Abstract
Caregiving in the last years of life is associated with increased depression and negative health outcomes for surviving spouses, many of whom are themselves in poor health. Yet it is unclear how often spouses are caregiving alone, how they differ from supported spouses, and whether lack of support affects postbereavement outcomes. We hypothesized that spouses who were solo caregivers—that is, the only caregivers (paid or unpaid) who provided assistance with a spouse’s self-care or household activities—would experience more depression after bereavement than supported spouses would. Using information from the Health and Retirement Study, we found that 55 percent of the spouses of community-dwelling married people with disability were solo caregivers. Solo caregiving was even common among people who cared for spouses with dementia and those with adult children living close by. Bereavement outcomes did not differ between solo and supported caregiving spouses. Caregiving spouses are often isolated and may benefit from greater support, particularly during the final years before bereavement. While some state and federal policy proposals aim to systematically recognize and assess caregivers, further innovations in care delivery and reimbursement are needed to adequately support seriously ill older adults and their caregivers. Ultimately, the focus of serious illness care must be expanded from the patient to the family unit.
Unpaid caregivers provide highly complex and physically demanding care to their family members throughout the course of illness, including the last years of life.1 Over 14.7 million unpaid caregivers, mostly family members, assist older adults with daily activities and health care decision making and provide financial and social support.2 Their care is particularly critical for people with serious illness at the end of life. In fact, it is so fundamental that strategies to improve the quality of end-of-life care consistently highlight the need to support family caregivers.3,4 Recent national guidelines on the core competencies and components of high-quality community-based serious illness care include caregiver assessment, support, and training.5
In the last years of life, caregiving tasks may include the management of pain and other symptoms, frequent hospitalizations, and decision making regarding nursing home entry and the use of life-sustaining treatments.3,6 High out-of-pocket health-related spending7 frequently adds additional stress on both individuals and families. Not surprisingly, caregivers who are providing care to family members in the last years of life are vulnerable to symptoms of depression and anxiety8,9 and related emotional, physical, and financial challenges.10
The caregiving experience itself may affect the health and well-being of the caregiver after bereavement. Families report worsened physical and mental health and more hospitalizations following a loved one’s death when intensive, life-sustaining treatments were performed at the end of life.11–13 On the other hand, comfort-focused treatments including hospice are associated with decreased depression.11,14,15 Additionally, bereavement itself is associated with negative consequences for spouses, including not only increased mortality16 but also reduced personal health maintenance and increased health care expenditures.17,18
While spouses are not the only family members involved in caregiving during the last years of life,4 they experience more burden and depression than other family members do,9,19 including increased anxiety about loss20 and negative consequences after bereavement.21 Spousal caregivers need to simultaneously fulfill their supportive roles and manage the burden brought about by the demands of caregiving. Caregiving spouses are less likely than other family caregivers to hire paid caregivers or use community services, especially if they are women.22,23 Spouses may feel reluctant to ask for help or may have a lack of perceived choice about care-giving that is associated with increased burden and depression.24 While there is an increasing awareness that many older adults are living alone25,26 and vulnerable to increased chronic illness and institutionalization, researchers have yet to examine whether there are implications to providing care alone for a dying spouse.
As the health care landscape in the US evolves to better meet the needs of seriously ill people through the continued growth of hospice and palliative care programs and the expansion of other home and community-based services, there is an imperative to support the family caregivers who provide care at home. Moreover, it is unclear whether these programs maybe shifting financial and other burdens to caregiving families.27 Understanding this process is critical for developing and monitoring programs and policies that meet the needs of older adults and their caregivers. This is especially salient for the growing population of dementia caregivers.
Therefore, the goals of this study were to determine how often spouses are caregiving alone and under what circumstances, and whether such isolation has implications for increased depression and other health outcomes after bereavement. We hypothesized that engaging in caregiving in isolation maybe particularly stressful and associated with increased depression and other negative outcomes after bereavement.
Study Data And Methods
SAMPLE
The study sample is from the Health and Retirement Study (HRS), a nationally representative, longitudinal survey of US adults ages fifty-one and older.28 Participants are surveyed face-to-face or via telephone in a core interview every two years. If participants are married or living with a partner, their partners (referred to here as spouses) are recruited into the study and surveyed. During each interview cycle, the HRS identifies participants who have died since the last interview wave. In these cases, a postdeath exit interview is conducted with the surviving spouse or another person knowledgeable about the deceased participant. Surviving spouses remain in the study after their partner’s death, completing subsequent core interviews.
Using eight waves of core interviews from 2000 to 2014, our study focused on decedents who were married at the time of death. Of the 9,243 decedents identified in the HRS, 9,094 completed an interview before death. Among these, 3,589 were married at the time of death. We further excluded the following people: spouses who did not have a predeath interview (n = 231), dyads whose members were not community dwelling (n = 269) or co-residing (n = 90), and decedents for whom a predeath interview occurred more than two years before death (n = 243). Of the resulting 2,756 dyads, we focused on 1,205 in which decedents required assistance with one or more self-care or house-hold activities at their last interview before death.
