Abstract
Background:
Despite the high prevalence of tobacco use during pregnancy among Alaska Native and American Indian (AI/AN) women, few efforts have focused on developing tobacco cessation interventions for this group. This paper describes development of messaging for a social media campaign targeting the entire community to reduce tobacco use in pregnancy (cigarette smoking and smokeless tobacco use including a homemade product known as Iqmik) among AN women, as part of a multi-component intervention.
Method:
The study (clinical trial registration #NCT02083081) used mixed methods with two rounds of assessments to develop and refine culturally relevant message appeals. Round 1 used qualitative focus groups and individual interviews (N=60), and Round 2 used quantitative survey interviews (N=52). Each round purposively sampled adult AN pregnant women, family/friends, and Elders in Western Alaska, and included tobacco users and non-users. Round 1 also assessed reasons for tobacco use in pregnancy.
Results:
Qualitative findings generally converged with quantitative results to indicate that many participants preferred factual, loss-framed, visual concepts on how maternal tobacco use harms the fetus, newborn, and child; in contrast to spiritual or emotional appeals, or gain-framed messaging. Stress was indicated as a major reason for tobacco use in pregnancy and strategies to manage stress along with other health pregnancy targets (e.g., prenatal care) were suggested.
Conclusions:
This preliminary study suggests campaign messages targeting the entire community to reduce tobacco use in pregnancy among rural AN women should include factual messaging for being tobacco-free as well as focus on reducing stress and other healthy pregnancy targets.
Keywords: tobacco, messaging, health communication, intervention, Alaska Natives, pregnancy
Introduction
Tobacco use during pregnancy is a major public health problem in the U.S [1, 2]. In 2010, data from the Pregnancy Risk Assessment Monitoring System (PRAMS) indicated 11% of women reported smoking during the last three months of pregnancy [3]. At 26%, American Indian/Alaska Native (AI/AN) (26%) females had the highest smoking prevalence during pregnancy. Adverse effects of cigarette smoking during pregnancy on maternal, fetal, and infant health are well documented [4, 5, 6]. Less than 1% of women worldwide use smokeless tobacco (ST) during pregnancy with its use higher among indigenous females [7]. Maternal ST use is associated with increased risk for preterm birth, stillbirth, and infant low birth weight [8]. Despite substantial progress in developing evidence-based behavioral interventions for diverse groups of pregnant cigarette smokers [9, 10], little research has focused on AI/AN females or those using ST [11].
Among AN women residing in the Yukon-Kuskokwim (Y-K) Delta region of southwest AK, 26% reported cigarette smoking and 42% reported ST use during pregnancy [12, 13]. The ST used in this region is primarily a homemade product known as Iqmik, a mixture of fungus ash and tobacco leaves [14]. Nicotine absorption is greatly enhanced by the ash, which increases the pH, thereby increasing the bioavailability of unionized nicotine in the product [15]. Although previous studies document there is no ceremonial use for tobacco in any form among AN people, Iqmik is considered a ‘natural’ product and thus perceived by some as safer to use during pregnancy compared to other tobacco products [15].
Our prior study conducted with Y-K Delta pregnant AN women evaluated an individual-based, culturally adapted tobacco (cigarettes and ST) cessation intervention with messaging content focused on pregnant women only [16]. The intervention had low reach to pregnant women and was not effective for tobacco cessation. These findings led us to consider a multi-level intervention targeting the entire community, not just pregnant women, to change social norms about tobacco use in pregnancy [17, 18]. Consistent with a social-ecological approach [19], the multi-component intervention consists of a community-wide social marketing campaign as well as individual peer-based counseling delivered by local female role models called ‘Native Sisters’ [20]. The current paper describes how the messaging for the social media campaign was developed and refined using mixed methods formative work. Subsequent papers will report results from: (1) the development of the peer-based individual counseling components, and (2) intervention efficacy outcomes from an ongoing group randomized trial.
Factual-based and culturally-specific messaging has potential for developing AN community level interventions to reduce tobacco use during pregnancy [21, 22]. In a qualitative study to develop a biomarker feedback prenatal smoking cessation intervention [23], AN women and their partners/family members preferred factual messaging illustrating the link between neonatal NNAL (a tobacco-specific nitrosamine and carcinogen) and adverse effects on the baby. The current investigation considers messaging directed not only to pregnant women but all community members.
Methods
This study extended a long-standing research partnership between [authors] and the [authors]. The [authors] institutional review boards, and the [authors] human studies committee and board of directors approved the study. The study was registered with clinicaltrials.gov (NCT02083081). Participant enrollment and data collection occurred between June 2014 and February 2015; data were analyzed 2015-16.
Study setting
The Y-K Delta region is located approximately 400 air miles from Anchorage, with a population of about 25,000. It comprises 58 tribes from 47 village locations ranging from 28 to 1,133 people. Bethel (population 6,000) is the hub for the 47 village locations. Residents are primarily of Yupik, Cupik, or Athabascan ethnicity, and are fairly homogeneous with respect to culture and language. The population is of low socio-economic status and most maintain a subsistence lifestyle [24]. No roads connect any of the villages; residents travel by small plane, boat, or snow machine. A typical village has a K-12 school, a local village council, health clinic, store, post office, and church.
The [authors] hospital, owned and operated by the [authors], is located in Bethel and provides health care for regional residents. Prenatal care visits are scheduled at village clinics and at the [authors] hospital (96% of women receive prenatal care) including a visit at week 36 gestation. Around this time, women from all villages stay at the Bethel pre-maternal home until delivery. There is an average of over 600 births each year to Y-K Delta women. [Authors] leaders and providers, as well as a community needs assessment, prioritized research focused on interventions to reduce tobacco use during pregnancy. This is consistent with the cultural value emphasizing the health and welfare of children as paramount [15].
