Abstract
Study Objectives:
Postpartum depression (PPD) occurs in 15% to 20% of mothers worldwide and is associated with adverse outcomes for mother and child. Prior research has established a relationship between concurrent sleep quality and PPD. We conducted a secondary analysis in 45 women with mood disorders to study overall sleep quality (and individual components of sleep), measured in the early postpartum period, as a predictor of subsequent PPD.
Methods:
We measured sleep quality using the Pittsburgh Sleep Quality Index (PSQI; subscale and total scores) at 1 month postpartum (and during the third trimester). We measured depressive symptoms using the Inventory of Depressive Symptoms, Self-Report (IDS-SR) at 3 months postpartum. We used bivariate and multivariate linear regression models to study the association between PSQI and IDS scores.
Results:
We found that higher global PSQI scores as well as higher component scores for self-reported sleep quality, sleep latency, sleep efficiency, sleep medication usage, and daytime dysfunction, measured 1 month postpartum, were associated with increased IDS scores (at 3 months postpartum (P = .01, .01, .01, .003, < .001, respectively). We did not find an association between poor sleep quality in the third trimester and PPD.
Conclusions:
Poor sleep quality in the early postpartum period independently predicts development of later PPD. This is clinically significant and highlights the importance of sleep interventions as an immediate postpartum therapeutic tool.
Citation:
McEvoy KM, Rayapati D, Washington Cole KO, Erdly C, Payne JL, Osborne LM. Poor postpartum sleep quality predicts subsequent postpartum depressive symptoms in a high-risk sample. J Clin Sleep Med. 2019;15(9):1303–1310.
Keywords: perinatal, postpartum, postpartum depression, risk factor, sleep quality
BRIEF SUMMARY
Current Knowledge/Study Rationale: Previous research has found an association between poor sleep postpartum and concurrent depressive symptoms, but there was insufficient evidence in the literature to determine whether poor sleep in pregnancy or the early postpartum period predicted later postpartum depression. We wished to explore this relationship further, given the detrimental effects of postpartum depression on individuals and families and the ready availability of sleep interventions.
Study Impact: We found that poor sleep quality at 1 month postpartum predicted depressive symptoms at 3 months postpartum. Our findings demonstrate the importance of sleep interventions (which are low cost and readily available) to prevent a devastating illness that affects 15% to 20% of women and their children, and may inform clinical practice in both obstetric and mental health settings.
INTRODUCTION
Postpartum depression (PPD) is a common and debilitating disorder, occurring in approximately 10% to 15% of women in the general population1 and at higher rates in women with preexisting mood disorders.2 PPD poses considerable risks for both mother and infant, including relationship discord, impaired infant-maternal bonding, and, more rarely, suicide and infanticide.3 PPD is also associated with cognitive, emotional, and behavioral problems in the developing child,4,5 at least in part because of changes in parenting practices and interactions of the depressed mother. Risk factors for PPD include personal or family history of PPD, depression or anxiety during the index pregnancy, gestational diabetes, poor partner support, and instrument-assisted or Cesarean delivery.2,6 Given its well-documented relationship with depression in general, reviewed by Lopresti et al,7 sleep disruption has been studied as a risk factor for both PPD and depression during pregnancy.
Existing literature has focused on sleep and depressive symptoms (not always making a distinction between a major depressive episode and depressive symptoms) at various time points across the perinatal period. These studies have used a variety of instruments to measure sleep and mood, in diverse populations of women, both with and without preexisting mood disorders. Most studies have relied on self-report (Edinburgh Postnatal Depression Scale [EPDS], Beck Depression Inventory [BDI]) or clinician-administered (the Hamilton Depression Rating Scale [HAM-D]) scales to measure depressive symptoms, whereas a small number8–11 have measured depression by clinician diagnosis using the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria.
