Abstract
Background: This study reviews long-term outcomes of partial wrist denervation focusing on need for and time to revision procedure. Methods: A retrospective study was conducted of all patients undergoing partial wrist denervation between 1994 and 2014. At average latest follow-up of 6.75 years (range, 1-21 years), clinical and radiographic data and need for revision surgery were recorded. Results: There were 100 wrists in 89 patients (61 male, 28 female) with average age at surgery of 54 years (range, 26-80). Principal diagnoses were arthritis (58%), inflammatory (19%), and posttraumatic arthritis (7%). Average flexion-extension arc was 83% and grip strength 75% of unaffected extremity. Average Mayo Wrist Scores improved from 48 preoperatively to 77 postoperatively. Sixty-nine percent of patients did not undergo other procedures during the time interval studied. Thirty-one percent underwent revision at an average of 26 months following denervation (range, 2-165). Conclusions: Partial wrist denervation is a motion-preserving procedure for patients with refractory wrist pain with 69% in this series requiring no further procedures. The remaining 31% experienced average symptom relief for 2 years prior to ultimately undergoing revision operation.
Keywords: partial denervation, wrist pain, arthritis, outcomes, reoperation
Introduction
Chronic wrist pain can significantly impact patients’ functional and emotional well-being.3 Despite nonoperative treatments, patients may continue to experience pain and limitation and may consider surgical intervention which, based on the primary pathology, can range from reconstruction to salvage procedures such as wrist arthrodesis.
Wrist denervation is a procedure which may be a viable alternative for patients with chronic wrist pain related to articular degeneration or chronic instability who wish to retain motion. The principle behind denervation is that removal of the sensory innervation to the wrist joint provides relief of pain, while maintaining function and mobility of the hand and wrist.7 After denervation, patients may have progression of degenerative changes. It is unclear if denervation affects the natural history of the degenerative process or if this alters whether or not patients elect to undergo further surgery.
Partial wrist denervation selectively eliminates the anterior interosseous nerves (AIN) and posterior interosseous nerves (PIN), which innervate the central two-thirds of the anterior and posterior carpal joint capsule.2 The nerves pass within 2 mm of each other just proximal to the distal radioulnar joint capsule in a relatively accessible anatomic location for resection.2 Weinstein and Berger published a series of 20 wrists undergoing partial denervation followed for an average of 2.5 years.19 Their series found an 85% satisfaction rate with no complications noted.19 The present study evaluated a larger series of patients over a longer follow-up period to determine whether similar outcomes were noted.
The purpose of the article is to evaluate the long-term clinical outcomes of patients treated with partial wrist denervation for wrist pain with specific aims to determine the percent of patients who ultimately undergo revision or salvage procedure and the average time to repeat operation.
Materials and Methods
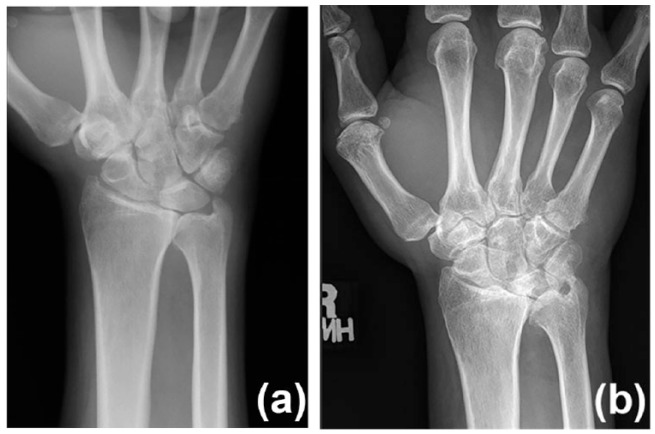
An institutional review board–approved retrospective analysis of all patients treated with partial wrist denervation (AIN and PIN neurectomy) between 1994 and 2014 by 2 fellowship-trained professors of hand surgery (R.A.B. and S.K.) was undertaken. The inclusion criteria included patients over the age of 18 years who were treated with partial denervation and in whom there was greater than 12 months of follow-up available (Figures 1a and 1b, Supplement Figures S1a, S1b and S2a, S2b). Patients were excluded if they underwent concomitant procedures to address underlying pathology such as radial styloidectomy, ulna shortening, fracture fixation, arthroplasty, arthrodesis, and ligament reconstructions. Primary clinical diagnosis was documented. For this series, patients with arthritis were subdivided into those with scapholunate advanced collapse (SLAC) or scaphoid nonunion advanced collapse (SNAC) arthritis and those without.
