Abstract
Purpose
This study aimed to evaluate the efficacy and safety of intratumoral IL-12 gene therapy in an HCC-hu-PBL-NOD/SCID mouse model.
Materials and methods
The HCC murine model was generated in NOD/SCID mice, and mice with grafted tumors were injected intraperitoneally with 2 × 107 human peripheral blood lymphocytes 14 days after modeling. After 4 days, mice were randomly divided into the 9597/IL-12 group, the 9597/plasmid group and the PBS group. The changes of tumor volume were measured and mouse peripheral blood was sampled post-treatment for ELISA and CBA analyses, and the grafted tumors were collected 28 days post-treatment for immunohistochemistry, ELISA, CBA and detection of cell cycle and apoptosis.
Results
The tumor volume was smaller in the 9597/IL-12 group than in the 9597/plasmid and PBS groups on days 7, 14, 21, and 28 post-treatment (P < 0.05). Higher IL-12 levels were detected in the peripheral blood and the supernatants of grafted tumor homogenates in the 9597/IL-12 group than in the 9597/plasmid and PBS groups 7, 14, 21 and 28 days post-treatment (P < 0.05). IHC revealed higher counts of CD3+T cells, CD4+T helper cells, IFN-γ Th1 cells+ and S-100 protein positive dentric cells and lower MVD in the 9597/IL-12 group than in the 9597/plasmid and PBS groups (P < 0.05). Flow cytometry showed a significantly higher proportion of HCC cells at the G0/G1 phase and a significantly lower proportion of HCC cells at the S phase in the 9597/IL-12 group than in the PBS group (P < 0.05) and a greater apoptotic rate of HCC cells in the 9597/IL-12 group than in the 9597/plasmid and PBS groups (P < 0.05).
Conclusion
Intratumoral IL-12 gene therapy may inhibit tumorigenesis with mild adverse effects in a HCC-hu-PBL-NOD/SCID murine model through inhibiting angiogenesis, arresting cells in G0/G1 phase and inducing apoptosis.
Keywords: hepatocellular carcinoma, IL-12, gene therapy, efficacy, toxicity
Introduction
Liver cancer is the fourth most common cancer and the second leading cause of cancer-related deaths in the world.1 Hepatocellular carcinoma (HCC), the most common histologic type of liver cancer, consists of over 80% of total malignancies and is characterized by rapid progression, high metastasis and recurrence, and poor prognosis.2,3 Currently, the therapy of HCC mainly includes surgical resection, chemotherapy, and radiotherapy.4–6 However, most HCC patients are at a middle or late stage upon diagnosis, resulting in loss of timing for surgery, chemotherapy, and radiotherapy.7–9 Liver transplantation has been accepted as the most beneficial option for the treatment of unresectable HCC; however, high costs and huge shortage of donors greatly limit its clinical application.10–12 Transcatheter arterial chemoembolization (TACE) and ablations have been reported to be effective to improve the survival for unresectable HCC; however, there are still problems limiting the long-term treatment outcomes.13–15 It is estimated that the 5-year overall survival rate is less than 5% in patients with advanced HCC.2
Since HCC has been considered as an immunogenic tumor, immunotherapy has shown potential for the treatment of HCC.16–18 The immunotherapy for HCC mainly includes non-specific and specific approaches.19 Non-specific immunotherapy is infusion of cytokines such as interleukin (IL)-2, interferon gamma (IFN-γ) and tumor necrosis factor (TNF), or immunocompetent cells like cytokine-induced killer (CIK) cells, lymphokine-activated killer (LAK) cells and tumor-infiltrating lymphocyte (TIL), to enhance the non-specific immune responses against HCC,20 while specific immunotherapy is vaccination of tumor vaccines or α-fetoprotein (AFP)-based polypeptide vaccines to activate specific immune responses against HCC.21 However, injection of cytokines may induce severe adverse events, infusion of immunocompetent cells requires multiple treatments, and the clinical efficacy of tumor and polypeptide vaccines remains unstable; these problems greatly limit the applicability of immunotherapy for HCC.22–24
In this study, we established an HCC-hu-PBL-nonobese diabetic/severe combined immunodeficiency (NOD/SCID) mouse model to mimic the human HCC microenvironment, and evaluated the efficacy and safety of intratumoral IL-12 gene therapy for HCC in this model.
Materials And Methods
Ethical Statement
This study was approved by the Ethics Review Committee of Fujian Cancer Hospital (permission number: B-201308). All animal experiments were performed in accordance with the international and national guidelines for laboratory animal care and management.
Animals
Female NOD/SCID mice at 4 to 6 weeks of age, each weighing 18 to 20 g, were purchased from Shanghai SLAC Laboratory Animal Company (Shanghai, China) and maintained in the Laboratory Animal Center of Fujian Medical University (Fuzhou, China) at a temperature of 20 to 25°C, relative humidity of 50% to 55% in a 12 h-light/12 h-dark cycle. All mice were given free access to clean water and food.
Cell Lines And Culture
The human HCC HepG2 cell line was purchased from the Cell Bank of Chinese Academy of Sciences (Shanghai, China) and maintained in the Laboratory of Immuno-Oncology, Fujian Medical University Cancer Hospital (Fuzhou, China). The 9597/IL-12 and 9597/plasmid cell lines were kindly presented by Dr. Xin Lin from The University of Texas MD Anderson Cancer Center (Houston, TX, USA). To construct the expression plasmid Pcmv-IL-12neo, the genes encoding human IL-12 p35 and p40 subunits were isolated and cloned into the mammalian expression vector. The 9597/IL-12 cell line was generated by transfection of human IL-12 gene into the human lung carcinoma 9597 cell line, and the 9597/plasmid cell line was generated by transfection of a blank plasmid into the 9597 cell line. Cells were cultured in DMEM (Invitrogen; Carlsbad, CA, USA) supplemented with 10% fetal bovine serum (FBS; Invitrogen; Carlsbad, CA, USA) at 37°C, in a 100% humidity incubator containing 5% CO2.
Establishment Of A HCC-Hu-PBL-NOD/SCID Model And IL-12 Gene Therapy
Six NOD/SCID mice were injected subcutaneously in the armpit with 1 × 107 HepG2 cells which were mixed with equal volumes of Matrigel matrix (BD Biosciences; San Jose, CA, USA). After 14 days of subcutaneous injection of HepG2 cells, five of the mice with grafted tumors were injected intraperitoneally with 2 × 107 human peripheral blood lymphocytes from healthy populations, and one mouse was injected with PBS as a control. After 4 weeks, all mice were sacrificed, and the grafted tumors were isolated for the subsequent assays.
The HCC mouse model was generated as above. On day 14 post-infection with HepG2 cells, 30 mice were injected intraperitoneally with 2 × 107 peripheral blood lymphocytes from healthy populations. After 4 days, mice were randomly grouped, of 10 mice in each group. Mice in the 9597/IL-12 group were injected intratumorally with lethally irradiated (27 Gy) 1 × 107 9597/IL-12 cells on days 1, 4 and 7, and animals in the 9597/plasmid group were given intratumoral injection with lethally irradiated (27 Gy) 1 × 107 9597/plasmid cells on days 1, 4 and 7, while mice in the PBS group were injected with PBS at the same time points.
