of an injury of a venous sinus explained by its anatomical proximity, increase in intra-thoracic pressure related to mechanical ventilation is often considered to be the cause of bleeding or at least as an aggravating factor.
Few authors have investigated the role of peak or mean pressure according to the modality of ventilation. The most commonly used ventilatory mode in the operating room is volume-controlled ventilation (VCV). Insufflation pressures generated by the ventilator depend on lung compliance and resistance in the airways and parenchyma. During the inspiratory time, the flow of insufflation is constant (square flow) and pressure in the airways increases gradually to the peak pressure then decreases to reach the plateau pressure before the beginning of the expiratory time. During pressure-controlled ventilation (PCV), the level of inspiratory pressure is set, and the tidal volume varies depending on thoracic characteristics. Contrary to VCV, insufflation decelerates to help maintain a constant pressure during the inspiratory time. This breathing pattern has been studied in several procedures during anesthesia, particularly during laparoscopic cholecystectomy,[2] laparoscopic interventions in obese patients,[3] gynecological laparoscopy,[4] and robot-assisted prostatectomy.[5] These studies show a lower peak pressure in PCV compared to VCV. A benefit on gas exchange does not appear to be significant in these studies, but PCV seems helpful to limit intrathoracic pressure. This decreasing pressure may favor venous drainage from the head – waterfall theory – and consequently could limit the risk of bleeding for “hydrostatic” reasons. Recently, Kang et al reported that PCV decreased intraoperative surgical bleeding in patients undergoing posterior lumbar interbody fusion and explained this result by a lower intraoperative peak inspiratory pressure.[6] The particularity of pituitary surgery is also the patient's positioning in a half-sitting position to ensure optimum jugular venous drainage (especially the cavernous sinus), and in the same way to potentially decrease airway pressure and induced bleeding.
The main objective of the study was to compare the quality of the vision of the operative field during the transsphenoidal approach depending on the ventilatory modality: VCV or PCV. We hypothesized that the intraoperative bleeding estimated by the operator would be lower using PCV because of lower airway pressure.
2. Methods
This prospective, single blinded, randomized, single-center study, was conducted in the Anesthesiology and Neurosurgery Departments of a University Hospital in accordance with the relevant guidelines (CONSORT Standard for RCT) and regulations.
2.1. Ethics
The study was approved by the Ethical Committee (Ile-de-France XI) and was registered on the international platform www.clinicaltrials.gov trials (NCT01891838; July 3, 2013).
2.2. Study population
Patients aged above 18 years and scheduled for an elective intervention on the pituitary gland, performed by transsphenoidal access were eligible. The exclusion criteria included an ongoing pregnancy, severe or morbid obesity defined by a body mass index (BMI) greater than 35 kg.m−2, a chronic respiratory disease (COPD, severe asthma…), a redo or emergent surgery and any constitutional or acquired (treatment) disorders of coagulation. Finally, patients were excluded from the analysis in case of withdrawal of consent, anesthetic or surgical complications except bleeding-related complications.
2.3. Randomization
Once the patient agreed to participate, a number was attributed corresponding to the acceptation range in the protocol. At the patient's entry in the operative room, the investigator scratched a corresponding card to know the technique of ventilation. These cards were previously prepared following a randomization list prepared by an independent statistician with 1:1 arm ratio (VCV or PCV group). Patients were distributed into a balanced block of either 4 or 6 patients and the sequence of the blocks was also randomized to prevent knowledge of previously attributed treatments. The patient and the surgeon were blinded to the modality of ventilation.
A non-respect of the arm of treatment or of the planned respiratory settings was considered as a major deviation from the protocol. Change of ventilation mode due to safety reason (hypoxemia or hypercarbia) was not considered as a major deviation and such case was analyzed in the original group of randomization (Intention to Treat analysis).
2.4. Protocol
Participation in the study was proposed by the surgeon and written informed consent was obtained during the preanesthetic consultation. On arrival in the operating room, randomization was performed before general induction.
