Abstract
Background
Healthcare disparities for psychiatric patients are common. Whether these inequalities apply to postresuscitation management in out‐of‐hospital cardiac arrest (OHCA) is unknown. We investigated differences in in‐hospital cardiovascular procedures following OHCA between patients with and without psychiatric disorders.
Methods and Results
Using the Danish nationwide registries, we identified patients admitted to the hospital following OHCA of presumed cardiac cause (2001‐2015). Psychiatric disorders were identified using hospital diagnoses or redeemed prescriptions for psychotropic drugs. We calculated age‐ and sex‐standardized incidence rates and incidence rate ratios (IRRs) of cardiovascular procedures during post‐OHCA admission in patients with and without psychiatric disorders. Differences in 30‐day and 1‐year survival were assessed by multivariable logistic regression in the overall population and among 2‐day survivors who received acute coronary angiography (CAG). We included 7288 hospitalized patients who had experienced an OHCA: 1661 (22.8%) had a psychiatric disorder. Compared with patients without psychiatric disorders, patients with psychiatric disorders had lower standardized incidence rates for acute CAG (≤1 day post‐OHCA) (IRR, 0.51; 95% CI, 0.45–0.57), subacute CAG (2–30 days post‐OHCA) (IRR, 0.40; 95% CI, 0.30–0.52), and implantable cardioverter‐defibrillator implantation (IRR, 0.67; 95% CI, 0.48–0.95). Conversely, we did not detect differences in coronary revascularization among patients undergoing CAG (IRR, 1.11; 95% CI, 0.94–1.30). Patients with psychiatric disorders had lower survival even among 2‐day survivors who received acute CAG: (odds ratio of 30‐day survival, 0.68; 95% CI, 0.52–0.91; and 1‐year survival, 0.66; 95% CI, 0.50–0.88).
Conclusions
Psychiatric patients had a lower probability of receiving post‐OHCA CAG and implantable cardioverter‐defibrillator implantation compared with nonpsychiatric patients but the same probability of coronary revascularization among patients undergoing CAG. However, their survival was lower irrespective of angiographic procedures.
Keywords: cardiovascular procedures, healthcare disparities, in‐hospital post‐arrest management, out‐of‐hospital cardiac arrest, psychiatric disorders
Subject Categories: Sudden Cardiac Death, Mental Health, Cardiopulmonary Resuscitation and Emergency Cardiac Care, Cardiopulmonary Arrest, Epidemiology
Clinical Perspective
What Is New?
Patients with psychiatric disorders who experience out‐of‐hospital cardiac arrest have a 50% reduced chance of receiving a coronary angiography and 30% reduced chance of having an implantable cardioverter‐defibrillator implanted in the postarrest hospitalization compared with patients without psychiatric disorders but the same probability of coronary revascularization among patients undergoing coronary angiography.
Patients with psychiatric disorders have lower short‐ and long‐term postarrest survival irrespective of acute cardiovascular procedures.
What Are the Clinical Implications?
A better understanding of the causes underlying cardiac arrest in patients with psychiatric disorders is warranted to tailor a more suitable postresuscitation management considering their special characteristics and their high postarrest mortality.
Considering the large burden of cardiovascular morbidity and mortality within psychiatric disorders, an aggressive cardiovascular postarrest management, equal to the general population, is required in case of out‐of‐hospital cardiac arrests of presumed cardiac cause.
Future works should focus on the reasons behind these treatment inequalities, especially from the healthcare providers’ side.
Introduction
An aggressive and prompt postresuscitation management can double the chances of long‐term survival following out‐of‐hospital cardiac arrest (OHCA).1, 2 Invasive cardiovascular procedures are key components of postarrest management considering that ischemic heart disease represents the most common cause of OHCA.1, 3 Patients with psychiatric disorders are at higher risk of cardiovascular morbidity and mortality, and sudden cardiac arrest, primarily attributable to acute coronary events, markedly contributes to their substantial shorter life expectancy compared with the general population.4, 5, 6, 7
Disparities in healthcare provision between patients with and without a known psychiatric disorder have been documented worldwide. They concern both medical and invasive cardiovascular treatments and contribute to the excess cardiovascular mortality in such patients.7, 8, 9, 10 These inequalities have been attributed to various factors such as mental health stigma, diagnostic overshadowing, low treatment compliance, and higher rates of complications after invasive procedures.7, 9, 11
Whether an inequitable management also occurs in relation to a life‐threatening condition such as OHCA is unknown. This prompted us to determine possible differences in selected postresuscitation cardiovascular procedures: coronary angiography (CAG), coronary revascularization, and implantable cardioverter‐defibrillator (ICD) implantation in patients who experience OHCA with and without psychiatric disorders.
Methods
The data, analytical methods, and study materials cannot be made available to other researchers for purposes of reproducing the results or replicating the procedure.
Data Sources and Definitions
All OHCAs from June 2001 through December 2015 were identified from the nationwide Danish Cardiac Arrest Registry.12 OHCA was defined when a clinical condition of cardiac arrest resulted in cardiopulmonary resuscitation (CPR), either by a bystander or emergency medical services personnel. The presumed cause of OHCA was defined using death certificates and discharge diagnoses from the index hospitalization. Cardiac disease, unknown disease, or unexpected collapse was defined as presumed cardiac cause of arrest.12
In Denmark, every citizen is provided a permanent and unique civil registration number upon birth or immigration, which permits individual‐level identification across the nationwide registries. Information on sex and age was retrieved from the Danish Civil Registration System. Household income was found through Statistics Denmark. Information on hospital admission and in‐hospital procedures was obtained from the Danish National Patient Registry, where diagnoses are encoded according to the International Classification of Diseases (ICD), until 1994 the International Classification of Diseases, Eighth Revision (ICD‐8) and from 1994 the International Classification of Diseases, Tenth Revision (ICD‐10). Vital status and information on causes of death, including primary and contributing causes, were retrieved from the Danish Register of Causes of Death; information on psychiatric hospitalizations and ambulatory contacts from the Danish Psychiatric Central Research Register; and information on claimed drug prescriptions from the National Prescription Register, where medications are classified according to the international Anatomical Therapeutic Chemical classification system.
Study Population
We included all patients between 18 and 100 years of age with OHCA of presumed cardiac cause who received an inpatient hospital admission following OHCA. Patients with emergency medical services–witnessed arrest, those declared dead before hospital arrival, and those who died in the emergency department were excluded (Figure 1).
Figure 1.
