Abstract
Background: We made a tin ring splint for osteoarthritis of the distal interphalangeal joint that looks attractive and is easy to wear. We report the treatment results with this splint. Methods: We enrolled 30 patients with painful osteoarthritis of the distal interphalangeal joint in this study. A tin ring splint was made with tin alloy containing small quantities of silver. Patients were instructed to wear the splint when they felt pain. Patients were assessed before splint use and after 1, 3, and 6 months of splint use. Endpoints included the numeric pain scale, active arc of motion of the distal interphalangeal joint, Hand 20, functional assessment criteria of the upper extremities, and treatment satisfaction. In addition, data were collected on time to symptom relief and satisfaction related to usability and appearance of the splint (0 = dissatisfied, 10 = satisfied). Results: The numeric pain scale showed significant pain improvement from 58.4 ± 4.1 at baseline to 33.1 ± 4.5 at 1 month, and the Hand 20 score also showed significant improvement from 35.0 ± 4.3 at baseline to 20.2 ± 3.2 after 6 months. Active arc of motion were not changed significantly. Most patients responded that symptoms were relieved by the 10th day after treatment. Satisfaction related to usability was 8.9 ± 0.3, and appearance was 7.6 ± 0.4. Conclusions: A tin ring splint quickly reduced pain, and satisfaction related to usability and appearance was high. This splint could be one choice for conservative treatment of osteoarthritis of the distal interphalangeal joint.
Keywords: osteoarthritis, splint, conservative therapy, distal interphalangeal joint, tin
Introduction
Although various treatments have been suggested for painful osteoarthritis of the distal interphalangeal (DIP) joint, conservative therapy is believed to be the first choice in the vast majority of patients. Of the conservative methods, good results have been reported with splinting,6,9 but they are generally difficult to apply and have cosmetic issues. In our experience, patient adherence to splinting therapy is not always good. Based on our belief that splints that are easier to wear and more cosmetically appealing will enhance adherence to splinting therapy and improve treatment results, we developed a ring-like splint made of a tin alloy that is also easily manipulated. In this study, we report our treatment results using this tin ring splint in DIP joint osteoarthritis.
Methods
The participants of this prospective study included consecutive 30 patients with painful DIP joint osteoarthritis including 28 women and 2 men aged 46 to 85 years (mean, 68 years). Finger involvement was the thumb in 2, index finger in 10, middle finger in 7, ring finger in 3, and little finger in 8 cases. The patients had been in pain for 1 month to 20 years (mean, 34 months). Osteoarthritis severity per Kellgren-Lawrence classification7 (Table 1) was Grade 0 in 1, Grade 1 in 2, Grade 2 in 9, Grade 3 in 6, and Grade 4 in 12 cases. The patients with secondary joint deformation due to comorbid conditions such as trauma, gout, or rheumatoid arthritis as well as those with severe deformations with joint subluxation were excluded from the study. In addition, those who received intra-articular injections of steroids or hyaluronic acid formulations within the last 6 months were also excluded.
Table 1.
Kellgren-Lawrence Classification.7.
| Grade | Radiographic findings |
|---|---|
| 0 | Normal |
| 1 | Doubtful narrowing of joint space, possible osteophytic lipping |
| 2 | Possible narrowing of joint space, definite osteophytes |
| 3 | Definite narrowing of joint space, moderate multiple osteophytes, some subchondral sclerosis, possible deformity of bone ends |
| 4 | Marked narrowing of joint space, large osteophytes, severe subchondral sclerosis, definite deformity of bone ends |
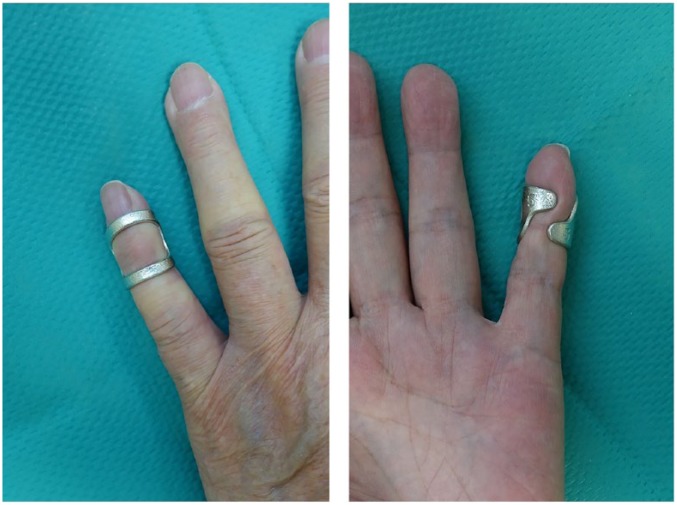
The splint was manufactured at Nousaku Corporation (Toyama, Japan). Based on the results of previous studies, the splint was created from a tin alloy containing small quantities of silver. As the splint has a degree of hardness such that it can be adjusted as needed, it is easy to apply and remove. However, it is not hard enough to fix the DIP joint completely. The main purpose of this splint is to restrict the motion of the DIP joint. The splint was a ring-like shape, but the dorsal side was left open so that it would not interfere with the DIP joint osteophytes (Figure 1). Splints were available in 3 sizes—S (equal to Japan Custom Size specifications size 5), M (equal to size 10), and L (equal to size 14)—and prescribed based on the size of the affected finger. Frequency or duration of use was not specified, and patients were told to wear or remove the splints freely depending on pain severity (Figure 2). No new oral or topical pain medications were prescribed for the duration of the study.
