Abstract
Background: In 2012, our unit published our experience with a pyrocarbon proximal interphalangeal joint (PIPJ) implant. Due to high subsidence rates, a decision was made to change to a cemented surface replacement proximal interphalangeal joint (SR-PIPJ) implant. The purpose of this study was to assess whether the change to a cemented implant would improve the subsidence rates. Methods: Retrospective review of all patients who had a cemented SR-PIPJ arthroplasty performed from 2011 to 2013 with at least 12 months follow-up. Results: A total of 43 joints were included with an average follow-up of 26.5 months. There was a significant (P = .02) improvement in arc of motion with an average satisfaction score of 3.3 (satisfied patient). Subsidence was noted in 26% of joints with a significant difference in range of motion (P = .003) and patient satisfaction (P = .001) between the group with and without subsidence. Conclusions: The change to a cemented implant resulted in satisfied patients with an improvement in range of motion. The rate of subsidence improved but remains unacceptably high.
Keywords: proximal interphalangeal joint arthroplasty, uncemented, subsidence, surface replacement, pyrocarbon
Introduction
The Swanson Finger Joint implant (Wright Medical Technology, Memphis, Tennessee) is the most commonly used proximal interphalangeal joint (PIPJ) arthroplasty implant,13 and some authors regard it as the most appropriate implant to use.5 Lateral stability remains an issue, especially in the index finger and middle finger where stability is important for pinch.4 Some authors16 therefore still recommend arthrodesis for the index finger. This has led to the development of the surface replacement arthroplasty for the PIPJ which relies on the intact collateral ligaments, bicondylar configuration, and soft tissue envelope around the PIPJ to provide lateral stability.9,10 At least 2 types of surface replacement arthroplasty are currently being used: An uncemented pyrocarbon implant and a cobalt-chrome (Co-Cr) on ultra-high-molecular-weight polyethylene (UHMWPE) implant which can be cemented or uncemented. In 2012, our institution reported on a series of 57 uncemented pyrocarbon PIPJ implants.12 The major concern was that subsidence was observed in 40% of the joints. Sweets and Stern noted radiological signs of loosening in 48% of their pyrocarbon implants and stopped using this implant.17 Importantly, Johnstone compared cemented versus uncemented surface replacement implants and noted subsidence in 68% of the uncemented group and in only 4% of the cemented group.9
The 40% subsidence noted in the pyrocarbon series and the results from these other authors led our senior author to change his practice for PIPJ arthroplasty from an uncemented pyrocarbon implant to a cemented Co-Cr on UHMWPE implant. The surgical approach and postoperative rehabilitation remained unchanged.
The aim of this study was to determine whether the change to a cemented Co-Cr on UHMWPE would lead to an improvement in subsidence rates as well as other complications.
Methods
We performed a retrospective chart review of all patients who had a cemented Co-Cr on UHMWPE surface replacement arthroplasty of the PIPJ performed from 2011 to 2013 with at least 12 months follow-up.
The surgical approach and postoperative rehabilitation remained the same as in the pyrocarbon series, but we will outline the important aspects. All surgeries were performed by the senior author. A dorsal approach with an extensor tendon splitting technique was performed. The central slip is split and sharply dissected off the middle phalanx. A small power saw is used to perform the bony resection of the articular surface of the proximal phalanx and middle phalanx. Care is taken to preserve the dorsal lip of the middle phalanx for later anatomic reattachment of the extensor. The collateral ligaments are preserved. The intramedullary canal of the proximal and middle phalanx is opened with an awl. A trial prosthesis is inserted to confirm the correct size. Before insertion of the definitive prosthesis, a drill hole is made in the dorsum of the base of the middle phalanx and sutures passed through it for attachment of the central slip. The prosthesis is cemented into position. The central slip is reattached to the middle phalanx with a suture passed through a drill hole. After skin closure, a bulky dressing is applied with a dorsal slab. The metacarpophalangeal joints (MCPJs) are held in 70° flexion and the interphalangeal joints in extension.