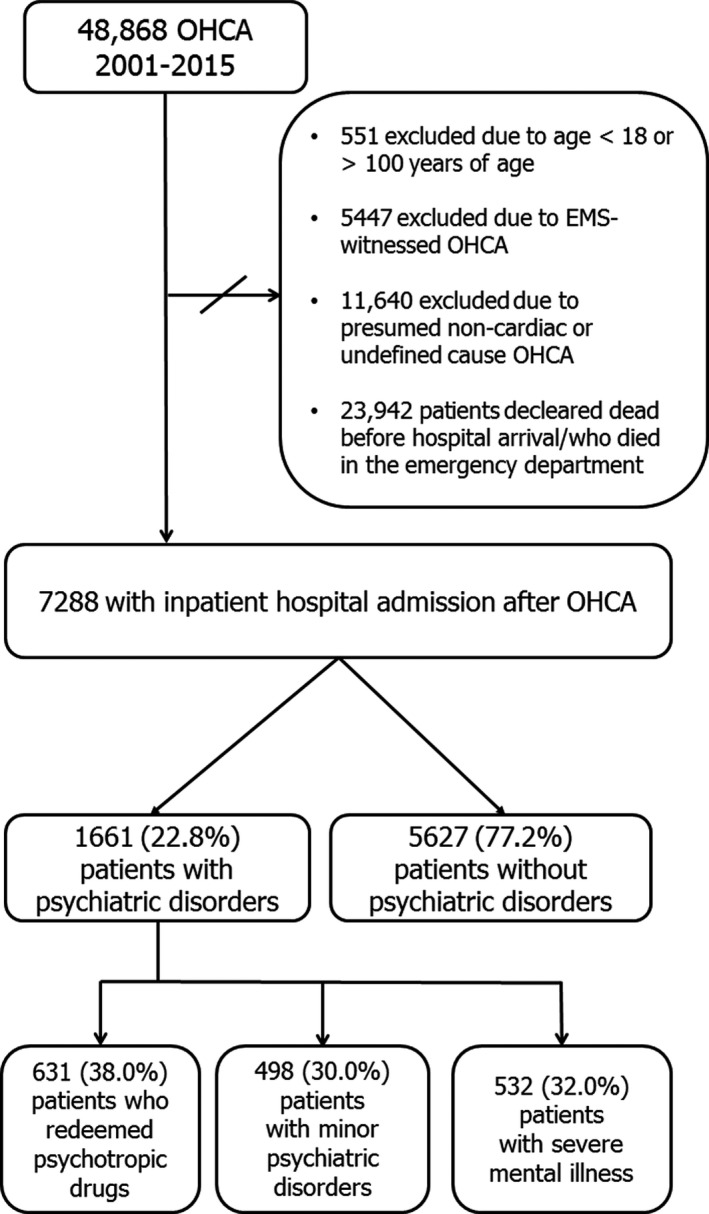
Patient selection. EMS indicates emergency medical services; OHCA, out‐of‐hospital cardiac arrest.
Patients were classified as having psychiatric disorders if they either:
-
Had a hospital‐based psychiatric discharge diagnosis (primary or secondary) or an ambulatory contact diagnosis from either the Danish Psychiatric Central Research Registry or the Danish National Patient Registry up to 10 years before OHCA. The ICD codes used are summarized in Table S1 (dementia, mental organic disorders, and acute substance intoxication were not regarded as psychiatric disorders).
or
Redeemed prescriptions for psychotropic drugs (either antidepressants, antipsychotics, or lithium; see Table S2) within 90 days before OHCA without having a hospital psychiatric diagnosis. These individuals represent a group of psychiatric patients treated in the primary sector, not reported in the hospital‐based registries.
In subanalyses, patients with psychiatric disorders were divided into 3 mutually exclusive subgroups according to the severity of the psychiatric disorder, as done previously13:
Severe mental illness (SMI)7: identified by hospital discharge diagnoses.
Minor psychiatric disorders (including substance‐induced mental disorders and other psychiatric disorders not encompassed in SMI): identified by hospital discharge diagnoses.
Patients who redeemed psychotropic drugs without having a hospital psychiatric contact.
The codes employed to classify patients with SMI and minor psychiatric disorders are listed in Table S1. If >1 diagnosis was present, the patient was assigned to the most severe subgroup in accordance with the diagnostic hierarchical order in the psychiatric ICD‐10 classification.13
The Charlson score was determined using discharge diagnosis codes up to 10 years before OHCA.14 As a proxy for diabetes mellitus, we identified redeemed prescriptions for antidiabetic drugs within 180 days before OHCA.14 Socioeconomic status was defined according to the average family income for the past 5 years before OHCA and was grouped into tertiles (low, middle, and high).15
Outcomes
Cardiovascular procedures following OHCA
We examined:
Acute CAG: within 0 to 1 day after OHCA.
Subacute CAG: between 2 and 30 days after OHCA.
In addition, among patients who received a CAG, we evaluated the composite outcome of coronary revascularization, encompassing coronary artery bypass graft and percutaneous coronary intervention (PCI).
Among ICD‐naïve patients surviving to discharge, we examined the rate of ICD implantation during index hospitalization excluding patients with acute myocardial infarction (I21–24) as presumed cause of OHCA, those who received coronary revascularization during the index hospitalization and patients with nonshockable or unknown initial cardiac rhythm (Figure S1).15, 16 Patients with ischemic heart disease as the presumed cause of OHCA were excluded from this analysis, as the ICD implantation in such patients is not always required and, if indicated, often postponed to a later phase, for example, following uptitration of anticongestive medication.16
Coronary revascularization and ICD implantation were evaluated during the index admission up to 30 days after OHCA, with the starting point at the day of hospitalization for OHCA. A patient contributed to the analysis only if still alive, still hospitalized, and if the outcome of interest was not met. The codes used for cardiovascular procedures are listed in Table S3.
Survival Outcomes
We assessed differences in 30‐day and 1‐year‐survival between patients with and without psychiatric disorders in the overall population and in 2‐day survivors who received an acute CAG.
Statistics
We computed age‐ and sex‐standardized incidence rates (SIRs), and relative incidence rate ratios (IRRs), for acute CAG, subacute CAG, coronary revascularization, and ICD implantation in patients with and without psychiatric disorders.17 SIRs were standardized to the sex and age distribution only of patients included in the respective analysis/subanalysis, using the following age‐groups: <60, 60 to 69, 70 to 79, and ≥80 years.
To account for differences in baseline characteristics in patients with and without psychiatric disorders, we repeated analyses for acute and subacute CAG in subsets of patients defined by the presence of factors potentially influencing the execution of a CAG15, 18, 19:
Patients with witnessed OHCA who received bystander CPR.
Patients with initial shockable rhythm.
Patients with return of spontaneous circulation (ROSC) upon hospital arrival.
Patients with initial shockable rhythm and ROSC upon hospital arrival.
Stratifying by socioeconomic status.
Stratifying by burden of comorbidity (Charlson score).
Separately for men and women.
Separately for 2 calendar‐year groups: 2001 to 2007 and 2008 to 2015.