Existing literature falls roughly into two groups—that which examines the relationship between antenatal sleep quality and concurrent or future depressive symptoms, and that which examines postpartum sleep quality as it relates to concurrent or future depressive symptoms. We identified at least 12 studies that found an association between sleep disturbance and concurrent depressive symptoms during pregnancy10,12–22—not surprising, given that sleep disturbance is one of the hallmark symptoms of depression. Four of these 12 studies also investigated whether sleep disturbance in pregnancy predicted subsequent depressive symptoms in pregnancy, three of which had positive findings10,19,20 and one of which did not (though sleep disturbance did predict subsequent anxiety and anger symptoms).14
At least 11 studies have found an association between sleep disturbance in pregnancy and subsequent depression or depressive symptoms in the postpartum period. In some cases,12,23–27 the association may simply have represented a marker of ongoing depression across the perinatal period. The remaining studies, however, were able to demonstrate an independent association between sleep disruption during pregnancy and subsequent postpartum depressive symptoms.11,28–32 One group demonstrated that poor sleep in the third trimester predicted not whether, but rather when, women with a prior history of PPD would have a recurrence of their illness, finding they were more likely to have a recurrence after 4 weeks postpartum rather than during the first 4 weeks.33
At least 14 studies have examined the relationship between postpartum sleep quality and depressive symptoms. Twelve of these found an association between poor sleep postpartum and concurrent depressive symptoms,8,12,15,23,29,34–40 whereas three found that poor postpartum sleep was a predictor of subsequent depressive symptoms.9,23,35 As with the antenatal literature, for two of these studies the relationship may have been a marker of ongoing depressive symptoms.23,35 In the remaining study, Okun and colleagues followed 51 women with a history of prior PPD or Major Depressive Disorder (MDD) longitudinally in the postpartum period. No participant was depressed during the index pregnancy (as defined by two clinical interviews by study psychiatrists). The authors found that for every 1-point increase on the Pittsburgh Sleep Quality Index (PSQI) across the first 17 weeks of the postpartum period, a woman’s risk of PPD recurrence increased by 23.9% when controlling for medication and changes in estradiol levels (PPD recurrence was defined by a score of > 15 on the HAM-D and a clinical diagnosis by two psychiatrists).9
In the current study, we set out to replicate these intriguing findings and also extend them by evaluating individual components of sleep (such as sleep onset latency and daytime dysfunction) and their association with postpartum depressive symptoms. Our primary hypothesis was that poor sleep quality at 1 month postpartum would predict depressive symptoms at 3 months postpartum, controlling for depressive symptoms at 1 month. Secondarily, we sought to examine whether poor sleep in the third trimester would predict depressive symptoms at 1 month and 3 months postpartum, after controlling for depressive symptoms in the third trimester.
METHODS
This was a secondary data analysis of a prospective study conducted at Johns Hopkins University School of Medicine in Baltimore, Maryland, and in collaboration with the University of North Carolina (UNC) at Chapel Hill. Detailed methods were published in the study by Kimmel et al41 Study participants were pregnant women who were at least 18 years old and had a history of a mood disorder (MDD, bipolar I disorder, bipolar II disorder or bipolar disorder-not otherwise specified). Exclusion criteria included active suicidal ideation, medical instability, and substance abuse or dependence in the preceding 90 days. Participants were recruited through the Johns Hopkins Women’s Mood Disorders clinic, the UNC perinatal clinic, and local psychiatrists, obstetricians, flyers, and advertisements. Women could enroll in the study during any trimester of pregnancy and were managed clinically by their treating psychiatrist. Informed consent was obtained from all participants. Mood disorder diagnoses were confirmed during each participant’s first study visit, using the Structured Clinical Interview for DSM-IV (SCID-4). The parent study included study visits at up to six time points in pregnancy and the postpartum period. Participants were eligible for inclusion in the current analysis if they completed the Inventory of Depressive Symptomatology-Self Report (IDS-SR) at 3 months postpartum and the Pittsburgh Sleep Quality Index (PSQI) in the third trimester (n = 51) or at 1 month postpartum (n = 45). The Institutional Review Boards at Johns Hopkins University and UNC Chapel Hill approved the study procedures.
Measures
Sleep, our independent variable, was measured by the PSQI. The PSQI is a 19-item questionnaire assessing sleep quality during the previous month. Poorer sleep quality is indicated by higher PSQI global and subscale scores, with a global score of > 5 indicating poor sleep in the general population (sensitivity 89.6%, specificity 86.5%).42 The PSQI shows good construct validity and reliability (Cronbach alpha 0.74), and correlates with depression and anxiety symptoms in a sample of US pregnant women.43 In the current analysis, we studied PSQI global scores (scored on a 0–21 scale), as well as the seven PSQI subscales (scored on a 0–3 scale): (1) self-reported sleep quality, (2) sleep latency, (3) duration of sleep, (4) sleep efficiency (total sleep time/time in bed × 100), (5) nocturnal sleep disturbance, (6) sleep medication usage, and (7) daytime dysfunction.
