Abstract
Background: Small olecranon fractures present a significant challenge for fixation, which has resulted in development of plates with proximal extension. Olecranon-specific plates with proximal extensions are widely thought to offer superior fixation of small proximal fragments but have distinct disadvantages: larger dissection, increased hardware prominence, and the increased possibility of impingement. Previous biomechanical studies of olecranon fracture fixation have compared methods of fracture fixation, but to date there have been no studies defining olecranon plate fixation strength for standard versus extended olecranon plates. The purpose of this study is to evaluate the biomechanical utility of the extended plate for treatment of olecranon fractures. Methods: Sixteen matched pairs of fresh-frozen human cadaveric elbows were used. Of the 16, 8 matched pairs received a transverse osteotomy including 25% and 8 including 50% of the articular surface on the proximal fragment. One elbow from each pair was randomly assigned to a standard-length plate, and the other elbow in the pair received the extended-length plate, for fixation of the fracture. The ulnae were cyclically loaded and subsequently loaded to failure, with ultimate load, number of cycles, and gap formation recorded. Results: There was no statistically significant difference between the standard and extended fixation plates in simple transverse fractures at either 25% or 50% from the proximal most portion of the articular surface of the olecranon. Conclusion: Standard fixation plates are sufficient for the fixation of small transverse fractures, but caution should be utilized particularly with comminution and nontransverse fracture patterns.
Keywords: elbow, biomechanics, olecranon fracture, plate fixation, internal fixation, cadaveric study
Introduction
Olecranon fractures are common injuries that often occur following low-energy falls in older patients or motor vehicle crashes in a younger population.6,18,20 A displaced noncomminuted proximal ulna fracture is the most prevalent type of olecranon fracture and has been reported to occur in up to 82% of olecranon fractures.6,18,20 Open reduction and internal fixation (ORIF) has become the standard of care for nearly all olecranon fractures; however, the method of fixation remains controversial.20 The most commonly described fixation methods include tension band wire fixation, precontoured plate fixation, and intramedullary screw fixation, and a number of studies have demonstrated good clinical and functional outcomes following ORIF using these various techniques. Plate fixation has been demonstrated to have increased biomechanical stability and decreased complications compared with other fixation methods; however, there certainly is a risk for hardware prominence necessitating removal, which is not unique to this fixation construct.2,5,12,19,25,26,28,29,31 The goals of operative fixation of displaced olecranon fractures are to gain anatomic reduction, ensure union, and provide stable fixation to allow for early motion.
Small olecranon fractures, particularly in osteoporotic bone, have increased failure rates when treated with standard olecranon plates. Loss of fixation secondary to implant failure is well demonstrated in this unique patient population.4,7-11,15-17,21,23,24 A number of different fixation techniques have failed to demonstrate any benefit in stabilizing olecranon fractures in osteoporotic bone.7 As such, plates with proximal extension have been developed with the hope of providing increased purchase in the proximal fragment. While previous biomechanical studies of olecranon fracture fixation have compared plate types with other methods of fracture fixation, to date there have been no studies defining olecranon plate fixation strength for standard versus extended olecranon plates particularly of the small olecranon fracture. This difference, if present, is critical to define as the use of these extended plates is at the cost of increased dissection, increased hardware prominence, and an increased likelihood of impingement in the olecranon fossa.1,3,19,22
The purpose of this study is to evaluate the biomechanical utility of the extended plate for treatment of small proximal olecranon fractures. We hypothesize that the more robust proximal fixation offered by the extended proximal olecranon plates will provide superior biomechanical stability demonstrated by increased load to failure compared with standard proximal fixation olecranon plates in the fixation of small olecranon fractures, while large olecranon fractures will not benefit from the increased purchase of proximally extended plates.
Materials and Methods
Sixteen matched pairs of fresh-frozen human cadaveric elbows, including the distal half of the humerus and the radius and ulna, were thawed at room temperature. All soft tissue was dissected free with the exception of the elbow joint capsule and triceps tendon. With visual inspection, there was no evidence of previous elbow injury or surgery in any of the tested elbow pairs.
