Abstract
A major burden of severe asthma is the future risk of adverse health outcomes. Patients with severe asthma are prone to serious exacerbation and deterioration of lung function and may experience side effects of medications such as oral corticosteroids (OCSs). However, such future risk is not easily measurable in daily clinical practice. In particular, currently available tools to measure asthma control and asthma-related quality of life incompletely predict the future risk of medication-related morbidity. This is a significant issue in asthma management. This review summarizes the current evidence of future risk in patients with severe asthma. As future risk is poorly perceived by controlled asthmatics, our review focuses on the risk in patients with ‘controlled’ severe asthma. Of note, it is likely that long-term OCS therapy may not prevent future asthma progression, including lung function decline. In addition, the risk of drug side effects increases even during low-dose OCS therapy. Thus, novel treatments are highly desirable for reducing future risks without any loss of asthma control.
Keywords: Asthma, severity, risk
INTRODUCTION
Severe asthma is an ‘invisible’ condition not readily observable to others.1 This condition is not just ‘bad’ asthma, but a serious threat to life as it involves physical, mental and social impairment. Many patients with severe asthma live with fears, switch or leave their jobs, and have difficulties with friend and family relationships.2,3 Despite high-intensity medications and good adherence to them, the burden of severe asthma is not successfully reduced.
A major burden of severe asthma is the future risk of adverse health outcomes. Patients with severe asthma are prone to exacerbation and serious deterioration in lung functions, and may also experience side effects from medications such as systemic corticosteroid (SCS). Hence, the European Respiratory Society (ERS)/American Thoracic Society (ATS) guidelines4 define this disease not only as asthma which remains “uncontrolled” despite aggressive drug therapy (such as high-dose inhaled corticosteroid [ICS] plus second controller and/or SCS), but also one that requires aggressive therapy to prevent from becoming “uncontrolled.” In essence, therefore, “controlled” severe asthma is considered a severe form of asthma due to the future risk of serious adverse events.4
Future risk factors for severe asthma are not easily detected in daily clinical practice. In particular, currently available tools to measure asthma control and asthma-related quality of life incompletely predict the future risk of medication-related morbidity, which is a significant issue in asthma management.5 In our clinical experience, the future risks of severe asthma are poorly recognized by patients themselves and even physicians, especially when asthma control is relatively well maintained by high-intensity treatments including intermittent oral corticosteroid (OCS) bursts. Therefore, we review here future risk existing in patients with severe asthma. This review starts with the question – “What are the possible future risks in severe asthma, and why is it important to address?” As the risk is poorly perceived by controlled patients, our review will more focus on the risks in patients with ‘controlled’ severe asthma.
CONCEPTS OF ASTHMA SEVERITY, CONTROL AND FUTURE RISKS
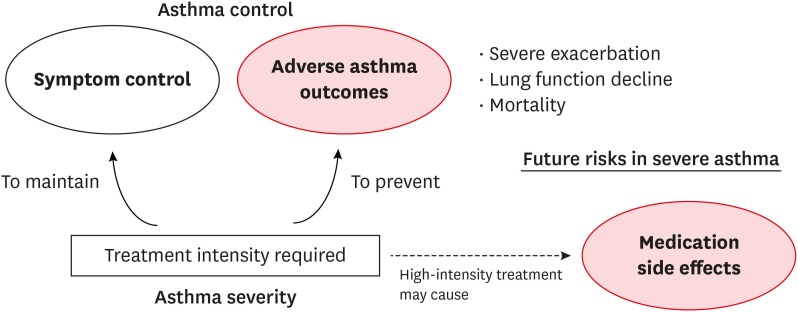
The concept of asthma severity has evolved during the last decade. The word ‘severity’ in the context of asthma had been used previously to describe the degree of airflow obstruction, symptoms, or exacerbations. In the Global Initiative for Asthma (GINA) guidelines 1995, asthma severity was used to classify the off-treatment status of a patient (such as intermittent, mild persistent, moderate persistent and severe persistent).6 This classification was used to determine initial treatment strategy. However, current clinical practice guidelines no longer classify asthma in terms of off-treatment severity, but are aimed at achieving disease control, which is now possible in most patients irrespective of their initial levels of off-treatment severity.7 Asthma severity is currently assessed by the intensity of treatment required to achieve good asthma control (symptoms and exacerbations) and, in very severe cases, by treatment refractoriness (Fig. 1).4 In this review, the definition of severe asthma followed the recommendations of the 2014 ERS/ATS guidelines.4
Fig. 1. Concepts of asthma control, asthma severity and future risk in severe asthmatics. Unlike other adverse asthma outcomes, future risk of medication side effects are not readily measurable in daily clinical practice for severe asthma.
