Abstract
Objectives
To explore the feasibility, fidelity, safety, and preliminary outcomes of a physical therapist-administered physical activity (PA) intervention after total knee replacement (TKR).
Methods
People with a unilateral TKR in outpatient PT were randomized to a control or intervention group. Both groups received standard PT for TKR. The intervention included providing a Fitbit Zip, step goals, and one phone call a month for six months after discharge from PT. Feasibility was measured by rates of recruitment and retention, safety by the frequency of adverse events, and fidelity of the intervention by adherence from the physical therapist creating weekly steps/day goal and the participant monitoring their steps/day. An ActigraphGT3X measured PA quantified as steps/day and minutes/week in moderate to vigorous physical activity (MVPA). Our preliminary outcome was the difference in PA at six months (6m) after discharge from PT between groups.
Results
Of the 43 people enrolled (mean(SD) age = 67.0 (7.0), BMI = 31.5 (5.9), 53.4% women), the recruitment and retention rates were 64% and 83.7%, respectively, no study-related adverse events occurred, and adherence to the intervention ranged from 45–60%. Those in the intervention group accumulated (mean [95%CI]) 1798 [240, 3355] more steps/day and spent 73.4 [−14.1, 160.9] more minutes/week in MVPA at 6m than the control group.
Conclusion
A physical therapist-administered PA intervention is feasible and safe, demonstrates treatment fidelity, and may increase PA after TKR. Future research is needed to establish the effectiveness of the intervention.
Knee osteoarthritis (OA) is a leading cause of pain and disability in older adults.[1] Total knee replacement (TKR) is the definitive treatment for knee OA which resolves most knee pain and limitations in physical function.[1] However, physical activity (PA), defined as any body movement that results in energy expenditure above a resting level,[2] remains mostly unchanged after TKR,[3, 4] leaving those after surgery at risk of inactivity-related health problems, such as weight gain[5, 6], cardiovascular disease[7], diabetes[8, 9], and premature death.[10, 11] Substantial growth is expected with the number of TKR surgeries, which have doubled over the past 15 years in the United States[12], and more than 3.5 million TKRs are expected to be performed every year by 2030.[13] Thus, there is a critical need to improve PA in individuals after TKR.
Outpatient physical therapy (PT) is an optimal setting to deliver a PA intervention. Physical therapists are experts in prescribing and tailoring therapeutic exercise programs to promote PA. After TKR, physical therapists often treat patients in the outpatient setting two to three times a week for six to eight weeks as part of standard post-operative care, which aligns with the recommended frequency of one-on-one visits needed to promote behavioral change to increase PA.[14, 15] Furthermore, over 90% of patients in PT agree that physical therapists should discuss PA as part of care.[16]
Recording steps/day with an activity tracker, e.g., a Fitbit Zip (Fitbit Inc., San Francisco, California), paired with a healthcare professional providing individuals with weekly steps/day goals is known to increase PA.[17–19] This type of intervention increases PA through a behavioral change technique that includes feedback from the activity tracker, and self-monitoring of the goal.[20, 21] At present, it is not known if a physical therapist-administered PA intervention is feasible and safe, and demonstrates fidelity. As well, it is not known if such an intervention can increase PA in people after TKR.
The purpose of this study was to explore the feasibility, safety, fidelity, and preliminary outcomes of a physical therapist-administered PA intervention after TKR.
Patients and Methods
Design
This was a single-center randomized controlled pilot study. This study was registered at ClinicalTrials.gov (trial number #NCT02724137), approved by the University of Delaware Institutional Review Board, and informed consent was obtained from all study participants.
Study participants
We recruited people receiving outpatient PT for a unilateral TKR at the Delaware Physical Therapy Clinic at the University of Delaware (UDPT) in Newark, Delaware. Potential study participants were informed about our study during the initial PT appointment at UDPT from their treating physical therapist. If the person was interested in participating in the study, a research assistant screened them for eligibility at their next PT appointment. Patients were eligible to participate if they were; 1) over 45 years of age, and 2) self-reported “yes” when asked if they were interested in increasing PA. Participants were excluded if they; 1) had any additional comorbidities that would prevent them from participating in a PA intervention, e.g., unstable angina, 2) had another lower extremity surgery in the previous six months, and 3) had another lower extremity surgery planned within six months after enrolling in the study.
