Abstract
Background
Previous incidence estimates may no longer reflect the current public health burden of cardiac arrest in hospitalized adult and pediatric patients across the US. The aim of this study was to estimate the contemporary annual incidence of in-hospital cardiac arrest in adults and children across the US and to describe trends in incidence between 2008 and 2017.
Methods and Results
Using the Get With The Guidelines®-Resuscitation registry, we developed a negative binomial regression model to estimate the incidence of index pulseless in-hospital cardiac arrest based on hospital-level characteristics. The model was used to predict the number of in-hospital cardiac arrests in all US hospitals, using data from the American Hospital Association Annual Survey. We performed separate analyses for adult (≥ 18 years) and pediatric (< 18 years) cardiac arrests. Additional analyses were performed for recurrent cardiac arrests and pediatric patients requiring cardiopulmonary resuscitation for poor perfusion (non-pulseless events). The average annual incidence of in-hospital cardiac arrest in the US was estimated at 292,000 (95% prediction interval: 217,600, 503,500) adult and 15,200 pediatric cases, of which 7,100 (95% prediction interval: 4,400, 9,900) cases were pulseless cardiac arrests and 8,100 (95% prediction interval: 4,700, 11,500) cases were non-pulseless events. The rate of adult cardiac arrests increased over time, while pediatric events remained more stable. When including both index and recurrent in-hospital cardiac arrests, the average annual incidence was estimated at 357,900 (95% prediction interval: 247,100, 598,400) adult and 19,900 pediatric cases, of which 8,300 (95% prediction interval: 4,900, 11,200) cases were pulseless cardiac arrests and 11,600 (95% prediction interval: 6,400, 16,700) cases were non-pulseless events.
Conclusions
There are approximately 292,000 adult in-hospital cardiac arrests and 15,200 pediatric in-hospital events in the US each year. This study provides contemporary estimates of the public health burden of cardiac arrest among hospitalized patients.
Subject Terms: Critical Care and Resuscitation – Cardiopulmonary Arrest, Epidemiology, Lifestyle, Prevention – Epidemiology, Quality and Outcomes – Quality and Outcomes
Keywords: Epidemiology, Incidence, Cardiac Arrest, Heart Arrest
Current national incidence estimates of adult in-hospital cardiac arrest in the United States are based on data from more than a decade ago.1 The most recent study used data from a prospective cardiac arrest registry to extrapolate the incidence of in-hospital cardiac arrest to the total population of hospitalized patients in the United States.2 The authors included data from 2003 to 2007 and concluded that in-hospital cardiac arrest occurs in approximately 211,000 adult patients in the United States each year. To our knowledge, there are no available contemporary incidence estimates and these findings may no longer reflect the current incidence of adult in-hospital cardiac arrest.
Incidence estimates of pediatric in-hospital cardiac arrest in the United States are more obscure, as the only nationwide estimate was calculated from several separate data sources, all of which were single-center studies using data prior to 2008.3 The estimate was published in the 2013 American Heart Association consensus statement concluding that in-hospital cardiac arrest occurs in approximately 6,000 hospitalized children each year.4 However, more rigorous methods using the most contemporary data are required to estimate the current incidence of pediatric in-hospital cardiac arrest.
Understanding the contemporary public health burden of in-hospital cardiac arrest is important for informing healthcare policies, research priorities, and tracking efforts to reduce events. In this study, we aimed to estimate the annual incidence of in-hospital cardiac arrest in adults and children across the United States and to describe trends in incidence between 2008 and 2017.
Methods
Study Design, Data Source, and Study Population
We analyzed prospectively collected data from the Get With The Guidelines®-Resuscitation (GWTG-R) registry. The GWTG-R registry is a voluntary, prospective, quality-improvement registry of in-hospital cardiac arrest in the United States, sponsored by the American Heart Association. Certified personnel at each participating hospital collect data on all in-hospital cardiac arrest patients without a do-not-resuscitate order. Cardiac arrest is defined as the loss of a palpable central pulse or the presence of a pulse with poor perfusion (pediatric patients only) requiring chest compressions, defibrillation or both, with a hospital-wide or unit-based emergency response by acute care personnel. The design, data collection, and validity of the registry have been described in detail elsewhere.2, 5, 6 All participating hospitals are required to comply with local regulatory guidelines. The Institutional Review Board at Beth Israel Deaconess Medical Center (Boston, MA, USA) have determined that research involving the GWTG-R registry does not meet the federal definition of human subject research.
