Abstract
Background: Dumping syndrome is a common complication of surgical treatment of gastric cancer, but conventional therapy has limitations related to symptom care due to its structural cause and the decreased quality of life. Objectives: The objective of this review was to assess the clinical evidence for the effectiveness of herbal medicine as a treatment for dumping syndrome. Methods: A literature review was conducted using 16 databases from their inceptions to March 2018. All randomized controlled trials (RCTs) of herbal medicine used to treat dumping syndrome patients were included and meta-analyzed. Methodological quality was assessed using the Cochrane Handbook for Systematic Reviews of Interventions. Results: A total of 174 dumping syndrome patients of 3 trials met all inclusion criteria. Two trials assessed the effectiveness of herbal medicine on the symptom response rate compared with conventional pharmacotherapy. Their results suggested significant effects in favor of herbal medicine (risk ratio [RR] = 1.37, 95% confidence interval [CI] = 1.16-1.63, P = .0003, heterogeneity τ2 = 0, χ2 = 0.02, P = .88, I2 = 0%). One trial assessed its effectiveness on the improvement rate of overall symptoms compared with conventional conservative complex therapy, such as postural management, diet regulation, and counseling (RR = 1.23, 95% CI = 0.96-1.58). Conclusions: Due to the small sample size, scarcity of reported articles, and lack of quality of the current RCTs, it was concluded that the effectiveness of herbal medicine in treating dumping syndrome is unclear.
Keywords: dumping syndrome, herbal medicine, decoction, systematic review
Introduction
Dumping syndrome, also referred to as rapid gastric emptying syndrome, is a gastrointestinal disease usually caused by gastric surgery. Hertz1 first described the postprandial symptoms associated with rapid gastric emptying after gastroenterostomy. Wyllys et al2 introduced the term “dumping” for this syndrome.
Gastric cancer is commonly diagnosed in locally advanced or metastatic stage because of its late-developed physical signs. Therefore, surgical therapy, suggested by its prognosis, is considered as the only curative option despite advances of perioperative chemotherapy and radiological therapy. Massive resection like total gastrectomy or Roux-en-Y reconstruction is recommended for diffuse type or depending on tumor location, and limited resection such as subtotal gastrectomy is considered for palliation or in very elderly patients.3 As a result of surgery, dumping syndrome is one of the major complications that is to be managed for postoperative care of gastric cancer patients.
Dumping syndrome is classified into 2 types based on characteristics of the symptoms. Early dumping syndrome is associated with gastrointestinal responses due to rapid gastric emptying, occurs within 10 to 30 minutes after meals, and results in symptoms such as nausea, vomiting, epigastric pain, bloating, and diarrhea. Late dumping syndrome is associated with neurohormonal responses, occurs 1 to 3 hours after meals, and results in vasomotor symptoms such as flushing, dizziness, palpitation, desire to lie down, and postprandial hypoglycemia with hyperinsulinemia. Consequently, dumping syndrome causes patients to develop a fear of eating, which results in malnutrition and weight loss and decreases quality of life. Konishi et al4 and Nguyen et al5 reported that rapid gastric and intestinal transit is a major pathology of dumping syndrome. The pancreatic β-cell causes dumping syndrome patients to suffer from hypoglycemia due to hyperinsulinemia.6,7 Intestinal hormones, such as GLP-1, which increases after meals, are also suggested to be involved in dumping syndrome.7,8 Dumping syndrome is primarily caused by gastric surgery but also by congenital microgastria9 or a dislocated feeding tube.10
The incidence of dumping syndrome is reported in 24.18% of patients who undergo a Roux-en-Y gastric bypass (RYGB),11-13 approximately 20% of patients who undergo a vagotomy with pyloroplasty, and up to 50% of patients who undergo an esophagectomy.14-18 Another study reported that 20.5% of patients who had other types of procedures, such as a sleeve gastrectomy and a vagotomy, also had an incidence of dumping syndrome.11-13
Dumping syndrome is diagnosed based on symptoms that become aggravated after meals, provocation tests, laboratory tests, gastric surgical history, or basal circumstances of rapid gastric emptying. Scale and scoring systems for dumping syndrome have been introduced, such as Sigstad’s score,19 Postgastrectomy Syndrome Assessment Scale (PGSAS)-45,20-22 and Dumping Symptom Rating Scale (DSRS).23 Provocation tests are also used, which include the oral glucose tolerance test and the hydrogen breath test. Laboratory and radiologic tests are helpful in making a diagnosis for late dumping syndrome patients, which include plasma glucose, insulin, GLP-1 after meals, and gastric emptying scintigraphy tests.24
Current treatment for dumping syndrome includes pharmacological and surgical interventions. Dietary supplements (pectin, guar gum, acarbose25-30), somatostatin analogs (pasireotide,5,31-33 octreotide31), miglitol,34-36 iraglutide,37 exendin-(9-39),38 and diazoxide39 are prescribed for postprandial hypoglycemia or hyperglycemia caused by dumping syndrome. The GLP-1 receptor blocker can improve hypoglycemia caused by dumping syndrome.40 RYGB reversal41,42 is an option to eliminate cause of dumping syndrome. Endoluminal revision43 is also considered for complications of RYGB. A loop duodenojejunal bypass44 is performed for dumping syndrome caused by RYGB or esophageal replacement.45 Dietary management46 is recommended to be combined with other interventions. Patients should consume a reduced amount of food at each meal and should delay fluid intake until at least 30 minutes after meals.46 High-fiber and protein-rich foods, fruits, and vegetables are also recommended.47 Limiting glucose48 can reduce symptoms.
Previous systematic reviews have been conducted to evaluate the symptoms based on the type of surgery, but no review on the effect and efficacy of herbal medicine has been conducted. Studies on herbal medicine treatment for dumping syndrome are limited in case reports, case series, and controlled trials.
The aims of this review were to gather information on current research and to evaluate the effectiveness and the safety of herbal medicine in the treatment of dumping syndrome.
Methods
Criteria for Considering Studies for This Review
The protocol for this review was registered at PROSPERO ID CRD42018090538 on March 19, 2018 (archived at http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018090538).
Search Methods for the Identification of Studies
The following databases were searched: PubMed, EMBASE, the Cochrane Central Register of Controlled Trials (CENTRAL), AMED, CINAHL, CNKI, Wanfang, VIP, CiNii, and 7 Korean medical databases (Koreantk, Oasis, RISS, DBPOA, KISS, KISTI, and NDSL). All searches ended in March 2018. The search terms included “Dumping syndrome,” “Postprandial syndrome,” and so on (see Appendixes A and B). Search strategies were used to find related studies, and a modified search formula for characteristics of each database was applied.