MEASURES
Data for our study were drawn from four HRS interviews per dyad: the decedent’s last core interview, the spouse’s last core interview before the decedent’s death, the postdeath exit interview, and the spouse’s first core interview after the decedent’s death.
Spousal and decedent factors were drawn from each participant’s last HRS core interview before death (mean time before death: 11.0 months; standard deviation: 6.7) and included age, sex, race/ethnicity, education, net worth, self-reported health, functional status, proximity of children, and level of comorbidity. Dementia status of the decedent was determined via an algorithm of probable dementia based on survey responses to multiple cognitive measures at the last interview before death.29 Caregiving in the last years of life was determined based on people identified as supporting the decedent for each self-care or household activity and hours of help provided. Self-care activity measures consisted of basic activities of daily living (ADLs), including dressing, walking, eating, bathing, using the toilet, and transferring to bed. Household activity measures were instrumental activities of daily living (IADLs), including meal preparation, grocery shopping, making phone calls, taking medications, and managing finances. Spousal depressive symptoms were measured via the eight-item Center for Epidemiologic Studies Depression Scale, with a score of 3 or more considered clinically significant.30
At the postdeath interview (mean time after death: 13.8 months; SD: 7.1), next of kin (76 percent of whom were spouses) reported the following characteristics about the death experience: residential status, location, and whether the death was expected. The next of kin also reported who assisted the decedent with self-care and household tasks in the last three months of life.
At the spouse’s first core interview after death (mean time after death: 13.2 months; SD: 7.1), information on the following postbereavement outcome measures was collected: depression, self-reported health, functional status, recent hospitalizations, and residential status.
ANALYSIS
We first determined how often spouses served as the solo caregiver—defined as the only paid or unpaid person who provided assistance to the decedent with basic self-care or household activities—in the last years of life in the overall sample and then stratified the results by sex and dementia status of the spouse. Next, we examined decedent and spousal caregiver clinical and sociodemographic characteristics and characteristics of the death experience to compare dyads in which the spouse was a solo caregiver and those in which the spouse was a caregiver supported by others. We compared differences between each group using t-tests and chi-square analyses. Finally, we compared spouses’ experiences after bereavement according to caregiving status (solo versus nonsolo). We estimated differences in postbereavement depression for spouses who were solo caregivers relative to those who had had support, adjusting for prebereavement depression status only and fully adjusting for other demographic and clinical characteristics using multivariable logistic regression analysis. Using the same approach, we compared secondary postbereavement outcomes—spousal self-reported health, functional dependence, hospitalization, nursing home placement, and death—by solo caregiving status. All analyses were conducted both unweighted and weighted to account for the HRS survey design. The weighting strategy is described in the online appendix.31
All analyses were completed using Stata, version 15.
LIMITATIONS
Our study had several limitations. First, the HRS assesses caregiving status based on task-oriented assistance.We were therefore unable to include caregivers who assisted only with other key activities such as providing social and emotional support, many of which may occur via distance. Such activities may serve as a vital support to spouses who are otherwise caregiving alone.
Second, we also did not have information on the use of palliative care services or support services such as respite care.
Third, on average, the predeath assessments occurred eleven months before death, and by design we restricted our focus to two years before death. The end-of-life period is not a clearly defined one, and this restriction might not be ideal for all illness trajectories. However, we focused on the last core interview before death, to eliminate the possibility that caregiver reports of activities would be biased by postdeath retrospect. We also did not include reports of caregiver activity too far in advance of death, when the prognosis may be uncertain.
Fourth, because grief is normal and expected in the first year after the death of a spouse, our approach might not have captured meaningful differences between solo and supported spouses that occurred over longer time periods.
Finally, we focused on the quantity of help, not the quality of help or satisfaction with help received or provided—which may be more important for spouses.32
Study Results
We identified 1,205 older decedents who received assistance with household or self-care activities and who were married and living with their spouse in the community in the period before death. Fifty-five percent of the spouses were serving as solo caregivers, and 36 percent were assisting their spouse with support from others (exhibit 1). Among spouses who received support, two out of three were helped by their children, 40 percent received paid help, and 11 percent received support from other family or friends. (See the appendix for a breakdown of sources of care among supported spouses.)31
EXHIBIT 1. Percent of spouses of married decedents who required assistance, by caregiving role, sex, and decedent dementia status, 2000–14.
