Abstract
Hodgkin lymphoma (HL) is a unique disease entity characterized by low number of neoplastic tumor cells surrounded by an inflammatory microenvironment composed of dysfunctional immune cells. Recent molecular and genetic studies have revealed that upregulation of the immune checkpoint pathway programmed death 1/programmed death 1-ligand (PD-1/PD-L1) is a key oncogenic driver in HL. Corroborating with these mechanistic studies, early phase clinical trials using the checkpoint inhibitors nivolumab and pembrolizumab in relapsed and/or refractory HL patients have demonstrated an impressive response rate, a promising durability of response, and a favorable side effect profile. Given their targeted mechanisms of action, safety, and activity, the checkpoint inhibitor nivolumab has been recently FDA approved as therapy for classical HL which is relapsed or has progressed after autologous hematopoietic stem cell transplantation (ASCT) and post-ASCT brentuximab vedotin (BV). In this article we review the scientific rationale, pre-clinical evidence, and most recent clinical data for checkpoint inhibitor therapy in relapsed HL.
Introduction
With over 9000 new cases diagnosed annually in the US, Hodgkin lymphoma (HL) relapsed Hodgkin lymphoma (HL) remains a significant clinical challenge (1). Classical HL is characterized by the presence of less than 1% multinucleated giant cells, the Hodgkin Reed Sternberg (HRS) cells, within a vast reactive milieu of immune cells including lymphocytes, histiocytes, eosinophils, macrophages, plasma cells and fibroblasts (2). This tumor micro-environment is supported by autocrine and/or paracrine production of inflammatory cytokines which promote tumor evasion from host growth control and immune-surveillance, and underlie the constitutional inflammatory symptoms associated with HL (3).
The initial treatment for HL patients is based on the stage and tumor burden at presentation. For patients with advanced disease, risk status is traditionally stratified based on the presence or absence of seven prognostic factors (IPS-7: male sex, age>=45, stage IV, hemoglobin<105 g/L, WBC >=15×109/L, lymphocyte count<0.6×109/L or <8% of differentia, and albumin < 40g/L) (4,5). More recently a streamlined IPS-3 has been proposed consisting of: age, stage, and hemoglobin level (6). Patients with early-stage, good risk disease are usually treated with either single modality cytotoxic chemotherapy, i.e. ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine), or combined-modality therapies including abbreviated courses of ABVD followed by involved-field radiation treatment. Patients with advanced-stage and/or poor risk disease usually receive a prolonged or more intense course of chemotherapy consisting of either ABVD or BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone), with the occasional inclusion of radiation treatment to sites of tumor bulk (7). For patients with relapsed or refractory disease, salvage chemotherapy followed by high-dose chemotherapy and autologous stem cell transplant (ASCT) remains the standard of care, and offers the highest chance for long term disease control and cure (7,8). Additional therapeutic options for patients who are ineligible for ASCT or those in whom ASCT has failed include brentuximab vedotin (BV), an antibody drug conjugate targeting CD30, palliative chemotherapy, targeted therapies such as mammalian toll-like receptor (mTOR) pathway and histone deacetylase inhibitors, allogeneic-SCT, or participation in a clinical trial (8). For patients who have relapsed after BV and allo-SCT the checkpoint inhibitor nivolumab is now FDA approved.
Two major challenges facing clinicians caring for HL patient are the minimization of long-term toxicities of therapy, and the improvement in salvage strategies for patients with relapsed and refractory disease. Longitudinal epidemiological studies have demonstrated a persistent risk of secondary malignancy for up to 40 years after curative treatment for HL (9,10). In addition, the risk of premature coronary artery disease in patients who receive radiation which encompasses the cardiac field increases 10 years post exposure (11). In terms of salvage therapy, despite the progress made in recent years, including the incorporation of BV and other novel targeted therapies such as mTOR pathway inhibitors, the cure rate for relapsed disease is still less than 50%. Allo-SCT can potentially provide a cure to a small subset of relapsed patients but is associated with considerable transplant-associated morbidity and mortality (12).
Under normal physiological conditions, the host utilizes a plethora of immunologic inhibitory pathways including the checkpoint blockade to maintain self-tolerance and to modulate the duration and amplitude of the physiological immune response (13). In solid tumors, the concept of checkpoint inhibitor based therapy derives from the understanding that most solid tumors have a myriad of genetic and epigenetic alterations which provide a diverse set of neoantigens used by the immune system to distinguish tumor cells from normal cells; and they use this mechanism to evade host immune surveillance (14).