Hospital-level data were obtained from the 2010 and 2013 American Hospital Association Annual Survey.7 Hospitals in the United States are registered by the American Hospital Association if the institution is listed as a hospital by the Joint Commission on Accreditation of Healthcare Organizations or is certified as a provider of acute services under Title 18 of the Social Security Act. Hospitals not meeting these criteria may be registered as a hospital by a number of alternative requirements.8 The response rate for the American Hospital Association Annual Survey averages approximately 75%. Incomplete data for selected characteristics of hospitals not responding or partially responding to the Annual Survey are imputed using previous records.9
Patients in the GWTG-R registry were linked to hospitals in the American Hospital Association dataset by the American Heart Association data management vendor. Because the GWTG-R registry extends to 2017 and the American Hospital Association dataset was based on data from 2010 and 2013, there is a small discrepancy in the number of patients and hospitals which can be matched (i.e., some hospitals have merged, closed, or have incomplete data).
For the primary analysis, we included adult (≥ 18 years of age) and pediatric (< 18 years of age) patients with an initial or subsequent pulseless index cardiac arrest from January 1, 2008 to December 31, 2017 within the GWTG-R registry. Patients at hospitals in the GWTG-R registry which could not be linked to the American Hospital Association dataset were excluded.
Hospitals only seeing adult patients (100% adult beds) were excluded from the pediatric analysis and hospitals only seeing pediatric patients (100% pediatric beds) were excluded from the adult analysis, based on the variable “fraction of adult beds” per hospital. Missing values for the “fraction of adult beds” were imputed prior to exclusion of hospitals (see “Statistical Analysis”). Hospitals in the American Hospital Association dataset with missing data for “total number of hospital beds” were also excluded.
The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist is provided in the Supplemental Material.10
Statistical Analysis – Overview
For the primary analysis, we estimated the adult and pediatric incidence of pulseless in-hospital cardiac arrests separately. For each analysis, we developed regression models using data from GWTG-R participating hospitals with the yearly hospital-level incidence as the dependent variable and hospital-level characteristics as the independent variables. Coefficients from the regression models were applied to the American Hospital Association dataset, which contains hospital-level data from the entire United States, to estimate annual national incidences.
Two additional preplanned analyses were performed. First, we included both index and recurrent events to estimate the overall burden of in-hospital cardiac arrest. Second, we calculated estimates for pediatric patients requiring cardiopulmonary resuscitation for poor perfusion (non-pulseless event), only including patients who maintained a pulse throughout the entire sequence. As a post hoc analysis, we repeated the primary analysis to obtain adult incidence estimates after adding the number of hospital admissions to the regression model. This variable included both adult and pediatric admissions and was therefore not used for the primary analysis.
SAS version 9.4 (SAS Institute, Cary, NC, USA) was used for all analyses.
Statistical Analysis #1 – Incidence in GWTG-R hospitals
We calculated the incidence of index in-hospital cardiac arrest in GWTG-R participating hospitals (i.e., the number of in-hospital cardiac arrests per hospital) per year from 2008 to 2017 yielding one estimate per hospital per year of GWTG-R participation. To ensure that hospitals entered data throughout the entire year, we only included hospital-level data for those years with ≥ 1 reported event per quarter for the adult analysis and ≥ 1 reported event per year for the pediatric analysis, given the lower incidence of the latter. We assumed that acute care hospitals were unlikely to encounter < 1 cardiac arrest over these time-periods.
Statistical Analysis #2 – Prediction Model Development
We developed two separate prediction models (pediatric and adult) using the annual number of in-hospital cardiac arrests per hospital as the dependent variable (i.e., “outcome”) and hospital-level data from GWTG-R participating hospitals as the independent variables (i.e., “predictors”). Variables used for the analyses are provided in Table 1 and 2. Based on the distribution of in-hospital cardiac arrest (Figure S1 and S2), we used a multivariable regression model with a negative binomial distribution to assess whether hospital-level characteristics were associated with the number of in-hospital cardiac arrests per hospital per year within the GWTG-R dataset. Variables associated with the number of events at a p-value < 0.20 in unadjusted analyses were subsequently included in a multivariable model. Backwards selection was then performed by sequentially eliminating variables until only those significant at a p-value < 0.05 remained. Year was included in the model as a categorical variable irrespective of statistical significance. Additional post hoc analyses were also performed including year as a continuous variable (linear trend). To account for multiple observations within the same hospitals over time (one incidence per year), we fit the negative binomial regressions using generalized estimation equations (GEE) with robust standard errors to account for any misspecification of the correlation among the repeated measures over time.11 An autoregressive variance-covariance structure was used for the adult analysis and an independent variance-covariance structure was used for the pediatric analysis to ensure convergence.
Table 1.