Moreover, since guidelines have specific recommendations for acute cardiovascular interventions in case of ST‐segment elevation myocardial infarction (STEMI) on the postresuscitation ECG,3, 20 using previously validated ICD‐10 diagnosis codes,21 we conducted a sensitivity analysis only among patients with STEMI as the presumed cause of OHCA.
The association between procedure outcomes (CAG, coronary revascularization, and ICD implantation) and psychiatric status was further assessed using Cox regression models (with death as competing risk) adjusted for age, sex, Charlson score, socioeconomic status, year of OHCA, and OHCA factors (location of arrest, witnessed status, initial cardiac rhythm, bystander CPR, and ROSC upon hospital arrival).
We used multivariable logistic regression to assess the association between psychiatric disorders and survival status at 30 days and 1 year following OHCA adjusted for sex, age, Charlson score, socioeconomic status, year of arrest, and prehospital OHCA characteristics (location of arrest, witnessed status, bystander CPR, initial cardiac rhythm, and ROSC upon hospital arrival). The analysis was conducted in the overall population (landmark point: day of OHCA) and among 2‐day survivors who received acute CAG (landmark point, 2 days after OHCA).
Missing data were handled by multiple imputation based on 200 imputed data sets based on fully conditional specification using the smcfcs package in R (R Development Core Team),22 and the estimates were combined using Rubin's rule.
We conducted sensitivity analyses including only patients who experienced OHCA for whom complete information on all variables was available (complete case analyses).
SAS version 9.4 (SAS Institute Inc., Cary, NC) and R version 3.5.1 were used for data management and statistical analyses.23
Ethics
The study was approved by the Danish Data Protection Agency (Ref. no. 2007‐58‐0015, local ref. no. GEH‐2014‐017, I‐Suite.nr. 02735). The information on the study population was encrypted and rendered anonymous by Statistics Denmark. For observational studies based on anonymous data in Denmark, informed consent and ethical approval is not required.
Results
We included 7288 patients; 1661 (22.8%) had a psychiatric disorder (Figure 1). Baseline and prehospital OHCA characteristics of the study population are presented in Table (in Table S4 stratified by subgroups of psychiatric disorder).
Table 1.
Patient and Arrest Characteristics According to Psychiatric Status—Overall Population
| Characteristic | Patients Without Psychiatric Disorders | Patients With Psychiatric Disorders | P Value | Missing Data (%)a |
|---|---|---|---|---|
| Total patients | 5627 (77.2) | 1661 (22.8) | ||
| Median age (IQR), y | 68 (58–76) | 67 (56–76) | 0.210 | 0 |
| Men, n (%) | 4311 (76.6) | 997 (66.0) | <0.001 | 0 |
| Charlson score, n (%) | ||||
| 0 | 2727 (48.5) | 483 (29.1) | <0.001 | 0 |
| 1 | 1128 (20.1) | 366 (22.0) | ||
| ≥2 | 1772 (31.5) | 812 (48.9) | ||
| Antipsychotics, n (%) | 0 (0.0) | 384 (23.1) | <0.001 | 0 |
| Antidepressants, n (%) | 0 (0.0) | 1063 (64.0) | <0.001 | 0 |
| Anxiolytics, n (%) | 242 (4.3) | 354 (21.3) | <0.001 | 0 |
| Living alone—yes, n (%) | 1604 (28.6) | 823 (49.7) | <0.001 | 31 (0.4) |
| Socioeconomic status | ||||
| Low tertile, n (%) | 1672 (29.7) | 757 (45.6) | <0.001 | 0 |
| Medium tertile, n (%) | 1850 (32.9) | 580 (34.9) | ||
| High tertile, n (%) | 2105 (37.4) | 324 (19.5) | ||
| OHCA factors | ||||
| Arrest in private home, n (%) | 2973 (58.1) | 1012 (66.7) | <0.001 | 655 (8.9) |
| Bystander‐witnessed arrest, n (%) | 4167 (76.5) | 1103 (69.4) | <0.001 | 251 (3.4) |
| Bystander CPR, n (%) | 3385 (62.1) | 890 (55.9) | <0.001 | 241 (3.3) |
| Bystander defibrillation, n (%) | 394 (7.6) | 63 (4.2) | <0.001 | 593 (8.1) |
| Median time interval from recognition of OHCA to EMS arrival, min (IQR) | 10 (6–14) | 10 (6–14) | 0.967 | 1091 (14.9) |
| Initial shockable rhythm, n (%) | 3523 (65.2) | 615 (38.9) | <0.001 | 301 (4.1) |
| ROSC at hospital arrival, n (%) | 3574 (70.0) | 1026 (69.7) | 0.139 | 711 (9.8) |
| Outcome | ||||
| 30‐day survival, n (%) | 2385 (42.4) | 453 (27.3) | <0.001 | 0 |
| 1‐y survival, n (%) | 2214 (39.4) | 382 (23.0) | <0.001 | 0 |
| In‐hospital procedure | ||||
| CAG | 2673 (47.5) | 438 (26.4) | <0.001 | 0 |
| Acute CAGb | 2076 (36.9) | 370 (22.3) | <0.001 | 0 |
| Subacute CAGc | 597 (10.6) | 68 (4.1) | <0.001 | 0 |
Note: In the calculation of percentages, we included only observations with data for the covariate involved. CAG indicates coronary angiography; CPR, cardiopulmonary resuscitation; EMS, emergency medical system; IQR, interquartile range; OHCA, out‐of‐hospital cardiac arrest; ROSC, return of spontaneous circulation.
Expressed as percentage of the entire population (7288 patients with OHCA).
≤24 h from OHCA.
During the index hospitalization from >24 h (ie, day 2) up to day 30 following OHCA.
Coronary Angiography
In total, 3111 (42.7%) patients underwent a CAG during the index hospitalization: 26.4% of the psychiatric population and 47.5% of the nonpsychiatric population (Figure 2). The majority of CAG was performed acute in both populations (Figure 2). SIRs for acute and subacute CAG were lower for patients with psychiatric disorders compared with patients without psychiatric disorders: IRR. 0.51 (95% CI, 0.45–0.57) and 0.40 (95% CI, 0.30–0.52), respectively (Figure 3). Similar results were seen when we stratified by the subgroups of psychiatric disorder (Figure 3).
Figure 2.