Antibodies against both the ligand or the receptor in immune checkpoint pathways have been developed, and are proving to be promising therapeutics in both solid tumors and HL. Cytotoxic T-lymphocyte-associated antigen 4 (CTLA4) antibodies were the first of this class to achieve FDA approval in malignant melanoma based a survival benefit of 30% over 3 years reported in phase III studies (15). More recently, checkpoint inhibitor antibodies against the protein programmed cell death protein 1 (PD-1) have been approved in several solid tumors including melanoma and non-small cell lung cancer (15). To date in hematological malignancies, development of these therapies has been slower with the exception of HL (16). This may be due to lower mutational burden in hematologic malignancies in particular HL, resulting in a lower level of neoantigens (17). However, HL stands out among all lymphomas with its high responsiveness to PD-1 blockade (>70% ORR) and significant clinical benefit in patient with relapsed and refractory HL (18-20).
Targeting Immune Systems in HL Pathogenesis
In many HL patients, deficiencies of host immune functions such as T-cell mediated viral clearance has been noted, sometimes even predating a diagnosis of HL (21). Interestingly, this immune deficiency may persist in some patients even years after successful treatment of HL (22). Supporting this notion, it has been long appreciated that patients with with HIV infection or autoimmune disease have an increased incidence and prevalence of both HL and non-Hodgkin lymphoma (NHL) (23).
In 2008, Yamamoto et al. showed for the first time that HRS cell lines and primary tumor sample overexpressed ligand for PD-1 (PD-L1) (24). Most importantly, PD-1 itself was markedly over-expressed in the tumor-infiltrating CD4 and CD8 T-cells of 3 HL patients (24). Artificial blocking of the PD-1 pathway restored gamma interferon production. This data suggested that activation of PD-1 pathway in T cells induces ‘T-cell exhaustion’, a chronic state of effector T-cell dysfunction through expression of inhibitory receptors and decreased activating cytokine production. The overexpression of PD-L1 on HRS cells and PD-1 on tumor-infiltrating lymphocytes (TiLs) forms a potent inhibitory signal in maintaining the immunosuppressive HL microenvironment, and allowing HRS evasion of immune surveillance (24). These findings were confirmed in a large set of primary HL tumor samples where HRS cells were found to express high level of PD-L1 and PD-L2 as compared to other aggressive NHLs (25). A subsequent immunohistochemistry study in primary HL tumor specimen confirmed significantly higher level of PD-L1 expression in classical HL compared to primary mediastinal B-cell lymphomas or diffuse large B-cell lymphoma (26). Finally, Muenst et al. used tissue microarray technology to evaluate 189 cases of classical HL and found that an increased number of PD-1+ TiLs was a stage-independent negative prognostic factor for overall survival (OS) (27), supporting the role of PD1-PDL1 pathway activation in the pathogenesis of HL
On the molecular level, several mechanisms have been proposed to account for the upregulation of the PD-1 pathway in HL. Genomic based approaches combining high-resolution copy number data with transcriptional profiles have identified selective amplification of 9p24.1 region in HRS cells, a region containing the PD-L1 gene (28). In addition, the Jak2 locus is also amplified leading to Jak2 protein overexpression and subsequent transcriptional activation of PD-L1 (28). Most recently, the prognostic significance of PD-L1 and PD-L2 genetic alterations has been demonstrated using FISH analysis of 108 primary HL patient samples; 97% of HL patients had concordant alterations of the PD-L1 and PD-L2 loci on 9p24.1, and this amplification was associated with more advanced stage of disease and worsened progression free survival (PFS) (29).
Several groups subsequently found additional mechanisms contributing to the upregulation of PD-L1 and PD-L2. Steidl et al. utilized whole-transcriptome pared-end sequencing in HL cell lines and identified a highly expressed chromosomal fusion gene involving CIITA MHC-II transcriptional activator, leading to downregulation of surface HLA class II expression and overexpression of PD-L1 and PD-L2 (30). Constitutive activation of the AP-1/JunB transcriptional complex through an enhancer element in the PD-L1 gene in HRS cells has also been described (31). In addition, Epstein Barr Virus (EBV) infection results in latent membrane protein 1-mediated (LMP-1), JAK/STAT-dependent promoter and AP-1-associated, increased expression of PD-L1 gene and protein (31). However, in 87 cases of primary HL samples no correlation between EBER expression and PD-1/PD-L1 expression was found (32). By overexpressing PD-L1 and PD-L2 on their surface, HRS cells are able to shut down the immune response thus evading immune surveillance. Figure 1 summarizes the mechanisms of upregulating PD-1/PD-L1 pathway in the HL microenvironment.
Figure 1.
