Abstract
Purpose: The purpose of this study was to report trends, complications, and costs associated with endoscopic carpal tunnel release (ECTR) and open carpal tunnel release (OCTR). Methods: Using Current Procedural Terminology (CPT) and International Classification of Diseases, Ninth Revision (ICD-9) codes, patients who had open versus endoscopic carpal tunnel release (CTR) were identified retrospectively in the PearlDiver database from both the Medicare and Humana (a private payer health insurance) populations from 2005 to 2014. These groups were then evaluated for postoperative complications, including wound infection within 90 days, wound dehiscence within 90 days, and intraoperative median nerve injury. We also used the data output for each group to compare the cost of the 2 procedure types. Data were analyzed via the Student t test. Statistical significance was set at P < .05. Results: A significantly lower percentage of patients in the endoscopic CTR group had a postoperative infection (5.21 vs 7.97 per 1000 patients per year, P < .001; 7.36 vs 11.23 per 1000 patients per year, P < .001) and wound dehiscence (1.58 vs 2.87 per 1000 patients per year, P < .001; 2.14 vs 3.73 per 1000 patients per year, P < .05) than open CTR group in the Medicare and Humana populations, respectively. Median nerve injury occurred 0.59/1000 ECTRs versus 1.69/1000 OCTRs (Medicare) and 1.96/1000 ECTRs versus 3.72/1000 OCTRs (Humana). Endoscopic CTR cost was more than open CTR for both the Medicare population ($1643 vs $1015 per procedure, P < .001) and Humana population ($1928 vs $1191 per procedure, P < .001). Conclusions: In both the Medicare and private insurance patient populations, endoscopic CTR is associated with fewer postoperative complications than open CTR, but is associated with greater expenses.
Keywords: carpal tunnel release, endoscopic carpal tunnel release, open carpal tunnel release, carpal tunnel release complications, median nerve injury, median nerve neuropathy
Introduction
Compressive median mononeuropathy at the wrist, known as carpal tunnel syndrome (CTS), is the most commonly diagnosed entrapment neuropathy with an incidence of 1 to 3 cases per 1000 patients per year and a prevalence of 50 cases per 1000 subjects in the general population.7,26 Various occupational and personal risk factors predispose to CTS, including age, sex, and obesity.32 Tingling, numbness, and pain in the median nerve distribution of the hand are the typical presentation. Advanced untreated disease may lead to permanent muscle atrophy of the thenar musculature and deficit in opposition function of the thumb; surgical restoration of opposition such as opponensplasty may be required in select patients depending on physician training and preference.15,21,23
Conservative nonsurgical approaches such as splinting, nonsteroidal anti-inflammatory drugs, and corticosteroids are often preferred in mild/moderate cases, whereas surgical carpal tunnel release (CTR) is indicated for cases involving severe symptoms or conservative treatment failures.14,31 Surgical treatment of CTS involves releasing the transverse carpal tunnel ligament to decrease pressure on the median nerve.30 Endoscopic carpal tunnel release (ECTR), which was first described in 1989,5,22 allows visualization and decompression of the nerve through smaller skin incisions than the traditional open technique.4
Currently, both open carpal tunnel release (OCTR) and ECTR are widely utilized with no clear superiority of one technique over the other. Over the past 2 decades, several studies have shown advantages and disadvantages to both surgical approaches.1,12,16,19,29,30,33 OCTR assures complete transverse carpal ligament release due to enhanced visualization; however, this approach results in slower recovery and return to work, has been shown to result in the formation of hypertrophic scars in incisions crossing the wrist, and has a greater incidence of persistent pain.12,20,33 ECTR is associated with reduced pain, better esthetic result, and a more rapid return to work and daily activities than OCTR.3,27 ECTR, in addition to increased cost, has been associated with complications such as incomplete transverse carpal ligament release requiring subsequent reoperation, tendon injury, and, most notably, minor and major nerve injuries.11,28
CTRs are commonly performed operations and have a relatively low complication rate. Using large population databases, we hope to elucidate important differences to provide further insight into the debate between ECTR and OCTR. With this retrospective study, we aim to assess the differences in operative and postoperative complications such as surgical site infection, wound dehiscence, and injury to median nerve along with differences in trends and costs (on an individual basis). We hypothesized that ECTR is associated with more complications but consistent with previous studies, has a higher associated cost for the patient relative to OCTR.