Characteristics of hospitals providing care to adult patients
| GWTG-R hospitals (n = 398) | Non-GWTG-R hospitals (n = 5,887) | |
|---|---|---|
| Adult hospital beds | ||
| 0 – 100 | 32 (8) | 3,387 (58) |
| 100 – 199 | 80 (20) | 1,186 (20) |
| 200 – 249 | 32 (8) | 345 (6) |
| 250 – 299 | 41 (10) | 264 (4) |
| 300 – 349 | 40 (10) | 166 (3) |
| 350 – 499 | 75 (19) | 304 (5) |
| > 499 | 98 (25) | 235 (4) |
| Geographical region | ||
| North-East | 73 (18) | 743 (13) |
| South-East | 104 (26) | 908 (15) |
| North-Central | 81 (20) | 1,629 (28) |
| South-Central | 63 (16) | 1,522 (26) |
| West | 77 (19) | 1,085 (18) |
| Geographical area | ||
| Urban | 360 (90) | 3,652 (62) |
| Rural | 38 (10) | 2,235 (38) |
| Ownership type | ||
| Government/Military | 64 (16) | 1,432 (24) |
| Non-profit | 275 (69) | 2,867 (49) |
| Private | 59 (15) | 1,588 (27) |
| Teaching hospital | ||
| Non-teaching | 173 (43) | 3,615 (78) |
| Minor | 121 (30) | 996 (17) |
| Major | 104 (26) | 276 (5) |
| Emergency department visits | ||
| 0 – 10,000 | 11 (3) | 3,011 (51) |
| 10,001 – 50,000 | 175 (44) | 2,174 (37) |
| 50,001 – 100,000 | 166 (42) | 559 (10) |
| > 100,000 | 46 (12) | 143 (2) |
GWTG-R denotes Get With The Guidelines®-Resuscitation
Table 2.
Characteristics of hospitals providing care to pediatric patients
| Pulseless cardiac arrests | Non-pulseless events | |||
|---|---|---|---|---|
| GWTG-R hospitals (n = 212) | Non-GWTG-R hospitals (n = 2,043) | GWTG-R hospitals (n = 158) | Non-GWTG-R hospitals (n = 2,097) | |
| Pediatric hospital beds | ||||
| None* | 32 (15) | 357 (17) | 23 (15) | 366 (17) |
| 1 – 10 | 44 (21) | 928 (45) | 25 (16) | 947 (45) |
| 2 – 25 | 65 (31) | 498 (24) | 46 (29) | 517 (25) |
| 26 – 50 | 31 (15) | 162 (8) | 25 (16) | 168 (8) |
| > 50 | 40 (19) | 98 (5) | 39 (25) | 99 (5) |
| Pediatric ICU beds | ||||
| None* | 112 (53) | 1,717 (84) | 71 (45) | 1,758 (84) |
| 1 – 10 | 40 (19) | 184 (9) | 30 (19) | 194 (9) |
| > 10 | 60 (28) | 142 (7) | 57 (36) | 145 (7) |
| Geographical region | ||||
| North-East | 32 (15) | 376 (18) | 24 (15) | 384 (18) |
| South-East | 59 (28) | 343 (17) | 45 (28) | 357 (17) |
| North-Central | 49 (23) | 517 (25) | 40 (19) | 536 (26) |
| South-Central | 38 (18) | 422 (21) | 28 (18) | 432 (21) |
| West | 34 (16) | 385 (19) | 31 (20) | 388 (19) |
| Geographical area | ||||
| Urban | 196 (92) | 1,509 (74) | 145 (92) | 1,560 (74) |
| Rural | 16 (8) | 534 (26) | 13 (8) | 537 (26) |
| Ownership type | ||||
| Government/Military | 30 (14) | 352 (17) | 23 (15) | 359 (17) |
| Non-profit | 158 (75) | 1,317 (64) | 121 (77) | 1,354 (65) |
| Private | 24 (11) | 374 (18) | 14 (9) | 384 (18) |
| Teaching hospital | ||||
| Non-teaching | 66 (31) | 1,263 (62) | 37 (23) | 1,292 (62) |
| Minor | 70 (33) | 564 (28) | 59 (37) | 575 (27) |
| Major | 76 (36) | 216 (11) | 62 (39) | 230 (11) |
| Emergency department visits | ||||
| 0 – 10,000 | 4 (2) | 278 (14) | 2 (1) | 280 (13) |
| 10,001 – 50,000 | 64 (30) | 1,089 (53) | 38 (24) | 1.115 (53) |
| 50,001 – 100,000 | 105 (50) | 531 (26) | 87 (55) | 549 (26) |
| > 100,000 | 39 (18) | 145 (7) | 31 (20) | 153 (7) |
GWTG-R denotes Get With The Guidelines®-Resuscitation, ICU denotes intensive care unit
Including hospitals with pediatric events in the Emergency Department, events where the patient was hospitalized in an adult bed, and hospitals with designated neonatal beds.
