Abstract
Background: Distal radius fractures (DRFs) are the most common upper extremity fractures in adults. This study seeks to elucidate the impact age, fracture type, and patient comorbidities have on the current treatment of DRFs and risk of complications. We hypothesized that comorbidities rather than age would relate to the risk of complications in the treatment of DRFs. Methods: A retrospective review of data was performed for patients treated between 2007 and 2014 using Truven Health MarketScan Research Databases. Patients who sustained a DRF were separated into “closed” versus “open” treatment groups, and the association between patient demographics, treatment type, and comorbidities with complication rates was analyzed, along with the trend of treatment modalities throughout the study time interval. Results: In total, 155 353 DRFs were identified; closed treatment predominated in all age groups with the highest percentage of open treatment occurring in the 50- to 59-year age group. Between 2007 and 2014, there was an increase in the rate of open reduction and internal fixation (ORIF) in all age groups <90 with the largest increase (11%) occurring in the 70- to 79-year age group. Higher complication rates were observed in the open treatment group in all ages <90 years with a trend toward decreasing complication rates as age increased. Comorbidities were more strongly associated with the risk of developing complications than age. Conclusions: Closed treatment of DRFs remains the predominant treatment method among all age groups, but DRFs are increasingly being treated with ORIF. Emphasis on the patients’ comorbidities rather than chronological age should be considered in the treatment decision-making process of elderly patients with DRFs.
Keywords: distal radius, fracture, age, comorbidities, complications, open, closed, treatment
Introduction
Distal radius fractures (DRFs) are the most common upper extremity fractures in adults and the second most common fracture after hip fractures in the elderly.9 The incidence in persons over the age of 65 estimated at 57 to 100 per 10 000.9,12 The majority of DRFs in the elderly are low-energy injuries usually resulting from a ground-level fall. Treatment options include closed reduction and casting, open reduction and internal fixation (ORIF), percutaneous pinning, or external fixation.11,19 The advent of the volar plate in the early 2000s revolutionized the treatment of DRFs in the elderly population and has led to an increase in these fractures being treated with ORIF despite few studies showing superior outcomes over nonoperative treatment.3,6,10,17,18,20
A recently published meta-analysis of operative versus nonoperative treatment of DRFs in patients over the age of 60 found no statistical differences in pain, range of motion (ROM), functional ability, and minor complications (complications not requiring surgical treatment) between the operative and nonoperative treatment groups, with the operative group showing improved grip strength and radiographic parameters at the cost of increased risk of major complications (complications requiring surgical treatment).7 In addition to fracture type, the age of the patient is increasingly being considered when deciding between operative and nonoperative management of DRFs.
In the United States, 65 years of age is often thought of as the cutoff between adults and the elderly largely because it is the age patients become eligible for Social Security and Medicare benefits. The Social Security Act of 1935 was established when life expectancy was 62; it is currently 78.1 Today, there are nearly 45 million people over the age of 65, and it is predicted that by 2030, there will be 74 million people over the age of 65 or nearly 1 in 5 US residents.1,14 While chronological age is easy to ascertain, it is not tightly correlated with measures of function or health. The optimal treatment for DRFs in the elderly remains ambiguous and based on a variety of factors including clinical setting, surgeon, and patient characteristics.11
The aim of this study is to further understand the impact age, fracture type, and patient comorbidities have on the current treatment of DRFs and risk of complications using claims data. We hypothesized that comorbidities rather than age would relate to the risk of complications in the treatment of DRFs.
Materials and Methods
A retrospective review of data from commercially insured patients was performed using Truven Health MarketScan Research Databases. This is a national, de-identified database of paid inpatient and outpatient claims generated for patients with private or employer-provided coverage, and contains data for approximately 55 million Americans from 2003 to 2014.