Asthma control refers to the extent to which the manifestations of asthma are reduced or removed by treatment.8 The assessment of asthma control incorporates 2 components - current symptoms and future risk of adverse health outcomes (such as exacerbations, fixed airway obstruction and drug side effects) (Fig. 1). Drug side effects can result from the use of a high-intensity treatment to achieve asthma control. However, it is important to note that current standard tools for asthma control, such as the asthma control test (ACT) or asthma control questionnaire (ACQ), do not include any items that address any future risk of drug side effect, even though this is a major burden on patients with severe asthma.5
EPIDEMIOLOGY OF SEVERE ASTHMA
Due to the evolving concepts of asthma severity, the definition and prevalence of severe asthma varies among published articles. In an observational study using the pharmacy database combined with a questionnaire survey in the Netherlands, it was estimated that 3.6% of adult asthmatics have severe refractory asthma as defined by a high-intensity treatment requirement, poor control, and good adherence and inhaler technique.9 When applying the ERS/ATS guideline definition,4 the prevalence of severe asthma has increased from 3.6% to 4.5%, suggesting that the prevalence of controlled severe asthmatics was about 0.9% among adult asthmatics in the community population.
In a Swedish general population-based study of 744 subjects with “active asthma” (as defined by asthma symptoms or medication in the prior year), 36.2% of the asthmatics had at least one sign of asthma severity, i.e., 1) multiple symptoms during the day despite the ongoing use of asthma medications; 2) an FEV1 of less than 70% of the predicted value; 3) daily, or almost daily, use of rescue medications; 4) night-time symptoms once a week or more; and 5) OCS use/emergency department (ED) visits.10 Importantly, the prevalence of OCS use/ED visits was 9% among active asthmatics, and about 13% reported at least 2 signs of severity,10 suggesting a potential burden of future risks related to severe asthma existing in asthmatic patients even in the general population.
In a systematic review of the epidemiology and burden of uncontrolled severe asthma, the percentage of patients with uncontrolled severe asthma among all asthmatics varied widely from 0.7% to 49.2%.11 There was a substantial heterogeneity in the tools used to define asthma control in the studies included, such as ACT, ACQ, and international guideline- or exacerbation history-based definitions. Of note, the percentage of uncontrolled severe asthmatics among overall severe patients in that study ranged from 14.2% to 79%, suggesting that the frequency of controlled severe asthma was also substantial.11
There are no solid longitudinal data on natural disease courses in patients with severe asthma or at the control status. The available evidence suggests that the severity of asthma may be an inherent characteristic of the affected patient. In a 12-month longitudinal follow-up study, a loss of control is common in severe asthmatics, but poor control is likely to be persistent over time.12 Several host factors, such as comorbidities and genetics, may interact with socio-environmental factors in determining the likelihood of persistence in asthma severity and these traits are not easily treatable or modifiable.
RELEVANCE OF POOR ASTHMA CONTROL TO FUTURE RISKS IN SEVERE ASTHMATICS
Patients with severe asthma frequently experience poor control.13,14,15,16,17,18,19 In the Epidemiology and Natural History of Asthma: Outcomes and Treatment Regimens (TENOR) II cohort study,19 a follow-up survey of 341 patients with severe or difficult-to-treat asthma more than 10 years after enrolment in the TENOR I study, more than half of the subjects (58.1%) were still very poorly controlled, and only 7.7% were well controlled.19
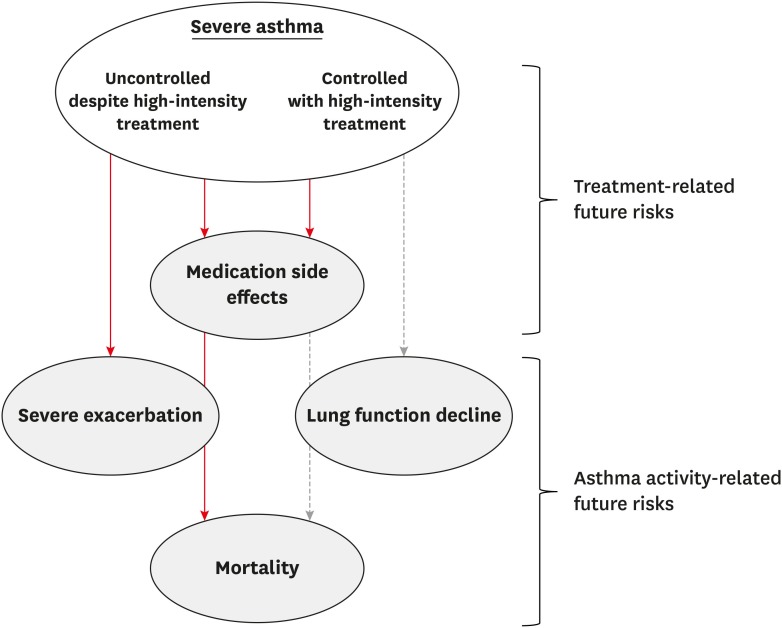