Materials and Methods
The PearlDiver Patient Record Database (PearlDiver Inc, Fort Wayne, Indiana; www.pearldiverinc.com) is a publically available database of over 4 billion insurance billing records. It contains the records of patients who have had an orthopedic International Classification of Diseases, Ninth Revision (ICD-9) or Current Procedural Terminology (CPT) code assigned to their billing record from both private insurance (Humana) and Medicare. The PearlDiver (PD) database was chosen because it contains a 100% sample of Medicare patients with an orthopedic ICD-9 or CPT code from 2005 to 2012 as well as up to 9 million patients per year of privately insured patients with an orthopedic ICD-9 or CPT code from 2007 to 2014. These large national health care data sets enabled us to perform high-throughput studies to evaluate the incidence of rare postoperative complications.
The database was queried for Medicare and Humana patient populations who had undergone open CTR (CPT 64721) and for those who had undergone endoscopic CTR (CPT 29848) from the respective time frames of the 2 data sets. To analyze trends in open versus endoscopic CTRs performed, incidence of each procedure per 10 000 patients was calculated for both the Medicare and Humana patient populations using the total number of procedures done per year. These 2 patient populations were then subsequently queried to evaluate the rates of associated postoperative complications according to surgical approach.
To evaluate for postoperative and operative complications, open and endoscopic CTR groups were each queried for postoperative infection diagnoses (ICD-9-D-998.5 or ICD-9-D-998.51 or ICD-9-D-998.59 or ICD-9-D-682.4 or ICD-9-D-680.4), wound dehiscence diagnoses (ICD-9-D-998.32 or ICD-9-D-998.3) entered within 3 months of the index CTR procedure, and intraoperative median nerve injury (ICD-9-D-955.1) entered on the same day as index procedure. The mean number of postoperative infections per 1000 CTRs per year was then compared between the open and endoscopic groups. Similar analysis was performed for wound dehiscence as a postoperative complication and median nerve injury as an intraoperative complication.
Last, a cost analysis was performed to evaluate the difference in cost between the 2 CTR groups and the 2 insurance populations. The mean amount of money paid per procedure for open versus endoscopic CTR was then compared. The cost data were obtained as part of the output data for queries of endoscopic (CPT 29848) and open (CPT 64721) CTRs in each of the payer populations.
Student 2-tailed t test was used to determine the statistical significance of differences in means between the endoscopic and open CTR groups. Statistical significance was set for all analyses to a P value of less than .05.
Results
There were a total of 9451 patients who underwent ECTR and 53 814 patients who underwent OCTR in the Humana patient population between 2007 and 2014 and 62 665 patients who underwent ECTR and 441 350 patients who underwent OCTR in the Medicare patient population between 2005 and 2012. The demographics of the aforementioned patient groups are broken down by age and gender in Table 1 (Medicare) and Table 2 (Humana). Within the Humana population, the majority of patients undergoing either ECTR (59.7%) or OCTR (60.0%) are seen in the 60 to 79 age range. No such demographic trend is seen in the Medicare patient populations as all patients fall within the elderly age group. In addition, in both payer populations, more females proportionally underwent CTR than males.
Table 1.
Patient Demographics According to Age Groups and Gender, Reported as Percent of Total Number of Endoscopic Carpal Tunnel Releases or Open Carpal Tunnel Releases From 2005 to 2012 Within the Medicare Group.
| Medicare population demographics | ||
|---|---|---|
| Group | Endoscopic (% of total) |
Open (% of total) |
| Female | 60.96 | 61.20 |
| Male | 38.02 | 37.62 |
| <65 | 16.35 | 19.25 |
| 65-69 | 22.47 | 20.63 |
| 70-74 | 19.84 | 18.67 |
| 75-79 | 18.13 | 17.94 |
| 80-84 | 14.18 | 14.51 |
| >85 | 9.50 | 10.02 |
| Total number of patients | 62 665 | 441 350 |
Table 2.