Study Procedures
Once consented and enrolled, participants were randomized into the control or intervention group. A research assistant randomized each participant using a manila envelope with note cards labeled “A” for intervention and “B” for control. The research assistant analyzing the PA data was masked to group assignment.
Control Group
Participants in the control group received standard outpatient PT provided by a licensed physical therapist using the Delaware Physical Therapy Clinic – Rehab Practice Guidelines for Unilateral TKR (supplementary material). Standard PT also included a printed home exercise program with an exercise log that was updated weekly by the physical therapist (supplementary material). Participants in the control group also received a monthly phone call after discharge from PT for six months to discuss their overall health and serve as a reminder for the PA data collection at 6m and 12m. These calls also served to match the number of points of contact between the intervention and control group. Weekly steps/day goals and feedback on PA was not provided to control group participants.
Intervention Group
The intervention group received a Fitbit Zip, weekly steps/day goal from a physical therapist, and monthly follow-up phone calls, for six months, by a research assistant to promote PA, in addition to the same standard outpatient PT provided to the control group.
Fitbit Zip (activity tracker): A Fitbit Zip was provided within one week of enrolling in the study. Participants were given written and face-to-face instructions on how to set up, use, and sync the Fitbit Zip to their smartphone, tablet, or home computer using the app provided by Fitbit. If the participant did not have a smartphone, tablet, or home computer they were instructed to use the Fitbit Zip as a pedometer. We asked participants to wear the Fitbit Zip around their waist at their right anterior-superior iliac crest, daily, during waking hours and to monitor their steps/day count with the Fitbit Zip and record steps/day count in their home exercise program. Extra batteries and instructions on how to install the batteries were provided as needed. After the 6m follow-up, participants returned their Fitbit Zip to the research team.
Weekly Steps/Day Goal Setting: Participants in the intervention group jointly set weekly steps/day goals with the physical therapist starting at least three weeks after TKR surgery. Several factors were considered to progress the steps/day goal including if weekly steps/day goal was achieved in at least four of the last seven days, the participant’s current health status, the physical therapist’s clinical judgment, and the participant’s personal PA goal. The end goal was to walk at least 6,000 steps/day by discharge. We used this as a goal because this threshold is known to protect against developing functional limitation in people with knee OA.[22] If the participant achieved 6,000 steps/day, they were encouraged to continue to increase their steps/day since health benefits persist with more PA. Weekly steps/day goal were recorded on a standardized goal setting form and a home exercise program log (supplemental material).
Monthly Follow-up Phone Calls: A research assistant contacted participants in the intervention group once a month for six months and continued jointly setting steps/day goals with the study participant after discharge from PT. The purpose of the phone calls once a month for six months was to provide an additional PA goal setting after discharge from PT. A research assistant called participants, instead of a physical therapist because this model of delivery is more feasible in the clinical practice.
Baseline Participant Characteristics
Using electronic medical records, research assistants extracted self-reported health history, demographic, and knee pain at worst on a visual analog scale (VAS), as well as objective knee range of motion (ROM) measurements collected by a licensed physical therapist at the initial PT evaluation, i.e., our study baseline. Quantifying knee pain at worst using a VAS is a valid and reliable method to assess pain.[23] ROM was measured in supine, using a standardize goniometer with the axis positioned at the lateral epicondyle, stationary arm in line with the greater trochanter and moveable arm aligned with the lateral malleolus.
Feasibility, Safety, and Fidelity
We assessed feasibility by evaluating recruitment and retention rates. The recruitment rate was calculated by the number of participants who enrolled in the study divided by the number of people who were screened for eligibility at UDPT. The retention rate was calculated by the number of participants who completed the study from baseline to 6m divided by the total number of enrolled participants. We measured fidelity two ways, 1) the physical therapist’s adherence to administering the intervention (establishing a weekly steps/day goal with the participant) and, 2) the participant’s ability to adhere to the intervention (steps/day monitoring). Adherence to administering the weekly steps/day goal by the physical therapist was measured by a research assistant counting the number of goals documented in the home exercise program log from baseline to discharge from PT. We classified adherence as “achieved” for participants who had ≥ 80% of weekly steps/day goal recorded by the physical therapist and “not achieved” for those with < 80% of weekly steps/day goals, which is consistent with the definition of adherence from a pharmacological perspective.[24] Participants documented the number of days they recorded steps/day using the Fitbit Zip, and those with ≥ 80% of documented of steps/day in the home exercise program log from baseline to discharge were classified as “achieved” adherence and < 80% as “not achieved.” Lastly, we assessed safety by reporting the number of adverse events recorded from baseline to 12m. An adverse event was defined as any unfavorable or unintended diagnosis, sign, symptom, or disease associated with the study, which may or may not be related to the intervention.