Community advisory board (CAB)
The study is guided by a project-specific CAB comprised of 10 professional and community members. Members provided guidance on study design, recruitment methods and materials, message concepts, and interview content and wording through email and seven in-person meetings held in Bethel. At each meeting, lunch was provided and members received an honorarium.
Health communication framework
The study used two frameworks to address cultural influences in designing messages: the cultural variance framework [25] and the surface/deep structure framework [26]. The cultural variance framework considers cultural influences on health behavior including identity affiliations (e.g., traditional lifestyle) and cultural attributes such as specific beliefs, norms (e.g., communication styles), and values (e.g., relationship orientation) [27, 28]. Surface and deep structure informed both content and message format. Surface structure involves matching materials and messages to observable social and behavioral characteristics familiar to the target audience (e.g., AN people and the tundra). It also involves identifying appropriate message delivery channels and settings. The second dimension, deep structure, incorporates cultural beliefs and values. Appropriate surface structure generally increases receptivity, comprehension, and acceptance of messages, whereas appropriate deep structure conveys salience.
Another consideration was message framing [29]. Test concepts were designed to provide information on the harms of tobacco use for mother and baby outcomes while either: (1) raising expectations of a healthier baby resulting from cessation or staying tobacco-free (gain-framed) or (2) raising expectations of adverse consequences to the infant of tobacco use (loss-framed).
Media development plan and channels of communication
Media partners included Northwest Strategies, Inc. an AN-owned graphics design company based in Anchorage; and nDigidreams, Inc., an indigenous focused production company [30]. Large media (e.g., radio, television, and newspapers) serve all village locations in this region; therefore, it was not possible to manipulate mass media channels for evaluation of the intervention using a randomized design. However, if successful, the program could be disseminated through these venues. Thus, the campaign was designed to include small media: DVD-based digital stories, posters, brochures, postcards, flyers, and promotional items displayed or distributed in villages by the Native Sisters along with community presentations.
Study design
Based on recommendations for developing health communications [31], this descriptive study used two rounds of assessments to develop and refine campaign messages. Round 1 utilized qualitative methods to understand perceptions and preferences to develop concepts. Round 2 used quantitative surveys with a different sample of participants to pre-test campaign message concepts and promotional materials developed from the qualitative work. In addition to pregnant women, both rounds sampled family members and Elders to learn from those who could influence and support women to use or not use tobacco. This approach was important because the campaign targeted the entire community, not only pregnant women.
Participants
Both rounds utilized a stratified purposeful sample [32] with key audience segments (pregnant women, family members, Elders), gender, and current tobacco use status (see Table 1). We targeted pregnant women tobacco users as well as nonusers to focus the campaign messages on both cessation and prevention (i.e., to reinforce abstinence during pregnancy and postpartum). The targeted sample for each round included 50 participants: 20 pregnant women, 20 spouse/family members, and 10 Elders. At least 10-15 interviews were estimated per strata before reaching data saturation, whereby no new information is being learned [33]. [Table 1 near here]
Table 1.
Sample composition among Y-K Delta Alaska Native participants in qualitative and quantitative work to develop a social marketing campaign to reduce tobacco use in pregnancy
| Sample composition* | Round 1 Qualitative work (N=60) n | Round 2 Quantitative surveys (N=52) n |
|---|---|---|
| Pregnant women | ||
| Tobacco user | 10 | 10 |
| Non-tobacco user | 13 | 10 |
| Family members/friends | ||
| Female tobacco user | 5 | 6 |
| Female non-tobacco user | 11 | 5 |
| Male tobacco user | 7 | 7 |
| Male non-tobacco user | 3 | 3 |
| Elders | ||
| Female tobacco user | 4 | 3 |
| Female non-tobacco user | 2 | 2 |
| Male tobacco user | 1 | 3 |
| Male non-tobacco user | 4 | 3 |
Tobacco users were defined as use of any form of tobacco at least once in the past 7 days.
Recruitment flyers were posted in Bethel at grocery stores, restaurants, the hospital, pre-maternal home, and other locations. The study was also advertised in regionally-specific newspapers ‘Tundra Drums’ and ‘Delta Discovery,’ the one local radio station (KYUK), Facebook, the [author’s] employee website and weekly bulletin, as well as by word of mouth. A recruitment booth was also established at the hospital.
Recruitment materials described the study as involving a discussion about healthy pregnancies. Study staff conducted a brief screening in person or by phone to assess eligibility criteria: (1) AN person, (2) >18 years of age, and (3) provided written informed consent. Family/friends were people who knew a pregnant woman. An Elder was someone > 55 years of age and/or selected by study staff or CAB members based their standing in the community. Individuals participating in Round 1 were not eligible to participate in Round 2.
Procedures
Round 1
A semi-structured moderator guide was developed, pre-tested, and revised prior to use. Topics were: (1) Reasons for Tobacco Use during Pregnancy: cultural beliefs, perceived benefits, perceived health risks, differences for continuing use versus starting to use during pregnancy; (2) Role of Family/Community Members: persons influencing pregnant women’s tobacco use and other health decisions; and (3) Culturally Relevant Campaign Messaging, Delivery Channels, and Promotional Items: Six different posters were designed to show participants that represented spiritual, emotional, and factual appeals for tobacco-free pregnancies. Within each appeal type, both a gain and loss-framed message was represented, for a total of six concepts. Each concept was shown on mood boards with varying color schemes. Figure 1a-c presents three of the six concepts. [Figure 1a-c near here]
Figure 1a-c.