Following injection, the changes of tumor volume were measured with calipers and calculated using the formula: (a × b2)/2, where a indicated the length of the tumor and b indicated the width. The body weight was measured and general conditions were observed. Mouse peripheral blood was sampled on days 1, 7, 14 and 21 from the tail and on day 28 from the orbit. On day 28, the mice were sacrificed and the tumors were isolated. A part of each tumor was fixed in formalin and 1.0 mg of tissue was suspended in homogenization with 4 mL of PBS. Then, 5 µL of the supernatant was collected after centrifugation to detect cytokines.
Immunohistochemistry (IHC)
Fixed tumor specimens were stained with hematoxylin and eosin (HE) for routine histological analysis. To investigate the tumor microenvironment, tumor specimens were incubated with rabbit anti-human CD3 (1:500; Maixin Biotechnology Development Company, Fuzhou, China), CD4 (1:500; Maixin Biotechnology Development Company, Fuzhou, China), CD8 (1:500; Maixin Biotechnology Development Company, Fuzhou, China), IFN-γ(1:500; Santa Cruz Biotechnology Company, Dallas, TX, USA) and S-100monoclonal antibodies (1:500; Maixin Biotechnology Development Company, Fuzhou, China), and rabbit anti-human CD20 (1:500; Maixin Biotechnology Development Company, Fuzhou, China), CD57 (1:500; Maixin Biotechnology Development Company, Fuzhou, China), CD68 (1:500; Maixin Biotechnology Development Company, Fuzhou, China) and IL-4 monoclonal antibodies (1:500; Santa Cruz Biotechnology Company, Dallas, TX, USA) for immunohistochemical analysis using the Ultrasensitive S-P kit (Maixin Biotechnology Development Company; Fuzhou, China) following the manufacturer’s instructions. Positively stained cells were counted in ten fields of vision at a magnification of 400 × and the mean cell count per high power field (HPF) was measured. In addition, the vascular endothelial cells were stained with rabbit anti-human VEGF monoclonal antibody (1:500; Santa Cruz Biotechnology Company, Dallas, TX, USA) to measure the microvessel density (MVD).
Enzyme-Linked Immunosorbent Assay (ELISA)
IL-12 expression was measured in the mouse peripheral blood and the homogenates from fresh tumor specimens using the high-sensitivity ELISA kit for human IL-12 (R & D Company; Minneapolis, MN, USA, and the alanine aminotransferase (ALT) and aspartate aminotransferase (AST) concentrations were measured in the mouse peripheral blood with the ELISA kits for murine ALT and AST (USCN Life Science, Inc.; Wuhan, China).
Cytometric Bead Array (CBA)
The levels of Th1, Th2 and Th17 cytokines, including IL-2, IL-4, IL-6, IL-10, TNF-α, IFN-γ and IL-17A, were measured in the peripheral blood and the supernatants of tumor homogenates with the Cytometric Bead Array for human Th1/Th2/Th17 cytokine kit (BD Biotechnology Company; San Jose, CA, USA) according to the manufacturer’s protocol.
Detection Of Apoptosis And Cell Cycle
After the fresh tumor homogenates were centrifuged, the supernatants were used to detect cytokines, and the precipitated cells were retained to analyze apoptosis and cell cycle. Some of the precipitants were re-suspended with the Binding Buffer in the ANNEXIN V apoptosis detection kit (BD Biotechnology Company; San Jose, CA, USA) at a concentration of 1 × 106 cells/mL, and the others were re-suspended with PBS at a concentration of 5 × 106 cells/mL. Then, 100 µL of homogenates were sampled to analyze apoptosis using the ANNEXIN V apoptosis detection kit and analyze the cell cycle using the Cell Cycle Test Plus kit (BD Biotechnology Company; San Jose, CA, USA) following the manufacturer’s guidelines.
Statistical Analysis
All data were processed using Microsoft Excel 2010 (Microsoft; Redmond, WA, USA), and all statistical analyses were performed using the software SPSS version 17.0 (SPSS, Inc.; Chicago, IL, USA). The differences of means for each variable were compared using one-way analysis of variance (ANOVA), followed by the least significant difference (LSD) Pairwise comparison t-test. A P value of < 0.05 was considered statistically significant.
Results
Identification Of The HCC-Hu-PBL-NOD/SCID Murine Model
Tumors developed in all NOD/SCID mice following subcutaneous injection of HepG2 cells, and the mean tumor volumes were 61.91 ± 31.38 and 278.71 ± 92.81 mm3 7 and 14 days post-infection. Following intraperitoneal injection of human peripheral blood lymphocytes, tumors continued to grow in NOD/SCID mice, and the mean tumor volumes were 275.77 ± 130.1, 355 ± 210.18, 602.63 ± 527.98 and 1024.75 ± 808.2 mm3 7, 14, 21 and 28 days post- injection.
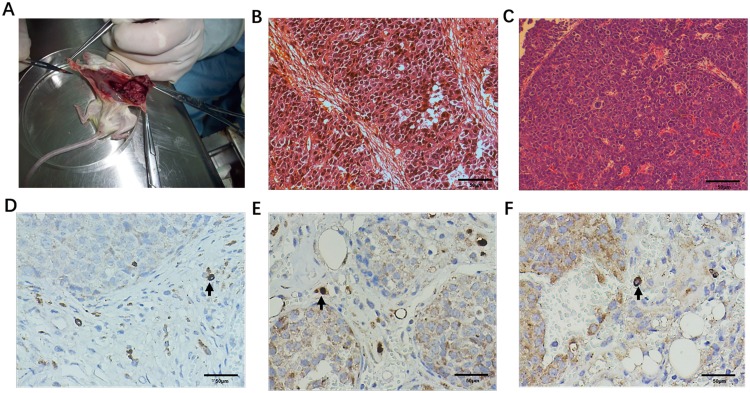
Mice were sacrificed 28 days following intraperitoneal injection with human peripheral blood lymphocytes, and the grafted tumors were sampled. The tumors appeared a lobulated shape and dark red and greyish yellow, and the tumor surface had intact capsules wrapped with fibrous tissues, which was infiltrated with mouse blood vessels (Figure 1A). HE staining showed that the HCC cells showed distinct architectural atypia, and grew in nests or nodules with internal blood sinus-like architecture and surrounding fibrous interstitium (Figure 1B and C). Cellular atypia was also seen as was heterogeneous size, huge nuclei, and even pathologic mitotic figures (Figure 1C). These tumor architectures and morphologic features of cancer cells are similar to those of human HCC. However, no metastasis of HCC to the liver, lung or spleen was observed.
Figure 1.
Identification of the HCC-hu-PBL-NOD/SCID murine model.(A) The tumors appear a lobulated shape and dark red and greyish yellow, and the tumor surface has intact capsules wrapped with fibrous tissues, which is infiltrated with mouse blood vessels; (B) HE staining shows that the HCC cells show distinct architectural atypia, and grow in nests or nodules with internal blood sinus-like architecture and surrounding fibrous interstitium (scale bar = 50 μm); (C) HE staining shows cellular atypia, heterogeneous size, huge nuclei, and even pathologic mitotic figures in HCC cells (scale bar = 50 μm); (D) IHC detects infiltration of human peripheral blood CD3+ lymphocytes (black arrow) in the grafted tumors (scale bar = 50 μm); (E) IHC detects infiltration of human peripheral blood CD4+ lymphocytes (black arrow) in the grafted tumors (scale bar = 50 μm); (F) IHC detects infiltration of human peripheral blood CD8+ lymphocytes (black arrow) in the grafted tumors (scale bar = 50 μm), positive cell.