Statistical Analysis #3 – Application to the American Hospital Association dataset
The American Hospital Association dataset had complete data on hospital-level characteristics for 5,999 (95%) hospitals prior to imputation in the adult analysis and 5,213 (77%) hospitals in the pediatric analysis (Table S1 and S2). Missing data on hospital-level characteristics were imputed under the assumption that data were “missing at random” using the fully conditional specification method.12 A single imputed dataset was created (see “Supplemental Methods” in the Supplemental Material). The developed negative binomial regression models (see “Statistical Analysis #2”) were applied to the imputed American Hospital Association dataset to estimate the annual national incidence of in-hospital cardiac arrest in the United States. Predicted estimates were obtained for all non-GWTG-R participating hospitals and combined with the observed estimates from GWTG-R participating hospitals. To obtain 95% prediction intervals13, we performed cluster bootstrapping, randomly sampling data on hospitals with replacements (n = 1,000 bootstrap samples). The predicted estimates from the bootstrapping of the number of in-hospital cardiac arrests per hospital per year accounted for sampling error from the prediction models (estimation uncertainty) and the fundamental variability of the cardiac arrest counts (negative binomial dispersion). The 95% prediction intervals for the annual national incidence estimates were obtained using the 2.5 and 97.5 percentiles of the bootstrap distribution of the estimates.
Results
Adult in-hospital cardiac arrest incidence
A total of 6,285 adult hospitals were included from the American Hospital Association database, of which 398 hospitals were linked to the GWTG-R registry (Table 1 and Figure S3). There were 167,013 cardiac arrests registered in the GWTG-R registry between 2008 and 2017 (Figure S4), with a median of 76 (quartiles: 39, 124) cases per hospital per year. Out of the six hospital characteristics available for the analysis, four remained in the final prediction model, including number of hospital beds, emergency department visits, geographical location, and geographical area (Table S3).
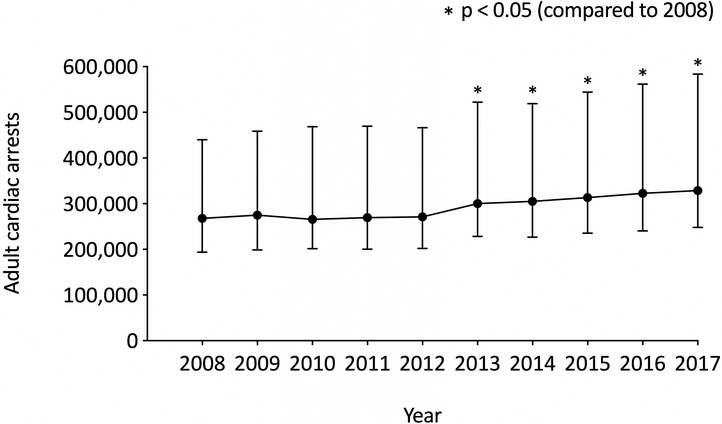
The average incidence across all hospitals in the United States between 2008 and 2017 was estimated at 292,000 (95% prediction interval: 217,600, 503,500) cases per year (Figure 1 and Table S4). The results were similar when adding the number of admissions to the model in the post hoc analysis, with an estimated average incidence of 309,000 (95% prediction interval: 210,000, 586,700) cases. There was an increase in adult in-hospital cardiac arrests over time, with an estimated incidence of 268,200 (95% prediction interval: 193,700, 440,300) cases in 2008 and 328,700 (95% prediction interval: 248,100, 583,900) cases in 2017 (p < 0.001). There was also an increase in cardiac arrests over time when considering year as a continuous variable (incidence rate ratio: 1.03, 95%CI: 1.02, 1.04, p < 0.001). When including both index and recurrent events, the average annual incidence between 2008 and 2017 was estimated at 357,900 (95% prediction interval: 247,100, 598,400) cases (Figure S5, Table S5 and S6).
Figure 1. Annual trends in the incidence of adult in-hospital cardiac arrest in the United States.
The average number of index cardiac arrests occurring in hospitalized adult patients between 2008 and 2017 was estimated at 292,000 (95% prediction interval: 217,600, 503,500) cases per year. There was an increase in cardiac arrests over time (incidence rate ratio: 1.03, 95%CI: 1.02, 1.03). Numerical estimates are provided in Table S4.