The relevance of current asthma control to future clinical outcomes has been consistently demonstrated in the literature. In the TENOR I study (severe persistent asthma cases, 54.1%), the asthma control score showed significant correlations with the health-related quality of life measure at baseline and during longitudinal follow-ups.20 In addition, the control status of asthma was significantly correlated with the number of OCS courses, unscheduled clinic visits, ED visits and hospitalizations.21 These correlations remained significant when adjusted for the baseline asthma severity (off-treatment).20,21 In a prior post hoc analysis of a randomized clinical trial (RCT) with an interleukin (IL)-4 receptor α antagonist in patients with moderate to severe atopic asthma, an increase in the ACQ score by 1 increased the future risk of exacerbations by 50%.22 Moreover, in a retrospective analysis of 5 budesonide/formoterol maintenance and reliever therapy trials, the current control status predicted the control status in the following week with at least 80% probability and was also significantly associated with future exacerbation risk.23 In a 24-month longitudinal follow-up in the TENOR I study, very poor control was significantly associated with future risk of exacerbations.24 These findings collectively indicate that the current asthma control status is highly relevant to the future risk of adverse clinical outcomes and that expected future risk may differ between controlled and uncontrolled severe asthmatics (Fig. 2).
Fig. 2. Different future risks in patients with severe asthma according to their control status. The red line denotes a high likelihood of a relationship. The grey dotted line indicates an uncertain likelihood (lack of evidence for the relationship).
FUTURE RISK OF EXACERBATIONS IN SEVERE ASTHMATICS
Exacerbation is a defining feature of severe asthma, which is defined by a worsening of symptoms requiring the use of SCS or an increase in the SCS doses in patients on a stable maintenance dose, to prevent serious outcomes.25 In a cross-sectional assessment of the TENOR II cohort participants with severe or difficult-to-treat asthma, 48.2% of the cases experienced exacerbation in the recent 12 months and 21.3% had severe exacerbations (defined as hospitalization or ED visit due to asthma requiring SCS).19 In the Australian Severe Asthma Web-Based Database, severe asthmatic patients experienced a median of 2 exacerbations during the 2-year follow-up.26
In a 5-year prospective longitudinal follow-up study of 177 patients with “problematic asthma” (as defined according to the Innovative Medicines Initiative27 which encompasses both difficult-to-treat asthma and severe asthma) from Singapore, there were 3 distinct trajectories described in terms of severe exacerbation rates: “infrequent exacerbators” (58.5%; stable disease with few intermittent severe exacerbations), “non-persistently frequent exacerbators” (32.0%; frequent severe exacerbations at baseline, but improved subsequently), and “persistently frequent exacerbators” (9.5%).17 The most unfavourable trajectory group had an annual mean incidence of severe exacerbation of around 4 person-years, whereas the other 2 groups showed a less than 1 person-year incidence at 5 years. The unfavourable group characteristics included a higher body mass index, more frequent history of near-fatal asthma or severe exacerbation as well as more frequent gastroesophageal reflux disease (GERD), obstructive sleep apnoea, and depression than the other 2 trajectory groups.17 However, no longitudinal correlations with asthma control status were presented.
It is expected that the future risk of exacerbations will be lower in severe controlled than uncontrolled asthmatics, but the precise incidence of this adverse event in controlled severe asthma has not been reported.
Overall, a history of exacerbation is one of the strongest predictors of the future risk of exacerbation events in different asthmatic populations.26,28,29,30,31,32,33,34 Various host factors, such as smoking history, poor lung function, nasal polyps, obesity, autoimmune disorders, GERD/vocal cord dysfunction, and comorbid depression, are also associated with the future risk of exacerbation in patients at various ages and with different asthma severity.26,34,35,36,37,38,39,40,41 In patients with severe asthma, uncontrolled type 2 airway inflammation is also significantly associated with high exacerbation rates.42,43,44,45 These findings collectively indicate that systematic assessments and interventions are required to achieve proper asthma control and to reduce the future risk of exacerbations in severe asthma cases.
