Abstract
Background:
Maltreated youth are at an elevated risk for the development of problem behaviors. Coping with the death of a family member or close friend during adolescence, referred to as bereavement, is a stressful event that could potentiate risk linked to maltreatment. However, developmental research suggests that youth adjustment is a product of multiple risk and protective factors. Although maltreated youth who experience loss may be particularly vulnerable to behavior problems, personal and contextual factors may attenuate or exacerbate youths’ risk for internalizing and externalizing psychopathology.
Objective:
The overarching goal of this study is to examine individual, family, and community-level protective factors for maltreated youth who experience bereavement. Specifically, we aim to examine the effect of age 12 bereavement on age 16 internalizing and externalizing psychopathology, and to investigate the moderating role of multi-level protective factors at ages 14 and 16.
Methods:
The study consisted of a sample of 800 youth (52.4% female, 45.1% African-American) drawn from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN), collected from 1998 to 2011.
Results:
Maltreated youth who experienced significant loss were at increased risk for externalizing symptoms, compared to non-bereaved maltreated youth (β = .085, p < .05). Individual future orientation (β = .103, p < .05) family future orientation (β = −.120, p < .05), parental monitoring (β = −.123, p < .01), and neighborhood collective efficacy (β = −.126, p < .01) each significantly moderated the association between bereavement and externalizing symptoms.
Conclusions:
These results have implications for future interventions aimed towards reducing problem behaviors in adolescents with a history of child maltreatment and who experience bereavement.
Keywords: Bereavement, child maltreatment, early adversity, externalizing behaviors, adolescence, resilience
Introduction
The death of a loved one is often an extremely stressful and traumatic event for adolescents, necessitating a supportive family environment for effective grieving and coping (Brent, Melhem, Masten, Porta, & Payne, 2012; Sandler et al., 2003). Adolescents reared in abusive families while experiencing bereavement may not have the resources necessary to cope with the loss, and therefore are particularly vulnerable to its deleterious effects. Specifically, abused or neglected youth who also experience bereavement may be particularly at risk for developing psychopathology in adolescence. Despite the documented risk linked to trauma and loss, there is substantial variability in youth developmental outcomes depending upon additional risk and protective factors that can exacerbate or mitigate this link (Cicchetti, 2013). In the present study, we aimed to test whether maltreated youth who also experience the death of a family member or close friend, referred to as bereavement, are at risk for developing internalizing (i.e., depressive, withdrawn, and anxious symptoms) and externalizing (i.e., aggressive and delinquent behaviors) in adolescence, compared to non-bereaved maltreated youth. In addition, we utilized a systems approach by examining the moderating effect of multi-level protective factors (i.e., individual, family and community levels) in the longitudinal link between bereavement and adjustment problems in youth with a history of child maltreatment.
Maltreatment and Youth Psychopathology: A Developmental Psychopathology Perspective
According to the developmental psychopathology perspective and the organizational theory of development, the experience of negative life events during childhood can lead to the disruption of stage-salient tasks, such as the development of self-regulation, resulting in maladaptive outcomes such as behavior problems (Davies, Manning, & Cicchetti, 2013). Exposure to early life stressors, such as maltreatment and bereavement, can deprive youth of internal resources that are necessary to complete stage-salient tasks such as the development of identity formation and emotional processing (Schultz, 2007; McLaughlin & Hatzenbuehler, 2009). In turn, the failure to reach these developmental tasks may compromise the ability to resolve subsequent phases of socioemotional development carrying into adolescence. Indeed, child maltreatment is associated with a range of internalizing and externalizing symptomology in adolescence (Begle et al., 2011; Hamilton, Falshaw, & Browne, 2002; Hussey, Chang, & Kotch, 2006; Kim & Cicchetti, 2006; Oshri, Rogosch, & Cicchetti, 2013). Specifically, a meta-analysis of eight cohort studies reported that 59% of depression and anxiety cases worldwide could potentially be attributed to child maltreatment (Li, D’Arcy, & Meng, 2016). Despite this pronounced risk, maltreated youth are not predetermined to exhibit patterns of maladaptation, as additional stressors and protective factors may play a critical role in subsequent developmental trajectories (Cicchetti & Banny, 2014).
Bereavement in Maltreated Youth
An additional stressor that may increase the risk of psychopathology among maltreated youth is the experience of bereavement. Studies show that the experience of bereavement is not uncommon in adolescence, with a majority (78%) of youth age 11 to 16 reporting to have experienced the death of a relative or close friend (Harrison & Harrington, 2001). When using the term bereavement, we are referring to the state of having lost someone to death or “the fact of loss,” as is suggested in previous reviews (see Zisook & Shear, 2009). This term is often used interchangeably with grief, which, unlike bereavement, describes the “emotional, cognitive, functional, and behavioral responses to the death” (Zisook & Shear, 2009). In this regard, bereavement itself is a major life stressor that can severely impact adjustment during adolescence (Balk & Corr, 2001; Stroebe, Hansson, Stroebe, & Schut, 2001). Whereas many individuals who experience loss are able to successfully adapt over time to a life without the deceased (Bonanno, 2004), approximately 10% to 15% of bereaved individuals will continue to show serious disruptions in functioning several years after the loss (Bonanno & Kaltman, 2001). Bereaved adolescents may be at even greater risk for maladjustment, as previous studies have reported that 50% or more youth exhibit problem behavior following loss (Lin, Sandler, Ayers, Wolchik, & Luecken, 2004; Lundberg et al., 2018; McCown & Davies, 1995).
However, not all youth who experience bereavement will exhibit problem behaviors. The variation in youth adjustment outcomes following the death of a loved one can often be attributed to the context in which adversity took place (Masten, 2018). Accordingly, adolescents who experience bereavement in a negative rearing environment may be at an increased risk for maladjustment, compared to youth with no previous exposure to family trauma. A plethora of research suggests that adolescents who experience significant loss are at risk for mental health problems, including both internalizing and externalizing behaviors (Brent, Melhem, Donohoe, & Walker, 2009; Draper & Hancock, 2011; Herberman Mash, Fullerton, & Ursano, 2013). Given the known adverse impact of child maltreatment on youth adjustment (English et al., 2005; Kim & Cicchetti, 2010), it is expected that maltreated youth who also endure bereavement will be vulnerable to internalizing and externalizing psychopathology.
However, research on youth resilience shows that the presence of personal and contextual factors may attenuate youths’ risk for problem behaviors (Afifi & MacMillan, 2011; Sandler, Wolchik, & Ayers, 2008). The heterogeneous consequences to childhood adversity have been conceptualized by multifinality, a fundamental principle to the developmental psychopathology framework. Multifinality refers to the process by which similar risk factors (i.e., the death of a loved one) can result in a wide range of outcomes (Cicchetti & Rogosch, 1996). Although it is impossible to unequivocally predict which youth will demonstrate patterns of maladaptive functioning following significant family stress, the investigation of protective mechanisms provides a unique opportunity to contribute to knowledge for the prevention of problem behaviors amongst at-risk youth.
Multilevel Protective Contexts: Intrapersonal, Family, and Community
According to the ecological framework for the development of psychopathology (Cicchetti & Valentino, 2006), the processes underlying the association between childhood adversity and psychopathology are often influenced by multiple factors in the child’s environment (Cicchetti & Valentino, 2006). Multilevel contexts refer to both proximal microsystem variables existing within the child’s immediate environment (e.g., family and peer environments) and distal exo- and macro-system variables that are further from the child (e.g., neighborhoods environments; Masten, 2018). This conceptualization of “development in context” acknowledges that discrete experiences are subject to various alterations engendered by the interface between multiple levels of the youths’ ecology. Accordingly, the way in which an adolescent interprets and responds to adverse events such as close loss will likely depend upon interacting resources that can support or assist youth to effectively cope with the loss, including intrapersonal characteristics, parents, neighborhoods, and peers (Oshri, Topple, & Carlson, 2017).
Intrapersonal.
Personal traits and characteristics can serve as protective assets for youth experiencing child maltreatment (Afifi & MacMillan, 2011) and other adversities, such as bereavement (Haine, Ayers, Sandler, Wolchik, & Weyer, 2003). An individual asset that is widely associated with positive adaptation in the context of adversity is the ability to maintain a positive outlook towards the future (Gillespie, Chaboyer, & Wallis, 2007; Masten, 2014), which is often referred to as future orientation. Future orientation is a multidimensional construct that represents an individual’s ability and tendency to set future goals and plans (Johnson, Blum, & Cheng, 2014). Extant research suggests that adolescents who have positive expectations for their future are more likely to develop competency and less likely to participate in problem behaviors, compared to youth with lower expectations (Chen & Vazsonyi, 2013; Robbins & Bryan, 2004). Empirical research shows that youth who experience early life adversity may have diminished aspirations for the future (Brent, Melhem, Masten, Porta, & Payne, 2012; Lansford et al., 2002; respectively). However, youth who see past immediate adversity such as bereavement or abuse, and visualize positive outcomes, can avoid the consequences of early life trauma (Oshri, Duprey, Kogan, Carlson, & Liu, 2018).
Family.
The examination of family-related variables is pertinent to the prevention of adolescent internalizing and externalizing problems, especially in the case of cumulative family stress, such as child maltreatment and bereavement. Literature suggests that the parent-child relationship plays a key role in protecting against mental health problems in youth (Cabrera, Cook, McFadden, & Bradley, 2011; Day & Padilla-Walker, 2009; Qu, Fuligni, Galvan, & Telzer, 2015). Further, developmental research has established the parent-child bond to be a prominent influence on child development during critical periods of transition (e.g., into adolescence; Ebbert, Infurna, & Luthar, 2018). The investigation of parenting quality as a protective factor for maltreated youth can be problematic, considering that children exposed to maltreatment are, by definition, receiving less than high-quality parenting (Bolger & Patterson, 2003). Nevertheless, previous studies have documented a significant association between parent-child relationships and behavioral outcomes in both bereaved (Haine, Wolchik, Sandler, Millsap, & Ayers, 2006; Kwok et al., 2005) and maltreated youth (Toth & Cicchetti, 1996; Wilkinson & Lantos, 2018). For example, maltreated youth who reported higher-quality relationships with their parents were significantly less likely to participate in both violent and nonviolent offending behavior, compared to maltreated youth with low-to-no quality relationships (Wilkinson & Lantos, 2018). These findings collectively suggest that the parent-child bond may be protective for maltreated adolescents enduring loss.
Parental monitoring is an additional familial factor that is defined as the active tracking and surveillance of children’s behavior, including their whereabouts, activities, and adaptations (Dishion & McMahon, 1998; Stattin & Kerr, 2000). There is evidence to suggest that youth who report higher levels of monitoring are less likely to participate in risky or delinquent behaviors (Lahey, Van Hulle, D’Onofrio, Rodgers, & Waldman, 2008; Robertson, Baird-Thomas, & Stein, 2008). Because low levels of surveillance can facilitate illegal or rule-breaking activity, parental monitoring is hypothesized to play a significant role in the prevention of externalizing problems during adolescence, when youth are specifically prone to exhibit delinquent behaviors (Agnew, 2003). Parental monitoring has also been associated with lower levels of depressive symptoms among adolescents (Hamza & Willoughby, 2011; Sagrestano, Paikoff, Holmbeck, & Fendrich, 2003), suggesting that active monitoring may buffer against the development of internalizing problems.
Community.
Community resources such as extrafamilial figures and neighborhood characteristics may also buffer the impact of bereavement for youth who have been maltreated (Oshri et al., 2017). We expected that the presence of a supportive adult figure would serve as a protective resource in the relation between preadolescent bereavement and psychopathology. Supportive adult figures, which may include teachers, mentors, coaches, and family friends, can help reduce the perceived isolation and lack of support that often stems from the experience of close loss (Lerner et al., 2013; Resnick, Harris, & Blum, 1993; Werner, 2005). Amongst children experiencing chronic adversity, supportive adult relationships have been shown to promote better adaptation (Masten, Best, & Garmezy, 1990) and predict fewer problem behaviors (Zimmerman, Bingenheimer, & Notaro, 2002). Supportive non-familial adult figures may be a particularly valuable resource for maltreated youth who do not have strong or consistent relationships with their caregivers.
Positive neighborhood characteristics have also been found to mitigate the link between stressful life events and adolescent behavior problems (Fagan, Wright, & Pinchevsky, 2014). Neighborhood collective efficacy is defined as a connection of social cohesion, mutual trust, and shared expectation for the common good of the community (Ohmer, 2007), and is a commonly reported protective factor among high-risk adolescents (Masten, 2014). When tragic life events occur, such as the death of a family member, neighbors in a community with high collective efficacy offer support and encouragement to families in need. Whereas higher levels of neighborhood collective efficacy have been associated with lower levels of externalizing (Yonas et al., 2010) and internalizing behaviors (Ma & Grogan-Kaylor, 2017), negative neighborhood contexts have been associated with problem and risk behaviors amongst maltreated youth (Jaffee, Caspi, Moffitt, Polo-Tomás, & Taylor, 2007). Thus, neighborhoods who exhibit positive characteristics, such as social cohesion and helpfulness, may serve to protect maltreated youth in the association between significant loss and internalizing and externalizing problems.