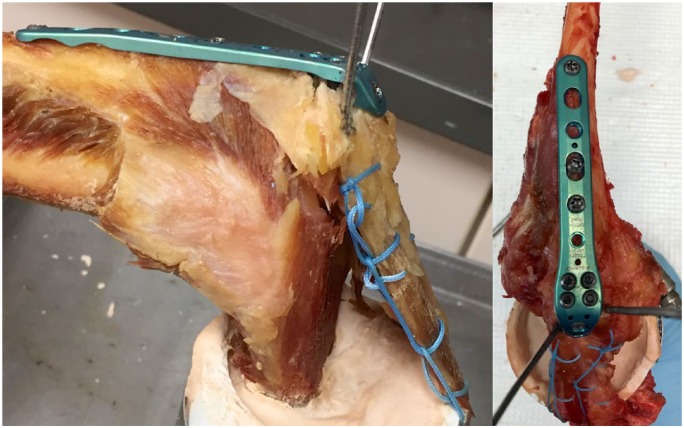
Eight matched pairs received a transverse osteotomy at a point including 25% of the articular surface of the olecranon on the proximal fragment, and 8 matched pairs received a transverse osteotomy at a point including 50% of the articular surface of the olecranon on the proximal fragment to simulate different fragment sizes. The osteotomy site was identified by measuring the distance with a handheld digital caliper between the articular surface of the tip of the olecranon and the articular surface of the tip of the coronoid, calculating 50% or 25% of that value and similarly marking the appropriate site for the osteotomy along the olecranon. The transverse osteotomy was performed using a fine-blade oscillating saw. The fragment was then reduced and held with a pointed reduction forceps under direct visualization. Fixation was then performed in this position by the plate to which each was randomly assigned according to the manufacturer’s product guide (Acumed Elbow Plating System Olecranon Plate, Hillsboro, OR). The proximal holes in each plate were all filled with locking screws. In the standard plate, this included 4 holes along the subcutaneous border of the ulna and a single screw into the olecranon tip. In the extended plate, this included 4 holes along the subcutaneous border of the ulna and 3 screws into the olecranon tip. Three nonlocking screws were placed in the first, third, and fourth hole in the diaphyseal section of each plate. One elbow from each matched pair was randomly assigned to a standard-length plate and the contralateral elbow received the extended-length plate for fixation of the fracture (Figures 1 and 2).
Figure 1.

Standard (a) and extended (b) precontoured olecranon plates.
Figure 2.
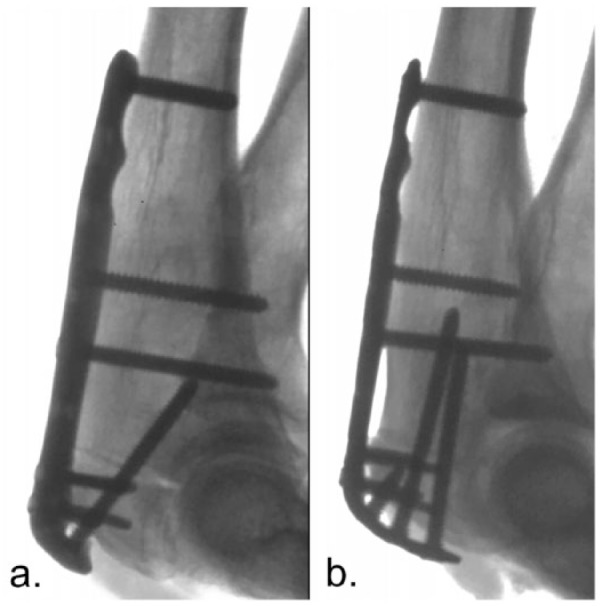
Radiographs of standard (a) and extended (b) precontoured olecranon plates as applied following osteotomy.
After fracture fixation was accomplished, the proximal humerus was potted into a 2-inch polyvinyl chloride (PVC) pipe utilizing dental cement (Heroes Kulzer Inc, South Bend, Indiana). The triceps mechanism was secured to the PVC pipe with 2 circular steel hose clamps (Tridon, Nashville, Tennessee) at an initial flexion angle of 90° with the triceps tendon reinforced with FiberWire suture and two 2-mm stainless steel wires (Figure 3). This method of loading applied tension along a physiologic vector through the pull of the triceps tendon.