Patient Demographics According to Age Groups and Gender, Reported as Percent of Total Number of Endoscopic Carpal Tunnel Releases or Open Carpal Tunnel Releases From 2007 to 2014 Within the Humana Group.
| Humana population demographics | ||
|---|---|---|
| Group | Endoscopic (% of total) |
Open (% of total) |
| Female | 61.26 | 59.91 |
| Male | 38.74 | 40.09 |
| <10 | 0 | 0 |
| 10-19 | 0 | 0.11 |
| 20-29 | 0.65 | 0.69 |
| 30-39 | 3.42 | 2.72 |
| 40-49 | 7.16 | 7.36 |
| 50-59 | 15.48 | 15.15 |
| 60-69 | 27.18 | 28.04 |
| 70-79 | 32.56 | 31.98 |
| 80-89 | 11.50 | 12.05 |
| >90 | 3.21 | 3.90 |
| Total number of patients | 9451 | 53 814 |
To assess trends in the amount of CTRs being done each year, incidence of both ECTRs and OCTRs was plotted in Figure 1 against time. There is an increase in incidence in both ECTRs and OCTRs in the Humana population since 2007 to 2014. However, in the Medicare population, there is decrease in the incidence of OCTRs up until 2012, although a clear trend is not apparent with ECTRs.
Figure 1.

Incidence of CTRs by year (Humana vs Medicare).
Note. Depiction of the trend in the Humana population (a) and in the Medicare population (b). Incidence is defined as number of index CTRs per 10 000 patients within the database. CTR = carpal tunnel release.
Figure 2 compares postoperative infections between the patient populations diagnosed within 3 months of index procedure. As expected, given the larger incisions required for OCTRs, there were significantly more postoperative infections seen relative to the ECTR group in both Humana and Medicare populations. Medicare patients had 5.21 postoperative infections diagnosed per 1000 ECTRs compared with 7.97 postoperative infections per 1000 OCTRs (P = 1.96 × 10-5). Similarly, Humana patients had 7.36 postoperative infections per 1000 ECTRs versus 11.23 postoperative infections per 1000 OCTRs (P = 3.89 × 10-5). Another postoperative complication assessed in this study is wound dehiscence. Figure 3 shows that within the Medicare population, 1.58 dehiscence per 1000 ECTRs versus 2.86 dehiscence per 1000 OCTRs were seen, a statistically significant difference (P = 5.87 × 10-8). The Humana population did have enough number of patients who had a diagnosis of wound dehiscence to see the true value per year (as per Health Insurance Portablity and Accountability Act of 1996 [HIPAA] terms and conditions, patient numbers cannot be reported if less than 11 total).
Figure 2.
Postoperative infections.
Note. Mean number of postoperative infections per year per 1000 carpal tunnel releases (CTRs) between 2007 and 2014 for Humana and between 2005 and 2012 for Medicare.
*Indicates statistical significance (P < .05).
Figure 3.
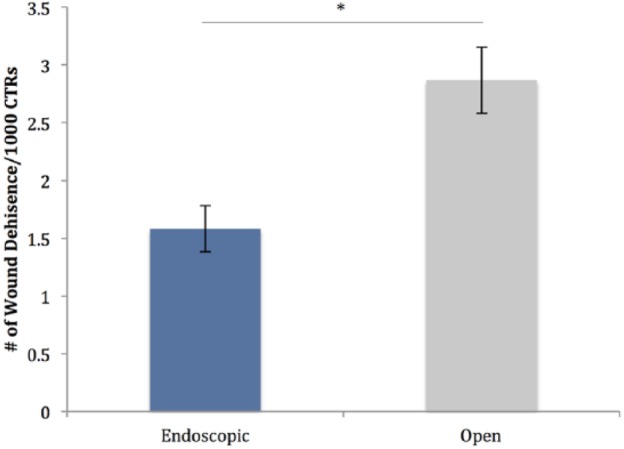
Wound dehiscence.