Pediatric in-hospital event incidence
A total of 2,255 pediatric hospitals were included from the American Hospital Association database, of which 212 hospitals with pulseless cardiac arrests and 158 hospitals with non-pulseless events were linked to the GWTG-R registry (Table 2 and Figure S6). There were 6,004 pulseless cardiac arrests and 5,022 non-pulseless events registered in the GWTG registry between 2008 and 2017 (Figure S7), with a median of 2 (quartiles: 1, 8) pulseless cardiac arrests and 4 (quartiles: 1, 11) non-pulseless events per hospital per year. Out of the seven hospital characteristics available for the analyses, two (number of hospital beds and teaching status) remained in the model on pulseless cardiac arrests and four (number of hospital beds, teaching status, emergency department visits, and ownership type) remained in the model on non-pulseless events (Table S7 and S8).
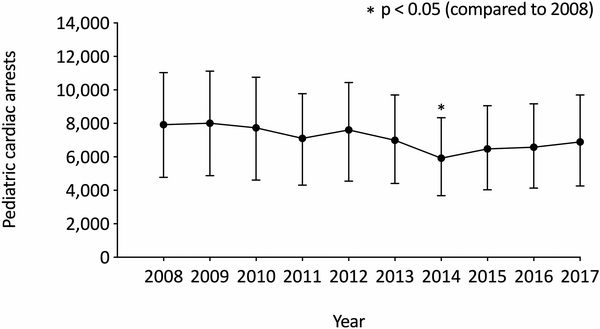
The average national pulseless in-hospital cardiac arrest incidence was estimated at 7,100 (95% prediction interval: 4,400, 9,900) cases per year (Figure 2 and Table S9). There was no clear change in incidence over time (incidence rate ratio: 0.97, 95%CI: 0.94, 1.00, p = 0.08), with an estimated incidence of 7,900 (95% prediction interval: 4,800, 11,000) cases in 2008 and 6,900 (95% prediction interval: 4,300, 9,700) cases in 2017. When including both index and recurrent pulseless cardiac arrests, the average annual incidence was estimated at 8,300 (95% prediction interval: 4,900, 11,200) cases (Figure S8, Table S10 and S11).
Figure 2. Annual trends in the incidence of pediatric pulseless in-hospital cardiac arrest in the United States.
The average number of index pulseless cardiac arrests occurring in hospitalized pediatric patients between 2008 and 2017 was estimated at 7,100 (95% prediction interval: 4,400, 9,900) cases per year. There was no clear change in incidences over time (incidence rate ratio: 0.97, 95%CI: 0.94, 1.00), p = 0.08). Numerical estimates are provided in Table S9.
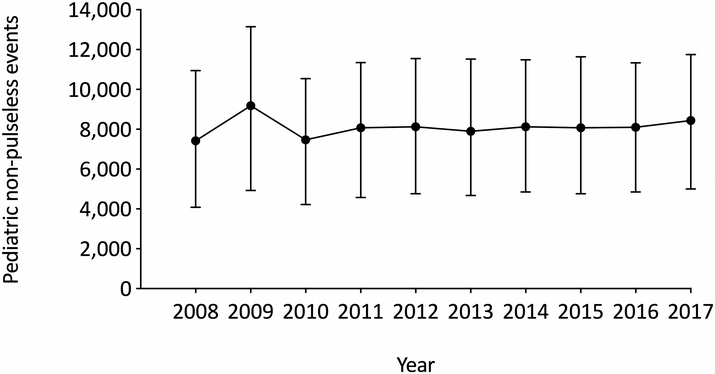
The average national non-pulseless event incidence was estimated at 8,100 (95% prediction interval: 4,700, 11,500) cases per year (Figure 3 and Table S12). There was again no clear difference in incidence over time (incidence rate ratio: 1.00, 95%CI: 0.97, 1.04, p = 0.09), with an estimated 7,400 (95% prediction interval: 4,100, 10,900) cases in 2008 and 8,400 (95% prediction interval: 5,000, 11,700) cases in 2017. When including both index and recurrent non-pulseless events, the average annual incidence was estimated at 11,600 (95% prediction interval: 6,400, 16,700) cases (Figure S9, Table S13 and S14).
Figure 3. Annual trends in the incidence of pediatric non-pulseless events in the United States.
The average number of index non-pulseless events requiring cardiopulmonary resuscitation in hospitalized pediatric patients between 2008 and 2017 was estimated at 8,100 (95% prediction interval: 4,700, 11,500) cases per year. There was no clear difference in incidences over time (incidence rate ratio: 1.00, 95%CI: 0.97, 1.04), p = 0.09). Numerical estimates are provided in Table S12.