Standard monitoring for both groups included electrocardiogram, non-invasive arterial blood pressure, pulse oximetry, capnography, inspiratory, and expiratory sevoflurane concentrations, and train of 4 monitoring (Anesthesia machine Aisys, Carescape Monitor B850, General Electric Healthcare, Chicago, Illinois, USA). General anesthesia was induced with sufentanil (0.2 to 0.3 mg/kg) and propofol (2.5 mg/kg) followed by atracurium (0.6 mg/kg). After intubation, anesthesia was maintained with sevoflurane and repeated boluses of sufentanil and of atracurium. The depth of anesthesia was adjusted to maintain the Bispectral index between 40 and 60 as recommended. Administration of atracurium was guided by neuromuscular monitoring to maintain the neuromuscular block constant all along the repair. Mechanical ventilation was performed with the workstation GE Healthcare Aisys CS2, operating in a closed circuit. In the VCV group, tidal volume was set at 7 ml kg−1 of theoretical ideal body weight, calculated using the Devine formula (for males: TIW = 50+2.3[height (inches)-60] and for females: TIW = 45.5 + 2.3 [height (inches)-60]). For the PCV group, the inspiratory pressure was initially set at 15 cm H2O and then modified to reach a tidal volume at 7 ml kg−1 of theoretical ideal weight. In both groups, end-expiratory positive pressure (PEEP) was zero and inspiratory-to-expiratory time (I:E) ratio was set to 1:2 while the fraction of inspired oxygen (FiO2) was maintained at 50%. Respiratory rate was the main acceptable variable with an initial rate at 12 cycles min−1 to reach an end-tidal carbon dioxide pressure between 35 and 40 mmHg. Mean arterial pressure was maintained above 65 mmHg throughout the procedure with the use of vasopressors (bolus of phenylephrine or continuous infusion of norepinephrine). Systolic arterial pressure above 140 mmHg was treated to avoid bleeding. Arterial blood gas monitoring was left to the discretion of the anesthesiologist. Neuromuscular blocking agents were systematically used to improve the condition of intubation and myorelaxation was continued during surgery to avoid any movement of the head. Monitoring of the neuromuscular block was performed with a piezoelectric sensor consisting of 2 quick-fit malleable plastic semicircular rings for the thumb and index finger with an interconnecting bending strip (General Electric Datex-Ohmeda, Helsinki, Finland).
The surgical management was exclusively performed by the same operator (SG) in the usual half-sitting position. The operator was kept blind to the ventilation mode and reported intensity of the intraoperative bleeding in a standardized manner. This position allows an enhanced exposure to the surgical field and reduces, combined with the absence of positive end-expiratory pressure, intra-thoracic pressure and central venous pressure. The neutral position of the head was carefully checked before starting surgery to avoid an elevation of the jugular vein pressure which may impact the bleeding.
After the end of surgery, the patient was immediately withdrawn from mechanical ventilation to be neurologically examined. Then, a stay in the post-anesthesia care unit (PACU) during the first night was planned with an hourly neurological assessment and detection of urinary retention or diabetes insipidus. Oral feeding was introduced at the 4th hour. Then on the following day, the patient came back to the neurosurgical department before leaving hospital.
2.5. Data collection
Demographic data were collected at inclusion and included: age, sex, American Society of Anesthesiologists classification, body mass index. All intraoperative monitoring variables (blood pressure, heart rate, pulse oximetry, ventilatory variables (tidal volume, ventilator frequency, peak, and mean airway pressures whatever the mode, partial tension of end-tidal carbon dioxide pressure) were collected using Centricity Anesthesia with one value per minute. This is an Anesthesia Information Management System which provides automated data collection and storage into a repository for subsequent exportation as an Excel file (GE Healthcare, Buc, France). In addition to that, number of alveolar recruitment maneuvers and a possible change in the ventilator modality were noticed.