Physical Activity
PA was objectively measured using the ActigraphGT3X, which is a reliable and valid measurement of PA in older adults after TKR.[25] PA was quantified in units of steps/day and time spent in MPVA/week. Participants wore the monitor on the waist positioned at the right anterior superior iliac spine from when they got up in the morning until they went to sleep. The participants were also instructed to remove the monitor when the device could get wet, e.g., showering, swimming. Participants wore the monitor for one week (7 days) at baseline, discharge (DC), 6m and 12m (Fig. 1). Data from the ActigraphGT3X was downloaded and analyzed following a standardized protocol reported by Troiano et al. (https://epi.grants.cancer.gov/nhanes_pam/).[26] Briefly, we defined a valid wear day as ≥ 10 hours of wear time, excluding time with 90 or more consecutive minutes of <100 activity counts, and we only included PA data with ≥ four valid wear days.[26]
Fig. 1.
CONSORT Diagram
Sample Size Calculation
This sample size for this study was based on the general notion for pilot studies to recruit at least 30 participants for each parameter and expect 20% to drop out.[27, 28] At the start of the study we intended to recruit 72 participants with 36 participants in each group to successfully retain a total of 60 participants in the control and intervention group at 12m. We stopped enrollment at 43 participants as we received funding for a larger trial to investigate the effectiveness of our intervention.
Statistical Analysis
We calculated the mean and 95% confidence intervals (95%CI) for continuous variables and frequency counts for categorical variables to describe participant characteristics. Independent t-tests and Chi-squared tests were used to evaluate baseline differences between intervention and control group for continuous and categorical variables, respectively. We described safety (“adverse event”/ “no event”) and intervention fidelity (“achieved”/ “not achieved”) in terms of frequencies. We calculated the mean, standard deviation (SD), and 95%CI between groups at baseline, DC, 6m, and 12m for PA outcomes, which included steps/day and minutes/week in MVPA. We also calculated within-group differences from baseline to 6m and 12m using the mean, SD, and 95%CI. For all statistical assessments, a p-value of less than 0.05 was considered statistically significant. Data were analyzed using SAS version 9.4 (SAS Institute, Cary, North Carolina).
Results
Study Sample
Of the enrolled participants, the mean (SD) age was 67.0 (7.0) years, BMI (kg/m2) 31.5 (5.9) kg/m2, 53.4% were women, and time from TKR surgery to the first PT appointment was 13.8 days (21.3) (Table 1). On average, participants in the intervention group attended PT for 20 (8) visits over 10.4 (5.5) weeks, and participants in the control group attended PT for 18 (7) visits over 9.0 (2.7) weeks. We did not adjust for any baseline characteristics in our statistical model (Table 1), since there were no differences between control and intervention groups, except for the side of TKR (p=0.004), which we did not consider as a potential confounder.
Table 1.
