Abstract
Objective: To determine the reliability of peak VO2 testing for individuals with spinal cord injury (SCI) in deep water and on land; and to examine the relationship between these two testing conditions.
Design: Reliability study.
Setting: Comprehensive rehabilitation center in Baltimore, MD, USA.
Participants: 17 participants (13 men, 4 women) with motor complete and incomplete SCI. Participants were randomized into either aquatic or arm cycle ergometer first measurements.
Intervention: Pilot study to assess peak VO2.
Outcome measures: Peak VO2 measured with metabolic cart in supported deep water with the addition of Aquatrainer® connection, and on land with arm cycle ergometer. Two trials were conducted for each condition with 48 h separating each test.
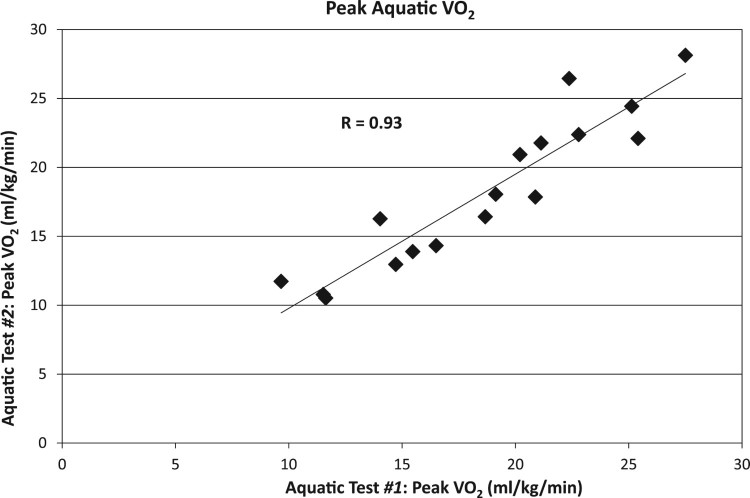
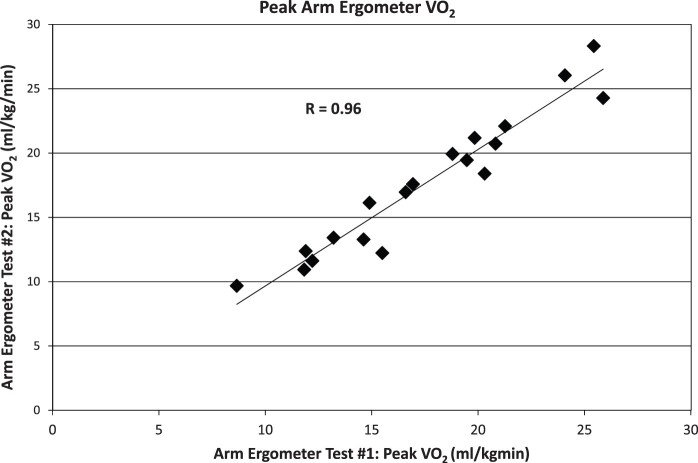
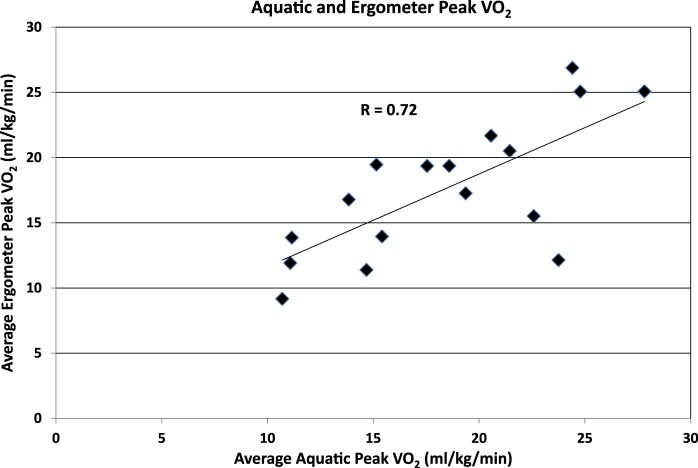
Results: Peak oxygen consumption reliability was statistically significant for both conditions, aquatic (r = 0.93, P < 0.001) and arm cycle ergometry (r = 0.96, P < 0.001). Additionally, aquatic and arm cycle peak VO2 correlation existed (r = 0.72, P < 0.001). For these 17 participants, lower extremity motor score influenced supported, deep water peak VO2, B = 0.57, P < 0.02, whereas age, sex, and weight did not impact deep water or ergometer values.
