Abstract
Supplemental Digital Content is available in the text
To the Editor: An extremely heterogeneous group of tumors that arises from the cerebellopontine angle (CPA) account for approximately only 5% of all intra-cranial neoplasms. Thus, here we report a series of four relatively rare CPA cases to provide additional insights into the pre-operative differentiation of this area.
Case 1: Hemangioblastoma. A 51-year-old woman was admitted to our hospital with a 6-month history of headache and vision impairment. Magnetic resonance imaging (MRI) revealed a lobulated and heterogeneous intense right CPA mass [Figure 1], and the neuroradiology reading indicated a meningioma. The pathological diagnosis showed hemangioblastoma which is World Health Organization (WHO) grade I.
Figure 1.
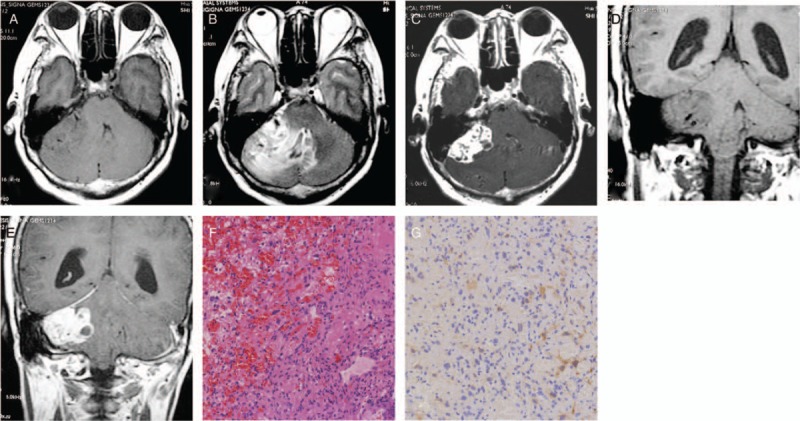
Hemangioblastoma in the right CPA in a 51-year-old woman. An axial (A) and a coronary T1-weighted (D) image demonstrating an iso-intense to hypo-intense tumor at the right CPA. (B): An axial T2-weighted image showing intra-tumoral hyper-intensity and highlighting the cerebellar brain parenchymal edema and compression of the brain stem and fourth ventricle. An axial (C) and a coronary T1-weighted (E) gadolinium-enhanced scan showing significant and heterogeneous enhancement of the right CPA tumor. (F): Hematoxylin-eosin staining (original magnification ×200) showing tumors composed of vacuolar stromal cells and abundant capillary network. (G): Positive staining of inhibin-α in tumor tissue stromal cell cytoplasm confirmed that the tumor was hemangioblastoma (immunohistochemistry staining, original magnification ×200). CPA: Cerebellopontine angle.
Case 2: Chondrosarcoma. A 35-year-old man with a 6-month history of intermittent headaches developed gait disorder and dysphagia 2 months previously. Cranial computed tomography (CT) and MRI were performed and revealed a large irregular mass in the right CPA region [Supplementary Figure 1]. Total surgical resection was performed, and the pathology results confirmed a CPA myxoid chondrosarcoma (WHO grade III).
Case 3: Anaplastic ependymoma. A 42-year-old woman had headaches associated with hearing loss in the left ear for 20 years. She was admitted to our hospital because of increased severity of hearing loss and abnormal gait 6 months previously. MRI scans revealed a large tumor in the left CPA space [Supplementary Figure 2]. Histopathology results showed that the tumor was typical of an anaplastic ependymoma (WHO grade III).
Case 4: Choroidal plexus papilloma. A 37-year-old woman presented at our hospital with a 6-month history of headache. CT and MRI revealed a lobulated mass in the right CPA [Supplementary Figure 3]. MRI indicated CPA meningioma or neurogenic tumor. The pathological diagnosis was choroid plexus papillomas (CPPs) (WHO grade I).