Data for this study were reviewed for patients treated between 2007 and 2014. Patients aged 18 years and older who sustained a DRF were identified with the International Classification of Diseases, Ninth Revision (ICD-9) codes “813.40,” “813.41,” “813.42,” “813.44,” “813.45,” “813.47,” “813.50,” “813.51,” “813.52,” “813.54,” which include closed and open DRFs (Supplemental Material). Current Procedural Terminology (CPT) coding was used to determine the treatment type patients received for their fracture, and was subdivided into closed and open treatment (Supplemental Material). Patients whose treatment claims included the CPT codes “256.00” and “256.05” were allocated to the “closed treatment” group, and patients with treatment CPT codes “256.06,” “256.07,” “256.08,” “256.09,” “206.90,” “206.92,” “256.11,” and “256.20” were allocated to the “open treatment” group. Patients who did not have any treatment CPT code associated with their fracture diagnosis codes or had both types of CPT treatment codes were excluded to minimize confounding and bias. Afterward, 110 ICD-9 codes relevant to distal forearm and hand were isolated, and only claims associated with these codes were filtered from the data to minimize bias in procedural frequency.
Except for the trend analysis, patients were included if they were continuously enrolled for 6 months prior and 12 months post fracture diagnosis date. Six-month prediagnosis period was considered justifiable to examine patients for disorders of distal forearm and hand to rule out postoperative complications as a result of preoperative disorders. Twelve-month postdiagnosis period was a justifiable period to include all the diagnostic and therapeutic procedures performed for the fracture and allowed for the calculation of complication rates.
The trend of treatment modalities was analyzed and plotted over the decade spanning the study time interval. Complication rates were assessed and compared between “closed” and “open” treatment groups within in each age group, and afterward, assessed for each treatment group among the age groups. Posttreatment complications examined included ICD-9 codes related to wound complication, infection, neurovascular injuries, tendon rupture, malunion, nonunion, and stiffness (Supplemental Material).
Prior to examining the effect of age and comorbidities on complication rates, the unadjusted mean incidence of complications and comorbidities by age group was recorded. To test the effects of age and other comorbidities on the complication rate, we produced a multivariate Poisson regression model of factors associated with complications and computed the incidence rate ratio (IRR) and 95% confidence interval (CI) for all the IRRs. The IRR estimate is the multiplier for the complication rate given an effect, compared with its reference group and controlling for all the other factors in the model. Simply said, the IRRs are the ratios of the rates of complications in one group compared with the reference group. The mean incidence rates reflect the IRRs. Patients without a particular comorbidity were chosen to be the reference group in the model. Similarly, the youngest age group was chosen as a reference when assessing the IRRs for the other age groups. Analyses were performed using IBM SPSS Statistics for Windows, version 21 (IBM Corp, Armonk, New York).
Results
A total of 155 353 DRFs were identified between 2007 and 2014. Of the examined age groups, the greatest number (39 718 or 26%) of DRFs occurred in the 50- to 59-year age group (Table 1). Closed treatment was the preferred treatment method for all age groups with the highest percentage of open treatment occurring in the 50- to 59-year age group (Table 2). When examining the distribution of DRFs by gender, the <40-year-old cohort had a slight male predominance at 51% (Table 1). Thereafter, females sustained a higher percentage of DRFs compared with their male counterparts in all age groups >40. The difference between genders increased with each decade of life (Table 1).
Table 1.
Number of Male or Female Patients With Distal Radius Fractures by Age.
| <40 | 40-49 | 50-59 | 60-69 | 70-79 | 80-89 | 90+ | Total | |
|---|---|---|---|---|---|---|---|---|
| Male | 12 633 (51%) | 8160 (39.9%) | 9378 (23.6%) | 5850 (20.7%) | 3467 (16.6%) | 2677 (15%) | 357 (10.7%) | 42 522 (27.4%) |
| Female | 12 146 (49%) | 12 313 (60.1%) | 30 340 (76.4%) | 22 439 (79.3%) | 17 455 (83.4%) | 15 156 (85%) | 2982 (89.3%) | 112 831 (72.6%) |
| Total | 24 779 | 20 473 | 39 718 | 28 289 | 20 922 | 17 833 | 3339 | 155 353 |
Table 2.