Figure 3.
The final set-up of the specimens before being placed in the materials testing machine.
Note. The fractures are fixed with precontoured olecranon plates, the humerus is potted in 2-inch PVC pipes, and the triceps tendon is reinforced with FiberWire suture and secured to the PVC pipe with 2 circular steel hose clamps. The initial flexion angle is 90°. PVC = polyvinyl chloride.
A materials testing machine (MTS 858 Mini-Bionix Test System, Minneapolis, Minnesota) was then utilized to apply a vertical force at a point on the subcutaneous border of the ulna 10 cm from the fracture. The ulnae were cyclically loaded from 0 to 100 N at a frequency of 1 Hertz (Hz) for 500 cycles and were subsequently loaded to failure. Fracture gap was measured with a handheld digital caliper at 5, 50, and 500 cycles by 3 independent observers and the average gap calculated. Load to failure criterion was defined as the force required to create a gap of 2 mm at the fracture site. The number of cycles; fracture gap displacement after 5, 50, and 500 cycles; and the ultimate load to failure were recorded.
Results
For specimens fixed with the standard olecranon plates (n = 16), 3 specimens failed during the cyclic loading phase, and 13 were loaded to failure. One of the failures was in a small fracture fragment, and the other 2 failures were found in specimens with a large fracture fragment. For the specimens fixed with the extended olecranon plates (n = 16), 4 specimens failed during the cyclic loading phase, and 12 were loaded to failure. All 4 of the failures occurred in specimens with small olecranon fracture fragments.
Gap formation was measured for each specimen at 5, 50, and 500 cycles. For the small (25%) fracture fragments fixed with a standard-length plate, the fracture gap averaged 0.08 mm, 0.13 mm, and 1.9 mm at each of the 3 time points. For the small (25%) fracture fragments fixed with an extended-length plate, the fracture gap averaged 0.85 mm, 1.06 mm, and 0.90 mm at each of the 3 time points (P = .08, P = .08, P = .87). For the large (50%) fracture fragments fixed with a standard-length plate, the fracture gap averaged 0.43 mm, 0.87 mm, and 1.05 mm at each of the 3 time points. For the large (50%) fracture fragments fixed with an extended-length plate, the fracture gap averaged 0 mm at each of the 3 time points (P = .03, P = . 17, P = .015) (Table 1).
Table 1.
Mean Gap Formation for the Standard and Extended Plates at Cycles 5, 50, and 500.
| Number of cycles | 5 | 50 | 500 | 5 | 50 | 500 |
|---|---|---|---|---|---|---|
| Small (25% Fracture) Standard Plate | Small (25% Fracture) Extended Plate | |||||
| Average gap formation | 0.08 | 0.13 | 0.83 | 0.86 | 1.07 | 0.90 |
| Standard deviation | 0.74 | 0.75 | 0.99 | 1.06 | 1.24 | 1.01 |
| P value | .08 | .08 | .87 | |||
| Large (50% Fracture) Standard Plate | Large (50% Fracture) Extended Plate | |||||
| Average gap formation | 0.43 | 0.87 | 1.05 | 0.00 | 0.00 | 0.00 |
| Standard deviation | 0.73 | 0.82 | 0.90 | 0.76 | 0.76 | 0.76 |
| P value | .04 | .02 | .02 | |||
Overall, the average load to failure in specimens with standard plates was 288 N ± 72.1 N (Table 2). The mean load to failure in specimens with standard plates and osteotomies at 25% (n = 8) was 189 N ± 35.4 N versus 387 N ± 135.1 N for specimens with osteotomies at 50% (n = 8). Overall, the average load to failure in specimens with the extended plate was 278 N ± 51.0 N. The mean load to failure in specimens with extended plates and osteotomies at 25% (n = 8) was 161 N ± 21.6 N versus 395 N ± 82.3 N for specimens with osteotomies at 50% (n = 8). Overall, there was no statistically significant difference in the load to failure force between plates (P = .865) or osteotomy sites (P = .587 at 25% osteotomy and P = .936 at 50% osteotomy).
Table 2.