FUTURE RISK OF LUNG FUNCTION DECLINE IN SEVERE ASTHMATICS
Only a few studies to date have examined the longitudinal changes in lung function in severe asthmatics. In a 6-year follow-up study of 97 patients with severe asthma in the Glenfield cohort, the recorded annual mean decline in the post-bronchodilator FEV1 was −25.7 mL/year.46 Of note, there were 3 clusters in that study differing in terms of eosinophilic airway inflammation and the rate of post-bronchodilator FEV1 decline, of which the cluster with low-grade but positive sputum eosinophilia (geometric mean eosinophils%, 4.28% [95% confidence interval {CI}, 1.07%–7.49%]) and large variations over time showed the highest rate of lung function decline (−40.9 mL/year).46
The longitudinal course of lung function was also examined over a period of 10 years in a prior retrospective study of 54 Japanese patients with severe asthma (as defined by the ATS criteria for refractory asthma47).48 The mean daily ICS dose was 1,830 mcg of beclomethasone dipropionate equivalent, the mean OCS use duration was 67.3 ± 62.9 days/year and annual exacerbation rate was 0.48 ± 0.51. Two phenotypes emerged in that study according to the rapidity of lung function decline, rapid (n = 17) and slow (n = 37), based on a forced vital capacity (FVC) decline rate of −20 mL/year. However, the mean annual rate of change in the FEV1 was +0.6 mL/year. Annual exacerbation rate, OCS use and age were positively associated with the rapid FVC decline in that Japanese cohort.48 However, the possible relationship between lung function decline and asthma control status was also not examined in detail.
In an 8-year longitudinal observation study of 234 patients with severe asthma from an under-privileged area in Brazil, the mean annual decrease in post-bronchodilator FEV1 measured −27.1 (95% CI, −51.1–1.4) mL/year.49 The subjects in this study were receiving appropriate treatment from specialists, and the daily ICS dose was 1,295.5 mcg (of beclomethasone dipropionate equivalent). OCS was required in 62% of these patients during the last year of observation. The percentage of patients with an ACQ score of ≥ 1.5 decreased from 60% at the initial presentation to 37%, and that with an ACQ score of ≤ 0.75 increased from 19% to 42%. The authors noted that lung function decline was not completely prevented by currently available and best-practice treatments, although asthma control was improved by these interventions.49
These longitudinal findings suggest that lung function may continue to decline in severe asthmatics despite high-intensity treatment and that improved asthma control is not sufficient to prevent such progressive deterioration.
FUTURE RISK OF CORTICOSTEROID-INDUCED MORBIDITY IN SEVERE ASTHMATICS
It is estimated that about 1% of the general population receives SCS treatments at any time point and respiratory conditions, including asthma, are reported to account for a major proportion (about 25%–40%) of these prescriptions.50,51,52 It is well known that the use of SCS in patients with different health conditions is positively associated with higher risk of psychiatric events, infection, gastric problems and fractures.53,54 Until recently, however, morbidities from SCS exposure had not been described in asthmatic populations. This knowledge gap was a significant issue, as susceptibility to developing drug-related morbidities may differ according to age, sex, underlying disease, and doses or durations of drug exposure.
Current findings on SCS-induced morbidity in asthmatic populations are summarized in Table. A major finding from these studies is that the risk of complications may increase even at low-dose SCS exposures. The study by Lefebvre et al.55 was the first to investigate the risk of SCS-induced morbidity in patients with severe asthma who had more than 6 months of continuous SCS use. By examining the Medicaid health insurance claims database (1997–2013) in the United States, the authors investigated the positive dose relationships between SCS exposure (≤ 6 mg/day, 6–12 mg/day, and > 12 mg/day of prednisolone equivalent) and the incidence of related complications. Patients with higher exposures to these drugs (> 6 mg/day) had significantly higher risk of complications, including cardiovascular, metabolic, psychiatric, ocular, gastrointestinal and bone disorders as well as infections (odds ratios [ORs] ranging between 1.23 and 2.12 by complication).55
Table. Summary of studies on SCS-induced morbidity in asthmatic populations.