At the end of the surgery, the neurosurgeon involved described the amount of bleeding using a 7-level score. Finally, postoperative data included pain assessment by nurses at admission to the Post-Anesthesia Care Unit (11-point Numerical Rating Scale where the end points are the extremes of no pain and worst pain), complications and the evolution of the primary disease (cured, sequelae) at month 3 according to imagery or biology.
2.6. Outcomes
The primary outcome was the intraoperative bleeding estimated by the operator on a 7-level score adapted from Boezaart et al who used it to describe surgical conditions during functional endoscopic sinus surgery.[7] Levels are minimal bleeding (level 1), low bleeding (level 3), bleeding with no significant change in the conduct of the surgical procedure (level 5), bleeding with significant change in the conduct of surgical procedure because it obscures the surgical vision of the operative field (level 7); intermediate levels were used to rate the levels of intermediate severity. The surgeon's estimation was also categorized into 3 groups: category 1 for mild bleeding including levels 1, 2, and 3; category 2 for moderate bleeding including levels 4 and 5, and Category 3 for major events grouping levels 6 and 7.
Secondary intraoperative outcomes were especially the conduct of ventilation (changes in ventilator settings necessary to maintain an end-tidal carbon dioxide pressure between 35 and 40 mmHg), risk of hypoxemia, and the intraoperative hemodynamic profile. Secondary postoperative outcomes included pain at admission to the Post-Anesthesia Care Unit measured by the nurse, complications and endocrine status at the 3rd postoperative month.
2.7. Statistical analysis
Calculation of the number of patients to be included in the study relied on the medical charts of patients having benefited from pituitary surgery in our institution during three months the year before the beginning the study. Operative reports were reviewed to estimate intraoperative bleeding using a 7-point scale (from 1 = minimal bleeding to 7 = heavy bleeding requiring corrective intervention). We anticipated that the experimental procedure would impact the highest three levels, which represented 15% of all cases. To be clinically relevant, a 50% improvement in the incidence of such cases was considered mandatory. These rates were introduced in a series of 20 simulations that allowed calculation of the expected differences and their standard deviations. With these figures, a sample size of 45 patients per group was found to achieve an 80% power at a bilateral .05 significance level.
Continuous variables were analyzed using Student t test (normal distribution) or the Mann–Whitney test (non-normal distribution). Categorical variables were analyzed using a chi-square test or Fisher exact test. Association between bleeding levels and ventilation type has also been estimated with proportional cumulative odds-ratio (OR) and [95% confidence intervals (CI)].
Data are expressed as the number of patients (percentages with 95% confidence interval) and means ± SD or medians [25 to 75%, interquartile range].
A P < .05 was considered statistically significant. All the analyses were performed with R software version 3.1.3. The datasets generated and analyzed during the current study are available in the Dryad repository.
3. Results
One hundred and 29 patients were eligible between July 2013 and March 2015. One hundred and one patients were approached and 86 who had given their written consent were randomized, 42 in the PCV group and 44 in the VCV group. The ventilation settings were changed in 1 patient in the VCV group to reach the objectives in terms of partial tension of end-tidal carbon dioxide but without adequate results; this patient was excluded from the study. Finally, comparisons concerned 42 in the PCV group and 43 in the VCV group (Fig. 1). Patient characteristics are presented in Table 1.
Figure 1.