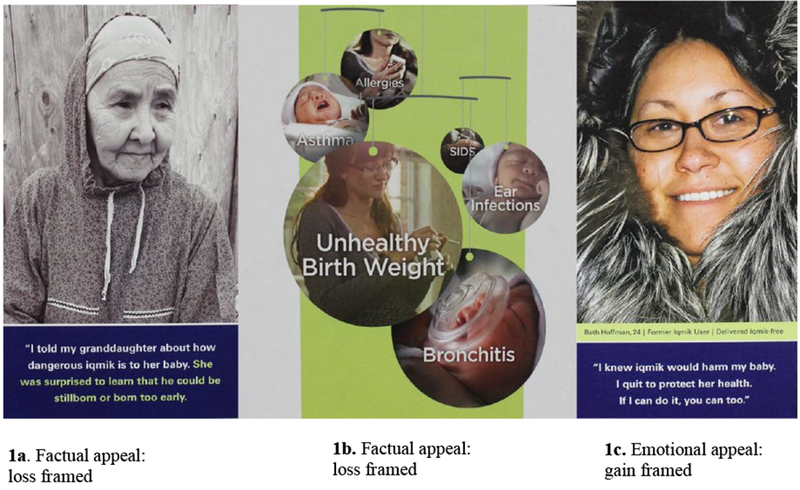
Examples of posters shown to Y-K Delta participants in Round 1 qualitative work.
The study planned to use focus groups with eight participants each to discuss community norms, i.e., shared cultural meanings, to inform the deeper structure. However, it was not feasible to recruit this number for focus groups due to scheduling barriers and difficulty recruiting non-tobacco users. Therefore, individual interviews or smaller focus groups were conducted as needed.
Sessions were held in a private room at the pre-maternal home or [author]. Prior to commencing the session, study staff individually assessed participant socio-demographics and tobacco use. Focus groups lasted about 90 minutes and individual interviews about 40 minutes. Each session was moderated by a study coordinator who received training in Bethel by the [authors] including four hours of didactic instruction followed by four practice hours of mock interviews and a certified completion interview [33]. A representative from Northwest Strategies attended some of the focus groups. All sessions were audiotaped and attended by a trained study observer who took detailed notes. Sessions were conducted in English but a translator was available for participants speaking the Yupik language. Each participant received a $75 gift card as a thank you for their time and a taxi voucher if requested. After each session, the moderator and observers summarized and documented emerging themes to facilitate analysis [34].
Round 2
Based on qualitative findings, three tri-fold brochures were designed for pre-testing: 1 factual, loss-framed appeal illustrating the negative impact of maternal tobacco use along the progression from the fetus in the womb through adulthood, 1 spiritual/cultural, gain-framed appeal, and 1 emotional, gain-framed appeal, being tobacco-free for sake of future generations (see Figure 2a-c). Brochures were written in English at the 5th grade reading level using readability analysis software. All 3 concepts had a similar color scheme incorporating shades of brown, maroon and yellow; these were based on participant color preferences from Round 1. All brochures included identical information on other healthy pregnancy targets such as managing stress. [Figure 2a-c near here]Individual interviews averaging 20.7 minutes (SD=9.4, range 10-60) were conducted privately in English by trained study staff. Participants were mailed (postal or email) the three concepts for review in advance. In addition to basic socio-demographic and tobacco use information, participants were asked seven items to assess perceived effectiveness [31] for each of the three brochures. Participants were shown the 3 brochures during the interview in the following order: (1) factual, (2) spiritual, and (3) emotional appeal and asked to rate each concept’s ability to: (1) attract attention, (2) convey its main point, (3) create a positive response, (4) promote salience, and (5) be culturally relevant, with response options very much, a little, or not at all. In addition, participants were asked after viewing each brochure: (6) the likelihood of quitting tobacco or telling someone else to quit, with response options very likely, somewhat likely, or not at all likely; and (7) if they were inspired to quit or would tell someone else to quit or not start using tobacco, with response options yes or no. Participants were then asked to indicate which concept they liked best and least. Next, participants were read a list of six promotional items and asked which item they liked best: berry picking bucket, baby items (e.g., onesies, bibs, blankets), t-shirt, water bottle, hoodie, or pen. Each participant received a $25 gift card as a thank you for their time and a taxi voucher if requested.
Figure 2a-c.
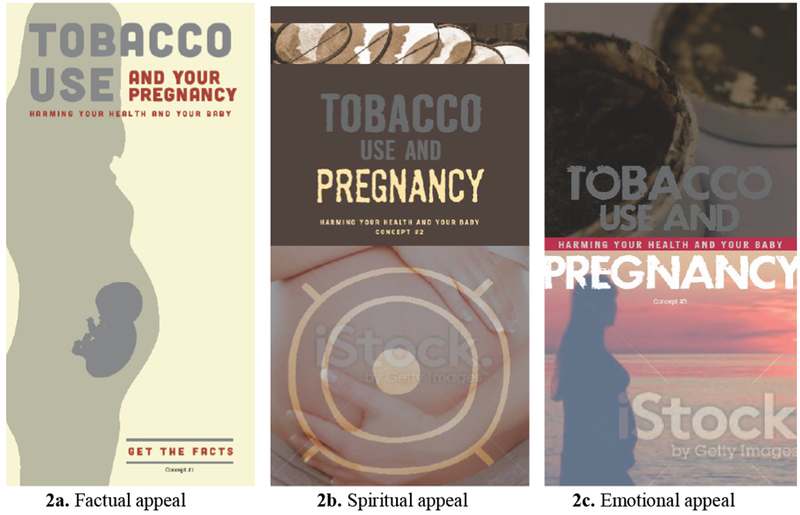
The cover of each of three tri-fold brochures (concepts) shown to Y-K Delta participants in Round 2 individual quantitative survey interviews.
Data analyses
Round 1
Sample characteristics were summarized using descriptive statistics. De-identified recordings were transcribed including statements in Yupik. A random sample of 25% of interviews was checked against transcripts for accuracy. Content analysis [35] supplemented by QSR NVivo software, version 10 (Doncaster, Victoria, Australia) was used to generate response themes. Codes and categories were developed based on topics in the moderator guide and then refined to incorporate themes emerging from the data. Two co-authors coded responses independently based on emergent themes for each topic area (95% inter-rater agreement). Coding discrepancies were resolved through discussion with a third co-author until consensus was reached.