Figure 1.

Tin ring splint. The dorsal side is shown on the left, whereas the volar side is shown on the right.
Figure 2.
This patient wore a small splint.
Patients were assessed before splint use and after 1, 3, and 6 months of splint use. Endpoints included the numeric pain scale (NPS), active arc of motion of the DIP joint, Hand 20,2 functional assessment criteria of the upper extremities, treatment satisfaction, and frequency of wearing the splint in the last week. The Hand 20 is a 20-item patient-based assessment method that is used to rate their overall function of the upper extremity in the last week; the score ranges from 0 (no issues) to 100 points (worst possible case). We evaluated the Hand 20 under the condition that the splint was used appropriately according to pain. Treatment satisfaction was rated on a 10-point scale (0 = dissatisfied to 10 = completely satisfied). In addition, a questionnaire administered at 1 month assessed satisfaction with the ease of wearing the splint and its cosmetic appeal rated on a 10-point scale, whether use of the splint helped lessen the pain, and when the pain began to lessen.
Statistically, 1-way analysis of variance was used to compare the data for range of motion, NPS, Hand 20, treatment satisfaction, and frequency of wearing the splint. If the comparison showed a significant difference, Bonferroni multiple comparison test was performed at a significance level of 5%.
Results
The baseline NPS of 58.4 ± 4.1 (mean ± SEM) decreased after splint use to 33.1 ± 4.5 after 1 month, 26.4 ± 4.0 after 3 months, and 21.6 ± 4.0 after 6 months. Significant improvement was observed after 1 month (P < .001; Figure 3). The active arc of motion was 35.0 ± 4.1 at baseline, 37.3 ± 4.2 after 1 month, 39.1 ± 4.3 after 3 months, and 39.5 ± 4.3 after 6 months. No significant change was observed during the follow-up period (Figure 4). The baseline Hand 20 score of 35.0 ± 4.3 decreased to 28.0 ± 3.5 after 1 month and 20.2 ± 3.2 after 6 months. Significant improvement was observed at 6 months (P < .001; Figure 5). Treatment satisfaction was 7.8 ± 0.4 after 1 month, 7.7 ± 0.3 after 3 months, and 7.8 ± 0.4 after 6 months. No significant change was observed during the follow-up period (Figure 6). Frequency of wearing the splint was decreased to 6.2 ± 0.3 days/week after 1 month, 4.7 ± 0.5 days/week after 3 months, and 3.8 ± 0.5 days/week after 6 months. Significant change was observed after 3 month (P < .001). Although the frequency of wearing decreased, the treatment satisfaction did not change during the follow-up period. Satisfaction related to usability was 8.9 ± 0.3, whereas that related to appearance was 7.6 ± 0.4. Regarding pain alleviation with splint use, 25 patients reported pain relief (83.3%), whereas 5 reported no change. Most patients responded that their symptoms were begun to lessen by the 10th day after treatment. No adverse events such as cutaneous symptoms were noted during this study.
Figure 3.