Conclusion: Determining peak VO2 for individuals with SCI is highly reproducible for arm cycle ergometry and in deep water assessment. Additionally, aquatic, deep water peak VO2 testing is valid when compared to arm cycle ergometry. Although the peak VO2 relationship between deep water and arm cycle ergometry is high, variance in the two conditions does exist. Therefore, it is important to assess peak VO2 via the same exercise modality utilized in the treatment intervention.
Keywords: Reliability, Validity, SCI, Exercise test, Aquatic test
Introduction
Due to inactivity people with spinal cord injury (SCI) are at greater cardiorespiratory health risk than the able body population.1 Approximately 50% of patients with SCI report no leisure-time physical activity and 15% report leisure-time physical activity below the threshold where meaningful health benefits could be realized.2 The study of Van der Berg et al.3 reported people who are wheelchair dependent (e.g. with spinal cord injury) display activity levels 40% lower than non-wheelchair users. Exercise recommendations for people with SCI4 highlight the importance of aerobic exercise. It is advised people with SCI undertake at least 30 min of moderate intensity activity, five days a week. An alternative recommendation would be the performance of vigorous aerobic exercise at least for 20 min, three days a week. Adherence to either of these recommendations facilitates aerobic capacity improvement for people with SCI.5 There is also evidence exercise in people with chronic SCI is effective in improving physical capacity and strength.6 To engage in effective therapeutic and wellness exercise programs safe and efficient cardiorespiratory baseline and outcome testing methods are needed.
Several studies examined peak oxygen consumption in individuals with SCI using arm cycle ergometry, functional electrical stimulation (FES) cycling and rowing,7 robotic assisted treadmill exercise,8 body weight supported treadmill training9 and wheelchair ergometry.10 Systematic review by Eerden et al.11 indicated an incremental arm ergometry test protocol with small individualized increases per stage seemed preferable for testing aerobic capacity. Arm cycle ergometry is one of the most commonly used among SCI population.11 It is a reliable, valid, and sensitive outcome measure for individuals with SCI.12 However, arm ergometry testing fails to incorporate whole body musculature and is difficult to complete for individuals with hand dysfunction, which might lead to potential underrepresentation of peak oxygen consumption.
The aquatic testing environment provides buoyancy and supports whole body muscle activation, in contrast to predominately upper extremity and limited trunk contraction during arm cycle ergometry. The hydrodynamic principles, particularly buoyancy,13 makes deep water an ideal environment to test cardiorespiratory responses in individuals with different chronic disabilities, who may be able to increase movement with gravity reduced. Water makes it easier for people with SCI to move and execute motor skills not possible on land.14 By permitting all muscles to contribute to the aerobic challenge via buoyancy support, a true peak cardiorespiratory measurement may be obtained. The aquatic environment also provides an optimal rehabilitation arena for pulmonary function15 strengthening, balance, and walking performance16 for people with SCI. Additionally, during cardiorespiratory testing hydrostatic pressure increases blood flow return from the periphery, and resists inhalation providing a training affect, and facilitates exhalation.16,17
A recent systematic review with meta-analysis showed weak evidence supporting aquatic exercise effectiveness to improve aerobic fitness17 which may reflect lack of in pool assessment methods, and not be a true reflection of cardiorespiratory gains. During our clinical work measuring peak VO2 in individuals with SCI, we noticed arm cycle ergometry testing did not reflect the clinical gains we observed with aquatic aerobic conditioning, and we began our attempts to match treatment and testing conditions. The published Aquatrainer® validation occurred with healthy younger indivdiuals.18 To our knowledge this is the first study to assess peak oxygen consumption in individuals with SCI in an aquatic, deep water environment. This study assessed the reliability of peak VO2 values during deep water exercise in individuals with SCI and its validity in comparison to an accepted exercise modality (arm cycle ergometry) in this population.