Study Selection
Two authors (BP and SH) selected studies for eligibility and checked them against the inclusion criteria independently. All randomized controlled trials (RCTs) were included in this review without restrictions on time or language.
Inclusion Criteria
Only RCTs of herbal medicine treatment for dumping syndrome patients were included. The patients were diagnosed with dumping syndrome based on their symptoms followed by any type of gastrointestinal surgery, and they were included without any restriction of sex, age, race, country, and onset. All treatments using herbal medicines were included without any limitations on number, administration methods, dosages, and durations of treatment. It was determined that the control treatments would include any type of conventional therapy, placebo medication, and no treatment. Primary outcomes included improvement in symptoms assessed by validated tools, such as Sigstad’s scoring system, Art’s questionnaire, the DSRS, overall symptoms improvement, and so on. Secondary outcomes included adverse events and quality of life. Trials that were case reports, cross-over designed, nonrandomized, and noncontrolled, and those that included nonherbal therapy, such as acupuncture or moxibustion, were excluded.
Data Extraction and Management
Two authors (BP and SH) extracted the data from the included studies independently. The data were extracted using a standard data extraction approach that included methodology, participants, intervention, duration of treatment, outcomes, and conclusions.
Assessment of Risk of Bias in Included Studies
Two authors (BP and SH) independently assessed the risk of bias, which is described in the Cochrane Handbook for Systematic Reviews of Interventions. The quality of studies was categorized into low, unclear, or high risk of bias according to the risk for each important outcome within the included studies, including adequacy of the generation of the allocation sequence, allocation concealment, and blinding and whether there were incomplete outcome data or a selective reporting of the results. Studies that met all criteria were categorized as a low risk of bias, studies that met none of the criteria were categorized as a high risk of bias, and those with insufficient information to draw a conclusion were categorized as an unclear risk of bias.
Data Analysis
Data analysis was performed using RevMan 5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark; The Cochrane Collaboration, 2016) software. Binary outcomes were summarized using a risk ratio (RR) with a 95% confidence interval (CI) for relative effect and a risk difference with 95% CI for absolute effect. The continuous outcomes were summarized using mean difference with a 95% CI. If there were sufficient data (similar clinical characteristics, such as study design, participants, interventions, control, and outcome measures) and an acceptable statistical heterogeneity, the data were pooled, and a meta-analysis was performed using the random effect model. Statistical heterogeneity was detected by the I2 test, and an I2 > 50% indicated the possibility of statistical heterogeneity among the studies. If the I2 was larger than 75%, which means there was a clear statistical heterogeneity among studies, the results from each study were evaluated independently rather than pooling the data for analysis. A funnel plot analysis was considered to detect publication bias.
Results
Results of the Search
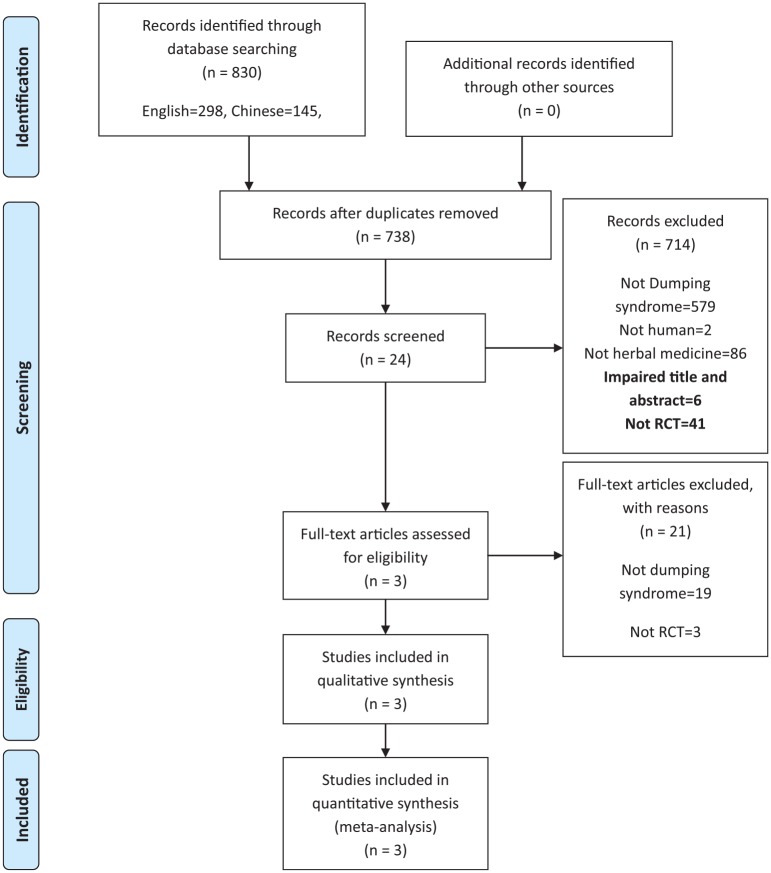
From the 16 electronic databases, 830 articles were identified (Figure 1). After excluding duplicate studies and articles that did not meet the inclusion criteria on the basis of reading the title and abstract, the full texts of 24 articles were retrieved and evaluated. After browsing full-text articles, 21 articles were excluded; 3 were not RCT, and 19 did not discuss dumping syndrome49-69 (Table 2). Consequently, 3 trials were included for the review process and data analysis70-72 (Table 1).
Figure 1.
Flow chart.
Table 2.
Excluded Studies by Full-Text Screening.
| No. | Author (Year) of Article | Reason of Exclusion |
|---|---|---|
| 1 | Nagasaka et al (2006)49 | 3 cases—case report |
| 2 | Nishi et al (2012)50 | Postoperative ileus after hepatectomy, RCT |
| 3 | Katsuno et al (2015)51 | Postoperative ileus after colon cancer resection, RCT |
| 4 | Qi et al (2007)52 | Postoperative ileus and gastroparesis after cholecystectomy, RCT |
| 5 | Koeda et al (2014)53 | Postoperative ileus after total gastrectomy on gastric cancer, RCT |
| 6 | Hatano et al (2012)54 | Postoperative ileus after hepatectomy, RCT |
| 7 | Endo et al (2006)55 | QOL of total gastrectomy and jejunal pouch reconstruction on gastric carcinoma, cross-over study |
| 8 | Yoshikawa et al (2015)56 | Postoperative ileus after total gastrectomy on gastric cancer, RCT |
| 9 | Takahashi et al (2009)57 | QOL and gastroparesis of pylorus preserving gastrectomy, cross-over study |
| 10 | Suehiro et al (2005)58 | Postoperative ileus after rectal resection, controlled study |
| 11 | Ge et al (2008)59 | Postoperative nausea and vomiting after renal transplantation, RCT |
| 12 | Nakamura et al (2016)60 | QOL of esophagectomy of esophageal cancer, controlled study |
| 13 | Xue et al (2007)61 | Postoperative gastroparesis after esophageal carcinoma, cardiac carcinoma resection, trial |
| 14 | Sunagawa and Oshiro (2011)62 | Portal blood flow after pancreas and duodenal resection, RCT |
| 15 | Xu et al (2015)63 | Postoperative ileus and gastroparesis after esophageal cancer resection, RCT |
| 16 | Dang (1987)64 | Postoperative care after gastric greater curvature resection, controlled study |
| 17 | Yu et al (1999)65 | Digestive function after gastric cancer resection, controlled study |
| 18 | Takiguchi (2012)66 | No available text/not RCT |
| 19 | Fu (2015)67 | Prevention of complication after laparoscopic gastric cancer resection, controlled study |
| 20 | Nishida (2009)68 | No available text/not dumping syndrome |
| 21 | Zhang and Mao (1983)69 | No available text/not RCT |
Abbreviations: RCT, randomized controlled trial; QOL, quality of life.