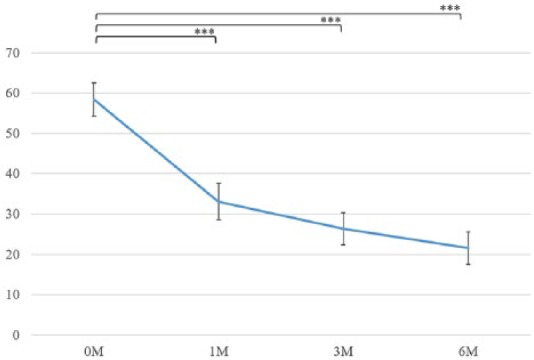
The numeric pain scale. Significant improvement was observed after 1 month.
***P < .001.
Figure 4.
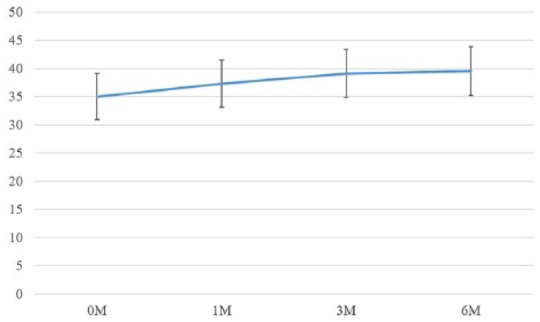
The active arc of motion. No significant change was observed.
Figure 5.
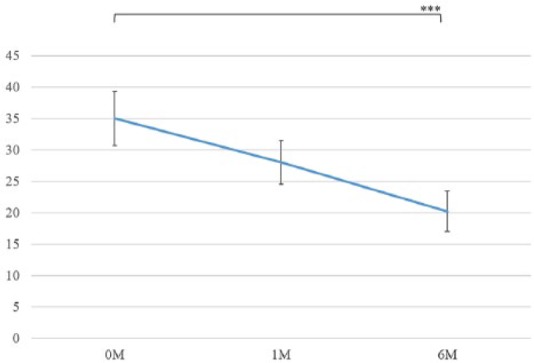
The Hand 20. Significant improvement was observed at 6 months.
***P < .001.
Figure 6.
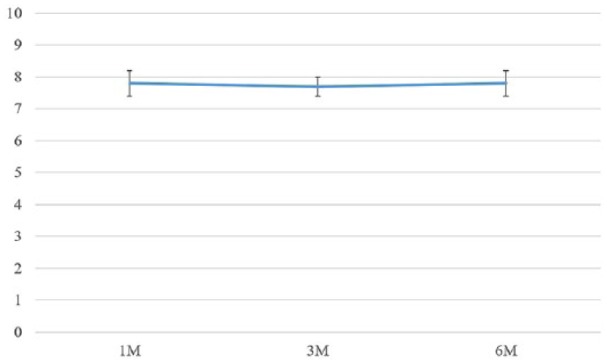
Treatment satisfaction. No significant change was observed.
Discussion
In addition to experiencing effective pain alleviation, patients were highly satisfied with splint ease of use and appearance without increasing joint stiffness. Therefore, this new finger splint appears to be a useful method that would easily fit into daily life.
DIP joint osteoarthritis is commonly encountered in clinical practice; according to previous reports, it affects as many as 30% to 40% of adults aged ≥40 years.1,3,10 Moreover, in 2016, Japanese epidemiological surveys reported a prevalence of 86% in patients aged ≥40 years.8 Although DIP joint osteoarthritis is an extremely common disease, its treatment remains unestablished. Currently, many reports are available on conservative and surgical therapy, but adequate evidence is lacking. Hill et al reported that patients with osteoarthritis of the fingers do not receive appropriate information at medical facilities.4 Furthermore, Horiuchi et al reported that active therapy is not instituted and patients are often left untreated.5
Splinting has been suggested as a conservative therapy for osteoarthritis of the DIP joints. It is unknown why splinting alleviates pain, but perhaps preventing mechanical irritation to the site lessens local inflammation and thus enhances tissue repair.9 Soft splints that are custom-designed specifically for a patient’s finger are reportedly effective at lessening pain.1 However, splints that are generally used for fingers are constructed of aluminum or thermoplastic substances and associated with problems such as becoming dirty or smelly after continued wear. Furthermore, these splints can hardly be said to consider cosmetic issues. Consequently, physicians are not as likely to aggressively recommend splinting therapy. If splints that looked appealing were available, splinting therapy might indeed become a viable treatment option. Therefore, we decided to develop a new type of splint.