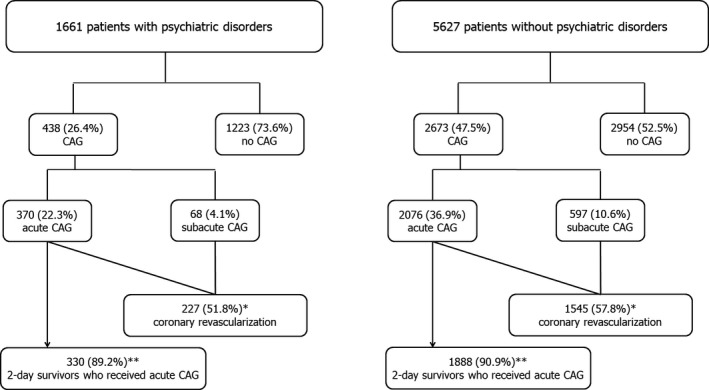
Number of total patients undergoing CAG, acute and subacute CAG, and coronary revascularization, and 2‐day survivors who received acute CAG during index hospitalization among patients with and without psychiatric disorders. *Percentage of patients who received a CAG (both acute and subacute); **Percentage of patients who received an acute CAG. CAG indicates coronary angiography.
Figure 3.
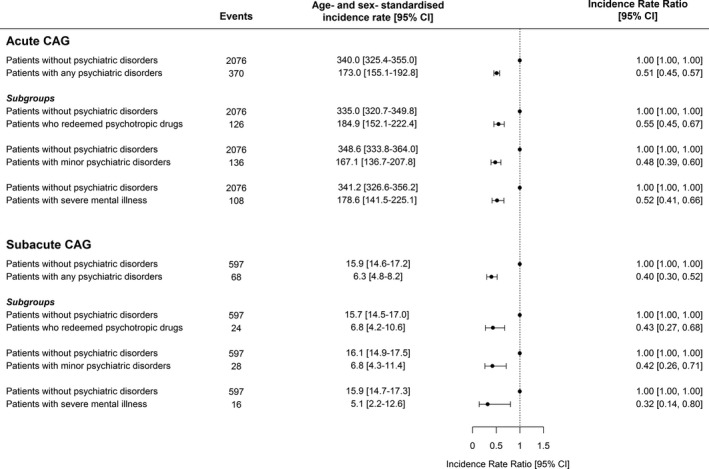
Number of events, age‐ and sex‐standardized incidence rates and incidence rate ratio for acute and subacute CAG in patients with and without psychiatric disorders. In the main analysis, patients with psychiatric disorders are pooled in a single group; in subanalyses, they are classified into 3 mutually exclusive subgroups. Unit: number of CAGs per 100 in‐hospital person‐days. CAG indicates coronary angiography.
Patients with psychiatric disorders were also associated with significantly lower rates of CAG in the subset of patients with favorable prehospital OHCA features, that is, patients with witnessed OHCA who received bystander CPR, patients with initial shockable rhythm, patients who achieved ROSC, and patients with initial shockable rhythm who achieved ROSC (Figure S2), and regardless of Charlson score and socioeconomic status (Figures S3 and S4). SIRs for acute CAG increased during the study period in both groups, but more markedly among patients without psychiatric disorders (Figure S5). Women had lower SIRs for CAG compared with men in both groups, but the difference between patients with and without psychiatric disorders were similar to main analysis in both sexes (Figure S6).
More patients without psychiatric disorders had AMI and particularly STEMI as the presumed cause of OHCA (Table S5). Nevertheless, even among patients who had STEMI, patients with psychiatric disorders less often received acute CAG (75.5% versus 86.7%) and had lower SIRs for acute CAG compared with patients without psychiatric disorders (Figure S7). The IRR points toward a difference between the 2 groups: 0.74 (95% CI, 0.53–1.02).
Coronary Revascularization
Among patients who underwent CAG, 1772 (57.0%) received coronary revascularization during the index hospitalization up to 30 days after OHCA (1578 PCI [89.1%] and 194 coronary artery bypass graft [10.9%]): 227 (51.8%) among patients with and 1545 (57.8%) without psychiatric disorders (Figure 2). We did not detect any significant differences in SIRs for coronary revascularization between the 2 groups (IRR, 1.11; 95% CI, 0.94–1.30) (Figure 4A).
Figure 4.
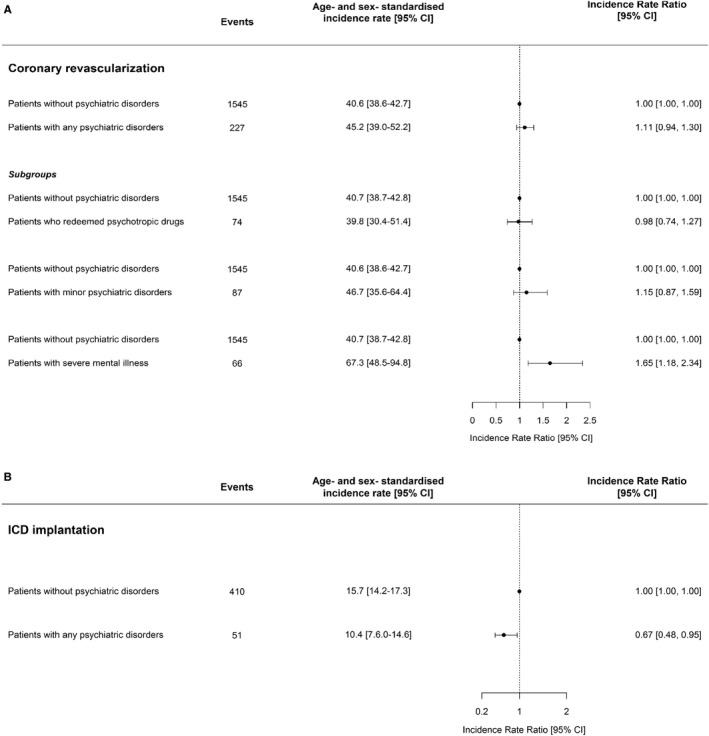
Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio in patients with and without psychiatric disorders for (A) coronary revascularization among patients experiencing OHCA who received a coronary angiography and (B) ICD implantation among ICD‐naïve patients surviving to discharge who had shockable initial cardiac rhythm and who did not have ischemic heart disease as the presumed cause of arrest. Unit: number of procedures per 100 person‐days in hospital. ICD indicates implantable cardioverter‐defibrillator; OHCA, out‐of‐hospital cardiac arrest.
Results were consistent when we investigated only rates of PCI (data not shown); because of sample size limitations, a separate analysis could not be performed for coronary artery bypass graft.
Stratifying by subgroups of psychiatric disorder, we found that patients undergoing CAG with SMI had significantly higher SIRs for coronary revascularization compared with patients undergoing CAG without psychiatric disorders (IRR, 1.65; 95% CI, 1.18–2.34) (Figure 4A).
ICD Implantation
A total of 942 (12.9%) patients were eligible for analysis for ICD implantation (Figure S1). Among these patients, 461 (46.0%) had an ICD implanted during the index hospitalization: 51 (32.5%) patients with and 410 (48.5%) without psychiatric disorders (Figure S1). SIRs for ICD implantation in patients with psychiatric disorders were significantly lower compared with those in patients without psychiatric disorders (IRR, 0.67; 95% CI, 0.48–0.95) (Figure 4B).