Depressive symptoms, our dependent variable, were measured by the IDS-SR. The IDS-SR is a 30-item questionnaire assessing the severity of depressive symptoms in the previous 7 days. IDS-SR scores range from 0 to 84, with higher scores indicating more severe depressive symptoms. It has been demonstrated to have good internal consistency (Cronbach alpha 0.76 to 0.82 for those with current depression), interrater reliability, and adequate face and discriminant validity in patients with MDD.44 It has also been shown to have good internal consistency (Cronbach alpha 0.89) and accuracy in diagnosing antenatal depression.45
Statistical Analyses
We used descriptive statistics to characterize the sample with respect to selected variables collected from study visit questionnaires. We used chi-square analyses and independent t tests to assess for differences in selected characteristics between the participants contributing sleep quality data in the third trimester and at 1 month postpartum. We used bivariate and multivariate linear regression models to study the association between PSQI global and subscale scores in the third trimester and at 1 month postpartum (independent variables), and IDS-SR scores at 3 months postpartum (dependent variable). We included PSQI and IDS-SR scores as continuous measures in regression models. We ran separate regression models for PSQI global scores and each of the PSQI subscales. In the multivariate models, we adjusted for several variables selected a priori for inclusion in the regression models because of their association with depressive symptoms: age, education (graduate school versuse less education), and history of childhood trauma as measured by the Childhood Trauma Questionnaire (due to the association of early life adversity with later depressive symptoms).46,47 We also controlled for use of antidepressants, because of their potential effect on depressive symptoms as well as sleep symptoms, and for depressive symptoms at the earlier time point. We completed two sensitivity analyses, first excluding antidepressant utilization from the models and then including diagnosis (major depressive disorder versus bipolar disorder) in the models. All analyses were completed using Stata 13 (College Station, Texas).
RESULTS
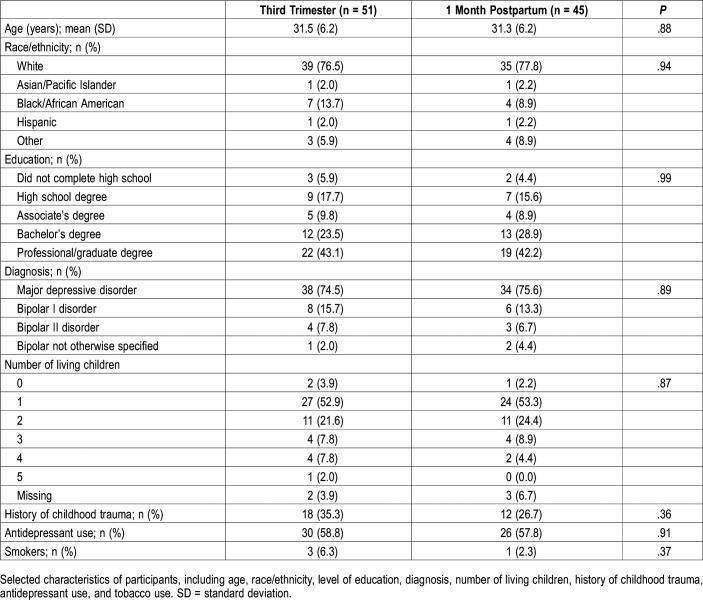
The final sample included 51 women who completed the PSQI in the third trimester and 45 women who completed the PSQI at 1 month postpartum. Overall, 42 women contributed sleep quality data at both time points. Descriptive statistics are included in Table 1. In both samples, the mean age was 31 years, and most of the participants were White, high income, had completed education beyond high school, had a diagnosis of MDD, had not experienced child abuse (included as it is associated with depression later in life), were nonsmokers, and were prescribed antidepressants during the time point when they reported sleep quality data. All the women had singleton pregnancies, and most of both samples had either one or two living children. There were no significant differences between the samples of women contributing sleep quality data in the third trimester compared to those who contributed sleep quality data at 1 month postpartum with respect to any of these characteristics.
Table 1.
Characteristics of participants.
Postpartum Sleep: Sleep Quality at 1 Month Postpartum and Depressive Symptoms at 3 Months Postpartum
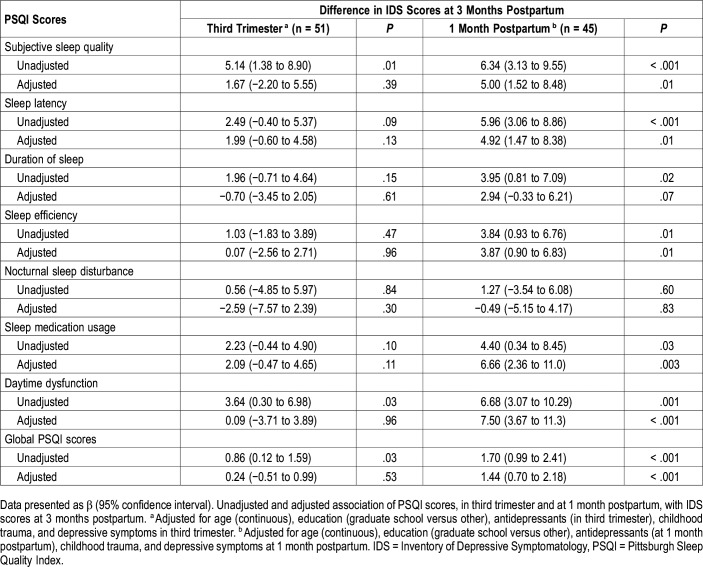
The unadjusted and adjusted associations between PSQI scores at 1 month postpartum with IDS-SR scores at 3 months postpartum are shown in Table 2. In multivariate models (controlling for age, education, history of child abuse, use of antidepressants, and depressive symptoms at 1 month postpartum), each one-unit increase in global PSQI score at 1 month postpartum was associated with an increase of 1.44 points in IDS-SR score at 3 months postpartum (95% confidence interval [CI] 0.70–2.18, P < .001). Similarly, each one-unit increase in PSQI component scores at 1 month postpartum was associated with higher IDS-SR scores at 3 months postpartum for the following domains: subjective sleep quality (β = 5.00, 95% CI 1.52–8.48, P = .01), sleep latency (β = 4.92, 1.47–8.38, P = .01), sleep efficiency (β = 3.87, 95% CI 0.90–6.83, P = .01), sleep medication usage (β = 6.66, 95% CI 2.36–11.0, P = .003), and daytime dysfunction (β = 7.50, 95% CI 3.67–11.3, P < .001). A sensitivity analysis removing antidepressant use from the model, and another controlling for type of mood disorder diagnosis, did not change these results (data not shown).