These splints should be easy to put on and take off, comfortable to wear, and esthetically pleasing. The tin used in our splint was once considered as precious as gold or silver. Also, the tin has a degree of hardness such that it can be adjusted as needed. By using metals with these properties, we believe that we succeeded in creating a splint that produces high patient satisfaction.
Several papers have reported that splinting effectively relieves pain. Ikeda et al reported that NPS improved from 56 before the use of a custom-made splint to 17 after 6 months of splint use.6 Watt et al used a night splint and found that the baseline NPS of 60 improved to 45 after 3 months and even further to 40 after 6 months.9 With our splint, the NPS decreased from 58.4 at baseline to 33.1 after only 1 month and even further to 21.6 after 6 months, results comparable with those of the prior reports. In addition, pain-relieving effect should be obtained promptly after the start of splint treatment, and short-term results should also be emphasized. The pain-relieving effect of the splint was an ideal result as it was recognized relatively early at 10 days of wear. Although the frequency of wearing decreased, the treatment satisfaction did not change during the follow-up period. Therefore, it was considered that the decreasing of wearing frequency was caused by reduced pain, and patient adherence to this splinting therapy did not decrease.
The limitation of this study is that there was no control group comparison. We thought that the natural history of osteoarthritis may have influenced the results of this study. However, we did not compare the results with those of the untreated control group. Thus, we cannot affirm whether there was a relationship. Furthermore, it was not possible to examine the influence of the severity of osteoarthritis and the duration of disease on the treatment outcome due to the small number of cases. Based on the results of this study, we are planning a larger comparative study with a control group without splint use.
Conclusions
A tin alloy splint for DIP joint osteoarthritis was developed to treat this condition. This splint alleviates pain, and is easy to wear and esthetically pleasing, achieving a high level of patient satisfaction.
Supplementary Material
Footnotes
Authors’ Note: This trial is registered with the University Hospital Medical Information Network (UMIN) Center (ID: UMIN000026637, http://www.umin.ac.jp/).
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the medical ethics review board of Kanazawa University (2015-242(2114)) on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
Declaration of Conflicting Interests: The authors have received tin ring splints from Nousaku Corporation, and declare that there is no other conflict of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: K Tada  https://orcid.org/0000-0001-8930-1093
https://orcid.org/0000-0001-8930-1093
References
- 1. Fujisawa K, Inada H, Kino S, et al. The incidence of the Heberden’s nodes in general population group. J Jpn Soc Surg Hand. 1987;4:769-772. (In Japanese) [Google Scholar]
- 2. Hand20. Date unknown. http://www.handfrontier.org/data/hand1020/hand20ver4.pdf. Accessed February 6, 2018.
- 3. Haugen IK, Englund M, Aliabadi P, et al. Prevalence, incidence and progression of hand osteoarthritis in the general population: the Framingham Osteoarthritis Study. Ann Rheum Dis. 2011;70:1581-1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hill S, Dziedzic KS, Nio Ong B. Patients’ perceptions of the treatment and management of hand osteoarthritis: a focus group enquiry. Disabil Rehabil. 2011;33:1866-1872. [DOI] [PubMed] [Google Scholar]
- 5. Horiuchi K, Horiuchi Y, Ochi K, et al. Questionnaire survey of Heberden’s node. J Jpn Soc Surg Hand. 2014;30:776-778. (In Japanese) [Google Scholar]
- 6. Ikeda M, Ishii T, Kobayashi Y, et al. Custom-made splint treatment for osteoarthritis of the distal interphalangeal joints. J Hand Surg Am. 2010;35:589-593. [DOI] [PubMed] [Google Scholar]
- 7. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kodama R, Muraki S, Oka H, et al. Prevalence of hand osteoarthritis and its relationship to hand pain and grip strength in Japan: the third survey of the ROAD study. Mod Rheumatol. 2016;26:767-773. [DOI] [PubMed] [Google Scholar]
- 9. Watt FE, Kennedy DL, Carlisle KE, et al. Night-time immobilization of the distal interphalangeal joint reduces pain and extension deformity in hand osteoarthritis. Rheumatology (Oxford). 2014;53:1142-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wilder FV, Barrett JP, Farina EJ. Joint-specific prevalence of osteoarthritis of the hand. Osteoarthritis Cartilage. 2006;14:953-957. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.