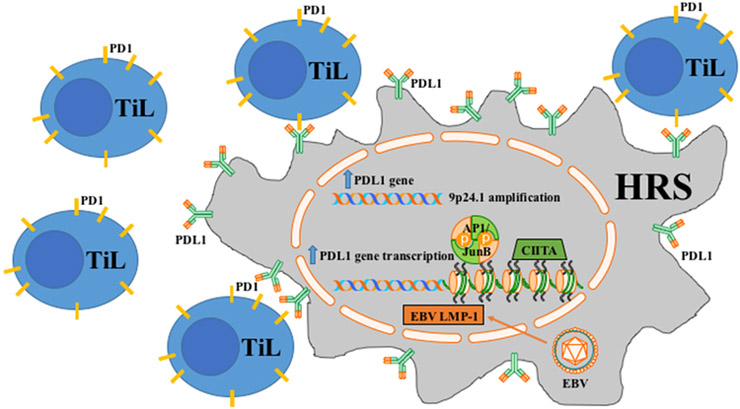
Mechanisms of upregulating PD-1/PD-L1 pathway in HL.
HRS: Hodgkin Reed Sternberg cells
TiL: Tumor infiltrating lymphocytes
PD1: Program death 1
PDL1: Program death 1 ligand
CIITA: CIITA MHCII transcription factor
EBV: Epstein Barr virus
LMP-1: Latent membrane protein 1
Clinical studies of checkpoint inhibition in HL
Anti-CTLA4 therapy
The safety and preliminary efficacy of the combination of BV and ipilimumab, an FDA approved anti-CTLA4 antibody, in a phase I study of 23 relapsed and refractory HL patients was presented at ASH in 2015 (33). Ipilimumab was dosed at 1 mg or 3 mg/kg following the typical induction-maintenance regimen and BV was dosed at 1.8 mg/kg every three weeks. The regimen was well tolerated with only manageable immune-related adverse events and no DLTs. Among 18 evaluable patients reported, the ORR was 72% and the CR rate was 50%. This study demonstrates that the combination of BV and the checkpoint inhibitor ipilimumab appears safe, has promising activity in relapsed HL, and suggests a proof of concept for the combination of checkpoint inhibitors and antibody drug conjugate or cytotoxic therapy platforms.
Anti-PD1 therapy
The landmark Checkmate-039 study of the checkpoint inhibitor nivolumab in relapsed and refractory HL was published this past year. In a phase I study of 23 relapsed and refractory heavily pretreated (78% treated with BV, ASCT, or both) HL patients received the anti-PD1 monoclonal antibody nivolumab at a starting dose of 1 mg/kg up to 3 mg/kg for up to 2 years. An 87% ORR was observed with a 20% CR rate (34). The drug was well tolerated without significant DLTs. Immunohistochemistry confirmed the high level of PD-L1 expression in HRS cells in this study. As updated at ASH in 2015, after an extended follow up of 101 weeks, the median duration of response and median PFS have yet to be reached, showing promising remission durability in this traditionally difficult to treat patient population (35). The OS was 91% at 1 year and was 83% at 1.5 years. Most importantly, this follow-up analysis included long term follow up data for the cohort of patients who received nivolumab until confirmed CR, or for up to 2 years if they had a PR or stable disease (SD), and then were followed for one year after treatment discontinuation. Among the 20 responding patients at the time of data cut-off, 3 patients remained on nivolumab treatment with ongoing responses, 13 came off treatment without progressive disease (PD); of these, 5 patients underwent allo-SCT, 4 patients developed PD following initial response, and 1 patient was retreated post-progression and achieved a second complete response (35). Based on these results, FDA has approved nivolumab for the treatment of relapsed/refractory classical HL after ASCT and BV.
A second clinical trial using a different anti-PD-1 monoclonal antibody pembrolizumab (MK-3475) has also been reported and updated showing similar safety and efficacy signals (Keynote-013) (36). Thirty-one HL patients who had failed BV (100%) and ASCT (71%) received 10 mg/kg of pembrolizumab every 2 weeks for up to 2 years. At the time of the report at the 2015 ASH meeting, the overall response rate was 65% with CR rate of 16%. For best responses, 90% of patients had a reduction of ≥50% in their target lesions compared with baseline. Among responders, 80% of responses occurred by week 12. Moreover, responses were durable for 71% of patients for at least 24 weeks. The PFS at 24 weeks was 69%. Only one immune related adverse event was noted and three patients went on to receive allogeneic-SCT as consolidation. Immunohistochemistry of pretreatment tumor tissue showed that most were positive for PD-L1/PD-L2 expression (36). Table 1 summarizes clinical efficacy results of these checkpoint inhibitors. Pembrolizumab has been granted breakthrough designation by the FDA.