Participant characteristics at baseline, sample size indicated if data is missing
| All Participant (N=43) |
Intervention (N=20) |
Control (N=23) |
||
|---|---|---|---|---|
| Mean ± SD or % (n) | Mean ± SD or % (n) | Mean ± SD or % (n) | p-value | |
| Age (years) | 67.0 ± 7.0 | 66.5 ± 6.9 | 67.5 ± 7.2 | 0.5 |
| Women | 53.4% (23) | 40.0% (8) | 65.2% (15) | 0.1 |
| BMI (kg/m2) (n=40) | 31.5 ± 5.9 | 31.1 ± 5.6 | 32.0 ± 6.3 | 0.6 |
| Education (≥College) | 51.3% (20) | 55.0% (10) | 47.6% (10) | 0.6 |
| White (Other) | 91% (39) | 95% (19) | 87% (20) | 0.7 |
| Time post-TKR to PT (days) | 13.8 ± 21.3 | 9.6 ± 7.0 | *18.0 ± 35.9 | 0.3 |
| Total number of PT visits (n=39) | 19 ± 8 | 20 ± 8 | 18 ± 7 | 0.4 |
| Duration of PT in weeks (n=39) | 9.7 ± 3.4 | 10.4 ± 5.5 | 9.0 ± 2.7 | 0.3 |
| Unilateral TKR side (right) | 52.7% (22) | 75.0% (15) | 30.4% (7) | <0.004 |
| Comorbidity (≥1) (n=42) | 50.3% (21) | 55.0% (11) | 45.5% (10) | 0.4 |
| Knee pain at worst (VAS) | 6.5 ± 2.9 | 6.5 ± 2.8 | 6.6 ± 3.0 | 0.9 |
| Knee flexion (degrees) (n=42) | 85.4 ± 31.4 | 76.3 ± 36.2 | 94.5 ± 26.6 | 0.07 |
| Knee extension^ (degrees) (n=42) | 5.7 ± 4.4 | 5.5 ± 3.8 | 5.9 ± 5.0 | 0.9 |
One participant in the control group started PT 6-months after unilateral TKR
Comorbidity present of; cardiovascular disease/chronic obstructive pulmonary disease/stroke/cancer/history of falls/diabetes/depression
Visual Analog Scale (VAS)
Knee flexion and extension passive range of motion on unilateral TKR side
- lacking knee extension
Feasibility, Safety, and Fidelity
Sixty-seven people after unilateral TKR were screened between March 2016 and June 2017, of which 43 were eligible, enrolled, and randomized in the study (Table 2). The recruitment rate was 64% (43/67) (Fig. 2). The overall retention rate at 6m was 83.7% (36/43) and at 12m was 67% (29/43) (Fig. 2). Three adverse events occurred with participants in the control group during the study. One participant had two adverse events by injuring the contralateral knee and bruising a tendon in the back of ipsilateral knee between the 6m to 12m follow-up. Another participant was diagnosed with gout in the first metatarsal joint during PT. All adverse events were unrelated to the PA intervention. Sixty percent (12/20) of those in the intervention group monitored steps/day at least 80% of the time while in PT, while 45% (9/20) of physical therapists adhered to administering the intervention by documenting a weekly steps/day goal ≥ 80% of the time.
Table 2:
Reasons patients did not enroll in the study
| Ineligible* | n=15 |
| Not meeting BMI criteria* | 1 |
| Not meeting number of days post-operative TKR* | 2 |
| Bilateral TKR | 1 |
| Lower extremity surgery within 6 months | 7 |
| Not Interested in increasing PA | 3 |
| Medical reason - orthostatic hypotension | 1 |
| Decline to participate | n=7 |
| Not interested in participating in research | 7 |
| Other reasons | n=2 |
| Unable to consent due to clinic logistics | 1 |
| Previously enrolled in a PA study | 1 |
eligibility criteria was modified at the start of the pilot study to remove two exclusion criterion: (1) BMI of < 30 and (2) < 6 weeks post-operative TKR to improve the feasibility of recruiting participants in clinical practice.
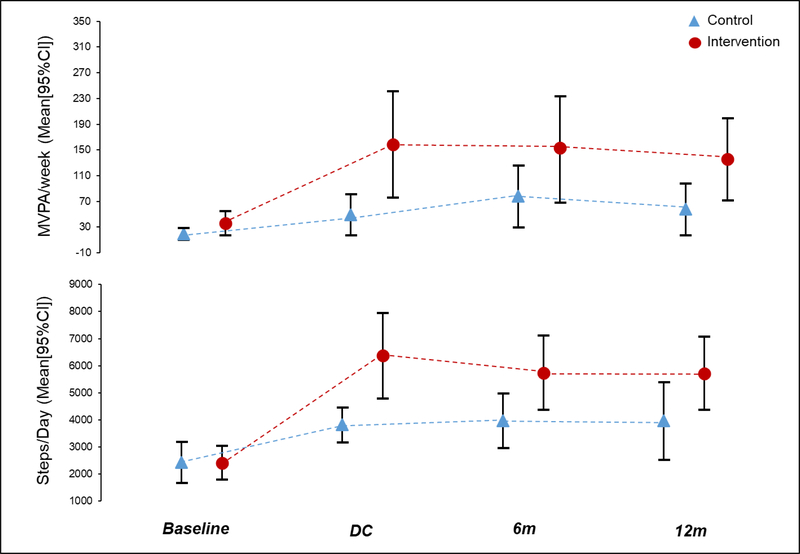
Fig. 2. Physical activity between groups at bassline, DC, 6m, and 12m.