Figure 1.
Preoperative (a) and postoperative films (b) of a 37-year-old man with scapholunate advanced collapse arthritis who experienced continued pain relief and required no further surgery after 9 years of follow-up.
Note. See supplemental online films for 3 other patients in the series including a patient undergoing proximal row carpectomy (see Figures S1a, S1b, S2a, S2b, and S3a, S3b).
The range of motion of the operative and contralateral wrist was measured using a goniometer. Data are reported as the total degrees of flexion/extension arc as well as the average arc when compared with the contralateral side at the last follow-up visit. Grip strength was measured as the average of 3 consecutive attempts at maximal grip using the dynamometer (setting 3; Jamar Hand Dynamometer, Sammons Preston Rolyan, Bolingbrook, Illinois). Latest radiographs were evaluated to evaluate progression of arthritis as indicated by increased subchondral sclerosis, joint space narrowing, cysts, or osteophytes and the presence of findings indicating a Charcot joint.18 Complications, including postoperative infection or delayed healing, were recorded. Mayo Wrist Score (MWS) as described by Cooney et al was calculated preoperatively and at most recent clinical follow-up when available.5 The MWS is scored out of 100 points and is defined as excellent (90-100), good (80-90), satisfactory (65-79), and poor (less than 65).2
Statistical analysis was performed using a Student t test to compare continuous variables or outcomes and Fisher exact test to compare categorical values. A Kaplan-Meier survival model was utilized to analyze revision-free survivorship and calculate hazard ratios for risk factors. Statistical significance was defined as P < .05. Data analysis was created to demonstrate progression of reoperation by year (Supplement Table 1), hazard conditions for revision surgery and revision related to initial diagnosis (Table 1).
Table 1.
Hazard Ratios for Revision Surgery and Subgroup Analysis of Survivorship.
| Risk factor | Hazard ratio | Confidence interval | P value |
|---|---|---|---|
| Age at surgery | 0.98 | 0.95-1.01 | .10 |
| Female gender | 1.54 | 0.73-3.15 | .25 |
| Laborer | 1.10 | 0.53-2.24 | .79 |
| Smoker | 1.67 | 0.56-4.05 | .32 |
| Dominant hand | 1.06 | 0.52-2.17 | .87 |
| Number of prior surgeries | 1.53 | 1.16-1.95 | .003* |
| Lawsuit pending | <0.01 | — | .38 |
| Worker’s compensation | <0.01 | — | .40 |
| Primary diagnosis | |||
| Non-SLAC/SNAC arthritis | 0.26 | 0.04-0.87 | .03* |
| Inflammatory arthritis | 1.07 | 0.43-2.37 | .87 |
| Posttraumatic arthritis | 2.26 | 0.54-6.50 | .23 |
| Ligamentous | 0.53 | 0.03-2.48 | .49 |
| SNAC/SLAC arthritis | 1.88 | 0.92-3.85 | .08 |
| Kienböck or Preiser disease | 1.36 | 0.08-6.37 | .77 |
| Unknown | 0.35 | 0.02-1.64 | .23 |
| Subgroup analysis of survivorship | |||
| Risk factor | % revised at any time point | 5-year survivorshipa | 10-year survivorshipa |
| Non-SLAC/SNAC arthritis (n = 21) | 9.5% | 86% | 86% |
| Unknown (n = 7) | 14% | 86% | 86% |
| Ligamentous only (n = 6) | 17% | 83% | 83% |
| Kienböck or Preiser (n = 3) | 33% | 67% | 67% |
| Inflammatory arthritis (n = 19) | 37% | 73% | 66% |
| Posttraumatic arthritis (n = 7) | 43% | 57% | 57% |
| SLAC or SNAC arthritis (n = 37) | 43% | 59% | 53% |
Note. SLAC = scapholunate advanced collapse; SNAC = scaphoid nonunion advanced collapse.