In aggregate, the national pediatric in-hospital event incidence was calculated at 15,200 cases per year. When considering both index and recurrent events, the aggregate annual incidence was calculated at 19,900 cases.
Discussion
We used a large, multicenter, resuscitation registry to derive the contemporary incidence of in-hospital cardiac arrest occurring annually in the United States. The adult in-hospital cardiac arrest incidence was estimated at 292,000 cases per year, whereas the incidence of pediatric in-hospital events was estimated at 15,200 cases per year, of which 7,100 cases were pulseless cardiac arrests and 8,100 cases were non-pulseless events, respectively. When predicting the number of index and recurrent events, we estimated an incidence of 357,900 adult in-hospital cardiac arrests and 19,900 pediatric in-hospital events requiring cardiopulmonary resuscitation annually, of which 8,300 cases were pulseless cardiac arrests and 11,600 cases were non-pulseless events.
Our findings indicate that the public health burden of adult and pediatric in-hospital cardiac arrest is approximately 38% and 18% greater than previously reported, respectively.2, 4 Moreover, the results suggest that in-hospital cardiac arrest occurs with nearly the same frequency as out-of-hospital cardiac arrest. When combining these findings with the previously reported out-of-hospital cardiac arrest incidence of 347,300 adult and 7,000 pediatric cases1, the total burden of cardiac arrest reaches approximately 640,000 adult and 22,000 pediatric index cases annually in the United States. The current data further demonstrate that the annual incidence of professionally treated adult in-hospital cardiac arrests is substantially higher compared to professionally treated out-of-hospital cardiac arrests, with a reported 180,200 adult EMS-treated cardiac arrests in the out-of-hospital setting1. This information may have important implications for hospital-based Basic Life Support and Advanced Cardiac Life Support training programs, which have traditionally focused on out-of-hospital cardiac arrests.
With a reported survival rate of 25.8% and 37.9% for adult and pediatric in-hospital cardiac arrests in 20161 and 53.0% for pediatric non-pulseless events between 2000 and 200814, our estimates can be translated to approximately 216,700 adult deaths from in-hospital cardiac arrest and 8,200 pediatric deaths from in-hospital events in the United States each year, corresponding to 4,400 pediatric deaths from in-hospital cardiac arrest and 3,800 pediatric deaths from non-pulseless events. Additionally, based on the reported 30.2 million adult and 5.6 million pediatric hospital stays in the United States during 201515, the estimated in-hospital event incidence can be extrapolated to 9.7 adult cardiac arrests and 2.7 pediatric events per 1,000 hospitalizations.
Few previous studies have estimated the national incidence of adult in-hospital cardiac arrest in the United States. The most recent estimate was published by Merchant et al. in 2011 who leveraged the GWTG-R registry and the American Hospital Association database using a similar approach as the current study.2 The authors estimated an average incidence between 2003 and 2007 of approximately 211,000 adult cases per year, compared to 292,000 cases in our study. There may be multiple explanations for the discrepant findings. First, while Merchant et al. included the volume of beds and intensive care unit beds as model predictors, it is unclear whether these variables were restricted to adult, pediatric, or all beds. Second, we and others2 have found an increase in the number of cardiac arrests over time, with an estimated increase of 23% from 2008 to 2017 in our study. Third, the number of hospitals in the United States and hospital-level characteristics may have changed since publication of the previous incidence estimates. Merchant et al. calculated the incidence based on 433 GWTG-R and 5,445 non-GWTG-R hospitals, compared to 398 GWTG-R and 5,887 non-GWTG-R hospitals in our dataset. These differences are partly due to different exclusion criteria and the former study may have included hospitals not reporting cardiac arrest cases to the GWTG registry. Lastly, the availability of some covariates used for the prediction model differed from the previous study, although most variables were overlapping.