To evaluate the infiltration of human peripheral blood lymphocytes in grafted tumors sampled from mice receiving intraperitoneal injection with human peripheral blood lymphocytes, CD3+, CD4+ and CD8+ T lymphocytes expression was detected in grafted tumors using IHC, and the mean count of CD3+, CD4+ and CD8+ T lymphocytes was 5.63 ± 3.48, 3.21 ± 2.83 and 1.18 ± 2.2 cells/HPF, respectively (Figure 1D–F). These infiltrated T lymphocytes were mainly dispersed throughout the grafted tumor interstitium.
Intratumoral 9597/IL-12 Cell Injection Inhibited HCC Growth
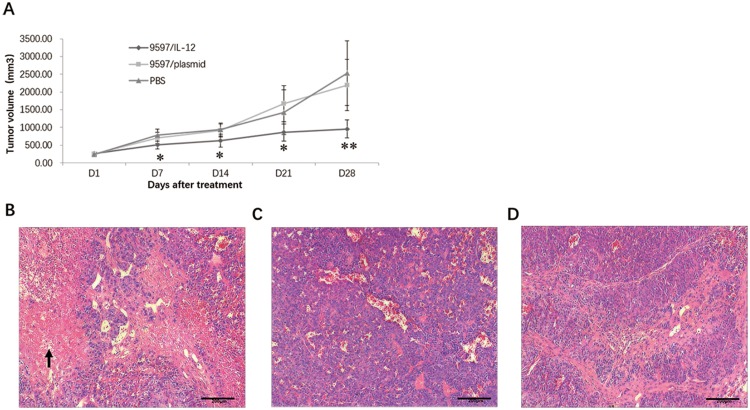
The HCC-hu-PBL-NOD/SCID murine model was generated to evaluate the in vivo activity of IL-12 gene therapy against HCC. The tumor volume was smaller in the 9597/IL-12 group than in the 9597/plasmid and PBS groups on days 7, 14, 21, and 28 post-treatment (P < 0.05) (Figure 2A).
Figure 2.
Intratumoral 9597/IL-12 cell injection inhibits HCC growth. (A) The tumor volume is smaller in the 9597/IL-12 group than in the 9597/plasmid and PBS groups on days 7, 14, 21, and 28 post-treatment; (B) HE staining shows infiltration of plenty of inflammatory cells in the grafted tumor interstitium with tissue necrosis in the 9597/IL-12 group, and the arrows indicate the necrotic tissues (scale bar = 200 μm); (C) HE staining shows lower degree of inflammatory cells infiltration and tissue necrosis in the 9597/plasmid than in the 9597/IL-12 group (scale bar = 200 μm); (D) HE staining shows lower degree of inflammatory cells infiltration and tissue necrosis in the PBS group than in the 9597/IL-12 group (scale bar = 200 μm). *P < 0.05; **P < 0.01.
HE staining showed infiltration of plenty of inflammatory cells in the grafted tumor interstitium with tissue necrosis in the 9597/IL-12 group (Figure 2B), and the degree of inflammatory cells infiltration and tissue necrosis was lower in the 9597/plasmid and PBS groups than in the 9597/IL-12 group (Figure 2C and 2D).
Toxicity Of Intratumoral 9597/IL-12 Cell Injection
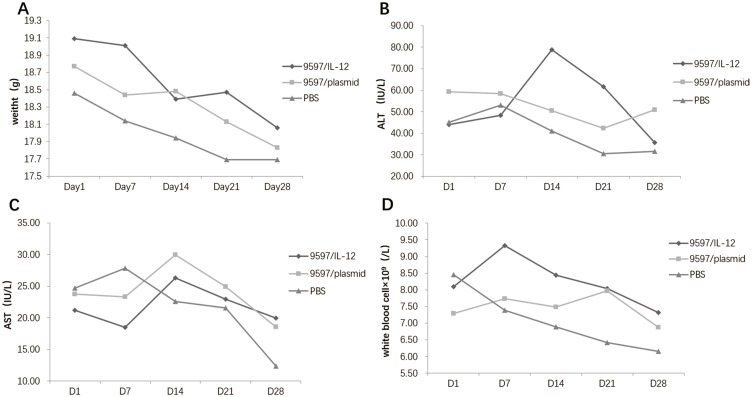
During the 28-day observation period, all mice had normal behaviors, normal diet and shiny coats. Sporadic mild diarrhea appeared in the 9597/IL-12 and 9597/plasmid groups 4 days post-treatment and completely disappeared 21 days post-treatment, while no abnormal stool was found in the PBS group.
The mouse body weight appeared a tendency towards a decline in all three groups, and there was no significant difference in the mouse body weight among the three groups over the study period (Figure 3A).
Figure 3.
Toxicity of intratumoral 9597/IL-12 cell injection. (A) The mouse body weight appears a tendency towards a decline in all three groups, and there is no significant difference in the mouse body weight among the three groups over the study period; (B) Higher ALT concentrations are measured in the 9597/IL-12 group than in the 9597/plasmid and PBS groups 14 and 21 days post-treatment; (C) There is no significant difference in the serum AST concentration among the three groups during the study period; (D) Greater peripheral white blood cell counts are measured in the 9597/IL-12 group than in the 9597/plasmid and PBS groups 7 days post-treatment.
The serum ALT activity peaked in the 9597/IL-12 group 14 days post-treatment, and then gradually reduced and returned to normal 28 days post-treatment. Higher ALT concentrations were measured in the 9597/IL-12 group than in the 9597/plasmid and PBS groups 14 and 21 days post-treatment (P < 0.05), while a lower ALT level was seen in the 9597/IL-12 group than in the 9597/plasmid group 28 days post-treatment (P < 0.05) (Figure 3B). During the study period, there was no significant difference in the serum AST concentration among the three groups (P > 0.05) (Figure 3C).
The peripheral white blood cell counts peaked in the 9597/IL-12 group 7 days post-treatment and then gradually reduced, while a continuous decline was seen in the white blood cell counts in the PBS group across the study period. Greater white blood cell counts were measured in the 9597/IL-12 group than in the 9597/plasmid and PBS groups 7 days post-treatment, and higher white blood cell counts were found in the 9597/IL-12 group than in the PBS group 21 days post-treatment (Figure 3D).