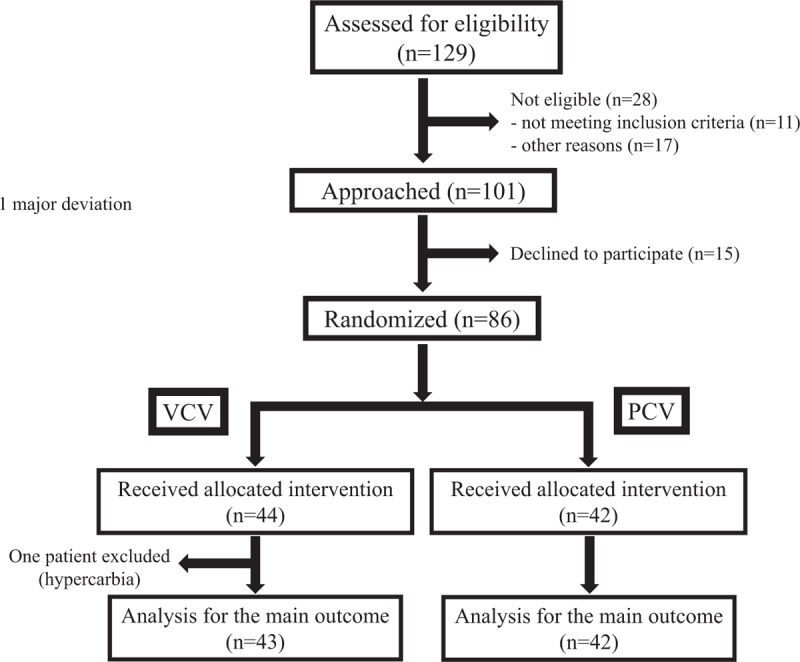
Consort flow. PCV = pressure-controlled ventilation, VCV = volume-controlled ventilation.
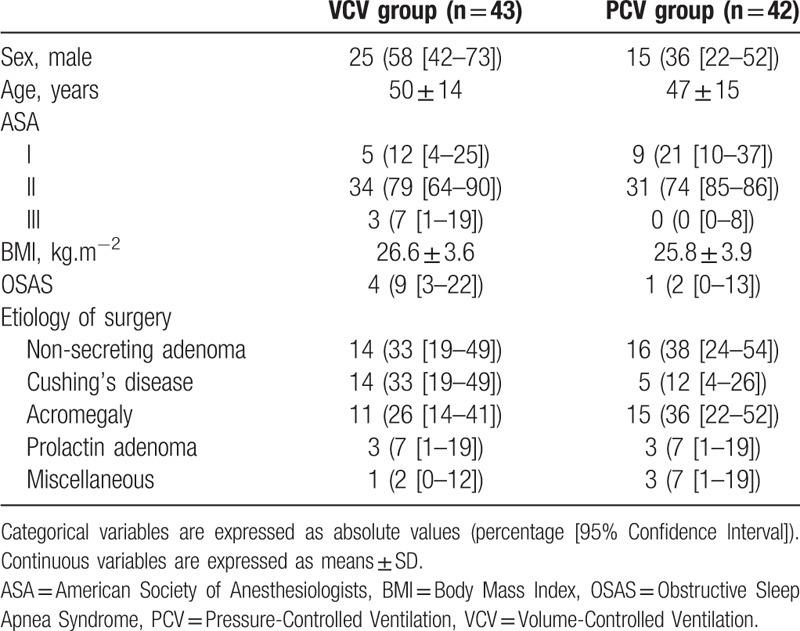
Table 1.
Characteristics of patients.
Intraoperative bleeding did not differ between the 2 groups whether statistical analysis focused on the seven levels of the score (P = .89; OR = 0.72 [0.34 – 1.54]) or on a stratification into 3 categories (P = .47; OR = 0.68 [0.31 – 1.51]) (Fig. 2). Sex, age, ASA class, BMI, and etiology of surgery did not emerge as factors influencing the level of intra-operative bleeding (P > .05 for each one).
Figure 2.