At 4 to 5 days postoperatively, the plaster slab is removed and exchanged for a hand-based dorsal thermoplastic splint. The splint keeps the MCPJ in 70° of flexion and the PIPJ in 15° of flexion. The patient is encouraged to flex to 45° in the first week and 60° in the second week. After the second week, unrestricted active flexion is allowed. No passive flexion is allowed for the first 4 weeks. After 2 weeks, the splint is only used at night.
The following data were recorded: age, gender, finger involved, indication for surgery, preoperative range of motion, range of motion at final follow-up, time to final follow-up, patient satisfaction, complications, presence or absence of subsidence on final follow-up radiograph, and any secondary surgery. Patient satisfaction was recorded according to a Likert scale (see Table 1 for details of the score). A score of 1 and 2 would be classified as poor, a score of 3 acceptable, and a score of 4 and 5 as good.
Table 1.
Likert Scale Used to Assess Patient Satisfaction.
| Score | Description |
|---|---|
| 1 | Unsatisfied/would not want same procedure again |
| 2 | Less than expected/would consider having same procedure again |
| 3 | Result as expected |
| 4 | Result better than expected |
| 5 | Fantastic result/would recommend procedure |
Subsidence was regarded as any change in position of the implant in relation to the bone when comparing the first postoperative radiograph to the radiograph at final follow-up. All radiographs were reviewed by the primary author and the senior author. The distance from the tip of the stem to the base of the phalanx was measured on both radiographs, and any change in distance was considered as subsidence (Figure 1). All measurements were done on the digital x-ray system.
Figure 1.
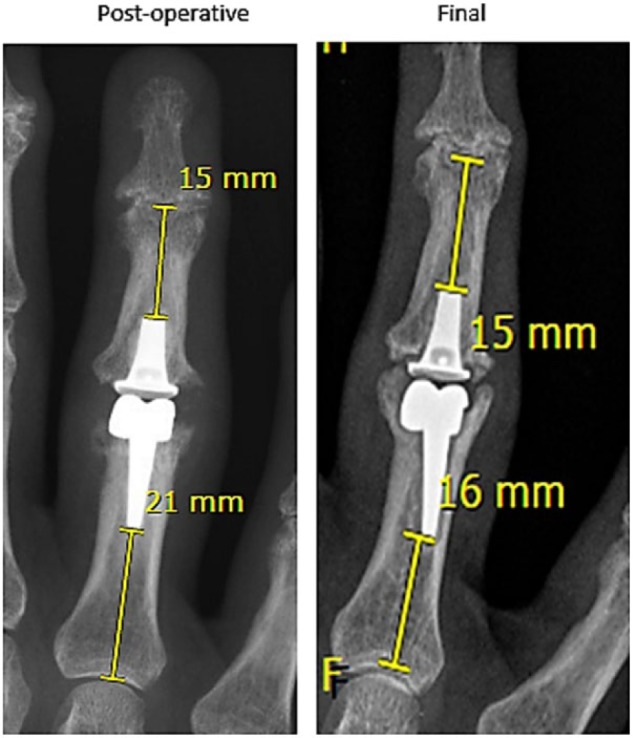
Technique for measurement of subsidence.
The primary aim of the study was to determine whether the change from an uncemented pyrocarbon to a cemented Co-Cr on UHMWPE implant would lead to an improvement in subsidence rates. The secondary aim was to determine the complication rate.
Statistical Analysis
Statistical analysis was performed using the Student t test. Statistical significance was defined as P < .05.
Results
Fifty-two replacements were performed in this time, of which 43 replacements, in 28 patients, had a 12-month follow-up. Final follow-up radiographs were obtained in 34 joints. There were 3 male patients and 25 female patients. The mean age was 59.5 (range, 51-80) years. The mean follow-up was 26.5 (range, 14-41) months. The ring finger was the most commonly operated finger, with 14 replacements, followed by the middle finger with 12 replacements, the index finger with 11 replacements, and the little finger with 5 replacements. The indication for replacement was primary osteoarthritis in 38 fingers, posttraumatic arthritis in 3 fingers, and inflammatory arthritis in 1 finger.