Methods
Participants
This study took place at a university affiliated comprehensive rehabilitation center. We certify all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. The associated university institutional review board (IRB) approved the study. Participants were recruited as a convenience sample from the outpatient population served by the center. Seventeen individuals (13 men, 4 women) with SCI enrolled in this pilot study. Nine individuals were classified as paraplegia with SCI levels documented at T1-T12 (n = 8) and L1 (n = 1). American Spinal Injury Association Impairment Scale (ASIA) classification included five people with A and B, four with C, and eight with D Table 1.
Table 1. Demographics, n = 17.
| Min | Max | Mean | SD | |
|---|---|---|---|---|
| Age (yrs) | 25 | 59 | 45.7 | 11.6 |
| Body Weight (kg) | 56.8 | 136.3 | 80.6 | 19.0 |
| Body Mass Index | 18.4 | 44.5 | 26.1 | 5.9 |
| Time Since Injury (yrs) | 1 | 46 | 13.7 | 13.1 |
| LEMS (0–50) | 0 | 47 | 21.1 | 17.4 |
yrs, years; kg, kilograms; LEMS, lower extremity motor score.
The inclusion criteria were as follows: age between 18 and 65 years; competency to provide informed consent; chronic (greater than six months) history of spinal cord injury from C4 through L1, ability to follow two or three step instructions. Exclusion criteria were as follows: stage III or greater open skin wound; pulmonary or cardiac disease compromising safe aerobic exercise participation; and based on the investigators’ clinical judgment, any other medical comorbidity precluding safe participation. All participants received study information and signed consent forms approved by the University of Maryland Baltimore Institutional Review Board.
Volunteer participants who met our criteria completed both: arm cycle ergometry and aquatic, deep water testing with each testing condition repeated, with 48 h interval between each cardiorespiratory assessment. Participants were asked to abstain from smoking and consuming alcohol or caffeine 48 h prior to the testing, and to avoid strenuous exercise 12 h prior testing. Individuals were randomized into test order to avoid training bias for VO2 assessment, possibly confounding the outcome data.
Aquatic deep water peak VO2 testing
All participants completed a 20-minute aquatic acclimation training session before two deep water peak exercise tests. The tests were conducted at a water depth of 2.13 m and temperature at 31–32°C. We used the Aquatrainer® unit (Cosmed, Rome, Italy), previously validated for gas analysis in healthy professional swimmers,18 to measure peak oxygen consumption. We added a ceiling mounted track system to provide support for the Aquatrainer® allowing forward and backward movement. Aquatic equipment selection (flotation belt, dumbbells, and weights) occurred during acclimation session and precisely duplicated between tests to insure reproducible testing procedures. Foam dumbbells for upper extremity resistance and weights were used, if needed, to prevent feet from floating. The participant was stabilized in the deep water by attaching an elastic band, affixed between the pool ladder and the flotation waist belt. The position of the participant in the pool was as described for deep water running testing.19 One research staff member insured protocol participant vertical positioning, and test safety (Fig 1).
Figure 1.
Deep water peak VO2 test displaying participant, researcher, and testing equipment.
The aquatic test was performed with systematic movement cadence adjustments to create increased work rates. The initial stage incorporated a three-minute warm-up with the movement cadence set at 40 bpm. The work rate (cadence) was adjusted by ten beats every minute until the participant reached volitional fatigue or failed to maintain the cadence. Participants performed running movements using all innervated musculature (arms, trunk, and legs). Upper extremity movement synchronized with each selected metronome cadence during the exercise test.