Developmental Timing of Protective Factors
Conforming to the developmental psychopathology perspective on adolescence (Cicchetti & Rogosch, 2002), it is expected that the protective effects of contextual factors will vary across developmental timing, due to the discrete developmental tasks associated with early versus later adolescence. Coping strategies or resources that work for a child at one point in time may reveal themselves as less advantageous at another point. For example, the parent-child relationship may be more salient during early adolescence, compared to later adolescence. As youth transition to adolescence, they increasingly strive for autonomy which is manifested in preference for time with peers versus parents (McElhaney, Allen, Stephenson, & Hare, 2009). Similarly, taking into account the increased autonomy associated with later adolescence (e.g., getting driver’s license, starting first job), it is possible that individual-level future orientation would be a more developmentally relevant and potent protective factor at this time point. Indeed, a previous study examining protective factors across adolescence observed that whereas some protective factors (e.g., community opportunities, family attachment, healthy beliefs) declined during middle school, many others emerged (e.g., community recognition, academic success, prosocial involvement) during the transition into high school (Kim, Oesterle, Catalano, & Hawkins, 2015). Therefore, in the present study, we anticipated that protective factors at age 14 and 16 would differentially impact maltreated youths’ vulnerability to problem behaviors following the death of a loved one.
The Present Study
The present study utilized a large longitudinal sample of youth with documented records of maltreatment (e.g., Child Protective Services) to examine the association between preadolescent bereavement and adolescent internalizing and externalizing symptomology in youth with a history of maltreatment. Further, guided by the ecological/transactional model of developmental psychopathology (Cicchetti & Valentino, 2006), the present study aimed to examine whether protective factors from multiple levels of the youths’ ecology influenced the impact of bereavement on adolescent psychopathology. The overall goal of this investigation was to enhance knowledge on the effects of youth bereavement in the context of families with child abuse and neglect histories.
This investigation addresses a significant gap in the literature on both bereavement and child abuse and neglect by examining two main research questions. First, will the experience of bereavement in early adolescence predict internalizing and externalizing symptomology in later adolescence for youth with a history of child maltreatment? Second, can the presence of multilevel protective factors (e.g., intrapersonal, family, community) buffer the link between adolescent bereavement and psychopathology in maltreated youth? To account for the fact that certain protective factors may reveal themselves more salient at different age points, the present study measured protective factors at two time-points (e.g., age 14 and 16). We hypothesized that the experience of bereavement would be associated with increased risk for internalizing and externalizing psychopathology in maltreated youth (Hypothesis 1). Further, we hypothesized that future orientation, parent-child relationships, parental monitoring, supportive adult figures, and neighborhood collective efficacy would each serve as moderators in the relation between bereavement and psychopathology outcomes (Hypothesis 2). With concern to developmental timing, we hypothesized that family-focused variables (parent-child relationships, parental monitoring, future orientation for family) would reveal themselves more salient during early adolescence, at age 14 than at age 16. Conversely, we hypothesized that, compared to age 14, individual-level future orientation would be more significant during later adolescence, at age 16. Lastly, we hypothesized that there would be no significant difference between the protective effects of community-level factors (neighborhood collective efficacy, supportive adult figures) at ages 14 or 16 (Hypothesis 3).
Methods
Sample
The data for this study were obtained from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) consortium of studies, which consists of a sample of youth and their primary caregivers (N = 1,354). Studies were initiated at five different geographical regions throughout the United States. Of the five sites, three were primarily urban communities (East, Midwest, and Northwest), one was primarily suburban (Southwest), and one included urban, suburban, and rural communities (South). The eligibility criteria to participate in the study differed across regions, with each cohort representing a different level of risk for exposure to child maltreatment. Thus, the LONGSCAN sample consists of both maltreated and non-maltreated youth. Data collection for the study began when children were four years old (Mage = 4.56, SD = .70) and evaluations took place every two years until the final assessment at age 18 (Mage = 18.51, SD = .62). Informed consent and assent were obtained from all individuals participating in the study, before any study procedures began (Runyan et al., 2014). Three data collection time points were used for this study: Time 1 (Mage = 12.37, SDage = .44), Time 2 (Mage =14.35, SDage = .45) and Time 3 (Mage = 16.32, SDage = .44).
In the present study, a secondary data analysis was conducted utilizing a subsample of youth who were maltreated at or before the age of 12 (N = 800; 52.4% female). Using the records provided from Child Protective Services, a dichotomous variable was created (0 = no maltreatment, 1 = maltreatment present) that indicated whether or not the child had any record of substantiated neglect, physical abuse, emotional abuse, and/or sexual abuse, between birth and the age-12-time point. Participants who reported a score of “0” across all of the maltreatment types were removed from the dataset. In this subsample, a majority of the participants were African-American (45.1%), followed by Caucasian (29.4%), Mixed Race (15.4%), Hispanic (8.6%), Native American, (0.8%), Asian/Pacific Islander (0.4%), and Other (0.3%). Further, a majority of families reported receiving federal financial assistance (58.9%), 41.5% of primary caregivers reported not having finished high school, and 30.4% reported high school as their highest level of education.
Measures
Bereavement.
Bereavement was measured using the Child’s Life Events Scale, which was adapted from a prior measure of significant life events (CLES; Coddington, 1972). At the age-12-time point, primary caretakers reported on significant life events that had occurred in the child’s life during the past year. Response options indicated whether or not the specific life event had occurred (0 = “no”, 1 = “yes”). In the present study, an item indicating the child’s experience of bereavement was utilized (“Did anyone who was close to the child die during the past year?”). Among the study sample utilized, 15.1% (N = 121) of youth were reported to have experienced close death within the past year.
Internalizing and Externalizing Symptoms.
Internalizing and externalizing symptomology was assessed utilizing the Child Behavior Checklist (CBCL/4–18; Achenbach, 1991). Primary caregivers were interviewed at the age-16-time point regarding their child’s behavior problems. The externalizing subscale of the CBCL is composed of delinquent and aggressive syndromes (e.g., argues a lot, steals at home, gets in many fights). The internalizing subscale of the CBCL is composed of anxiety/depression, social withdrawal, and somatic complaints scales (e.g., feels worthless, fearful or anxious). Scores ranged from 0 to 62, with higher scores indicating higher levels of behavioral problems. The internal consistencies for the internalizing and externalizing scales of the CBCL at age-16 were excellent (α = .90; α = .94, respectively). Raw total scores were utilized in the analysis, as recommended for longitudinal data analysis (Moeller, 2015).
Future Orientation.
Future orientation (FO) was measured using the Future Events Questionnaire (Knight, Smith, Martin, Lewis, & the LONGSCAN Investigators, 2008). Adolescents responded to items assessing their level of future expectation in regards to family, education/career, and employment. The family subscale consisted of four items asking about the adolescent’s future expectations for their family life (e.g., “How likely is it that you will have a child without being married?”). The education subscale consisted of five items regarding the child’s expectations for their future education and career (e.g., “How likely is that you will go to college?”; “How likely is it that you will have a successful career?”). The employment subscale consisted of three items assessing future employment concerns (e.g., “How likely is it that you will lose your job?”). Youth indicated the likelihood to which they believed each specific event would occur using a 5-point scale, ranging from 1 (very unlikely) to 5 (very likely). For the present study, the education and employment subscales were summed to create “Individual FO,” due to conceptual overlap. A mean score of the responses was derived and used for analysis. Internal consistencies at the age 14-time point were α = .64 for family FO and α = .79 for individual FO. Internal consistencies at the age 16-time point were α = .77 for family FO and α = .66 for individual FO.
Parent-Child Relationship Quality.
Parent-child relationships were measured via adolescent self-report using the Quality of Parent-Child Relationship measure, adapted from the National Longitudinal Study of Adolescent Health (Add Health: Resnick et al., 1997). The domain measuring the adolescent’s perception of the overall relationship quality was used in this study. This subscale consisted of six questions regarding closeness, caring, understanding, trust, getting along, and shared decision making, (e.g., “How close do you feel to your father/mother?”; “Do you and he/she get alone?”). Responses were assessed using a 5-point Likert scale ranging from 1 (not at all or never) to 5 (very much or always). The quality of relationship score for both father and mother was created by computing a mean score of the six items. An overall parent-child relationship quality index was created by averaging these two scores. Internal consistency for the quality of relationship subscale at age 14 (maternal α = .85; paternal α = .88) and age 16 (maternal α = .85; paternal α = .89) were good.
Parental Monitoring.
The adolescent’s level of parental monitoring was assessed using the Parental Monitoring measure (adapted from Patterson & Stouthamer-Loeber, 1984). Primary caregivers responded to five items regarding parental monitoring amongst three broad domains, including knowledge about children’s friends, activities, and use of money. Responses ranged from 0 (don’t know) to 2 (know a lot). Mean scores were computed across all domains, with higher scores representing higher levels of parental monitoring. The reliability of the parental monitoring scale was α = .79 at the age-14-time point and α = .82 at the age-16-time point.
Supportive Adult Figures.
The presence of supportive adult figures was measured using the Resilience Factors measure (Knight, Smith, Martin, Lewis, & LONGSCAN Investigators, 1998). The measure includes four domains: supportive adults, religiosity, extracurricular activities, and leadership. This study utilized the supportive adult subscale, which consisted of six items assessing the level of familial and extrafamilial adult support available to the child, (e.g., “Is there an adult you can turn to for help if you have a serious problem?”; “Has there ever been an adult, outside of your family, who has encouraged you and believed in you?”). Responses were assessed utilizing a binary variable indicating whether or not the statement was true (0 = “no”, 1 = “yes”). Counts were derived across items to create a total sum score of supportive adult figures.
Neighborhood Collective Efficacy.
Neighborhood collective efficacy was measured using the Quality of Neighborhood, Residential Stability Organizational and Religious Affiliation questionnaire, which was adapted from previous measures of neighborhood context (Coulton, Korbin, & Su, 1996; Sampson, Raudenbush, & Earls, 1997). The subscale of neighborhood collective efficacy was utilized in this study as an indicator of social cohesion amongst the child’s neighborhood. Primary caregivers responded to items asking about community cohesion, and willingness to intervene on behalf of the neighborhood (e.g., “People around here help their neighbors”; “Neighbors can be trusted”). Responses ranged from 1 (strongly disagree) to 4 (strongly agree). Mean scores were derived from these items, with higher scores indicating higher degrees of collective efficacy. Internal consistency for the neighborhood efficacy subscale was strong (Age 14 α = .91; Age 16 α = .91).
Covariates.
Control variables in this study included gender, race, socio-economic status (SES), internalizing and externalizing symptoms at age 12, bereavement at age 14, maltreatment ages 12–16, and other major life events. Participants’ gender was coded as “1” = male and “2” = female. Race of the participant was included as a dichotomous variable where “1” = African-American and “0” = Other. No other ethnicities were included as covariates due to their small representativeness and lack of correlation with the study variables. SES was measured using a cumulative index that included both measured and perceived indicators of socioeconomic status (Diemer, Mistry, Wadsworth, López, & Reimers, 2013). A score of “1” was given for the following risk factors: use of government financial assistance, caretakers on average holding less than high school education, income between $15,000 to $19,999 or less annually, and a response of either “somewhat bothered” or “bothered a great deal” to a question regarding worries about having money for basic necessities. Scores on this summed measure of socioeconomic risk ranged from zero (not socioeconomically disadvantaged) to four (very socioeconomically disadvantaged), with a mean score of 1.96 (SD = 1.32). Age 12 internalizing (α = .88) and externalizing (α = .92) symptoms were included as covariates utilizing data from the CBCL. Maltreatment between ages 12–16 were included using records from Child Protective Services. Bereavement at age 14 was measured using the CLES, with 15.0% of youth reporting to have experienced loss. Lastly, to account for other major life events, CLES items that were endorsed by at least 15% of the sample at the age-12-time point were included as covariates: child or family moved to a new place (15.9%), child began in a new school or changed schools (34.4%).