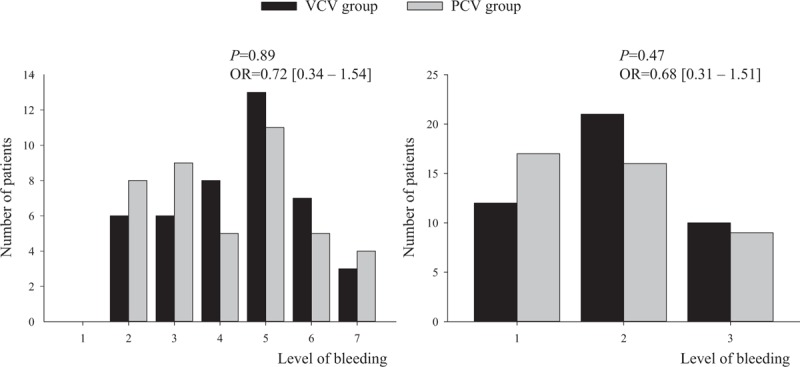
Intensity of intraoperative bleeding depending on the ventilation mode. In abscissa, the scale of bleeding. A: 7 levels from 1 (minimal bleeding) to 7 (heavy bleeding leading to a change in the surgery). B: 3 categories: category 1 (levels 1 + 2 + 3), category 2 (levels 4 + 5), category 3 (levels 6 + 7). P values and proportional cumulative OR (Odds ratio [95% Confidence Interval]) for the differences between the levels of bleeding.
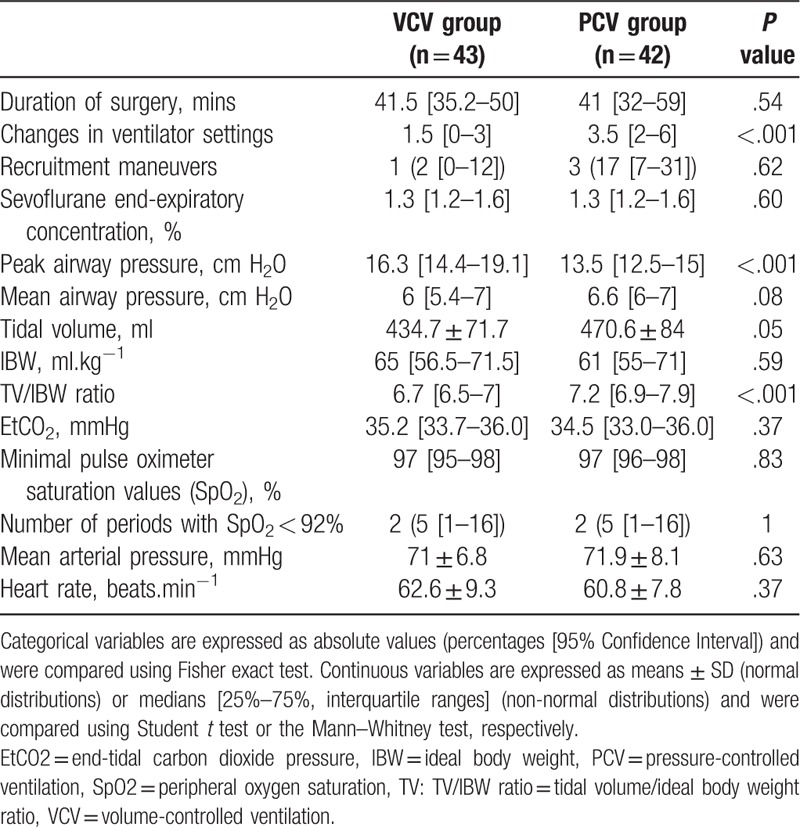
Intraoperative data are reported in Table 2. In the other hand, changes in ventilator settings were more frequent in the PCV group than in the VCV group (3.5 [2–5.8] and 1.5 [0–3] respectively; P < .001). Peak airway pressure was lower in the PCV group (P < .001) while mean airway pressures were similar in both groups (P = .08). Tidal volumes were lower in the VCV group when expressed as absolute values (P = .05) or as tidal volume / theoretical ideal weight ratio (P < .001) but similar partial tension of end-tidal carbon dioxide was measured in both groups (P = .37). Other intraoperative variables were also similar between groups especially mean arterial pressure (Table 2). No patient required blood transfusion.
Table 2.
Intraoperative data.