Mean Load to Failure for Specimens With Standard and Extended Plates.
| Standard plate, mean ± SEM (N) | Extended plate, mean ± SEM (N) | P value | |
|---|---|---|---|
| Overall | 288 ± 72.1 | 278 ± 51.0 | .865 |
| Osteotomy 25% | 189 ± 35.4 | 161 ± 21.6 | .587 |
| Osteotomy 50% | 387 ± 135.1 | 395 ± 82.3 | .936 |
Note. SEM = standard error of the mean.
All 32 specimens failed catastrophically during the cyclic loading or load to failure phases. Failure in every specimen involved screw cutout and a gradual increase in size of the fracture gap. No specimens failed due to hardware breakage.
Discussion
In this cadaveric study, we attempted to determine whether the extended proximal fixation olecranon plates provided superior biomechanical stability when compared with standard proximal fixation olecranon plates in the fixation of olecranon fractures, particularly those with small proximal fragments. Previous study has demonstrated that elbow stability and articular reduction of these olecranon fractures are less critical than preserving muscular attachment of the triceps to the tip of the olecranon.4,7,19 This is particularly true in those fractures with small olecranon fragments, which are particularly prone to redisplacement and nonunion.4,7,19 While studies have compared various fixation techniques, there are no other studies that have investigated the difference in stability between standard and extended plates. The results of this investigation failed to demonstrate a statistically significant difference in load to failure between standard and extended plates for the fixation of small or large simple, transverse fractures of the proximal olecranon.
Biomechanical models of the elbow have been used to estimate the force seen by the elbow in various activities of daily living (ADLs), and these models have reported peak joint forces seen in light ADLs (eating, dressing, personal hygiene) range from 70 to 350 N and in moderate ADLs (opening a door, lifting a small bag or gallon of milk) range from 419 to 698 N.14 This is particularly relevant given the load to failure that was seen in this cadaveric study, which is well below the normal loads seen by the elbow in activities of daily living. Due to this, the elbow should be strictly nonweightbearing until some signs of bony union are present. The current standard of postoperative care at our institution involves 7 to 10 days of immobilization and an additional 6 to 8 weeks of nonweightbearing while beginning to work to regain range of motion.
Plate fixation for olecranon fractures has demonstrated superior biomechanical stability compared with alternate methods of fracture fixation. This trend of superior load to failure was demonstrated in this cadaveric study, as mean load to failure in this study was 288 N and 278 N in the standard and extended groups, respectively. These values are much higher than load to failure reported in the literature for alternate fixation methods. A similar cadaveric study looking at a variety of fixation methods, including tension band wiring and screw fixation, reported mean load to failure ranging from 35 to 84 N at 90°.27
Although plate fixation for olecranon fractures has been shown to have increased biomechanical stability compared with other methods, this technique is not without complications. Especially in osteoporotic bone, the extensor mechanism can fail and pull off of the fixed olecranon fragment.13,30 Along with failure of the extensor mechanism, previous studies have reported limitations in extension and prominence of hardware following fixation of olecranon fractures, with more severe limitation found after fixation with longer plates.1,3,19,22 Future studies should investigate whether extended plates offer superior stability for fixation of olecranon fractures with more complex fracture patterns, as these fractures are also subjected to increased failure rates relative to simple fracture patterns and these fractures may provide a role for the extended plates. Also to be investigated is the differences in limitation of extension which occur between standard and extended plate types. Based on the reported data, along with the known risk of decreased range of motion and lack of evidence for increased stability with extended plates, we posit that standard plates are sufficient for fixation of simple olecranon fractures of varying sizes greater than and including those with only 25% of the articular surface attached to the proximal fragment. This information must be used with caution as it does not necessarily apply to smaller or more comminuted fragments of the proximal ulna.
Conclusion
The goal of this study was to determine if extended olecranon fixation plates provided increased biomechanical stability compared with standard plates in olecranon fractures that were 25% or 50% from the proximal most portion of the articular surface of the olecranon. While we hypothesized that extended plates would be superior to standard plates for fractures 25% from the proximal most portion of the articular surface of the olecranon, there was no statistically significant difference found. In conclusion, even with small fragments, the standard fixation plates are sufficient for the fixation of simple fractures. However, this recommendation must be tempered with clinical judgment, particularly with comminuted and nontransverse fractures, where there may be continued utility for the extended plate or suture augmentation to increase the stability of the construct.