Analytic Plan
To test the study hypotheses, path analysis models were created using Mplus 7.4 (Muthén & Muthén, 1998–2010). Missing data varied for each variable and time point, ranging from 0% to 43.8%. At the age-16-time point missing data due to attrition was 33.4%. A missing data analysis was conducted, revealing that missing data were related to observed study variables. Therefore, analyses were performed under the assumption of data missing at random (MAR; Schafer & Graham, 2002). Further, a full information maximum likelihood (FIML) method was utilized to estimate missing data. FIML has been found to result in unbiased parameter estimates when working with data assumed to be MAR (Enders & Bandalos, 2001). Fit indices were used to assess whether or not the data was a good fit for the model based on published criteria (Hu & Bentler, 1999). Absolute fit was evaluated using the root mean square error of approximation (RMSEA) and the standardized root mean square residual (SRMR), with values below 0.06 and 0.08, respectively, representing a good fit. Further, the Comparative Fit Index (CFI) was utilized to determine relative model fit, with values of 0.95 or higher indicating a good fit (Hu & Bentler, 1999). If the measurement models met the fit index standards mentioned above, they were determined to be satisfactory.
Path models were utilized to test if bereavement at age 12 significantly predicated internalizing and externalizing symptoms at age 16. Then, to test for moderation, separate models were tested for each protective factor at each time point. Variables were mean-centered and interaction terms were computed between the predictor (bereavement) and each potential moderating factor (e.g., bereavement * future orientation). The interaction term was covaried with the predictor and moderator variable in each model, as per standard guidelines. Control variables included race, SES risk, gender, age 12 internalizing and externalizing, age 14 bereavement, age 12–16 maltreatment, and other major life events. Non-significant covariates were trimmed from the final model. Last, the simple slopes procedure was performed in order to probe significant interactions (Aiken & West, 1991).
Results
Descriptive Statistics and Bivariate Correlations
See Table 1 and Table 2 for descriptive statistics and bivariate correlations. Correlations revealed that there was a significant positive association between bereavement and externalizing problems, r =.14, p < .01. However, the correlation coefficient for this association was much lower than expected, indicating the possible presence of moderators in this association. Thus, we continued with additional moderation analyses.
Table 1.
Bivariate Correlations and Descriptive Statistics for Age 14 Protective Factors
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Bereavement (age 12) | — | |||||||||||||
| 2. FO for individual (age 14) | −.03 | — | ||||||||||||
| 3. FO for family (age 14) | −.06 | .36 *** | — | |||||||||||
| 4. Supportive adults (age 14) | .00 | .20*** | .10* | — | ||||||||||
| 5. Parent-child RQ (age 14) | −.03 | .28*** | .12* | .12* | — | |||||||||
| 6. Parental monitoring (age 14) | −.16*** | .04 | .04 | .08 | .09 | — | ||||||||
| 7. Neighborhood (age 14) | .05 | .13** | .08 | .02 | −.01 | .14** | — | |||||||
| 8. Sex (1 = Male, 2 = Female) | .01 | .05 | −.02 | .01 | −.21*** | .07 | .02 | — | ||||||
| 9. Race (1 = Black, 0 = Other) | .03 | .14** | .00 | .04 | .17** | −.12* | −.08 | .03 | — | |||||
| 10. Family/child moved (age 12) | .02 | − .09 | −.07 | −.01 | −.00 | .02 | −.03 | −.01 | −.06 | — | ||||
| 11. Externalizing (age 12) | .09* | −.16** | −.05 | −.05 | −.15** | −.20*** | −.15** | −.14** | −.11** | .01 | — | |||
| 12. Internalizing (age 12) | .11** | −.14** | −.04 | −.03 | −.19** | −.11* | −.14** | .01 | −.17*** | .06 | .67*** | — | ||
| 13. Externalizing (age 16) | .14** | −.17** | −.07 | −.11* | −.16** | −.19*** | −.02 | −.07 | −.12** | −.06 | .62*** | .39*** | — | |
| 14. Internalizing (age 16) | .04 | −.17** | −.08 | −.06 | −.14* | −.13* | −.08 | .10* | −.17*** | −.00 | .45*** | .52*** | .70*** | — |
| M | .22 | 7.51 | 3.91 | 5.09 | 4.05 | 1.75 | 2.95 | 1.52 | .45 | .23 | 13.57 | 8.31 | 12.27 | 8.13 |
| SD | .41 | 1.29 | .74 | 1.31 | .63 | .35 | .50 | .50 | .50 | .42 | 10.36 | 7.23 | 11.08 | 8.20 |
| Skewness | 1.39 | −.03 | −.11 | −1.68 | −.75 | −2.16 | −.42 | −.10 | .20 | 1.31 | 1.10 | 1.33 | 1.48 | 1.48 |
Notes. Bereavement is coded as 0 = No 1 = Yes; FO = Future orientation; RQ = Relationship quality; Neighborhood = Neighborhood efficacy.
p < .05
p < .01
p < .001
Table 2.
Bivariate Correlations and Descriptive Statistics for Age 16 Protective Factors
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Bereavement (age 12) | — | |||||||||||||
| 2. FO for individual (age 16) | −.01 | — | ||||||||||||
| 3. FO for family (age 16) | −.04 | .26*** | — | |||||||||||
| 4. Supportive adults (age 16) | −.02 | .15** | .15** | — | ||||||||||
| 5. Parent-child RQ (age 16) | −.05 | .06 | −.00 | .25*** | — | |||||||||
| 6. Parental monitoring (age 16) | −.11* | .04 | .08 | .07 | .16** | — | ||||||||
| 7. Neighborhood (age 16) | −.06 | .08 | .11* | .10* | .01 | .17** | — | |||||||
| 8. Sex (1 = Male, 2 = Female) | .01 | .17*** | .14** | .03 | −.08 | .06 | .04 | — | ||||||
| 9. Race (1 = Black, 0 = Other) | .03 | .08 | −.12** | .07 | .16** | −.17** | −.17*** | .03 | — | |||||
| 10. Family/child moved (age 12) | .02 | .04 | .08 | −.00 | .08 | .05 | −.01 | −.01 | −.06 | — | ||||
| 11. Externalizing (age 12) | .09* | −.08 | −.03 | −.06 | −.13** | −.21** | −.19*** | −.14** | .11** | .01 | — | |||
| 12. Internalizing (age 12) | .11** | .01 | −.02 | −.10* | −.15** | −.11* | −.17** | .01 | −.17*** | .06 | .67*** | — | ||
| 13. Externalizing (age 16) | .14** | −.04 | .08 | −.15** | −.26*** | −.39** | −.12** | −.07 | −.12** | −.06 | .62*** | .39*** | — | |
| 14. Internalizing (age 16) | .04 | −.05 | .07 | −.21*** | −.22*** | −.25** | −.14** | .10* | −.17*** | −.00 | .45*** | .52*** | .70*** | — |
| M | .22 | 3.22 | 3.82 | 5.22 | 3.90 | 1.64 | 2.95 | 1.52 | .45 | .23 | 13.57 | 8.31 | 12.27 | 8.13 |
| SD | .41 | .49 | 1.00 | 1.39 | .74 | .45 | .53 | .50 | .50 | .42 | 10.36 | 7.23 | 11.08 | 8.20 |
| Skewness | 1.39 | −.47 | −.84 | −2.15 | −.63 | −1.65 | −.60 | −.10 | .20 | 1.31 | 1.10 | 1.33 | 1.48 | 1.48 |
| Kurtosis | −.08 | 2.13 | .45 | 4.31 | −.03 | 2.38 | 1.50 | −2.00 | −1.97 | −.29 | 1.30 | 2.11 | 2.32 | 2.55 |
Notes. Bereavement is coded as 0 = No 1 = Yes; FO = Future orientation; RQ = Relationship quality; Neighborhood = Neighborhood efficacy.
p < .05
p < .01
p < .001
Moderation Analyses
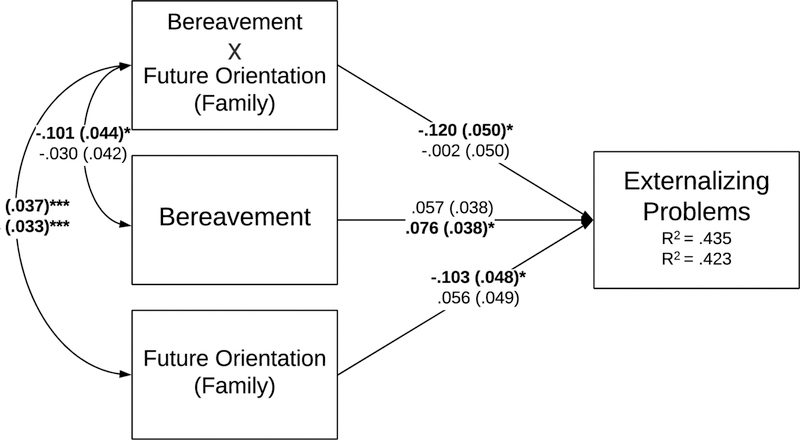
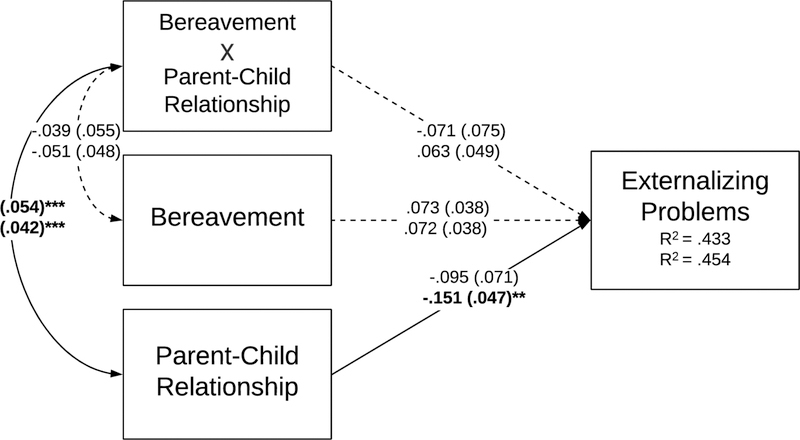
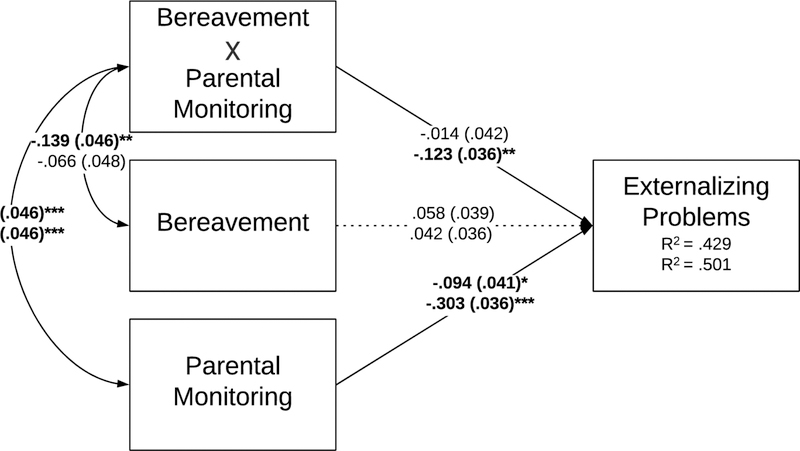
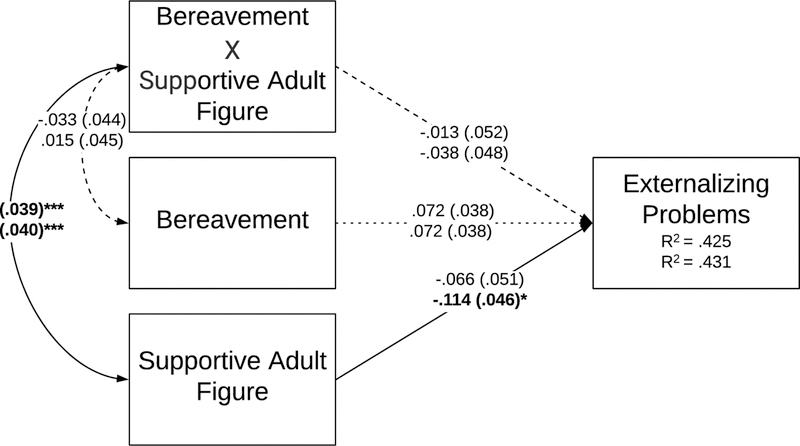
A path model was created to test the direct link between bereavement and problem behaviors. When controlling for internalizing and externalizing at age 12, the analysis revealed that close loss significantly predicted prospective symptoms of externalizing (β = .085, SE = .041, p < .05, 95% CI [.005, .164]), but not internalizing symptoms (β = −.007, SE = .044, p = .881, 95% CI [−.093, .080]). Thus, subsequent moderation analysis models were focused on externalizing outcomes. Interaction terms were used to test the moderating role of individual assets (e.g., future orientation), family factors (e.g., parental monitoring), and community resources (e.g., neighborhood efficacy) in the association between bereavement and externalizing behavior problems (Table 3; Figures 1–6). Path analyses showed that individual future orientation (age 14), family future orientation (age 14), parental monitoring (age 16) and neighborhood collective efficacy (age 16) each significantly moderated the pathway between bereavement and externalizing symptoms (See Figures 7–10).