Table 2.
Association of PSQI scores (in third trimester and at 1 month postpartum) with IDS scores at 3 months postpartum.
Antenatal Sleep: Sleep Quality in the Third Trimester and Depressive Symptoms at 3 Months Postpartum
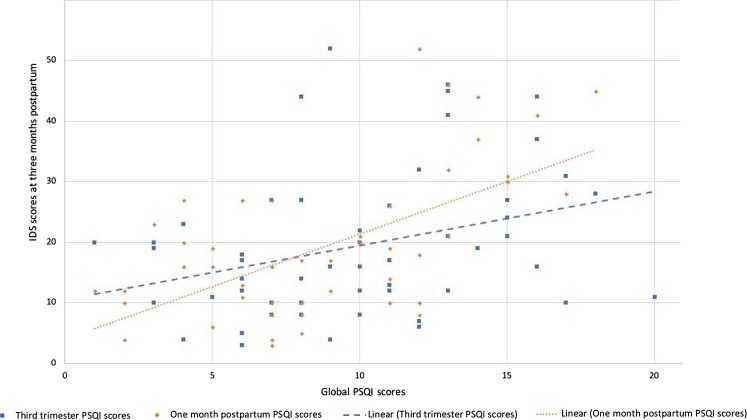
The unadjusted and adjusted associations between PSQI scores in the third trimester with IDS-SR scores at 3 months postpartum are shown in Table 2. In multivariate analysis (controlling for age, education, history of child abuse, use of antidepressants, and depressive symptoms in the third trimester), there were no associations between PSQI scores in the third trimester (global or subscale) and IDS-SR scores at 1 month postpartum. Figure 1 illustrates the relationship between PSQI scores in the third trimester and at 1 month postpartum and IDS-SR scores at 3 months postpartum.
Figure 1. Association between IDS scores and global PSQI scores.
The relationship between IDS scores at 3 months postpartum and global PSQI scores in the third trimester and at 1 month postpartum. IDS = Inventory of Depressive Symptomatology, PSQI = Pittsburgh Sleep Quality Index.
DISCUSSION
Our main finding, that poor sleep quality in the early postpartum period predicts the later development of postpartum depressive symptoms, supports and extends the findings of Okun and colleagues,9 who demonstrated that poor sleep quality across the postpartum conferred an increased risk of PPD recurrence for high-risk women. In the sample by Okun and colleagues, participants were euthymic during the index pregnancy, and the change in postpartum sleep quality was measured sequentially across the first 17 weeks postpartum as it related to PPD recurrence. In our study, we looked specifically at the early postpartum time point as a predictor of later symptoms and we controlled for depression at the earlier time point to be sure we were measuring a predictor and not simply a marker of ongoing depression.
In addition, our study advances existing knowledge by going beyond global scores to analyze sleep component scores. We found that problems with self-reported sleep quality, sleep latency, sleep efficiency, sleep medication usage, and daytime dysfunction (measured at 1 month postpartum) all predicted depressive symptoms at 3 months postpartum. Other studies have identified postpartum sleep latency and sleep efficiency as correlates of depressive symptoms,8,29,37,48 but not as predictors. Studies that have used actigraphy to measure objective sleep suggest that sleep efficiency and consolidation of sleep are more important than total duration of sleep with respect to improving mood.29,37 This finding is also supported by one of the few intervention-based studies of sleep and PPD, in which Swanson and colleagues used cognitive behavioral therapy (CBT) for insomnia in an open pilot manner to treat sleep problems in 12 women with PPD, which resulted in improvement in mood.49 If interrupted or disjointed sleep in particular, and not just decreased amount of sleep, negatively affects mood, it is not surprising that the postpartum period is a time of elevated risk of depression for certain women.