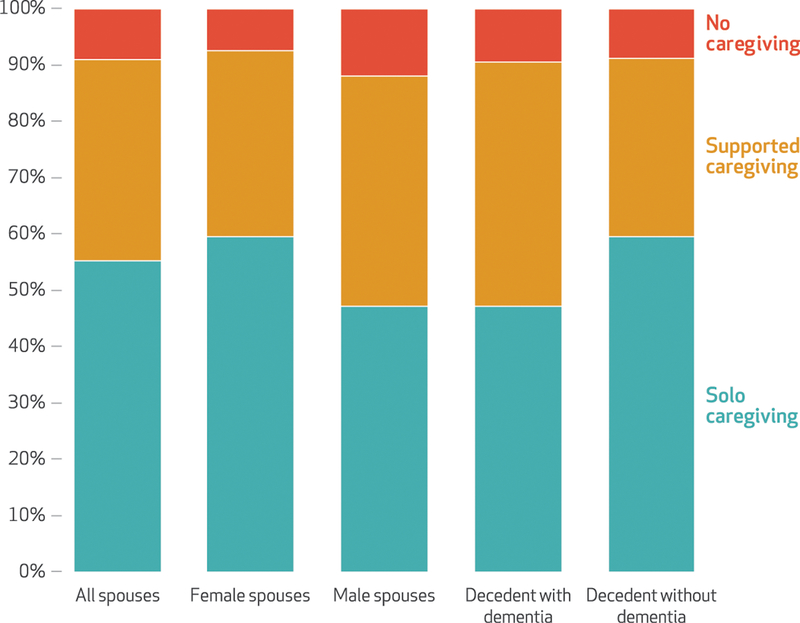
SOURCE Authors’ analysis of the Health and Retirement Study core interviews for 2000–14. NOTES Spouses’ caregiving roles were categorized as solo (that is, without additional paid or unpaid support), supported by others, or no caregiving, based on data from the decedent’s final core interview (mean: 11 months before death; range: 0–24). The analysis was based on 1,205 decedents married and living in the community with a spouse who required assistance with one or more self-care or household activities at their final core interview.
Nine percent of spouses provided no task-oriented support to their dying spouse (exhibit 1). Of these spouses, 66 percent were themselves in poor or fair health, 40 percent were ADL dependent, and more than half reported having had a hospitalization within two years. (See the appendix for characteristics of spouses who did not provide task-oriented support.)31
The proportion of spouses who were solo caregivers in the last years of life was considerable among all subgroups examined. When we restricted the sample to surviving male spouses (34 percent of the sample), we found that 47 percent were caregiving alone (exhibit 1). Similarly, among decedents with dementia, 47 percent of spouses were caregiving alone. If we also included data collected after death from the next of kin on the last three months of life, we found that an even higher proportion of spouses (61 percent) were serving as solo caregivers to dying spouses (see the appendix).31
There were significant differences across decedents when we compared them by solo caregiver status. While the majority had functional deficits in the last years of life, those with caregiver support beyond their spouses were significantly more likely to be ADL dependent than those who received help only from their spouses (85 percent versus 61 percent) (exhibit 2). They were also significantly more likely to have dementia (42 percent versus 29 percent). Commensurate with increased impairment, decedents who received care from spouses and others received twice as many hours of care per week (90 versus 43), including 20 hours more from the spouse. Additionally, decedents with solo caregiving spouses were significantly more likely than those with supported spouses to be non-Hispanic white (81 percent versus 71 percent) and less likely to be non-Hispanic black (10.1per-cent versus 16.2 percent).
EXHIBIT 2.
Characteristics of married decedents who required assistance and of their solo and supported spouse end-of-life caregivers, 2000–14
| Solo spouse caregiver (n = 666) |
Supported spouse caregiver (n = 430) |
|
|---|---|---|
| DECEDENT CHARACTERISTICS | ||
| Mean age at death (years) | 76.65 | 77.69 |
| Female (%) | 29.78 | 38.73*** |
| Race/ethnicity (%) | ||
| Non-Hispanic white | 81.27 | 71.36*** |
| Non-Hispanic black | 10.12 | 16.20*** |
| Hispanic | 7.51 | 9.84 |
| Net worth (2012 $) | 448,866.33 | 525,543.68 |
| Has Medicaid (%) | 10.02 | 19.19*** |
| Children co-reside or live within 10 miles (%) | 59.31 | 73.49*** |
| At least 1 unemployed child co-resides or lives within 10 miles (%) | 18.77** | 32.79*** |
| Comorbiditiesa (%) | ||
| 0 | 2.74 | 3.11 |
| 1–3 | 61.85 | 56.22 |
| 4–6 | 33.28 | 38.04 |
| 7 or more | 2.13 | 2.63 |
| Self-rated health poor or fair (%) | 77.89 | 82.33 |
| ADL dependent (%) | 60.90 | 85.28*** |
| IADL dependent (%) | 80.69 | 93.90*** |
| Dementia (%) | 29.13 | 41.63*** |
| Mean care received per week (hours) | 43.40 | 90.19*** |
| Death expected by familyb (%) | 61.06 | 64.68 |
| Died in hospitalb (%) | 38.50 | 34.19 |
| Nursing home resident at deathb (%) | 22.22 | 23.02 |
| SPOUSE CHARACTERISTICSc | ||
| Mean age at death (years) | 73.53 | 74.58 |
| Female (%) | 71.02 | 61.27*** |
| Comorbidities (%) | ||
| 0 | 19.14 | 15.40 |
| 1–3 | 72.13 | 74.17 |
| 4–6 | 8.73 | 10.43 |
| ADL dependent (%) | 4.95 | 8.37** |
| IADL dependent (%) | 7.81 | 17.48*** |
| Depressiond (%) | 28.62 | 35.61** |
| Self-reported health poor or fair (%) | 32.48 | 37.44 |
| Hospitalized in past 2 years (%) | 26.20 | 28.84 |
| Mean care provided per week (hours) | 43.40 | 63.34*** |
| Geographic region (%) | ||
| Northeast | 12.76 | 16.28 |
| South | 43.39 | 45.35 |
| Midwest | 26.88 | 20.93** |
| West | 16.67 | 17.21 |
| Metropolitan area | 73.12 | 75.12 |
SOURCE Authors’ analysis of the Health and Retirement Study core interviews for 2000–14 and exit interviews for 2002–14. NOTES Decedent characteristics are based on the last core interview before death unless otherwise noted (n = 1,096). Significance refers to the difference between solo and supported caregivers. Solo caregiving is explained in the notes to exhibit 1. ADL is activity of daily living. IADL is instrumental activity of daily living.