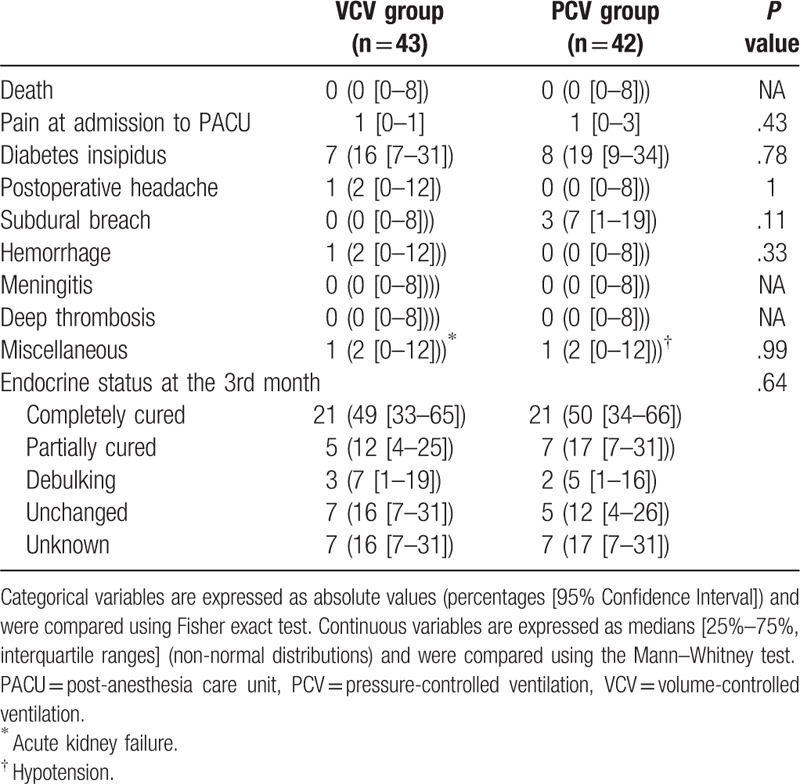
Occurrence of postoperative complications was similar between groups (Table 3). Most of the patients were completely or partially cured in both groups (Table 3). No relationship to intraoperative bleeding was detected.
Table 3.
Postoperative complications and evolution of the disease at the 3rd month.
4. Discussion
Our study did not show any difference in the intensity of bleeding during transsphenoidal endonasal endoscopic pituitary surgery whatever the ventilation mode (PCV or VCV) although peak airway pressure was slightly lower during PCV (around 3 cm H2O). One patient in the VCV group required a change in the ventilator modality to reach the objectives in terms of partial tension of end-tidal carbon dioxide and tidal volume. Changes in the ventilator settings were more frequent in the PCV group. Oxygenation and control of the mean arterial pressure were similar in both groups.
The possible relationship between intracranial surgery and intrathoracic pressure is an old concept and the present study did not find such a relationship with protective tidal volume whatever the modality of ventilation: pressure support or controlled volume. In fact, according to Poiseuille's law, venous return flow is determined by a pressure gradient (venous pressure minus right atrial pressure which varies in parallel with pleural pressure) divided by the venous vascular resistance.[8] In a patient breathing spontaneously, the pleural pressure is negative and its oscillation is transmitted to the right atrium increasing venous return. On the contrary, under mechanical ventilation, intrathoracic pressure is reversed with positive pressure ventilation all along the respiratory cycle and leads to an increase in right atrial pressure and to a decrease in venous return.[9] This response contributes to the decrease in cardiac output.[10] Van Den Berg et al showed that right atrial pressure increases proportionally to the pressure in the airways.[11] Reducing insufflation pressures could improve venous return and thus intraoperative bleeding. This relationship has been explored during ENT surgery because the consequence of bleeding, similar on visualization for the operator, is improved with reduced mean airway pressure.[12] The absence of measured difference between groups may be partially explained by the absence of difference in mean airway pressure in healthy lungs and it is possible that airway pressure is modified in the half-sitting position, due to the facilitated movement of the diaphragm. Moreover, the prescribed volume was respected and very close in both groups.