Arm cycle ergometry testing
Participants completed two peak arm cycle ergometer tests on a standard desktop mounted device (Monark®, Vansbro, Sweden). A three-minute warm-up phase was performed during the initial exercise stage with the work rate set at zero watts and the pedal cadence maintained at 50-rpm. The work rate was increased by five watts every minute after the warm-up until the participant reached volitional fatigue or failed to maintain the pedal cadence (50- rpm) at the selected work rate. Hand stability positioning straps were used during arm cycle ergometry as needed.
For both test conditions participants identified perceived exertion rating (RPE) at each test endpoint using the Borg Scale. Termination of each test occurred with volitional fatigue or if the participant was unable to perform the required work rate.
Peak VO2 value determination
During both, aquatic and arm cycle ergometer peak VO2 tests, air flow and gas exchange data were continuously monitored with a metabolic cart (Cosmed, Rome, Italy). A computer software program integrated the data to determine VO2, VCO2, pulmonary ventilation and respiratory exchange ratio (RER) on a breath by breath basis. Our VO2 peak value was calculated using the average of three highest consecutive ten second sampling points.
Statistical analyses
Test-retest reliability for both aquatic deep water and arm cycle ergometry oxygen consumption was determined. A correlation coefficient indicated the reliability of the repeated measures for the peak VO2 measurements in each setting separately. The relationship between aquatic deep water and arm cycle ergometry was evaluated with Pearson coefficient correlation. Multiple regression assessed the demographic factors potentially impacting deep water and arm ergometer peak VO2 outcomes. The statistical significance was set at P < 0.05 for all tests. Number of participants needed arose from our previous work assessing peak VO2 arm cycle ergometry and robotically assisted body weight support locomotor psychometrics.9
Results
Peak VO2
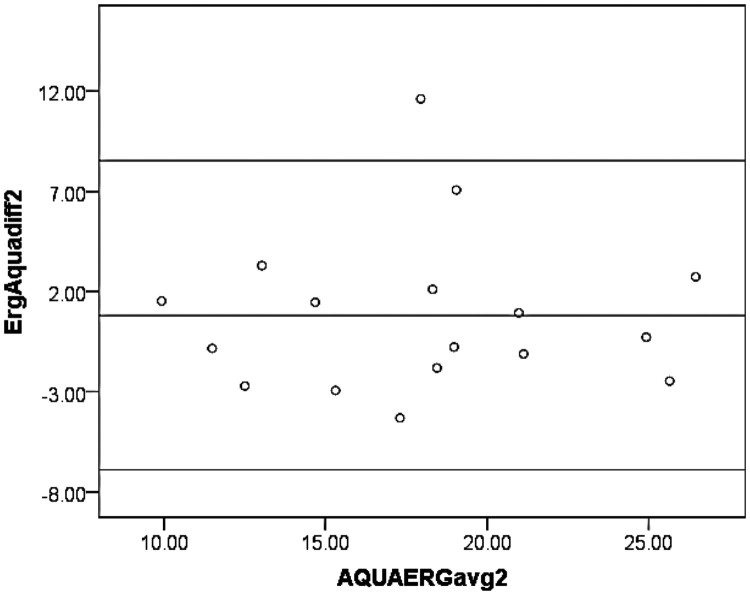
Seventeen participants, 13 men and 4 women, completed two sessions each of deep water and arm cycle ergometry peak VO2 testing. Individuals varied widely in their peak VO2 measurements. For the peak VO2 deep water condition, results extended from 9.66 to 25.88 ml/kg/min with test 1 average equaling 18.63 ± 5.26, and 10.52–28.13 with an average of 18.17 ± 5.49 for test 2. The arm cycle ergometry results (ml/kg/min) ranged from 8.66 to 25.88 for test 1 average equaling 17.54 ± 5.00 and 9.68–28.32 with an average of 17.68 ± 5.55 for test 2. Peak oxygen consumption correlated clinically and statistically significantly for both conditions, aquatic (r = 0.93, P < 0.001) and arm cycle ergometry (r = 0.96, P < 0.001) (Figs 2 and 3). Aquatic and arm cycle peak VO2 correlation existed at (r = 0.72, P < 0.001) (Fig 4). To thoroughly assess the data relationships Bland–Altman statistics were applied with no statistical impact (Fig 5). Table 2 provides means, standard deviation, standard error, and 95% confidence intervals for aquatic and ergometer test 1 and 2 data. No significant differences were observed between test 1 and 2 in either exercise modality. No significant differences occurred between cardiorespiratory testing modalities.
