Abstract
Background
The apparent rise of antidepressant use seems to be explained to a large extent by an increase in long-term use. Both professionals and patients appear reluctant to discontinue antidepressant medication (ADM). It is not known what factors determine this reluctance.
Aim
This study aimed to identify factors that enable the shared decision-making process about discontinuation of ADM between long-term users and their GPs.
Design and setting
Concept-mapping study of a purposive sample of both patients and professionals from primary and secondary mental health care in the Netherlands.
Method
Concept mapping was used to conceptualise and structure the topics relevant to the discontinuation process from the perspective of both patients and professionals. Participants generated topics in brainstorming sessions and subsequently prioritised and sorted them. Multidimensional scaling and hierarchical cluster analyses were used for the cluster topics.
Results
Thirty-seven patients and 27 professionals generated 50 separate topics. Hierarchical cluster analysis revealed six clusters of topics: ‘Process of discontinuation’, ‘Expectations’, ‘Professional guidance’, ‘Current use’, ‘Environment’, and ‘Side effects’. Patients and professionals came up with largely similar topics. Nevertheless, a difference was found between these groups regarding the perceived importance of professional guidance.
Conclusion
This study yielded an informed selection of the topics that seem most important to discuss when considering whether to discontinue ADM. As perspectives of both patients and professionals were combined, the topics may provide patients and GPs with a broader and more balanced scope of factors to consider, and thus facilitate a better shared decision-making process.
Keywords: antidepressive agents, decision making, deprescriptions, general practice
INTRODUCTION
Antidepressant medicine (ADM) use continues to rise in many countries worldwide.1–4 This seems to be explained mainly by an increase in long-term users.5,6 Despite being effective for some patients in reducing symptoms of depression and anxiety, and the risk of depressive relapse,7 ADM may also have side effects such as sleep disturbance, weight gain, sexual dysfunction, and gastrointestinal bleeding.8,9 In addition, they are sometimes associated with more serious adverse events, such as falls, attempted suicide or self-harm, stroke, and epilepsy.10 Current international guidelines advise to re-evaluate the use of ADM 6 months after remission of a first episode of depression or anxiety, and 1–2 years after a recurrent depression.11 However, many patients are reluctant to discontinue as they fear relapse or recurrence of a depressive or anxiety disorder. Previous unsuccessful attempts to discontinue ADM make it more difficult to stop,12–14 and withdrawal symptoms may easily be misidentified as signs of a relapse. As a possible consequence, both patients and their GPs seem to be reluctant to take the initiative to discuss discontinuation.15 Moreover, providing GPs with patient-tailored multidisciplinary advice to discontinue ADM does not appear to be successful.16 Taken together, it seems that patients may need more information and guidance while professionals may be in need of tools to better taper their support. A shared decision-making (SDM) approach incorporating these elements may make discontinuation more successful. SDM may help patients to be more actively involved, resulting in better health outcomes and healthcare experiences.17,18 Decision aids (DAs) are interventions or tools designed to facilitate SDM and patient participation in healthcare decisions. DAs prepare patients and professionals to discuss options in a structured and informed way. A systematic review19 demonstrated that DAs reduced the proportion of undecided participants and appeared to have a positive effect on patient–clinician communication.
Therefore, the aim of the current study was to identify topics that can shape the dialogue on the discontinuation of ADM, and support the SDM process between long-term users of ADM and their GPs. Subsequently, these themes were included in a concept DA to support the SDM process.
METHOD
A concept-mapping study with patients and healthcare professionals was performed.
Participant recruitment
The study population consisted of both patients and professionals. Patients were recruited from the Dutch patient organisations for depression and anxiety (Depressie Vereniging, and Angst, Dwang en Fobie Stichting). The only inclusion criterion was that patients were current or past users of ADM. Professionals (GPs, primary care mental health assistants, psychiatrists, and psychologists) were recruited through the networks of the Radboud University Medical Centre and professional organisations such as the Dutch Expertise Center for Anxiety and Depression (NedKAD) and the Mental Health Expert Group of Dutch GPs (PsyHAG). Data collection took place from January–November 2016.