Note: MVPA = Moderate-to-vigorous physical activity, 95%CI = 95% Confidence Interval
Control group sample size: baseline (n=21), DC (n=17), 6m (n=19), 12m (n=15)
Intervention group sample size: baseline (n=18), DC (n=19), 6m (n=17), 12m (n=14)
Physical Activity
Participants in the control group (n=23) had similar daily steps counts at baseline as the intervention group (n=20) (Table 3, mean steps/day [95%CI]: Control 2214 [1573, 2855]; Intervention 2494 [1803, 3168]). However, MVPA minutes/week was less in the control group than the intervention, though this difference did not meet statistical significance (Table 3, mean minutes/week: Control 19.4 [9.9, 28.9]; Intervention 35.6 [16.7, 54.5]). Of the 43 participants, 15 in the control group and 14 in the intervention group had complete PA data from baseline to 12m (Fig. 1).
Table 3.
Physical activity between groups at baseline, DC, 6m, 12m
| Control |
Intervention |
Difference Between Groups |
|
|---|---|---|---|
| Mean ± SD [95%CI] | Mean ± SD [95%CI] | Mean ± SD [95%CI] | |
| Steps/Day (steps) | |||
| Baseline | 2214 ± 1407 [1573, 2855] | 2494 ± 1391 [1803, 3186] | 280 ± 1340 [–631, 1191] |
| Discharge | 3823 ± 1356 [3126, 4520] | 6389 ± 3279 [4808, 7969] | 2566 ± 2561 [828, 4303] |
| 6m | 3941 ± 1910 [3021, 4863] | 5739 ± 2665 [4369, 7109] | 1798 ± 2296 [240, 3355] |
| 12m | 4169 ± 1890 [3123, 5217] | 6114 ± 1989 [4966, 7262] | 1945 ± 1938 [466, 3422] |
| MVPA/Week (min) | |||
| Baseline | 19.4 ± 20.8 [9.9, 28.9] | 35.6 ± 37.9 [16.7, 54.5] | 16.2 ± 29.9 [−3.7, 35.7] |
| Discharge | 46.4 ± 65.4 [12.8, 80.0] | 158.4 ± 172.3 [75.2, 241.3] | 112.0 ± 133.1 [21.5, 202.2] |
| 6m | 77.2 ± 91.3 [33.3, 121.2] | 150.6 ± 161.2 [67.7, 233.5] | 73.4 ± 129.0 [−14.1, 160.9] |
| 12m | 57.7 ± 72.7 [17.5, 98.0] | 133.8 ± 98.1 [77.1, 190.4] | 76.1 ± 85.9 [10.5, 141.5] |
At 6m, the intervention group accumulated 1798 more steps/day [240, 3355] and spent 73.4 more minutes/week [−14.1, 160.9] in MVPA than the control group (Table 3). In particular, the control group walked 3941 [3021, 4863] steps/day and spent 77.2 [33.3, 121.2] minutes/week in MVPA, while the intervention group walked 5739 [4369, 7109] and spent 150.6 [67.7, 233.5] minutes/week in MPVA at 6m (Table 3). At 12m the intervention group accumulating 1945 more steps/day [466, 3422] and spent 76.1 more minutes/week [10.5, 141.5] in MVPA than the control group (Table 3). The control group walked 4169 [3123, 5217] steps/day and spent 57.7 [17.5, 98.0] minutes/week in MVPA, while the intervention group walked 6114 [4966, 7276] and spent 133.8 [77.1, 190.4] minutes/week in MPVA at 12m (Table 3).