Knowing which components of sleep predict postpartum depressive symptoms allows for more specific therapeutic interventions and more accurate monitoring of symptom resolution. CBT for insomnia is an effective modality for reducing sleep onset latency and improving maintenance of sleep.50 If unavailable or ineffective, short term use of sleep medication may be indicated, although medications will likely only help with sleep onset. Maximizing uninterrupted sleep could be helpful in reducing sleep latency and increasing sleep efficiency. This would require increased partner and family involvement or use of a night nurse when feasible.
After adjustment for confounders, we did not find an association between sleep quality in the third trimester and subsequent postpartum depressive symptoms. This is at odds with existing literature and may be because our small sample size gave us limited power to detect this association.
Strengths of our study include the use of a well-characterized sample of women with diagnoses of mood disorders confirmed by study psychiatrists, as well as the prospective longitudinal design. Both of these elements are rare in similar studies. There were several limitations as well. This was a secondary analysis with a small sample size, so was not powered to answer the question we addressed; this may have affected the internal validity of our results. The participants had heterogeneous diagnoses, with most having MDD but approximately 25% having a diagnosis of bipolar spectrum disorder. We were unable to repeat our analyses separately according to mood disorder diagnosis due to our small sample size; we did not want to miss a possible effect due to insufficient numbers. Although diagnostically separate studies will be important in the future, this particular study sought to understand the relationship between poor sleep and depressed mood, regardless of diagnostic category, and should be clinically useful for those treating patients with either diagnosis. The mood scale we used (IDS-SR) is not validated for use in the postpartum population, though it has been demonstrated to be reliable and accurate in diagnosing antenatal depression when compared to a clinician-based diagnosis.45 The IDS-SR and the PSQI have inherent limitations as self-report measures. Sleep diaries, which may help to substantiate the relationships found by self-report measures, might have been a useful addition, and their absence in our study must count as a limitation.48 It is not clear whether including objective sleep measures would have been beneficial; however; studies that have used objective measures of sleep, such as actigraphy, in addition to self-report measures, have had mixed results.11,12,21–23,29,37 There is a stronger association between symptoms of depression and self-report measures of sleep, such as the PSQI, than with objective measures, such as actigraphy.51 It is not known exactly why this is the case—it has been suggested that the PSQI relates more to the psychological components of sleep disturbance and that a “hyperarousal” state can contribute both to problematic sleep and to distress symptoms, such as depression.52 It is also possible that complications with labor and delivery, for which we did not adjust due to small numbers as well as missing data, may have influenced the results—instrumental or Cesarean section deliveries are risk factors for PPD and physical injury and pain as a consequence of labor and delivery may result in inadequate sleep. Additionally, data on infant characteristics and behavior, which clearly can have an effect on postpartum sleep and potentially depressive symptoms, were also not collected in the original study. Sleep is known to vary by ethnicity and level of education, being better in more highly educated and Caucasian individuals,46 both of which were overrepresented in our sample. This may have skewed our results, leading to better sleep outcomes than what may be seen in the general population (though the inclusion of participants with worse sleep outcomes might actually have served to enhance the relationship we found). Finally, some studies have suggested that the “sleep medication use” and “daytime dysfunction” subscales are not reliable indicators of sleep quality and caution against their use in making clinical interpretations.47 This limitation would apply particularly in the postpartum period, when women are more likely to report daytime dysfunction.
Despite these limitations, our work clearly emphasizes the importance of quality sleep in the immediate postpartum time period for women with mood disorders. Future directions might include replicating this work with a larger sample size, controlling for further variables associated with pregnancy and delivery, separating the sample by mood disorder diagnosis, and including women without a prior history to see whether these results are generalizable outside the population of women with a mood disorder. The most urgently needed research to arise out of this must, however, be interventional. If maternal sleep disruption (not total amount) in women with a history of a mood disorder is a strong a risk factor for the subsequent development of depressive symptoms, we need to develop and test therapeutic interventions, such as CBT for insomnia, targeted at this population and these specific symptoms. Although it may take some time to develop and test such interventions, there are urgent clinical actions we can take now. During postpartum visits, whether in obstetrics, primary care, or psychiatry, providers should obtain a detailed account of sleep and all the factors involved in order to formulate a sleep management plan with the patient and family. If physicians do not take sleep disruption seriously, neither will patients or their families.
In conclusion, poor sleep quality in the early postpartum period independently predicts development of later PPD symptoms. This is clinically significant and highlights the importance of sleep interventions as an immediate postpartum therapeutic tool.