Note. Mean number of wound dehiscence complications per year per 1000 carpal tunnel releases (CTRs) between 2005 and 2012 in the Medicare population.
*Indicates statistical significance (P < .05).
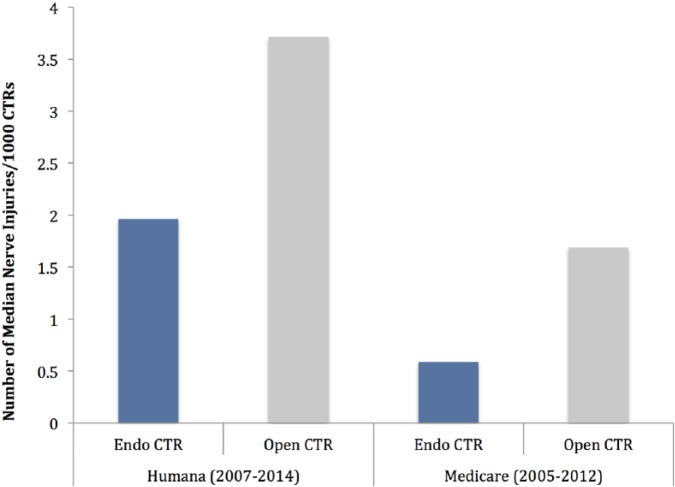
Iatrogenic median nerve injury is an important complication to consider between the 2 CTR approaches. Though uncommon, significant clinical sequela such as thenar atrophy can result.2,8,12,23 In the Medicare population, cumulatively from 2005 to 2012, median nerve injury occurred 0.59/1000 ECTRs versus 1.69/1000 OCTRs. Similarly, in the Humana population, cumulatively from 2007 to 2014, median nerve injury occurred 1.96/1000 ECTRs versus 3.72/1000 OCTRs (Figure 4).
Figure 4.
Median nerve injury.
Note. Total number of median nerve injuries per 1000 index carpal tunnel releases (CTRs) between 2005 and 2012 in the Medicare population and between 2007 and 2014 in the Humana population.
Last, Figure 5 shows a cost comparison between the 2 procedures in question. In the Medicare population, $1643.38 was the average paid amount per ECTR, while $1015.75 was the average paid per OCTR (P = 3.85 × 10-8) between 2005 and 2012. Similarly, in the Humana population, $1928.50 was the average paid amount per ECTR, while $1191.25 was the average paid per OCTR (P = 1.28 × 10-8) between 2007 and 2014. As expected, ECTR on average had a higher cost than OCTR in both insurance groups within their respective years.
Figure 5.
Mean cost per carpal tunnel release (CTR).
Note. Average paid (cost) per CTR in the Humana (2007-2014) and Medicare (2005-2012) patient populations. This cost includes all expenses that the insurer paid for on the day of surgery.
*Indicates a statistically significant difference (P < .05).
Discussion
Looking at the demographics between the study groups, the gender and age groups are very similar in number, providing reassurance against intrinsic bias in the data sets and increasing the validity of the study itself. Interestingly, in both Humana and Medicare, the majority of patients undergoing CTR were between 60 and 79 years old. Though expected in Medicare, this finding in the Humana population is higher and different that previous studies on CTRs.15 We postulate that this could be due to improving conservative therapies delaying surgery in combination with increasing surgeon willingness to perform surgery on older patients among other factors.
Various complications associated with CTR have been extensively studied,10,13 with a mixed picture of some studies reporting no statistical difference in complications19,33 while others report a difference in complications.1,30 It is widely accepted that postoperative infections and wound dehiscence are rare complications of CTR but using a large database, we were able to demonstrate a statistically significant increase in postoperative infection and wound dehiscence in OCTR compared with ECTR.