Discussion
We found that a physical therapist-administered PA intervention was feasible and safe, and had modest fidelity. Also, the intervention was potentially effective for people after TKR as we found improvements in PA that met clinically meaningful levels. For instance, the intervention group walked about 6,000 steps/day after discharge from outpatient PT, which is a meaningful threshold for reducing the risk of functional limitation in people with knee OA.[22] In contrast, the control walked about the same as the general population ~4,000 steps/day.[29] Moreover, the intervention group spent >150 minutes/week in MVPA at discharge and 6m meeting the 2018 Department of Health and Human Services PA guidelines for aerobic activity.[10] Our results are promising to target inactivity and subsequent weight gain that is common after TKR.
Despite gains in PA adherence to the intervention was modest from both participants and treating physical therapists. Less than half (45%) of the physical therapists documented that they consistently provided weekly steps/day goals and 60% of participants monitored their steps/day. While we were unable to track how often patients looked at their Fitbit, it is possible that self-monitoring steps/day from a device with a daily goal may be more useful to increase PA than a weekly goal given by a PT. The intervention was safe as no participants in the intervention group reported an adverse event. We also note that the monthly phones made by a research assistant from the 6m to 12m follow-up did not result in a noticeable change in PA.
Our findings that using a Fitbit monitor paired with step goals is feasible and safe, showed good fidelity and can increase physical activity after TKR is consistent with other studies.[30–32] For people after TKR, Losina et al. reported financial incentives with telephone health coaching and a Fitbit led to a clinically meaningful increase in steps/day within the first six months after TKR.[33] Furthermore, our finding that PA does not change from 6 to 12 months after surgery is consistent with the literature.[3, 34, 35] In a meta-analysis Hammett et al., observed no change in PA at six months after TKR with only a small change in PA at 12 months.[3] Both the control and intervention group in our study had no significant differences in PA from DC to 6m and 12m, indicating that providing a PA intervention during outpatient PT may be an optimal time to improve PA
Strengths of our study included measuring PA using an accelerometer-enabled device, and a brief PA intervention. Our intervention took roughly 5 minutes/week to set and progress weekly steps/day goals, which improved the feasibility for clinical implementation. However, our study was not without limitations. We had a small sample size with a moderate dropout rate at 12m. The dropout rate was equal between the control and intervention group, with most participants dropping out after the 6m follow-up. This indicates a study follow-up of more than six months may be challenging in this patient population. Since this was a pilot study, i.e., we sought to determine feasibility, safety, and fidelity, we felt it was acceptable to have a small and underpowered sample size. There was high variability around the number of days after surgery participants started outpatient PT and enrolled our study; the mean time participants enrolled in the study was 14 days after TKR, the standard deviation was 21 days, and the range was 2 to 175 days. Outpatient PT typically commences between 2 to 12 weeks after TKR and the time post-surgery when participants enrolled in our study was within this range. Therefore, this variability is expected.[36] Lastly, we only included people after TKR who were interested in increasing their PA that may limit the generalizability of our sample to all-comers. We did so because those who are not interested in PA may require additional behavioral change techniques, e.g., motivational interviewing, to increase PA, which was not feasible in our study.
Overall, a physical therapist-administered PA intervention was feasible and safe, demonstrated modest fidelity, and may promote an increase in PA after TKR that appeared to remain up to 12 months after discharge from PT. Our preliminary findings support that PT may indeed be a practical delivery model for a PA intervention after TKR. Given these study findings, further research is needed, with appropriate power, to establish the effectiveness of this intervention.
Supplementary Material
Significance and Innovation.