Table 1.
Included Studies.
| First Author (Year) Country | Sample Size/Age (Years) | Diagnoses | Intervention (Regimen); Control (Regimen) | Outcomes | Summary of Results | Adverse Events |
|---|---|---|---|---|---|---|
| Peng (2015),70 China | N = 102/54.6 (T), 53.7 (C) | Gastric cancer = 102 | T: Modified Houpu Shengjiang Ban Xia Gan Cao Ren Shen decoction (厚朴生薑半夏甘草人蔘湯加減), regimen was not mentioned C: Domperidone 10 mg tid |
Symptom response rate Symptom score (total 24) Overall symptom improvement rate |
Symptom response ratea: 94.23% (T)/68.00% (C) Overall symptom improvement ratea: 90.38% (T)/66.00% (C) |
Not mentioned |
| Quan (2004),71 China | N = 30/52 ± 11.06474 (T), 57 ± 8.17546 (C) | Gastric cancer = 30 | T: Pingyun Tiao Wei decoction (平運調胃湯) 100cc bid C: Atropin 0.3 mg bid |
Symptom response rate Symptom score (total 24) |
Symptom response rate: 100.00% (T)/73.33% (C) | Not mentioned |
| Zhou (2014),72 China | N = 42/51.1 ± 2.3 (T), 50.4 ± 3.1 (C) | Gastric cancer = 11 Gastroduodenal ulcer = 9 (T) Gastric cancer = 12 Gastroduodenal ulcer = 10 (C) |
T: Modified Bozhongyiqi decoction (補中益氣湯加減) or modified Xiangshaliujunzi decoction (香砂六君子湯加減) or modified Shengjiangxiexin decoction (生薑瀉心湯加減) twice a day, the rest of the regimen was not mentioned + Control group Tx C: regulation of posture, diet, electrolyte, medication, counseling, ATx |
Symptom response rate | Symptom response rate: 95.00% (T)/77.27% (C) | Not mentioned |
Abbreviations: T, treatment group; C, control group; tid, thrice a day; bid, twice a day.
Effectiveness (%) = [complete recovery + remarkably effective + effective]/n × 100%.
Characteristics of the Included Studies
A total of 174 dumping syndrome patients were included, and there was no report of dropouts. All 3 trials included dumping syndrome patients without a classification of surgery or disease cause or a classification of early/late dumping syndrome. One trial71 did not report patients’ characteristics, such as age or sex. The mean sample size was 58 patients, but no trial reported the calculation sequence of the sample size. The duration of treatment ranged from 10 to 35 days.
All 3 trials used different herbal decoctions via oral administration. Two trials70,71 used 1 decoction during the trial, but 1 trial72 used 3 modified decoctions according to individual symptom patterns based on oriental medicine diagnoses.
For the control group treatment, 2 trials used conventional pharmacotherapy. One70 used domperidone, and the other71 used atropine; however, another one72 used a complex therapy for the control group, which included postural and diet regulation, counseling, and acupuncture.
Outcome Assessment
All the included studies used the symptom response rate, which was designed to evaluate subjective symptoms of dumping syndrome and is similar to the Likert-type scale. This scale lists gastrointestinal symptoms, such as epigastric discomfort, belching, loss of appetite, general weakness, abdominal distension, loose stool, hyperperistaltic sound, and postprandial somnolence. Two trials70,72 used the overall symptoms improvement rate, which is scored based on the improvement of symptoms after treatment as complete recovery, remarkably effective, effective, or not effective.
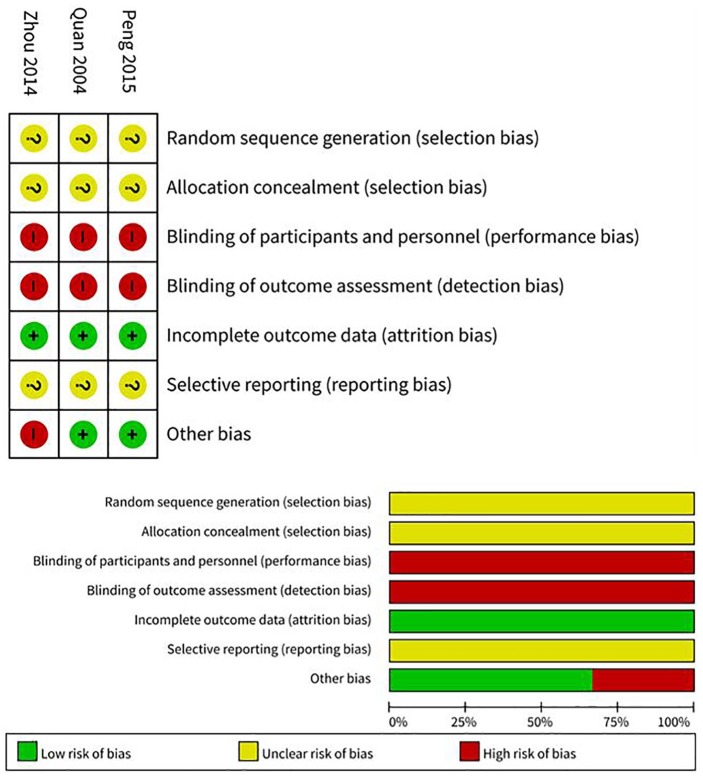
Risk of Bias of Included Studies
According to the predefined methodological quality criteria, all 3 trials were evaluated by 2 authors (BP, SH). All 3 trials mentioned the randomization, but no trials reported the generation of sequence, blinding, or dropout. All studies appeared to have a high risk of bias in the blinding of both patients and operators. Because none of the trials was found to have preregistered protocols in the electronic databases, “selective reporting” was basically assessed as an “unclear risk of bias” by checking the methods and results sections from each trial (Figure 2).