Incidence estimates of pediatric pulseless in-hospital cardiac arrest are more scarce and the current national estimate is based on data from smaller observational studies.4 In a systematic review and meta-analysis from 2010, the number of rapid-response team activations for in-hospital cardiac arrest was calculated from five single-center studies (3.26 activations per 1,000 admissions)3, which after extrapolation by the national number of pediatric hospital admissions yielded approximately 6,000 pediatric pulseless cardiac arrests per year4. In comparison, our estimated average incidence of 7,100 cases suggests that the burden of pediatric pulseless in-hospital cardiac arrest is 18% greater than that previously estimated. While we found no indication that the number of pediatric events has increased over time, our estimates are based on a larger database and provides the most robust estimate of pediatric in-hospital cardiac arrest cases in the United States to date. Additionally, a study from 2012 utilized the Healthcare Cost and Utilization Project (HCUP) Kids Inpatient Database to estimate the total (pulseless and non-pulseless) incidence of pediatric events requiring cardiopulmonary resuscitation in the United States, including both index and recurrent events.16 The authors reported an annual incidence of 5,800 (95% CI: 5,259, 6,355) cases which is considerably lower compared to the reported 19,900 cases in our study, although administrative data are inherently limited by the current coding system and the absence of detailed clinical information.17
No previous study has specifically estimated the national incidence of pediatric non-pulseless events, although an earlier report from the GWTG-R registry suggest that about 35% of all children requiring cardiopulmonary resuscitation never become pulseless.14 Since children may present with bradycardia and poor perfusion prior to deteriorating into pulseless cardiac arrest, the Pediatric Advanced Life Support guidelines (PALS) recommend the provision of chest compressions and ventilation to these patients.18 In comparison to the previous report, we estimated an average incidence of 8,100 non-pulseless events, corresponding to about 53% of all pediatric events. The higher ratio of non-pulseless events may be explained by the weighting of our estimates to all United States hospitals. Furthermore, hospitals reporting non-pulseless events were fewer and reported a greater number of cases per hospital per year, compared to hospitals reporting pediatric pulseless cardiac arrests (Figure S2).
Our study should be interpreted in the context of some limitations. First, we excluded hospitals which could not be linked to the GWTG-R dataset and the overall number of GWTG-R hospitals providing data for the prediction model was relatively small (Figure S3 and S6). Mandatory reporting requirements for in-hospital cardiac arrest and higher hospital participation in the GWTG-R registry may allow for more precise incidence estimates. Second, we were limited by the time of matching between the GWTG-R registry and the 2010 and 2013 American Hospital Association database. Hospital-level characteristics were therefore assumed to be static over time. Third, the prediction model was dependent on the number of cardiac arrest cases registered in the GWTG-R registry. It is possible that hospitals could have underreported the number of cardiac arrests and/or not entered consecutive cases into the registry, which could lead to an underestimation of the true incidence when the GWTG-R data were extrapolated to all United States hospitals. In addition, cases not receiving a hospital-wide or unit-based emergency response (e.g., cardiac arrests in the catheterization laboratory and operating room) and patients declared dead without provision of cardiopulmonary resuscitation are not included in the registry. The estimated incidences in this study should therefore be considered conservative. Fourth, the prediction model was limited by the variables available in the American Hospital Association dataset and there is a possibility that more granular hospital-level characteristics (including patient case-mix) could have improved the validity and precision of our estimates. Lastly, we assumed that the relationship between the incidence in GWTG-R participating hospitals were transferable to non-GWTG-R participating hospitals, although we were not able to assess the validity of this assumption.
Conclusions
Our analyses indicate that there are approximately 292,000 adult in-hospital cardiac arrests and 15,200 pediatric in-hospital events requiring cardiopulmonary resuscitation in the United States each year. The incidence of adult in-hospital cardiac arrests has increased over time, while pediatric events remained more stable. These estimates provide contemporary annual estimates of the public health burden from in-hospital cardiac arrest in the United States.
Supplementary Material
What is Known
Previous studies have reported a national incidence of 211,000 adult and 6,000 pediatric pulseless in-hospital cardiac arrests across the US.
These previous incidence estimates may no longer reflect the current public health burden of cardiac arrest in the US.
What the Study Adds
We estimate that there are approximately 292,000 adult in-hospital cardiac arrests and 15,200 pediatric in-hospital events requiring cardiopulmonary resuscitation in the US each year.
Compared to previous reports, the public health burden of adult and pediatric pulseless in-hospital cardiac arrest is approximately 38% and 18% greater than previously estimated.
The incidence of adult in-hospital cardiac arrests increased between 2008 and 2017, while pediatric events have remained more stable
Acknowledgments
Mathias J. Holmberg and Lars W. Andersen were responsible for data acquisition, performed the statistical analyses, and drafted the manuscript. All authors contributed to the design of the study, interpreted the results, critically revised the manuscript, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
Sources of Funding
There was no specific funding for this study. Dr. Andersen serves as a compensated statistical reviewer for JAMA. Dr. Donnino is supported by grant 1K24HL127101–01 and Dr. Chan is supported by grant 1R01HL123980 from the National Heart, Lung, and Blood Institute.
Appendix:
Get With The Guidelines®-Resuscitation Investigators
Besides the authors Paul Chan, M.D., M.Sc. and Anne V. Grossestreuer, Ph.D., members of the Get With The Guidelines®-Resuscitation Adult Research Task Force include:
Ari Moskowitz, M.D., Dana Edelson, M.D., M.S., Joseph Ornato, M.D., Katherine Berg, M.D., Mary Ann Peberdy, M.D., Matthew Churpek, M.D., M.P.H., Ph.D., Michael Kurz, M.D., M.S.-H.E.S., Monique Anderson Starks, M.D., M.H.S., Saket Girotra, M.B.B.S., S.M., Sarah Perman, M.D., M.S.C.E., Zachary Goldberger, M.D., M.S.