Footnotes
Ethical Approval: This study was exempt from institutional review board approval.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: This article does not contain any studies with human or animal subjects and as such was exempt from informed consent.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: MBG has received research support from Acumed as Primary Investigator for completion of this research and declares that this is his sole conflict of interest. The remainder of the authors declare that they have no conflict of interest.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research support was provided by Acumed (Grant Number 16012). This outside source of funds was used in performance of the specimen testing and data collection. Michael B. Gottschalk, MD, has received research support from Acumed as Primary Investigator for completion of this research. Allison L. Boden, BA, Charles A. Daly, MD, Poonam P. Dalwadi, BS, Stephanie A. Boden, BA, William C. Hutton, DSc, and Raghuveer C. Muppavarapu, MD, have no financial disclosures.
ORCID iD: CA Daly  https://orcid.org/0000-0002-9843-635X
https://orcid.org/0000-0002-9843-635X
References
- 1. Anderson ML, Larson AN, Merten SM, et al. Congruent elbow plate fixation of olecranon fractures. J Orthop Trauma. 2007;21(6):386-393. [DOI] [PubMed] [Google Scholar]
- 2. Bailey CS, MacDermid J, Patterson SD, et al. Outcome of plate fixation of olecranon fractures. J Orthop Trauma. 2001;15(8):542-548. [DOI] [PubMed] [Google Scholar]
- 3. Buijze G, Kloen P. Clinical evaluation of locking compression plate fixation for comminuted olecranon fractures. J Bone Joint Surg Am. 2009;91(10):2416-2420. [DOI] [PubMed] [Google Scholar]
- 4. Chao EY, Inoue N, Koo TK, et al. Biomechanical considerations of fracture treatment and bone quality maintenance in elderly patients and patients with osteoporosis. Clin Orthop Relat Res. 2004;(425):12-25. [DOI] [PubMed] [Google Scholar]
- 5. De Giacomo AF, Tornetta P, Sinicrope BJ, et al. Outcomes after plating of olecranon fractures: a multicenter evaluation. Injury. 2016;47(7):1466-1471. [DOI] [PubMed] [Google Scholar]
- 6. Duckworth AD, Clement ND, Aitken SA, et al. The epidemiology of fractures of the proximal ulna. Injury. 2012;43(3):343-346. [DOI] [PubMed] [Google Scholar]
- 7. Edwards SG, Martin BD, Fu RH, et al. Comparison of olecranon plate fixation in osteoporotic bone: do current technologies and designs make a difference? J Orthop Trauma. 2011;25(5):306-311. [DOI] [PubMed] [Google Scholar]
- 8. Frankle MA, Herscovici D, Jr, DiPasquale TG, et al. A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular distal humerus fractures in women older than age 65. J Orthop Trauma. 2003;17(7):473-480. [DOI] [PubMed] [Google Scholar]
- 9. Hausman M, Panozzo A. Treatment of distal humerus fractures in the elderly. Clin Orthop Relat Res. 2004;(425):55-63. [DOI] [PubMed] [Google Scholar]
- 10. Hewins EA, Gofton WT, Dubberly J, et al. Plate fixation of olecranon osteotomies. J Orthop Trauma. 2007;21(1):58-62. [DOI] [PubMed] [Google Scholar]
- 11. Huang TL, Chiu FY, Chuang TY, et al. The results of open reduction and internal fixation in elderly patients with severe fractures of the distal humerus: a critical analysis of the results. J Trauma. 2005;58(1):62-69. [DOI] [PubMed] [Google Scholar]
- 12. Hume MC, Wiss DA. Olecranon fractures. A clinical and radiographic comparison of tension band wiring and plate fixation. Clin Orthop Relat Res. 1992;(285):229-235. [PubMed] [Google Scholar]
- 13. Izzi J, Athwal GS. An off-loading triceps suture for augmentation of plate fixation in comminuted osteoporotic fractures of the olecranon. J Orthop Trauma. 2012;26(1):59-61. [DOI] [PubMed] [Google Scholar]