| Study | Database, region | Population and definition | Comparison by SCS exposure | Observation duration | Positive findings* |
|---|---|---|---|---|---|
| Lefebvre et al. (2015)55 | Health insurance claims database (1997–2013: Medicaid), US | • Severe asthma (≥ 12 years old): ≥ 2 administrative charges associated with a diagnosis of asthma and had > 6 months of continuous chronic SCS use (with daily doses of > 5 mg of prednisone equivalent with no gap of 14 days or more between 2 SCS claims) | • Chronic low dose exposure: < 6 mg/day | • 3.8 ± 3.4 years (up to 16 years) | • Infection |
| • Non-matched | • Chronic medium dose exposure: 6–12 mg/day | • Gastrointestinal | |||
| • Mean age at index date: 57.6 ± 16.3 years | • Chronic high dose exposure: > 12 mg/day of prednisolone equivalent | • Bone/muscle | |||
| • Cardiovascular | |||||
| • Metabolic | |||||
| • Psychiatric | |||||
| • Ocular | |||||
| Zazzali et al. (2015)77 | Health insurance claims database (2008–2009), US | • Asthma (≥ 18 years old): ≥ 2 medical claims with asthma and ≥ 2 asthma medication fillings | • No exposure: no OCS supply during the year | • 2 years | • Osteoporosis |
| • Matched by age, sex and geographic region | • High dose exposure: ≥ 30 days of OCS supply in a year, regardless of cumulative dose | • Fracture | |||
| • Mean age at index date: 54.4 ± 12.7 years | • Pneumonia | ||||
| • Opportunistic infection | |||||
| • Hypertension | |||||
| • DM | |||||
| • Cataract | |||||
| • Obesity | |||||
| Dalal et al. (2016)56 | Large administrative claims databases (2003–2014 and 2006–2013; Truven Health MarketScan Research), US | • Asthma (≥ 12 years old): ≥ 2 administrative claims associated with an asthma diagnosis | • No exposure | • No exposure group: 1.1 ± 0.9 years | • Infection |
| • Propensity score matched (based on demographic and clinical co-variates) | • Chronic low dose exposure: < 5 mg/day | • Chronic SCS user group: 2.0 ± 1.9 years | • Bone/muscle | ||
| • Mean age at index date: 62.4 ± 15.2 years | • Chronic medium dose exposure: ≥ 5–10 mg/day | • Skin disease | |||
| • Chronic high dose exposure: > 10 mg/day (of prednisolone equivalent of ≥ 6 months' duration) | • Gastrointestinal (not in low dose group) | ||||
| • Cardiovascular (not in low dose group) | |||||
| • Metabolic (not in low dose group) | |||||
| • Psychiatric (not in low dose group) | |||||
| • Ocular (not in low dose group) | |||||
| Sweeney et al. (2016)58 | Primary care database (OPCRD), UK | • Asthma (≥ 12 years old): ≥ 2 years of continuous medical records of asthma | • No exposure (non-asthmatic control) | • Cross-sectional analysis of database information over 2 years | • Type 2 DM |
| • Severe asthma: step 5 GINA asthma treatment and ≥ 4 OCS prescriptions in each of two consecutive study years | • Mild/moderate asthma: a cumulative OCS dose over the 2 years: median 250 mg (IQR, 150–420 mg) | • Obesity | |||
| • Matched by age and sex | • Severe asthma: a cumulative OCS dose: 3,920 mg (2,395–6,500 mg) | • Osteopenia | |||
| • Mean age: 58 ± 17 years | • Osteoporosis | ||||
| • Fracture | |||||
| • Dyspeptic | |||||
| • Cataract | |||||
| • Cardiovascular | |||||
| • Hypertension | |||||
| • Psychiatric | |||||
| • Sleep disorder | |||||
| • Chronic kidney disease | |||||
| BTS Difficult Asthma Registry (2013), UK | • Severe asthma: diagnosed by specialists | • Severe non-OCS-dependent asthma: not requiring maintenance OCS but requirement for frequent OCS rescue | • Cross-sectional | • Type 2 DM | |
| • Mean age: 50 ± 14.5 years (2.1 years older in severe OCS-dependent asthma group) | • Severe OCS-dependent asthma: requiring daily OCS to maintain asthma control | • Hypertension | |||
| • Hypercholesterolemia | |||||
| • Obesity | |||||
| • Obstructive sleep apnoea | |||||
| • Dyspeptic | |||||
| • Psychiatric | |||||
| Lefebvre et al. (2017)78 | Health insurance claims database (1997–2013: Medicaid), US | • Asthma (≥ 12 years old): ≥ 2 administrative claims associated with an asthma diagnosis | • No exposure | • No exposure group: 2.1 ± 1.6 years | • Gastrointestinal |
| • Non-matched | • Chronic low dose exposure: < 6 mg/day | • Chronic SCS exposure group: 3.8 ± 3.4 years (up to 15 years) | • Infection | ||
| • Mean age at index date: 57.6 ± 16.3 years (for chronic SCS user) and 27.4 ± 17.7 years (for non-user) | • Chronic medium dose exposure: ≥ 6–12 mg/day | • Psychiatric | |||
| • Chronic high dose exposure: > 12 mg/day (of prednisolone equivalent of ≥ 6 months' duration) | • Ocular | ||||
| • Haemato/oncologic | |||||
| • Bone/muscle (not in low dose group) | |||||
| • Cardiovascular (not in low dose group) | |||||