Comorbidity count based on self-report of cancer, lung disease, congestive heart failure, other heart condition, stroke, memory problems, hypertension, diabetes, or psychiatric problems.
Based on an exit (postdeath) interview of the spouse or another knowledgeable person.
Based on the spouse’s last core interview before bereavement.
Defined as a score of 3 or more on the eight-item Center for Epidemologic Studies Depression Scale.
p < 0.05
p < 0.01
Despite differences in decedents’ functional needs by solo caregiving status, we did not find significant differences by location of death, nursing home residence, or reports by next of kin that death was expected. Of note, while the majority of decedents with solo spouse caregivers had children living close by (59 percent), decedents who were cared for by their spouse and others were more likely to have children co-residing with them or living within ten miles (73 percent). One-third of supported spouses had at least one unemployed child living close by, compared to only 19 percent of solo spouse caregivers. The solo spouses differed from those who received support in providing care: They were significantly less likely to have functional limitations (5 percent versus 8 percent had ADL dependence).
Solo caregivers were engaged in extensive care tasks at the end of the decedent’s life (exhibit 3), averaging more than forty hours per week (exhibit 2). For example, more than one-third of these caregivers provided assistance with bathing. Solo caregivers of decedents with dementia spent more time helping (mean: 61.9 hours per week), compared to all solo caregivers (data not shown). They were more likely than all solo caregivers to assist with key self-care activities such as bathing (42 percent) as well as with all household activities (exhibit 3).
EXHIBIT 3. Percent of spouses who provided assistance with self-care and household tasks among solo caregiving spouses of married decedents in the last years of life, by type of assistance and decedent dementia status, 2000–14.
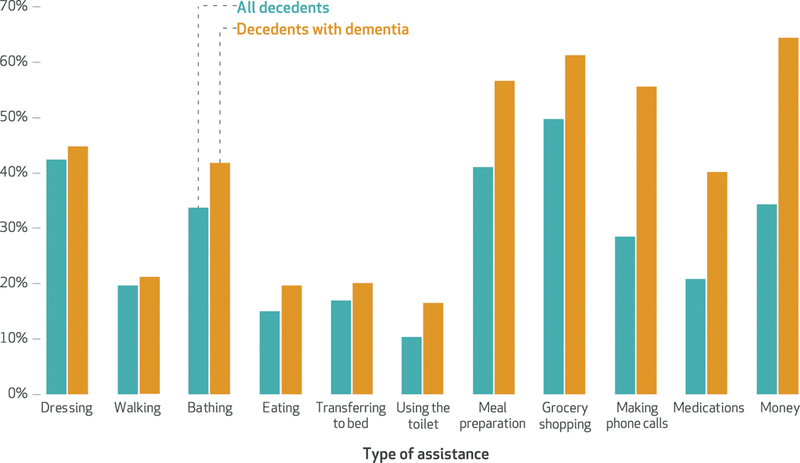
SOURCE Authors’ analysis of the Health and Retirement Study core interviews for 2000–14. NOTES The analysis was based on 666 solo caregiving spouses married to a decedent who required assistance with one or more self-care or household activities at their final core interview. Solo caregiving is explained in the notes to exhibit 1. “Money” is managing finances.
Finally, we compared surviving spouses’ level of depression and other key indicators of health and function after bereavement based on solo caregiver status, and we examined the association of solo caregiving status with depression and other negative postbereavement outcomes. Although solo caregivers were less likely to be depressed before bereavement, compared to supported caregivers (exhibit 2), the two groups had similarly elevated levels of depression after bereavement (39 percent versus 42 percent) (exhibit 4).While solo caregivers were less likely to have ADL and IADL dependence and to have been hospitalized than other spouses in the two years after bereavement, there were no differences in postbereavement mortality or nursing home entry between the groups. When we controlled for decedent and spouse characteristics, including the surviving spouse’s outcome measures before bereavement, we found no association between solo caregiving status and any post-bereavement outcomes. (Additional analyses using sampling weights are in the appendix.)31
EXHIBIT 4.