Figure 2.
Risk of bias of included studies.
Therapeutic Effects of Interventions: Herbal Medicine Versus Conventional Medicine
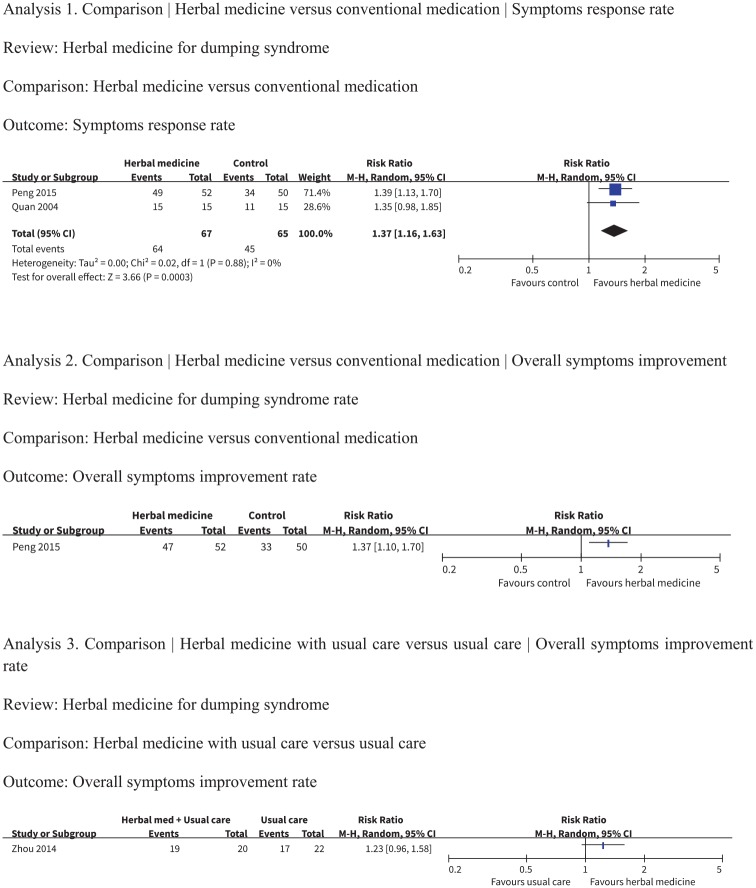
As pharmacotherapy and other types of diet and lifestyle supportive management are conventional therapies for dumping syndrome, all 3 trials were only analyzed for the therapeutic or adjunctive effects of herbal medicine against conventional therapies (Figure 3).
Figure 3.
Forest plot of included studies.
Two trials70,71 investigated herbal medicine compared with conventional medication for dumping syndrome. These studies reported results using the symptom response rate, but different herbal decoctions were used. One trial70 reported that 14 days of modified Houpu Shengjiang Ban Xia Gan Cao Ren Shen decoction administration (RR = 1.35, 95% CI = 0.98-1.85) led to a better improvement compared with the domperidone group but did not identify a significant difference between groups. The other trial71 reported that 10 days of Pingyun Tiao Wei decoction administration (RR = 1.39, 95% CI = 1.13-1.70) was found to have a significant effect on improving the symptom response rate score when compared with the atropine group. The meta-analysis showed significant effects of herbal decoction compared with conventional medication (n = 132, RR = 1.37, 95% CI = 1.16-1.63, P = .0003, I2 = 0%).
One trial70 also reported results using the overall symptoms improvement rate. Fourteen days of modified Houpu Shengjiang Ban Xia Gan Cao Ren Shen decoction administration (RR = 1.37, 95% CI = 1.10-1.70) was found to have a significant effect on improving the symptom response rate score when compared with the domperidone group.
One trial72 investigated adjunctive herbal medicine compared with the group provided with conventional care for dumping syndrome. Using the overall symptoms improvement rate, the author reported that 21 to 35 days of herbal decoctions (RR = 1.23, 95% CI = 0.96-1.58) treatment, which included modified Buzhongyiqi decoction, modified Xiangshaliujunzi decoction, or modified Shengjiangxiexin decoction, with conventional care relieved patients’ symptoms, but there was no significant effect on improving the symptom response rate score when compared with the conventional treatment group.
Adverse Events
None of the studies mentioned adverse events following herbal medicine treatment.
Discussion
According to the 3 trials that reported the results of 174 dumping syndrome patients who were administered herbal medicines for their symptoms, which were measured by the symptom response rate and the overall symptoms improvement rate, the modified Houpu Shengjiang Ban Xia Gan Cao Ren Shen decoction was shown to significantly improve the score compared with conventional medicine; however, for the Pingyun Tiao Wei decoction, modified Buzhongyiqi decoction, modified Xiangshaliujunzi decoction, and modified Shengjiangxiexin decoction, significant improvement was difficult to determine.
Electronic databases that were likely to contain most trials that investigated herbal medicine were searched; however, only 24 studies were identified after screening, and 21 studies did not match the review’s objectives. Therefore, a small number of trials for dumping syndrome patients who were treated with herbal medicine met the inclusion criteria. This suggests that further research is needed to evaluate the effectiveness of herbal medicine in treating dumping syndrome. Although there was a lack of quality related to study design, the trials indicated that using herbal medicine to treat dumping syndrome could be more beneficial than conventional therapy alone. Currently, only an unclear possibility of the effectiveness of herbal medicine in treating dumping syndrome is suggested, and thus RCTs with an improved design and performance are needed.
Although the databases were searched without limitations related to language and country, all included trials were published in China. This suggests that the conclusions of these trials could contain publication bias if there is a positive tendency of researchers and journals in China.
The trials evaluated the effectiveness of herbal medicine on symptom scores related to gastrointestinal symptoms. There are clear limitations to interpret the result, as included trials of this review evaluated categorical scores about improvement of symptoms. None of the included trials considered Sigstad’s score, PGSAS-45, DSRS, provocation tests that are already been established; laboratory tests for blood glucose or insulin; or radiological evidence of rapid gastric emptying. Although all trials showed a positive effect after treatment, information related to changes, such as blood glucose after meals, hyperinsulinemia, or quality of life, was not found. In addition, the scale used for the trials mostly referred to early dumping syndrome symptoms and did not specify whether the symptoms were related to early or late dumping syndrome. Thus, whether herbal medicine is effective for early or late dumping syndrome is unclear.