Given the small number of median nerve injuries per year, we were unable to calculate the annual incidence (per PD HIPAA guidelines) and thus had to report cumulative prevalence over the previously mentioned time span of the respective insurance populations. Interestingly, over an 8-year time span, median nerve injury with open CTR occurred about 1.9 times and 2.9 times (in Humana and Medicare, respectively) more than with endoscopic CTR. This finding is in contrary to some previous large retrospective studies that have reported an increase in relative risk of nerve injury with ECTR when compared with OCTR. However, it remains unclear, as nerve injury has been defined differently in different studies.18,25,27 Ultimately, this highlights the need for large prospective studies to determine the rates and consequences of iatrogenic nerve injury rates between ECTRs and OCTRs.
Last, cost is an important consideration for patients when deciding between surgery options. We performed a cost analysis to extrapolate the average paid for each respective procedure by Medicare and Humana. Previous cost-effective studies have reported ECTR to be more expensive than OCTR due to the increased time and equipment required for ECTR.6,10,17 Our results further support these findings, underscoring the importance of differentiating complication risks and determining if the increased risks of OCTR outweigh the increased costs of ECTR along with its associated risks as well.
Some major limitations of this study are directly related to the intrinsic limitations of the PD database itself. There is a strong reliance on accurate coding by practitioners and health care administrators that needs to be taken into account. In addition, laterality cannot be discerned based solely on billing codes, preventing us from looking at important complications such as incomplete transection of the transverse carpal ligament requiring repeat CTR as well as rare complications such as complex regional pain syndrome and opponensplasty secondary to intraoperative median nerve injury. Furthermore, due to the limitations of the database, we were unable to study and address the use of local anesthesia versus regional anesthesia, which undoubtedly is an important factor to consider for surgeons choosing between OCTR and ECTR. Though large databases such as PD rely on proper coding, they have shown to efficiently answer questions and present important evidence.9
The importance of this study is highlighted in the need to identify the pros and cons of ECTR and OCTR to determine the right procedure for patients. Database studies such as this one are highly powered and enable dissection of subtle differences in trends and complications due to their large number of patient records.24 With our results, we provide insight into complications and costs that not only equip clinicians with more information to make informed decisions with their patient regarding procedure method but also help generate hypotheses for further risk-benefit studies in regard to CTR techniques.
Conclusion
Overall, based on our results, ECTR is associated with less surgical site infections, wound dehiscence, and injury to median nerve but with a greater financial impact to the patient when compared with OCTR. Ideally, other factors such as anesthesia, secondary procedures, and functional outcomes should be compared. However, we believe our findings based on such large patient populations provide important information for physicians to consider in choosing the right procedure for their patients.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects
Statement of Informed Consent: No patient identifying information is available through the Pearl-Diver Inc database; thus, informed consent is not required.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: JCW—Royalties: Aesculap, Biomet, Amedica, Seaspine, Synthes; Stock Ownership: Fziomed; Private Investments: Promethean Spine, Paradigm Spine, Benevenue, NexGen, Vertiflex, ElectroCore, Surgitech, CoreSpine, Expanding Orthopedics, Osprey, Bone Biologics, Curative Biosciences, PearlDiver; Board of Directors: North American Spine Society (nonfinancial, reimbursement for travel for board meetings, courses, etc), North American Spine Foundation (nonfinancial), Cervical Spine Research Society (nonfinancial, reimbursement for travel for board meetings), AO Spine/AO Foundation (honorariums for board position); Fellowship Support: AO Foundation (spine fellowship funding paid to institution). ZB—Consultancy: Xenco Medical, AO Spine. FP—Personal fees from Zimmer Biomet, outside the submitted work. All other authors declare that they have no conflict of interests.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Aslani HR, Alizadeh K, Eajazi A, et al. Comparison of carpal tunnel release with three different techniques. Clin Neurol Neurosurg. 2012;114(7):965-968. doi: 10.1016/j.clineuro.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 2. Bindra RR, Bhandarkar DS, Taraporvala JC. Opponensplasty—an experience of twenty-three cases using three techniques. J Postgrad Med. 1990;36(1):9-12. [PubMed] [Google Scholar]
- 3. Chen L, Duan X, Huang X, et al. Effectiveness and safety of endoscopic versus open carpal tunnel decompression. Arch Orthop Trauma Surg. 2014;134(4):585-593. doi: 10.1007/s00402-013-1898-z. [DOI] [PubMed] [Google Scholar]
- 4. Cho YJ, Lee JH, Shin DJ, et al. Comparison of short wrist transverse open and limited open techniques for carpal tunnel release: a randomized controlled trial of two incisions. J Hand Surg Eur Vol. 2016;41(2):143-147. doi: 10.1177/1753193415603968. [DOI] [PubMed] [Google Scholar]
- 5. Chow JC. Endoscopic release of the carpal ligament: a new technique for carpal tunnel syndrome. Arthroscopy. 1989;5(1):19-24. [DOI] [PubMed] [Google Scholar]
- 6. Chung KC, Walters MR, Greenfield ML, et al. Endoscopic versus open carpal tunnel release: a cost-effectiveness analysis. Plast Reconstr Surg. 1998;102(4):1089-1099. [DOI] [PubMed] [Google Scholar]
- 7. Clapham P. Optimal management of carpal tunnel syndrome. IJGM. 2010;2010:255-257. doi: 10.2147/IJGM.S7682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ebata T, Imai K, Tokunaga S, et al. Thumb opposition in severe carpal tunnel syndrome with undetectable APB-CMAP. Hand Surg. 2014;19(2):199-204. doi: 10.1142/S0218810414500208. [DOI] [PubMed] [Google Scholar]
- 9. Grauer JN, Leopold SS. Editorial: large database studies—what they can do, what they cannot do, and which ones we will publish. Clin Orthop Relat Res. 2015;473(5):1537-1539. doi: 10.1007/s11999-015-4223-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Harness NG, Inacio MC, Pfeil FF, et al. Rate of infection after carpal tunnel release surgery and effect of antibiotic prophylaxis. J Hand Surg Am. 2010;35(2):189-196. doi: 10.1016/j.jhsa.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 11. Helm R, Vaziri S. Evaluation of carpal tunnel release using the Knifelight instrument. J Hand Surg Br. 2003;28(3):251-254. doi: 10.1016/S0266-7681(02)00395-9. [DOI] [PubMed] [Google Scholar]
- 12. Hu K, Zhang T, Xu W. Intraindividual comparison between open and endoscopic release in bilateral carpal tunnel syndrome: a meta-analysis of randomized controlled trials. Brain Behav. 2016;6(3):e00439. doi: 10.1002/brb3.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Karl JW, Gancarczyk SM, Strauch RJ. Complications of carpal tunnel release. Orthop Clin North Am. 2016;47(2):425-433. doi: 10.1016/j.ocl.2015.09.015. [DOI] [PubMed] [Google Scholar]
- 14. Kim P-T, Lee H-J, Kim T-G, et al. Current approaches for carpal tunnel syndrome. Clin Orthop Surg. 2014;6(3):253-255. doi: 10.4055/cios.2014.6.3.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kleopa KA. Carpal tunnel syndrome. Ann Intern Med. 2015;163(5):ITC1-ITC1. doi: 10.7326/AITC201509010. [DOI] [PubMed] [Google Scholar]
- 16. Larsen MB, Sorensen AI, Crone KL, et al. Carpal tunnel release: a randomized comparison of three surgical methods. J Hand Surg Eur Vol. 2013;38(6):646-650. doi: 10.1177/1753193412475247. [DOI] [PubMed] [Google Scholar]