Postbereavement outcomes for surviving spouses of married decedents who required assistance, by caregiving status, 2000–14
| Solo caregivers |
Supported caregivers |
Odds ratio |
||
|---|---|---|---|---|
| (n = 626) | (n = 389) | Model 1a | Model 2b | |
| Depressionc | 39.46% | 41.55% | 1.05 | 1.05 |
| Self-reported health poor or fair | 32.91 | 38.40 | 0.81 | 0.96 |
| ADL dependent | 6.07 | 12.34*** | 0.47*** | 0.67 |
| IADL dependent | 15.20 | 23.65*** | 0.73 | 0.95 |
| Hospitalizations in past 2 years | 29.70 | 36.95** | 0.74** | 0.76 |
| Nursing home residentd | 2.40 | 2.57 | 0.69 | 0.93 |
| Spouse died within 12 months of decedent deathd | 3.60 | 5.12 | 0.68 | 0.83 |
SOURCE Authors’ analysis of the Health and Retirement Study core interviews for 2000–14 and exit interviews for 2002–14. NOTES Significance refers to the difference between solo and supported caregivers.The difference in percentages is based on chi-square analyses.
Logistic regression that controlled for dependent variable status before bereavement only.
Logistic regression that controlled for surviving spouse’s age, sex, race/ethnicity, depression, self-rated health, hospitalizations, and activity of daily living (ADL) and instrumental activity of daily living (IADL) dependence before bereavement; and decedent’s Medicaid status, dementia status, presence of children within ten miles, and hours of help received from all sources before bereavement.
Defined as a score of 3 or more on the eight-item Center for Epidemologic Studies Depression Scale.
Because surviving spouses co-resided with their partner before bereavement, spousal death and nursing home status models did not control for prebereavement status.
p < 0.05
p< 0.01
Discussion
This nationally representative study of older adults in the US found that people frequently serve as the only caregiver for their spouse during the last years of life. The majority of spouses who provided care at home in the last years of life did not receive any support—paid or unpaid—for self-care or household tasks. People who were cared for by their spouses alone had less functional and cognitive impairment than those whose spouses were supported, which suggests that nonspousal family members or paid caregivers might not become involved with self-care and household tasks until care needs increase, regardless of prognosis. However, decedents cared for by solo spouses were still highly dependent, requiring more than forty hours of care per week, on average. Solo caregiving was also common among spouses of people with dementia in the last years of life, despite the fact that dementia caregiving poses unique difficulties and increased burden for caregivers,33,34 especially to-ward the end of life.35
Depression was common among bereaved spouses regardless of solo caregiving status, and we did not observe an increase in depression after bereavement among solo caregivers compared to those who had had support, as we hypothesized. We also did not detect significant declines in self-reported health, functional impairment, or increased health care use for solo caregivers compared to supported caregivers. While according to the stress process model36 the increased stress of caregiving alone and the provision of more care should result in increased psychological distress for solo caregivers and challenges after bereavement, this is not always the case. Indeed, individual characteristics—including genetic predisposition—are associated with caregiver depression,37 and many caregivers report low levels of stress and experience benefits from caregiving.38
Although we hypothesized that receiving more help from other family members would reduce stress,39 supported spouses may face additional challenges—including disagreements about decision making and increased strain—when they receive support from other caregivers.40 Continued research in this area is especially important as demographic trends portend fewer children41 and greater distance among family members,42 thus increasingly leaving available spouses to serve alone. Simultaneously, the personal preferences of the caregiver, including the desire to care alone for spouses as long as possible, must be considered. Choosing to play a caregiving role independently maybe a spouse’s preference and offer a meaningful and highly valued personal experience. For some spouses, stepping into the role of solo caregiver maybe beneficial and help them feel more connected to their loved one.43–45
Our findings are the first to document wide-spread solo spousal caregiving for people with serious illness in the last years of life using a national sample, and they can inform supportive interventions and policies. While the availability of adult children to provide support is a key factor in determining whether a spouse will provide care alone, it does not guarantee support. Among solo caregiving spouses, more than half had children living with them or not far away, which suggests that geographic proximity might not be enough to mobilize caregiving action. In our sample, the majority of adult children living with or close to a dying parent were employed at least part time, which may limit flexibility to provide assistance.
The nearly one in ten co-resident spouses who were not involved in helping with any self-care or household tasks were often themselves in poor health. These findings challenge assumptions that the availability of family translates into actual caregiving support and underscores the need to more thoroughly assess the health, capacity, and unmet needs of the caregiver in all clinical settings.46
Our finding that female spouses were caregiving alone more often than male spouses is consistent with evidence that female caregivers are less likely to ask for help and more likely to sacrifice competing priorities, including work and social activities, than male caregivers are. Gender differences in the provision of caregiving and its negative consequences on well-being are well documented.47–49 During the last years of life, women may feel particularly burdened by additional financial strains.50,51 Yet we found that almost half of male caregivers were unsupported, which highlights the need to reexamine beliefs around gender differences in caregiving. In particular, traditional assumptions about help-seeking behaviors and postbereavement depression might not fully take into account the heterogeneity of caregivers and their circumstances.