How this fits in
| Despite international guidelines advising discontinuation of antidepressant medication, its long-term use continues to rise in many countries worldwide. Both professionals and patients appear reluctant to initiate discontinuation, and seem to be in need of more practical guidance to support this process. This study yields an informed selection of the topics that seem most important to discuss when considering whether to discontinue antidepressants, based on perspectives of both patients and healthcare professionals. Considering a broad and balanced scope of factors before and during discontinuation may facilitate a better shared decision-making process. |
Concept mapping
Data collection and analysis was performed within the framework of concept mapping,20,21 developed to organise diverse ideas into a coherent framework. Through the usage of group processes and joint discussion, it encourages participants to bring up more ideas than would emerge from individual interviews. The internal validity of the method is high and the findings allow identification of similarities and differences between various perspectives.22 The procedure consisted of three stages: generating, prioritising, and sorting topics.
Generation of topics
In this study, participants were encouraged to brainstorm the question: Which topics should be discussed in a consultation between GP and patient about whether or not to discontinue ADM? Two brainstorming sessions were conducted for patients and one for professionals, each lasting 1.5 hours. Participants sat in a focus group-style setup and wrote on pads that were subsequently displayed on several boards. Sessions were guided by one member of the research team. Participants were asked to answer the central question by generating as many relevant topics as possible in silence for 15 minutes. Subsequently, topics were collected and shared. Participants explained and reflected on the topics as a group and were encouraged to add new topics. Then two researchers independently eliminated topics that were unrelated to the question (for example, the use of benzodiazepines) or those that were overlapping. Findings were discussed and any differences were solved by discussion between the researchers until consensus was reached. This procedure resulted in a final list of topics to be used in the following phase.
Prioritising and sorting topics
Prioritising and sorting topics was performed individually on a computer using Ariadne software, which is designed to support concept mapping.23,24 Participants were asked to prioritise the topics by dividing them into five equal groups, group 1 being defined as ‘least important to discuss’, and group 5 as ‘most important to discuss’. Afterwards, sorting took place as each participant was asked to cluster those statements that they considered similar in content. Participants distributed topics over a minimum of two and maximum of 10 clusters. After sorting, the participants were asked to provide a descriptive label for each cluster.
Statistical analysis
Data were analysed using Ariadne and SPSS (version 22). For each topic, average priority scores were calculated based on the individual ratings (1–5) by participants. This was done for the group as a whole, for the patient group, and for the professionals group. The overall priority score was used to construct the concept DA, in conjunction with the clusters resulting from the sorting task (concept DA is available from the authors on request).
To enable an exploration of possible differences in the perspectives of patients versus professionals, the priority ratings of these subgroups were compared with independent samples t-tests. Subsequently, the multidimensional scaling analyses positioned the topics as points in a two-dimensional map, in which the distance between the topics represented how often the participants sorted them into the same group. Thereafter, Ward’s hierarchical cluster analysis20,25,26 was used to create clusters within this point map, ranging from general (few clusters) to specific (many clusters). Because no clearly defined standards exist to determine the number of clusters, this was determined by the researchers. The main criteria were that clusters had to contain meaningful, distinguishable information, and had to consist of ≥3 statements. Labelling was based on the content of the topics included in the clusters.
RESULTS
Participants
To recruit individuals participating from the patient perspective, an email invitation to participate in the study was sent out to two patient organisations for patients with depression and anxiety in the Netherlands, who then sent the invitation on to their members. Forty-one patients from different regions of the Netherlands responded to the research team, of whom 12 were able to participate in one of the two patients’ brainstorming sessions. Subsequently, 25 patients (including all 12 participants from the brainstorming sessions) participated in the prioritising and sorting task.
Professionals were recruited by email invitation through the networks of the Radboud University Medical Center and two professional organisations: NedKAD and PsyHAG. Thirty-nine healthcare professionals responded, of whom 14 participated in the professionals’ brainstorming session. Subsequently, 27 participated in the computerised prioritising and sorting activity (including seven who also participated in the brainstorming). Numbers and characteristics of participants are displayed in Table 1.
Table 1.
Participants attending concept-mapping process to collect topics to discuss discontinuation of antidepressant medication
| Participant characteristics | Patients (n = 37) | Professionals (n = 27) |
|---|---|---|
| Brainstorming session, n | 12a | 14b |
|
| ||
| Prioritising and sorting, n | 37 | 27 |
|
| ||
| Female, % | 51 | 63 |
|
| ||
| Mean agec | — | — |
|
| ||
| Current ADM use, % | 34 | not assessed |
|
| ||
| Profession | ||
| GP, % | — | 37 |
| Psychiatrist, % | — | 37 |
| Mental health nurse, % | — | 15 |
| Psychologist, % | — | 11 |
All 12 brainstorming session patient-participants completed the prioritising and sorting assignment.
Seven brainstorming session professional-participants completed the prioritising and sorting assignment.