DISCLOSURE STATEMENT
Work for this study was performed at Johns Hopkins University School of Medicine, Women’s Mood Disorders Center, Department of Psychiatry and Behavioral Sciences. In the past year, Dr. Jennifer Payne has performed legal consulting work for Abbott Pharmaceuticals and Johnson and Johnson. She also has a patent on epigenetic biomarkers for postpartum depression. The remaining authors report no conflicts of interest. Dr. Osborne’s work was supported by NIH 1K23 MH110607-01A1 and the Doris Duke Early Clinician Investigator Award. Dr. Payne’s work was supported by NIMH K23 MH074799. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
ACKNOWLEDGMENTS
The authors thank Samantha Meilman and Meeta Pangtey, research staff who assisted with the collection of data and preparation of this manuscript
ABBREVIATIONS
- BDI
Beck Depression Inventory
- CBT
cognitive behavioral therapy
- DSM
Diagnostic and Statistical Manual for Mental Disorders
- EPDS
Edinburgh Postnatal Depression Scale
- HAM-D
Hamilton Depression Rating Scale
- ISD-SR
Inventory of Depressive Symptomatology-Self Report
- MDD
major depressive disorder
- PPD
postpartum depression
- PSQI
Pittsburgh Sleep Quality Index
- SCID-4
Structured Clinical Interview for DSM-IV
- UNC
University of North Carolina
REFERENCES
- 1.Becker M, Weinberger T, Chandy A, Schmukler S. Depression during pregnancy and postpartum. Curr Psychiatry Rep. 2016;18(3):32. doi: 10.1007/s11920-016-0664-7. [DOI] [PubMed] [Google Scholar]
- 2.Silverman ME, Reichenberg A, Savitz DA, et al. The risk factors for postpartum depression: a population-based study. Depress Anxiety. 2017;34(2):178–187. doi: 10.1002/da.22597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart DE, Vigod S. Postpartum depression. N Engl J Med. 2016;375(22):2177–2186. doi: 10.1056/NEJMcp1607649. [DOI] [PubMed] [Google Scholar]
- 4.Grace SL, Evindar A, Stewart DE. The effect of postpartum depression on child cognitive development and behavior: a review and critical analysis of the literature. Arch Women Ment Health. 2003;6(4):263–274. doi: 10.1007/s00737-003-0024-6. [DOI] [PubMed] [Google Scholar]
- 5.Abbott R, Dunn VJ, Robling SA, Paykel ES. Long-term outcome of offspring after maternal severe puerperal disorder. Acta Psychiatr Scand. 2004;110(5):365–373. doi: 10.1111/j.1600-0447.2004.00406.x. [DOI] [PubMed] [Google Scholar]
- 6.Milgrom J, Gemmill AW, Bilszta JL, et al. Antenatal risk factors for postnatal depression: a large prospective study. J Affect Disord. 2008;108(1-2):147–157. doi: 10.1016/j.jad.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 7.Lopresti AL, Hood SD, Drummond PD. A review of lifestyle factors that contribute to important pathways associated with major depression: diet, sleep and exercise. J Affect Disord. 2013;148(1):12–27. doi: 10.1016/j.jad.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 8.Posmontier B. Sleep quality in women with and without postpartum depression. J Obstet Gynecol Neonatal Nurs. 2008;37(6):722–735. doi: 10.1111/j.1552-6909.2008.00298.x. quiz 735-737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okun ML, Luther J, Prather AA, Perel JM, Wisniewski S, Wisner KL. Changes in sleep quality, but not hormones predict time to postpartum depression recurrence. J Affect Disord. 2011;130(3):378–384. doi: 10.1016/j.jad.2010.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Okun ML, Kiewra K, Luther JF, Wisniewski SR, Wisner KL. Sleep disturbances in depressed and nondepressed pregnant women. Depress Anxiety. 2011;28(8):676–685. doi: 10.1002/da.20828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krawczak EM, Minuzzi L, Simpson W, Hidalgo MP, Frey BN. Sleep, daily activity rhythms and postpartum mood: a longitudinal study across the perinatal period. Chronobiol Int. 2016;33(7):791–801. doi: 10.3109/07420528.2016.1167077. [DOI] [PubMed] [Google Scholar]
- 12.Bei B, Milgrom J, Ericksen J, Trinder J. Subjective perception of sleep, but not its objective quality, is associated with immediate postpartum mood disturbances in healthy women. Sleep. 2010;33(4):531–538. doi: 10.1093/sleep/33.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dørheim SK, Bjorvatn B, Eberhard-Gran M. Insomnia and depressive symptoms in late pregnancy: a population-based study. Behav Sleep Med. 2012;10(3):152–166. doi: 10.1080/15402002.2012.660588. [DOI] [PubMed] [Google Scholar]
- 14.Field T, Diego M, Hernandez-Reif M, Schanberg S, Kuhn C. Sleep disturbances in depressed pregnant women and their newborns. Infant Behav Dev. 2007;30(1):127–133. doi: 10.1016/j.infbeh.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Goyal D, Gay CL, Lee KA. Patterns of sleep disruption and depressive symptoms in new mothers. J Perinat Neonatal Nurs. 2007;21(2):123–129. doi: 10.1097/01.JPN.0000270629.58746.96. [DOI] [PubMed] [Google Scholar]