Figure 2.
Test-retest reliability of peak oxygen consumption (peak VO2) obtained during aquatic exercise. Each data point represents an individual subject.
Figure 3.
Test-retest reliability of peak oxygen consumption (peak VO2) obtained during arm cycle ergometer exercise. Each data point represents an individual subject.
Figure 4.
Correlation between peak oxygen consumption (peak VO2) obtained during aquatic and arm ergometer tests. Values of the x and y coordinates for each subject represent the averages of the two trials for each testing modality.
Figure 5.
Bland-Altman Plot for peak VO2 data for all subjects. Means and ± 2 standard deviation lines are drawn.
Table 2. Paired samples test.
| Paired samples test (Paired differences) | ||||||
|---|---|---|---|---|---|---|
| Mean | Standard deviation | Standard error of mean | 95% Confidence interval | |||
| lower | upper | p value | ||||
| Aquatic (test 1–2) | 0.46 | 1.98 | 0.48 | −0.56 | 1.48 | 0.36 |
| Ergometer (test 1–2) | −0.13 | 1.56 | 0.38 | −0.93 | 0.67 | 0.73 |
| *Aquatic – Ergometer | 0.79 | 3.94 | 0.96 | −1.23 | 2.82 | 0.42 |
*(Test 1 + Test 2)/2.
We hypothesized a priori lower extremity motor score (LEMS), age, and weight could potentially impact peak VO2 outcomes in both conditions. For these 17 participants, only LEMS influenced supported deep water, peak VO2 (B = 0.58, P < 0.02). It is important to note for these calculations we used ml/min instead of ml/kg/min as body size might also have impacted the data, therefore including it in peak volume calculations as well as a separate weight factor would confound the regression results. The LEMS scores for eight individuals with tetraplegia was 30.5 (SD 15.23), and the nine participants with paraplegia equaled 12.67 (SD 15.20) with a p value equaling 0.03. The ASIA classification level peak VO2 average (ml/kg/min) for combined levels A and B: aquatic = 17.54 ± 5.01, arm cycle = 16.36 ± 5.39; level C: aquatic=14.74 ± 3.45, arm cycle = 14.34 ± 3.11; and level D: aquatic = 20.77 ± 5.46, arm cycle = 20.03 ± 5.26.
Rate perceived exertion (RPE)
Aquatic peak tests RPE (n = 13) reliability demonstrated a significant correlation, (R = 0.85, P = 0.001), and arm cycle ergometer peak testing rate of perceived exertion (n = 15) reliability also portrayed a significant relationship, (R = 0.91, P = 0.001). Participants consistently reported RPEs (n = 11) between aquatic and arm cycle ergometer modalities with aquatic RPE average equaling 17.41 (SD 2.88) and an arm cycle RPE average of 18.50 (SD 1.75), (R = 0.80, P = 0.003).
Discussion
To date, this is the first published study to evaluate the reliability of peak oxygen consumption in the aquatic setting for people with SCI and to investigate its relationship to arm cycle ergometry. Our findings show reliable peak VO2 results during deep water and peak arm cycle ergometry tests and between exercise modalities in individuals with chronic SCI. Aquatic, deep water peak VO2 testing can be used as an alternative exercise modality in individuals with SCI who are unable to follow a treadmill protocol, or their hand function does not permit adequate grip for arm ergometry testing. Additionally, proper assessment of aquatic cardiorespiratory adaptations may be enhanced by matching intervention with testing modality. Aquatic therapy or exercise is frequently employed for cardiorespiratory and strength training with individuals with SCI17 therefore it is essential to use a reliable tool to assess peak oxygen consumption as a surrogate marker of cardiorespiratory fitness.
