Abstract
Background and Purpose
Emergency medical services (EMS) stroke recognition facilitates rapid care, however prehospital stroke screening tools rely on signs that are often absent in posterior circulation strokes. We hypothesized that addition of the finger-to-nose (FTN) test to the Cincinnati Prehospital Stroke Scale would improve EMS posterior stroke recognition.
Methods
In this controlled before-and-after study of consecutive EMS-transported posterior ischemic strokes, paramedics in a single EMS agency received in-person training in the use of the FTN test. Paramedics at two other local EMS agencies served as controls. We compared the change in posterior stroke recognition, door-to-CT (DTCT) times, and alteplase delivery between the FTN (intervention) and control agencies.
Results
Over 21 months, 51 posterior circulation strokes were transported by the FTN agency, and 88 in the control agencies. Following training, posterior stroke recognition improved from 46% to 74% (p=0.039) in the FTN agency, whereas there was no change in the control agencies (32% before versus 39% after, p=0.467). Mean DTCT time in the FTN agency also improved following training (62 to 41 minutes, p=0.037), but not in the control agencies (58 to 61 minutes, p=0.771). There was no difference in alteplase delivery.
Conclusion
Paramedics trained in the FTN test were more likely to identify posterior stroke. If future studies confirm these findings, such training may expedite the care of posterior stroke patients transported by EMS.
Keywords: Emergency Medical Services, stroke, diagnosis
Introduction
The efficacy of acute ischemic stroke treatment is time-dependent,1 requiring coordinated, efficient systems of care to ensure rapid evaluation of stroke patients. Patients with ischemic stroke in the posterior circulation are less likely to exhibit unilateral weakness and more likely to present with nonspecific symptoms such as dizziness, altered mental status, and imbalance than anterior strokes.2 As a result, these patients are at higher risk of ED misdiagnosis3, 4 and delays in treatment.5, 6
Emergency medical services (EMS) transported stroke patients receive faster emergency department (ED) evaluations and treatment,7 benefits closely tied to EMS stroke recognition and hospital prenotification.8–10 Difficulties with posterior stroke recognition are exacerbated in the prehospital setting because prehospital stroke screening tools such as the Cincinnati Prehospital Stroke Scale (CPSS)11 rely on unilateral motor deficits, which preferentially identify anterior strokes.2, 5 We previously noted that 30% of EMS unrecognized stroke patients exhibited limb ataxia in the ED.9 Based on this, we hypothesized that training paramedics to assess for upper limb ataxia using the finger-to-nose (FTN) examination12 would enhance prehospital posterior stroke recognition.
Methods
The data supporting the study findings are available from the corresponding author.
Design
This pilot study was embedded within a larger quality improvement project wherein all paramedics in a single county received stroke training followed by performance feedback.13 In addition to the standard training, paramedics within the largest agency received training in the FTN test with a prespecified plan to examine posterior stroke recognition in this agency using a controlled before-and-after design.12 The study was approved with waiver of consent by the IRBs of Michigan State University and each participating hospital.
Patients
Cases with a hospital discharge diagnoses indicating a posterior circulation ischemic stroke were identified from a database of all EMS-transported stroke cases in the county.14 Patients with unspecified stroke location were excluded. Additionally, we restricted analysis to patients transported within 12 months prior and up to 9 months following the intervention (excluding cases the one-month training period) because the FTN agency contributed 9 months of post-training data (figure 1). Cases were considered EMS-recognized if the prehospital record indicated a primary or secondary impression of stroke or transient ischemic attack.
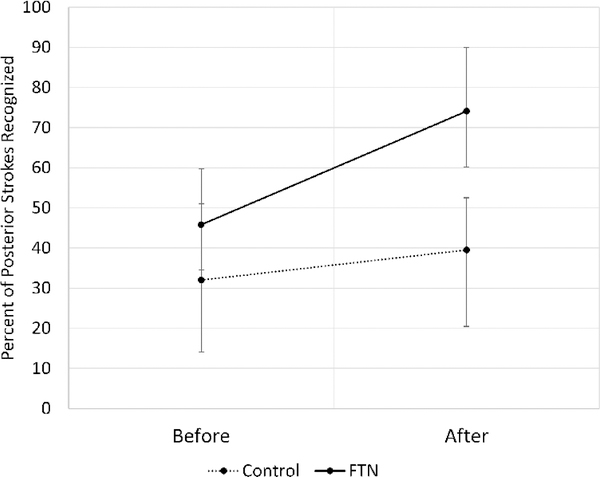
Figure :
EMS posterior stroke recognition by study group and period
FTN Training
All 146 paramedics in the FTN agency watched a video describing the performance and interpretation of the FTN test. Paramedics were instructed to perform the FTN test for patients with neurological symptoms (weakness, dizziness, vision changes, altered mental status, or focal neurological symptoms) and an otherwise negative CPSS. Paramedics were required to demonstrate competency in the FTN test by performing it in-person for an EMS educator.