As the result shows, there were improvements in both herbal medicine group and conventional medication group. Although Quan’s71 result did not show significant benefit of herbal medicine as shown in Figure 3, Analysis 1, the meta-analysis that was performed in low heterogeneity showed favor to herbal medicine within level of significance. However, the change of overall symptom improvement rate was compared with different control managements in each of the studies as shown in Figure 3, Analyses 2 and 3; and therefore, it was not proper to synthesize and perform meta-analysis. Additionally, owing to lack of sufficient sample size (n = 132 in Figure 3, Analysis 1), these synthesized data were not fully considered to conclude a single firm opinion. If more samples are retained in further studies, it will give a better view of the effectiveness of herbal medication.
Various herbal formulas were used in each trial, respectively, but were composited with similar herbs that relieve gastrointestinal symptoms. Herbs such as Zingiberis Rhizoma Recens (生薑; ginger), Pinelliae Tuber (半夏), Magnoliae Cortex (厚朴), which are used by Peng70 and Zhou,72 and herbs like Coicis Semen (薏苡仁), Codonopsis Pilosulae Radix (黨蔘), which are used by Quan71 and Zhou,72 are to facilitate and improve digestive function. However, Zhou72 modified the herbal decoction depending on disease pattern diagnosis (辯證) of each patient. This results in a change of treatment group not only by the individual herbal action but also by systemic pattern of each patient. As an example, Zhou72 used 3 different decoctions, modified Buzhongyiqi decoction (補中益氣湯加減) for energy-depression of digestive system pattern (中氣下陷), modified Xiangshaliujunzi decoction (香砂六君子湯加減) for energy deficiency of digestive system pattern (脾胃虛弱), and modified Shengjiangxiexin decoction (生薑瀉心湯加減) for pathologic wet heat of digestive system pattern (濕熱中阻). Therefore, strict interpretation of the results would be needed, while the authors suggested the potential effectiveness of herbal medicine with current evidence. Pharmacologic mechanisms of these herbs are partially known. For example, Zingiberis Rhizoma Recens contains phytochemicals like gingerol, which affect the gastric mobility and secretion of gastric acid.73 Pinelliae Tuber is reported to have antiemetic effect via chemoreceptor trigger zone.74 Magnoliae Cortex contains magnolol, which is thought to be related with gastric histamine release, and antiemetic effect.75,76 Most herbs that were used in trials are related with digestive function; however, more research is needed to discuss the mechanism of herbal medicine because of various combination of herbal decoctions and also pattern diagnosis of each patient.
After treatment, the symptoms of all the patients who participated in all trials were reduced, but there was no follow-up observation after improvement. As dumping syndrome is a recurring syndrome based on diet and its gastric emptying mechanism, the symptoms should be observed during the posttreatment period. Whether the recurrence of symptoms could be prevented could not be determined due to a lack of information. In addition, the evaluation of adverse events was not mentioned. In future research studies, reporting adverse events must be considered to obtain high-quality evidence and to apply the findings to clinical practice.
There was no declaration of dropouts during the trials. None of the included studies mentioned clear randomization or blinding methods. Moreover, the concealment of allocation was not reported. Although these trials were RCTs, there is a high risk of bias related to overestimating the effect of herbal medicine due to a lack of reliability and inadequate randomization.
Conclusion
Herbal medicines may improve the gastrointestinal symptoms of dumping syndrome patients compared with conventional medicine; however, the included trials had limitations, such as a lack of information, a lack of quality, and a small sample size. Additional research studies that include adequate methodological procedures to prevent biases and a larger sample with results calculated by statistical methods are needed to clearly determine the effectiveness of herbal medicine in treating dumping syndrome.
Appendix A
EMBASE (via Ovid) Search Strategy
#1. exp dumping syndrome/
#2. (dumping syndrome$) or (postgastrectomy syndrome$) or complication$ or hypoglyc$ or diarrhea or dizziness or sweating or diaphoresis or syncope or perspiration or nausea or palpitation or tremor or confusion or tachycardia or hypotension).mp.
#3. (gastrectomyor gastroenterostomy or (gastric surgery) or (Roux-en-Y) or (gastric bypass) or (bariatric surgery) or antrectomy or pylorectomy or pyloroplasty or jejunostomy or (bowel resection) or vagotomyoresophagectomy).mp.
#4. #1 or (#2 and #3)
#5. exp Medicinal plant/
#6. exp Traditional medicine/
#7. ((traditional Korean medicine) or (traditional Chinese medicine) or (traditional oriental medicine) or (Kampo medicine) or (alternative medicine) or (complementary medicine) or herb$ or herbal$ or decoction$ or botanic$).mp.
#8. or/ #5 -#7
#9. exp Randomized Controlled Trial (topic)/
#10. exp controlled clinical trial (topic)/
#11. (randomized controlled trial$ or controlled clinical trial$ or randomized$ or randomly$ or placebo or clinical trial$ or controlled trial$).mp.
#12. or/ #9-#11
#13. #4 and #8 and #12
Appendix B
MEDLINE (via Ovid) Search Strategy
#1. exp dumping syndrome/
#2. (dumping syndrome$) or (postgastrectomy syndrome$) or complication$ or hypoglyc$ or diarrhea or dizziness or sweating or diaphoresis or syncope or perspiration or nausea or palpitation or tremor or confusion or tachycardia or hypotension).mp.
#3. (gastrectomy or gastroenterostomy or (gastric surgery) or (Roux-en-Y) or (gastric bypass) or (bariatric surgery) or antrectomy or pylorectomy or pyloroplasty or jejunostomy or (bowel resection) or vagotomyoresophagectomy).mp.
#4. #1 or (#2 and #3)
#5. exp Drugs, Chinese herbal/
#6. exp Herbal Medicine/
#7. exp Plants, Medicinal/
#8. exp Medicine, Chinese Traditional/
#9. (traditional Korean medicine) or (traditional Chinese medicine) or (traditional oriental medicine) or (Kampo medicine) or (alternative medicine) or (complementary medicine) or herb$ or herbal$ or decoction$ or botanic$).mp.
#10. or/ #5-#9
#11. exp Randomized Controlled Trials as Topic/
#12. exp controlled clinical trials as topic/
#13. (randomized controlled trial$ or controlled clinical trial$ or randomized$ or randomly$ or placebo or clinical trial$or controlled trial$).mp.