Table 3.
Parameters for Path Models Testing Moderation
| Models testing protective factors at age-14 | Models testing protective factors at age-16 | ||||
|---|---|---|---|---|---|
| Model 1a | B (SE) | 95% CI | Model 1b | B (SE) | 95% CI |
| Externalizing (age 16) | Externalizing (age 16) | ||||
| Bereavement (age 12) | 2.75 (1.32) | [.006, .154]* | Bereavement (age 12) | 2.57 (1.33) | [−.001, .149]† |
| FO (individual) | −0.22 (.54) | [−.109, .079] | FO (individual) | 0.12 (.53) | [−.081, .102] |
| Bereavement X FO (ind) | 3.25 (1.54) | [.018, .210]* | Bereavement X FO (ind) | −0.42 (1.58) | [−.105, .080] |
| Sex (1=Male, 2=Female) | 0.81 (.79) | [−.029, .109] | Sex (1=Male, 2=Female) | 0.80 (.81) | [−.035, .106] |
| Race (1=Black, 0=Other) | −0.75 (.81) | [−.102, .038] | Race (1=Black, 0=Other) | −0.88 (.80) | [−.109, .031] |
| Family/child moved | −2.19 (.98) | [−.152, −.009]* | Family/child moved | −2.07 (.99) | [−.150, −.005]* |
| Externalizing (age 12) | 0.68 (.41) | [.566, .684]*** | Externalizing (age 12) | 0.69 (.04) | [.556, .694]*** |
| Model 2a | B (SE) | 95% CI | Model 2b | B (SE) | 95% CI |
| Externalizing (age 16) | Externalizing (age 16) | ||||
| Bereavement (age 12) | 1.97 (1.33) | [−.019, .132] | Bereavement (age 12) | 2.62 (1.32) | [.001, .150]* |
| FO (family) | −1.15 (.54) | [−.197, −.008]* | FO (family) | 0.63 (.55) | [−.040, .152] |
| Bereavement X FO (fam) | −3.82 (1.60) | [−.219, −.021]* | Bereavement X FO (fam) | −0.05 (1.64) | [−.100, .097] |
| Sex (1=Male, 2=Female) | 0.70 (.79) | [−.038, .100] | Sex (1=Male, 2=Female) | 0.63 (.81) | [−.043, .098] |
| Race (1=Black, 0=Other) | −0.97 (.80) | [−.112, .026] | Race (1=Black, 0=Other) | −0.68 (.81) | [−.100, .040] |
| Family/child moved | −2.02 (.98) | [−.147, −.004]* | Family/child moved | −2.07 (.98) | [−.149, −.005]* |
| Externalizing (age 12) | 0.68 (.04) | [.567, .685]*** | Externalizing (age 12) | 0.68 (.04) | [.574, .691]*** |
| Model 3a | B (SE) | 95% CI | Model 3b | B (SE) | 95% CI |
| Externalizing (age 16) | Externalizing (age 16) | ||||
| Bereavement (age 12) | 2.54 (1.32) | [−.002, .148]† | Bereavement (age 12) | 2.51 (1.30) | [−.001, .146]† |
| Parent-child relationship | −1.07 (.80) | [−.234, .043] | Parent-child relationship | −1.68 (.53) | [−.244, −.058]** |
| Bereavement X PCR | −2.19 (2.30) | [−.217, .075] | Bereavement X PCR | 2.03 (1.57) | [−.033, .159] |
| Sex (1=Male, 2=Female) | 0.54 (.85) | [−.050, .097] | Sex (1=Male, 2=Female) | 0.37 (.78) | [−.052, .085] |
| Race (1=Black, 0=Other) | −0.59 (.84) | [−.098, .046] | Race (1=Black, 0=Other) | −0.28 (.79) | [−.081, .057] |
| Family/child moved | −1.86 (.99) | [−.142, −.003]† | Family/child moved | −1.63 (.98) | [−.132, .010]† |
| Externalizing (age 12) | 0.68 (.04) | [.562, .686]*** | Externalizing (age 12) | 0.65 (.04) | [.543, .666]*** |
| Model 4a | B (SE) | 95% CI | Model 4b | B (SE) | 95% CI |
| Externalizing (age 16) | Externalizing | ||||
| Bereavement (age 12) | 2.02 (1.36) | [−.019, .135] | Bereavement (age 12) | 1.46 (1.24) | [−.028, .113] |
| Parental monitoring | −1.06 (.46) | [−.175, −.014]* | Parental monitoring | −3.39 (.40) | [−.373, −.234]*** |
| Bereavement X PM | −0.43 (1.31) | [−.096, .068] | Bereavement X PM | −3.87 (1.13) | [−.193, −.053]** |
| Sex (1=Male, 2=Female) | 0.91 (.79) | [−.029, .110] | Sex (1=Male, 2=Female) | 0.69 (.74) | [−.034, .095] |
| Race (1=Black, 0=Other) | −1.21 (.82) | [−.125, .017] | Race (1=Black, 0=Other) | −2.02 (.76) | [−.156, −.024]** |
| Family/child moved | −2.12 (.98) | [−.151, −.007]* | Family/child moved | −1.60 (.92) | [−.127, .007]† |
| Externalizing (age 12) | 0.67 (.04) | [.555, .678]*** | Externalizing (age 12) | 0.61 (.04) | [.499, .623]*** |
| Model 5a | B (SE) | 95% CI | Model 5b | B (SE) | 95% CI |
| Externalizing | Externalizing | ||||
| Bereavement (age 12) | 2.50 (1.32) | [−.003, .147]† | Bereavement (age 12) | 2.48 (1.31) | [−.003, .146]† |
| Supportive adult figure | −0.74 (.57) | [−.166, .034] | Supportive adult figure | −1.27 (.52) | [−.204, −.023]* |
| Bereavement X SAF | −0.42 (1.71) | [−.114, .088] | Bereavement X SAF | −1.27 (1.60) | [−.131, .055] |
| Sex (1=Male, 2=Female) | 0.83 (.80) | [−.033, .106] | Sex (1=Male, 2=Female) | 0.86 (.79) | [−.031, .107] |
| Race (1=Black, 0=Other) | −0.78 (.80) | [−.104, .035] | Race (1=Black, 0=Other) | −0.77 (.80) | [−.104, .035] |
| Family/child moved | −2.00 (.98) | [−.147, −.003]* | Family/child moved | −1.98 (.98) | [−.145, −.003]* |
| Externalizing (age 12) | 0.68 (.04) | [.573, .690]*** | Externalizing (age 12) | 0.67 (.04) | [.566, .684]*** |
| Model 6a | B (SE) | 95% CI | Model 6b | B (SE) | 95% CI |
| Externalizing | Externalizing | ||||
| Bereavement (age 12) | 2.37 (1.33) | [−.007, .143]† | Bereavement (age 12) | 2.15 (1.32) | [−.012, .136] |
| Neighborhood efficacy | 0.75 (.55) | [−.029, .163] | Neighborhood efficacy | −0.55 (.43) | [−.125, .027] |
| Bereavement X NE | −0.28 (1.60) | [−.109, .091] | Bereavement X NE | −3.87 (1.21) | [−.204, −.049]** |
| Sex (1=Male, 2=Female) | 0.86 (.80) | [−.031, .107] | Sex (1=Male, 2=Female) | 0.84 (.79) | [−.032, .106] |
| Race (1=Black, 0=Other) | −0.65 (.80) | [−.099, .041] | Race (1=Black, 0=Other) | −0.61 (.81) | [−.098, .043] |
| Family/child moved | −1.95 (.98) | [−.145, − .001]* | Family/child moved | −1.90 (.97) | [−.142, .000]† |
| Externalizing (age 12) | 0.70 (.04) | [.589, .708]*** | Externalizing (age 12) | 0.68 (.04) | [.572, .693]*** |
Notes. FO future orientation, PCR parent-child relationship, PM parental monitoring, SAF supportive adult figure, NE neighborhood efficacy; fam = family. In bold are significant interactions indicating moderation.
p < .10,
p < .05,
p < .01,
p < .001
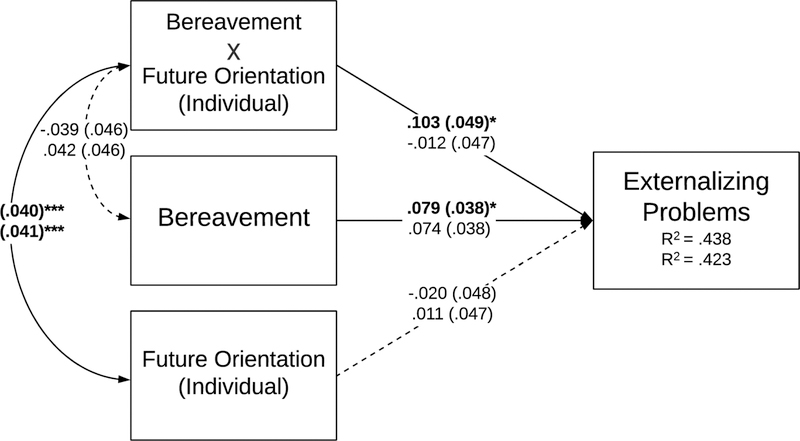
Figure 1.
Path Analysis Model of the Moderating Effect of Future Orientation (Individual) on the Association between Bereavement and Externalizing Problems (N = 800).
Notes. Standardized parameters are shown in figure. In each path, the top numbers are for the model using the age 14 protective factor and the bottom numbers are for the model using the age 16 protective factor. Model fit was good; Age-14 Model: RMSEA = .00, CFI = 1.00, TLI = 1.03, SRMR = .004; Age-16 Model: RMSEA = .00, CFI = 1.00, TLI = 1.04, SRMR = .002.
*p < .05, **p < .01, ***p < .001
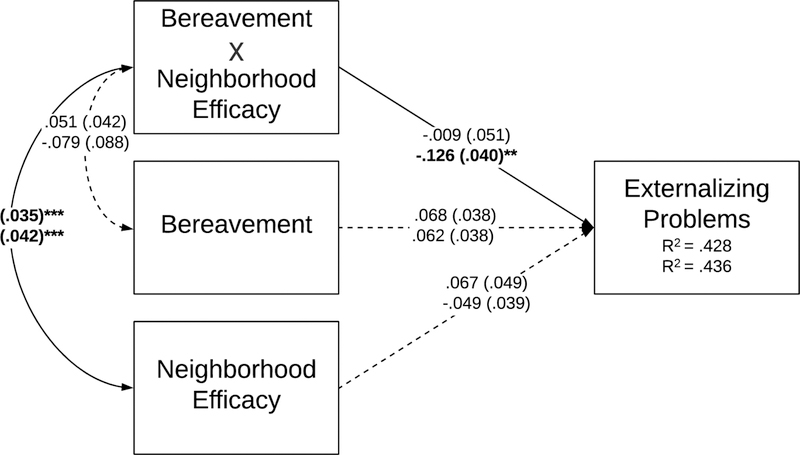
Figure 6.
Path Analysis Model of the Moderating Effect of Neighborhood Efficacy on the Association between Bereavement and Externalizing Problems (N = 800).
Notes. Standardized parameters are shown in figure. In each path, the top numbers are for the model using the age 14 protective factor and the bottom numbers are for the model using the age 16 protective factor. Model fit was good; Age-14 Model: RMSEA = .046, CFI = .995, TLI = .939, SRMR = .013; Age-16 Model: RMSEA = .00, CFI = 1.00, TLI = 1.03, SRMR = .005.