The median score of bleeding was rather high with 31 patients in the VCV group (72%) and 25 patients in the PCV group (59%) with a score >3. The surgeon declared significant bleeding in 10 patients in the VCV group (23%) and 9 patients in the PCV group (21%), which confirms that this problem requires special attention. The ventilation mode does not appear to have any impact on this event but other means can be involved including the half-sitting position promoting spontaneous venous drainage, slight flexion of the head with rotation to the right side avoiding jugular compression and deliberate hypotension.[13] Otherwise hypercapnia should be avoided during intracranial surgery because it can promote vasodilation and thus increase the cerebral blood flow.[14] In our study, partial tension of end-tidal carbon dioxide did not differ between the groups.
Our study has some strengths and some limitations. First, the operations were all performed by a single operator unaware of the group of ventilation, which is a strength of the study avoiding a risk of bias related to the surgery and assessment of the bleeding. We did not however precisely measure the intraoperative bleeding, the 2 main bleeding classes are easily reported by the surgeon and only these classes could be taken into account. Second, we did not classify our cases according to the parasitic spread of the tumor using the classification system proposed by Knosp et al[15] or its modified classification proposed by Micko et al.[16] Indeed, the evaluation of the invasion of the cavernous sinus should have been a parameter included in the analysis. Third, we did not apply positive end-expiratory pressure to prevent alveolar de-recruitment during expiration but a meta-analysis showed recently that the beneficial role of positive end-expiratory pressure to prevent postoperative mortality and respiratory complications exists at least among undifferentiated surgical patients.[17,18]
In conclusion, during transsphenoidal endonasal endoscopic pituitary surgery, bleeding frequently affects the quality of visualization of the operative field and may modify the expected repair. The modalities of mechanical ventilation (PCV or VCV) do not influence the bleeding despite a reduction of the peak airway pressure when using PCV. Given these results, other therapeutic measures should be considered to reduce bleeding and improve the operating conditions.
Acknowledgments
The authors acknowledge Polly Gobin for her linguistic help.
Author contributions
Conceptualization: Morgan Le Guen, Alexis Paternot, Stephan Gaillard, Marc Fischler.
Data curation: Morgan Le Guen, Alexis Paternot, Agnes Declerck, Elodie Feliot, Etienne Gayat, Stephan Gaillard.
Formal analysis: Elodie Feliot, Etienne Gayat.
Investigation: Morgan Le Guen, Alexis Paternot, Agnes Declerck.
Methodology: Morgan Le Guen, Marc Fischler.
Project administration: Marc Fischler.
Validation: Morgan Le Guen.
Writing – original draft: Morgan Le Guen, Alexis Paternot, Agnes Declerck, Elodie Feliot, Etienne Gayat, Stephan Gaillard, Marc Fischler.
Writing – review & editing: Morgan Le Guen, Alexis Paternot, Agnes Declerck, Elodie Feliot, Etienne Gayat, Stephan Gaillard, Marc Fischler.
Marc Fischler orcid: 0000-0003-0729-5430.
Footnotes
Abbreviations: BMI = body mass index, PCV = pressure-controlled ventilation, TIW = theoretical ideal body weight, VCV = volume-controlled ventilation.
How to cite this article: Le Guen M, Paternot A, Declerck A, Feliot E, Gayat E, Gaillard S, Fischler M. Impact of the modality of mechanical ventilation on bleeding during pituitary surgery. Medicine. 2019;98:38(e17254).
Institutional Funding by Foch Hospital (no role in the study design, study execution, and study analysis)
The authors have no conflicts of interests to disclose.