| • Metabolic (not in low dose group) | |||||
| Barry et al. (2018)59 | Primary care database (OPCRD), UK | • Asthma (≥ 12 years old): ≥ 2 years of continuous medical records of asthma | • No exposure (non-asthmatic control) | • Cross-sectional analysis of database information over 2 years | • Overall risk of SCS-related comorbidities was more frequent in younger patients (≤ 45 years old) |
| • Severe asthma: step 5 GINA asthma treatment and ≥ 4 OCS prescriptions in each of two consecutive study years (same population and definitions as the study by Sweeney 201658) | • Mild/moderate asthma with a cumulative OCS dose over 2 years: median 250 mg (IQR, 150–420 mg) | • Risk of fracture was more frequent in older patients (> 70 years old) | |||
| • Matched by age and sex | • Severe asthma with a cumulative OCS dose: 3,920 mg (2,395–6,500 mg) | ||||
| Bloechliger et al. (2018)60 | Primary care database (2000–2015: Clinical Practice Research Datalink), UK | • Asthma (≥ 18 years old): aged 18 years or older with incident or prevalent asthma (defined as requiring at least GINA step 2 treatment) | • Never vs. ever exposure (≥ 1 OCS prescription recorded at any time before the index date) | • Up to 16 years | • Severe infection |
| • Matched by index date, follow-up duration, year of birth, sex, and duration of history in the database | • Timing of exposure (current, recent, or past users, when their last prescription was recorded < 180, 180–365, or > 365 days before the index date) | • Peptic ulcer | |||
| • Cumulative dose (< 500, 500–2,000, and > 2,000 mg) | • Affective disorders | ||||
| • Average daily dose (≤ 1, > 1–5, and > 5 mg) | • Cataract | ||||
| • Frequency of prescriptions (low use: on average 1 prescription/year; medium use: on average 2–3 prescriptions per year; and high use: on average ≥ 4 prescriptions per year) | • Herpes zoster | ||||
| • Cardiovascular events | |||||
| • Type 2 DM | |||||
| • Bone-related conditions | |||||
| Daugherty et al. (2018)61 | Primary care database (2004–2012: Clinical Practice Research Datalink), UK | • Severe asthma (≥ 18 years old): receiving GINA step 4/5 treatment during the pre-index phase | • Average cumulative SCS daily dose: 0, 0–2.5, 2.5–5, 5–7.5, and > 7.5 mg/day | • 3.83 ± 2.4 years (range: 0–8 years) | • Increased risk even at low dose exposure (0–2.5 mg/day vs. no exposure: DM, myocardial infarction and osteoporosis |
| • Mean age: 53.42 ± 18.1 years | |||||
| Price et al. (2018)62 | Primary care databases (1984–2017: OPCRD and Clinical Practice Research Datalink), UK | • Active asthma (≥ 18 years old; with at least two prescriptions for asthma medication in the period) without any record of SCS prescription before index date | • SCS arm (≥ 1 additional prescription for SCS within 18 months after first recorded SCS prescription) vs. non-SCS arm (no recorded parenteral or oral prescription ever) | • SCS arm: median 9.9 years (IQR 4.1–20.0) | • Osteoporosis and osteoporotic fracture |
| • Matched by sex, asthma diagnosis, index date, and the availability of Hospital Episode Statistics linkage | • Non-SCS arm: median 8.7 years (IQR, 3.7–18.2) | • Pneumonia | |||
| • Heart failure | |||||
| • Cardio-/cerebrovascular disease | |||||
| • Cataract | |||||
| • Myocardial infarction | |||||
| • Sleep apnoea | |||||
| • Renal impairment | |||||
| • Depression/anxiety | |||||
| • Cerebrovascular accident | |||||
| • Type 2 DM | |||||
| • Weight gain | |||||
| Sullivan et al. (2018)57 | Health insurance claims database (2000–2014: MarketScan), US | • Asthma (≥ 18 years old): 1) a diagnosis in at least 2 outpatient claims with primary or secondary diagnoses of asthma at least 1 of which must have been during the baseline period; or 2) at least 1 ED or hospitalization claim with a primary diagnosis of asthma during the baseline period | • No OCS exposure | • Range: 2–10 years | • High-level exposure: osteoporosis, hypertension, obesity, type 2 DM, cataract, gastrointestinal ulcers/bleeds, fracture |
| • Propensity score matched (based on age, sex, number of asthma-related ED visits, number of asthma-related inpatient visits, short-acting β agonist use and comorbidity burden) | • Lower level of exposure: 1 to 3 current OCS prescriptions in the current year (or in the past year) | ||||
| • Mean age: 38 years | • Higher level of exposure: 4 or more prescriptions for OCS drugs in the current year (or in the past year) |
SCS, systemic corticosteroid; OCS, oral corticosteroid; DM, diabetes mellitus; OPCRD, Optimum Patient Care Research Database; GINA, Global Initiative for Asthma; IQR, interquartile range; BTS, British Thoracic Society.