Not assessed. ADM = antidepressant medication.
Concept mapping
Generating and prioritising of topics
Patients and healthcare professionals generated 99 topics that were subsequently reduced by two researchers to a final topic set of 50. Prioritising by patients and professionals revealed a top 10 ranking of topics perceived as most useful to discuss from the perspective of both patients and professionals (Table 2). Five of the top 10 topics were considered important by both patients and professionals: ‘Individual dose-reduction schedule’, ‘Relapse prevention’, ‘Fear of relapse’, ‘Provide information about withdrawal symptoms’, and ‘Previous experiences with dose reduction’. Besides these five overlapping topics, the additional topics from the patients’ and professionals’ top 10 were included in the concept DA.
Table 2.
Top 10 topics perceived as most useful to discuss in a consultation regarding discontinuation of antidepressant medication by patients and professionals, followed by their mean and rank order of priority scores
| Topics (top 10)a,b | Patients (n = 37) | Professionals (n = 27) | ||
|---|---|---|---|---|
| Mean | Rank | Mean | Rank | |
| Individual dose-reduction schedule (#22) | 4.43 | 1 | 3.96 | 7 |
| Relapse prevention (#50) | 4.27 | 2 | 4.11 | 4 |
| Current quality of life and psychological functioning (#6) | 4.16 | 3 | 3.74 | 12 |
| Fear of relapse (#11) | 4.03 | 4 | 3.96 | 8 |
| Advantages and disadvantages of discontinuing antidepressants (#3) | 4.03 | 5 | 3.74 | 13 |
| Regular counselling sessions to provide guidance (check-ups) (#43) | 4.00 | 6 | 3.67 | 14 |
| Time period and rate of dose reduction (phasing of the dosage) (#23) | 4.00 | 7 | 3.67 | 15 |
| Provide information about withdrawal symptoms (#17) | 3.95 | 8 | 4.30 | 1 |
| What options are there if things do not go well after you stop (#19) | 3.84 | 9 | 3.33 | 24 |
| Previous experiences with dose reduction (#21) | 3.78 | 10 | 4.19 | 2 |
| Current effect: What effect do you notice from the medicine (for example, calm, balanced, flat) and what do you think of that? (#12) | 3.65 | 12 | 4.11 | 5 |
| Expectations: What do you hope to achieve? (#1) | 3.65 | 13 | 3.93 | 10 |
| Reason(s) to stop taking antidepressants (#4) | 3.65 | 14 | 4.11 | 6 |
| Suicidality (#8) | 3.54 | 20 | 4.15 | 3 |
| Signalling plan: Which situations do not go so well, what happens, what can you do about it? (#18) | 3.51 | 23 | 3.93 | 9 |
# = topic number from Figure 1.
Fifteen topics listed as both patient and professional groups provided five of the same topics within their top 10.
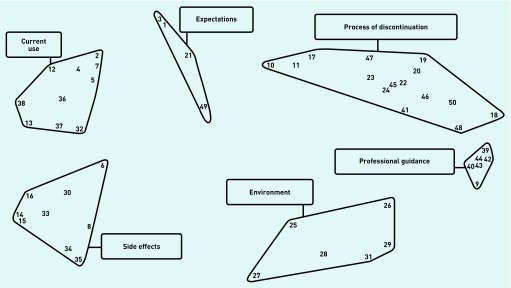
Sorting of topics in clusters
A six-cluster solution was considered to reflect the best balance between ‘being specific’ and ‘being substantial’. For each of the final six clusters the authors formulated a descriptive title based on the content of its topics.20 This resulted in the following clusters: ‘Process of discontinuation’, ‘Expectations’, ‘Professional guidance’, ‘Current use’, ‘Environment’ (for example, social context and work), and ‘Side effects’ (see Table 3 for their constituent topics). The point cluster map can be seen in Figure 1. In the process of selecting the optimal number of clusters, the authors considered a five, six, and seven-cluster solution. A cluster solution containing five clusters resulted in a combination of the clusters ‘Expectations’ and ‘Current use’, which were considered to be both meaningful and distinguishable clusters. The seven-cluster solution singled out one topic: ‘Primary care guideline depression’ from the ‘Expectations’ cluster. This was not considered to be substantial enough, and therefore a six-cluster solution was preferred over a seven-cluster solution.
Table 3.