- 17. Lorgelly PK, Dias JJ, Bradley MJ, et al. Carpal tunnel syndrome, the search for a cost-effective surgical intervention: a randomised controlled trial. Ann R Coll Surg Engl. 2005;87(1):36-40. doi: 10.1308/1478708051469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. MacDermid JC, Richards RS, Roth JH, et al. Endoscopic versus open carpal tunnel release: a randomized trial. J Hand Surg Am. 2003;28(3):475-480. doi: 10.1053/jhsu.2003.50080. [DOI] [PubMed] [Google Scholar]
- 19. Michelotti B, Romanowsky D, Hauck RM. Prospective, randomized evaluation of endoscopic versus open carpal tunnel release in bilateral carpal tunnel syndrome: an interim analysis. Ann Plast Surg. 2014;73:S157-S160. doi: 10.1097/SAP.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 20. Murthy PG, Goljan P, Mendez G, et al. Mini-open versus extended open release for severe carpal tunnel syndrome. Hand. 2014;10(1):34-39. doi: 10.1007/s11552-014-9650-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Newington L, Harris EC, Walker-Bone K, et al. Carpal tunnel syndrome and work. Best Pract Res Clin Rheumatol. 2015;29(3):440-553. doi: 10.1016/j.berh.2015.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Okutsu I, Ninomiya S, Takatori Y, et al. Endoscopic management of carpal tunnel syndrome. Arthroscopy. 1989;5(1):11-18. [DOI] [PubMed] [Google Scholar]
- 23. Park I-J, Kim H-M, Lee S-U, et al. Opponensplasty using palmaris longus tendon and flexor retinaculum pulley in patients with severe carpal tunnel syndrome. Arch Orthop Trauma Surg. 2010;130(7):829-834. doi: 10.1007/s00402-010-1053-z. [DOI] [PubMed] [Google Scholar]
- 24. Pugely AJ, Martin CT, Harwood J, et al. Database and registry research in orthopaedic surgery: part I: claims-based data. J Bone Joint Surg Am. 2015;97(15):1278-1287. doi: 10.2106/JBJS.N.01260. [DOI] [PubMed] [Google Scholar]
- 25. Rab M, Grünbeck M, Beck H, et al. Intra-individual comparison between open and 2-portal endoscopic release in clinically matched bilateral carpal syndrome. J Plast Reconstr Aesthet Surg. 2006;59(7):730-736. doi: 10.1016/j.bjps.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 26. Rojo-Manaute JM, Capa-Grasa A, Chana-Rodriguez F, et al. Ultra-minimally invasive ultrasound-guided carpal tunnel release: a randomized clinical trial. J Ultrasound Med. 2016;35(6):1149-1157. doi: 10.7863/ultra.15.07001. [DOI] [PubMed] [Google Scholar]
- 27. Sayegh ET, Strauch RJ. Open versus endoscopic carpal tunnel release: a meta-analysis of randomized controlled trials. Clin Orthop Relat Res. 2015;473(3):1120-1132. doi: 10.1007/s11999-014-3835-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thoma A, Veltri K, Haines T, et al. A meta-analysis of randomized controlled trials comparing endoscopic and open carpal tunnel decompression. Plast Reconstr Surg. 2004;114:1137-1146. [DOI] [PubMed] [Google Scholar]
- 29. Vasen AP, Kuntz KM, Simmons BP, et al. Open versus endoscopic carpal tunnel release: a decision analysis. J Hand Surg Am. 1999;24(5):1109-1117. doi: 10.1053/jhsu.1999.1109. [DOI] [PubMed] [Google Scholar]
- 30. Vasiliadis HS, Nikolakopoulou A, Shrier I, et al. Endoscopic and open release similarly safe for the treatment of carpal tunnel syndrome. A systematic review and meta-analysis. PLoS One. 2015;10(12):e0143683. doi: 10.1371/journal.pone.0143683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Verdugo RJ, Salinas RA, Castillo JL, et al. Surgical versus non-surgical treatment for carpal tunnel syndrome. Cochrane Database Syst Rev. 2003;3:CD001552. [DOI] [PubMed] [Google Scholar]
- 32. Zimmerman M, Dahlin E, Thomsen NOB, et al. Outcome after carpal tunnel release: impact of factors related to metabolic syndrome. J Plast Surg Hand Surg. 2017;51:165-171. doi: 10.1080/2000656X.2016.1210521. [DOI] [PubMed] [Google Scholar]
- 33. Zuo D, Zhou Z, Wang H, et al. Endoscopic versus open carpal tunnel release for idiopathic carpal tunnel syndrome: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2015;(10):12. doi: 10.1186/s13018-014-0148-6. [DOI] [PMC free article] [PubMed] [Google Scholar]