- 16.Mellor R, Chua SC, Boyce P. Antenatal depression: an artefact of sleep disturbance? Arch Women Ment Health. 2014;17(4):291–302. doi: 10.1007/s00737-014-0427-6. [DOI] [PubMed] [Google Scholar]
- 17.Okun ML, Kline CE, Roberts JM, Wettlaufer B, Glover K, Hall M. Prevalence of sleep deficiency in early gestation and its associations with stress and depressive symptoms. J Womens Health (Larchmt) 2013;22(12):1028–1037. doi: 10.1089/jwh.2013.4331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Polo-Kantola P, Aukia L, Karlsson H, Karlsson L, Paavonen EJ. Sleep quality during pregnancy: associations with depressive and anxiety symptoms. Acta Obstet Gynecol Scand. 2017;96(2):198–206. doi: 10.1111/aogs.13056. [DOI] [PubMed] [Google Scholar]
- 19.Skouteris H, Germano C, Wertheim EH, Paxton SJ, Milgrom J. Sleep quality and depression during pregnancy: a prospective study. J Sleep Res. 2008;17(2):217–220. doi: 10.1111/j.1365-2869.2008.00655.x. [DOI] [PubMed] [Google Scholar]
- 20.Skouteris H, Wertheim EH, Germano C, Paxton SJ, Milgrom J. Assessing sleep during pregnancy: A study across two time points examining the Pittsburgh Sleep Quality Index and associations with depressive symptoms. Womens Health Issues. 2009;19(1):45–51. doi: 10.1016/j.whi.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 21.Tsai SY, Lin JW, Wu WW, et al. Sleep disturbances and symptoms of depression and daytime sleepiness in pregnant women. Birth. 2016;43(2):176–183. doi: 10.1111/birt.12215. [DOI] [PubMed] [Google Scholar]
- 22.Volkovich E, Tikotzky L, Manber R. Objective and subjective sleep during pregnancy: Links with depressive and anxiety symptoms. Arch Women Ment Health. 2016;19(1):173–181. doi: 10.1007/s00737-015-0554-8. [DOI] [PubMed] [Google Scholar]
- 23.Coo S, Milgrom J, Trinder J. Mood and objective and subjective measures of sleep during late pregnancy and the postpartum period. Behav Sleep Med. 2014;12(4):317–330. doi: 10.1080/15402002.2013.801348. [DOI] [PubMed] [Google Scholar]
- 24.MacLean JV, Faisal-Cury A, Chan YF, et al. The relationship between sleep disturbance in pregnancy and persistent common mental disorder in the perinatal period (sleep disturbance and persistent CMD) J Ment Health. 2015;24(6):375–378. doi: 10.3109/09638237.2015.1036969. [DOI] [PubMed] [Google Scholar]
- 25.Marques M, Bos S, Soares MJ, et al. Is insomnia in late pregnancy a risk factor for postpartum depression/depressive symptomatology? Psychiatry Res. 2011;186(2-3):272–280. doi: 10.1016/j.psychres.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 26.Sarberg M, Bladh M, Svanborg E, Josefsson A. Postpartum depressive symptoms and its association to daytime sleepiness and restless legs during pregnancy. BMC Pregnancy Childbirth. 2016;16(1):137. doi: 10.1186/s12884-016-0917-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tzeng YL, Chen SL, Chen CF, Wang FC, Kuo SY. Sleep trajectories of women undergoing elective cesarean section: Effects on body weight and psychological well-being. PLoS One. 2015;10(6):e0129094. doi: 10.1371/journal.pone.0129094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dørheim SK, Bjorvatn B, Eberhard-Gran M. Can insomnia in pregnancy predict postpartum depression? A longitudinal, population-based study. PLoS One. 2014;9(4):e94674. doi: 10.1371/journal.pone.0094674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park EM, Meltzer-Brody S, Stickgold R. Poor sleep maintenance and subjective sleep quality are associated with postpartum maternal depression symptom severity. Arch Women Ment Health. 2013;16(6):539–547. doi: 10.1007/s00737-013-0356-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tham EK, Tan J, Chong YS, et al. Associations between poor subjective prenatal sleep quality and postnatal depression and anxiety symptoms. J Affect Disord. 2016;202:91–94. doi: 10.1016/j.jad.2016.05.028. [DOI] [PubMed] [Google Scholar]
- 31.Tomfohr LM, Buliga E, Letourneau NL, Campbell TS, Giesbrecht GF. Trajectories of sleep quality and associations with mood during the perinatal period. Sleep. 2015;38(8):1237–1245. doi: 10.5665/sleep.4900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu M, Li X, Feng B, Wu H, Qiu C, Zhang W. Poor sleep quality of third-trimester pregnancy is a risk factor for postpartum depression. Med Sci Monit. 2014;20:2740–2745. doi: 10.12659/MSM.891222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Okun ML, Hanusa BH, Hall M, Wisner KL. Sleep complaints in late pregnancy and the recurrence of postpartum depression. Behav Sleep Med. 2009;7(2):106–117. doi: 10.1080/15402000902762394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clout D, Brown R. Sociodemographic, pregnancy, obstetric, and postnatal predictors of postpartum stress, anxiety and depression in new mothers. J Affect Disord. 2015;188:60–67. doi: 10.1016/j.jad.2015.08.054. [DOI] [PubMed] [Google Scholar]