Number of Patients With Distal Radius Fractures Treated Closed or Open by Age.
| <40 | 40-49 | 50-59 | 60-69 | 70-79 | 80-89 | >90 | Total | |
|---|---|---|---|---|---|---|---|---|
| Closed tx | 17 127 (69.1%) | 12 534 (61.2%) | 23 693 (59.7%) | 17 314 (61.2%) | 14 629 (69.9%) | 14 087 (79%) | 2 928 (87.7%) | 102 312 (65.9%) |
| Open tx | 7652 (30.9%) | 7939 (38.8%) | 16 025 (40.3%) | 10 975 (38.8%) | 6293 (30.1%) | 3746 (21%) | 411 (12.3%) | 53 041 (34.1%) |
| Total | 24 779 | 20 473 | 39 718 | 28 289 | 20 922 | 17 833 | 3339 | 155 353 |
Note. tx = treatment.
When examining the change in treatment type by age group from 2007 to 2014, an increase in the rate of ORIF of DRFs in all age groups below the age of 90 was observed with the largest increase (11%) occurring in the 70- to 79-year-old age group (Figure 1). Subanalysis of nonclosed treatment over the same time period revealed a 12% increase in the rate of open treatment of intra-articular DRF with internal fixation of 3 or more fragments and a 17% decrease in the rate of percutaneous fixation (Figure 2).
Figure 1.
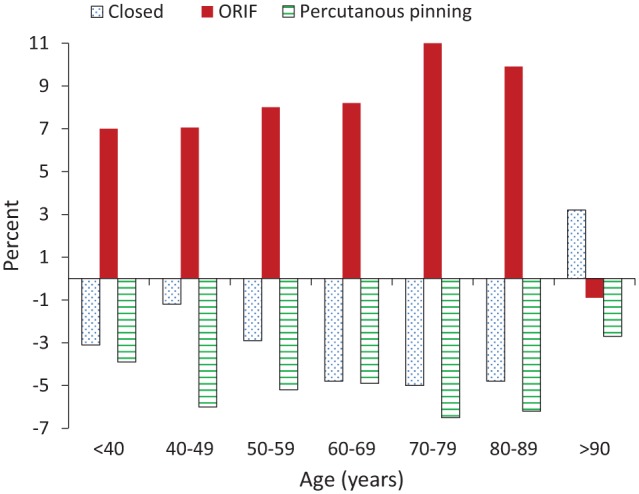
Change in distal radius fracture treatment type by age group between 2007 and 2014.
Note. ORIF = open reduction and internal fixation.
Figure 2.
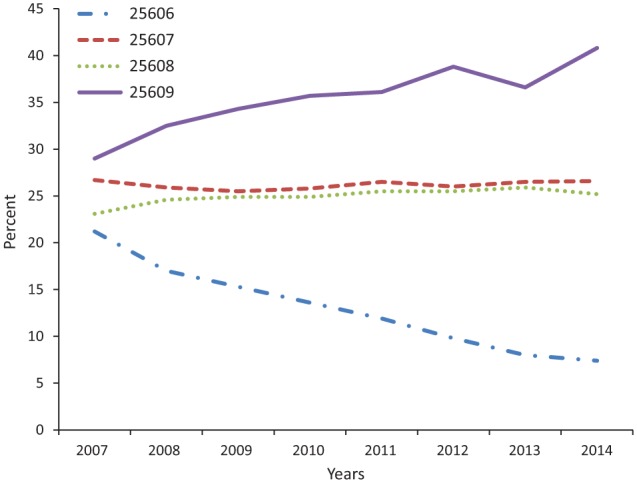
Percentage of nonclosed treatment of DRFs between 2007 and 2014.
Note. Current Procedural Terminology codes: 25606: percutaenous fixation of DRF, 25607: open treatment of extra-articular DRF, 25608: open treatment of intra-articular DRF with internal fixation of 2 fragments, and 25609: open treatment of intra-articular DRF with internal fixation of 3 or more fragments. DRF = distal radius fracture.