Clusters and topics, and their priority scores (ranging from 1–5), as provided by patients and professionals
| Clustera,b | Mean priority (SD) all participants | Mean priority patients | Mean priority professionals | Effect size differencec (Cohen’s d) |
|---|---|---|---|---|
| Process of discontinuation | 3.41 (0.37) | 3.45 | 3.36 | 0.25 |
| Individual dose-reduction schedule (#22) | 4.23 (0.96) | 4.43 | 3.96 | 0.49d |
| Relapse prevention (#50) | 4.20 (1.04) | 4.27 | 4.11 | 0.15 |
| Provide information about withdrawal symptoms (#17) | 4.09 (1.04) | 3.95 | 4.30 | 0.35 |
| Fear of relapse (#11) | 4.00 (1.10) | 4.03 | 3.96 | 0.07 |
| Time period and rate of dose reduction (phasing of the dosage) (#23) | 3.86 (1.34) | 4.00 | 3.67 | 0.25 |
| Signalling plan: Which situations do not go so well, what happens, what can you do about it? (#18) | 3.69 (1.08) | 3.51 | 3.93 | 0.40 |
| What options are there if things do not go well after you stop? (#19) | 3.63 (1.18) | 3.84 | 3.33 | 0.44 |
| You can start again, if you are not able to cut back/it is OK if you cannot stop/you have not failed if you change your mind (#20) | 3.52 (1.18) | 3.41 | 3.67 | 0.23 |
| How to continue without antidepressants, offer alternatives (#47) | 3.48 (1.30) | 3.51 | 3.44 | 0.05 |
| What is needed to build up the patient’s personal strengths? (#48) | 3.28 (1.29) | 3.27 | 3.30 | 0.02 |
| What would your life look like without medication? (#10) | 2.81 (1.26) | 3.14 | 2.37 | 0.64d |
| The patient’s expectations about the role of their GP (#41) | 2.73 (1.10) | 2.89 | 2.52 | 0.35 |
| Other therapeutic options (#46) | 2.64 (1.29) | 2.57 | 2.74 | 0.13 |
| Possible (temporary) alternative medication (such as sleep medication) (#45) | 2.59 (1.15) | 2.68 | 2.48 | 0.17 |
| Explanation of tapering strips (if available) (#24) | 2.34 (1.43) | 2.19 | 2.56 | 0.26 |
| Expectations | 3.35 (0.56) | 3.28 | 3.45 | 0.31 |
| Previous experiences with dose reduction (#21) | 3.95 (1.08) | 3.78 | 4.19 | 0.39 |
| Advantages and disadvantages of discontinuing antidepressants (#3) | 3.91 (1.15) | 4.03 | 3.74 | 0.25 |
| Expectations: What do you hope to achieve? (#1) | 3.77 (1.14) | 3.65 | 3.93 | 0.25 |
| The guideline of the Dutch College of General Practitioners: What does it say about antidepressants? (#49) | 1.78 (1.03) | 1.65 | 1.96 | 0.29 |
| Professional guidance | 3.34 (0.59) | 3.47 | 3.15 | 0.56d |
| Regular counselling sessions to provide guidance (check-ups) (#43) | 3.86 (1.10) | 4.00 | 3.67 | 0.30 |
| Supervision: Who is going to supervise the dose reduction? (#39) | 3.58 (1.22) | 3.65 | 3.48 | 0.14 |
| How quickly can the person providing counselling be contacted? (#44) | 3.56 (1.20) | 3.59 | 3.52 | 0.06 |
| What support would help you reduce your medication? (#9) | 3.48 (1.23) | 3.59 | 3.33 | 0.21 |
| Option of accompanying counselling sessions with, for example, a psychologist (#42) | 2.95 (1.30) | 3.15 | 2.19 | 1.21e |
| Sessions with POH-GGZ (GP support division of the Dutch Mental Healthcare Association) (#40) | 2.58 (1.31) | 2.46 | 2.74 | 0.22 |
| Current use | 3.28 (0.47) | 3.21 | 3.36 | 0.32 |
| Current effect. What effect do you notice of the medicine (that is, calm, balanced, flat) and what do you think of that? (#12) | 3.84 (1.07) | 3.65 | 4.11 | 0.44 |
| Reason(s) to stop taking antidepressants (#4) | 3.84 (1.19) | 3.65 | 4.11 | 0.40 |
| Current side effects of medication (#13) | 3.67 (1.20) | 3.54 | 3.85 | 0.26 |
| Advantages and disadvantages of using antidepressants (#2) | 3.52 (1.17) | 3.59 | 3.41 | 0.15 |
| Other medication and possible interaction with antidepressants (#32) | 3.33 (1.21) | 3.30 | 3.37 | 0.06 |
| How many previous depressive episodes has the patient had? (#37) | 3.05 (1.40) | 2.84 | 3.33 | 0.35 |