*Medical condition for which a significantly increased risk is reported and/or dose response (odds ratio > 1 with statistical significance).
In another study that utilized US administrative claims database analysis of severe asthmatic patients and matched controls, the ORs of developing SCS-related complications were found to increase significantly in a dose-dependent manner. Importantly, even the patients with low-dose exposures (< 5 mg/day of prednisolone equivalent) showed higher risks of complications compared to those without any SCS exposure (OR, 2.50; 95% CI, 1.22–5.10).56 In a further report that analyzed the US MarketScan claims database (2000–2014) for asthmatic patients with a recent history of severe exacerbation (asthma-related ED visit or hospitalization), the number of OCS prescriptions was positively associated with greater odds of osteoporosis, hypertension, obesity, type 2 diabetes mellitus (DM), gastrointestinal ulcers/bleeding, fractures and cataracts (ORs, 1.21–1.44 by complication).57
In the UK, primary care databases have been utilized to assess the risk of SCS-induced morbidity in asthmatic patients. Analyses of the Optimum Patient Care Research Database (OPCRD) has shown that patients with severe asthma and with a median cumulative OCS dose of 3,920 mg over the 2-year study period (interquartile range [IQR], 2,395-6,500 mg) had more comorbidities related to SCS exposure such as type 2 DM, osteoporosis, dyspeptic disorders or cataracts, than those with mild/moderate asthma or non-asthmatic controls.58 Similar findings were observed in another UK study of patients in the British Thoracic Society (BTS) Difficult Asthma Registry. It was notable that 57.4% of the patients in the BTS registry had corticosteroid-dependent severe asthma and had significantly greater occurrence of type 2 DM, hypertension, hypercholesterolemia, obesity, obstructive sleep apnoea, dyspeptic disorders and depression/anxiety/low mood than non-corticosteroid-dependent severe asthmatics (42.6% of the registry who did not require regular maintenance of OCS, but required frequent rescue courses of corticosteroids).58 However, the latter group also frequently had treatment-related complications: 75% and 20% of these patients had ≥1 and ≥3 corticosteroid-related morbidities, respectively.58 In another report involving extended analyses of the OPCRD for age and sex associations, high-dose OCS-related morbidity was more frequent in younger patients (e.g., the OR for type 2 DM was 4.7 [95% CI, 1.5–15.1] in patients ≤45 years, but was 1.2 [95% CI, 0.7–2.0] in those aged 61–70 years).59 Other retrospective cohort analyses utilizing the Clinical Practice Research Datalink or OPCRD demonstrated that the risk of complications was positively associated with cumulative doses, daily average doses, and frequencies of OCS use.60,61,62 Of note, increased risk of a few adverse outcomes (such as cerebrovascular accident, type 2 DM, or depression/anxiety) was observed at a very low threshold of cumulative SCS exposure (0.5–1 g of prednisolone equivalent; vs. 0–0.5 g as the reference), which is equivalent to just 4 lifetime SCS courses.62
ICS is generally considered safe but can cause systemic side effects at chronic high-dose exposures, such as hypothalamic-pituitary-adrenal axis suppression, osteoporosis, DM and ophthalmic complications.63 In a prior longitudinal follow-up study of 196 adults with asthma (aged 20–40 years), a higher cumulative ICS dose (median duration of exposure: 6 years [range, 0.5–24 years]) was inversely correlated with the bone-mineral density.64 In a recent retrospective cohort study of severe asthmatic patients in Korea, cumulative doses of SCS and ICS were significantly correlated with trabecular bone score.65 In another systematic review of case-control studies of non-vertebral fracture risk in adult asthmatics, the relative risk of fracture increased by 12% for each 1,000 µg per day administration of beclomethasone dipropionate or equivalent.66 The cumulative dose of ICS was also significantly correlated with the risk of cataract extraction in a further study.67