- 35.Dennis CL, Ross L. Relationships among infant sleep patterns, maternal fatigue, and development of depressive symptomatology. Birth. 2005;32(3):187–193. doi: 10.1111/j.0730-7659.2005.00368.x. [DOI] [PubMed] [Google Scholar]
- 36.Dørheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Sleep and depression in postpartum women: a population-based study. Sleep. 2009;32(7):847–855. doi: 10.1093/sleep/32.7.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goyal D, Gay C, Lee K. Fragmented maternal sleep is more strongly correlated with depressive symptoms than infant temperament at three months postpartum. Arch Women Ment Health. 2009;12(4):229–237. doi: 10.1007/s00737-009-0070-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang CM, Carter PA, Guo JL. A comparison of sleep and daytime sleepiness in depressed and non-depressed mothers during the early postpartum period. J Nurs Res. 2004;12(4):287–296. doi: 10.1097/01.jnr.0000387513.75114.bb. [DOI] [PubMed] [Google Scholar]
- 39.Tsai SY, Thomas KA. Sleep disturbances and depressive symptoms in healthy postpartum women: a pilot study. Res Nurs Health. 2012;35(3):314–323. doi: 10.1002/nur.21469. [DOI] [PubMed] [Google Scholar]
- 40.Swanson LM, Pickett SM, Flynn H, Armitage R. Relationships among depression, anxiety, and insomnia symptoms in perinatal women seeking mental health treatment. J Womens Health (Larchmt) 2011;20(4):553–558. doi: 10.1089/jwh.2010.2371. [DOI] [PubMed] [Google Scholar]
- 41.Kimmel M, Hess E, Roy PS, et al. Family history, not lack of medication use, is associated with the development of postpartum depression in a high-risk sample. Arch Women Ment Health. 2015;18(1):113–121. doi: 10.1007/s00737-014-0432-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 43.Qiu C, Gelaye B, Zhong QY, Enquobahrie DA, Frederick IO, Williams MA. Construct validity and factor structure of the Pittsburgh Sleep Quality Index among pregnant women in a pacific-northwest cohort. Sleep Breath. 2016;20(1):293–301. doi: 10.1007/s11325-016-1313-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The inventory of depressive symptomatology (IDS): psychometric properties. Psychol Med. 1996;26(3):477–486. doi: 10.1017/s0033291700035558. [DOI] [PubMed] [Google Scholar]
- 45.Brunoni AR, Benute GR, Fraguas R, et al. The self-rated inventory of depressive symptomatology for screening prenatal depression. Int J Gynaecol Obstet. 2013;121(3):243–246. doi: 10.1016/j.ijgo.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 46.Grandner MA, Williams NJ, Knutson KL, Roberts D, Jean-Louis G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18. doi: 10.1016/j.sleep.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A. The Pittsburgh Sleep Quality Index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev. 2016;25:52–73. doi: 10.1016/j.smrv.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 48.Dørheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Subjective and objective sleep among depressed and non-depressed postnatal women. Acta Psychiatr Scand. 2009;119(2):128–136. doi: 10.1111/j.1600-0447.2008.01272.x. [DOI] [PubMed] [Google Scholar]
- 49.Swanson LM, Flynn H, Adams-Mundy JD, Armitage R, Arnedt JT. An open pilot of cognitive-behavioral therapy for insomnia in women with postpartum depression. Behav Sleep Med. 2013;11(4):297–307. doi: 10.1080/15402002.2012.683902. [DOI] [PubMed] [Google Scholar]
- 50.Taylor DJ, Pruiksma KE. Cognitive and behavioural therapy for insomnia (CBT-I) in psychiatric populations: a systematic review. Int Rev Psychiatry. 2014;26(2):205–213. doi: 10.3109/09540261.2014.902808. [DOI] [PubMed] [Google Scholar]
- 51.Buysse DJ, Hall ML, Strollo PJ, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), epworth sleepiness scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4(6):563–571. [PMC free article] [PubMed] [Google Scholar]
- 52.Klumpp H, Roberts J, Kapella MC, Kennedy AE, Kumar A, Phan KL. Subjective and objective sleep quality modulate emotion regulatory brain function in anxiety and depression. Depress Anxiety. 2017;34(7):651–660. doi: 10.1002/da.22622. [DOI] [PMC free article] [PubMed] [Google Scholar]