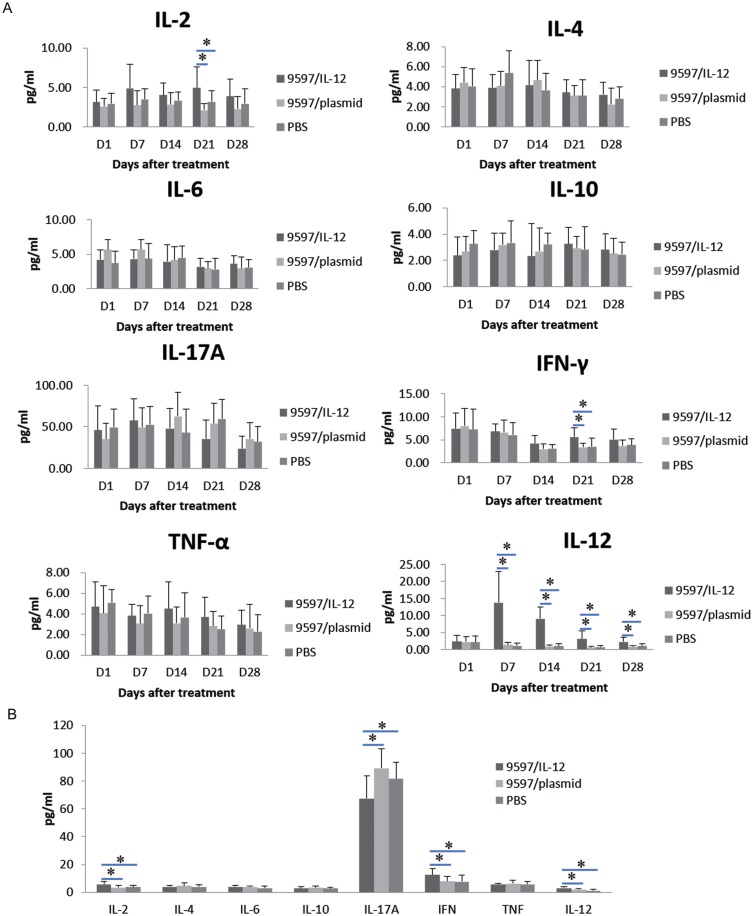
Changes Of Cytokines In Mouse Peripheral Blood And Supernatants Of Tumor Homogenates
The IL-12 concentration peaked in the peripheral blood in the 9597/IL-12 group 7 days-treatment, and then gradually reduced. Higher IL-12 levels were detected in the peripheral blood in the 9597/IL-12 group than in the 9597/plasmid and PBS groups 7, 14, 21 and 28 days post-treatment (P < 0.05), and greater IL-2 and IFN-γ levels were found in the 9597/IL-12 group than in the 9597/plasmid and PBS groups 21 days post-treatment (P < 0.05), while no significant differences were observed in terms of IL-4, IL-6, IL-10, IL-17A or TNF-α levels in the peripheral blood among the three groups across the study period (P > 0.05) (Figure 4A). In addition, higher IL-2, IL-12, and IFN-γ concentrations were detected in the supernatants of grafted tumor homogenates in the 9597/IL-12 group than in the 9597/plasmid and PBS groups (P < 0.05), and a significant lower IL-17A level was seen in the 9597/IL-12 group than in the 9597/plasmid and PBS groups (P < 0.05), while no significant differences were seen in IL-4, IL-6, IL-10 or TNF levels among the three groups (P > 0.05) (Figure 4B).
Figure 4.
Changes of cytokines in mouse peripheral blood and supernatants of tumor homogenates. (A) Changes of cytokine levels in mouse peripheral blood 7, 14, 21 and 28 days post-treatment; (B) Changes of cytokine levels in mouse supernatants of tumor homogenates post-treatment. *P < 0.05.
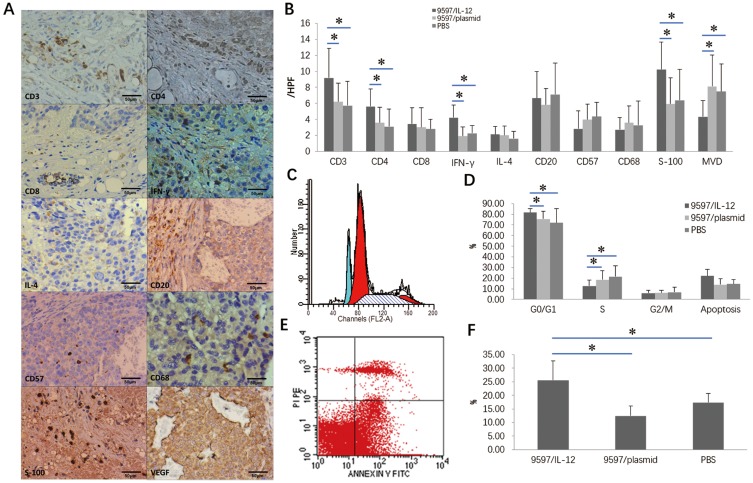
Intratumoral 9597/IL-12 Cell Injection Altered Tumor Microenvironments, Cell Cycle And Apoptosis
The grafted tumors were isolated 28 days post-treatment and subjected to IHC for detection of tumor microenvironments. IHC revealed higher counts of CD3+T cells, CD4+T helper cells, IFN-γ Th1 cells+ and S-100 protein positive dentric cells (DCs) in the 9597/IL-12 group than in the 9597/plasmid and PBS groups (P < 0.05), and the MVD was significantly lower in the 9597/IL-12 group than in the 9597/plasmid and PBS groups (P < 0.05) (Figure 5A and B).
Figure 5.
Intratumoral 9597/IL-12 cell injection altered tumor microenvironments, cell cycle and apoptosis. (A) IHC detects expression of CD3+T cells, CD4+T helper cells, IFN-γ Th1 cells+ and S-100 protein positive DCs and MVD in tumor microenvironments (scale bar = 50 μm); (B) higher counts of CD3+T cells, CD4+T helper cells, IFN-γ Th1 cells+ and S-100 protein positive dentric cells (DCs) in the 9597/IL-12 group than in the 9597/plasmid and PBS groups, and the MVD was significantly lower in the 9597/IL-12 group than in the 9597/plasmid and PBS groups; (C) Flow cytometry detects cell cycle in tumor microenvironments; (D) A significantly higher proportion of HCC cells at the G0/G1 phase and a significantly lower proportion of HCC cells at the S phase are seen in the 9597/IL-12 group than in the PBS group, and no significant difference is detected in the proportion of HCC cells at the G2/M phase among the three groups; (E) Flow cytometry detects cell apoptosis in tumor microenvironments; (F) A greater apoptotic rate of HCC cells is determined in the 9597/IL-12 group than in the 9597/plasmid and PBS groups. *P < 0.05.
Flow cytometry showed a significantly higher proportion of HCC cells at the G0/G1 phase and a significantly lower proportion of HCC cells at the S phase in the 9597/IL-12 group than in the PBS group (P < 0.05), while no significant difference was detected in the proportion of HCC cells at the G2/M phase among the three groups (Figure 5C and D). In addition, a greater apoptotic rate of HCC cells was determined in the 9597/IL-12 group than in the 9597/plasmid and PBS groups (P < 0.05) (Figure 5E and F).
Discussion
Currently, xenograft models through transplantation of human or murine cancer cell lines into mice, such as murine H22, human HepG2, BEL-7402, and SMMC-7221 cells,25–27 are a predominant tool in oncology research.28,29 Since mice lack human immune cells, the murine xenograft model cannot completely recapitulate the state of in situ human HCC.27 Transplanting human lymphocytes into immunodeficient mice can establish a humanized mouse model with a simulated, but limited human immune system, to evaluate the effect of immunotherapy.30,31 Humanized mouse models can be generated by transplanting human peripheral blood lymphocytes (hu-PBL mouse model), or human embryonic hematopoietic tissues into mice (mice-hu-model),30,31 and the hu-PBL mouse model is more convenient to be generated because human peripheral blood lymphocytes are easily harvested.32
In this study, the HCC-hu-PBL-NOD/SCID murine model was generated by injecting human peripheral blood lymphocytes into the grafted tumors derived from HepG2 cells in mice, to mimic the human HCC microenvironment. IHC showed that CD3+, CD4+ and CD8+ T lymphocytes were dispersed throughout the grafted tumor interstitium, and CBA detected T lymphocytes in the supernatants of grafted tumor homogenates, suggesting the transfected peripheral blood lymphocytes remain to survive and function in the grafted tumors.