Round 2
Sample characteristics and perceived effectiveness items were summarized using descriptive statistics including means, percentages, and frequencies. For perceived effectiveness items participants were asked to rate all three brochures and thus statistical tests were not performed because the concepts (brochures) were not independent groups. We used the Chi-square goodness of fit test to analyze the message concept most and least preferred by participants. We used the Chi-square test to examine the association of select participant characteristics (audience segment, gender, current tobacco use, and traditional lifestyle) with preferred message concept.
Results
Round 1
Participants
Recruitment and data collection occurred between June-October, 2014. Eighty-eight persons were screened, of which 63 (72%) were eligible and provided written informed consent. Of these, 60 showed for the focus group/interview. Eight focus groups were conducted comprising 2-8 participants each (n=25) and 35 individual interviews were conducted. Data saturation was reached with 60 participants. Table 2 provides sample characteristics; the mean age was 35 years, 75% were female, and 45% were current tobacco users. [Table 2 near here]
Table 2.
Socio-demographic and tobacco use characteristics among Y-K Delta Alaska Native participants in qualitative and quantitative work to develop a social marketing campaign to reduce tobacco use in pregnancy
| Characteristic | Round 1 Qualitative work (N=60) n (%) | Round 2 Quantitative surveys (N=52) n (%) |
|---|---|---|
| Audience segment | ||
| Pregnant women | 23 (38) | 20 (39) |
| Family members/friends | 26 (43) | 21 (40) |
| Elders | 11 (18) | 11 (21) |
| Female gender | 45 (75) | 36 (69) |
| Ethnicity | ||
| Yupik | 54 (90) | 46 (88) |
| Cupik | 4 (7) | 5 (10) |
| Inupiat | 2 (3) | 1 (2) |
| Age, mean (SD) | 34.6 (17.0) | 39.6 (17.3) |
| Range | 18-80 | 19-78 |
| Education | ||
| Less than high school | 8 (13) | 11 (21) |
| High school/GED degree | 25 (42) | 27 (52) |
| Some college/college degree | 27 (45) | 14 (27) |
| Employed | 30 (50) | 21 (40) |
| Married/living with partner | 40 (67) | 31 (60) |
| Language spoken | ||
| Yupik | 36 (60) | 36 (69) |
| Cupik | 4 (7) | 3 (6) |
| English | 60 (100) | 52 (100) |
| Language read/write | ||
| Yupik | 30 (50) | 22 (42) |
| Cupik | 3 (5) | 3 (6) |
| English | 60 (100) | 52 (100) |
| Follows traditional Native way of life | ||
| Not at all | 4 (7) | 1 (2) |
| Some | 22 (37) | 23 (44) |
| A lot | 28 (47) | 28 (54) |
| Missing | 6 (10) | 0 (0) |
| Use traditional medicine (e.g., herbs, teas, salves) | ||
| Not at all | 15 (25) | 6 (11) |
| Some | 40 (67) | 31 (60) |
| A lot | 5 (8) | 15 (29) |
| Current tobacco user (past 7 days) | 27 (45) | 29 (56) |
| Types of tobacco used (of current users) | n=27 | n=29 |
| Iqmik | 15 (56) | 18 (62) |
| Copenhagen or other chew | 3 (11) | 1 (3) |
| Cigarettes | 14 (52) | 13 (45) |
| E-cigarettes | 0 (0) | 0 (0) |
| Planning to quit next 30 days (of current users) | n=27 | n=29 |
| 15 (56) | 19 (65) | |
| Spouse/partner uses tobacco ( of those with a spouse/partner) | n=40 | n=31 |
| 25 (62) | 22 (71) | |
| Pregnant women only | n=23 | n=20 |
| First pregnancy | 5 (22) | 5 (25) |
| Week gestation, mean (SD) | 32.7 (7.1) | 28.4 (10.6) |
| Range | 10-40 | 9-41 |
| Family members/friends only | n=26 | n=21 |
| Relationship with a pregnant woman | ||
| Friend | 3 (11) | 6 (29) |
| Niece | 4 (15) | 4 (19) |
| Sister | 3 (11) | 4 (19) |
| Spouse/partner | 4 (15) | 3 (14) |
| Daughter | 2 (8) | 3 (14) |
| Cousin | 9 (35) | 1 (5) |
| Missing | 1 (4) | 0 (0) |
| Pregnant woman uses tobacco | 14 (54) | 14 (67) |
Percentages do not add to 100% due to rounding and also for types of tobacco-possibility of more than one type of tobacco used.
Qualitative themes
Except where noted, results are presented for the entire sample because themes were consistent across major subgroups (strata) of interest. Overall, tobacco use during pregnancy is a top concern; only use of alcohol and drugs was felt to be more important for the health of both mothers and babies. Other common responses were getting adequate prenatal care and maternal stress.
1. Stress is a major reason for tobacco use during pregnancy.
Stress during pregnancy was indicated as a common concern and considered the main reason for tobacco use. Other reasons included: negative affect (depression, anxiety, and anger), boredom, a way to avoid alcohol use, constant exposure to tobacco users, and tobacco addiction.
‘Stress and depression have been my weaknesses to stop smoking.’ (Pregnant Woman - Tobacco User)
Most participants believed high rates of Iqmik use during pregnancy were due to perceptions that it is safer than other forms of tobacco. However, regardless of their own tobacco use status, the majority of participants thought women should not use Iqmik or other tobacco products during pregnancy. Other reasons Iqmik is used include: addiction, a way to fit in socially with other users, and perceived stigma associated with cigarette smoking. In contrast, women can hide their Iqmik and they are not judged for using it. No clear generational or cultural reasons to use Iqmik or other tobacco products in pregnancy emerged.