The subanalyses stratified by subgroups of psychiatric disorders were not reported because of too few events to get meaningful results.
Results From Cox Analyses
The results from multivariable analyses for CAG, coronary revascularization, and ICD implantation did not differ from the main results (Table S6).
Survival Outcomes
Among patients with psychiatric disorders, 453 (27.3%) and 382 (23.0%) survived at 30 days and 1 year after OHCA, respectively, versus 2385 (42.4%) and 2214 (39.4%) patients without psychiatric disorders. Patients with psychiatric disorders had overall significantly lower odds of both 30‐day and 1‐year survival compared with patients without psychiatric disorders (Figure 5), as well as when stratified by subgroups of psychiatric disorders (Figure S8A). Among patients who received acute CAG, 330 (89.2%) patients with and 1888 (90.9%) patients without psychiatric disorders were still alive at day 2 (Figure 2): In this population, having a mental disorder was still associated with lower survival (Figure 5). Particularly, stratifying by psychiatric subgroups, patients with SMI had significantly lower chances of both 30‐day and 1‐year survival (Figure S8B). Characteristics of patients who underwent acute CAG still alive at day 2 are shown in Table S7, and stratified by psychiatric subgroups in Table S8.
Figure 5.
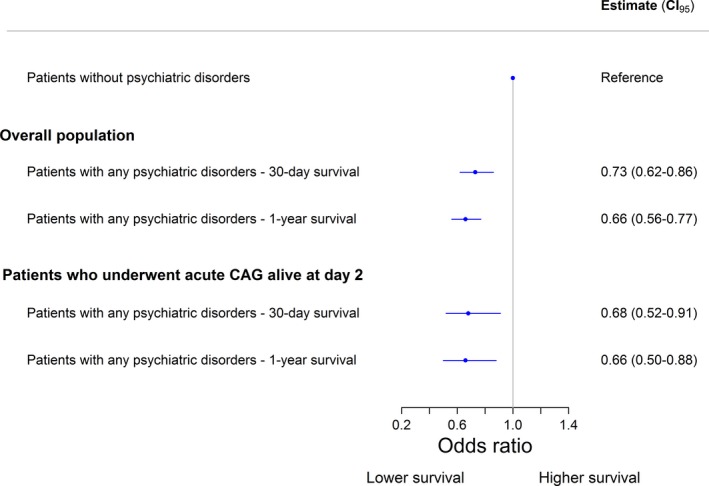
Odds ratio for 30‐day and 1‐year survival in patients with any psychiatric disorders compared with patients without psychiatric disorders in overall population and among patients who received acute CAG still alive at day 2. The models are adjusted for sex, age, Charlson score, socioeconomic status, year of arrest, and prehospital OHCA characteristics (location of arrest, witnessed status, initial cardiac rhythm, bystander CPR, and ROSC upon hospital arrival). Reference: patients without psychiatric disorders. CAG indicates coronary angiography; CPR, cardiopulmonary resuscitation; OHCA, out‐of‐hospital cardiac arrest; ROSC, return of spontaneous circulation.
Sensitivity Analysis
The results of complete case analysis (performed in 6324 cases) did not differ from the main analysis (Figure S9).
Discussion
In this nationwide cohort study including patients admitted to the hospital after OHCA of presumed cardiac cause, we found that having a psychiatric disorder was associated with lower rates of CAG and ICD implantation during the index hospitalization. Among patients undergoing CAG, no differences between the 2 groups were seen in the rates of coronary revascularization. Patients with psychiatric disorders were less likely to survive 30 days and 1 year after OHCA both in the overall population and among 2‐day survivors who received acute CAG.
Cardiovascular Postresuscitation Care and Psychiatric Disorders
Despite the importance of hospital‐based cardiovascular procedures for outcomes following OHCA and the Danish publicly financed healthcare system,1, 2, 3, 15 we found patients with psychiatric disorders to be significantly associated with lower likelihood of receiving both acute and subacute CAG as well as ICD implantation compared with psychiatric healthy patients.
Notably, autopsy studies have demonstrated that acute coronary events attributable to ischemic heart disease represent the most common cause of cardiac arrest regardless of psychiatric status.1, 3, 4, 24 Accordingly, the rate of coronary revascularization in patients with and without a psychiatric disorder did not differ when a CAG was performed in our cohort. Our psychiatric population had almost half the probability of receiving a CAG; hence, the possibility of underdiagnosis and undertreatment of coronary lesions among patients who experienced OHCA with a presumed cardiac cause seems to be high, in particular when considering the excess cardiovascular morbidity in patients with mental disorders.6, 7
Since 2006, the guidelines for management of cardiac arrest survivors have recommended a more aggressive postresuscitation cardiovascular intervention.16 Correspondingly, we found an increase in CAG rates in both patients with and without psychiatric disorders during the study period; however, this increase was more pronounced in patients without psychiatric disorders: For acute CAG, the CAG rates per 100 in‐hospital person‐days more than doubled for psychiatric healthy patients (from 180 in the period 2001–2007 to 427.5 in 2008–2015), while they increased from 119 to 191.5 for patients with psychiatric disorders.
While our study is the first to demonstrate such differences in patients who had OHCA, our findings confirm previous studies claiming an inequitable access to lifesaving procedures for patients who are mentally ill, even in the setting of acute cardiovascular events.7, 8, 9, 10 This disparity is advocated as one of the major factors leading to the increasing gap in cardiovascular mortality between patients with and without psychiatric disorders.7, 9
Causes Underlying Postresuscitation Care Inequalities
The reasons for disparities in post‐resuscitation care provision are diverse and may be related to the patients' pre‐hospital OHCA‐factors and baseline characteristics and the treating physicians.9 In our cohort, patients with psychiatric disorders were more likely to have unfavorable prehospital OHCA factors such as nonshockable heart rhythm or unwitnessed arrest. These features may have influenced the choice of diagnostic workup and treatment.18 However, the difference in CAG rates remained significant in subgroups of patients with characteristics associated with more favorable outcomes including initial shockable rhythm and in case of STEMI.1, 3, 18, 20 Similarly, we found a higher burden of comorbidity and a lower socioeconomic status among patients with psychiatric disorders, both factors previously shown to reduce the chances of receiving invasive postresuscitation cardiac procedures.15, 18 Nonetheless, in subgroup analyses, psychiatric disorders were related to lower rates of CAG regardless of these features.