Table 1.
Clinical efficacy of checkpoint inhibitors in relapsed/refractory HL
| Target | Drug | Trial | N | ORR (%) |
CR (%) |
SD (%) |
DOR | PFS | OS |
|---|---|---|---|---|---|---|---|---|---|
| CTLA4 | Ipilimumab (34, 35) | Phase I | 21 | 14 | 10 | 0 | NR | NR | NR |
| Ipilimumab + BV (36) | Phase I | 23 | 72 | 50 | 3 | NR | 1.02 yr | Not reached | |
| PD-1 | Nivolumab (37, 38) | Phase I | 23 | 87 | 22 | 13 | Not reached | Not reached | 91% at 1 year |
| Pembrolizumab (39) | Phase I | 31 | 65 | 16 | 23 | 71% >= 24 wks | 69% at 24 wks | NR |
Abbreviations:
N: Number of patients
ORR: Overall response rate
CR: Complete response rate
SD: Stable disease rate
DOR: Duration of response
PFS: Progression free survival
OS: Overall survival
NR: Not reported
Based on theFDA approval of Nivolumab , the 2016 v1 NCCN guidelines outline that nivolumab be considered an option in cHL patients relapsed or progressed through ASCT and BV maintenance (48). The use of checkpoint inhibitors prior to ASCT and / or BV, in combination with other chemotherapy or targeted agents,, or in earlier lines of therapy, should ideally be investigated in the context of a clinical trial.
Checkpoint inhibition in the setting of allogeneic-SCT
The FDA approved anti-CTLA4 antibody, ipilimumab, has been investigated in a phase I study of 29 patients with advanced hematological malignancies relapsed after allogeneic-SCT, which included 14 patients with HL (37). Given the concern for worsening chronic graft versus host disease (GVHD), a wide dose rage of 0.1 to 3.0 mg/kg ipilimumab was used. Dose-limiting toxicity (DLT) was not reached and no worsening GVHD or graft rejection occurred. Complete remission (CR) was achieved in two patients with HL and partial remission (PR) in a patient with refractory mantle cell lymphoma. Ipilimumab was well tolerated and organ-specific immune adverse events were seen in four patients (grade 3 arthritis, grade 2 hyperthyroidism, recurrent grade 4 pneumonitis).
The preliminary results of the expansion cohort of this study were reported at the American Society of Hematology Meeting (ASH) in 2015. Repeated dosing at 3 mg and 10 mg/kg were used according to an induction and maintenance schedule (38). Twenty-eight patients with relapsed hematological malignancies after allogeneic-SCT were included, including 7 with HL. In 21 evaluable patients, the overall response rate (ORR) was 33%, including 5 out of 12 acute myelogenous leukemia (AML) patients who achieved CR, and only 1 patient with HL who achieved a PR. Five GVHD related DLT were reported along with four immune-related events. These studies suggested that anti-CTLA therapy is reasonably safe in this setting for patients post AlloSCT without evidence of GVHD, particularly at a low dose. The surprising high response rate for the AML cohort also supports the notion that immune checkpoint inhibition may have some role in augmenting the graft versus tumor effect.
The safety and the optimal timing of checkpoint inhibitor therapy prior to or following allogeneic-SCT (allo-SCT) remains unknown. The desired graft versus tumor effect induced by allo-SCT induces generalized immune stimulation and inhibition of normal checkpoint function (39). Tumor relapse after allo-SCT invariably involves escape from immune surveillance by mechanisms such as increased PD-1/PD-L1 expression on CD8(+) T cells (40). Checkpoint inhibition has a theoretical risk of worsening GVHD. In a murine model of acute GVHD, both PD-L1 and PD-L2 expression were increased at the baseline, and blockade of PD-1/PD-L1 signaling exacerbated acute GVHD and enhanced lethality (41). Moreover, in PD-L1-deficient hosts, donor T-cells have increased aerobic glycolysis and oxidative phosphorylation leading to increased proliferation and activation, and this enhanced metabolic activity may contribute to acute GVHD (41). Similar findings have also been demonstrated in a murine model of chronic GVHD (42).