- 14. Kincaid BL, An KN. Elbow joint biomechanics for preclinical evaluation of total elbow prostheses. J Biomech. 2013;46(14):2331-2341. [DOI] [PubMed] [Google Scholar]
- 15. Korner J, Lill H, Muller LP, et al. Distal humerus fractures in elderly patients: results after open reduction and internal fixation. Osteoporos Int. 2005;(16)(Suppl 2):S73-79. [DOI] [PubMed] [Google Scholar]
- 16. LaPorte DM, Murphy MS, Moore JR. Distal humerus nonunion after failed internal fixation: reconstruction with total elbow arthroplasty. Am J Orthop (Belle Mead NJ). 2008;37(10):531-534. [PubMed] [Google Scholar]
- 17. Moroni A, Hoang-Kim A, Lio V, et al. Current augmentation fixation techniques for the osteoporotic patient. Scand J Surg. 2006;95(2):103-109. [DOI] [PubMed] [Google Scholar]
- 18. Niéto H, Billaud A, Rochet S, et al. Proximal ulnar fractures in adults: a review of 163 cases. Injury. 2015;(46)(Suppl 1):S18-23. [DOI] [PubMed] [Google Scholar]
- 19. Niglis L, Bonnomet F, Schenck B, et al. Critical analysis of olecranon fracture management by pre-contoured locking plates. Orthop Traumatol Surg Res. 2015;101(2):201-207. [DOI] [PubMed] [Google Scholar]
- 20. Powell AJ, Farhan-Alanie OM, Bryceland JK, et al. The treatment of olecranon fractures in adults. Musculoskelet Surg. 2017;101(1):1-9. [DOI] [PubMed] [Google Scholar]
- 21. Schmidt AH. The changing face of orthopaedic trauma: fragility and periprosthetic fractures. Instr Course Lect. 2008;57:11-16. [PubMed] [Google Scholar]
- 22. Simpson NS, Goodman LA, Jupiter JB. Contoured LCDC plating of the proximal ulna. Injury. 1996;27(6):411-417. [DOI] [PubMed] [Google Scholar]
- 23. Srinivasan K, Agarwal M, Matthews SJ, et al. Fractures of the distal humerus in the elderly: is internal fixation the treatment of choice? Clin Orthop Relat Res. 2005;(434):222-230. [DOI] [PubMed] [Google Scholar]
- 24. Stromsoe K. Fracture fixation problems in osteoporosis. Injury. 2004;35(2):107-113. [DOI] [PubMed] [Google Scholar]
- 25. Tarallo L, Mugnai R, Adani R, et al. Simple and comminuted displaced olecranon fractures: a clinical comparison between tension band wiring and plate fixation techniques. Arch Orthop Trauma Surg. 2014;134(8):1107-1114. [DOI] [PubMed] [Google Scholar]
- 26. Wagner FC, Konstantinidis L, Hohloch N, et al. Biomechanical evaluation of two innovative locking implants for comminuted olecranon fractures under high-cycle loading conditions. Injury. 2015;46(6):985-989. [DOI] [PubMed] [Google Scholar]
- 27. Wang W, Wu G, Shen F, et al. A biomechanical experiment and clinical study of the use of figure of eight plus circular wiring fixation for the treatment of olecranon fractures. Exp Ther Med. 2012;4(6):1081-1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wang YH, Tao R, Xu H, et al. Mid-term outcomes of contoured plating for comminuted fractures of the olecranon. Orthop Surg. 2011;3(3):176-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wellman DS, Lazaro LE, Cymerman RM, et al. Treatment of olecranon fractures with 2.4- and 2.7-mm plating techniques. J Orthop Trauma. 2015;29(1):36-43. [DOI] [PubMed] [Google Scholar]
- 30. Wild JR, Askam BM, Margolis DS, et al. Biomechanical evaluation of suture-augmented locking plate fixation for proximal third fractures of the olecranon. J Orthop Trauma. 2012;26(9):533-538. [DOI] [PubMed] [Google Scholar]
- 31. Wilson J, Bajwa A, Kamath V, et al. Biomechanical comparison of interfragmentary compression in transverse fractures of the olecranon. J Bone Joint Surg Br. 2011;93(2):245-250. [DOI] [PubMed] [Google Scholar]