*p < .05, **p < .01, ***p < .001
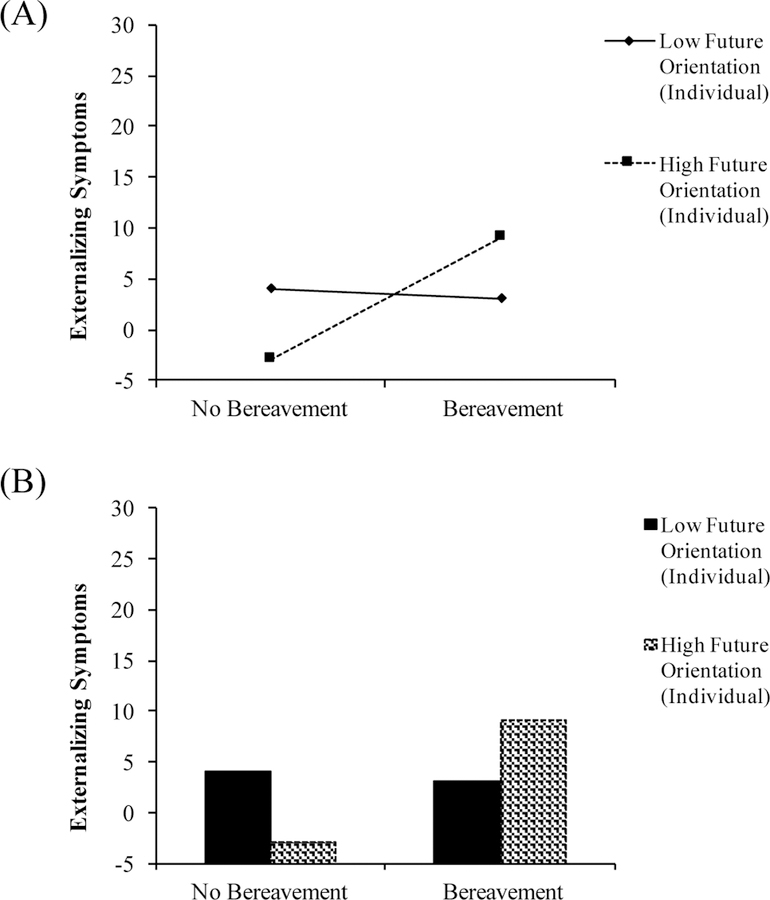
Figure 7.
Moderation effect of future orientation (individual) on the association between bereavement and externalizing behaviors.
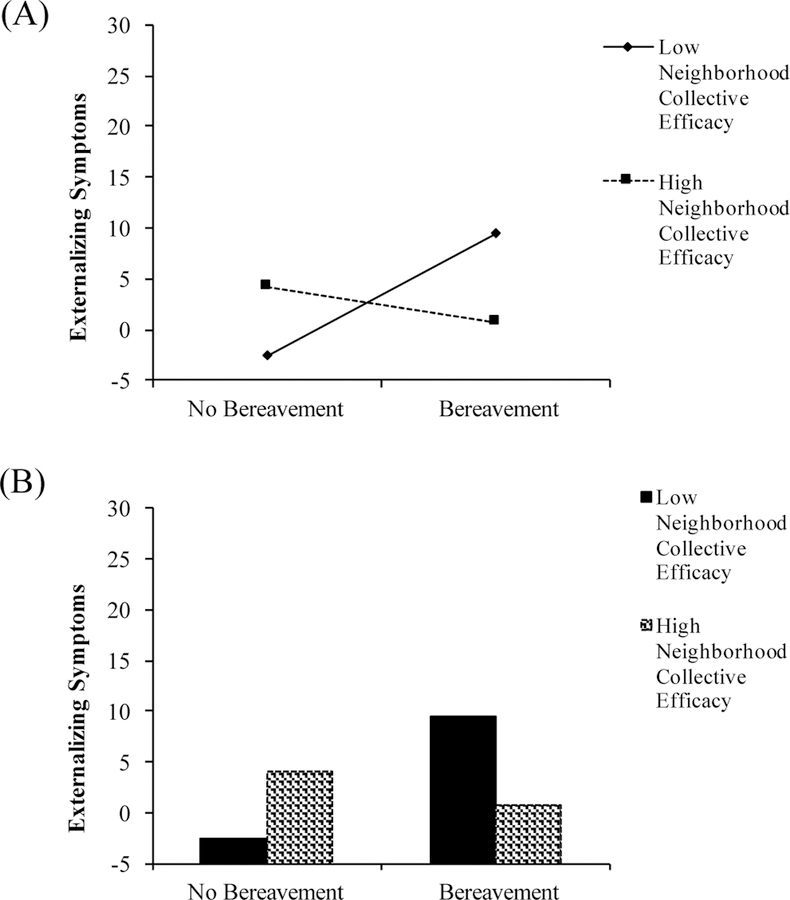
Figure 10.
Moderation effect of neighborhood collective efficacy on the association between bereavement and externalizing behaviors.
In the Model 1a testing individual-level future orientation at age 14, bereavement significantly predicted externalizing (β = .079, SE = 1.321, p < .05, 95% CI [.006, .154]), but individual FO did not (β = −.020, SE = .539, p = .680, 95% CI [−.109, .079]). Further, the interaction term (bereavement * individual FO) significantly predicted externalizing symptomology, indicating moderation (β = .103, SE = 1.535, p < .05, 95% CI [.018, .210]). The moderation was then probed using the simple slopes technique (See Figure 7). For youth who did not experience bereavement, high levels of individual FO predicted lower levels of externalizing problems. However, for youth who experienced bereavement, high levels of individual FO were associated with higher levels of externalizing symptoms, and lower levels of FO were associated with lower externalizing symptoms.
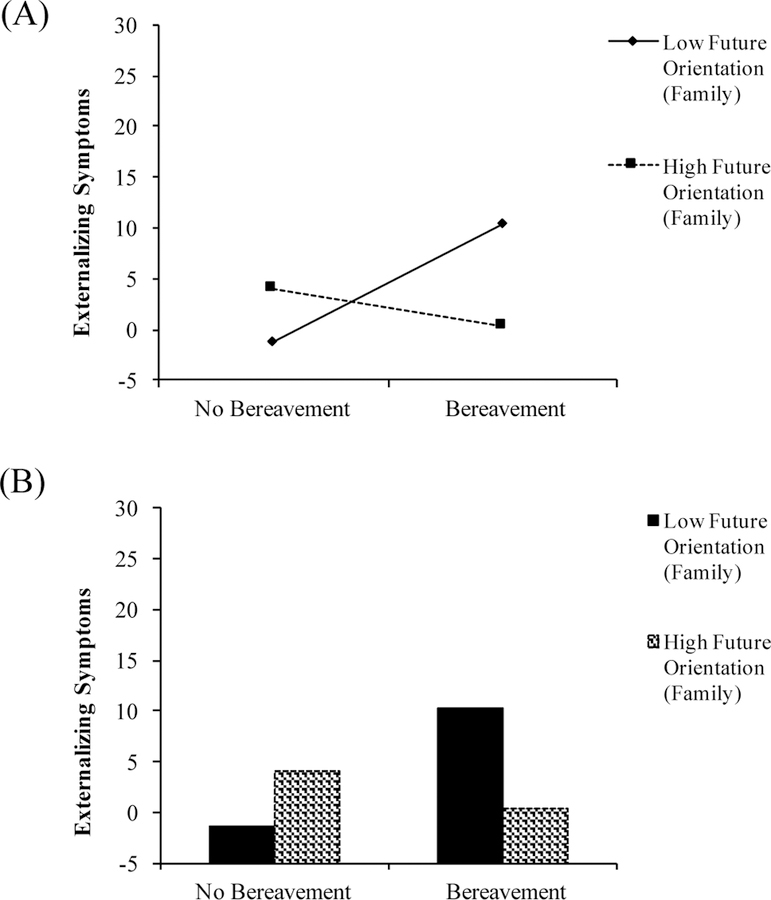
In the Model 2a testing family-related future orientation at age 14, bereavement did not predict prospective symptoms of externalizing (β = .057, SE = 1.334, p = .140, 95% CI [−.019, .132]). However, FO (family) did significantly predict less externalizing symptomology (β = - .103, SE = .544, p < .05, 95% CI [−.197, −.008]). Further, the interaction term significantly predicted externalizing symptomology, indicating moderation (β = −.120, SE = 1.603, p < .05, 95% CI [−.219, −.021]). The moderation was probed using simple slopes analysis (See Figure 8). Youth with low levels of family-related future orientation who experienced bereavement were more likely to exhibit high levels of externalizing symptoms, whereas high levels of family-related future orientation buffered the association between bereavement and externalizing symptoms.
Figure 8.
Moderation effect of future orientation (family) on the association between bereavement and externalizing behaviors.
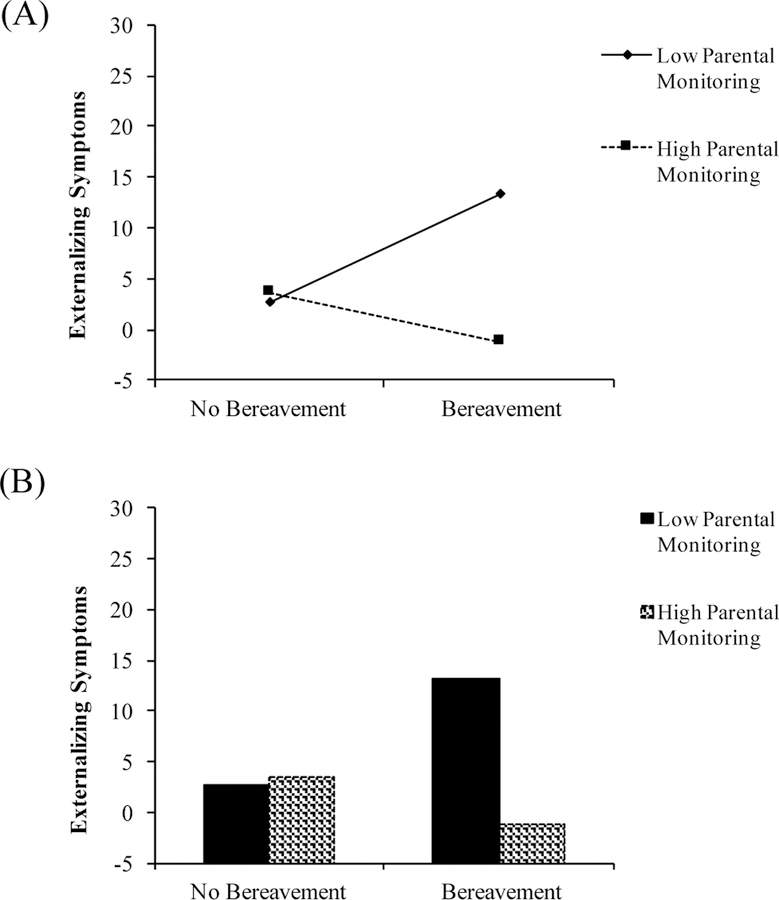
In Model 4b testing parental monitoring at age 16, bereavement did not significantly predict externalizing symptoms (β = .042, SE = 1.243, p = .239, 95% CI [−.028, .113]). Parental monitoring was a significant predictor of adolescent externalizing problems (β = −.303, SE = .402, p < .001, 95% CI [−.373, −.234]). In addition, the interaction term (bereavement * parental monitoring) significantly predicted change in externalizing behaviors, indicating moderation (β = −.123, SE = 1.125, p < .01, 95% CI [−.193, −.053]). The moderation was then probed using the simple slopes technique (See Figure 9). For youth who did not experience bereavement, there was no difference in externalizing symptoms by level of parenting monitoring. However, for youth who experienced bereavement, low levels of parental monitoring was associated with higher externalizing symptomology, whereas high levels of parental monitoring was associated with lower externalizing symptomology. Thus, low levels of parental monitoring exacerbated the deleterious effect of bereavement on externalizing symptoms.
Figure 9.
Moderation effect of parental monitoring on the association between bereavement and externalizing behaviors.
Lastly, in Model 6b testing neighborhood collective efficacy at age 16, neither bereavement nor neighborhood efficacy were significant predictors of externalizing problems (β = .062, SE = 1.316, p = .103, 95% CI [−.012, .136]; (β = −.049, SE = .434, p = .208, 95% CI [−.125, .027]; respectively). However, the interaction term (bereavement * collective efficacy) significantly predicted change in externalizing behaviors at age 16, indicating moderation (β = −.126, SE = 1.214, p < .01, 95% CI [−.204, −.049]). The moderation was probed using the simple slopes technique (See Figure 10). Results showed that high neighborhood collective efficacy buffered the association between bereavement and externalizing symptomology, such that there was no difference in externalizing symptomology between the bereaved and non-bereaved group in the context of high neighborhood collective efficacy. Alternatively, low neighborhood collective efficacy exacerbated the effect of bereavement on level of externalizing symptoms.
Discussion
The present study utilized an ecological/transactional framework (Cicchetti & Valentino, 2006) to investigate the role of multilevel protective factors in the association between preadolescent bereavement and adolescent psychopathology in maltreated youth. The results of the present study support some of our hypotheses. First, the present study revealed that, compared to non-bereaved maltreated youth, maltreated youth who experienced significant loss were at an increased risk for the development of externalizing behaviors at age 16. In contrast to our hypothesis, there was not a significant association between bereavement and internalizing symptomology at age 16. In addition, path analysis models provided partial support for our second hypothesis, revealing that future orientation for family (age 14), parental monitoring (age 16), and neighborhood collective efficacy (age 16) each significantly attenuated the pathway between bereavement and externalizing problems. That is, a higher degree of these protective factors were associated with lower levels of externalizing symptomology following the experience of close loss. Contrary to our hypothesis, bereaved youth who reported higher levels of individual future orientation (age 14) exhibited more severe externalizing symptoms. Lastly, despite our expectations, the presence of supportive adult figures and parent-child relationships did not significantly moderate the link between close loss and problem behaviors.