The limited clinical data suggests careful investigation of this question is warranted. The anti-CTLA4 antibody ipilumumab appears safe to use after allo-SCT at low to intermediate doses (1 mg/kg and 3 mg/kg), however, at the highest dose (10 mg/kg) worsening of chronic GVHD was seen (33). The safety and efficacy of nivolumab treatment for relapsed HL after allo-SCT was presented at ASH 2015 in a single institution, retrospective analysis of 12 patients. Patients were without history of grade 3–4 acute or chronic GVHD, and were required to be off immunosuppression for more than 4 weeks. Nivolumab was given at 3 mg/kg every two weeks and the median number of cycles was four. The ORR was 87.5% with three CR and four PR. Two grade 3–4 acute GVHD developed necessitating dose delay or dose reduction (43). Similarly, pembrolizumab was used successfully in two HL patients relapsed after allo-SCT who were maintained on low dose prednisone. Both patients responded without evidence of acute GVHD (44). However, case reports of severe and fatal GVHD have also been described in patients receiving anti-PD-1 therapy after allo-SCT for HL (45,46).
The safety of allo-SCT following checkpoint inhibitor therapy remains unknown, however there is at least a theoretical risk of acute GVHD in this setting due to the long half-live of the antibody. Not yet reported in publications but described in the nivolumab label, significant complications, including fatal events, have occurred in patients who received allo-SCT after nivolumab at varying intervals (47). In total, data for 17 patients have been described; 15 underwent reduced-intensity conditioning and 2 underwent myeloablative conditioning. The median age at allo-SCT was 33 and a median of 9 doses of nivolumab were administered (range: 4 to 16). Six of 17 patients (35%) died from complications of allo-SCT after nivolumab. Five deaths occurred in the setting of severe or refractory GVHD. Grade 3 or higher acute GVHD was reported in 5/17 patients (29%). Hyperacute GVHD, a steroid-requiring febrile syndrome, encephalitis, and hepatic veno-occlusive disease, have also been reported (47).
Checkpoint inhibition and the future of HL therapy
The reduction of long term toxicity of treatment for low risk HL patients and the improvement in efficacy for treating high risk patients remains a high priority for HL clinical research. The high response rate, favorable side effect profile, and potential durability of checkpoint inhibitor therapy suggests it has great promise as a cornerstone of therapy for relapsed and refractory HL, both as a single agent and potentially in novel combination treatment platforms with antibody-drug conjugates or other cytotoxic chemotherapy regimens. A number of clinical trials are underway to test these hypotheses, with the goal of identifying rational combinations which can increase the CR rate and durable response rate for these patients. In addition, given the persistent risk of long term therapy related toxicity, especially for high risk HL patients treated with extensive alkylator based therapy, the activity of checkpoint inhibitors in the relapsed setting suggests a potential role for these agents as a component of upfront therapy.
References
- 1.Ansell SM. Hodgkin lymphoma: 2016 update on diagnosis, risk-stratification, and management. Am J Hematol. 2016;91:435–42. [DOI] [PubMed] [Google Scholar]
- 2.Haluska FG, Brufsky AM, Canellos GP. The cellular biology of the Reed-Sternberg cell. Blood 1994;84:1005–19. [PubMed] [Google Scholar]
- 3.Steidl C, Connors JM, Gascoyne RD. Molecular pathogenesis of Hodgkin’s lymphoma: increasing evidence of the importance of the microenvironment. J Clin Oncol 2011; 29:1812–26. [DOI] [PubMed] [Google Scholar]
- 4.Hasenclever D, Diehl V. A prognostic score for advanced Hodgkin’s disease. International Prognostic Factors Project on Advanced Hodgkin’s Disease. N Engl J Med 1998;339:1506–14. [DOI] [PubMed] [Google Scholar]