Statistical analysis
Descriptive statistics were used to characterize the study population. Chi-square tests for trend were used to assess quarterly recognition rates during the pre-intervention period. We compared EMS posterior stroke recognition after training to the pre-training period in both the FTN and control agencies. Secondary outcomes included mean door-to-CT (DTCT) times and alteplase delivery. Comparisons were made using chi square tests, t-tests, and Kruskal-Wallis tests. We also performed a difference-in-differences (DID) regression analysis to estimate the change in recognition rates attributable to transport in the post-intervention period by the intervention group.14
Results
Over 21 months, EMS transported 777 hospital-confirmed acute ischemic stroke patients; 139 (18%) were posterior circulation strokes (Table 1). Pre-training posterior stroke recognition rates were non-significantly different between the FTN agency and control agencies (45.5% vs 32.0%, p=0.247) and there were no significant trends in quarterly posterior stroke recognition rates in either the control (p=0.454) or the FTN (p=0.334) agencies.
Table 1:
Characteristics of 129 EMS Transported Posterior Ischemic Strokes
| Control (N=88) | FTN (N=51) | |||||
|---|---|---|---|---|---|---|
| Before n=50 (%) | After n=38 (%) | p-value | Before n=24 (%) | After n=27 (%) | p-value | |
| Mean Age (SD) | 74 (15) | 71 (14) | 0.337 | 75 (12) | 72 (14) | 0.481 |
| Female | 22 (44) | 13 (34) | 0.353 | 9 (38) | 14 (52) | 0.304 |
| Non-White Race | 11 (22) | 3 (8) | 0.200 | 4 (17) | 7 (26) | 0.415 |
| Dispatched for Stroke | 15 (30) | 15 (40) | 0.353 | 9 (38) | 13 (48) | 0.443 |
| Vomiting | 9 (18) | 9 (24) | 0.513 | 4 (17) | 4 (15) | 0.856 |
| Headache | 9 (18) | 7 (18) | 0.960 | 3 (13) | 2 (7) | 0.542 |
| Dizziness | 8 (16) | 14 (37) | 0.025 | 4 (17) | 1 (4) | 0.120 |
| Ataxia | 5 (10) | 9 (24) | 0.082 | 1 (4) | 4 (15) | 0.202 |
| Gaze Preference | 3 (6) | 1 (3) | 0.452 | 3 (13) | 1 (4) | 0.244 |
| Vision Change | 3 (6) | 2 (5) | 0.882 | 2 (8) | 1 (4) | 0.483 |
| Median NIHSS (IQR) | 7 (4–13) | 3 (1–6) | 0.003 | 6 (3–10) | 6 (2–9) | 0.574 |
EMS=Emergency medical services; FTN=finger-to-nose; IQR=Interquartile range; DTCT=Door-to-CT
Following the intervention, posterior stroke recognition increased significantly from 45.8% to 74.1% in the FTN agency (p=0.039) but not the control agencies (32.0% to 39.5%, p=0.467, Figure). Prenotification rates and overcall rates among recognized strokes did not change (supplemental tables I and II). Average DTCT time decreased following the intervention in the FTN group (62 to 41 minutes, p=0.037, Table 2) but not among controls (58 to 61 minutes, p=0.771). There were no differences in alteplase delivery (Table 2).
Table 2:
Secondary outcomes by study group and period.
| Control (N=88) | FTN (N=51) | |||||
|---|---|---|---|---|---|---|
| Before (n=50) | After (n=38) | p-value | Before (n=24) | After (n=27) | p-value | |
| Mean DTCT Time (SD) | 58 (46) | 61 (47) | 0.771 | 62 (43) | 41 (22) | 0.037* |
| Alteplase Delivery (%) | 5 (10.0) | 8 (21.5) | 0.148 | 3 (12.5) | 1 (3.7) | 0.244† |
EMS=Emergency Medical Services; DTCT=Door-to-CT; SD=Standard deviation.
t-test
chi square test
DID analysis revealed a 21% absolute increase in EMS posterior stroke recognition attributable to the intervention (DID 20.8%, 95% CI −12.7% to 54.3%) but this difference was not statistically significant (p=0.223).
Discussion
Patients with posterior circulation ischemic stroke are at risk for misdiagnosis3, 4 and delayed treatment.5 Earlier recognition by EMS may expedite care, however prehospital stroke screening tools rely on signs more common among anterior strokes.2, 5 We present a pilot study suggesting that educating paramedics in the FTN examination may improve prehospital posterior stroke recognition.
Prior to training, a minority of EMS-transported posterior circulation strokes were recognized (36%). Following FTN training, paramedics demonstrated a 28% increase in posterior stroke recognition, while those who received general stroke training improved only 7%. Difference in differences analysis suggested about 21% absolute improvement in the FTN group following training, however the confidence interval around this estimate was very wide (−12% to 54%) due to the small sample size of this pilot study.