Stigmatization of mental illness among healthcare providers is known to impact the decision of in‐hospital treatment.11 Accordingly, the difference between patients with and without psychiatric disorders in rates of subacute CAG, at which time patient‐related characteristics are more known by the clinicians, was even larger than that for acute CAG. Various factors related to mental disorders may discourage physicians from offering these patients invasive procedures: higher rates of complications and postoperative mortality, lower tolerance to intensive treatment, potential drug interactions with psychotropic medications (especially sedatives and anesthetics), poor physical condition, and self‐hygiene as well as poor adherence to the therapy.25, 26, 27
Survival Outcomes
Among patients admitted to the hospital following OHCA, having a psychiatric disorder was significantly related to higher short‐ and long‐term mortality. Similarly, other studies have previously observed a higher mortality among patients with psychiatric disorders following an index cardiovascular event compared with psychiatric healthy patients.10, 28
A deficient postresuscitation management only partly explains the larger mortality following OHCA associated with psychiatric disorders. In fact, our analyses showed that the imbalance in postarrest survival persisted when we examined patients receiving acute CAG—a proxy for more aggressive postarrest management. Furthermore, the difference in survival remained despite adjustments for prehospital OHCA factors, burden of comorbidity, and socioeconomic status.
Patients with psychiatric disorders often suffer from cognitive impairment, reduced pain responsiveness, limited self‐recognition, and lack of insight of their illness, which hamper their capacity to recognize symptoms and communicate with healthcare givers resulting in poor compliance and delayed diagnosis.25, 26, 27, 29 Similarly, physicians may focus more dominantly on alleviating psychiatric symptoms on the cost of poorer somatic disease control and care.11 The development during the hospital stay of delirium or other psychiatric symptoms requiring sedation and/or a combination of psychotropic medications may also lead to excess mortality.29, 30
Subgroups of Psychiatric Disorders
Lower CAG rates compared with patients without psychiatric disorders were seen for all the subgroups of psychiatric disorders, even among patients treated in primary care redeeming psychotropic medications.
The probability of survival following OHCA seemed to be particularly reduced for patients with SMI regardless of the aggressiveness of the postarrest management. In fact, these patients are more negatively marked by their mental illness in term of stigmatization and cognitive limitations with a likely impact on comorbidity burden.8, 10 This notion is supported by higher rates of coronary revascularization in this subgroup and underline the correlation between severity of psychiatric disorder and somatic disease.6, 31
Implications of the Study
Future studies should focus and shed light on the causes underlying OHCA in patients with psychiatric disorders to optimize their postresuscitation management. However, considering the large burden of cardiovascular morbidity and mortality in patients with psychiatric disorders and the results of our study and of some postmortem studies,4, 5, 24 an aggressive acute cardiac postresuscitation management, equal to the general population, could be warranted in case of OHCAs of presumed cardiac cause. Finally, a more focused and tailored postresuscitation management is required for such patients considering their special characteristics and their high postarrest mortality.
Limitations
Because of the observational nature of our study, we report associations that are not necessarily causal. Moreover, the Danish registries do not contain information about important clinical features, such as left ventricular ejection fraction and detailed history of tobacco and alcohol intake, which may have influenced the postarrest management.
Another important limitation is the lack of complete information about the treatment in the intensive care unit, including targeted temperature management, which is not sufficiently registered in the Danish National Patient Register. Nonetheless, during recent years, the intensive treatment, at least for patients with shockable rhythm, has been standardized and conformed to the European guidelines in the whole of Denmark.3, 12
Our study was conducted in Denmark, which limits the generalizability of the results considering variations in healthcare systems in different countries. Nevertheless, many other studies worldwide have previously documented inequalities in provision of acute cardiovascular procedures and higher cardiovascular mortality in patients with psychiatric disorders compared with the general population.7, 8, 9, 10, 30
Some of the prehospital OHCA factors such as initial heart rhythm and ROSC used in the subanalyses for CAG had a limited amount of missing data. However, the results based on complete case analysis did not differ substantially from the main results.
Finally, we used claimed prescriptions for antipsychotics and antidepressants before OHCA to identify patients with psychiatric disorders treated in the primary sector. The indication for psychotropic drugs was unknown, and, albeit rarely, conditions other than mental diseases are treated with these drugs.32 However, a sensitivity analysis excluding tricyclic antidepressants—the antidepressants mostly used for indications other than psychiatric disorders—yielded similar results.
Conclusions
Patients with psychiatric disorders who experience OHCA have half the probability of receiving CAG and a lower likelihood of having an ICD implanted during the index hospitalization for OHCA compared with patients without psychiatric disorders. Among patients undergoing a CAG, we did not detect differences in the rate of acute coronary revascularization between the 2 groups. Finally, compared with psychiatric healthy patients, patients with psychiatric disorders had a significantly lower 30‐day and 1‐year survival following OHCA, even among those who received acute invasive cardiovascular management.
Sources of Funding
This project has received funding from the European Union's Horizon 2020 Research and Innovation Program ESCAPE‐NET under grant agreement No. 733381. This institution does not have any commercial interest in the field of cardiac arrest.
Disclosures
Dr Gislason is supported by an unrestricted clinical research scholarship from the Novo Nordisk Foundation. Dr Kessing reports being expert witness for Sunovion. Dr Kragholm reports receiving research grant from the Laerdal Foundation, and lecture fees from Novartis Healthcare. Dr Torp‐Pedersen reports receiving grant support and honoraria from Bayer and grant support from Biotronik. Dr Polcwiartek reports receiving speaking fees from Lundbeck and research grants from the Danish Heart Foundation and the Eva and Henry Frænkel Memorial Foundation. The remaining authors have no disclosures to report.
Supporting information
Table S1. Diagnosis Codes Used to Define Patients With Psychiatric Disorders
Table S2. List of Psychotropic Drugs Used to Identify Patients With Psychiatric Disorders
Table S3. Diagnosis Codes Used to Define Cardiovascular Procedures
Table S4. Subgroups of Patients With Psychiatric Disorders
Table S5. Number of Patients With AMI as Cause of Cardiac Arrest in Our Cohort Stratified by Psychiatric Status
Table S6. Hazard Ratio With 95% Confidence Interval (CI) for Coronary Angiography, Coronary Revascularization, and ICD Implantation in Patients With and Without Psychiatric Disorders
Table S7. Patients Who Received Acute CAG and Still Alive at Day 2
Table S8. Patients Who Received Acute CAG and Still Alive at Day 2 Stratified by Severity of the Psychiatric Disorders
Figure S1. Flowchart for patients potentially eligible for ICD implantation during index hospitalization.
Figure S2. Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute and subacute coronary angiography in patients with and without psychiatric disorders among subsets of individuals who were identified by the presence of selected prehospital OHCA characteristics: (A) patients with witnessed OHCAs who received bystander CPR, (B) patients with OHCAs with shockable rhythm, (C) patients with OHCAs who achieved ROSC upon hospital arrival, and (D) patients with OHCAs with shockable rhythm who achieved ROSC upon hospital arrival.
Figure S3. Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute and subacute coronary angiography in patients with and without psychiatric disorders according to the Charlson score (Charlson=0, 3210 patients; Charlson=1, 1494; Charlson ≥2, 2584).