- 5.Moccia AA, Donaldson J, Chhanabhai M, Hoskins PJ, Klasa RJ, Savage KJ, Shenkier TN, Slack GW, Skinnider B, Gascoyne RD, Connors JM, Sehn LH. International Prognostic Sire in advanced Hodgkin’s lymphoma: altered utility in the modern era. J Clin Oncol 2012;30:3383–3388. [DOI] [PubMed] [Google Scholar]
- 6.Diefenbach CS, Li H, Hong F, Gordon LI, Fisher RI, Bartlett NL, Crump M, Gascoyne RD, Wagner H Jr, Stiff PJ, Cheson BD, Stewart DA, Kahl BS, Friedberg JW, Blum KA, Habermann TM, Tuscano JM, Hoppe RT, Horning SJ, Advani RH. Evaluation of the international prognostic score (IPS-7) and a simpler prognostic score (IPS-3) for advanced Hodgkin lymphoma in the modern era. Br J Haematol. 2015;171:530–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson P, McKenzie H. How I treat advanced classic Hodgkin’s lymphoma. Blood 2015;125:1717–23. [DOI] [PubMed] [Google Scholar]
- 8.Montanari F, Diefenbach C. Relapsed Hodgkin’s lymphoma: management startegies. Curr Hematol Malig Rep. 2014;9:284–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schaapveld M, Aleman BM, van Eggermond AM, Janus CP, Krol AD, van der Maazen RW, Roesink J, Raemaekers JM, de Boer JP, Zijlstra JM, van Imhoff GW, Petersen EJ, Poortmans PM, Beijert M, Lybeert ML, Mulder I, Visser O, Louwman MW, Krul IM, Lugtenburg PJ, van Leeuwen FE. Second cancer risk up to 40 years after treatment for Hodgkin’s lymphoma. N Engl J Med 2015;373:2499–511. [DOI] [PubMed] [Google Scholar]
- 10.Swerdlow AJ, Barber JA, Hudson GV, Cunningham D, Gupta RK, Hancock BW, Horwich A, Lister TA, Linch DC. Risk of second malignancy after Hodgkin’s disease in a collaborative British cohort: the relation to age at treatment. J Clin Oncol. 2000;18:498–509. [DOI] [PubMed] [Google Scholar]
- 11.Heidenreich PA, Schnittger I, Strauss HW, Vagelos RH, Lee BK, Mariscal CS, Tate DJ, Horning SJ, Hoppe RT, Hancock SL. Screening for coronary artery disease after mediastinal irradiation for Hodgkin’s disease. J Clin Oncol. 2007;25:43–9. [DOI] [PubMed] [Google Scholar]
- 12.Sureda A, Domenech E, Schmitz N, Dreger P; Lymphoma Working Party of the European Group for Stem Cell Transplantation. The role of allogeneic stem cell transplantation in Hodgkin’s lymphoma. Curr Treat Options Oncol. 2014;15:238–47. [DOI] [PubMed] [Google Scholar]
- 13.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 2012;12:252–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell 2011;144:646–74. [DOI] [PubMed] [Google Scholar]
- 15.Postow MA, Callahan MK, Wolchok JD. Immune checkpoint blockade in cancer therapy. J Clin Oncol. 2015;33:1974–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Armand P Immune checkpoint blockade in hematologic malignancies. Blood 2015;125:3393–40. [DOI] [PubMed] [Google Scholar]
- 17.Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SA, Behjati S, Biankin AV, Bignell GR, Bolli N, Borg A, Børresen-Dale AL, Boyault S, Burkhardt B, Butler AP, Caldas C, Davies HR, Desmedt C, Eils R, Eyfjörd JE, Foekens JA, Greaves M, Hosoda F, Hutter B, Ilicic T, Imbeaud S, Imielinski M, Jäger N, Jones DT, Jones D, Knappskog S, Kool M, Lakhani SR, López-Otín C, Martin S, Munshi NC, Nakamura H, Northcott PA, Pajic M, Papaemmanuil E, Paradiso A, Pearson JV, Puente XS, Raine K, Ramakrishna M, Richardson AL, Richter J, Rosenstiel P, Schlesner M, Schumacher TN, Span PN, Teague JW, Totoki Y, Tutt AN, Valdés-Mas R, van Buuren MM, van ‘t Veer L, Vincent-Salomon A, Waddell N, Yates LR; Australian Pancreatic Cancer Genome Initiative; ICGC Breast Cancer Consortium; ICGC MMML-Seq Consortium; ICGC PedBrain, Zucman-Rossi J, Futreal PA, McDermott U, Lichter P, Meyerson M, Grimmond SM, Siebert R, Campo E, Shibata T, Pfister SM, Campbell PJ, Stratton MR. Signatures of mutational processes in human cancer. Nature 2013;500:415–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Novakovic BJ. Checkpoint inhibitors in Hodgkin’s lymphoma. Eur J Haematol. 2016;96:335–43. [DOI] [PubMed] [Google Scholar]
- 19.Villasboas JC, Ansell S. Checkpoint inhibition: program cell death 1 and program cell death 1 ligand inhibitors in Hodgkin lymphoma. Cancer J. 2016;22:17–22. [DOI] [PubMed] [Google Scholar]