The mean complication rates between closed and open treatment of DRFs by age revealed a significantly higher complication rate in the open treatment group in all ages less than 90 (P < .001). No difference in complication rates was seen in the >90-year-group between closed and open treatment. There was a trend toward decreasing complication rates in the open treatment group with the largest decrease occurring between the 60- to 69- and 70- to 79-year age groups (Figure 3).
Figure 3.
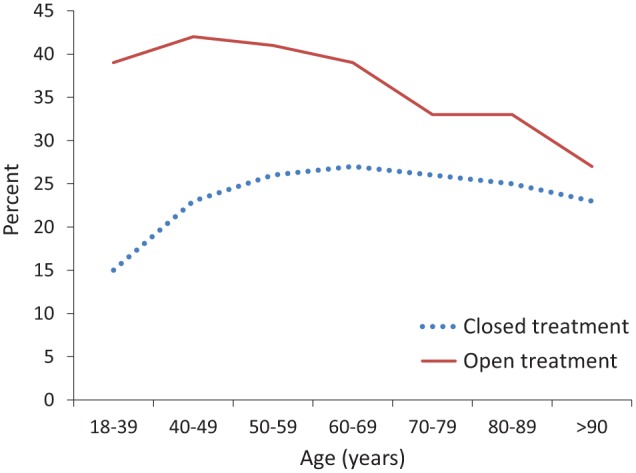
Complication rate between closed and open treatment.
As expected, the unadjusted mean incidence of complications and comorbidities tended to increase proportional to age (Figure 4). The multivariate Poisson regression model revealed that age, chronic heart failure (CHF), depression, diabetes, hypertension (HTN), chronic kidney disease (CKD), obesity, osteoporosis, and tobacco use were associated with a higher risk of complications. Controlling for HTN (the strongest correlate of complication incidence rate), the 45- to 54-year age group had the highest rate and older age groups had slightly lower rates as evidenced by the decreasing IRR. Large N made the standard errors small and the CIs narrow. All were highly significant. As the other comorbidities were less strongly associated with complication rates than HTN, we would not expect age to have a much different pattern in the fully adjusted model. Indeed, controlling for other comorbidities that are more common in older age groups, the adjusted complication rates are even lower in the oldest groups relative to the 45- to 54-year age group (Table 3).
Figure 4.
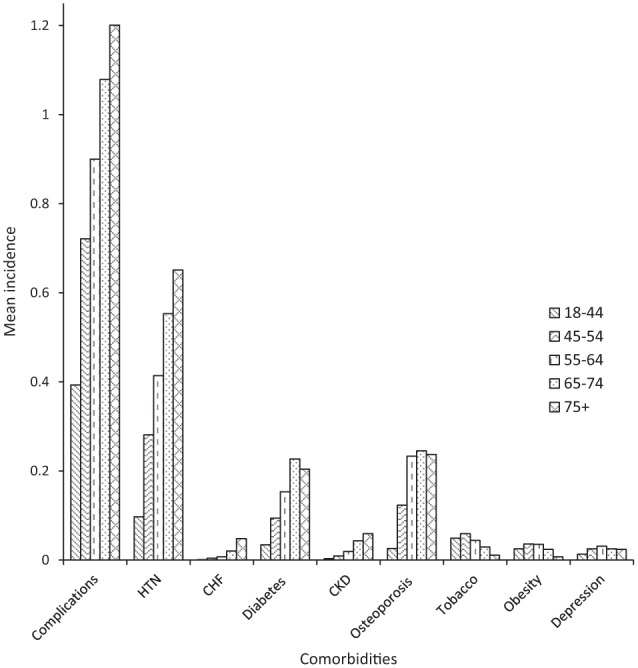
Unadjusted mean incidence of complications and comorbidities by age group.
Note. HTN = hypertension; CHF = chronic heart failure; CKD = chronic kidney disease.
Table 3.