2. Healthy pregnancies include being tobacco-free and other wellness behaviors.
In addition to being tobacco-free, aspects of a healthy pregnancy mentioned included lowering and managing stress, managing depression, getting enough rest and exercise, eating healthy, as well as attending prenatal appointments and learning about breastfeeding. All participants thought a focus on health and wellness, including positive cultural activities during pregnancy, would resonate with the community.
3. Support from others is important for pregnant women to be tobacco-free and manage stress.
Many participants believed the most important things women deal with during pregnancy were not using tobacco, alcohol, or drugs, in part due to difficulty stopping their use. Most participants felt comfortable sharing their concerns with a pregnant woman but others said it would depend on their relationship with the woman. The need for social support from the baby’s father along with family and friends was perceived by most participants as important to help women stay tobacco-free. For those deciding to quit, asking others to not use when around her, keeping busy with sewing and beading, and avoiding stress by getting help from others was important. Most female participants who had quit tobacco during pregnancy did so for their child and emphasized that support from others was essential in managing stress.
‘…talk to somebody when they have…when they have stress. Tell about your problem, problems with somebody that you…you trust and know very well. And get it out of your system.’ (Elder – Male – Non-Tobacco User)
4. The pregnant woman’s mother, Elders, and her immediate family are most credible and influential.
The pregnant woman’s mother, along with Elders and the community at large were mentioned by most participants as being influential and credible to advise women during their pregnancy. ‘I see my mom as a role model. She didn’t use tobacco. She talked to me growing up and telling me it’s bad for mom and baby. (Pregnant woman - Non-Tobacco User)
The woman’s spouse/partner and immediate family were mentioned as other sources of support. Not using or sharing tobacco with a pregnant woman was the primary way of showing support. Additionally, listening if she needs to talk, promoting non-tobacco use in the community, and taking part in healthy activities with a pregnant woman were perceived as supportive.
5. Graphic, factual-based messaging is preferred to convey the harms of using tobacco during pregnancy.
Most participants preferred factual messaging that was shocking and/or showed graphic visual harmful effects of maternal tobacco use on the baby. This strategy was viewed as more effective than spiritual/cultural or emotional appeals (e.g., quitting tobacco for future generations).
‘Like I said, I like hard facts, and I think those are more – most effective.’ (Male - Spouse - Former Tobacco User)
People liked the factual, loss-framed message concept shown in Figure 1a because it was thought that more Elders needed to pass along these types of messages. They also liked that the Elder was advising and not ‘scolding,’ while still conveying factual information. Participants thought the poster with this message would make them think about quitting tobacco, and emotional reactions were generated. Participants thought people who saw this poster would be inspired to share the negative effects of tobacco use on the fetus with pregnant women but suggested a more graphic image of what can actually happen to the baby.
‘It’s sad. I just saw them standing by a grave, and I don’t like this. I was thinking there – it would be more powerful if they were by a grave and she was saying that, if you keep using Iqmik, that he could be stillborn or born too early.’ (Family – Female – Non-Tobacco User)
Accordingly, the loss-framed, factual concept shown in Figure 1b was viewed as the most powerful and effective message. This is because pictures showing what can happen to the baby were taken much more seriously than someone simply telling them what could happen. Emotional reactions to this poster were generated, especially among pregnant women, whether participants used tobacco or not.
‘See, this is – this is hard, but it’s – it’ll grab people’s attention. They’ll say, basically, What? Why is he on the breather? And then they’ll read the message. Honestly, this over these, or if he had something to the side, you know, that tied it with it. That this, I think would be more effective.’ (Family – Female - Tobacco User)
Most participants wanted the facts with pictures showing harmful effects the child may experience throughout his/her life due to maternal tobacco use. A timeline from the fetus to adulthood represented by pictures was suggested.
‘I wouldn’t use just words. I’d like to use pictures like that, so they can actually see the actual picture.’ (Elder – Female – Non-Tobacco User)
In contrast, most reactions to the poster shown in Figure 1c (gain-framed emotional appeal) were that it was not strong enough and would have been more powerful if the baby would have been with her in the picture and illustrated specific effects. Moreover, three additional posters illustrating loss-framed emotional appeals, or loss- or gain-framed spiritual appeals, were not viewed as persuasive as the three concepts described above.
6. Campaign delivery feedback.
Combining graphic, factual campaign material along with providing support to be tobacco-free during pregnancy was viewed by the majority of participants as an effective intervention model. The Native Sisters could be helpful by distributing the campaign materials and information on village-specific Facebook pages; by giving presentations; holding individual or small group discussions; and by attending festivals, potlatches, and gatherings. There were mixed thoughts about presentations/discussions done at church, basketball games, bingo, or dances because at these venues people are focusing on the reason they are there and not to get information about the program. However, posters could be displayed and promotional items distributed to community members at these events. Preferred campaign promotional items were baby items, hoodies, t-shirts, and berry picking buckets.
Round 2
Participants
Recruitment and interviews were done between January-February, 2015. Fifty-six persons were screened, of which 52 (93%) were eligible and provided written informed consent. Table 2 provides sample characteristics; the mean age was 40 years, 69% were female, and 56% were current tobacco users.
Message preferences
Table 3 presents results on perceived effectiveness ratings for each of the three brochures. The three concepts were rated fairly similarly with some variation across items. Table 4 shows that the factual concept was preferred by half (50%) the sample, whereas 25% liked the emotional and 25% liked the spiritual concept best. With respect to least preferred concept, 40% indicated the spiritual, 31% the factual, and 29% the emotional appeal. There were no significant differences in preferred message concepts by audience segment (pregnant women, family members, Elders), traditional lifestyle, or current tobacco use (Table 4). Significant gender differences were detected (χ2=9.208, df=2, p=0.01); males strongly preferred the factual appeal (81% vs. 36% for females). [Table 3 near here] [Table 4 near here]
Table 3.