The findings of the current study suggest that maltreated youth are at significant risk for the development of externalizing psychopathology when faced with bereavement. The present findings corroborate previous studies that show bereavement as a risk factor for externalizing problems in adolescence (Draper & Hancock, 2011; McCown & Davies, 1995). Similarly, these results are consistent with the stress sensitization hypothesis (Hammen, Henry, & Daley, 2000), suggesting that the experience of negative life events create a multiplicative vulnerability to the experience of subsequent adverse experiences. Such sensitivity has been illustrated in a previous study by McLaughlin and colleagues (2010), revealing that high levels of childhood adversity represented a diathesis for multiple types of mental disorders in the context of a later stressful event. Although the stress sensitization hypothesis was not specifically tested in the present study, we did find evidence that maltreated youth who also experience bereavement are uniquely at risk for deleterious outcomes.
Contrary to our expectations, we did not find that bereavement intensified the risk for internalizing symptoms. This may have been due to a ceiling effect in which youth with maltreatment experiences were already showing significant elevation in internalizing problems (Mills et al., 2013), masking the effect related to bereavement. Similarly, given that the sample is demographically homogenous, with most of the youth coming from a rural low-SES background, it is possible that variability in internalizing problems was too small to detect significance within-group differences. Lastly, the utilization of parent-reported internalizing symptomology may have resulted in lower estimates of youths’ anxious and depressive behaviors, as is often the case for adolescents experiencing subjective feelings of distress (Long, Forehand, & Wierson, 1992).
The results of this study also illustrate the importance of contextual influences following the experience of early life adversity. These findings support previous literature that advocates for a contextual framework on adaptation following bereavement (Lin et al., 2004; Sandler et al., 2008). Similarly, this study corroborates empirical work on the protective role of future expectations (Oshri et al., 2018), parental monitoring (Oberlander et al., 2011), and neighborhood characteristics (Yonas et al., 2010) in the link between child maltreatment and mental health problems. The consistency of these findings is significant for initiatives seeking ways to foster resilience among youth who endure multiple adversities. Specifically, the above-mentioned contextual factors could be translated into various resources that help maltreated youth cope with the loss of a loved one. For example, prevention programs and clinicians may provide psychoeducational tools to families in order to enhance parental monitoring and youths’ future expectations. Although the present study does not examine both negative and positive outcomes following loss (an implicit focus of the resilience framework; Luthar & Cicchetti, 2000), it provides meaningful information for the avoidance of negative outcomes in the context of adversity, thus adding to the overall literature on resilience among maltreated youth.
One of the unexpected findings in our study was the observation that individual-level future orientation exacerbated the risk for externalizing symptoms. It is possible that grieving youth who set extremely high (and potentially unrealistic) goals can actually be harmed by these expectations later in life. Indeed, extant research suggests that adolescents who set excessively high standards for themselves are at risk for some problematic outcomes, including delinquency (Luthar & Becker, 2002). Further, it has been observed that self-oriented perfectionism (i.e., high achievement expectations) paired with acute life stress can lead to symptoms of psychological distress (e.g., anxiety; O’Connor, Rasmussen, & Hawton, 2010). Therefore, it is plausible that these high individual expectations can worsen youths’ risk for problem behaviors following close loss. However, more research examining the harmful effects of individual level future orientation is needed to further contextualize and replicate these results.
Consistent with the developmental psychopathology perspective (Cicchetti & Rogosch, 2002; Duprey, Oshri, & Caughy, 2017), the current study highlights the importance of considering the developmental timing of protective factors in youth development. Due to the multifarious challenges that arise during the transition into adolescence, youth who experience significant stress during this critical period may exhibit heterogeneous trajectories of recovery (e.g., adaptive versus maladaptive), depending upon their ability to utilize developmental assets and resources to achieve stage-salient tasks. Accordingly, the present study found that future orientation (family and individual) significantly moderated the link between bereavement and externalizing problems at age 14, but not 16. These results could be attributed to the natural fluctuation in ones’ hopes and expectations for the future, as is documented in a recent study uncovering multiple trajectories of future orientation among maltreated youth (Oshri et al., 2018). Further, it is possible that future orientation was especially salient in early adolescence due to its pertinence to developmental tasks emerging at or near this time point (e.g., planning for future). In addition, the present study also observed that parental monitoring and neighborhood collective efficacy were protective at age 16, but not 14. We initially expected that parental monitoring would be more salient during early adolescence, based on previous research showing decreases in monitoring levels across youth development (Pettit, Keiley, Laird, Bates, & Dodge, 2007). However, it is conceivable that both parental monitoring and neighborhood characteristics may reveal themselves more advantageous in later adolescence, when delinquency often peaks (e.g., age 16; Agnew, 2003).
Developmental timing may also serve to explain some of the nonsignificant findings of our study, namely, the lack of protective effects of supportive adult figures and parent-child relationships. Because the achievement of autonomy is a primary developmental task in the transition into adolescence (Cicchetti & Banny, 2014), it is likely that in the face of significant stress (e.g., bereavement), youth entering adolescence may feel less comfortable seeking support from adult figures, attempting to overcome the burden of this major life disruption on their own. Further, whereas parental support reveals itself as a prominent protective resource following the death of a loved one (Balk, Zaengle, & Corr, 2011; Sandler et al., 2003), youth with a history of maltreatment may not have the emotional capacity to perceive their once-abusive parent as a supportive resource in the context of later adversity. In consideration of these findings, we echo prior calls for more longitudinal research focusing on the developmental timing of protective factors (Zimmerman et al., 2013). Such detailed investigations can help inform targeted prevention and interventions for at-risk youth.
Limitations and Future Directions
The contributions of the current study should be taken in the context of its limitations. First, because the LONGSCAN sample is comprised of youth who present risk for exposure or experienced maltreatment, as well as socioeconomic risk, the findings may not generalize well to samples from other demographic backgrounds. Secondly, the present study utilized substantiated Child Protective Service (CPS) reports of child maltreatment to comprise the observed sample. Because research suggests that many cases of child abuse and neglect are underreported (Flaherty et al., 2008), the subsample of maltreated youth observed in this study may be less representative than that actual number of participants who were exposed to child maltreatment. In addition, the present study utilized a subsample of youth who had been exposed to any form of maltreatment (e.g., physical abuse, emotional abuse, sexual abuse, and/or neglect). Because there is evidence to suggest that different forms of child maltreatment (e.g., abuse versus neglect) result in unique consequences (Lambert, King, Monahan, & McLaughlin, 2017; Petrenko, Friend, Garrido, Taussig, & Culhane, 2012), future studies could benefit from examining the impact of close loss amongst youth who endured specific forms of maltreatment.
The present study also contained several limitations concerning methodology. For example, the dataset obtained for the study administered measurements in waves of two years. Future studies examining bereavement might benefit from investigating hypotheses in shorter waves, such as one year. In addition, the utilization of caregiver reports (CBCL) for adolescent internalizing and externalizing symptomology is a potential limitation, seeing as previous reviews have noted discrepant results between parent-reported and youth-reported assessments of problem behaviors (De Los Reyes & Kazdin, 2005). However, the use of CBCL raw scores, rather than truncated T scores, can help reduce this discrepancy by employing the full range of variation in data analysis (Thurber & Sheehan, 2012). Further, internal consistencies reported for the Future Events Questionnaire were fairly low. This may have been due to the negative wording of the items on the ‘family’ and ‘employment’ subscales, which could have led to response bias (e.g., social desirability bias), wherein youth answered more agreeably and consistently with the positive items versus the negative. It is also possible that the items on these subscales appeared less clear to the child (e.g., “how likely is it that you will get married within two years after high school?”; “how likely is it that you will have to go on welfare at some point?”). Lastly, the present study measured bereavement using a single item that indicated whether or not the child had experienced close loss in the past year (at age 12). Future research may benefit from a) observing the cumulative impact of close loss and b) specifying the type of loss that was experienced by the child (e.g., traumatic versus normative loss).
Conclusions and Implications
The results of this study augment literature examining the predictive relationship between bereavement and internalizing and externalizing psychopathology, by investigating the impact of bereavement in a sample of maltreated youth. Specifically, the present study illustrates how the experience of an additional negative life event (i.e., the death of a loved one) can impact youth who have already endured previous traumatic family events, namely child abuse and neglect. Despite the additional risk for maltreated youth posed by close loss, several protective factors buffered the link between bereavement and externalizing behaviors. These findings have important implications for future preventive and clinical interventions for youth who are involved with child protective services and/or who have experiences of child maltreatment. By promoting the importance of multi-level protective factors at specific stages of adolescent development, mental health problems can be prevented among at-risk youth. Specifically, interventions that work to bolster youths’ future orientation for family, parental monitoring, and that involve neighborhood and community resources, may alleviate the impact of bereavement for maltreated youth.
Figure 2.
Path Analysis Model of the Moderating Effect of Future Orientation (Family) on the Association between Bereavement and Externalizing Problems (N = 800).
Notes. Standardized parameters are shown in figure. In each path, the top numbers are for the model using the age 14 protective factor and the bottom numbers are for the model using the age 16 protective factor. Model fit was good; Age-14 Model: RMSEA = .009, CFI = 1.00, TLI = .997, SRMR = .009; Age-16 Model: RMSEA = .00, CFI = 1.00, TLI = 1.02, SRMR = .007.
*p < .05, **p < .01, ***p < .001
Figure 3.
Path Analysis Model of the Moderating Effect of Parent-Child Relationship on the Association between Bereavement and Externalizing Problems (N = 800).
Notes. Standardized parameters are shown in figure. In each path, the top numbers are for the model using the age 14 protective factor and the bottom numbers are for the model using the age 16 protective factor. Model fit was good; Age-14 Model: RMSEA = .00, CFI = 1.00, TLI = 1.04, SRMR = .004; Age-16 Model: RMSEA = .00, CFI = 1.00, TLI = 1.02 SRMR = .007.
*p < .05, **p < .01, ***p < .001
Figure 4.
Path Analysis Model of the Moderating Effect of Parental Monitoring on the Association between Bereavement and Externalizing Problems (N = 800).
Notes. Standardized parameters are shown in figure. In each path, the top numbers are for the model using the age 14 protective factor and the bottom numbers are for the model using the age 16 protective factor. Model fit was good; Age-14 Model: RMSEA = .071, CFI = .970, TLI = .807, SRMR = .023; Age-16 Model: RMSEA = .051, CFI = .994, TLI = .925, SRMR = .014.
*p < .05, **p < .01, ***p < .001
Figure 5.
Path Analysis Model of the Moderating Effect of Supportive Adult Figures on the Association between Bereavement and Externalizing Problems (N = 800).
Notes. Standardized parameters are shown in figure. In each path, the top numbers are for the model using the age 14 protective factor and the bottom numbers are for the model using the age 16 protective factor. Model fit was good; Age-14 Model: RMSEA = .00, CFI = 1.00, TLI = 1.04, SRMR = .001; Age-16 Model: RMSEA = .00, CFI = 1.00, TLI = 1.03, SRMR = .004.
*p < .05, **p < .01, ***p < .001
Acknowledgments:
The data used in this publication were made available by the National Data Archive on Child Abuse and Neglect, Cornell University, Ithaca, NY, and have been used with permission. Data from Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) Assessments 0–12 were originally collected by Desmond K. Runyan, Howard Dubowitz, Diana J. English, Jonathan Kotch, Alan Litrownik, Richard Thompson and Terri Lewis & The LONGSCAN Investigator Group. Funding for the project was provided by the Office on Child Abuse and Neglect (OCAN), Children’s Bureau, Administration for Children and Families, Dept. of Health and Human Services (The National Center on Child Abuse and Neglect (NCCAN), under the Office of Human Services funded this consortium of studies during the early years of data collection from 04/01/1991 until NCCAN became part of OCAN in 1998.) The collector of the original data, the funder, NDACAN, Cornell University and their agents or employees bear no responsibility for the analyses or interpretations presented here.