Effect of Age and Comorbidities on Complication Rates After Surgery.
| Parameter | IRR | 95% CI | P value |
|---|---|---|---|
| Age | |||
| 18-44 | 1.00 | ||
| 45-54 | 1.13 | 1.10-1.15 | <.0001 |
| 55-64 | 1.10 | 1.07-1.12 | <.0001 |
| 65-74 | 1.06 | 1.04-1.08 | <.0001 |
| 75+ | 1.04 | 1.02-1.06 | .0004 |
| CHF | 1.7 | 1.66-1.74 | .0001 |
| Depression | 1.19 | 1.16-1.22 | .0001 |
| Diabetes | 1.05 | 1.03-1.06 | .0001 |
| Hypertension | 5.62 | 5.53-5.7 | <.0001 |
| CKD | 1.13 | 1.11-1.16 | <.0001 |
| Obesity | 1.17 | 1.15-1.2 | <.0001 |
| Osteoporosis | 1.1 | 1.09-1.11 | <.0001 |
| Tobacco | 1.17 | 1.14-1.2 | <.0001 |
Note. IRR = incidence rate ratio; CI = confidence interval; CHF = chronic heart failure; CKD = chronic kidney disease.
Discussion
DRFs occur in a bimodal distribution with high-energy mechanisms seen in younger patients and low-energy mechanisms, usually ground-level falls, seen in the elderly.9 The number of US adults with osteoporosis and low bone mass peaks in the 50- to 59-year age group; women are affected at higher rates than men, with a progressive decrease in the total number of US adults afflicted with the condition despite an increase in prevalence.22 Accordingly, women sustain DRFs at higher rates than their male counterparts as bone mineral density decreases.11 This is consistent with our study’s findings of near equal rates of women and men who sustain DRFs in the <40-year age group and thereafter women more likely to sustain a DRF with the largest difference between males and females occurring in the 50- to 59-year age group (Table 1).
In a study of Medicare claims data, Chung et al found that while closed treatment of DRFs predominated, rates of internal fixation increased from 3% in 1996 to 16% in 2005.8 Our study found that from 2007 to 2014, the rates of internal fixation increased from 18.4% to 22.4%. A study based on the American Board of Orthopaedic Surgery Part II oral examination data from 1999 to 2007 found that the proportion of DRFs treated with ORIF increased from 42% to 81%.16 These studies corroborate our findings that closed treatment remains the predominant treatment type over open treatment in all age groups (Table 2) despite an increase in the rates of open treatment in all age groups <90 years between 2007 and 2014 (+10.8% in <40; +3.1 in 40-49; +6.9% in 50-59; +12.2% in 60-69; +16.5% in 70-79; +21.2% in 80-89) (Figure 1).
The 11% increase in the rates of ORIF of DRFs with 3 or more fragments between 2007 and 2014 can largely be attributed to the advent of the volar plate in 2000 (Figure 2). While the popularity of this fixation method has grown, its benefits in the elderly remain unclear. A randomized controlled trial of patients over the age of 65 with Arbeitsgemeinschaft für Osteosynthesefragen (AO) type C DRFs compared ORIF with closed reduction and casting and concluded that ORIF provides marginal increase in mobility, functionality, and quality of life over closed reduction and casting at 12 months.3,18 Lutz et al found higher complication rates in patients older than 65 years with open treatment of a DRF compared with closed treatment but controlled only for HTN and diabetes and had significantly more open fracture in the open treatment group compared with no open fractures in the closed treatment group.18
Our study revealed that complication rates were higher in the open treatment group for all ages except for the >90-year age group. As patients’ age increased, there was a trend toward increasing complication in the closed treatment group with a decreasing trend in the open treatment group (Figure 3). Our complication rate for the open treatment group ranged from a high of 42% in the 40- to 49-year age group to a low of 27% in the >90-year age group. For the closed treatment group, complication rates ranged from a low of 15% in the 40- to 49-year age group to a high of 27% in the 60- to 69-year age group. The complication rates are comparable with previous studies examining complication rates in elderly patients with DRFs treated open or closed: 29% versus 17%,18 16% versus 9%,10 and 36% versus 14%.2 The downward trend in complications seen in the open treatment group is likely due to an increasingly higher threshold for patient comorbidities as the patient age increases.