#14. or/#11-#13
#15. #4 and #10 and #14
Footnotes
Author Contributions: Conceptualization: Bongki Park
Data curation: Bongki Park, Seungcheol Hong
Formal analysis: Bongki Park, Seungcheol Hong
Investigation: Bongki Park, Seungcheol Hong
Methodology: Bongki Park
Project administration: Bongki Park, Dong-Jun Choi
Software: Seungcheol Hong, Hyeonseok Noh
Supervision: Bongki Park, Hyeonseok Noh, Dong-Jun Choi
Validation: Bongki Park, Seungcheol Hong, Dong-Jun Choi
Writing—original draft: Bongki Park, Seungcheol Hong
Writing—review and editing: Bongki Park, Hyeonseok Noh, Dong-Jun Choi
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Seungcheol Hong  https://orcid.org/0000-0002-5218-3959
https://orcid.org/0000-0002-5218-3959
References
- 1. Hertz AF., IV The cause and treatment of certain unfavorable after-effects of gastro-enterostomy. Ann Surg. 1913;58:466-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wyllys E, Andrews E, Mix CL. “Dumping stomach” and other results of gastrojejunostomy: operative cure by disconnecting old stoma. Surg Clin Chicago. 1920;4:879-892. [Google Scholar]
- 3. Weledji EP. The principles of the surgical management of gastric cancer. Int J Surg Oncol (N Y). 2017;2:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Konishi H, Nakada K, Kawamura M, et al. Impaired gastrointestinal function affects symptoms and alimentary status in patients after gastrectomy. World J Surg. 2016;40:2713-2718. [DOI] [PubMed] [Google Scholar]
- 5. Nguyen NQ, Debreceni TL, Bambrick JE, et al. Rapid gastric and intestinal transit is a major determinant of changes in blood glucose, intestinal hormones, glucose absorption and postprandial symptoms after gastric bypass. Obesity (Silver Spring). 2014;22:2003-2009. [DOI] [PubMed] [Google Scholar]
- 6. Vaurs C, Brun JF, Bérard E, du Rieu MC, Hanaire H, Ritz P. β-Cell pancreatic dysfunction plays a role in hyperglycemic peaks observed after gastric bypass surgery of obese patients. Surg Obes Relat Dis. 2016;12:795-802. [DOI] [PubMed] [Google Scholar]
- 7. Hamasaki H, Moriyama S, Yanai H. A possible difference in the mechanism for postprandial hypoglycemia associated with dumping syndrome between patients with and without type 2 diabetes. Obes Res Clin Pract. 2015;9:622-624. [DOI] [PubMed] [Google Scholar]
- 8. Akimov VP, Dvaladze LG, Shengelia TD, Veselov IE. A new view on pathogenesis of dumping-syndrome [in Russian]. Vestn Khir Im I Grek. 2008;167:22-25. [PubMed] [Google Scholar]
- 9. Filisetti C, Maestri L, Meroni M, Marinoni F, Riccipetitoni G. Severe dumping syndrome in a 6-year-old girl with congenital microgastria treated by Hunt-Lawrence pouch. Eur J Pediatr Surg Rep. 2017;5:e17-e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shimoda M, Saraya T, Ogawa Y, Tanaka Y. Dumping syndrome due to the misplacement of the gastrostomy feeding tube. Intern Med. 2015;54:2529. [DOI] [PubMed] [Google Scholar]
- 11. Ramadan M, Loureiro M, Laughlan K, et al. Risk of dumping syndrome after sleeve gastrectomy and Roux-en-Y gastric bypass: early results of a multicentre prospective study. Gastroenterol Res Pract. 2016;2016:2570237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Patton C, Okosieme OE, Evans LM. Dumping syndrome presenting three decades after vagotomy. N Z Med J. 2007;120:U2807. [PubMed] [Google Scholar]
- 13. Mine S, Sano T, Tsutsumi K, et al. Large-scale investigation into dumping syndrome after gastrectomy for gastric cancer. J Am Coll Surg. 2010;211:628-636. [DOI] [PubMed] [Google Scholar]
- 14. Vecht J, Masclee AA, Lamers CB. The dumping syndrome. Current insights into pathophysiology, diagnosis and treatment. Scand J Gastroenterol Suppl. 1997;223:21-27. [PubMed] [Google Scholar]
- 15. McLarty AJ, Deschamps C, Trastek VF, Allen MS, Pairolero PC, Harmsen WS. Esophageal resection for cancer of the esophagus: long-term function and quality of life. Ann Thorac Surg. 1997;63:1568-1572. [DOI] [PubMed] [Google Scholar]
- 16. Banerjee A, Ding Y, Mikami DJ, Needleman BJ. The role of dumping syndrome in weight loss after gastric bypass surgery. Surg Endosc. 2013;27:1573-1578. [DOI] [PubMed] [Google Scholar]
- 17. Tzovaras G, Papamargaritis D, Sioka E, et al. Symptoms suggestive of dumping syndrome after provocation in patients after laparoscopic sleeve gastrectomy. Obes Surg. 2012;22:23-28. [DOI] [PubMed] [Google Scholar]
- 18. Papamargaritis D, Koukoulis G, Sioka E, et al. Dumping symptoms and incidence of hypoglycaemia after provocation test at 6 and 12 months after laparoscopic sleeve gastrectomy. Obes Surg. 2012;22:1600-1606. [DOI] [PubMed] [Google Scholar]
- 19. Loss AB, de Souza AA, Pitombo CA, Milcent M, Madureira FA. Analysis of the dumping syndrome on morbid obese patients submitted to Roux en Y gastric bypass [in Portuguese]. Rev Col Bras Cir. 2009;36:413-419. [DOI] [PubMed] [Google Scholar]
- 20. Tanizawa Y, Tanabe K, Kawahira H, et al. ; Japan Postgastrectomy Syndrome Working Party. Specific features of dumping syndrome after various types of gastrectomy as assessed by a newly developed integrated questionnaire, the PGSAS-45. Dig Surg. 2016;33:94-103. [DOI] [PubMed] [Google Scholar]
- 21. Takiguchi N, Takahashi M, Ikeda M, et al. Long-term quality-of-life comparison of total gastrectomy and proximal gastrectomy by Postgastrectomy Syndrome Assessment Scale (PGSAS-45): a nationwide multi-institutional study. Gastric Cancer. 2015;18:407-416. [DOI] [PubMed] [Google Scholar]
- 22. Nakada K, Ikeda M, Takahashi M, et al. Characteristics and clinical relevance of postgastrectomy syndrome assessment scale (PGSAS)-45: newly developed integrated questionnaires for assessment of living status and quality of life in postgastrectomy patients. Gastric Cancer. 2015;18:147-158. [DOI] [PubMed] [Google Scholar]
- 23. Laurenius A, Olbers T, Näslund I, Karlsson J. Dumping syndrome following gastric bypass: validation of the Dumping Symptom Rating Scale. Obes Surg. 2013;23:740-755. [DOI] [PubMed] [Google Scholar]