| Meaning of ADM in your life (#7) | 2.97 (1.17) | 3.00 | 2.93 | 0.06 |
| Why was the patient initially prescribed ADM, original indication(depression, anxiety, other reasons) (#36) | 2.95 (1.34) | 3.14 | 2.70 | 0.32 |
| Attribution: What according to the patient caused the complaint(s)? (#5) | 2.84 (1.34) | 2.54 | 3.26 | 0.57d |
| Duration of ADM use: How long has the patient been using antidepressants? (#38) | 2.73 (1.16) | 2.89 | 2.52 | 0.32 |
| Environment | 2.67 (0.58) | 2.68 | 2.66 | 0.03 |
| Ensure stable life circumstances during reduction (no life event) (#26) | 3.48 (1.17) | 3.57 | 3.37 | 0.17 |
| Involve partner and social environment (#29) | 3.28 (1.02) | 3.11 | 3.52 | 0.41 |
| Can patients count on support from social environment if they struggle? (#31) | 3.16 (1.12) | 3.11 | 3.22 | 0.10 |
| Attitude of the social environment (partner, friends, colleagues) towards reduction or use of antidepressants (#28) | 2.41 (1.15) | 2.24 | 2.63 | 0.34 |
| Situation at work (#27) | 2.05 (1.06) | 2.32 | 1.67 | 0.64d |
| Suitable time of year (#25) | 1.64 (0.88) | 1.70 | 1.56 | 0.16 |
| Side effects | 2.52 (0.53) | 2.49 | 2.56 | 0.13 |
| Current quality of life and psychological functioning (#6) | 3.98 (1.03) | 4.16 | 3.74 | 0.41 |
| Suicidality (#8) | 3.80 (1.30) | 3.54 | 4.15 | 0.49 |
| Problems with emotions (emotional blunting) (#16) | 3.05 (1.10) | 3.27 | 2.74 | 0.50d |
| Genetic vulnerability for depression (#30) | 2.41 (1.37) | 2.59 | 2.15 | 0.33 |
| Problems with sexuality (#14) | 2.36 (1.13) | 2.32 | 2.41 | 0.08 |
| Addiction(s) (#34) | 1.95 (1.15) | 1.68 | 2.33 | 0.57c |
| Problems with weight (#15) | 1.92 (1.03) | 1.81 | 2.07 | 0.25 |
| Chance of falls: Has patient ever had a fall? (#33) | 1.52 (0.82) | 1.32 | 1.78 | 0.56c |
| Smoking and/or drinking (#35) | 1.70 (1.17) | 1.73 | 1.67 | 0.06 |
# = topic number from Figure 1
Priority scores of the clusters were calculated based on the average of constituent topics.
Difference in mean priority scores between patients and professionals.
P<0.05.
P<0.01. ADM = antidepressant medication. SD = standard deviation.
Figure 1.
Six-cluster map showing the distribution of topics that are considered important to discuss in a consultation between GP and patient about whether or not to discontinue antidepressant medication. Each number represents a topic, and distance between the topics represents how often participants sorted them into the same group. For details see Table 3.
Differences between patients’ and professionals’ perspectives
An overview of the clusters and their corresponding topics, sorted by participants’ priority scores, is presented in Table 3. Concerning the priorities of clusters, independent samples t-tests showed that there were no significant differences between patients’ and professionals’ ratings for five out of six clusters. One significant difference in cluster priority ratings between patients and professionals did emerge: patients perceived the cluster ‘Professional guidance’ significantly more useful to discuss than professionals did.
This significant difference seemed to be driven primarily by the topic ‘Option of accompanying counselling sessions with, for example, a psychologist’. This topic was significantly more relevant to patients with a large effect size (Cohen’s d = 1.21). Other topics that were also significantly more useful to patients than professionals, but with a moderate effect size, were: ‘Problems with emotions’, ‘What would your life look like without medication?’, and ‘Situation at work’. Topics that were significantly more useful from the perspective of the professionals, with moderate effect sizes, were: ‘Attribution: What according to the patient caused the complaint(s)?’, ‘Chance of falls’, and ‘Addiction(s)’.