In our study, complication rates were significantly higher in patients with at least one of the examined comorbidities: diabetes, osteoporosis, CKD, CHF, HTN, obesity, tobacco use, and depression. HTN was by far the strongest correlate of complication incidence rate, with CHF next. This is consistent with the study by Jiang et al, who found that certain comorbidities such as CHF and HTN were associated with higher complication rates following open treatment of a DRF while age was not a significant predictor.15 Schick et al also found HTN to be an independent risk factor for developing complications following DRF ORIF.21 The exact mechanism of HTN’s role in increased rates of complication is unclear; it has been proposed that HTN may have a deleterious effect on the immune system. In theory, this could affect a patient’s ability to ward off infection and impact wound healing.5 While age was a significant factor in developing postoperative complications, comorbidities appear to be more strongly associated than chronological age in complication rates.
Many factors are considered when selecting open versus closed treatment including fracture type and increasingly the age of the patient. Age is often used as a proxy of functional status and is also considered when weighing the risk of developing arthritis. Chronological and physiological ages are 2 distinct patient characteristics that need to be differentiated when recommending treatment options to patients. This study helps to shift the focus from age to comorbidities as an important factor to consider during the shared decision-making process of discussing operative or nonoperative treatment of DRFs.
While many studies have shown acceptable function and quality of life for elderly patients with DRFs treated operatively and nonoperatively, the decision should be based on the physiological age of the patient rather than the chronological age. One of the major benefits of ORIF over closed treatment is early return to function. While the aforementioned studies show equivocal functional and quality of life benefits of ORIF over closed treatment in elderly patients in the intermediate postoperative period to 1 year, the difference in the immediate postoperative period is less clear.3,7,9,10 Chan et al demonstrated earlier return of grip strength and ROM in elderly patients with DRFs treated with volar plating compared with cast immobilization.6 Earlier return of grip strength, ROM, and less time immobilized in a cast may be particularly important to elderly patients with little support at home when attempting to perform their activities of daily living.
Stable restoration of the articular surface of a joint is important in preventing the development of arthritis. Rates of arthritis are higher in patients with intra-articular DRFs treated nonsurgically.4,10,13 While the long-term consequence of arthritis on function in the elderly patient is unclear, it should be considered given the increasing life span of the US population and further analysis is recommended.
Analyzing large, population-based databases can be challenging and should be done carefully; however, the use of the MarketScan database in our study has several strengths. It contains 11 consecutive years of inpatient, outpatient, and prescribing data from a significant nationwide sample accumulating and capturing data of nearly 55 million Americans, which would make our results more generalizable when compared with studies that work with smaller population samples, and provide external validity to the study. A rigorous narrowing of the data was performed to limit the possible confounding variables, and patients were appropriately selected according to narrow enrollment criteria to minimize capturing claims of patients not related to DRF. By examining the treatment trends by subtype of fracture, we have been able to better understand which fractures are driving the increased rates of ORIF. The types of treatment complications examined are extensive and insured that the majority of complications sustained after DRF treatment were captured in this study (Supplemental Material).
Limitations of this study are those that are inherent with any study using claims data. A major limitation of the MarketScan database is the exclusion of uninsured and Medicaid patients. Only Medicare patients with supplemental insurance were included in the database, which is particularly significant given this study’s emphasis on patients over the age of 65. A change in DRF CPT coding occurred in 2007 which allowed for more specific analysis of treatment trends at the cost of a longer time period for analysis. The input values included in the database are subject to entry error and do not include any clinical information related to patient function.
In conclusion, our study revealed that DRFs are increasingly being treated with ORIF in patients between the ages of 40 and 90 years. While complication rates are higher in the open treatment group, there is a trend toward decreasing complication rates as the age of the patient increases, likely related to surgeons being more mindful of elderly patients’ overall health. Emphasis on the patient’s comorbidities, functional status, and desire for rapid return to activity, rather than chronological age, should be considered in the decision-making process of elderly patients with DRFs.
Supplementary Material
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: This was a de-identified patient database study, and no informed consent was required.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by internal/departmental funding.
Supplemental material is available in the online version of the article.