IL-12, a member of the larger family of IL-12-related cytokines, is a heterodimeric cytokine that is produced by natural killer (NK) cells, T cells, dendritic cells (DCs), and macrophages.33 Firstly discovered from an Epstein-Barr virus-transformed B lymphoblastoid RPMI 8866 cell line as “NK cell stimulatory factor” in 1989,34 IL-12 has been identified as a cytokine with important regulatory functions that bridges innate and adaptive immunity, and has been proposed as an immune adjuvant for immunotherapy in infectious diseases and malignancies.35
In a phase I dose escalation trial to determine the potential antineoplastic effects of intravenous administration of recombinant human IL-12 (rhIL-12), there was a partial response (renal cell cancer) and a transient complete response (melanoma) in previously untreated patients, and four additional patients received all proposed treatment without disease progression.36 In a phase I trial to evaluate the efficacy and safety of rhIL-12 at an escalating dose for the treatment of advanced renal cell carcinoma, of all treatment regimens, the best treatment regimen achieved complete response in a case, stable progression in 34 cases, progression in 14 cases and an inevaluable case.37 In a phase I dose escalation trial to assess the efficacy and adverse effects of subcutaneous or intralesional administration of rhIL-12 for 10 cutaneous T-cell lymphoma patients, including 5 with extensive plaque, 3 with Sezary syndrome, and 2 with extensive tumors with large cell transformation, subcutaneous dosing resulted in complete responses in 2 of 5 plaque, partial responses in 2 of 5 plaque, 1 of 2 Sezary syndrome, and a minor response in 1 of 5 plaque patients, and intralesional dosing resulted in individual tumor regression in 2 of 2 patients.38 Results from a randomized phase II study to compare the efficacy of rhIL-12 versus interferon-alpha (IFN-alpha) for patients with previously untreated, advanced renal cell cancer showed a partial response in 7% of 30 patients treated with rhIL-12.39 In phase II study to evaluate the activity and toxicity of intravenous rhIL-12 administration for patients with recurrent or refractory epithelial ovarian cancer that failed first-line platinum-based chemotherapy regimen, no complete response was achieved; however, 3.8% of the subjects achieved a partial response and 50% had a stable disease.40 Among 29 previously treated patients with peritoneal carcinomatosis from Müllerian carcinomas, gastrointestinal tract carcinomas and peritoneal mesothelioma, weekly intraperitoneal rhIL-12 injection resulted in no remaining disease in a case with ovarian cancer and a case with mesothelioma at laparoscopy, stable disease in 8 cases and progressive disease in 19 cases.41 In addition, results from clinical trials also showed activity of rhIL-12 administration against head and neck squamous cell carcinoma,42 advanced cervical cancer,43 recurrent superficial transitional cell carcinoma of the bladder,44 advanced digestive tumors,45 relapsed and refractory non-Hodgkin’s lymphoma and Hodgkin’s disease46 and plateau phase multiple myeloma.47 However, rhIL-12 therapy may cause adverse events, such as chills, fever, fatigue, nausea, vomiting, headache, anemia, neutropenia, lymphopenia, abnormal liver function, and even death,48 and the antitumor activity of IL-12 was found to be dose-dependent.49 Since IL-12 is rapidly metabolized in the body,33 attempts have been made to increase the dose to increase the titer in the tumor, but this contributes to more serious adverse reactions, even death,36–38 which limits the clinical utilization of IL-12.
Currently, vectors used for a delivery system involve IL-12 gene containing plasmids or virus and transfection of normal or abnormal human cells like DC, fibroblasts, or tumor cells,50–53 Intratumoral administration of electroporation-mediated mouse IL-12 gene therapy elevated serum IL-12 and IFN-γ, significantly inhibited the growth not only of HCC into which the mIL-12 vector had been directly transferred, but also of the distant HCC, suppressed spontaneous lung metastasis, delayed establishment of HCC injected 3 days after electroporation-mediated mouse IL-12 gene therapy, induced more lymphocyte infiltration by NK cells, CD3+ cells, and Mac-1-positive cells into the tumor and reduced the number of microvessels.54 Intramuscular injection of 10 μg IL-12 DNA plasmid followed by electroporation prevented the establishment of squamous cell carcinoma tumor in 40% of experimental animals and reduced the volume of established tumors by 75% compared to controls (P < 0.05).55 In addition, injection of autologous or allogeneic fibroblasts engineered IL-12 efficiently eliminated or suppressed the growth of the MCA207 sarcoma in a dose-dependent manner, and IL-12 delivery by fibroblasts significantly reduced the 7-day established lung metastases of MCA102 and MC38 sarcoma, suggesting that IL-12-engineered fibroblasts seem to serve as a safe and efficient means to deliver IL-12 in these three tumor models.56 Recently, cationic polyphosphazene vesicles57 and the nanoparticle MPEG-PLA and DOTAP with zeta-potential value of 38.5 mV and size of 37.5 nm58 have been proved to be an efficient delivery system for IL-12 immunotherapy for cancers.
Since IL-12 gene therapy delivered via the systemic system achieves a lower efficiency on cancer inhibition and causes more adverse events than the local delivery system,59 a delivery system that continuously secreted IL-12 into the local tumor environment was employed which exhibited a high antitumor function and minimized adverse reactions in this study. In our HCC-hu-PBL-NOD/SCID murine model, lethally irradiated 9597/IL-12 cells were injected into the tumor at multiple sites on days 1, 4, and 7, and injection of 9597/IL-12 cells caused greater suppression of tumor growth than injection of 9597/plasmid cells or PBS. During the 28-day study period, the serum IL-12 level was found to peak 7 days post-treatment in the 9597/IL-12 group, and remained detectable 28 days post-treatment. In addition, intratumoral injection of 9597/IL-12 cells caused mild diarrhea and a transient increase of ALT during the study period. Taken together, these findings suggest that intratumoral IL-12 gene therapy is effective and lowly toxic for HCC.