- 24. Hejazi RA, Patil H, McCallum RW. Dumping syndrome: establishing criteria for diagnosis and identifying new etiologies. Dig Dis Sci. 2010;55:117-123. [DOI] [PubMed] [Google Scholar]
- 25. Cadegiani FA, Silva OS. Acarbose promotes remission of both early and late dumping syndromes in post-bariatric patients. Diabetes Metab Syndr Obes. 2016;9:443-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang C, Pang S, Jiang Q, Duan G, Sun Y, Li M. Treatment with acarbose in severe hypoglycaemia due to late Dumping syndrome. West Indian Med J. 2013;62:861-863. [DOI] [PubMed] [Google Scholar]
- 27. Buscemi S, Mattina A, Genova G, Genova P, Nardi E, Costanzo M. Seven-day subcutaneous continuous glucose monitoring demonstrates that treatment with acarbose attenuates late dumping syndrome in a woman with gastrectomy for gastric cancer. Diabetes Res Clin Pract. 2013;99:e1-e2. [DOI] [PubMed] [Google Scholar]
- 28. Valderas JP, Ahuad J, Rubio L, Escalona M, Pollak F, Maiz A. Acarbose improves hypoglycaemia following gastric bypass surgery without increasing glucagon-like peptide 1 levels. Obes Surg. 2012;22:582-586. [DOI] [PubMed] [Google Scholar]
- 29. De Cunto A, Barbi E, Minen F, Ventura A. Safety and efficacy of high-dose acarbose treatment for dumping syndrome. J Pediatr Gastroenterol Nutr. 2011;53:113-114. [DOI] [PubMed] [Google Scholar]
- 30. Moreira RO, Moreira RB, Machado NA, Gonçalves TB, Coutinho WF. Post-prandial hypoglycemia after bariatric surgery: pharmacological treatment with verapamil and acarbose. Obes Surg. 2008;18:1618-1621. [DOI] [PubMed] [Google Scholar]
- 31. Mohammadi A, Sulaiman RA, Grossman AB. Pasireotide and octreotide in the treatment of severe late dumping syndrome. Clin Case Rep. 2017;5:1608-1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sato D, Morino K, Ohashi N, et al. octreotide improves early dumping syndrome potentially through incretins: a case report. Endocr J. 2013;60:847-853. [DOI] [PubMed] [Google Scholar]
- 33. Arts J, Caenepeel P, Bisschops R, et al. Efficacy of the long-acting repeatable formulation of the somatostatin analogue octreotide in postoperative dumping. Clin Gastroenterol Hepatol. 2009;7:432-437. [DOI] [PubMed] [Google Scholar]
- 34. Amagai M, Tsuchiya H, Chiba Y, et al. Incretin kinetics before and after miglitol in Japanese patients with late dumping syndrome. J Clin Med Res. 2017;9:879-885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hirose S, Iwahashi Y, Seo A, Sumiyoshi M, Takahashi T, Tamori Y. Concurrent therapy with a low-carbohydrate diet and miglitol remarkably improved the postprandial blood glucose and insulin levels in a patient with reactive hypoglycemia due to late dumping syndrome. Intern Med. 2016;55:1137-1142. [DOI] [PubMed] [Google Scholar]
- 36. Fujita Y, Tamada D, Kozawa J, et al. Successful treatment of reactive hypoglycemia secondary to late dumping syndrome using miglitol. Intern Med. 2012;51:2581-2585. [DOI] [PubMed] [Google Scholar]
- 37. Chiappetta S, Stier C. A case report: liraglutide as a novel treatment option in late dumping syndrome. Medicine (Baltimore). 2017;96:e6348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Calabria AC, Charles L, Givler S, De León DD. Postprandial hypoglycemia in children after gastric surgery: clinical characterization and pathophysiology. Horm Res Paediatr. 2016;85:140-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Thondam SK, Nair S, Wile D, Gill GV. Diazoxide for the treatment of hypoglycaemic dumping syndrome. QJM. 2013;106:855-858. [DOI] [PubMed] [Google Scholar]
- 40. Craig CM, Liu LF, Deacon CF, Holst JJ, McLaughlin TL. Critical role for GLP-1 in symptomatic post-bariatric hypoglycaemia. Diabetologia. 2017;60:531-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shoar S, Nguyen T, Ona MA, et al. Roux-en-Y gastric bypass reversal: a systematic review. Surg Obes Relat Dis. 2016;12:1366-1372. [DOI] [PubMed] [Google Scholar]
- 42. Lakdawala M, Limas P, Dhar S, et al. Laparoscopic revision of Roux-en-Y gastric bypass to sleeve gastrectomy: a ray of hope for failed Roux-en-Y gastric bypass. Asian J Endosc Surg. 2016;9:122-127. [DOI] [PubMed] [Google Scholar]
- 43. Stier C, Chiappetta S. Endoluminal revision (OverStitch™, Apollo Endosurgery) of the dilated gastroenterostomy in patients with late dumping syndrome after proximal Roux-en-Y gastric bypass. Obes Surg. 2016;26:1978-1984. [DOI] [PubMed] [Google Scholar]
- 44. Huang CK, Wang MY, Das SS, Chang PC. Laparoscopic conversion to loop duodenojejunal bypass with sleeve gastrectomy for intractable dumping syndrome after Roux-en-Y gastric bypass—two case reports. Obes Surg. 2015;25:947. [DOI] [PubMed] [Google Scholar]
- 45. Garritano S, Irino T, Scandavini CM, Tsekrekos A, Lundell L, Rouvelas I. Long-term functional outcomes after replacement of the esophagus in pediatric patients: a systematic literature review. J Pediatr Surg. 2017;52:1398-1408. [DOI] [PubMed] [Google Scholar]
- 46. Davis JL, Ripley RT. Postgastrectomy syndromes and nutritional considerations following gastric surgery. Surg Clin North Am. 2017;97:277-293. [DOI] [PubMed] [Google Scholar]
- 47. van Beek AP, Emous M, Laville M, Tack J. Dumping syndrome after esophageal, gastric or bariatric surgery: pathophysiology, diagnosis, and management. Obes Rev. 2017;18:68-85. [DOI] [PubMed] [Google Scholar]
- 48. Wölnerhanssen BK, Meyer-Gerspach AC, Peters T, Beglinger C, Peterli R. Incretin effects, gastric emptying and insulin responses to low oral glucose loads in patients after gastric bypass and lean and obese controls. Surg Obes Relat Dis. 2016;12:1320-1327. [DOI] [PubMed] [Google Scholar]
- 49. Nagasaka K, Fukuda H, Natori M. Clinical experience of Keishi-to type herbal medication for dumping syndrome. Jpn J Orient Med. 2006;57:278. [Google Scholar]