Figure S4. Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute and subacute coronary angiography in patients with and without psychiatric disorders according to the socioeconomic status (low tertile, 2429 patients; middle tertile, 2430 patients; high tertile, 2429 patients).
Figure S5. Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute and subacute coronary angiography in patients with and without psychiatric disorders stratified by the calendar year of cardiac arrest (2001–2007, 2385 patients; 2008–2015, 4903 patients).
Figure S6. Age‐standardized incidence rates and incidence rate ratio for acute and subacute coronary angiography in patients with and without psychiatric disorders stratified by sex (male, 5308 patients; female, 1980 patients).
Figure S7. Number of patients, events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute coronary angiography (≤1 day post‐OHCA) in patients with STEMI with and without psychiatric disorders.
Figure S8. Odds ratio for 30‐day and 1‐year survival in patients with psychiatric disorders stratified by severity of the disorder compared with patients without psychiatric disorders: (A) overall population and (B) patients who received acute CAG still alive at day 2.
Figure S9. (A) Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute and subacute CAG in patients with and without psychiatric disorders. Unit: number of CAGs per 100 person‐days in hospital. (B) Odds ratio for 30‐day and 1‐year survival in patients with any psychiatric disorders compared with patients without psychiatric disorders in overall population and among patients who received acute CAG still alive at day 2.
(J Am Heart Assoc. 2019;8:e012708 DOI: 10.1161/JAHA.119.012708.)
References
- 1. Yannopoulos D, Bartos JA, Aufderheide TP, Callaway CW, Deo R, Garcia S, Halperin HR, Kern KB, Kudenchuk PJ, Neumar RW, Raveendran G; American Heart Association Emergency Cardiovascular Care Committee . The evolving role of the cardiac catheterization laboratory in the management of patients with out‐of‐hospital cardiac arrest: a scientific statement from the American Heart Association. Circulation. 2019;139:e530–e552. [DOI] [PubMed] [Google Scholar]
- 2. Camuglia AC, Randhawa VK, Lavi S, Walters DL. Cardiac catheterization is associated with superior outcomes for survivors of out of hospital cardiac arrest: review and meta‐analysis. Resuscitation. 2014;85:1533–1540. [DOI] [PubMed] [Google Scholar]
- 3. Nolan JP, Soar J, Cariou A, Cronberg T, Moulaert VRM, Deakin CD, Bottiger BW, Friberg H, Sunde K, Sandroni C. European Resuscitation Council and European Society of Intensive Care Medicine guidelines for post‐resuscitation care 2015: section 5 of the European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation. 2015;95:202–222. [DOI] [PubMed] [Google Scholar]
- 4. Sweeting J, Duflou J, Semsarian C. Postmortem analysis of cardiovascular deaths in schizophrenia: a 10‐year review. Schizophr Res. 2013;150:398–403. [DOI] [PubMed] [Google Scholar]
- 5. Risgaard B, Waagstein K, Winkel BG, Jabbari R, Lynge TH, Glinge C, Albert C, Correll CU, Haunsø S, Fink‐Jensen A, Tfelt‐Hansen J. Sudden cardiac death in young adults with previous hospital‐based psychiatric inpatient and outpatient treatment: a nationwide cohort study from Denmark. J Clin Psychiatry. 2015;76:e1122–e1129. [DOI] [PubMed] [Google Scholar]
- 6. DE Hert M, Correll CU, Bobes J, Cetkovich‐Bakmas M, Cohen D, Asai I, Detraux J, Gautam S, Möller H‐J, Ndetei DM, Newcomer JW, Uwakwe R, Leucht S. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10:52–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schulman‐Marcus J, Goyal P, Swaminathan RV, Feldman DN, Wong S‐C, Singh HS, Minutello RM, Bergman G, Kim LK. Comparison of trends in incidence, revascularization, and in‐hospital mortality in ST‐elevation myocardial infarction in patients with versus without severe mental illness. Am J Cardiol. 2016;117:1405–1410. [DOI] [PubMed] [Google Scholar]
- 8. Druss BG, Bradford DW, Rosenheck RA, Radford MJ, Krumholz HM. Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA. 2000;283:506–511. [DOI] [PubMed] [Google Scholar]
- 9. De Hert M, Cohen D, Bobes J, Cetkovich‐Bakmas M, Leucht S, Ndetei DM, Newcomer JW, Uwakwe R, Asai I, Möller H‐J, Gautam S, Detraux J, Correll CU. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. 2011;10:138–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mitchell AJ, Lawrence D. Revascularisation and mortality rates following acute coronary syndromes in people with severe mental illness: comparative meta‐analysis. Br J Psychiatry. 2011;198:434–441. [DOI] [PubMed] [Google Scholar]
- 11. Henderson C, Noblett J, Parke H, Clement S, Caffrey A, Gale‐Grant O, Schulze B, Druss B, Thornicroft G. Mental health‐related stigma in health care and mental health‐care settings. Lancet Psychiatry. 2014;1:467–482. [DOI] [PubMed] [Google Scholar]
- 12. Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, Jans H, Hansen PA, Lang‐Jensen T, Olesen JB, Lindhardsen J, Fosbol EL, Nielsen SL, Gislason GH, Kober L, Torp‐Pedersen C. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out‐of‐hospital cardiac arrest. JAMA. 2013;310:1377–1384. [DOI] [PubMed] [Google Scholar]
- 13. Mathiasen R, Hansen BM, Forman JL, Kessing LV, Greisen G. The risk of psychiatric disorders in individuals born prematurely in Denmark from 1974 to 1996. Acta Paediatr. 2011;100:691–699. [DOI] [PubMed] [Google Scholar]
- 14. Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sørensen HT. The predictive value of ICD‐10 diagnostic coding used to assess Charlson comorbidity index conditions in the population‐based Danish National Registry of Patients. BMC Med Res Methodol. 2011;11:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Winther‐Jensen M, Hassager C, Lassen JF, Køber L, Torp‐Pedersen C, Hansen SM, Lippert F, Christensen EF, Kragholm K, Kjaergaard J. Association between socioeconomic factors and ICD implantation in a publicly financed health care system: a Danish nationwide study. Europace. 2018;20:1129–1137. [DOI] [PubMed] [Google Scholar]
- 16. Priori SG, Blomström‐Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, Elliott PM, Fitzsimons D, Hatala R, Hindricks G, Kirchhof P, Kjeldsen K, Kuck K‐H, Hernandez‐Madrid A, Nikolaou N, Norekvål TM, Spaulding C, Van Veldhuisen DJ; ESC Scientific Document Group . 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the Task Force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36:2793–2867. [DOI] [PubMed] [Google Scholar]
- 17. Standardize proportions and absolute risks to a given age distribution [Internet]. Available at: https://rdrr.io/github/tagteam/heaven/man/standardize.rate.html. Accessed July 12, 2019.