Range of Motion
Postoperative range of motion was obtained for all 43 fingers, but preoperative range of motion was only available for 37 fingers. Average range of motion was calculated for these 37 fingers.
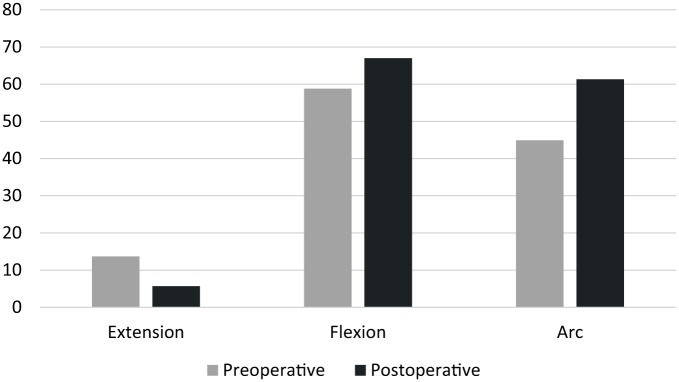
The average preoperative range of motion was 13.7° (range, 0°-60°) to 58.6° (range, 25°-80°) with an arc of motion of 44.9°. The average postoperative range of motion was 5.7° (range, 10°-80°) to 67° (range, 0°-100°) with an arc of motion of 61.3° (Figure 2), showing a significant improvement in arc of motion (P = .02).
Figure 2.
Range of motion.
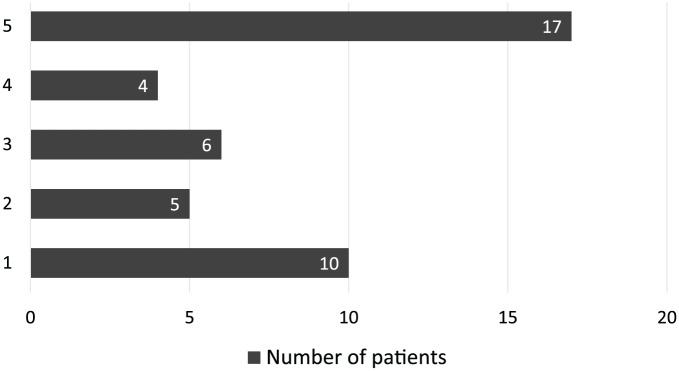
Patient Satisfaction
Patient satisfaction was measured according to a 5-point Likert scale. The average satisfaction was 3.3 (acceptable to good) out of 5. Figure 3 has the complete patient satisfaction results, showing the number of patients who recorded their satisfaction on a scale of 1 to 5. Seven of the 10 patients with a satisfaction score of 1 were living far away.
Figure 3.
Patient satisfaction.
Complications
The total number of fingers with complications were 13 (31%), which included stiffness, swan neck deformities, fixed flexion deformities, and a cement loose body.
Stiffness was encountered in 8 fingers. Any patient with an arc of motion of less than 30° was regarded as being stiff. The indication in one of the patients was posttraumatic arthritis, and the patient had a poor range of motion preoperatively already. An extensor tenolysis and capsulotomy were performed in 2 patients of which one had a very good result and the other patient progressed to a stiff swan neck deformity. One patient had loosening noted and had a revision performed with no improvement in range of motion with loosening noted again on final follow-up radiograph. One patient was a revision from a pyrocarbon implant. The other patients with stiffness were satisfied with their result and has had no further surgery.
Three fingers developed a swan neck deformity after the initial arthroplasty. Two were successfully managed with splinting and one is awaiting surgery for a flexor digitorum superficialis tenodesis.
A fixed flexion deformity occurred in 1 patient. This was managed with a surgical release, but the deformity recurred.
One patient had a cement loose body which was successfully removed.