Perceived effectiveness ratings of message concepts among Y-K Delta Alaska Native participants in quantitative survey interviews to develop a social marketing campaign to reduce tobacco use in pregnancy (N=52)*
| Message concept n (%) |
|||
|---|---|---|---|
| Item | Factual | Spiritual | Emotional |
| Does it grab your attention? (recall) ‘very much’ | 33 (63.5) | 22 (42.3) | 29 (55.8) |
| Is it interesting to you? (reaction) ‘very much’ | 32 (61.5) | 31 (60.0) | 32 (61.5) |
| Is it direct/to the point? (comprehension) ‘very much’ | 38 (73.1) | 41 (78.8) | 36 (69.2) |
| Is the information useful to you? (salience) ‘very much’ | 34 (65.4) | 39 (75.0) | 40 (76.9) |
| Is it appropriate for people like yourself? (cultural relevance) ‘very much’ | 36 (69.2) | 41 (78.8) | 42 (80.8) |
| If you saw this brochure displayed in your community, how likely do you think you would be to quit tobacco or tell someone else to quit in the next month? ‘very likely’ | 20 (38.5) | 16 (30.8) | 16 (30.8) |
| Inspired to quit tobacco or to tell someone else to quit or not start using tobacco, ‘yes’ | 13 (25.0) | 10 (19.2) | 6 (11.5) |
Statistical comparisons were not performed across the factual, spiritual, and emotional concepts for each question because of the lack of independence across groups.
Table 4.
Message concept preferred most by select demographic characteristics among Y-K Delta Alaska Native participants in quantitative survey interviews to develop a social marketing campaign to reduce tobacco use in pregnancy (N=52)
| Preferred message concept n (%) |
||||
|---|---|---|---|---|
| Characteristic | Factual | Spiritual | Emotional | P value |
| Overall (N=52) | 26 (50.0) | 13 (25.0) | 13 (25.0) | 0.04a |
| Audience segment | 0.19b | |||
| Pregnant women (n=20) | 6 (30.0) | 7 (35.0) | 7 (35.0) | |
| Family members and friends (n=21) | 12 (57.1) | 4 (19.1) | 5 (23.8) | |
| Elders (n=11) | 8 (72.7) | 2 (18.2) | 1 (9.1) | |
| Current tobacco user | 0.28b | |||
| Yes (n=29) | 15 (51.7) | 9 (31.0) | 5 (17.2) | |
| No (n=23) | 11 (47.8) | 4 (17.4) | 8 (34.8) | |
| Gender | 0.01b | |||
| Female (n=36) | 13 (36.1) | 11 (30.6) | 12 (33.3) | |
| Male (n=16) | 13 (81.3) | 2 (12.5) | 1 (6.2) | |
| Follows traditional way of lifec | ||||
| Some (n=23) | 12 (52.2) | 6 (26.1) | 5 (21.7) | 0.85b |
| Very much (n=28) | 13 (46.4) | 7 (25.0) | 8 (28.6) | |
Chi-square goodness of fit test.
Chi-square test.
n=51; one individual who indicated ‘not at all’ was deleted from the analysis.
Promotional items
Baby items (38%) and hoodies (33%) were preferred because these were reported as useful and lacked availability in the villages.
Discussion
This preliminary study developed and refined health communication messaging for a social marketing campaign targeting the entire community to reduce tobacco use during pregnancy among AN women. Using mixed methods, this formative work indicated that many AN participants preferred factual loss-framed messaging appeals, including visual aids, to understand the harms of Iqmik and other maternal tobacco use on babies, children, and throughout adulthood. Efforts such as ours to develop culturally relevant health messaging are important because, despite decades of research evaluating treatments for smoking cessation during pregnancy, few prior efforts focused on interventions for AN or AI women. In a primarily Caucasian treatment sample, Toll et al. [29] found that gain-framed messages were effective for smoking cessation but have not yet evaluated impact of our campaign messaging on tobacco use outcomes. . Nonetheless, our preliminary findings highlight the need to develop targeted health communication messaging among diverse populations [21, 36].
Another key study finding was from the qualitative work which indicated the importance of messages focused on healthy pregnancies - health and wellness during pregnancy including reducing stress and use of positive cultural activities (e.g., berry picking). A recent study of 118 AN women (54 smokers, 64 nonsmokers) receiving prenatal care in Anchorage found that 73% of participants indicated the primary reason to smoke during pregnancy was to help manage stress [37]. Consistent with our current study, not endorsed were generational or cultural reasons to use Iqmik or smoke cigarettes during pregnancy.
A major strength of the study is the expansion of the end user group to include AN family/friends and Elders, and both men and women, who are all targets of the campaign, acknowledging the importance of messaging directed toward the health of the community at large. As potential sources of social support, these individuals could have a large influence on success or failure of tobacco cessation interventions for pregnant women. Additional strengths included use of mixed methodologies, use of the cultural variance and surface/deep structure health communication frameworks, a community-based participatory approach with substantial input from our CAB, and our longstanding partnership with the community. In addition, multiple actions were taken to ensure accurate interpretation of qualitative responses including two independent coders (inter-rater agreement was excellent) and debriefing of moderator and observers after each session.
This study has some limitations. First, as this was a formative study, we did not systematically test health communication messages using an experimental design [38] and are therefore not able to single out perceived effectiveness of individual message components. For example, appeal type may have been confounded by differences in visual elements (e.g., image design, format), or the order which participants rated test concepts. Future research using an experimental design could evaluate direct and interaction effects of message components (frame, appeal, content, visual elements) on persuasive effectiveness; controlling for order effects. Second, we did not evaluate messaging effects on perceived social norms, intention to use tobacco, or other behavioral outcomes [38]. However, perceived effectiveness is a useful indicator for assessing the likelihood of success of potential messages when large scale efficacy pretesting for behavioral impact is impractical [39]. Third, some aspects of the study population may limit generalizability to other AI/AN communities such as use of Iqmik and restricted geographic location. Nonetheless, use of non-cigarette forms of tobacco including homemade forms of ST is prevalent or gaining in popularity worldwide among girls and women of reproductive age [7, 40]. Thus, with some modifications, the messaging may have broader dissemination potential to other AI/AN communities and in populations with a high prevalence of prenatal tobacco use. Fourth, because a random sampling scheme was not employed, the opinions and responses from participants may not be representative of all AN people in the Y-K Delta region.