- 18. Rab T, Kern KB, Tamis‐Holland JE, Henry TD, McDaniel M, Dickert NW, Cigarroa JE, Keadey M, Ramee S; Interventional Council, American College of Cardiology . Cardiac arrest: a treatment algorithm for emergent invasive cardiac procedures in the resuscitated comatose patient. J Am Coll Cardiol. 2015;66:62–73. [DOI] [PubMed] [Google Scholar]
- 19. Hanuschak TA, Peng Y, Day A, Morrison LJ, Zhan CC, Brooks SC; Rescu Investigators . Patient and hospital factors predict use of coronary angiography in out‐of‐hospital cardiac arrest patients. Resuscitation. 2019;138:182–189. [DOI] [PubMed] [Google Scholar]
- 20. Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, Leary M, Meurer WJ, Peberdy MA, Thompson TM, Zimmerman JL. Part 8: post‐cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S465–S482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sundbøll J, Adelborg K, Munch T, Frøslev T, Sørensen HT, Bøtker HE, Schmidt M. Positive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: a validation study. BMJ Open. 2016;6:e012832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bartlett JW, Seaman SR, White IR, Carpenter JR; Alzheimer's Disease Neuroimaging Initiative* . Multiple imputation of covariates by fully conditional specification: accommodating the substantive model. Stat Methods Med Res. 2015;24:462–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. R Development Core Team . R: A Language and Environment for Statistical Computing. [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2008. Available at: http://www.R-project.org/. Accessed February 10, 2015. [Google Scholar]
- 24. Ifteni P, Correll CU, Burtea V, Kane JM, Manu P. Sudden unexpected death in schizophrenia: autopsy findings in psychiatric inpatients. Schizophr Res. 2014;155:72–76. [DOI] [PubMed] [Google Scholar]
- 25. Daumit GL, Pronovost PJ, Anthony CB, Guallar E, Steinwachs DM, Ford DE. Adverse events during medical and surgical hospitalizations for persons with schizophrenia. Arch Gen Psychiatry. 2006;63:267–272. [DOI] [PubMed] [Google Scholar]
- 26. Copeland LA, Zeber JE, Pugh MJ, Mortensen EM, Restrepo MI, Lawrence VA. Postoperative complications in the seriously mentally ill: a systematic review of the literature. Ann Surg. 2008;248:31–38. [DOI] [PubMed] [Google Scholar]
- 27. Gacouin A, Maamar A, Fillatre P, Sylvestre E, Dolan M, Le Tulzo Y, Tadié JM. Patients with preexisting psychiatric disorders admitted to ICU: a descriptive and retrospective cohort study. Ann Intensive Care. 2017;7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bodén R, Molin E, Jernberg T, Kieler H, Lindahl B, Sundström J. Higher mortality after myocardial infarction in patients with severe mental illness: a nationwide cohort study. J Intern Med. 2015;277:727–736. [DOI] [PubMed] [Google Scholar]
- 29. Eisendrath SJ, Shim JJ. Management of psychiatric problems in critically ill patients. Am J Med. 2006;119:22–29. [DOI] [PubMed] [Google Scholar]
- 30. Shen H‐N, Lu C‐L, Yang H‐H. Increased risks of acute organ dysfunction and mortality in intensive care unit patients with schizophrenia: a nationwide population‐based study. Psychosom Med. 2011;73:620–626. [DOI] [PubMed] [Google Scholar]
- 31. Verhaak PF. Somatic disease and psychological disorder. J Psychosom Res. 1997;42:261–273. [DOI] [PubMed] [Google Scholar]
- 32. Trifirò G, Tillati S, Spina E, Ferrajolo C, Alacqua M, Aguglia E, Rizzi L, Caputi AP, Cricelli C, Samani F. A nationwide prospective study on prescribing pattern of antidepressant drugs in Italian primary care. Eur J Clin Pharmacol. 2013;69:227–236. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Diagnosis Codes Used to Define Patients With Psychiatric Disorders
Table S2. List of Psychotropic Drugs Used to Identify Patients With Psychiatric Disorders
Table S3. Diagnosis Codes Used to Define Cardiovascular Procedures
Table S4. Subgroups of Patients With Psychiatric Disorders
Table S5. Number of Patients With AMI as Cause of Cardiac Arrest in Our Cohort Stratified by Psychiatric Status
Table S6. Hazard Ratio With 95% Confidence Interval (CI) for Coronary Angiography, Coronary Revascularization, and ICD Implantation in Patients With and Without Psychiatric Disorders
Table S7. Patients Who Received Acute CAG and Still Alive at Day 2
Table S8. Patients Who Received Acute CAG and Still Alive at Day 2 Stratified by Severity of the Psychiatric Disorders
Figure S1. Flowchart for patients potentially eligible for ICD implantation during index hospitalization.
Figure S2. Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute and subacute coronary angiography in patients with and without psychiatric disorders among subsets of individuals who were identified by the presence of selected prehospital OHCA characteristics: (A) patients with witnessed OHCAs who received bystander CPR, (B) patients with OHCAs with shockable rhythm, (C) patients with OHCAs who achieved ROSC upon hospital arrival, and (D) patients with OHCAs with shockable rhythm who achieved ROSC upon hospital arrival.
Figure S3. Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute and subacute coronary angiography in patients with and without psychiatric disorders according to the Charlson score (Charlson=0, 3210 patients; Charlson=1, 1494; Charlson ≥2, 2584).
Figure S4. Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute and subacute coronary angiography in patients with and without psychiatric disorders according to the socioeconomic status (low tertile, 2429 patients; middle tertile, 2430 patients; high tertile, 2429 patients).
Figure S5. Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute and subacute coronary angiography in patients with and without psychiatric disorders stratified by the calendar year of cardiac arrest (2001–2007, 2385 patients; 2008–2015, 4903 patients).
Figure S6. Age‐standardized incidence rates and incidence rate ratio for acute and subacute coronary angiography in patients with and without psychiatric disorders stratified by sex (male, 5308 patients; female, 1980 patients).
Figure S7. Number of patients, events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute coronary angiography (≤1 day post‐OHCA) in patients with STEMI with and without psychiatric disorders.
Figure S8. Odds ratio for 30‐day and 1‐year survival in patients with psychiatric disorders stratified by severity of the disorder compared with patients without psychiatric disorders: (A) overall population and (B) patients who received acute CAG still alive at day 2.
Figure S9. (A) Number of events, age‐ and sex‐standardized incidence rates, and incidence rate ratio for acute and subacute CAG in patients with and without psychiatric disorders. Unit: number of CAGs per 100 person‐days in hospital. (B) Odds ratio for 30‐day and 1‐year survival in patients with any psychiatric disorders compared with patients without psychiatric disorders in overall population and among patients who received acute CAG still alive at day 2.