Subsidence
We classified subsidence as any change of the position of the implant in relation to the bone when comparing the initial postoperative radiograph with the final follow-up radiograph. Subsidence was noted in 9 (26%) joints. Of the 9 joints, 4 were in the index finger (Figure 4), 3 in the middle finger, and 2 in the ring finger. This group’s average range of motion was 1° to 29° (arc 28°) compared with the 4.2° to 69.1° (arc 64.9°) of the group without subsidence (n = 25). This difference in range of motion was statistically significant (P = .003). Their average satisfaction was 1.6 compared with 4 of the group without subsidence (P = .001).
Figure 4.

Radiograph of patient showing lucency around the distal component and migration of the proximal component of the index finger.
Discussion
In 2010, Amadio said that PIPJ arthritis remains an unsolved problem. Results in terms of restoration of motion and durability have been disappointing, but postoperative pain relief has been good.3 The SR-PIPJ replacement was developed to provide a more stable implant by retaining the collateral ligaments.10 This provides an alternative to arthrodesis in especially the index finger where the silicone implants have failed to provide enough stability.4 A number of authors have published on their experiences with SR-PIPJ implants, but the main purpose of this study was to determine whether the change from pyrocarbon to cemented Co-Cr on UHMWPE at our institution would improve our results in terms of specifically subsidence and complications.12
There were 43 replacements with a mean age of 59.5 years and mean follow-up of 26.5 months. The most common indication by an overwhelming majority was primary osteoarthritis. This compares well with McGuire et al who had 57 implants with a mean age of 61 years and mean follow-up of 27 months and with their most common indication being osteoarthritis.12
There was a significant improvement in range of motion, which differs from McGuire et al who found an extremely significant improvement in range of motion. Our results are similar to other authors who found only a small or no increase in range of motion.1,16 Johnstone et al9 and Johnstone8 found that postoperative range of motion will be determined by preoperative range of motion and therefore a large improvement in motion should not be expected. Herren et al stated that most patients accept their limited range of motion, because they are satisfied with being pain free.6
The average patient satisfaction was 3.3, which is not as good as in the study by McGuire et al who had an average score of 4.2 (we used the same satisfaction score). A score of 3.3 does however equate to a satisfied patient with a result as expected. When looking only at patients with no radiological signs of subsidence (Figure 5), the average satisfaction score does improve to 4 (result better than expected). Interestingly, 7 of the 10 patients with a satisfaction score of 1 were living far away. We can only speculate, but this may be due to a decreased number of postoperative follow-up visits or lack of sufficient postoperative rehabilitation. This should be discussed with patients preoperatively, and plans should be made to address this.
Figure 5.

A patient who had all 4 of her proximal interphalangeal joints replaced. Her satisfaction score for each finger was 5, and range of motion in each finger was 0° to 90°.
In a meta-analysis on PIPJ replacements, it was noted that 28% of all replacements were associated with at least one complication in the first 12 Months.1 Linscheid et al also noted a significant number of complications.10 The number (31%) and type of complications we found are similar to what the literature suggests. There was however an improvement in complications when compared with the pyrocarbon series12 who found complications in 42% of their cases. We did not expect to see an improvement in complications as the surgical approach remained the same. Complications are mostly related to surgical approach rather than implant as it is related to soft tissue (especially the extensor mechanism) problems.10,11,15 This explains why stiffness and swan neck deformities were the most common complications. The volar approach leaves the extensor mechanism undisturbed, but can potentially lead to bow stringing and fixed flexion deformities.10,14 The lateral approach gives the best preservation of tendinous structures, but violates the lateral ligaments and makes preparing the canal more difficult, which can lead to subsequent malalignment.10,14 The dorsal approach violates the extensor mechanism, but gives the best exposure.10,14 We continued to use the dorsal approach, as it is the approach the senior author is the most familiar with. Murray et al14 also noted the best long-term survival through the dorsal approach.
Subsidence in our series was seen in 26% of joints, which is an improvement when compared with McGuire et al who noticed subsidence in 40% of joints. They did not see a correlation between subsidence and range of motion and regarded the subsidence as settling into a stable position.12 This is in contrast to what we found. The group with subsidence had a statistically significant decrease in arc of motion (P = .003) as well as satisfaction score (P = .001).