Care for seriously ill older adults is increasingly shifting toward home and community-based settings. While this shift is intended to maximize health care value and is a key strategy for delivering coordinated, patient-centered care, we must assess to what extent this confers additional burden on family caregivers and how best to mediate that impact. A national strategy for caregivers and supportive caregiving policies is in progress as a result of the Recognize, Assist, Include, Support, and Engage (RAISE) Family Caregivers Act52 and was highlighted in Families Caring for an Aging America, a 2016 report from the National Academies of Sciences, Engineering, and Medicine.1 Related recommendations include identifying family caregiver needs by routinely assessing the caregiving situation and determining caregivers’ ability and willingness to assist a care recipient.53 This assessment approach is a critical first step toward elucidating family structure, resources, and potential challenges. Caregiver assessment is not widely integrated in health care delivery settings but is particularly important in settings where seriously ill older adults frequently receive care, such as oncology and geriatrics practices, as well as in the context of end-of-life hospice care.
The Caregiver Advise, Record, Enable (CARE) Act,54 which has been passed in forty states and territories and requires hospitals to identify family caregivers and engage them as the care recipient transitions from hospital to home, affords opportunities to expand caregiver assessment and support. Medicare’s implementation of new reimbursement codes for dementia care planning may also prove beneficial. The codes reimburse providers for time spent creating a comprehensive care plan that includes caregiver assessment.55
Finally, there is a need to broaden the comprehensiveness, availability, and diversity of supports that afford individuals and families the ability to balance work and family responsibilities. More robust community supports are needed, such as those available through the National Family Caregiver Support Program.56 Despite substantial state policy action, few Americans have access to paid family leave.57 Furthermore, there is a need for more widespread availability of palliative care services for seriously ill patients in homes and communities, especially in the last years of life.58 Such patients, who may have significant care needs for years, are ineligible for hospice until the final months of life and may have limited access to nonhospice palliative care services outside of the hospital. The expansion of community-based palliative care would provide critical support to vulnerable, seriously ill patients and their caregivers.59
The strengths of our study include the prospective collection of data, the linked nature of decedent and caregiver surveys, and a design that limited recall bias.60 While this study focused on spousal caregivers, future research should examine the likelihood and consequences of solo caregiving experiences for nonspouses as well, including non-kin support networks.
Conclusion
There is an increased reliance on family caregivers who have little or no training to assist seriously ill older adults at home in the last years of life with personal care and household tasks. Spouses, who are commonly undertaking this role alone, are particularly vulnerable caregivers as they themselves are older, in poor health, and facing the negative emotional and financial experience of a spouse’s death. Assessing caregiver strain and providing support for family caregivers of people with serious illness is crucial in the last years of life. Doing so will ultimately require changing the focus of serious illness care from the patient to the family unit.
Supplementary Material
Acknowledgments
The study investigators were supported by the National Institute on Aging (Grant Nos. K01AG047923 and R01AG060967 to Katherine Ornstein, R01AG054540 to Amy Kelley, and R01AG047859 to Jennifer Wolff). The Health and Retirement Study is sponsored by the National Institute on Aging (Grant No. NIA U01AG009740) and the Social Security Administration and is conducted by the University of Michigan.
Contributor Information
Katherine A. Ornstein, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, in New York City..
Jennifer L. Wolff, Johns Hopkins University, in Baltimore, Maryland..
Evan Bollens-Lund, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai..
Omari-Khalid Rahman, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai..
Amy S. Kelley, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai..
NOTES
- 1.National Academies of Sciences, Engineering, and Medicine. Families caring for an aging America. Washington (DC): National Academies Press; 2016. [PubMed] [Google Scholar]
- 2.Wolff JL, Spillman BC, Freedman VA, Kasper JD. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med. 2016; 176(3):372–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Dying in America: improving quality and honoring individual preferences near the end of life. Washington (DC): National Academies Press; 2015. [PubMed] [Google Scholar]