Arm cycle ergometry is accepted as one standard metric to measure peak oxygen consumption.20 Gorman et al.9 evaluated reliability of peak VO2 assessments during body weight supported treadmill training and its validity as compared to arm cycle ergometry in people with chronic motor incomplete SCI. Jack et al.8 compared arm ergometry with robotic assisted treadmill exercise in ten individuals. Both studies showed statistically significant correlation, concluding that both testing conditions are reliable for peak VO2 measurement. In our study, we also found statistically significant correlation between aquatic deep water and arm ergometry peak VO2 testing (P < 0.002).
Deep water testing allows peak oxygen consumption measurement for people with SCI and can accommodate all levels of injury. Nagle et al.21 report moderate correlation for peak oxygen consumption in shallow water and on land in healthy individuals and suggest developing standardized non-swimming protocols to accurately measure cardiorespiratory fitness in the aquatic setting. Phillips et al.22 report lower peak heart rate and oxygen consumption during maximal exercise intensities while deep water running compared to treadmill walking for older, overweight women. Simmons et al.23 established reference values of cardiorespiratory fitness for untrained individuals with SCI demonstrating values of 8.8 ml/kg/min (tetraplegia) and 16.0 ml/kg/min (paraplegia). Our study group consisted of nine individuals with paraplegia and eight people with tetraplegia with an overall mean peak VO2 above 17 ml/kg/min indicating we tested higher functioning individuals. It is important to understand LEMS data demonstrated a stronger relationship to peak VO2 than ASIA impairment scale levels and paraplegia or tetraplegia classification. Our observations indicate many factors may impact cardiopulmonary conditioning including daily activity levels, personality, available peer and family support and other mitigating features not easily quantified.
Self-reported exertion scale data demonstrated consistent results within each testing condition and across testing conditions with exertion level of arm cycle ergometry reported slightly higher than in the water environment. It is unclear however if this consistency is an accurate reflection of workload. We noted several participants consistently reporting in both testing conditions high RPE scores but did not appear to be working near their full cardiorespiratory potential. Conversely a few individuals reported moderate RPE levels but demonstrated signs of working near their maximum cardiorespiratory abilities.
Main limitation of our study is small sample size. Additional participants would allow injury level stratification to critically assess if deep water peak VO2 testing differences exist between individuals across injury levels.
Conclusions
Identifying and assessing methods for individuals with SCI to maintain cardiorespiratory fitness is essential to a health and wellness paradigm. Paralleling Li’s findings17 and the work of Jung et al.,15 we demonstrated one protocol measuring VO2 in deep water in individuals with SCI to be a safe option for cardiorespiratory testing. During aquatic cardiorespiratory training and assessment buoyancy supports more musculature recruitment. Also, higher cardiorespiratory demands occur as hydrostatic pressure increases fluid return to vascular system and the vertical position allows the diaphragm to work more efficiently than in the seated arm ergometer position. The moderate relationship between land and aquatic cardiorespiratory testing aligns with our premise that the testing condition should match the training condition when possible as the hydrodynamic principles impact both cardiorespiratory training and testing for individuals with SCI. This technique allows us to test what is actually occurring from a cardiorespiratory response during aquatic deep water training.
Working collaboratively with multi-disciplinary healthcare practitioners and community fitness personnel to assess cardiorespiratory function prior to and post aquatic activity enables critical fitness level evaluation. Annual fitness assessment and the requisite intervention for individuals with spinal cord injury cardiorespiratory fitness may potentially limit secondary complications due to inactivity and compromised cardiorespiratory fitness.