Concept decision aid
Largely based on International Patient Decision Aid Standards criteria,27,28 a concept DA was developed. The DA was constructed by selecting the topics with the highest priority ratings — that is, the top 10 as rated by patients plus the top 10 by professionals — and presenting these within the clusters that emerged from the sorting phase. The top two topics from the cluster ‘Environment’ were added to the DA. Although not top 10 ranked, they were included to ensure the DA also accommodates patients for whom environment (for example, life events, social support) is a relevant issue and because it might be easily overlooked.
DISCUSSION
Summary
The aim of this study was to identify the most important themes to discuss between patients and GPs when deciding whether or not to discontinue ADM. Six core themes were identified that may support the dialogue between patients and their GPs: ‘Process of discontinuation’, ‘Expectations’, ‘Professional guidance’, ‘Current use’, ‘Environment’, and ‘Side effects’.
Strengths and limitations
To the authors’ knowledge, this is the first study to explore what issues should be discussed with regard to tapering and discontinuing ADM. The concept-mapping method is an established method for rigorously exploring differing themes and perspectives among participants, combining both qualitative and quantitative aspects. As a result, the reliability of these findings is supported by the fact that they have included both patients and professionals.
Obviously, the current study also has its limitations. For example, caution should be taken in generalising differences to other countries, as participants and situations are specific to the Dutch primary care setting. The patient sample, consisting only of those who were interested in the topic of discontinuation, may have been biased. Only a small quantity of information was collected regarding patients’ psychiatric history (Table 1). With regard to the professional sample, one potential bias could be the intragroup variability, as GPs, psychiatrists, mental health nurses, and psychologists may have had differing experiences. Larger samples of professionals may shed some light on these different perspectives.
Another limitation is that the comparison of priority ratings between patients and professionals included a large number of variables, which may have led to an increased risk of type I errors. Therefore, the results may need to be replicated in a larger, more representative sample before recommendations can be made.
Comparison with existing literature
This study’s themes are in line with a recent systematic review and thematic synthesis describing barriers and facilitators to discontinue ADM from a patient perspective.29 This review yielded nine themes including patients’ psychological and physical capabilities, perception of ADM, fears, and support from doctors and significant others. Although the methodology of this review is different from the current study, there is an extensive overlap in the resulting themes. Notably, being given incongruent and insufficient information about discontinuation was mentioned as an impeding factor in the review. The authors concluded that barriers and facilitators to discontinuation are numerous and complex, and require detailed conversations between patients and GPs. The current study follows up on this recommendation by providing more specific items to discuss and enabling patients and their clinicians to better prepare the tapering process. This process should also encompass the different perspectives that they may have.
Examining the data on patients’ and professionals’ perspectives on the core themes revealed that patients rated ‘Professional guidance’ as more important to discuss than did professionals. More specifically, this effect was driven by a large difference in perception on the topic ‘Option of accompanying counselling sessions with, for example, a psychologist’. These findings seem to align with previous studies that have indicated that the level of professional guidance during tapering ADM varies widely. For example, Verbeek-Heida et al13 proposed that patients are in need of more guidance, and the current study indeed suggests that doctors and other mental healthcare providers could support their clients by playing a more active role in discontinuing ADM. This not only applies to the phase of actually tapering and stopping the medication, but also to initiating the process of stopping and making sound plans to do so. Indeed, the availability of supportive guidance seems to affect the motivation of patients to start the tapering process, that is, the absence of this kind of support has been found to be a barrier.15 Taken together, previous studies and results from the current study signal towards the notion that professionals are unlikely to initiate adjunctive support, despite their patients’ desire for such.
When looking at the single topics that were considered most important, patients particularly valued discussing an ‘Individual dose-reduction schedule’, ‘Relapse prevention’, and ‘Current quality of life and psychological functioning’. Professionals, on the other hand, considered ‘Withdrawal symptoms’, ‘Previous experiences with dose reduction’, and ‘Suicidality’ as most important to discuss. Previous studies describe that the way information is presented can have significant effects on decision making,30 and that professionals may be concerned that discussing possible negative effects will evoke a nocebo effect.31 Indeed, results of the current study indicate that clinicians are largely concerned with risk management. Obviously, reviewing and sharing scientific medical knowledge is an essential element of clinical decision making that should not be disregarded. However, it may not be the entire story. Considering the patient perspective, there seems to be a need for shifting towards a patient-centred approach. For example, rather than fully explaining the entire list of withdrawal symptoms that could occur during discontinuation, as described in the literature, clinicians may want to ask their patient what type(s) of withdrawal symptoms they expect or worry about. A balanced approach could consist of providing clear and concise information about possible withdrawal symptoms and relapse risk, while at the same time communicating and asking about possible feelings of uncertainty and fear with regard to the tapering of support. This information may serve as a starting point for additional psychological support. In addition, a personalised dose-reduction schedule that takes into account an individual’s personal schedule, external factors (for example, work–life events), and psychological functioning (for example, anxiety) may work better than a standardised schedule.