Previous studies have demonstrated that IL-12 is active against cancers through inducing Th0 cells to Th1 cell development to enhance the cellular immunity, promoting the proliferation of NK and T cells and the expansion of LAK and TIL populations, inducing the secretion of IFN-γ from Th1 and NK cells and NO from macrophages, inhibiting angiogenesis, enhancing the expression of MHC-I, MHC-II and the costimulatory molecule B7 to improve the sensitivity of immune cells to tumors, and increasing the tumor antigen presentation of antigen presenting cells.60,61 In our study, the counts of CD3+ T-cells, CD4+ Th cells, IFN-γ+ Th1 cells, S-100+ DCs, IL-2, IFN-γ, and IL-12 were greater in the 9597/IL-12 group than in the 9597/plasmid group and the PBS group, which was in agreement with the role of Th1 cells and DCs in antitumor responses.62,63 DCs capture and present tumor antigens to Th1 cells and then activate Th1 cells to assist the activation of CTL and induce the antitumor activity.62,63 The number of MVD in the grafted tumors was significantly lower in the 9597/IL-12 group than in the 9597/plasmid and PBS groups, suggesting that IL-12 gene therapy may inhibit angiogenesis. In addition, flow cytometry determined a higher percentage of HCC cells at the G0/G1 phase and a greater apoptotic rate of HCC cells in the 9597/IL-12 group than in the 9597/plasmid and PBS groups (P < 0.05). This is consistent with the mechanisms by which IL-12 inhibits tumor growth through arresting cells in G0/G1 phase and inducing apoptosis.60,61
Th17 T-cells are a type of helper T cells that secrete IL-17, IL-17F, IL-21, and IL-22, and IL-17 may promote inflammation by activating NF-κB and the MAPK pathway after binding receptors on target cells.63 The function of Th17 in tumorigenesis remains controversial.64,65,66 Th17 cells both promote and suppress tumor growth, and Th17 cells also exhibit a bystander function [65, 66]. Previous studies have shown that IL-17 improves tumorgenicity by promoting angiogenesis in cervical carcinoma and ovarian carcinoma,67,68 and IL-17F suppressed the growth of HCC through inhibiting angiogenesis.69 In IL-17-deficient mice, the tumor development and metastasis were promoted, suggesting that IL-17 may exhibit an antitumor activity.70 In the current study, the tumor volume was smaller in the 9597/IL-12 group than in the 9597/plasmid and PBS groups on days 7, 14, 21, and 28 post-treatment (P < 0.05), and a significant lower IL-17A level was seen in the supernatants of grafted tumor homogenates in the 9597/IL-12 group than in the 9597/plasmid and PBS groups (P < 0.05), suggesting that IL-17A promotes tumorigenesis.
In summary, the results of the present study demonstrate that intratumoral IL-12 gene therapy may inhibit tumorigenesis with mild adverse effects in a HCC-hu-PBL-NOD/SCID murine model through inhibiting angiogenesis, arresting cells in G0/G1 phase and inducing apoptosis. Our data suggest that intratumoral IL-12 gene therapy may be a promising strategy for the treatment of HCC, and further clinical trials to evaluate the safety and toxicity of intratumoral IL-12 gene therapy for HCC are warranted.
Acknowledgments
We would like to thank the staff working at the Laboratory Animal Center of Fujian Medical University for their kind help during the animal experiments. Many thanks are expressed to Dr. Xin Lin from the University of Texas MD Anderson Cancer Center for gifting us cell lines and Dr. Xiao-Bin Zheng from Fujian Medical University for her assistance during the study. We also thank Prof. Qiang Chen from Fujian Medical University for giving us valuable comments during the preparation and revision of the manuscript. This study was supported by the grants from the Fujian Provincial Department of Health (grant no. 2009-2-30), Fujian Natural Science Foundation (grant no. 2008I0012), the National Clinical Key Specialty Construction Program of China and Key Clinical Specialty Discipline Construction Program of Fujian.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. doi: 10.3322/caac.21551 [DOI] [PubMed] [Google Scholar]
- 2.Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391(10127):1301–1314. doi: 10.1016/S0140-6736(18)30010-2 [DOI] [PubMed] [Google Scholar]
- 3.Sayiner M, Golabi P, Younossi ZM. Disease burden of hepatocellular carcinoma: a global perspective. Dig Dis Sci. 2019;64(4):910–917. doi: 10.1007/s10620-019-05537-2 [DOI] [PubMed] [Google Scholar]
- 4.Song P, Cai Y, Tang H, Li C, Huang J. The clinical management of hepatocellular carcinoma worldwide: a concise review and comparison of current guidelines from 2001 to 2017. Biosci Trends. 2017;11(4):389–398. doi: 10.5582/bst.2017.01202 [DOI] [PubMed] [Google Scholar]
- 5.Daher S, Massarwa M, Benson AA, Khoury T. Current and future treatment of hepatocellular carcinoma: an updated comprehensive review. J Clin Transl Hepatol. 2018;6(1):69–78. doi: 10.14218/JCTH.2017.00031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colombo M, Sangiovanni A. Treatment of hepatocellular carcinoma: beyond international guidelines. Liver Int. 2015;35(Suppl 1):129–138. doi: 10.1111/liv.12713 [DOI] [PubMed] [Google Scholar]
- 7.Pascual S, Herrera I, Irurzun J. New advances in hepatocellular carcinoma. World J Hepatol. 2016;8(9):421–438. doi: 10.4254/wjh.v8.i9.421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liang Q, Shen X, Sun G. Precision medicine: update on diagnosis and therapeutic strategies of hepatocellular carcinoma. Curr Med Chem. 2018;25(17):1999–2008. doi: 10.2174/0929867325666180117101532 [DOI] [PubMed] [Google Scholar]
- 9.Cassinotto C, Aubé C, Dohan A. Diagnosis of hepatocellular carcinoma: an update on international guidelines. Diagn Interv Imaging. 2017;98(5):379–391. doi: 10.1016/j.diii.2017.01.014 [DOI] [PubMed] [Google Scholar]
- 10.Dageforde LA, Fowler KJ, Chapman WC. Liver transplantation for hepatocellular carcinoma: current update on treatment and allocation. Curr Opin Organ Transplant. 2017;22(2):128–134. doi: 10.1097/MOT.0000000000000385 [DOI] [PubMed] [Google Scholar]
- 11.Mancuso A, Perricone G. Hepatocellular carcinoma and liver transplantation: state of the art. J Clin Transl Hepatol. 2014;2(3):176–181. doi: 10.14218/JCTH.2014.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Rourke JM, Shetty S, Shah T, Perera MTPR. Liver transplantation for hepatocellular carcinoma: pushing the boundaries. Transl Gastroenterol Hepatol. 2019;4:1. doi: 10.21037/tgh.2019.06.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nault JC, Sutter O, Nahon P, Ganne-Carrié N, Séror O. Percutaneous treatment of hepatocellular carcinoma: state of the art and innovations. J Hepatol. 2018;68(4):783–797. doi: 10.1016/j.jhep.2017.10.004 [DOI] [PubMed] [Google Scholar]