Our minimum follow-up of 12 months is similar to McGuire et al.12 With pyrocarbon implants, it is thought that subsidence and settling occurs within the first 12 months. The reason for changing to a cemented implant was to avoid subsidence as other authors9,10 who have used cemented implants noted very little to no subsidence. The subsidence we noticed therefore probably represents early failure rather than just subsidence, which would explain the poor range of motion and satisfaction scores in this group.
Other authors, Amirtharajah et al, showed significant subsidence with cemented implants. In their retrospective review of 18 SR-PIP joints, which were all cemented, 7 of the 11 patients (64%) with serial radiographs at 1-year follow-up showed signs of subsidence.4 Many other authors showed very little subsidence with cemented implants.
Jennings and Livingstone compared cemented with uncemented implants. Two of the 45 (4%) cemented components loosened and 16 of the 41 (39%) of the uncemented components loosened. Eleven (26%) of their joints were revised, of which most were due to loosening. All of these were uncemented.7
Johnstone et al performed a retrospective review comparing cemented with uncemented surface replacement implants. They noted subsidence in only 4% of the cemented group (n = 24) and in 68% of the uncemented group (n = 19).9
In a long-term follow-up (average 8.8 years) by Murray et al of 67 joints (SR-PIP implant), a radiolucency was noted in 12% of joints and frank loosening in only 1 joint. They found no difference between cemented and uncemented implants in terms of failure but found better functional outcomes in the cemented group.14
Our numbers are too small to draw meaningful conclusions regarding the longevity of arthroplasty in the index and middle fingers, but of the 9 joints with subsidence, 7 were in either the index finger or middle finger. Murray et al14 did not see a higher failure rate in the index or middle finger, and Luther et al in a series of uncemented implants still recommends PIPJ replacements for the index and middle finger.11
The major weakness is that this is a retrospective review and therefore our follow-up is not complete in all patients. A further factor which effected our follow-up is some patients live far away which limited our ability to obtain complete follow-up. We still managed to achieve our goal of comparing this group of patients with our unit’s previous series of pyrocarbon implants12 and showed less subsidence and less complications. It also shows that the good results obtained by other authors are not always reproducible by all surgeons.
In 2014, Amadio2 said that he PIPJ constantly challenges the hand surgeon, but “progress is clearly being made. But it seems that we can expect future episodes in the ongoing saga of the PIPJ in future editions of this report.”
Even once the perfect prosthesis has been found, soft tissue balance around the PIPJ will still remain a major challenge.
Conclusion
The change from pyrocarbon to cemented Co-Cr on UHMWPE has resulted in satisfied patients with a significant improvement in range of motion. It has resulted in less complications and a decrease in the number of joints with subsidence. The rate of subsidence, however, is still high and work will continue in an attempt to improve this.
Footnotes
Ethical Approval: This research was approved by the University of Cape Town Department of Surgery Research committee (2014/032) and the University of Cape Town Faculty of Health Sciences Ethics Committee (HREC/REF: 325/2014).
Statement of Human and Animal Rights: This study adheres to the Declaration of the Helsinki, 2013 version.