References
- 1. Arias E. United States Life Tables, 2010. National Vital Statistics Reports. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. [Google Scholar]
- 2. Arora R, Lutz M, Deml C, et al. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93:2146-2153. [DOI] [PubMed] [Google Scholar]
- 3. Bartl C, Stengel D, Bruckner T, et al. The treatment of displaced intra-articular distal radius fractures in elderly patients. Dtsch Arztebl Int. 2014;111:779-787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barton T, Chambers C, Bannister G. A comparison between subjective outcome score and moderate radial shortening following a fractured distal radius in patients of mean age 69 years. J Hand Surg Eur Vol. 2007;32:165-169. [DOI] [PubMed] [Google Scholar]
- 5. Case AJ, Zimmerman MC. Sympathetic-mediated activation versus suppression of the immune system: consequences for hypertension. J Physiol. 2016;594:527-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chan Y-H, Foo T-L, Yeo C-J, et al. Comparison between cast immobilization versus volar locking plate fixation of distal radius fractures in active elderly patients, the Asian perspective. Hand Surg. 2014;19:19-23. [DOI] [PubMed] [Google Scholar]
- 7. Chen Y, Chen X, Li Z, et al. Safety and efficacy of operative versus nonsurgical management of distal radius fractures in elderly patients: a systematic review and meta-analysis. J Hand Surg Am. 2016;41:404-413. [DOI] [PubMed] [Google Scholar]
- 8. Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91:1868-1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Diaz-Garcia RJ, Oda T, Shauver MJ, et al. A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. J Hand Surg Am. 2011;36:824-835.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Egol KA, Walsh M, Romo-Cardoso S, et al. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010:92;1851-1857. [DOI] [PubMed] [Google Scholar]
- 11. Fanuele J, Koval KJ, Lurie J, et al. Distal radial fracture treatment: what you get may depend on your age and address. J Bone Joint Surg Am. 2009;91:1313-1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gehrmann SV, Windolf J, Kaufmann RA. Distal radius fracture management in elderly patients: a literature review. J Hand Surg Am. 2008;33:421-429. [DOI] [PubMed] [Google Scholar]
- 13. Grewal R, MacDermid JC. The risk of adverse outcomes in extra-articular distal radius fractures is increased with malalignment in patients of all ages but mitigated in older patients. J Hand Surg Am. 2007;32:962-970. [DOI] [PubMed] [Google Scholar]
- 14. Jennifer M, Ortman Projections of the size and composition of the U.S. population: 2014 to 2060. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. Published 2015. Accessed December 15, 2017.
- 15. Jiang JJ, Phillips CS, Levitz SP, et al. Risk factors for complications following open reduction internal fixation of distal radius fractures. J Hand Surg Am. 2014;39:2365-2372. [DOI] [PubMed] [Google Scholar]
- 16. Koval KJ, Harrast JJ, Anglen JO, et al. Fractures of the distal part of the radius. The evolution of practice over time. Where’s the evidence? J Bone Joint Surg Am. 2008;90: 1855-1861. [DOI] [PubMed] [Google Scholar]
- 17. Larouche J, Pike J, Slobogean GP, et al. Determinants of functional outcome in distal radius fractures in high-functioning patients older than 55 years. J Orthop Trauma. 2016;30:445-449. [DOI] [PubMed] [Google Scholar]
- 18. Lutz K, Yeoh KM, MacDermid JC, et al. Complications associated with operative versus nonsurgical treatment of distal radius fractures in patients aged 65 years and older. J Hand Surg Am. 2014;39:1280-1286. [DOI] [PubMed] [Google Scholar]
- 19. MacIntyre NJ, Dewan N. Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther. 2016;29:136-145. [DOI] [PubMed] [Google Scholar]
- 20. Orbay JL. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000;5:103-112. [DOI] [PubMed] [Google Scholar]
- 21. Schick CW, Koehler DM, Martin CT, et al. Risk factors for 30-day postoperative complications and mortality following open reduction internal fixation of distal radius fractures. J Hand Surg. 2014;39:2373-2380. [DOI] [PubMed] [Google Scholar]
- 22. Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29:2520-2526. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