Besides the author Jordan Duval-Arnould, M.P.H., Dr.P.H., members of the Get With The Guidelines®-Resuscitation Pediatric Research Task Force include:
Anne-Marie Guerguerian, M.D., Ph.D., F.R.C.P.C., Dianne Atkins, M.D., Elizabeth Foglia, M.D., M.S.C.E., Ericka Fink, M.D., Javier J. Lasa, M.D., F.A.A.P., Joan Roberts, M.D., Melanie Bembea, M.D., M.P.H., Michael Gaies, M.D., M.P.H., M.Sc., Monica Kleinman, M.D., Punkaj Gupta, M.B.B.S., Robert Sutton, M.D., M.S.C.E., Taylor Sawyer, D.O.Med.
Footnotes
Disclosures
None.
References
- 1.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P and Subcommittee AHACoEaPSCaSS. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 2.Merchant RM, Yang L, Becker LB, Berg RA, Nadkarni V, Nichol G, Carr BG, Mitra N, Bradley SM, Abella BS, Groeneveld PW and Investigators AHAGWTG-R. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39:2401–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan PS, Jain R, Nallmothu BK, Berg RA and Sasson C. Rapid Response Teams: A Systematic Review and Meta-analysis. Arch Intern Med. 2010;170:18–26. [DOI] [PubMed] [Google Scholar]
- 4.Morrison LJ, Neumar RW, Zimmerman JL, Link MS, Newby LK, McMullan PW, Hoek TV, Halverson CC, Doering L, Peberdy MA, Edelson DP and American Heart Association Emergency Cardiovascular Care Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation. 2013;127:1538–63. [DOI] [PubMed] [Google Scholar]
- 5.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G and Lane-Trultt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. [DOI] [PubMed] [Google Scholar]
- 6.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane-Truitt T, Potts J, Ornato JP, Berg RA and Investigators NRoCR. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–7. [DOI] [PubMed] [Google Scholar]
- 7.American Hospital Association (AHA). AHA Annual Survey Database Fiscal Year 2010 and 2013. AHA website. https://www.ahadataviewer.com/book-cd-products/aha-survey. Accessed March 8, 2018.
- 8.American Hospital Association (AHA). AHA Registration Requirements for Hospitals. AHA website. https://www.aha.org. Accessed February 28, 2018.
- 9.American Hospital Association (AHA). AHA Estimation Process. AHA website. https://www.ahadataviewer.com. Accessed February 28, 2018.
- 10.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP and Initiative S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7. [DOI] [PubMed] [Google Scholar]
- 11.Zeger SL and Liang KY. An overview of methods for the analysis of longitudinal data. Stat Med. 1992;11:1825–39. [DOI] [PubMed] [Google Scholar]
- 12.van Buuren S Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16:219–42. [DOI] [PubMed] [Google Scholar]
- 13.Stine RA. Bootstrap Prediction Intervals for Regression. Journal of the American Statistical Association. 1983;80:1026–1031. [Google Scholar]
- 14.Donoghue A, Berg RA, Hazinski MF, Praestgaard AH, Roberts K, Nadkarni VM and Investigators AHANRoC. Cardiopulmonary resuscitation for bradycardia with poor perfusion versus pulseless cardiac arrest. Pediatrics. 2009;124:1541–8. [DOI] [PubMed] [Google Scholar]
- 15.HCUP Fast Stats. Healthcare Cost and Utilization Project (HCUP). August 2018.
- 16.Knudson JD, Neish SR, Cabrera AG, Lowry AW, Shamszad P, Morales DL, Graves DE, Williams EA and Rossano JW. Prevalence and outcomes of pediatric in-hospital cardiopulmonary resuscitation in the United States: an analysis of the Kids’ Inpatient Database*. Crit Care Med. 2012;40:2940–4. [DOI] [PubMed] [Google Scholar]
- 17.Khera R, Spertus JA, Starks MA, Tang Y, Bradley SM, Girotra S and Chan PS. Administrative Codes for Capturing In-Hospital Cardiac Arrest. JAMA Cardiol. 2017;2:1275–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Caen AR, Berg MD, Chameides L, Gooden CK, Hickey RW, Scott HF, Sutton RM, Tijssen JA, Topjian A, van der Jagt É, Schexnayder SM and Samson RA. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S526–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.