Values are given as the Kaplan-Meier survival estimate.
Values in bold represent significant P value.
Surgical Technique
Patients may be evaluated preoperatively with AIN/PIN local anesthetic block. This allows the patient and surgeon to “trial” the neurectomy to see whether patients improve with respect to pain or grip strength. Details of block technique have been previously described.2 Preoperative block may be useful to the surgeon and the patient once the differential diagnosis has been narrowed to determine potential efficacy of denervation.2 However, later studies noted that improvement with preoperative block did not correlate with ultimate outcome and may lead to high false-positive response.19
The surgical technique used in this series was carried out as described by Berger for a single-incision denervation.2 A 3 to 4 cm dorsal incision centered between the radius and ulna is made on the distal forearm, extending distally to one fingerbreadth above the ulnar head. After the skin is incised, superficial veins are retracted or cauterized. The deep antebrachial fascia is incised longitudinally, and the extensor tendons are retracted to expose the underlying interosseous membrane.
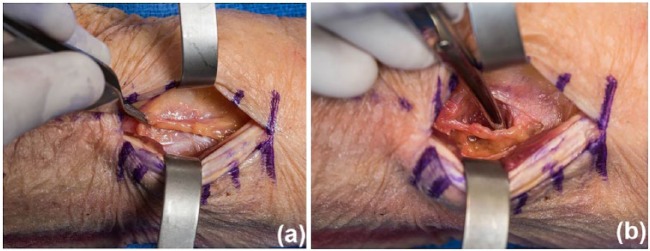
Lying on the interosseous membrane is the posterior division of the anterior interosseous artery with its venae comitantes and the PIN (Figures 2a and 2b). The nerve and artery are separated and 2 cm of the nerve is excised. The interosseous membrane is incised longitudinally to the distal radioulnar joint capsule. Just deep to the membrane is the deep head of the pronator quadratus. The AIN will be either just deep to the interosseous membrane or within 1 mm dorsal of the pronator quadratus muscle. The nerve may be accompanied by the anterior interosseous artery and its venae comitantes. At least 2 cm of the nerve is resected. The patient is placed into a posterior splint for 2 weeks until the wound heals before wrist motion commences as tolerated.
Figure 2.
(a) Isolation of the posterior interosseous nerve on the floor of the fourth dorsal compartment through dorsal midline approach (proximal to the right, distal left); (b) isolation of the anterior interosseous nerve immediately volar to interosseous septum.
Results
One hundred wrists in 89 patients (61 male, 28 female) were included (Table 2). During the study period (1994-2015), 227 wrists were identified which underwent denervation. Of these, 56 wrists had insufficient follow-up (<2 years) with an additional 71 excluded due to undergoing concomitant procedures which would obscure results. Eleven patients had bilateral wrist denervation. The affected wrist was the dominant side in 50 wrists. Average age at time of surgery was 54 years (range, 26-80). The principal diagnoses were arthritis (58%), including those with SLAC of SNAC arthritis (37%) and those without (21%); inflammatory arthritis (19%); and posttraumatic arthritis (7%) (Table 2). Forty-eight percent of patients were laborers and 16% were smokers. One patient had an active legal suit related to an injury from a motor vehicle accident and 1 patient was a workers’ compensation case. Thirty-two patients had undergone 1 or more operations before partial denervation surgery. Previous surgeries included wrist arthroscopy (n = 15), fracture fixation (distal radius n = 7,scaphoid n = 1), carpal tunnel release (n = 5), tenosynovectomy (n = 3), ganglion excision (n = 2), scapholunate ligament reconstruction (n = 2), ulnar head replacement (n = 1), proximal row carpectomy (n = 1), or other soft-tissue procedure (n = 11). The average number of procedures was 1.9 (range, 1-4). No patient had documentation of prior neurectomy based on review of patient’s medical record.