We acknowledge that this preliminary research makes its essential contribution primarily based on the qualitative findings. For example, while most participants preferred the factual based concept in the qualitative phase, but only half preferred this concept in the quantitative phase. This discrepancy is likely due to differences in methodology. Focus groups used in Round 2 in particular drew more on group consensus and opinions whereas all Round 2 quantitative interviews were conducted individually. Moreover, in Round 1 concepts were presented in no particular order across participants whereas in Round 2 there was a set presentation order. The quantitative work (Table 3) also indicated several discrepancies across the three concepts for perceived effectiveness items. For example, emotional and spiritual concepts were preferred over factual for item “appropriate for people like yourself.” In addition, males strongly preferred the factual concept whereas 36% of women liked this concept most. And 30% of pregnant women endorsed the factual concept compared to 35% for the spiritual and 35% for the emotional concepts. However, no differences were observed for preferred message concept across audience segments (pregnant women, Elders, family members), encouraging because the entire community, not just one particular subset, was the intended campaign target. We chose the factual concept based on multiple sources of data across different audience segments, but recognize that larger experimental studies could more fully tease out the inconsistencies noted. Our findings are exploratory and preliminary but could be useful to design these future studies.
In conclusion, our findings demonstrate a process that others could follow for developing culturally tailored interventions in diverse AI/AN communities. Subsequent reports will focus on: (1) development of the individual peer-counseling intervention manual for the Native Sisters to use with pregnant women that aligns closely with the campaign messages, and (2) outcome results from an ongoing cluster randomized trial evaluating the efficacy of the multi-level intervention for cessation and prevention of tobacco use during pregnancy and the postpartum period.
Acknowledgements
We wish to acknowledge the contributions of the following people for assisting with the implementation of the study: Christine Hughes, Tabetha Brockman, and Carrie Bronars from Mayo Clinic, Rochester, MN, and Rahnia Boyer from the Yukon-Kuskokwim Health Corporation, Bethel, AK. We also want to thank our Community Advisory Board members. We appreciate the contributions of Tiffany Tutuliak and Bailey Beaty at Northwest Strategies, Inc., and Brenda Manuelito and Carmelita Rodriguez at nDigiDreams, Inc. for developing the media produced in this study. We appreciate the assistance of Dr. Pamela Sinicrope (Mayo Clinic) with manuscript editing. Finally, we thank the people of the Y-K Delta region who participated in this research.
Copies of the media developed for this study are available by contacting the first author.
Funding details
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number R01CA164533. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of interest
The authors have no financial or other conflicts of interest or disclosures to report.
Geolocation information
The study was conducted in Bethel, Alaska.
References
- 1.Curtin SC, Matthews TJ. Smoking prevalence and cessation before and during pregnancy: Data from the birth certificate, 2014. Natl Vital Stat Rep. 2016. February 10;65(1):1–14. [PubMed] [Google Scholar]
- 2.Bauld L, Oncken C. Smoking in pregnancy: An ongoing challenge. Nicotine Tob Res. 2017. May 01;19(5):495–496. [DOI] [PubMed] [Google Scholar]
- 3.Tong VT, Dietz PM, Morrow B, et al. Trends in smoking before, during, and after pregnancy--pregnancy risk assessment monitoring system, united states, 40 sites, 2000-2010. MMWR Surveill Summ. 2013. November 08;62(6):1–19. [PubMed] [Google Scholar]
- 4.Bruin JE, Gerstein HC, Holloway AC. Long-term consequences of fetal and neonatal nicotine exposure: A critical review. Toxicol Sci. 2010. August;116(2):364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cnattingius S The epidemiology of smoking during pregnancy: Smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob Res. 2004. April;6 Suppl 2:S125–S140. [DOI] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services. The health consequences of smoking: 50 years of progress A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 7.Caleyachetty R, Tait CA, Kengne AP, et al. Tobacco use in pregnant women: Analysis of data from demographic and health surveys from 54 low-income and middle-income countries. Lancet Glob Health. 2014. September;2(9):e513–e520. [DOI] [PubMed] [Google Scholar]
- 8.Inamdar AS, Croucher RE, Chokhandre MK, et al. Maternal smokeless tobacco use in pregnancy and adverse health outcomes in newborns: A systematic review. Nicotine Tob Res. 2015. September;17(9):1058–1066. [DOI] [PubMed] [Google Scholar]
- 9.Chamberlain C, O’Mara-Eves A, Porter J, et al. Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database Syst Rev. 2017. February 14;2:CD001055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fiore MC, Jaen CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update Clinical practice guideline. Rockville, MD: Public Health Service, U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 11.Gould GS, Patten C, Glover M, et al. Smoking in pregnancy among indigenous women in high-income countries: A narrative review. Nicotine Tob Res. 2017. May 01;19(5):506–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alaska Native Epidemiology Center. Statewide data: Prenatal tobacco use [Internet]. 2016. [cited 2018 Feb 5]. Available from: http://anthctoday.org/epicenter/healthData/factsheets/prenatal_tobacco_use_statewide_3_31_2016.pdf
- 13.Alaska Native Epidemiology Center. Statewide data: Prenatal chew tobacco use [Internet]. 2016. [cited 2018 Feb 5]. Available from: http://anthctoday.org/epicenter/healthData/factsheets/prenatal_chew_tobacco_use_statewide_3_31_2016.pdf