Funding: This work was partially supported by a National Institute of Drug Abuse grant awarded to Dr. Oshri (1K01DA045219–01) and the University of Georgia’s Center for Undergraduate Research Opportunities (CURO)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM (1991). Integrative Guide to the 1991 CBCL/4–18 YSR, and TRF Profiles. University of Vermont, Department of Psychology Pediatrics Burlington, VT: University of Vermont, Department of Psychiatry; Retrieved from http://www.aseba.org/ [Google Scholar]
- Afifi TO, & MacMillan HL (2011). Resilience following Child Maltreatment: A Review of Protective Factors. The Canadian Journal of Psychiatry, 56(5), 266–272. 10.1177/070674371105600505 [DOI] [PubMed] [Google Scholar]
- Agnew R (2003). An integrated theory of the adolescent peak in offending. Youth & Society, 34(3), 263–299. 10.1177/0044118X02250094 [DOI] [Google Scholar]
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions Thousand Oaks, CA, US: Sage Publications, Inc; Retrieved from http://proxy-remote.galib.uga.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=1991-97932-000&site=eds-live [Google Scholar]
- Balk DE, & Corr C. a. (2001). 2I - Bereavement during adolescence - A review of research. In Handbook of bereavement research - Consequences, coping, and care [Google Scholar]
- Balk David E, Zaengle D, & Corr CA (2011). Strengthening grief support for adolescents coping with a peer’s death. School Psychology International, 32(2), 144–162. 10.1177/0143034311400826 [DOI] [Google Scholar]
- Begle AM, Hanson RF, Danielson CK, McCart MR, Ruggiero KJ, Amstadter AB, … Kilpatrick DG (2011). Longitudinal pathways of victimization, substance use, and delinquency: Findings from the National Survey of Adolescents. Addictive Behaviors 10.1016/j.addbeh.2010.12.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolger KE, & Patterson CJ (2003). Sequelae of child maltreatment: Vulnerability and resilience. In Luthar S (Ed.), Resilience and Vulnerability: Adaptation in the Context of Childhood Adversities (pp. 156–181). Cambridge: Cambridge University Press; 10.1017/CBO9780511615788.009 [DOI] [Google Scholar]
- Bonanno GA (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist, 59(1), 20. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, & Kaltman S (2001). The varieties of grief experience. Clinical Psychology Review, 21(5), 705–734. [DOI] [PubMed] [Google Scholar]
- Brent DA, Melhem N, Donohoe MB, & Walker M (2009). The incidence and course of depression in bereaved youth 21 months after the loss of a parent to suicide, accident, or sudden natural death. American Journal of Psychiatry 10.1176/appi.ajp.2009.08081244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Melhem NM, Masten AS, Porta G, & Payne MW (2012). Longitudinal Effects of Parental Bereavement on Adolescent Developmental Competence. Journal of Clinical Child and Adolescent Psychology, 41(6), 778–791. 10.1080/15374416.2012.717871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabrera NJ, Cook GA, McFadden KE, & Bradley RH (2011). Father residence and father-child relationship quality: Peer relationships and externalizing behavioral problems. Family Science 10.1080/19424620.2011.639143 [DOI] [Google Scholar]
- Chen P, & Vazsonyi AT (2013). Future Orientation, School Contexts, and Problem Behaviors: A Multilevel Study. Journal of Youth and Adolescence 10.1007/s10964-012-9785-4 [DOI] [PubMed] [Google Scholar]
- Cicchetti D (2013). Annual Research Review: Resilient functioning in maltreated children – past, present, and future perspectives. Journal of Child Psychology and Psychiatry, 54(4), 402–422. 10.1111/j.1469-7610.2012.02608.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, & Banny A (2014). A developmental psychopathology perspective on child maltreatment. Handbook of Developmental Psychopathology: Third Edition. 10.1007/978-1-4614-9608-3_37 [DOI] [Google Scholar]
- Cicchetti D, & Rogosch FA (1996). Equifinality and multifinality in developmental psychopathology. Development and Psychopathology 10.1017/S0954579400007318 [DOI] [Google Scholar]
- Cicchetti D, & Rogosch FA (2002). A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology Cicchetti, Dante: Shirley Cox Kearns Professor of Psychology, Psychiatry, and Pediatrics, University of Rochester, and Director, Mt. Hope Family Center, 187 Edinburgh Street, Rochester, NY, US, 14608: American Psychological Association 10.1037/0022-006X.70.1.6 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Valentino K (2006). An Ecological-Transactional Perspective on Child Maltreatment: Failure of the Average Expectable Environment and Its Influence on Child Development. In Developmental Psychopathology: Second Edition. 10.1002/9780470939406.ch4 [DOI] [Google Scholar]
- Coddington RD (1972). Coddington Life Events Scales North Tonawanda, NY: MHS Inc; Retrieved from http://www.aseba.org/ [Google Scholar]
- Coulton CJ, Korbin JE, & Su M (1996). Measuring Neighborhood Context for Young Children in an Urban Area. American Journal of Community Psychology, 24(1), 5–32. 10.1007/BF02511881 [DOI] [Google Scholar]
- Davies PT, Manning LG, & Cicchetti D (2013). Tracing the Cascade of Children’s Insecurity in the Interparental Relationship: The Role of Stage-Salient Tasks. Child Development 10.1111/j.1467-8624.2012.01844.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day RD, & Padilla-Walker LM (2009). Mother and Father Connectedness and Involvement During Early Adolescence. Journal of Family Psychology 10.1037/a0016438 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, & Kazdin AE (2005). Informant Discrepancies in the Assessment of Childhood Psychopathology: A Critical Review, Theoretical Framework, and Recommendations for Further Study. Psychological Bulletin, 131(4), 483–509. 10.1037/0033-2909.131.4.483 [DOI] [PubMed] [Google Scholar]
- Diemer MA, Mistry RS, Wadsworth ME, López I, & Reimers F (2013). Best practices in conceptualizing and measuring social class in psychological research. Analyses of Social Issues and Public Policy, 13(1), 77–113. 10.1111/asap.12001 [DOI] [Google Scholar]
- Dishion TJ, & McMahon RJ (1998). Parental monitoring and the prevention of child and adolescent problem behavior: A conceptual and empirical formulation. Clinical Child and Family Psychology Review 10.1023/A:1021800432380 [DOI] [PubMed] [Google Scholar]
- Draper A, & Hancock M (2011). Childhood parental bereavement: The risk of vulnerability to delinquency and factors that compromise resilience. Mortality 10.1080/13576275.2011.613266 [DOI] [Google Scholar]
- Duprey EB, Oshri A, & Caughy MO (2017). Childhood Neglect, Internalizing Symptoms and Adolescent Substance Use: Does the Neighborhood Context Matter? Journal of Youth and Adolescence, 46(7), 1582–1597. 10.1007/s10964-017-0672-x [DOI] [PubMed] [Google Scholar]
- Ebbert AM, Infurna FJ, & Luthar SS (2018). Mapping developmental changes in perceived parent–adolescent relationship quality throughout middle school and high school. Development and Psychopathology, 1–16. [DOI] [PubMed] [Google Scholar]
- Enders CK, & Bandalos DL (2001). The Relative Performance of Full Information Maximum Likelihood Estimation for Missing Data in Structural Equation Models. Structural Equation Modeling: A Multidisciplinary Journal, 8(3), 430–457. 10.1207/S15328007SEM0803_5 [DOI] [Google Scholar]
- English DJ, Upadhyaya MP, Litrownik AJ, Marshall JM, Runyan DK, Graham JC, & Dubowitz H (2005). Maltreatment’s wake: The relationship of maltreatment dimensions to child outcomes. Child Abuse and Neglect, 29(5), 597–619. 10.1016/j.chiabu.2004.12.008 [DOI] [PubMed] [Google Scholar]
- Fagan AA, Wright EM, & Pinchevsky GM (2014). The Protective Effects of Neighborhood Collective Efficacy on Adolescent Substance Use and Violence Following Exposure to Violence. Journal of Youth and Adolescence, 43(9), 1498–1512. 10.1007/s10964-013-0049-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaherty EG, Sege RD, Griffith J, Price LL, Wasserman R, Slora E, … Binns HJ (2008). From Suspicion of Physical Child Abuse to Reporting: Primary Care Clinician Decision-Making. Pediatrics, 122(3), 611–619. Retrieved from http://pediatrics.aappublications.org/content/122/3/611.abstract [DOI] [PubMed] [Google Scholar]
- Gillespie BM, Chaboyer W, & Wallis M (2007). Development of a theoretically derived model of resilience through concept analysis. Contemporary Nurse 10.5172/conu.2007.25.1-2.124 [DOI] [PubMed] [Google Scholar]
- Haine RA, Ayers TS, Sandler IN, Wolchik SA, & Weyer JL (2003). Locus of control and self-esteem as stress-moderators or stress-mediators in parentally bereaved children. Death Studies, 27(7), 619–640. [DOI] [PubMed] [Google Scholar]
- Haine RA, Wolchik SA, Sandler IN, Millsap RE, & Ayers TS (2006). Positive parenting as a protective resource for parentally bereaved children. Death Studies 10.1080/07481180500348639 [DOI] [PubMed] [Google Scholar]
- Hamilton CE, Falshaw L, & Browne KD (2002). The link between recurrent maltreatment and offending behaviour. International Journal of Offender Therapy and Comparative Criminology 10.1177/0306624X02461006 [DOI] [PubMed] [Google Scholar]
- Hammen C, Henry R, & Daley SE (2000). Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology 10.1037/0022-006X.68.5.782 [DOI] [PubMed] [Google Scholar]
- Hamza CA, & Willoughby T (2011). Perceived Parental Monitoring, Adolescent Disclosure, and Adolescent Depressive Symptoms: A Longitudinal Examination. Journal of Youth and Adolescence, 40(7), 902–915. 10.1007/s10964-010-9604-8 [DOI] [PubMed] [Google Scholar]
- Harrison L, & Harrington R (2001). Adolescents’ bereavement experiences. Prevalence, association with depressive symptoms, and use of services. Journal of Adolescence 10.1006/jado.2001.0379 [DOI] [PubMed] [Google Scholar]
- Mash H. B. Herberman, Fullerton CS, & Ursano RJ (2013). Complicated grief and bereavement in young adults following close friend and sibling loss. Depression and Anxiety 10.1002/da.22068 [DOI] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hussey JM, Chang JJ, & Kotch JB (2006). Child Maltreatment in the United States: Prevalence, Risk Factors, and Adolescent Health Consequences. PEDIATRICS 10.1542/peds.2005-2452 [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Caspi A, Moffitt TE, Polo-Tomás M, & Taylor A (2007). Individual, family, and neighborhood factors distinguish resilient from non-resilient maltreated children: A cumulative stressors model. Child Abuse & Neglect, 31(3), 231–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SRL, Blum RW, & Cheng TL (2014). Future orientation: A construct with implications for adolescent health and wellbeing. International Journal of Adolescent Medicine and Health, 26(4), 459–468. 10.1515/ijamh-2013-0333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim BKE, Oesterle S, Catalano RF, & Hawkins JD (2015). Change in protective factors across adolescent development. Journal of Applied Developmental Psychology, 40, 26–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2006). Longitudinal Trajectories of Self-System Processes and Depressive Symptoms Among Maltreated and Nonmaltreated Children. Child Development, 77(3), 624–639. 10.1111/j.1467-8624.2006.00894.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry and Allied Disciplines, 51(6), 706–716. 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight ED, Smith JB, Martin L, Lewis T, & LONGSCAN Investigators. (1998). Measures for Assessment of Functioning and Outcomes in Longitudinal Research on Child Abuse Volume 3: Early Adolescence (Ages 12–14) Accessible at the LONGSCAN web site (http://www.iprc.unc.edu/longscan/). [Google Scholar]
- Knight ED, Smith JS, Martin LM, Lewis T, & the LONGSCAN Investigators. (2008). Measures for Assessment of Functioning and Outcomes in Longitudinal Research on Child Abuse-Volume 3: Early Adolescence (Ages 12–14) Retrieved from http://www.unc.edu/depts/sph/longscan/ [Google Scholar]
- Kwok OM, Haine RA, Sandler IN, Ayers TS, Wolchik SA, & Tein JY (2005). Positive parenting as a mediator of the relations between parental psychological distress and mental health problems of parentally bereaved children. Journal of Clinical Child and Adolescent Psychology 10.1207/s15374424jccp3402_5 [DOI] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, D’Onofrio BM, Rodgers JL, & Waldman ID (2008). Is parental knowledge of their adolescent offspring’s whereabouts and peer associations spuriously associated with offspring delinquency? Journal of Abnormal Child Psychology 10.1007/s10802-008-9214-z [DOI] [PubMed] [Google Scholar]