Implications for research and practice
In conclusion, given the large variation in policies of GPs around long-term use and discontinuation of ADM,15 more concrete tools are needed to move towards optimal care. The clusters and topics that were found in the current study could be used in combination with ongoing scientific knowledge to construct a comprehensive DA for the decision to taper ADM or other types of psychopharmacological medication. Such a DA should not only include the best available knowledge but also address the possible doubts and fears that patients may have. Moreover, many topics were related to ‘Process of discontinuation’; apparently this is a notable orientation towards the practicalities of discontinuation that require attention.
Using a DA during a conversation between patient and professional may support a balanced perspective, lead to a more confident decision regarding discontinuation, and to a more tailored type of guidance. From a more fundamental point of view, one of the recommendations for future research could be to disentangle the direct (more physiological) from the indirect (more psychological) effects of tapering medication using a placebo-controlled study design. The results of such a study could, in turn, yield useful information to include in a DA. From a clinical point of view, one of the first steps is to study the effectiveness of using a DA to enhance tapering support in primary healthcare. In addition, it seems worthwhile to study the effectiveness of additional forms of psychological support, such as cognitive behavioural therapy, mindfulness-based cognitive therapy, interpersonal therapy, or other approaches.
Acknowledgments
The authors would like to thank all patients and professionals for their time and willingness to participate in this study.
Funding
Funding for this study was provided by a grant from the Dutch Health Care Insurers Innovation Foundation (reference number: 3.048).
Ethical approval
This study is part of a project on discontinuation of antidepressant medication that was approved by the Medical Ethics Committee Arnhem-Nijmegen (reference number: 2016-2527).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.NHS Digital Prescriptions dispensed in the community England 2006 to 2016. 2017. https://files.digital.nhs.uk/publication/s/o/pres-disp-com-eng-2006-16-rep.pdf (accessed 16 Sep 2019)
- 2.Noordam R, Aarts N, Verhamme KM, et al. Prescription and indication trends of antidepressant drugs in the Netherlands between 1996 and 2012: a dynamic population-based study. Eur J Clin Pharmacol. 2015;71(3):369–375. doi: 10.1007/s00228-014-1803-x. [DOI] [PubMed] [Google Scholar]
- 3.Mojtabai R, Olfson M. National trends in long-term use of antidepressant medications: results from the U.S. National Health and Nutrition Examination Survey. J Clin Psychiatry. 2014;75(2):169–177. doi: 10.4088/JCP.13m08443. [DOI] [PubMed] [Google Scholar]
- 4.McCarthy M. Antidepressant use has doubled in rich nations in past 10 years. BMJ. 2013;347:f7261. doi: 10.1136/bmj.f7261. [DOI] [PubMed] [Google Scholar]
- 5.Moore M, Yuen HM, Dunn N, et al. Explaining the rise in antidepressant prescribing: a descriptive study using the general practice research database. BMJ. 2009;339:b3999. doi: 10.1136/bmj.b3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huijbregts KM, Hoogendoorn A, Slottje P, et al. Long-term and short-term antidepressant use in general practice: data from a large cohort in the Netherlands. Psychother Psychosom. 2017;86(6):362–369. doi: 10.1159/000480456. [DOI] [PubMed] [Google Scholar]
- 7.Borges S, Chen YF, Laughren TP, et al. Review of maintenance trials for major depressive disorder: a 25-year perspective from the US Food and Drug Administration. J Clin Psychiatry. 2014;75(3):205–214. doi: 10.4088/JCP.13r08722. [DOI] [PubMed] [Google Scholar]
- 8.Bet PM, Hugtenburg JG, Penninx BW, Hoogendijk WJ. Side effects of antidepressants during long-term use in a naturalistic setting. Eur Neuropsychopharmacol. 2013;23(11):1443–1451. doi: 10.1016/j.euroneuro.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Ferguson JM. SSRI antidepressant medications: adverse effects and tolerability. Prim Care Companion J Clin Psychiatry. 2001;3(1):22–27. doi: 10.4088/pcc.v03n0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coupland C, Dhiman P, Morriss R, et al. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ. 2011;343:d4551. doi: 10.1136/bmj.d4551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence . Depression in adults: recognition and management CG90. London: NICE; 2009. https://www.nice.org.uk/guidance/cg90 (accessed 13 Sep 2019) [PubMed] [Google Scholar]