Table 2.
Demographic Data.
| No. total patients (No. wrists) | 89 (100) |
| Gender (No. male : female) | 61: 28 |
| Follow-up years (average, range) | 6.7 (1-20.75) |
| Age years (average, SD, range) | 54 (12, 26-80) |
| Dominant side involved (n, %) | 50 (50%) |
| Laborer (n, %) | 42 (42%) |
| Smoker (n, %) | 14 (14%) |
| Worker’s compensation (n, %) | 1 (1%) |
| Legal claim pending (n, %) | 1 (1%) |
| Preoperative symptoms | |
| Average preoperative duration symptoms months (average, SD, range) |
60 (89, 3-540) |
| Patients with previous operation (n, %) | 32 (32%) |
| Average number of previous operations (n, range) | 1.9 (1-4) |
| Primary diagnosis (n, % of total) | |
| Arthritis | 58 (58%) |
| SLAC or SNAC arthritis | 37 (37%) |
| Non-SLAC/SNAC arthritis | 21 (21%) |
| Inflammatory arthritis | 19 (19%) |
| Posttraumatic arthritis | 7 (7%) |
| Unknown | 7 (7%) |
| Ligamentous injury | 6 (6%) |
| Kienböck or Preiser disease | 3 (3%) |
Note. SLAC = scapholunate advanced collapse; SNAC = scaphoid nonunion advanced collapse.
Preoperative temporary local anesthetic block of the AIN/PIN was performed in 43 of 100 wrists. All 43 patients noted improvement in grip and/or pain scores with nerve blockade. Of these 43, 34 had objective grip strength recorded which improved on average 156% with injection (range, 100%-250%), and 30 had recorded subjective improvement of pain relief with injection.
Average follow-up time for clinical evaluation was 6.75 years (range, 1-21 years). Average postoperative flexion/extension arc was 95° on the affected extremity compared with 120° of the contralateral extremity, with average motion of unaffected side of 83% (Supplement Table 2). Grip strength was 25 kg vs 34 kg on the contralateral side, giving average grip strength of 75% of unaffected extremity (Supplement Table 2). There were no postoperative complications noted in this series; specifically no delayed wound healing, infection, painful neuroma formation, or episodes of complex regional pain syndrome.
Preoperative MWSs were available for 80 wrists. Average score was 48 (range, 10-70) with a breakdown of satisfactory (15) and poor (65). Postoperatively, MWS was available in 42 of 69 patients not undergoing revision (61%). Average MWS score at most recent follow-up was 77 (range, 35-100) at average time of 69 months postoperatively (range, 12-191). Postoperative MWS by category included excellent (13), good (7), satisfactory (15), and poor (7).
Average radiographic follow-up was 5 years (range, 1-19 years) and showed progression of arthritis in about half of cases (47 of 100). Within this series, a total of 31 patients (31%) underwent a revision operation at an average of 26 months postoperatively (range, 2-165) (Table 3, Supplement Figures S3a, S3b). The overall survival rate of partial wrist denervation surgery was 85% at 1 year, 71% at 5 years, 66% at 10 years, and 57% at 15 years as shown in Supplement Table 1 and Supplement Figure S4.
Table 3.