Determining peak VO2 in deep water for individuals with SCI and using arm cycle ergometry are both highly reproducible. Additionally, aquatic deep water peak VO2 testing is valid when compared to arm cycle ergometry. To optimally obtain and document treatment efficacy it is important to assess peak VO2 after aquatic intervention paralleling the treatment conditions. Both deep water and arm cycle ergometer provide reliable and valid peak VO2 outcomes to measure clinical change with individuals with spinal cord injury. Deep water peak VO2 testing could optimally measure cardiorespiratory fitness outcomes for individuals with other chronic conditions with muscle weakness such as cerebral vascular accident, cerebral palsy, and multiple sclerosis.
Acknowledgements
We appreciate the time and effort of all patients who eagerly participated in this study. We thank the facilities engineer who constructed our modified Aquatrainer testing system.
Disclaimer statements
Contributors None.
Funding The Kernan Endowment Fund purchased the Aquatrainer and covered testing structural modification cost. Kosciuszko Foundation funded the scholarship for one of the researchers.
Conflicts of interest Authors have no conflicts of interest to declare.
ORCID
Anna Ogonowska-Slodownik http://orcid.org/0000-0002-3318-6513
References
- 1.Kressler J, Cowan RE, Bigford GE, Nash MS.. Reducing cardiometabolic disease in spinal cord injury. Phys Med Rehabil Clin N Am 2014;25(3):573–604. doi: 10.1016/j.pmr.2014.04.006 [DOI] [PubMed] [Google Scholar]
- 2.Miller LE, Herbert W.. Health and economic benefits of physical activity for patients with spinal cord injury. Clinicioecon Outcomes Res 2016;8:551–8. doi: 10.2147/CEOR.S115103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van den Berg-Emons RJ, Bussmann JB, Stam HJ.. Accelerometry-based activity spectrum in persons with chronic physical conditions. Arch Phys Med Rehabil 2010;91(12):1856–61. doi: 10.1016/j.apmr.2010.08.018 [DOI] [PubMed] [Google Scholar]
- 4.Tweedy SM, Beckman EM, Geraghty T, Theisen D, Perret C, Harvey LA, et al. Exercise and sports science Australia (essa) position statement on exercise and spinal cord injury. J Sci Med Sport 2017;20(2):108–15. doi: 10.1016/j.jsams.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 5.Pelletier CA, Totosy de Zepetnek JO, MacDonald MJ, Hicks AL.. A 16-week randomized controlled trial evaluating the physical activity guidelines for adults with spinal cord injury. Spinal Cord 2015;53(5):363–7. doi: 10.1038/sc.2014.167 [DOI] [PubMed] [Google Scholar]
- 6.Hicks AL, Martin Ginis KA, Pelletier CA, Ditor DS, Foulon B, Wolfe DL.. The effects of exercise training on physical capacity, strength, body composition and functional performance among adults with spinal cord injury: a systematic review. Spinal Cord 2011;49(11):1103–27. doi: 10.1038/sc.2011.62 [DOI] [PubMed] [Google Scholar]
- 7.Verellen J, Vanlandewijck Y, Andrews B, Wheeler GD.. Cardiorespiratory responses during arm ergometry, functional electrical stimulation cycling, and two hybrid exercise conditions in spinal cord injured. Disabil Rehabil Assist Technol 2007;2(2):127–32. doi: 10.1080/09638280600765712 [DOI] [PubMed] [Google Scholar]
- 8.Jack LP, Purcell M, Allan DB, Hunt KJ.. Comparison of peak cardiopulmonary performance parameters during robotics-assisted treadmill exercise and arm crank ergometry in incomplete spinal cord injury. Technol Health Care 2010;18(4–5):285–96. [DOI] [PubMed] [Google Scholar]