Outpatient PT is an ideal setting to increase physical activity since physical therapists are experts in exercise and commonly see patients after TKR for multiple visits, but it is unclear if a physical activity intervention in PT is feasible and safe, demonstrates fidelity, and can increase physical activity after TKR
We found the physical therapist-administered physical activity intervention to be feasible and safe, have modest fidelity and observed clinically meaningful increases in physical activity among those in the intervention group
Study participants receiving the intervention reached levels of physical activity consistent with the 2018 Physical Activity Guidelines for Americans, and the majority of those in the intervention walked > 6000 steps/day, a level needed to prevent the development of functional limitation, six months after discharge from PT
Acknowledgments
Funding: NIH- R21-AR071079–01A1, U54 GM104941, K12HD055931–01
Footnotes
Potential conflict of interest: none
References
- 1.Weinstein AM, Rome BN, Reichmann WM, Collins JE, Burbine SA, Thornhill TS, Wright J, Katz JN, Losina E: Estimating the Burden of Total Knee Replacement in the United States. The Journal of Bone & Joint Surgery 2013, 95(5):385–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caspersen CJ, Powell KE, Christenson GM: Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Reports 1985, 100(2):126–131. [PMC free article] [PubMed] [Google Scholar]
- 3.Hammett T, Simonian A, Austin M, Butler R, Allen KD, Ledbetter L, Goode AP: Changes in physical activity after total hip or knee arthroplasty: A systematic review and meta-analysis of 6 and 12 month outcomes. Arthritis care & research 2017. [DOI] [PubMed] [Google Scholar]
- 4.Booth FW, Roberts CK, Laye MJ: Lack of exercise is a major cause of chronic diseases. Comprehensive Physiology 2012, 2(2):1143–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeni JA Jr., Snyder-Mackler L: Most patients gain weight in the 2 years after total knee arthroplasty: comparison to a healthy control group. Osteoarthritis Cartilage 2010, 18(4):510–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riddle DL, Singh JA, Harmsen WS, Schleck CD, Lewallen DG: Clinically important body weight gain following knee arthroplasty: a five-year comparative cohort study. Arthritis care & research 2013, 65(5):669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shortreed SM, Peeters A, Forbes AB: Estimating the effect of long-term physical activity on cardiovascular disease and mortality: evidence from the Framingham Heart Study. Heart (British Cardiac Society) 2013, 99(9):649–654. [DOI] [PubMed] [Google Scholar]
- 8.Sowers MR, Karvonen-Gutierrez CA: The evolving role of obesity in knee osteoarthritis. Curr Opin Rheumatol 2010, 22(5):533–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piva SR, Susko AM, Khoja SS, Josbeno DA, Fitzgerald GK, Toledo FG: Links between osteoarthritis and diabetes: implications for management from a physical activity perspective. Clin Geriatr Med 2015, 31(1):67–87, viii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.US Department of Health and Human Services: 2018 physical activity guidelines for Americans. In.; 2018: 1–10.
- 11.Hawker GA, Croxford R, Bierman AS, Harvey PJ, Ravi B, Stanaitis I, Lipscombe LL: All-cause mortality and serious cardiovascular events in people with hip and knee osteoarthritis: a population based cohort study. PLoS One 2014, 9(3):e91286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN: The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am 2012, 94(3):201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kurtz S, Ong K, Lau E, Mowat F, Halpern M: Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. The Journal of Bone & Joint Surgery 2007, 89(4):780–785. [DOI] [PubMed] [Google Scholar]
- 14.Guide to Physical Therapist Practice. Second Edition. American Physical Therapy Association. Phys Ther 2001, 81(1):9–746. [PubMed] [Google Scholar]
- 15.Brawley LR, Rejeski WJ, King AC: Promoting physical activity for older adults: The challenges for changing behavior. American Journal of Preventive Medicine 2003, 25(3, Supplement 2):172–183. [DOI] [PubMed] [Google Scholar]
- 16.Black B, Ingman M, Janes J: Physical Therapists’ Role in Health Promotion as Perceived by the Patient: Descriptive Survey. Physical therapy 2016, 96(10):1588–1596. [DOI] [PubMed] [Google Scholar]
- 17.Chase J-AD: Interventions to Increase Physical Activity Among Older Adults: A Meta-Analysis. The Gerontologist 2015, 55(4):706–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Furber S, Monger C, Franco L, Mayne D, Jones LA, Laws R, Waters L: The effectiveness of a brief intervention using a pedometer and step-recording diary in promoting physical activity in people diagnosed with type 2 diabetes or impaired glucose tolerance. Health promotion journal of Australia: official journal of Australian Association of Health Promotion Professionals 2008, 19(3):189–195. [DOI] [PubMed] [Google Scholar]