Need for, Type of, and Time to Revision Surgery.
| Type of revision surgery after partial wrist denervation | Total number | Average time to revision (mo, range) | Indication(s) |
|---|---|---|---|
| No revision (n, %) | 69 (69%) | ||
| Any revision (n, %) | 31 (31%) | 26 (2-165) | |
| Total wrist fusion | 5 (5%) | 23 (7-71) | Recurrence of pain |
| Partial wrist fusion | 15 (15%) | 26 (2-165) | Recurrent pain, pain with grip in laborer |
| Othera | 11 (11%) | 30 (2-122) | DRUJ symptoms, recurrent pain |
Note. DRUJ = distal radioulnar joint.
Type of procedure performed (n): Proximal row carpectomy (5), Sauve-Kapandji (1), Darrach (1), ulnar head implant arthroplasty (1), radial styloidectomy (1), hemiresection interposition arthroplasty (1), total wrist arthroplasty (1).
Of the 31 revision operations, 5 patients underwent a total wrist fusion (5%) and 15 patients (15%) underwent partial or limited fusion including scaphoidectomy and 4-corner fusion6 and radioscapholunate (RSL) fusion7 (Table 3). The other 11 operations (11%) included a proximal row carpectomy (5), total wrist arthroplasty (1), Sauve-Kapandji (1), Darrach procedure (1), ulnar head implant arthroplasty (1), radial styloidectomy (1), and hemiresection interposition arthroplasty (1).
Hazard ratio analysis demonstrated that patients who had undergone surgery for the wrist prior to partial denervation were more likely to require revision surgery, which was a significant finding (P = .003) (Table 1). Hazard analysis by primary diagnosis showed that patients with arthritis had the most durable outcomes following denervation (P = .03). Subgroup analysis of Kaplan-Meier survivorship model echoed these findings as noted in Table 1; arthritis had the lowest revision rate (9.5%) compared with SNAC, SLAC or posttraumatic arthritis which had the highest rates (43%).
Discussion
The principle of partial wrist denervation is to reduce pain stemming from intra-articular pathology by resecting peripheral nerves whose terminal fibers innervate the joint capsule.2 Selective denervation does not impact motor input; therefore, wrist motion and strength are not affected.2 Importantly, denervation does not preclude future surgical procedures if pain complaints are not resolved.
Wilhelm popularized total wrist denervation as a treatment option for wrist pain; surgical technique was based on his anatomical studies and resected 10 nerves approached through 5 incisions.20 Rostlund et al described a modified technique with 4 incisions for full denervation.15 Later studies demonstrated primary innervation of the wrist is via the AIN and PIN,2,4,8 and a single-incision technique for selective AIN/PIN denervation has since been described.2
The contribution of the AIN/PIN to wrist proprioception has been studied, questioning the clinical sequelae of denervation particularly in a young active patient. Hagert and Persson studied the ligamentomuscular reflex patterns following desensitization of the PIN on 8 volunteers.12 Volunteers underwent electromyography testing associated with stimulation of the scapholunate ligament before and after anesthetizing the PIN. They found altered reflex patterns following desensitization, concluding that partial denervation alters joint proprioception and should be avoided. Conversely, Gay et al performed a double-blinded randomized study on 80 volunteers in which control and test groups underwent saline or anesthetic block, respectively, of the AIN/PIN.10 Subjects then performed active and passive wrist repositioning tasks. There was no difference between control and test groups in repositioning errors.
Wilhelm’s initial surgical indications were management of Kienböck disease or scaphoid nonunion.20 Indications have since been expanded to any intra-articular conditions leading to pain which is refractory to conservative management.2,16 In this series, surgical indications included patients with refractory wrist pain of which the primary diagnosis was most commonly arthritis (Table 2).