Although all four of these CPA neoplasms are rare, they can be detected in the differential diagnosis of the CPA region. Hemangioblastomas are classified as WHO grade I. Radiologically, our case presented typical features of solid hemangioblastoma. It is noteworthy that the tumor is associated with meninges. Although the lesion was located in the cerebellum without adhering to the petrous bone, it strongly involved meninges at the time of the surgery.
Intra-cranial chondrosarcomas are believed to occur preferentially in the skull base. Punctate and arc linear calcium, was commonly observed in well-differentiated lesions. In addition, focal bone destruction is another radiological feature. MRI images revealed hyper-intense signal on T2-weighted images that may be attributable to the cartilage matrix that consisted abundant water and mucus. In general, the tumors were hyper-vascular with intense enhancement. The potential radiological signs including heterogeneous intensity signals with poorly demarcated and irregular appearance, the presence of bone destruction and decrease or disappearance of calcium in the lesion may indicate a malignant transformation.
Ependymal tumors and CPPs are more commonly infratentorial, and particularly occur in the fourth ventricle.
Anaplastic ependymomas are classified as WHO Grade III neoplasms and are considered clinically more aggressive with a higher risk of recurrence and drop metastasis.[1] Clinically, the present case was different from that reported by Reni et al[2] where more rapid signs and symptoms were found owing to the relatively aggressive nature of the tumor. In terms of the radiological findings, owing to the relatively progressive characteristics, these tumors may show predilection for parenchymal involvement as well as focal dural thickness with enhancement (“dural tail” sign). There was calcification, necrosis, hemorrhage, or cystic components within the mass; therefore, they showed mixed-intensity on both T1- (hypo-intense to iso-intense) and T2- (iso-intense to hyper-intense) weighted images. Most lesions showed heterogeneous enhancement. These lesions account for 8% to 33%[1] of all lesions and are particularly detected in infratentorial lesions. Therefore, imaging protocols, including intra-cranial and spinal MRI examinations, are essential pre-operatively.
CPPs are relatively rare, historically benign (WHO grade I) intra-cranial neoplasms that arise from the choroid plexus epithelial cells and occur more frequently in children. Similarly, the CPPs are typically confined to the ventricular system and are rarely located in the CPA; they represent about 9% of all CPPs and are mostly seen in adults.[3] Local invasion and dissemination through CSF were not noted in our case; however, this should be considered despite the benign histological features. Petrous bone and mastoid or cavernous sinus erosion are extremely rare in CPA-CPPs. The lateral foramen of the fourth ventricle is frequently pressed or disappears.
In summary, although these four kinds of tumors arise from the CPA region with typical imaging characteristics of this site (meninges involvement and absence of edema), they had their own intra-axial characteristics. Chondrosarcomas and anaplastic ependymomas showed progressive features (with parenchymal and bone involvement).
Funding
This study was supported by grants from the Natural Science Foundation of China (No. 81871423), Shanghai Municipal Commission of Health and Family Planning (No. 20160064), and Jing’an District Scientific Committee and Health and Family Planning Commission (No. 2016MS03).
Conflicts of interest
None.
Supplementary Material
Footnotes
How to cite this article: Dou YF, Liang ZH. Cerebellopontine angle neoplasms in four cases: intra-axial or extra-axial? Chin Med J 2019;132:1870–1871. doi: 10.1097/CM9.0000000000000338
References
- 1.Marsecano C, Bruno F, Michelini G, Perri M, Calvisi G, Di Cesare E, et al. Systemic metastases from central nervous system ependymoma: case report and review of the literature. Neuroradiol J 2017; 30:274–280. doi: 10.1177/1971400916689371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reni M, Gatta G, Mazza E, Vecht C. Ependymoma. Crit Rev Oncol Hematol 2007; 63:81–89. doi: 10.1016/j.critrevonc.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Qi Q, Ni S, Zhou X, Huang B, Li X. Extraventricular intraparenchymal choroid plexus tumors in cerebral hemisphere: a series of 6 cases. World Neurosurg 2015; 84:1660–1667. doi: 10.1016/j.wneu.2015.07.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