- 14.Zhu L, Yang R, Zhu X. Transcatheter arterial chemoembolization experience for advanced hepatocellular carcinoma with right atrial tumor thrombus. J Cancer Res Ther. 2019;15(2):305–311. doi: 10.4103/jcrt.JCRT_923_17 [DOI] [PubMed] [Google Scholar]
- 15.Zhu J, Yin T, Xu Y, Lu XJ. Therapeutics for advanced hepatocellular carcinoma: recent advances, current dilemma, and future directions. J Cell Physiol. 2019;234(8):12122–12132. doi: 10.1002/jcp.28048 [DOI] [PubMed] [Google Scholar]
- 16.Buonaguro L, Mauriello A, Cavalluzzo B, Petrizzo A, Tagliamonte M. Immunotherapy in hepatocellular carcinoma. Ann Hepatol. 2019;18(2):291–297. doi: 10.1016/j.aohep.2019.04.003 [DOI] [PubMed] [Google Scholar]
- 17.Okusaka T, Ikeda M. Immunotherapy for hepatocellular carcinoma: current status and future perspectives. ESMO Open. 2018;3(Suppl 1):e000455. doi: 10.1136/esmoopen-2018-000455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tagliamonte M, Petrizzo A, Tornesello ML, Ciliberto G, Buonaguro FM, Buonaguro L. Combinatorial immunotherapy strategies for hepatocellular carcinoma. Curr Opin Immunol. 2016;39:103–113. doi: 10.1016/j.coi.2016.01.005 [DOI] [PubMed] [Google Scholar]
- 19.Longo V, Gnoni A, Casadei Gardini A, et al. Immunotherapeutic approaches for hepatocellular carcinoma. Oncotarget. 2017;8(20):33897–33910. doi: 10.18632/oncotarget.15406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang R, Zhang Z, Liu Z, et al. Adoptive cell transfer therapy for hepatocellular carcinoma. Front Med. 2019;13(1):3–11. doi: 10.1007/s11684-019-0684-x [DOI] [PubMed] [Google Scholar]
- 21.Baradaran Noveiry B, Hirbod-Mobarakeh A, Khalili N, et al. Specific immunotherapy in hepatocellular cancer: a systematic review. J Gastroenterol Hepatol. 2017;32(2):339–351. doi: 10.1111/jgh.13449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rai V, Abdo J, Alsuwaidan AN, Agrawal S, Sharma P, Agrawal DK. Cellular and molecular targets for the immunotherapy of hepatocellular carcinoma. Mol Cell Biochem. 2018;437(1–2):13–36. doi: 10.1007/s11010-017-3092-z [DOI] [PubMed] [Google Scholar]
- 23.Cheng JW, Lv Y. New progress of non-surgical treatments for hepatocellular carcinoma. Med Oncol. 2013;30(1):381. doi: 10.1007/s12032-012-0381-y [DOI] [PubMed] [Google Scholar]
- 24.Harding JJ, El Dika I, Abou-Alfa GK. Immunotherapy in hepatocellular carcinoma: primed to make a difference? Cancer. 2016;122(3):367–377. doi: 10.1002/cncr.29769 [DOI] [PubMed] [Google Scholar]
- 25.He L, Tian DA, Li PY, He XX. Mouse models of liver cancer: progress and recommendations. Oncotarget. 2015;6(27):23306–23322. doi: 10.18632/oncotarget.4202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fausto N, Campbell JS. Mouse models of hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):87–98. doi: 10.1055/s-0030-1247135 [DOI] [PubMed] [Google Scholar]
- 27.Santos NP, Colaço AA, Oliveira PA. Animal models as a tool in hepatocellular carcinoma research: a review. Tumour Biol. 2017;39(3):1010428317695923. doi: 10.1177/1010428317695923 [DOI] [PubMed] [Google Scholar]
- 28.Heindryckx F, Colle I, Van Vlierberghe H. Experimental mouse models for hepatocellular carcinoma research. Int J Exp Pathol. 2009;90(4):367–386. doi: 10.1111/j.1365-2613.2009.00656.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown ZJ, Heinrich B, Greten TF. Mouse models of hepatocellular carcinoma: an overview and highlights for immunotherapy research. Nat Rev Gastroenterol Hepatol. 2018;15(9):536–554. doi: 10.1038/s41575-018-0033-6 [DOI] [PubMed] [Google Scholar]
- 30.Mosier DE, Gulizia RJ, Baird SM, Wilson DB. Transfer of a functional human immune system to mice with severe combined immunodeficiency. Nature. 1988;335(6187):256–259. doi: 10.1038/335256a0 [DOI] [PubMed] [Google Scholar]
- 31.Tary-Lehmann M, Saxon A, Lehmann PV. The human immune system in hu-PBL-SCID mice. Immunol Today. 1995;16(11):529–533. doi: 10.1016/0167-5699(95)80046-8 [DOI] [PubMed] [Google Scholar]
- 32.Zhang L, Meissner E, Chen J, Su L. Current humanized mouse models for studying human immunology and HIV-1 immuno-pathogenesis. Sci China Life Sci. 2010;53(2):195–203. doi: 10.1007/s11427-010-0059-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vignali DA, Kuchroo VK. IL-12 family cytokines: immunological playmakers. Nat Immunol. 2012;13(8):722–728. doi: 10.1038/ni.2366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kobayashi M, Fitz L, Ryan M, et al. Identification and purification of natural killer cell stimulatory factor (NKSF), a cytokine with multiple biologic effects on human lymphocytes. J Exp Med. 1989;170(3):827–845. doi: 10.1084/jem.170.3.827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Behzadi P, Behzadi E, Ranjbar R. IL-12 family cytokines: general characteristics, pathogenic microorganisms, receptors, and signaling pathways. Acta Microbiol Immunol Hung. 2016;63(1):1–25. doi: 10.1556/030.63.2016.1.1 [DOI] [PubMed] [Google Scholar]
- 36.Atkins MB, Robertson MJ, Gordon M, et al. Phase I evaluation of intravenous recombinant human interleukin 12 in patients with advanced malignancies. Clin Cancer Res. 1997;3(3):409–417. [PubMed] [Google Scholar]
- 37.Motzer RJ, Rakhit A, Schwartz LH, et al. Phase I trial of subcutaneous recombinant human interleukin-12 in patients with advanced renal cell carcinoma. Clin Cancer Res. 1998;4:1183–1191. [PubMed] [Google Scholar]
- 38.Rook AH, Wood GS, Yoo EK, et al. Interleukin-12 therapy of cutaneous T-cell lymphoma induces lesion regression and cytotoxic T-cell responses. Blood. 1999;94(3):902–908. [PubMed] [Google Scholar]
- 39.Motzer RJ, Rakhit A, Thompson JA, et al. Randomized multicenter phase II trial of subcutaneous recombinant human interleukin-12 versus interferon-alpha 2a for patients with advanced renal cell carcinoma. J Interferon Cytokine Res. 2001;21(4):257–263. doi: 10.1089/107999001750169934 [DOI] [PubMed] [Google Scholar]
- 40.Hurteau JA, Blessing JA, DeCesare SL, Creasman WT. Evaluation of recombinant human interleukin-12 in patients with recurrent or refractory ovarian cancer: a gynecologic oncology group study. Gynecol Oncol. 2001;82(1):7–10. doi: 10.1006/gyno.2001.6255 [DOI] [PubMed] [Google Scholar]
- 41.Lenzi R, Rosenblum M, Verschraegen C, et al. Phase I study of intraperitoneal recombinant human interleukin 12 in patients with müllerian carcinoma, gastrointestinal primary malignancies, and mesothelioma. Clin Cancer Res. 2002;8(12):3686–3695. [PubMed] [Google Scholar]