- 9.Gorman PH, Geigle PR, Chen K, York H, Scott W.. Reliability and relatedness of peak VO2 assessments during body weight supported treadmill training and arm cycle ergometry in individuals with chronic motor incomplete spinal cord injury. Spinal Cord 2014;52(4):287–91. doi: 10.1038/sc.2014.6 [DOI] [PubMed] [Google Scholar]
- 10.Tørhaug T, Brurok B, Hoff J, Helgerud J, Leivseth G.. Clinical study arm crank and wheelchair ergometry produce similar peak oxygen uptake but different work economy values in individuals with spinal cord injury. Biomed Res Int 2016;10:1–7. doi: 10.1155/2016/5481843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eerden S, Dekker R, Hettinga FJ.. Maximal and submaximal aerobic tests for wheelchair-dependent persons with spinal cord injury: a systematic review to summarize and identify useful applications for clinical rehabilitation. Disabil Rehabil 2017;3:1–25. [DOI] [PubMed] [Google Scholar]
- 12.Myers J, Lee M, Kiratli J.. Cardiorespiratory disease in spinal cord injury. Am J Phys Med Rehabil 2007;86(2):142–52. doi: 10.1097/PHM.0b013e31802f0247 [DOI] [PubMed] [Google Scholar]
- 13.Brody LT, Geigle PR.. Aquatic exercise for rehabilitation and training. Champaign, IL: Human Kinetics 2009. [Google Scholar]
- 14.Iucksch D, Israel V, Ribas D, Manffra E.. Gait characteristics of persons with incomplete spinal cord injury in shallow water. J Rehabil Med 2013;45(9):860–5. doi: 10.2340/16501977-1193 [DOI] [PubMed] [Google Scholar]
- 15.Jung J, Chung E, Kim K, Lee B, Lee J.. The effects of aquatic exercise on pulmonary function in patients with spinal cord injury. J Phys Ther Sci 2014;26:707–9. doi: 10.1589/jpts.26.707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stevens SL, Caputo JL, Fuller DK, Morgan DW.. Effects of underwater treadmill training on leg strength, balance, and walking performance in adults with incomplete spinal cord injury. J Spinal Cord Med 2014;38(1):91–101. doi: 10.1179/2045772314Y.0000000217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li C, Khoo S, Adnan A.. Effects of aquatic exercise on physical function and fitness among people wit*h spinal cord injury. Medicine 2017;96(11):e6328–6. doi: 10.1097/MD.0000000000006328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baldari C, Fernandes R, Meucci M, Ribeiro J, Vilas-Boas JP, Guidetti L.. Is the new aquatrainer® snorkel valid for VO2 assessment in swimming? Int J Sports Med 2013;34(04):336–44. [DOI] [PubMed] [Google Scholar]
- 19.Cuesta-Vargas AI, Heywood S.. Aerobic fitness testing in chronic nonspecific low back pain. Am J Phys Med Rehabil 2011;90(12):1030–5. doi: 10.1097/PHM.0b013e318238a29c [DOI] [PubMed] [Google Scholar]
- 20.Bulthuis Y, Drossaers-Bakker W, Oosterveld F, van der Palen J, van de Laar M.. Arm crank ergometer is reliable and valid for measuring aerobic capacity during submaximal exercise. J Strength Cond Res 2010;24(10):2809–15. doi: 10.1519/JSC.0b013e3181e31242 [DOI] [PubMed] [Google Scholar]
- 21.Nagle EF, Sanders ME, Gibbs BB, Franklin BA, Nagle JA, Prins PJ, et al. Reliability and accuracy of a standardized shallow water running test to determine cardiorespiratory fitness. J Strength Cond Res 2017 Jun;31(6):1669–77. doi: 10.1519/JSC.0000000000001638 [DOI] [PubMed] [Google Scholar]
- 22.Phillips VK, Legge M, Jones LM.. Maximal physiological responses between aquatic and land exercise in overweight women. Med Sci Sports Exerc 2008;40(5):959–64. doi: 10.1249/MSS.0b013e318164d0e0 [DOI] [PubMed] [Google Scholar]
- 23.Simmons OL, Kressler J, Nash MS.. Reference fitness values in the untrained spinal cord injury population. Arch Phys Med Rehabil 2014;95(12):2272–8. doi: 10.1016/j.apmr.2014.06.015 [DOI] [PubMed] [Google Scholar]