- 19.Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, Stave CD, Olkin I, Sirard JR: Using pedometers to increase physical activity and improve health: a systematic review. JAMA 2007, 298(19):2296–2304. [DOI] [PubMed] [Google Scholar]
- 20.Lyons EJ, Lewis ZH: Behavior change techniques implemented in electronic lifestyle activity monitors: a systematic content analysis. 2014, 16(8):e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conroy DE, Dubansky A, Remillard J, Murray R, Pellegrini CA, Phillips SM, Streeper NM: Using Behavior Change Techniques to Guide Selections of Mobile Applications to Promote Fluid Consumption. Urology 2017, 99:33–37. [DOI] [PubMed] [Google Scholar]
- 22.White DK, Tudor-Locke C, Zhang Y, Fielding R, LaValley M, Felson DT, Gross KD, Nevitt MC, Lewis CE, Torner J, et al. : Daily walking and the risk of incident functional limitation in knee OA: An observational study. Arthritis care & research 2014, 66(9):1328–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, Fainsinger R, Aass N, Kaasa S: Studies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature Review. Journal of Pain and Symptom Management 2011, 41(6):1073–1093. [DOI] [PubMed] [Google Scholar]
- 24.Morrison A, Stauffer ME, Kaufman AS: Defining medication adherence in individual patients. Patient preference and adherence 2015, 9:893–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Almeida GJ, Irrgang JJ, Fitzgerald GK, Jakicic JM, Piva SR: Reliability of Physical Activity Measures During Free-Living Activities in People After Total Knee Arthroplasty. Physical Therapy 2016, 96(6):898–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.TROIANO RP, BERRIGAN D, DODD KW, MÂSSE LC, TILERT T, MCDOWELL M: Physical Activity in the United States Measured by Accelerometer. Medicine & Science in Sports & Exercise 2008, 40(1):181–188. [DOI] [PubMed] [Google Scholar]
- 27.Browne RH: On the use of a pilot sample for sample size determination. Statistics in Medicine 1995, 14(17):1933–1940. [DOI] [PubMed] [Google Scholar]
- 28.Lancaster GA, Dodd S, Williamson PR: Design and analysis of pilot studies: recommendations for good practice. Journal of Evaluation in Clinical Practice 2004, 10(2):307–312. [DOI] [PubMed] [Google Scholar]
- 29.Thoma LM, Dunlop D, Song J, Lee J, Tudor-Locke C, Aguiar EJ, Master H, Christiansen MB, White DK: Are older adults with symptomatic knee osteoarthritis less active than the general population?: Analysis from the Osteoarthritis Initiative and NHANES. Arthritis care & research 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paxton RJ, Forster JE, Miller MJ, Gerron KL, Stevens-Lapsley JE, Christiansen CL: A Feasibility Study for Improved Physical Activity After Total Knee Arthroplasty. J Aging Phys Act 2018, 26(1):7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang JB, Cadmus-Bertram LA, Natarajan L, White MM, Madanat H, Nichols JF, Ayala GX, Pierce JP: Wearable Sensor/Device (Fitbit One) and SMS Text-Messaging Prompts to Increase Physical Activity in Overweight and Obese Adults: A Randomized Controlled Trial. Telemedicine journal and e-health: the official journal of the American Telemedicine Association 2015, 21(10):782–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cadmus-Bertram LA, Marcus BH, Patterson RE, Parker BA, Morey BL: Randomized Trial of a Fitbit-Based Physical Activity Intervention for Women. Am J Prev Med 2015, 49(3):414–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Losina E, Collins JE, Deshpande BR, Smith SR, Michl GL, Usiskin IM, Klara KM, Winter AR, Yang HY, Selzer F, et al. : Financial incentives and health coaching to improve physical activity following total knee replacement: a randomized controlled trial. Arthritis care & research 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith TO, Mansfield M, Dainty J, Hilton G, Mann CJV, Sackley CM: Does physical activity change following hip and knee replacement? Matched case-control study evaluating Physical Activity Scale for the Elderly data from the Osteoarthritis Initiative. Physiotherapy 2017. [DOI] [PubMed] [Google Scholar]
- 35.Kahn TL, Schwarzkopf R: Does Total Knee Arthroplasty Affect Physical Activity Levels? Data from the Osteoarthritis Initiative. J Arthroplasty 2015, 30(9):1521–1525. [DOI] [PubMed] [Google Scholar]
- 36.Artz N, Elvers KT, Lowe CM, Sackley C, Jepson P, Beswick AD: Effectiveness of physiotherapy exercise following total knee replacement: systematic review and meta-analysis. BMC Musculoskeletal Disorders 2015, 16:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.