- 4.Ornstein KA, Kelley AS, Bollens-Lund E, Wolff JL. A national profile of end-of-life caregiving in the United States. Health Aff (Millwood). 2017;36(7):1184–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teno JM, Montgomery R, Valuck T, Corrigan J, Meier DE, Kelley A, et al. Accountability for community-based programs for the seriously ill. J Palliat Med. 2018;21(S2):S81–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stajduhar K, Funk L, Toye C, Grande G, Aoun S, Todd C. Part 1: home-based family caregiving at the end of life: a comprehensive review of published quantitative research (1998–2008). Palliat Med. 2010; 24(6):573–93. [DOI] [PubMed] [Google Scholar]
- 7.Kelley AS, McGarry K, Fahle S, Marshall SM, Du Q, Skinner JS. Out-of-pocket spending in the last five years of life. J Gen Intern Med. 2013;28(2):304–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pottie CG, Burch KA, Thomas LP, Irwin SA. Informal caregiving of hospice patients. J Palliat Med. 2014;17(7):845–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pinquart M, Sörensen S. Differences between caregivers and noncore-givers in psychological health and physical health: a meta-analysis. Psychol Aging. 2003;18(2):250–67. [DOI] [PubMed] [Google Scholar]
- 10.Wolff JL, Dy SM, Frick KD, Kasper JD. End-of-life care: findings from a national survey of informal care-givers. Arch Intern Med. 2007; 167(1):40–6. [DOI] [PubMed] [Google Scholar]
- 11.Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008; 300(14):1665–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ornstein KA, Aldridge MD, Garrido MM, Gorges R, Bollens-Lund E, Siu AL, et al. The use of life-sustaining procedures in the last month oflife is associated with more depressive symptoms in surviving spouses. J Pain Symptom Manage. 2017;53(2): 178–187.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ornstein KA, Garrido MM, Siu AL, Bollens-Lund E, Langa KM, Kelley AS. Impact of in-hospital death on spending for bereaved spouses. Health Serv Res. 2018;53(Suppl 1): 2696–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright AA, Keating NL, Balboni TA, Matulonis UA, Block SD, Prigerson HG. Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers’ mental health. J Clin Oncol. 2010;28(29):4457–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ornstein KA, Aldridge MD, Garrido MM, Gorges R, Meier DE, Kelley AS. Association between hospice use and depressive symptoms in surviving spouses. JAMA Intern Med. 2015; 175(7):1138–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sullivan AR, Fenelon A. Patterns of widowhood mortality. J Gerontol B Psychol Sci Soc Sci. 2014;69(1): 53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah SM, Carey IM, Harris T, Dewilde S, Victor CR, Cook DG. Impact of partner bereavement on quality of cardiovascular disease management. Circulation. 2013; 128(25):2745–53. [DOI] [PubMed] [Google Scholar]
- 18.Ornstein KA, Garrido MM, Siu AL, Bollens-Lund E, Rahman OK, Kelley AS. An examination of downstream effects of bereavement on healthcare utilization for surviving spouses in a national sample of older adults. Pharmacoeconomics. 2019. March 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pinquart M, Sorensen S. Spouses, adult children, and children-in-law as caregivers of older adults: a meta-analytic comparison. Psychol Aging. 2011;26(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Savundranayagam MY, Orange JB. Relationships between appraisals of caregiver communication strategies and burden among spouses and adult children. Int Psychogeriatr. 2011;23(9):1470–8. [DOI] [PubMed] [Google Scholar]
- 21.Schulz R, Hebert R, Boerner K. Bereavement after caregiving. Geriatrics. 2008;63(1):20–2. [PMC free article] [PubMed] [Google Scholar]
- 22.Seltzer MM, Li LW. The dynamics of caregiving: transitions during a three-year prospective study. Gerontologist. 2000;40(2):165–78. [DOI] [PubMed] [Google Scholar]
- 23.Robinson KM, Buckwalter KC, Reed D. Predictors of use of services among dementia caregivers. West J Nurs Res. 2005;27(2):126–40, discussion 141–7. [DOI] [PubMed] [Google Scholar]
- 24.Schulz R, Beach SR, Cook TB, Martire LM, Tomlinson JM, Monin JK. Predictors and consequences of perceived lack of choice in becoming an informal caregiver. Aging Ment Health. 2012;16(6):712–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Verdery AM, Margolis R. Projections of white and black older adults without living kin in the United States, 2015 to 2060. Proc Natl Acad Sci USA. 2017;114(42):11109–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klinenberg E Social isolation, loneliness, and living alone: identifying the risks for public health. Am J Public Health. 2016;106(5):786–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dong J, Pollack H, Konetzka RT. Effects of long-term care setting on spousal health outcomes. Health Serv Res. 2019;54(1):158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Health and Retirement Study [home page on the Internet]. Ann Arbor (MI): University of Michigan, Institute for Social Research; [cited 2019 Apr 4]. Available from: http://hrsonline.isr.umich.edu/ [Google Scholar]
- 29.Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14): 1326–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Radloff L The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 31.To access the appendix, click on the Details tab of the article online.