- 42.Van Herpen CM, Huijbens R, Looman M, et al. Pharmacokinetics and immunological aspects of a phase Ib study with intratumoral administration of recombinant human interleukin-12 in patients with head and neck squamous cell carcinoma: a decrease of T-bet in peripheral blood mononuclear cells. Clin Cancer Res. 2003;9(8):2950–2956. [PubMed] [Google Scholar]
- 43.Wadler S, Levy D, Frederickson HL, et al. Eastern Cooperative Oncology Group. A phase II trial of interleukin-12 in patients with advanced cervical cancer: clinical and immunologic correlates. Eastern Cooperative Oncology Group study E1E96. Gynecol Oncol. 2004;92(3):957–964. doi: 10.1016/j.ygyno.2003.12.022 [DOI] [PubMed] [Google Scholar]
- 44.Weiss GR, O’Donnell MA, Loughlin K, Zonno K, Laliberte RJ, Sherman ML. Phase 1 study of the intravesical administration of recombinant human interleukin-12 in patients with recurrent superficial transitional cell carcinoma of the bladder. J Immunother. 2003;26(4):343–348. [DOI] [PubMed] [Google Scholar]
- 45.Sangro B, Mazzolini G, Ruiz J, et al. Phase I trial of intratumoral injection of an adenovirus encoding interleukin-12 for advanced digestive tumors. J Clin Oncol. 2004;22(8):1389–1397. doi: 10.1200/JCO.2004.04.059 [DOI] [PubMed] [Google Scholar]
- 46.Younes A, Pro B, Robertson MJ, et al. Phase II clinical trial of interleukin-12 in patients with relapsed and refractory non-hodgkin’s lymphoma and hodgkin’s disease. Clin Cancer Res. 2004;10(16):5432–5438. doi: 10.1158/1078-0432.CCR-04-0540 [DOI] [PubMed] [Google Scholar]
- 47.Lacy MQ, Jacobus S, Blood EA, Kay NE, Rajkumar SV, Greipp PR. Phase II study of interleukin-12 for treatment of plateau phase multiple myeloma (E1A96): a trial of the Eastern Cooperative Oncology Group. Leuk Res. 2009;33(11):1485–1489. doi: 10.1016/j.leukres.2009.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lissoni P. Therapy implications of the role of interleukin-2 in cancer. Expert Rev Clin Immunol. 2017;13(5):491–498. doi: 10.1080/1744666X.2017.1245146 [DOI] [PubMed] [Google Scholar]
- 49.Smyth MJ, Taniguchi M, Street SE. The anti-tumor activity of IL-12: mechanisms of innate immunity that are model and dose dependent. J Immunol. 2000;165(5):2665–2670. doi: 10.4049/jimmunol.165.5.2665 [DOI] [PubMed] [Google Scholar]
- 50.Schatzlein AG. Non-viral vectors in cancer gene therapy: principles and progress. Anticancer Drugs. 2001;12(4):275–304. [DOI] [PubMed] [Google Scholar]
- 51.Shim G, Kim D, Le QV, Park GT, Kwon T, Oh YK. Nonviral delivery systems for cancer gene therapy: strategies and challenges. Curr Gene Ther. 2018;18(1):3–20. doi: 10.2174/1566523218666180119121949 [DOI] [PubMed] [Google Scholar]
- 52.Robbins PD, Ghivizzani SC. Viral vectors for gene therapy. Pharmacol Ther. 1998;80(1):35–47. [PubMed] [Google Scholar]
- 53.Manjila SB, Baby JN, Bijin EN, Constantine I, Pramod K, Valsalakumari J. Novel gene delivery systems. Int J Pharm Investig. 2013;3(1):1–7. doi: 10.4103/2230-973X.108958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yamashita YI, Shimada M, Hasegawa H, et al. Electroporation-mediated interleukin-12 gene therapy for hepatocellular carcinoma in the mice model. Cancer Res. 2001;61(3):1005–1012. [PubMed] [Google Scholar]
- 55.Hanna E, Zhang X, Woodlis J, Breau R, Suen J, Li S. Intramuscular electroporation delivery of IL-12 gene for treatment of squamous cell carcinoma located at distant site. Cancer Gene Ther. 2001;8(3):151–157. doi: 10.1038/sj.cgt.7700287 [DOI] [PubMed] [Google Scholar]
- 56.Zitvogel L, Tahara H, Robbins PD, et al. Cancer immunotherapy of established tumors with IL-12. Effective delivery by genetically engineered fibroblasts. J Immunol. 1995;155(3):1393–1403. [PubMed] [Google Scholar]
- 57.Gao M, Zhu X, Wu L, Qiu L. Cationic polyphosphazene vesicles for cancer immunotherapy by efficient in vivo cytokine IL-12 plasmid delivery. Biomacromolecules. 2016;17(6):2199–2209. doi: 10.1021/acs.biomac.6b00433 [DOI] [PubMed] [Google Scholar]
- 58.Liu X, Gao X, Zheng S, et al. Modified nanoparticle mediated IL-12 immunogene therapy for colon cancer. Nanomedicine. 2017;13(6):1993–2004. doi: 10.1016/j.nano.2017.04.006 [DOI] [PubMed] [Google Scholar]
- 59.Men K, Huang R, Zhang X, et al. Local and systemic delivery of interleukin-12 gene by cationic micelles for cancer immunogene therapy. J Biomed Nanotechnol. 2018;14(10):1719–1730. doi: 10.1166/jbn.2018.2593 [DOI] [PubMed] [Google Scholar]
- 60.Lu X. Impact of IL-12 in cancer. Curr Cancer Drug Targets. 2017;17(8):682–697. doi: 10.2174/1568009617666170427102729 [DOI] [PubMed] [Google Scholar]
- 61.Lasek W, Zagożdżon R, Jakobisiak M. Interleukin 12: still a promising candidate for tumor immunotherapy? Cancer Immunol Immunother. 2014;63(5):419–435. doi: 10.1007/s00262-014-1523-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nishimura T, Iwakabe K, Sekimoto M, et al. Distinct role of antigen-specific T helper type 1 (Th1) and Th2 cells in tumor eradication in vivo. J Exp Med. 1999;190(5):617–627. doi: 10.1084/jem.190.5.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hansen M, Andersen MH. The role of dendritic cells in cancer. Semin Immunopathol. 2017;39(3):307–316. doi: 10.1007/s00281-016-0592-y [DOI] [PubMed] [Google Scholar]
- 64.Korn T, Bettelli E, Oukka M, Kuchroo VK. IL-17 and Th17 cells. Annu Rev Immunol. 2009;27:485–517. doi: 10.1146/annurev.immunol.021908.132710 [DOI] [PubMed] [Google Scholar]
- 65.Tesmer LA, Lundy SK, Sarkar S, Fox DA. Th17 cells in human disease. Immunol Rev. 2008;223:87–113. doi: 10.1111/j.1600-065X.2008.00628.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Asadzadeh Z, Mohammadi H, Safarzadeh E, et al. The paradox of Th17 cell functions in tumor immunity. Cell Immunol. 2017;322:15–25. doi: 10.1016/j.cellimm.2017.10.015 [DOI] [PubMed] [Google Scholar]
- 67.Kato T, Furumoto H, Ogura T, et al. Expression of IL-17 mRNA in ovarian cancer. Biochem Biophys Res Commun. 2001;282(3):735–738. doi: 10.1006/bbrc.2001.4618 [DOI] [PubMed] [Google Scholar]
- 68.Tartour E, Fossiez F, Joyeux I, et al. Interleukin 17, a T-cell-derived cytokine, promotes tumorigenicity of human cervical tumors in nude mice. Cancer Res. 1999;59(15):3698–3704. [PubMed] [Google Scholar]
- 69.Xie Y, Sheng W, Xiang J, Ye Z, Yang J. Interleukin-17F suppresses hepatocarcinoma cell growth via inhibition of tumor angiogenesis. Cancer Invest. 2010;28(6):598–607. doi: 10.3109/07357900903287030 [DOI] [PubMed] [Google Scholar]
- 70.Kryczek I, Wei S, Szeliga W, Vatan L, Zou W. Endogenous IL-17 contributes to reduced tumor growth and metastasis. Blood. 2009;114(2):357–359. doi: 10.1182/blood-2008-09-177360 [DOI] [PMC free article] [PubMed] [Google Scholar]