Statement of Informed Consent: No personal identifiable patient information was used in this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Adams J, Ryall C, Pandyan A, et al. Proximal interphalangeal joint replacement in patients with arthritis of the hand: a meta-analysis. J Bone Joint Surg Br. 2012;94(10):1305-1312. doi: 10.1302/0301-620X.94B10.29035. [DOI] [PubMed] [Google Scholar]
- 2. Amadio PC. Specialty update—what’s new in hand surgery. J Bone Joint Surg Br. 2014;96(6):522-526. doi: 10.1016/S0021-9355(14)74112-8. [DOI] [PubMed] [Google Scholar]
- 3. Amadio PC. What’s new in hand surgery. J Bone Joint Surg Br. 2010;92(3):783-789. doi: 10.2106/JBJS.I.01620. [DOI] [PubMed] [Google Scholar]
- 4. Amirtharajah M, Fufa D, Lightdale N, et al. Conical, radiographic, and patient-reported results of surface replacing proximal interphalangeal joint arthroplasty of the hand. Iowa Orthop J. 2011;31:140-144. [PMC free article] [PubMed] [Google Scholar]
- 5. Chan K, Ayeni O, McKnight L, et al. Pyrocarbon versus silicone proximal interphalangeal joint arthroplasty: a systematic review. Plast Reconstr Surg. 2013;131(1):114-124. doi: 10.1097/PRS.0b013e3182729f27. [DOI] [PubMed] [Google Scholar]
- 6. Herren DB, Keuchel T, Marks M, et al. Revision arthroplasty for failed silicone proximal interphalangeal joint arthroplasty: indications and 8-year results. J Hand Surg Am. 2014;39(3):462-466. doi: 10.1016/j.jhsa.2013.11.035. [DOI] [PubMed] [Google Scholar]
- 7. Jennings CD, Livingstone DP. Surface replacement arthroplasty of the proximal interphalangeal joint using the PIP-SRA implant: results, complications, and revisions. J Hand Surg Am. 2008;33(9):1-11. doi: 10.1016/j.jhsa.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 8. Johnstone BR. Proximal interphalangeal joint surface replacement arthroplasty. Hand Surg. 2001;6(1):1-11. http://www.ncbi.nlm.nih.gov/pubmed/11677661. [DOI] [PubMed] [Google Scholar]
- 9. Johnstone BR, Fitzgerald M, Smith KR, et al. Cemented versus uncemented surface replacement arthroplasty of the proximal interphalangeal joint with a mean 5-year follow-up. J Hand Surg Am. 2008;33(5):726-732. doi: 10.1016/j.jhsa.2008.01.030. [DOI] [PubMed] [Google Scholar]
- 10. Linscheid RL, Murray PM, Vidal MA, et al. Development of a surface replacement arthroplasty for proximal interphalangeal joints. J Hand Surg Am. 1997;22(2):286-298. doi: 10.1016/S0363-5023(97)80165-7. [DOI] [PubMed] [Google Scholar]
- 11. Luther C, Germann G, Sauerbier M. Proximal interphalangeal joint replacement with surface replacement arthroplasty (SR-PIP): functional results and complications. Hand. 2010;5(3):233-240. doi: 10.1007/s11552-009-9246-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McGuire DT, White CD, Carter SL, et al. Pyrocarbon proximal interphalangeal joint arthroplasty: outcomes of a cohort study. J Hand Surg Eur Vol. 2012;37(6):490-496. doi: 10.1177/1753193411434053. [DOI] [PubMed] [Google Scholar]
- 13. Murray PM. Perspectives on modern orthopaedics new-generation implant arthroplasties of the finger joints. J Am Acad Orthop Surg 2003; 11(5):295-301. [DOI] [PubMed] [Google Scholar]
- 14. Murray PM, Linscheid RL, Cooney WP, et al. Long-term outcomes of proximal interphalangeal joint surface replacement arthroplasty. J Bone Joint Surg Am. 2012;94(12):1120-1128. doi: 10.2106/JBJS.J.01375. [DOI] [PubMed] [Google Scholar]
- 15. Pritsch T, Rizzo M. Reoperations following proximal interphalangeal joint nonconstrained arthroplasties. J Hand Surg Am. 2011;36(9):1460-1466. doi: 10.1016/j.jhsa.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 16. Sweets TM, Stern PJ. Proximal interphalangeal joint prosthetic arthroplasty. J Hand Surg Am. 2010;35(7):1190-1193. doi: 10.1016/j.jhsa.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 17. Sweets TM, Stern PJ. Pyrolytic carbon resurfacing arthroplasty for osteoarthritis of the proximal interphalangeal joint of the finger. J Bone Joint Surg Am. 2011;93(15):1417-1425. doi: 10.2106/JBJS.J.00832. [DOI] [PubMed] [Google Scholar]