- 32.Savundranayagam MY. Receiving while giving: the differential roles of receiving help and satisfaction with help on caregiver rewards among spouses and adult-children. Int J Geriatr Psychiatry. 2014;29(1):41–8. [DOI] [PubMed] [Google Scholar]
- 33.Dassel KB, Carr DC, Vitaliano P. Does caring for a spouse with dementia accelerate cognitive decline? Findings from the Health and Retirement Study. Gerontologist. 2017;57(2):319–28. [DOI] [PubMed] [Google Scholar]
- 34.Kim Y, Schulz R. Family caregivers’ strains: comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. J Aging Health. 2008;20(5): 483–503. [DOI] [PubMed] [Google Scholar]
- 35.Vick JB, Ornstein KA, Szanton SL, Dy SM, Wolff JL. Does caregiving strain increase as patients with and without dementia approach the end of life? J Pain Symptom Manage. 2019;57(2):199–208.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30(5):583–94. [DOI] [PubMed] [Google Scholar]
- 37.Vitaliano PP, Strachan E, Dansie E, Goldberg J, Buchwald D. Does care-giving cause psychological distress? The case for familial and genetic vulnerabilities in female twins. Ann Behav Med. 2014;47(2):198–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roth DL, Fredman L, Haley WE. In-formal caregiving and its impact on health: a reappraisal from population-based studies. Gerontologist. 2015;55(2):309–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Friedemann ML, Buckwalter KC. Family caregiver role and burden related to gender and family relationships. J Fam Nurs. 2014;20 (3):313–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wittenberg-Lyles E, Kruse RL, Oliver DP, Demiris G, Petroski G. Exploring the collective hospice caregiving experience. J Palliat Med. 2014; 17(1):50–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gobbi PE. A model of voluntary childlessness. J Popul Econ. 2013; 26(3):963–82. [Google Scholar]
- 42.Ruggles S The decline of intergenerational coresidence in the United States, 1850 to 2000. Am Sociol Rev. 2007;72(6):964–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roff LL, Burgio LD, Gitlin L, Nichols L, Chaplin W, Hardin JM. Positive aspects of Alzheimer’s caregiving: the role of race. J Gerontol B Psychol Sci Soc Sci. 2004;59(4):185–90. [DOI] [PubMed] [Google Scholar]
- 44.Tarlow BJ, Wisniewski SR, Belle SH, Rubert M, Ory MG, Gallagher-Thompson D. Positive aspects of caregiving: contributions of the REACH project to the development of new measures for Alzheimer’s caregiving. Res Aging. 2004 2004; 26(4):429–53. [Google Scholar]
- 45.Cohen CA, Colantonio A, Vernich L. Positive aspects of caregiving: rounding out the caregiver experience. Int J Geriatr Psychiatry. 2002;17(2):184–8. [DOI] [PubMed] [Google Scholar]
- 46.Ferrell BR, Twaddle ML, Melnick A, Meier DE. National Consensus Project Clinical Practice Guidelines for Quality Palliative Care guidelines, 4th edition. J Palliat Med. 2018. September 4. [DOI] [PubMed] [Google Scholar]
- 47.Morgan T, Ann Williams L, Trussardi G, Gott M. Gender and family caregiving at the end-of-life in the context of old age: a systematic review. Palliat Med. 2016;30(7): 616–24. [DOI] [PubMed] [Google Scholar]
- 48.Washington KT, Pike KC, Demiris G, Parker Oliver D, Albright DL, Lewis AM. Gender differences in caregiving at end of life: implications for hospice teams. J Palliat Med. 2015;18(12):1048–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pinquart M, Sörensen S. Gender differences in caregiver stressors, social resources, and health: an up-dated meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2006;61(1): 33–45. [DOI] [PubMed] [Google Scholar]
- 50.Burkhauser RV, Giles P, Lillard DR, Schwarze J. Until death do us part: an analysis of the economic well-being of widows in four countries. J Gerontol B Psychol Sci Soc Sci. 2005;60(5):S238–46. [DOI] [PubMed] [Google Scholar]
- 51.DiGiacomo M, Lewis J, Phillips J, Nolan M, Davidson PM. The business of death: a qualitative study of financial concerns of widowed older women. BMC Womens Health. 2015; 15:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.S.1028—RAISE Family Caregivers Act [Internet].Washington (DC): Congress.gov; 2017. September 27 [cited 2019 Apr 4]. Available from: https://www.congress.gov/bill/115th-congress/senate-bill/1028?q=%7B”search”%3A%5B”RAISE+Family+Caregivers+Act”%5D%7D&r=1 [Google Scholar]
- 53.Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood). 2013;32(2):223–31. [DOI] [PubMed] [Google Scholar]
- 54.AARP. New state law to help family caregivers [Internet]. Washington (DC): AARP; [cited 2019 Apr 4]. Available from: https://www.aarp.org/politics-society/advocacy/caregiving-advocacy/info-2014/aarp-creates-model-state-bill.html [Google Scholar]
- 55.Borson S, Chodosh J, Cordell C, Kallmyer B, Boustani M, Chodos A, et al. Innovation in care for individuals with cognitive impairment: can reimbursement policy spread best practices? Alzheimers Dement. 2017;13(10):1168–73. [DOI] [PubMed] [Google Scholar]
- 56.Administration for Community Living. National Family Caregiver Support Program [Internet]. Washington (DC): ACL; [last modified 2019. Mar 26; cited 2019 Apr 4]. Available from: https://acl.gov/programs/support-caregivers/national-family-caregiver-support-program [Google Scholar]
- 57.Feinberg LF. Paid family leave: an emerging benefit for employed family caregivers of older adults. J Am Geriatr Soc. 2019. March 18. [DOI] [PubMed] [Google Scholar]
- 58.Meier DE, Back AL, Berman A, Block SD, Corrigan JM, Morrison RS. A national strategy for palliative care. Health Aff (Millwood). 2017;36(7): 1265–73. [DOI] [PubMed] [Google Scholar]
- 59.Ornstein KA, Schulz R, Meier DE. Families caring for an aging America need palliative care. J Am Geriatr Soc. 2017;65(4):877–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Teno JM. Measuring end-of-life care outcomes retrospectively. J Palliat Med. 2005;8(Suppl 1):S42–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