- 50. Nishi M, Shimada M, Uchiyama H, et al. The beneficial effects of Kampo medicine Dai-ken-chu-to after hepatic resection: a prospective randomized control study. Hepatogastroenterology. 2012;59:2290-2294. [DOI] [PubMed] [Google Scholar]
- 51. Katsuno H, Maeda K, Kaiho T, et al. Clinical efficacy of Daikenchuto for gastrointestinal dysfunction following colon surgery: a randomized, double-blind, multicenter, placebo-controlled study (JFMC39-0902). Jpn J Clin Oncol. 2015;45:650-656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Qi QH, Wang J, Liang GG, Wu XZ. Da-Cheng-Qi-Tang promotes the recovery of gastrointestinal motility after abdominal surgery in humans. Dig Dis Sci. 2007;52:1562-1570. [DOI] [PubMed] [Google Scholar]
- 53. Koeda K, Wakabayashi G, Shimada M, et al. Mo1798 Daikenchuto (DKT) helps improve postoperative functional gastrointestinal disorder after total gastrectomy in patients with gastric cancer: a multicenter, randomized, double-blind, placebo-controlled trial (JFMC42-1002). Gastroenterology. 2014;146(5 suppl 1):S-1074. [Google Scholar]
- 54. Hatano E, Uemoto S, Shimada M, et al. Daikenchuto improves functional gastrointestinal disorder after hepatic resection in patients with liver cancer: a multicenter, randomized, double-blind, placebo-controlled phase II trial (JFMC40-1001). Hepatology. 2012;56:492A.22334511 [Google Scholar]
- 55. Endo S, Nishida T, Nishikawa K, et al. Daikenchu-to, a Chinese herbal medicine, improves stasis of patients with total gastrectomy and jejunal pouch interposition. Am J Surg. 2006;192:9-13. [DOI] [PubMed] [Google Scholar]
- 56. Yoshikawa K, Shimada M, Wakabayashi G, et al. Effect of Daikenchuto, a traditional Japanese herbal medicine, after total gastrectomy for gastric cancer: a multicenter, randomized, double-blind, placebo-controlled, phase II trial. J Am Coll Surg. 2015;221:571-578. [DOI] [PubMed] [Google Scholar]
- 57. Takahashi T, Endo S, Nakajima K, Souma Y, Nishida T. Effect of Rikkunshito, a Chinese herbal medicine, on stasis in patients after pylorus-preserving gastrectomy. World J Surg. 2009;33:296-302. [DOI] [PubMed] [Google Scholar]
- 58. Suehiro T, Matsumata T, Shikada Y, Sugimachi K. The effect of the herbal medicines Dai-kenchu-to and Keishi-bukuryo-gan on bowel movement after colorectal surgery. Hepatogastroenterology. 2005;52:97-100. [PubMed] [Google Scholar]
- 59. Ge HY, Chen B, Li YT. Effects of acupuncture on gastrointestinal responses after renal transplantation [in Chinese]. Zhongguo Zhen Jiu. 2008;28:177-178. [PubMed] [Google Scholar]
- 60. Nakamura M, Nakamori M, Ojima T, et al. The effects of rikkunshito on body weight loss after esophagectomy. J Surg Res. 2016;204:130-138. [DOI] [PubMed] [Google Scholar]
- 61. Xue T, Zhang J, Pan LQ, et al. Enteroclyster with composite Dachengqi decoction in the treatment of gastroparesis syndromes after resection of esophageal carcinoma or cardiac carcinoma. J Clin Rehabil Tissue Eng Res. 2007;11:4953-4956. [Google Scholar]
- 62. Sunagawa H, Oshiro N. Influence of Daikenchuto on patient’s portal blood flow after pancreatoduodenectomy. HPB. 2011;13:209. [Google Scholar]
- 63. Xu Z, Xu C, Ge H, et al. Modified Dachengqi tang improves decreased gastrointestinal motility in postoperative esophageal cancer patients. J Tradit Chin Med. 2015;35:249-254. [DOI] [PubMed] [Google Scholar]
- 64. Dang ZX. Postoperative therapy of 255 cases of subtotal gastrectomy with traditional Chinese medicine combined with Western medicine [in Chinese]. Zhong Xi Yi Jie He Za Zhi. 1987;7:389,412-414. [PubMed] [Google Scholar]
- 65. Yu Q, Chen Z, Tang X. Study on early application of Chinese medicinal herbs after total gastrectomy [in Chinese]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 1999;19:592-594. [PubMed] [Google Scholar]
- 66. Takiguchi S. Ghrelin and clinical research: review about post-gastrectomy patients. Improvement on dysfunction and increase of acylated ghrelin of post-gastrectomy patients by administrating Rikkunshi-to. Sci Kampo Med. 2012;36:198-201. [Google Scholar]
- 67. Fu Y. Application of integrated medical care for complication after laparoscopic gastric cancer surgery. Yunnan J Tradit Chin Med Mater Med. 2015;1:104-105. [Google Scholar]
- 68. Nishida S. “Opening the traditional Chinese medicine’ (#90): Rikkunshi-to significantly stimulates the discharge of solid food in the gastric emptying capacity after gastrectomy. Sci Kampo Med. 2009;33:410-412. [Google Scholar]
- 69. Zhang W, Mao Y. Oriental medical doctor Huang Bingliang’s clinical experience of gastric diseases. Liaoning J Tradit Chin Med. 1983;3:28-30. [Google Scholar]
- 70. Peng R. Fifty-two cases of early dumping syndrome after the operation on stomach cancer treated with decoction of officinal magnolia bark and fresh ginger and pinellia and licorice and ginseng. Henan Tradit Chin Med. 2015;35:2906-2907. [Google Scholar]
- 71. Quan GM. Clinical Research of Dumping Syndrome After Gastric Cancer Surgery Treated With Pingyuntiaowei Decoction [thesis]. Nanjing, China: Nanjing University of Chinese Medicine; 2004. [Google Scholar]
- 72. Zhou ZC. Clinical trial of 20 cases of dumping syndrome after gastric surgery treated with integrated medicine. J Pract Tradit Chin Med. 2014;30:731. [Google Scholar]
- 73. Wu KL, Rayner CK, Chuah SK, et al. Effects of ginger on gastric emptying and motility in healthy humans. Eur J Gastroenterol Hepatol. 2008;20:436-440. [DOI] [PubMed] [Google Scholar]
- 74. Niijima A, Okui Y, Kubo M, et al. Effect of Pinellia ternata tuber on the efferent activity of the gastric vagus nerve in the rat. Brain Res Bull. 1993;32:103-106. [DOI] [PubMed] [Google Scholar]
- 75. Wang YS. Pharmacology and Applications of Chinese Materia Medica. Beijing, China: People’s Health Publisher; 1983:770-775. [Google Scholar]
- 76. Kawai T, Kinoshita K, Koyama K, Takashi K. Anti-emetic principles of Magnolia obovata bark and Zingiber officinale rhizome. Planta Med. 1994;60:17-20. [DOI] [PubMed] [Google Scholar]