Corresponding to the increase in posterior stroke recognition rates in the FTN group, we observed a decrease in average DTCT time (−21 minutes, 95% CI −1 to −41 minutes). This finding supports a previously hypothesized link between EMS stroke recognition and faster DTCT times.8, 9 Despite gains in evaluation efficiency, patients transported by the FTN agency received alteplase less often. While it there is no logical reason for the training to reduce alteplase delivery, this finding highlights the fact that many posterior circulation strokes are not alteplase candidates.
This study has several limitations. First, the sample size in this pilot study was very small, thus we were unable to adjust for differences in stroke symptoms or severity, which might contribute to stroke recognition. Second, due to limitations in EMS documentation, we are unable to attribute stroke recognition to FTN test performance directly. Finally, this study was conducted in the context of a universal EMS stroke training program, which may have biased our findings toward the null.
Nevertheless, the dramatic improvement in posterior stroke recognition and concomitant reduction in mean DTCT times we observed following FTN training are promising findings. If confirmed by a larger study, this simple training could meaningfully enhance care for patients with posterior circulation ischemic stroke.
Supplementary Material
Acknowledgments
Funding: American Heart Association Mentored Clinical and Population Research Award (Oostema, Reeves, 15MCPRP24470121).
Funding: American Heart Association Mentored Clinical and Population Research Award (15MCPRP24470121).
Footnotes
Disclosures: none
Contributor Information
J. Adam Oostema, Spectrum Health, Michigan State University College of Human Medicine, Secchia Center, 15 Michigan, NE, Grand Rapids, MI 49503.
Todd Chassee, Kent County Emergency Medical Services.
William Baer, Mercy Health St Mary’s Hospital.
Allison Edberg, Metro Health Hospital.
Mathew J. Reeves, Michigan State University College of Human Medicine.
References
- 1.Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: A meta-analysis of individual patient data from randomised trials. The Lancet. 2014;384:1929–1935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tao W-D, Liu M, Fisher M, Wang D-R, Li J, Furie KL, et al. Posterior versus anterior circulation infarction: How different are the neurological deficits? Stroke. 2012;43:2060–2065 [DOI] [PubMed] [Google Scholar]
- 3.Madsen TE, Khoury J, Cadena R, Adeoye O, Alwell KA, Moomaw CJ, et al. Potentially missed diagnosis of ischemic stroke in the emergency department in the Greater Cincinnati/Northern Kentucky stroke study. Acad Emerg Med. 2016;23:1128–1135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Venkat A, Cappelen-Smith C, Askar S, Thomas PR, Bhaskar S, Tam A, et al. Factors associated with stroke misdiagnosis in the emergency department: A retrospective case-control study. Neuroepidemiology. 2018;51:123–127 [DOI] [PubMed] [Google Scholar]
- 5.Sarraj A, Medrek S, Albright K, Martin-Schild S, Bibars W, Vahidy F, et al. Posterior circulation stroke is associated with prolonged door-to-needle time. International Journal of Stroke. 2015;10:672–678 [DOI] [PubMed] [Google Scholar]
- 6.Sommer P, Seyfang L, Posekany A, Ferrari J, Lang W, Fertl E, et al. Prehospital and intra-hospital time delays in posterior circulation stroke: Results from the Austrian stroke unit registry. Journal of Neurology. 2017;264:131–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ekundayo OJ, Saver JL, Fonarow GC, Schwamm LH, Xian Y, Zhao X, et al. Patterns of emergency medical services use and its association with timely stroke treatment: Findings from Get with the Guidelines-Stroke. Circulation: Cardiovascular Quality and Outcomes. 2013;6:262–269 [DOI] [PubMed] [Google Scholar]
- 8.Abboud ME, Band R, Jia J, Pajerowski W, David G, Guo M, et al. Recognition of stroke by ems is associated with improvement in emergency department quality measures. Prehosp Emerg Care. 2016;20:729–736 [DOI] [PubMed] [Google Scholar]
- 9.Oostema JA, Konen J, Chassee T, Nasiri M, Reeves MJ. Clinical predictors of accurate prehospital stroke recognition. Stroke. 2015;46:1513–1517 [DOI] [PubMed] [Google Scholar]
- 10.Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, et al. Patterns, predictors, variations, and temporal trends in emergency medical service hospital prenotification for acute ischemic stroke. Journal of the American Heart Association. 2012;1:e002345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kothari R, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati prehospital stroke scale: Reproducibility and validity. Ann Emerg Med. 1999;33:373–378 [DOI] [PubMed] [Google Scholar]
- 12.Fugl-Meyer AR, Jaasko L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. A method for evaluation of physical performance. The Scandinavian Journal of Rehabilitation Medicine. 1975;7:13–31 [PubMed] [Google Scholar]
- 13.Oostema JA, Chassee T, Baer W, Edberg A, Reeves MJ. Brief educational intervention improves emergency medical services stroke recognition. Stroke. 2019;50:1193–1200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: The difference-in-differences approach. JAMA. 2014;312:2401–2402 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.