- 12.Fava GA, Gatti A, Belaise C, et al. Withdrawal symptoms after selective serotonin reuptake inhibitor discontinuation: a systematic review. Psychother Psychosom. 2015;84(2):72–81. doi: 10.1159/000370338. [DOI] [PubMed] [Google Scholar]
- 13.Verbeek-Heida PM, Mathot EF. Better safe than sorry — why patients prefer to stop using selective serotonin reuptake inhibitor (SSRI) antidepressants but are afraid to do so: results of a qualitative study. Chronic Illn. 2006;2(2):133–142. doi: 10.1177/17423953060020020801. [DOI] [PubMed] [Google Scholar]
- 14.Leydon GM, Rodgers L, Kendrick T. A qualitative study of patient views on discontinuing long-term selective serotonin reuptake inhibitors. Fam Pract. 2007;24(6):570–575. doi: 10.1093/fampra/cmm069. [DOI] [PubMed] [Google Scholar]
- 15.Bosman RC, Huijbregts KM, Verhaak PF, et al. Long-term antidepressant use: a qualitative study on perspectives of patients and GPs in primary care. Br J Gen Pract. 2016. [DOI] [PMC free article] [PubMed]
- 16.Hoven-Eveleigh R. Inappropriate long-term antidepressant use in primary care: a challenge to change. Nijmegen: Radboud University; 2015. [Google Scholar]
- 17.Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood) 2013;32(2):207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- 18.Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision-making and interpersonal behavior: evidence, models and interventions. Patient Educ Couns. 2006;61(3):319–341. doi: 10.1016/j.pec.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Stacey D, Legare F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kane M, Trochim WM. Concept mapping for planning and evaluation. Thousand Oaks, CA: Sage Publications; 2007. [Google Scholar]
- 21.Trochim WMK. An introduction to concept mapping for planning and evaluation. Eval Program Plann. 1989;12(1):1–16. [Google Scholar]
- 22.Rosas SR, Kane M. Quality and rigor of the concept mapping methodology: a pooled study analysis. Eval Program Plann. 2012;35(2):236–245. doi: 10.1016/j.evalprogplan.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 23.Trimbos Instituut. Handboek concept mapping met Ariadne, beslissingsondersteuning voor groepen [Handbook concept mapping using Ariadne, decision support for groups]. Utrecht: Nederlands Centrum Geestelijke Volksgezondheid, Talcott; 1995. [Google Scholar]
- 24.Nabitz U, van Randeraad-van der Zee C, Kok I, et al. An overview of concept mapping in Dutch mental health care. Eval Program Plann. 2017;60:202–212. doi: 10.1016/j.evalprogplan.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 25.Hair JF, Black WC, Babin BJ, et al. Multivariate data analysis. 5th edn. Upper Saddle River, NJ: Prentice Hall; 1998. [Google Scholar]
- 26.Clatworthy J, Buick D, Hankins M, et al. The use and reporting of cluster analysis in health psychology: a review. Br J Health Psychol. 2005;10(Pt 3):329–358. doi: 10.1348/135910705X25697. [DOI] [PubMed] [Google Scholar]
- 27.Elwyn G, O’Connor A, Stacey D, et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333(7565):417. doi: 10.1136/bmj.38926.629329.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joseph-Williams N, Newcombe R, Politi M, et al. Toward minimum standards for certifying patient decision aids: a modified Delphi consensus process. Med Decis Making. 2014;34(6):699–710. doi: 10.1177/0272989X13501721. [DOI] [PubMed] [Google Scholar]
- 29.Maund E, Dewar-Haggart R, Williams S, et al. Barriers and facilitators to discontinuing antidepressant use: a systematic review and thematic synthesis. J Affect Disord. 2019;245:38–62. doi: 10.1016/j.jad.2018.10.107. [DOI] [PubMed] [Google Scholar]
- 30.Edwards A, Elwyn G, Covey J, et al. Presenting risk information — a review of the effects of ‘framing’ and other manipulations on patient outcomes. J Health Commun. 2001;6(1):61–82. doi: 10.1080/10810730150501413. [DOI] [PubMed] [Google Scholar]
- 31.Colloca L, Miller FG. The nocebo effect and its relevance for clinical practice. Psychosom Med. 2011;73(7):598–603. doi: 10.1097/PSY.0b013e3182294a50. [DOI] [PMC free article] [PubMed] [Google Scholar]