- 14.Alaska Department of Health and Social Services. Alaska tobacco facts 2016 [Internet]. 2016. [cited 2017 Jun 7]. Available from: http://dhss.alaska.gov/dph/Chronic/Documents/Tobacco/PDF/2016_AKTobaccoFacts.pdf
- 15.Renner CC, Patten CA, Enoch C, et al. Focus groups of y-k delta alaska natives: Attitudes toward tobacco use and tobacco dependence interventions. Prev Med. 2004. April;38(4):421–431. [DOI] [PubMed] [Google Scholar]
- 16. [Author] [Google Scholar]
- 17.Biener L, Hamilton WL, Siegel M, et al. Individual, social-normative, and policy predictors of smoking cessation: A multilevel longitudinal analysis. Am J Public Health. 2010. March;100(3):547–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hymowitz N, Mueller MD, Lynn WR, et al. Background for a comprehensive community-based trial for smoking control Smoking and tobacco control monograph 6: Community-based interventions for smokers: The commit field experience. Bethesda, MD: National Cancer Institute; 2009. p. 15–25. [Google Scholar]
- 19.Trickett EJ, Beehler S, Deutsch C, et al. Advancing the science of community-level interventions. Am J Public Health. 2011. August;101(8):1410–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burhansstipanov L, Dignan MB, Schumacher A, et al. Breast screening navigator programs within three settings that assist underserved women. J Cancer Educ. 2010. June;25(2):247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gould GS, McEwen A, Watters T, et al. Should anti-tobacco media messages be culturally targeted for indigenous populations? A systematic review and narrative synthesis. Tob Control. 2013. July;22(4):e7. [DOI] [PubMed] [Google Scholar]
- 22.McAfee T, Davis KC, Alexander RL Jr., et al. Effect of the first federally funded us antismoking national media campaign. Lancet. 2013. December 14;382(9909):2003–2011. [DOI] [PubMed] [Google Scholar]
- 23.Koller KR, Flanagan CA, Day GE, et al. Developing a biomarker feedback intervention to motivate smoking cessation during pregnancy: Phase ii maw study. Nicotine Tob Res. 2017. August 1;19(8):930–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alaska Native Epidemiology Center. Alaska native health status report [Internet]. Anchorage, AK: Alaska Native Tribal Health Consortium; 2017. [cited 2016 Dec 15]; 2nd:[Available from: http://anthctoday.org/epicenter/publications/HealthStatusReport/AN_HealthStatusReport_FINAL2017.pdf [Google Scholar]
- 25.Davis RE, Resnicow K. The cultural variance framework for tailoring health messages In: Cho H, editor. Health communication message design: Theory and practice. Thousand Oaks, CA: Sage Publications, Inc.; 2012. p. 115–135. [Google Scholar]
- 26.Resnicow K, Braithwaite RL. Cultural sensitivity in public health In: Braithwaite RL, Taylor SE, editors. Health issues in the black community. 2nd ed. San Francisco, CA: Jossey-Bass Inc.; 2001. p. 516–542. [Google Scholar]
- 27.Wolsko C, Lardon C, Hopkins S, et al. Conceptions of wellness among the yup’ik of the yukon-kuskokwim delta: The vitality of social and natural connection. Ethn Health. 2006. November;11(4):345–363. [DOI] [PubMed] [Google Scholar]
- 28.Wolsko C, Mohatt GV, Lardon C, et al. Smoking, chewing, and cultural identity: Prevalence and correlates of tobacco use among the yup’ik-the center for alaska native health research (canhr) study. Cultur Divers Ethnic Minor Psychol. 2009. April;15(2):165–172. [DOI] [PubMed] [Google Scholar]
- 29.Toll BA, O’Malley SS, Katulak NA, et al. Comparing gain- and loss-framed messages for smoking cessation with sustained-release bupropion: A randomized controlled trial. Psychol Addict Behav. 2007. December;21(4):534–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Manuelito BK, Rodriguez C. Planting “new media” seeds to promote cancer education and policy across indian country. 7th Biennial Cancer, Culture , and Literacy: Methodologies, Skills and Innovations Conference; May 20-22; Tampa, FL: 2010. [Google Scholar]
- 31.National Cancer Institute. Making health communication programs work. Washington, DC: US Department of Health and Human Services. National Institutes of Health, National Cancer Institute; 2004. [Google Scholar]
- 32.Patton MQ. Qualitative research & evaluation methods: Integrating therory and practice. 4th ed. Thousand Oaks, CA: Sage Publications, Inc.; 2015. [Google Scholar]
- 33.Krueger RA, Casey MA. Focus groups: A practical guide for applied research. 5th ed. Thousand Oaks, CA: Sage Publications, Inc.; 2015. [Google Scholar]
- 34.Birks M, Chapman Y, Francis K. Memoing in qualitative research: Probing data and processes. J Res Nurs. 2008;13(1):68–75. [Google Scholar]
- 35.Krippendorff KH. Content analysis: An introduction to its methodology. 3rd ed. Thousand Oaks, CA: Sage Publications, Inc.; 2013. p. 42–46. [Google Scholar]
- 36.Davis KC, Duke J, Shafer P, et al. Perceived effectiveness of antismoking ads and association with quit attempts among smokers: Evidence from the tips from former smokers campaign. Health Commun. 2017. August;32(8):931–938. [DOI] [PubMed] [Google Scholar]
- 37.Bronars C, Patten C, Koller K, et al. Perceived risks and reasons to smoke cigarettes during pregnancy among alaska native women. Ethn Health. 2016. November 14:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Popova L, Linde BD, Bursac Z, et al. Testing antismoking messages for air force trainees. Tob Control. 2016. November;25(6):656–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yzer M, LoRusso S, Nagler RH. On the conceptual ambiguity surrounding perceived message effectiveness. Health Commun. 2015;30(2):125–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Cancer Institute. Smokeless tobacco and public health: A global perspective [Internet]. Bethesda, MD: National Cancer Institute; 2014. [cited 2017 Jun 7]. Available from: https://cancercontrol.cancer.gov/brp/tcrb/global-perspective/ [Google Scholar]