Bivariate analysis demonstrated that prior surgery was associated with revision surgery (Table 1). Trending toward significance for high revision rates were patients with SLAC, SNAC, or posttraumatic arthritis. Lowest revision rates were noted among the non-SNAC/SLAC arthritis cohort. Based on the results of this series, patients with multiple previous surgeries and SNAC, SLAC, or posttraumatic arthritis should be counseled on a less reliable outcome with denervation surgery. This is in keeping with other studies which have shown that denervation tends to work well for early stages of arthritis but less so in advanced changes.13,14 The studies by Schweizer et al and Buck-Gramcko echoed our findings of less reliable outcomes in posttraumatic arthritis.4,16
We found that 20% of patients underwent later fusion and 31% underwent any revision surgery. Weinstein and Berger found that 15% of patients required a secondary procedure.19 Other series have reported revision rates of 14%16 and 28%.13 On average, partial denervation was able to provide just over 2 years of additional time before patients underwent a revision procedure.
Mayo Wrist Scores were used in our series to evaluate improvements in pain and function. Mayo Wrist Scores improved from on average 48 preoperatively to 77 postoperatively. Approximately half of patients (48%) had good to excellent results and 36% satisfactory which highlights the opportunity for improved pain and function. However, 16% had poor results underscoring the fact that denervation does not prevent ongoing degenerative changes in the wrist and patients may not expect full relief of symptoms. No significant correlation was identified by etiology for which patients noted improved or worsening MWS at final follow-up. This is in keeping with the literature which notes overall satisfaction rates ranging from 69%-89%.4,11,14-16,19 Two studies have shown much less favorable rates of 29%13 and 56%.9
No complications were noted in the cohort, specifically no infection, painful neuroma formation, or episodes of complex regional pain syndrome. Other series have noted hematoma or neuroma formation.3 Charcot arthropathy is a theoretical risk that could progress in a denervated joint. Charcot arthropathy is rare in the upper extremity, often related to syringomyelia or diabetes, and is characterized by joint destruction, bony fragmentation, fracture, and eventual fusion of the joint in an often rapid sequence.1 To our knowledge, there have been no reports of Charcot arthropathy related to denervation surgery and we found no evidence in our series with average radiographic follow-up of 61 months (range, 12-228).
We recognize the limitations inherent to retrospective studies. The study ranged over a 20-year time frame with patients subsequently lost to follow-up during this period. Complication and revision rates may be underestimated if patients have received additional cares elsewhere. Using reoperation as an outcome carries inherent bias as decision for reoporation can be affected by patient and/or surgeon preferences. In addition, there may be a selection bias among this group of patients that choose surgery for treatment at a higher rate than the general population. The series includes limited patient outcomes with the MWS available in 60% of patients and is a weakness of this study. The radiographic observer was not blinded, which could allow for potential bias. Patients were treated for a variety of conditions with no alternative surgical procedure for comparison.
These limitations notwithstanding, the study provides long-term data regarding the outcomes of partial wrist denervation. We have found that this is a reliable motion-preserving procedure for patients with chronic wrist pain which does not preclude future surgical interventions. In the series, 69% of patients did not undergo revision surgery at average follow-up of approximately 7 years. The 31% who did require revision were able to buy almost 2 years prior to undergoing reoperation, with 20% requiring partial or total wrist fusion. These results better enable surgeons to give revision rates, time estimates, and chances for symptom relief following wrist denervation in the patient with chronic wrist pain.
Supplemental Material
Supplemental material, HAN760031_Supplemental_Material for Buying Time: Long-Term Results of Wrist Denervation and Time to Repeat Surgery by Maureen A. O’Shaughnessy, Eric R. Wagner, Richard A. Berger and Sanjeev Kakar in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board (15-000196).