- 20.Hawkes EA, Grigg A, Chong G. Program cell death-1 inhibition in lymphoma. Lancet Oncol. 2015;16:e234–45. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy-Nasser AA, Hanley P, Bollard CM. Hodgkin’s disease and the role of immune system. Pediatr Hematol Oncol. 2011;28:176–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Björkholm M, Holm G, Mellstedt H. Persisting lymphocyte deficiencies during remission in Hodgkin’s disease. Clin Exp Immunol. 1977;28:389–93. [PMC free article] [PubMed] [Google Scholar]
- 23.Robert NJ, Schneiderman H. Hodgkin’s disease and the acquired immunodeficiency syndrome. Ann Intern Med. 1984;101:142–3. [DOI] [PubMed] [Google Scholar]
- 24.Yamamoto R, Nishikori M, Kitawaki T, Sakai T, Hishizawa M, Tashima M, Kondo T, Ohmori K, Kurata M, Hayashi T, Uchiyama T. PD-1-PD-1 ligand interaction contributes to immunosuppressive microenvironment of Hodgkin lymphoma. Blood 2008;111:3220–4. [DOI] [PubMed] [Google Scholar]
- 25.Chen BJ, Chapuy B, Ouyang J, Sun HH, Roemer MG, Xu ML, Yu H, Fletcher CD, Freeman GJ, Shipp MA, Rodig SJ. PD-L1 expression is characteristic of a subset of aggressive B-cell lymphomas and virus-associated malignancies. Clin Cancer Res. 2013;19:3462–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menter T, Bodmer-Haecki A, Dirnhofer S, and Tzankov A. Evaluation of the diagnostic and prognostic value of PDL1 expression in Hodgkin and B-cell lymphomas. Human Pathology 2016;54:17–24. [DOI] [PubMed] [Google Scholar]
- 27.Muenst S, Hoeller S, Dirnhofer S, Tzankov A. Increased programmed death-1+ tumor-infiltrating lymphocytes in classical Hodgkin lymphoma substantiate reduced overall survival. Hum Pathol. 2009;40:1715–22. [DOI] [PubMed] [Google Scholar]
- 28.Green MR, Monti S, Rodig SJ, Juszczynski P, Currie T, O’Donnell E, Chapuy B, Takeyama K, Neuberg D, Golub TR, Kutok JL, Shipp MA. Integrative analysis reveals selective 9p24.1 amplification, increased PD-L1 ligand expression, and further induction via JAK2 in nodular sclerosing Hodgkin lymphoma and primary mediastinal large B-cell lymphoma. Blood 2010;116:3268–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roemer MG, Advani RH, Ligon AH, Natkunam Y, Redd RA, Homer H, Connelly CF, Sun HH, Daadi SE, Freeman GJ, Armand P, Chapuy B, de Jong D, Hoppe RT, Neuberg DS, Rodig SJ, Shipp MA. PD-L1 and PD-L2 genetic alterations define classical Hodgkin’s lymphoma and predict outcome. J Clin Oncol. 2016. April 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steidl C, Shah SP, Woolcock BW, Rui L, Kawahara M, Farinha P, Johnson NA, Zhao Y, Telenius A, Neriah SB, McPherson A, Meissner B, Okoye UC, Diepstra A, van den Berg A, Sun M, Leung G, Jones SJ, Connors JM, Huntsman DG, Savage KJ, Rimsza LM, Horsman DE, Staudt LM, Steidl U, Marra MA, Gascoyne RD. MHC class II activator CIITA is a recurrent gene fusion partner in lymphoid cancers. Nature 2011;471:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Green MR, Rodig S, Juszczynski P, Ouyang J, Sinha P, O’Donnell E, Neuberg D, Shipp MA. Constitute AP-1 activity and EBV infection induce PD-L1 in Hodgkin lymphomas and posttransplant lymphoproliferative disorders: implications for targeted therapy. Clin Cancer Res. 2012;18:1611–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paydas S, Bağır E, Seydaoglu G, Ercolak V, Ergin M. Programmed death-1 (PD-1), programmed death-ligand 1 (PD-L1), and EBV-encoded RNA (EBER) expression in Hodgkin lymphoma. Ann Hematolol. 2015;94:1545–52. [DOI] [PubMed] [Google Scholar]
- 33.Diefenbach CS, Hong F, Cohen JB, Robertson MJ, Ambinder RF, Fenske TS, Advani RH, Kahl BS, Ansell S. Preliminary safety and efficacy of the combination of brentuximab vedotin and ipilimumab in relapsed/refractory Hodgkin’s lymphoma: a trial of the ECOG-ACRIN Cancer Research Group (E4412). Blood 2015;126:585. [Google Scholar]