- Lambert HK, King KM, Monahan KC, & McLaughlin KA (2017). Differential associations of threat and deprivation with emotion regulation and cognitive control in adolescence. Development and Psychopathology, 29(03), 929–940. 10.1017/S0954579416000584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansford JE, Dodge KA, Pettit GS, Bates JE, Crozier J, & Kaplow J (2002). A 12-year prospective study of the long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence. Archives of Pediatrics and Adolescent Medicine 10.1001/archpedi.156.8.824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerner RM, Agans JP, Arbeit MR, Chase PA, Weiner MB, Schmid KL, & Warren AEA (2013). Resilience and positive youth development: A relational developmental systems model. In Handbook of Resilience in Children: Second Edition. 10.1007/978-1-4614-3661-4_17 [DOI] [Google Scholar]
- Li M, D’Arcy C, & Meng X (2016). Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: systematic review, meta-analysis, and proportional attributable fractions. Psychological Medicine, 46(4), 717–730. 10.1017/S0033291715002743 [DOI] [PubMed] [Google Scholar]
- Lin KK, Sandler IN, Ayers TS, Wolchik SA, & Luecken LJ (2004). Resilience in parentally bereaved children and adolescents seeking preventive services. Journal of Clinical Child and Adolescent Psychology 10.1207/s15374424jccp3304_3 [DOI] [PubMed] [Google Scholar]
- Long P, Forehand R, & Wierson M (1992). Internalizing Problems of Adolescents: The Role of the Informant in Identifying Family and Individual Difficulties. Journal of Child & Family Studies, 1(4), 329–339. Retrieved from http://10.0.3.239/BF01321289 [Google Scholar]
- Lundberg T, Forinder U, Olsson M, Fürst CJ, Årestedt K, & Alvariza A (2018). Bereavement stressors and psychosocial well-being of young adults following the loss of a parent – A cross-sectional survey. European Journal of Oncology Nursing, 35, 33–38. [DOI] [PubMed] [Google Scholar]
- Luthar SS, & Becker BE (2002). Privileged but Pressured? A Study of Affluent Youth. Child Development, 73(5), 1593–1610. 10.1111/1467-8624.00492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, & Cicchetti D (2000). The construct of resilience: Implications for interventions and social policies. Development and Psychopathology 10.1017/S0954579400004156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J, & Grogan-Kaylor A (2017). Longitudinal associations of neighborhood collective efficacy and maternal corporal punishment with behavior problems in early childhood. Developmental Psychology Ma, Julie: Social Work Department, School of Education and Human Services, University of Michigan–Flint, 303 East Kearsley Street, Flint, MI, US, 48502, majul@umich.edu: American Psychological Association 10.1037/dev0000308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS (2014). Ordinary magic: Resilience in development. Ordinary magic: Resilience in development New York, NY, US: Guilford Press. [Google Scholar]
- Masten AS (2018). Resilience Theory and Research on Children and Families: Past, Present, and Promise. Journal of Family Theory & Review, 10(1), 12–31. 10.1111/jftr.12255 [DOI] [Google Scholar]
- Masten AS, Best KM, & Garmezy N (1990). Resilience and development: Contributions from the study of children who overcome adversity. Development and Psychopathology 10.1017/S0954579400005812 [DOI] [Google Scholar]
- McCown DE, & Davies B (1995). Patterns of grief in young children following the death of a sibling. Death Studies, 19(1), 41–53. 10.1080/07481189508252712 [DOI] [Google Scholar]
- McElhaney KB, Allen JP, Stephenson JC, & Hare AL (2009). Attachment and Autonomy During Adolescence. In Lerner RM & Steinberg L (Eds.), Handbook of Adolescent Psychology 10.1002/9780470479193.adlpsy001012 [DOI] [Google Scholar]
- McLaughlin KA, & Hatzenbuehler ML (2009). Mechanisms Linking Stressful Life Events and Mental Health Problems in a Prospective, Community-Based Sample of Adolescents. Journal of Adolescent Health, 44(2), 153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills R, Scott J, Alati R, O’Callaghan M, Najman JM, & Strathearn L (2013). Child maltreatment and adolescent mental health problems in a large birth cohort. Child Abuse & Neglectfile:///Users/Jerisasser/Desktop/Screen Shot 2019–06-25 at 5.37.55 PM.Png, 37(5), 292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller J (2015). A word on standardization in longitudinal studies: don’t. Frontiers in Psychology, 6, 1389 10.3389/fpsyg.2015.01389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2010). Mplus User’s Guide: Sixth Edition. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- O’Connor RC, Rasmussen S, & Hawton K (2010). Predicting depression, anxiety and self-harm in adolescents: The role of perfectionism and acute life stress. Behaviour Research and Therapy, 48(1), 52–59. [DOI] [PubMed] [Google Scholar]
- Oberlander SE, Wang Y, Thompson R, Lewis T, Proctor LJ, Isbell P, … Black MM (2011). Childhood maltreatment, emotional distress, and early adolescent sexual intercourse: Multi-informant perspectives on parental monitoring. Journal of Family Psychology Black, Maureen M.: Department of Pediatrics, University of Maryland School of Medicine, 737 West Lombard Street, Room 161, Baltimore, MD, US, 21201, mblack@peds.umaryland.edu: American Psychological Association 10.1037/a0025423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohmer ML (2007). Citizen Participation in Neighborhood Organizations and Its Relationship to Volunteers’ Self- and Collective Efficacy and Sense of Community. Social Work Research, 31(2), 109–120. Retrieved from 10.1093/swr/31.2.109 [DOI] [Google Scholar]
- Oshri A, Duprey EB, Kogan SM, Carlson MW, & Liu S (2018). Growth patterns of future orientation among maltreated youth: A prospective examination of the emergence of resilience. Developmental Psychology 10.1037/dev0000528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A, Rogosch FA, & Cicchetti D (2013). Child Maltreatment and Mediating Influences of Childhood Personality Types on the Development of Adolescent Psychopathology. Journal of Clinical Child and Adolescent Psychology 10.1080/15374416.2012.715366 [DOI] [PubMed] [Google Scholar]
- Oshri A, Topple TA, & Carlson MW (2017). Positive Youth Development and Resilience: Growth Patterns of Social Skills Among Youth Investigated for Maltreatment. Child Development, 88(4), 1087–1099. 10.1111/cdev.12865 [DOI] [PubMed] [Google Scholar]
- Patterson GR, & Stouthamer-Loeber M (1984). The Correlation of Family Management Practices and Delinquency. Child Development, 55(4), 1299 10.2307/1129999 [DOI] [PubMed] [Google Scholar]
- Petrenko CLM, Friend A, Garrido EF, Taussig HN, & Culhane SE (2012). Does subtype matter? Assessing the effects of maltreatment on functioning in preadolescent youth in out-of-home care. Child Abuse and Neglect, 36(9), 633–644. 10.1016/j.chiabu.2012.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettit GS, Keiley MK, Laird RD, Bates JE, & Dodge KA (2007). Predicting the developmental course of mother-reported monitoring across childhood and adolescence from early proactive parenting, child temperament, and parents’ worries. Journal of Family Psychology : JFP : Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 21(2), 206–217. 10.1037/0893-3200.21.2.206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu Y, Fuligni AJ, Galvan A, & Telzer EH (2015). Buffering effect of positive parent-child relationships on adolescent risk taking: A longitudinal neuroimaging investigation. Developmental Cognitive Neuroscience 10.1016/j.dcn.2015.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, … Udry R (1997). Protecting adolescents from harm: Findings from the national longitudinal study on adolescent health. JAMA, 278(10), 823–832. Retrieved from 10.1001/jama.1997.03550100049038 [DOI] [PubMed] [Google Scholar]
- Resnick MD, Harris LJ, & Blum RW (1993). The impact of caring and connectedness on adolescent health and well-being. Journal of Paediatrics and Child Health, 29(s1), S3–S9. 10.1111/j.1440-1754.1993.tb02257.x [DOI] [PubMed] [Google Scholar]
- Robbins RN, & Bryan A (2004). Relationships between future orientation, impulsive sensation seeking, and risk behavior among adjudicated adolescents. Journal of Adolescent Research 10.1177/0743558403258860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson AA, Baird-Thomas C, & Stein JA (2008). Child victimization and parental monitoring as mediators of youth problem behaviors. Criminal Justice and Behavior, 35(6), 755–771. 10.1177/0093854808316096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runyan D, Dubowitz H, English DJ, Kotch JB, Litrownik A, Thompson R, & Group TLI (2014). Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) Assessments 0–18 [Dataset] [Google Scholar]
- Sagrestano LM, Paikoff RL, Holmbeck GN, & Fendrich M (2003). A longitudinal examination of familial risk factors for depression among inner-city African American adolescents. Journal of Family Psychology Sagrestano, Lynda M.: Southern Illinois U, Dept of Psychology, Carbondale, IL, US, 62901–6502, sagresta@siu.edu: American Psychological Association 10.1037/0893-3200.17.1.108 [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, & Earls F (1997). Neighborhoods and violent crime: A multilevel study of collective efficacy. Science, 277(5328), 918–924. Retrieved from http://science.sciencemag.org/content/277/5328/918.abstract [DOI] [PubMed] [Google Scholar]
- Sandler IN, Ayers TS, Wolchik SA, Tein J-Y, Kwok O-M, Haine RA, … Griffin WA (2003). The Family Bereavement Program: Efficacy evaluation of a theory-based prevention program for parentally bereaved children and adolescents. Journal of Consulting and Clinical Psychology. American Psychological Association 10.1037/0022-006X.71.3.587 [DOI] [PubMed] [Google Scholar]
- Sandler IN, Wolchik SA, & Ayers TS (2008). Resilience rather than recovery: A contextual framework on adaptation following bereavement. Death Studies 10.1080/07481180701741343 [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods Schafer, Joseph L.: Pennsylvania State U, The Methodology Ctr, Henderson S-159, University Park, PA, US, 16802, jls@stat.psu.edu: American Psychological Association 10.1037/1082-989X.7.2.147 [DOI] [PubMed] [Google Scholar]
- Schultz LE (2007). The Influence of Maternal Loss on Young Women’s Experience of Identity Development in Emerging Adulthood. Death Studies, 31(1), 17–43. 10.1080/07481180600925401 [DOI] [PubMed] [Google Scholar]
- Stattin H, & Kerr M (2000). Parental monitoring: A reinterpretation. Child Development United Kingdom: Blackwell Publishing; 10.1111/1467-8624.00210 [DOI] [PubMed] [Google Scholar]
- Stroebe MS, Hansson RO, Stroebe W, & Schut H (2001). Handbook of bereavement research consequences, coping, and care. Journal of Social Personal Relationships 10.1037/10436-000 [DOI] [Google Scholar]
- Thurber S, & Sheehan WP (2012). Note on truncated T scores in discrepancy studies with the Child Behavior Checklist and Youth Self Report. Archives of Assessment Psychology, 2(1), 73–80. [Google Scholar]
- Toth SL, & Cicchetti D (1996). Patterns of relatedness, depressive symptomatology, and perceived competence in maltreated children. Journal of Consulting and Clinical Psychology US: American Psychological Association. 10.1037/0022-006X.64.1.32 [DOI] [PubMed] [Google Scholar]
- Werner EE (2005). What Can We Learn about Resilience from Large-Scale Longitudinal Studies? BT - Handbook of Resilience in Children In Goldstein S & Brooks RB (Eds.) (pp. 91–105). Boston, MA: Springer US; 10.1007/0-306-48572-9_7 [DOI] [Google Scholar]
- Wilkinson A, & Lantos H (2018). How school, family, and community protective factors can help youth who have experienced maltreatment. Child Trends Bethesda, MD: Child Trends; Retrieved from https://www.childtrends.org/publications/school-family-community-protective-factors-can-help-youth-experienced-maltreatment [Google Scholar]
- Yonas MA, Lewis T, Hussey JM, Thompson R, Newton R, English D, & Dubowitz H (2010). Perceptions of neighborhood collective efficacy moderate the impact of maltreatment on aggression. Child Maltreatment 10.1177/1077559509349445 [DOI] [PubMed] [Google Scholar]
- Zimmerman MA, Bingenheimer JB, & Notaro PC (2002). Natural Mentors and Adolescent Resiliency: A Study with Urban Youth. American Journal of Community Psychology 10.1023/A:1014632911622 [DOI] [PubMed] [Google Scholar]
- Zimmerman MA, Stoddard SA, Eisman AB, Caldwell CH, Aiyer SM, & Miller A (2013). Adolescent Resilience: Promotive Factors That Inform Prevention. Child Development Perspectives, 7(4), 215–220. 10.1111/cdep.12042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisook S, & Shear K (2009). Grief and bereavement: What psychiatrists need to know. World Psychiatry 10.1002/j.2051-5545.2009.tb00217.x [DOI] [PMC free article] [PubMed] [Google Scholar]