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Bayne O, Lu EJ. Diabetic Charcot’s arthropathy of the wrist: case report and literature. Clin Orthop Relat Res. 1998;357:122-126. [DOI] [PubMed] [Google Scholar]
- 2. Berger RA. Partial denervation of the wrist: a new approach. Tech Hand Up Extrem Surg. 1998;2:25-35. [DOI] [PubMed] [Google Scholar]
- 3. Braga-Silva J, Roman JA, Padoin AV. Wrist denervation for painful conditions of the wrist. J Hand Surg Am. 2011;36:961-966. [DOI] [PubMed] [Google Scholar]
- 4. Buck-Gramcko D. Denervation of the wrist joint. J Hand Surg Am. 1977;2:54-61. [DOI] [PubMed] [Google Scholar]
- 5. Cooney WP, Bussey R, Dobyns JH, et al. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987(214):136-147. [PubMed] [Google Scholar]
- 6. Dellon AL. Partial dorsal wrist denervation: resection of the distal posterior interosseous nerve. J Hand Surg Am. 1985;10:527-533. [DOI] [PubMed] [Google Scholar]
- 7. Dellon AL. Partial joint denervation I: wrist, shoulder, and elbow. Plast Reconstr Surg. 2009;123:197-207. [DOI] [PubMed] [Google Scholar]
- 8. Dellon AL, Mackinnon SE, Daneshvar A. Terminal branch of anterior interosseous nerve as source of wrist pain. J Hand Surg Br. 1984;9:316-322. [DOI] [PubMed] [Google Scholar]
- 9. Ekerot L, Holmberg J, Eiken O. Denervation of the wrist. Scand J Plast Reconstr Surg. 1983;17: 155-157. [DOI] [PubMed] [Google Scholar]
- 10. Gay A, Harbst K, Hansen DK, et al. Effect of partial wrist denervation on wrist kinesthesia: wrist denervation does not impair proprioception. J Hand Surg. 2011;36:1774-1779. [DOI] [PubMed] [Google Scholar]
- 11. Geldmacher J, Legal HR, Brug E. Results of denervation of the wrist and wrist joint by Wilhelm’s method. Hand. 1972;4:57-59. [DOI] [PubMed] [Google Scholar]
- 12. Hagert E, Persson JKE. Desensitizing the posterior interosseous nerve alters wrist proprioceptive reflexes. J Hand Surg. 2010;35:1059-1066. [DOI] [PubMed] [Google Scholar]
- 13. Ishida O, Tsai TM, Atasoy E. Long-term results of denervation of the wrist joint for chronic wrist pain. J Hand Surg Br. 1993;18:76-80. [DOI] [PubMed] [Google Scholar]
- 14. Radu CA, Schachner M, Trankle M, et al. [Functional results after wrist denervation]. Handchir Mikrochir Plast Chir. 2010;42:279-286. [DOI] [PubMed] [Google Scholar]
- 15. Rostlund T, Somnier F, Axelsson R. Denervation of the wrist joint—an alternative in conditions of chronic pain. Acta Orthop Scand. 1980;51:609-616. [DOI] [PubMed] [Google Scholar]
- 16. Schweizer A, von Kanel O, Kammer E, et al. Long-term follow-up evaluation of denervation of the wrist. J Hand Surg Am. 2006;31:559-564. [DOI] [PubMed] [Google Scholar]
- 17. Slutsky DJ. Outcomes assessment in wrist surgery. J Wrist Surg. 2013;2(1):1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tatkow RW. Charcot disease of the wrist and the carpus. Clin Orthop Relat Res. 1966;46:115-119. [PubMed] [Google Scholar]
- 19. Weinstein LP, Berger RA. Analgesic benefit, functional outcome, and patient satisfaction after partial wrist denervation. J Hand Surg Am. 2002;27:833-839. [DOI] [PubMed] [Google Scholar]
- 20. Wilhelm A. Articular denervation and its anatomical foundation. A new therapeutic principle in hand surgery. On the treatment of the later stages of lunatomalacia and navicular pseudarthrosis. Hefte Unfallheilkd. 1966;86:1-109. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, HAN760031_Supplemental_Material for Buying Time: Long-Term Results of Wrist Denervation and Time to Repeat Surgery by Maureen A. O’Shaughnessy, Eric R. Wagner, Richard A. Berger and Sanjeev Kakar in HAND