- 34.Ansell SM, Lesokhin AM, Borrello I, Halwani A, Scott EC, Gutierrez M, Schuster SJ, Millenson MM, Cattry D, Freeman GJ, Rodig SJ, Chapuy B, Ligon AH, Zhu L, Grosso JF, Kim SY, Timmerman JM, Shipp MA, Armand P. PD-1 blockade with nivoluman in relapsed or refractory Hodgkin’s lymphoma. N Engl J Med. 2015;372:311–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ansell S, Armand P, Timmerman JM, Shipp MA, Garelik MBB, Zhu L, Lesokhin AM. Nivolumab in patients (pts) with relapsed or refractory classical Hodgkin lymphoma (R/R cHL): clinical outcomes from extended follow-up of a phase I study (CA209–039). Blood 2015,126:583. [Google Scholar]
- 36.Armand P, Shipp MA, Ribrag V, Michot JM, Zinzani PL, Gutierrez M, Snyder E, Ricart AD, Balakumaran A, Moskowitz CH. PD-1 blockade with pembrolizumab in patients with classical Hodgkin lymphoma after brentuximab vedotin failure: safety, efficacy, and biomarker assessment. Blood 2015;126:584. [Google Scholar]
- 37.Bashey A, Medina B, Corringham S, Pasek M, Carrier E, Vrooman L, Lowy I, Solomon SR, Morris LE, Holland HK, Mason JR, Alyea EP, Soiffer RJ, Ball ED. CTLA4 blockade with ipilimumab to treat relapse of malignancy after allo-geneic hematopoietic cell transplantation. Blood 2009;113;1581–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Davids MS, Kim HT, Costello CL, McSweeney PA, Liguori R, Lukez A, Avigan D, Chen Y, LeBoeuf N, Ho VT, Cutler CS, Koreth J, Alyea EP, Antin JH, Ritz J, Armand P, Ball ED, Bashey A, Soiffer RJ. A multicenter phase I/Ib study of ipilimumab for relapsed hematologic malignancies after allogeneic hematopoietic stem cell transplantation. Blood 2015;126:860. [Google Scholar]
- 39.Mosaad YM. Immunology of hematopoietic stem cell transplant. Immunol Invest. 2014;43:858–87. [DOI] [PubMed] [Google Scholar]
- 40.Norde WJ, Maas F, Hobo W, Korman A, Quigley M, Kester MG, Hebeda K, Falkenburg JH, Schaap N, de Witte TM, van der Voort R, Dolstra H. PD-1/PD-L1 interactions contribute to functional T-cell impairment in patients who relapse with cancer after allogeneic stem cell transplantation. Cancer Res. 2011;71:5111–22. [DOI] [PubMed] [Google Scholar]
- 41.Saha A, Aoyama K, Taylor PA, Koehn BH, Veenstra RG, Panoskaltsis-Mortari A, Munn DH, Murphy WJ, Azuma M, Yagita H, Fife BT, Sayegh MH, Najafian N, Socie G, Ahmed R, Freeman GJ, Sharpe AH, Blazar BR. Host programmed death ligand 1 is dominant over programmed death ligand 2 expression in regulating graft-versus-host disease lethality. Blood 2013;122:3602–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fujiwara H, Maeda Y, Kobayashi K, Nishimori H, Matsuoka K, Fujii N, Kondo E, Tanaka T, Chen L, Azuma M, Yagita H, Tanimoto M. Programmed death-1 pathway in host tissues ameliorates Th17/Th1-mediated experimental chronic graft-versus-host disease. J Immunol. 2014;193:2565–73. [DOI] [PubMed] [Google Scholar]
- 43.Herbaux C, Gauthier J, Brice P, Fornecker L, Bouabdallah K, Manson G, Ghesquières H, Thiebaut-Bertrand A, Demarquette H, Boyle E, Ysebaert L, Houot R, Yakoub-Agha I, Morschhauser F. Nivolumab is effective and reasonably safe in relapsed or refractory Hodgkin’s lymphoma after allogeneic hematopoietic cell transplantation: s study from the Lysa and SFGM-TC. Blood 2015;126:3979. [Google Scholar]
- 44.Villasboas JC, Ansell SM, Witzig TE. Targeting the PD-1 pathway in patients with relapsed classic Hodgkin lymphoma following allogeneic stem cell transplant is safe and effective. Oncotarget 2016. February 3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mori S, Ahmed W, Patel RD, Dohrer AL. Steroid refractory acute liver GvHD in a Hodgkin’s patient after allogeneic stem transplant cell transplantation following treatment with anti PD-1 antibody, nivolumab, for relapsed disease. Biol Blood Marrow Transplant 22: S392–S393. [Google Scholar]
- 46.Singh AK, Porrata F, Aljitawi O, Lin T, Shune L, Ganguly S, McGuirk JP, Adhyankar S. Fatal GvHD induced by PD-1 inhibitor prebrolizuman in a patient with Hodgkin’s lymphoma. Bone Marrow Transplantation. 2016,1–3. [DOI] [PubMed] [Google Scholar]
- 47.Opdivo full prescribing information (accessed May 26th, 2016): http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/125554s019lbl.pdf
- 48.2016 v1. NCCN Guideline on Hodgkin’s Lymphoma.