References
- [1].Wang F, Zhou T, Wei S, et al. Endoscopic endonasal transsphenoidal surgery of 1,166 pituitary adenomas. Surg Endosc 2015;29:1270–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Tyagi A, Kumar R, Sethi AK, et al. A comparison of pressure-controlled and volume-controlled ventilation for laparoscopic cholecystectomy. Anaesthesia 2011;66:503–8. [DOI] [PubMed] [Google Scholar]
- [3].Cadi P, Guenoun T, Journois D, et al. Pressure-controlled ventilation improves oxygenation during laparoscopic obesity surgery compared with volume-controlled ventilation. Br J Anaesth 2008;100:709–16. [DOI] [PubMed] [Google Scholar]
- [4].Jeon WJ, Cho SY, Bang MR, et al. Comparison of volume-controlled and pressure-controlled ventilation using a laryngeal mask airway during gynecological laparoscopy. Korean J Anesthesiol 2011;60:167–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Choi EM, Na S, Choi SH, et al. Comparison of volume-controlled and pressure-controlled ventilation in steep Trendelenburg position for robot-assisted laparoscopic radical prostatectomy. J Clin Anesth 2011;23:183–8. [DOI] [PubMed] [Google Scholar]
- [6].Kang WS, Oh CS, Kwon WK, et al. Effect of mechanical ventilation mode type on intra- and postoperative blood loss in patients undergoing posterior lumbar interbody fusion surgery: a randomized controlled trial. Anesthesiology 2016;125:115–23. [DOI] [PubMed] [Google Scholar]
- [7].Boezaart AP, van der Merwe J, Coetzee A. Comparison of sodium nitroprusside- and esmolol-induced controlled hypotension for functional endoscopic sinus surgery. Can J Anaesth 1995;42:373–6. [DOI] [PubMed] [Google Scholar]
- [8].Guyton AC, Polizo D, Armstrong GG. Mean circulatory filling pressure measured immediately after cessation of heart pumping. Am J Physiol 1954;179:261–7. [DOI] [PubMed] [Google Scholar]
- [9].Chihara E, Hashimoto S, Kinoshita T, et al. Elevated mean systemic filling pressure due to intermittent positive-pressure ventilation. Am J Physiol 1992;262:H1116–21. [DOI] [PubMed] [Google Scholar]
- [10].Cournand A, Motley HL, Werko L, et al. Physiological studies of the effects of intermittent positive pressure breathing on cardiac output in man. Am J Physiol 1948;152:162–74. [DOI] [PubMed] [Google Scholar]
- [11].van den Berg PC, Jansen JR, Pinsky MR. Effect of positive pressure on venous return in volume-loaded cardiac surgical patients. J Appl Physiol 19852002;92:1223–31. [DOI] [PubMed] [Google Scholar]
- [12].Gilbey P, Kukuev Y, Samet A, et al. The quality of the surgical field during functional endoscopic sinus surgery–the effect of the mode of ventilation–a randomized, prospective, double-blind study. Laryngoscope 2009;119:2449–53. [DOI] [PubMed] [Google Scholar]
- [13].Boonmak P, Boonmak S, Laopaiboon M. Deliberate hypotension with propofol under anaesthesia for functional endoscopic sinus surgery (FESS). Cochrane Database Syst Rev 2016;10:Cd006623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Fortune JB, Feustel PJ, deLuna C, et al. Cerebral blood flow and blood volume in response to O2 and CO2 changes in normal humans. J Trauma 1995;39:463–71. [DOI] [PubMed] [Google Scholar]
- [15].Knosp E, Steiner E, Kitz K, et al. Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 1993;33:610–7. [DOI] [PubMed] [Google Scholar]
- [16].Micko AS, Wohrer A, Wolfsberger S, et al. Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J Neurosurg 2015;122:803–11. [DOI] [PubMed] [Google Scholar]
- [17].Barbosa FT, Castro AA, de Sousa-Rodrigues CF. Positive end-expiratory pressure (PEEP) during anaesthesia for prevention of mortality and postoperative pulmonary complications. Cochrane Database Syst Rev 2014;CD007922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].McGuire G, Crossley D, Richards J, et al. Effects of varying levels of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure. Crit Care Med 1997;25:1059–62. [DOI] [PubMed] [Google Scholar]