FUTURE RISK OF MORTALITY IN SEVERE ASTHMATICS
Asthma mortality has decreased in recent decades, which is quite possibly related to the introduction of ICS therapy. However, the risk of mortality may still exist in patients with severe asthma. In a recent 20-year follow-up study of 52 patients with severe asthma (baseline age: 49.9 ± 18.9 years) at an expert clinic in France, the mortality rate was 50% (19% attributed to fatal asthma) and the relative survival rate (compared to the expected survival rate adjusted for location) was 0.778 (95% CI, 0.57–0.99), indicating an excess risk of death of 22% in this severe asthmatic population.68 In another study from France involving a 3-year longitudinal follow-up of severe asthmatics in a representative claims database, the 3-year cumulative mortality rate was significantly higher in severe asthmatics than in matched non-asthmatic controls (7.1% vs. 4.5%; P = 0.007).69 In a nested case-control study of severe asthmatic patients from Brazil (58 mortality and 232 non-mortality cases, at a 1:4 ratio), most of the deaths were from respiratory causes (60.3%). In the multivariate analyses in that study, male sex, poor asthma control and a lower pre-bronchodilator FEV1 < 60% of predicted were significantly associated with higher mortality risk.70
IS CONTROLLED SEVERE ASTHMA COMPLETELY BEING ‘CONTROLLED’?
As reviewed above, the future risks of adverse outcomes in patients with controlled severe asthma have not been completely studied. These patients may belong to a “grey zone,” because their future health risk is not readily measurable but is also poorly perceived by this group. For this reason, there is an important question as to whether controlled severe asthma is completely being controlled. At the very least, the answer is ‘No’ in terms of the future risk of drug side effects. The risk of drug side effects increases even at low-dose SCS exposure. In addition, it is likely that chronic corticosteroid therapy will not prevent future asthma progression. Lung function decline was not prevented in severe asthmatics despite improvements in asthma control with higher-intensity treatments.49
CAN T2-TARGETED BIOLOGICAL THERAPY PREVENT FUTURE RISKS IN SEVERE ASTHMATICS?
Considering frequent drug side effects in severe asthmatic patients, novel treatments are highly desirable that will enable the tapering of OCS use without any loss of asthma control.71 T2-targeted biological therapies, such as monoclonal antibodies targeting IL-5 and IL-4 pathways, have been demonstrated to reduce OCS maintenance doses in patients with OCS-dependent severe asthmatics.72,73,74 However, although the OCS-sparing benefits of these biologics were superior to those of a placebo, they were still partial in terms of absolute responses. In a 24-week placebo-controlled trial of 135 patients with OCS-dependent severe eosinophilic asthma (median daily OCS dose at baseline: 12.5 mg of prednisone equivalent in the treatment group), the median reduction in OCS dose was 50% from baseline (range: 20%–75% reduction) in the mepolizumab treatment group, compared to 0% (range: 20%–33.3% reduction) in the placebo group (P = 0.007).72 The reduction in daily OCS dose to a level of ≤ 5 mg occurred in 54% of the mepolizumab group and in 32% of the placebo group (OR, 2.45; 95% CI, 1.12–5.37; P = 0.02).72 In a 28-week RCT of 220 patients with OCS-dependent severe eosinophilic asthma (mean daily OCS dose at baseline: 10 mg of prednisolone or equivalent [range: 7.5–40 mg]), the OR of OCS dose reduction was 4.12 (95% CI, 2.22–7.63) with benralizumab compared to placebo. However, the mean OCS dose at the final visit was 5 mg (range: 0–30 mg) in the every-8-week benralizumab treatment group and 10 mg (range: 0–40 mg) in the placebo group.73 The percentages of patients with a reduction in the daily OCS dose to a level ≤ 5 mg was 59% in the benralizumab treatment group and 33% in the placebo group (OR, 2.74; 95% CI, 1.41–5.31; P = 0.002).73 In a 24-week RCT of OCS-dependent severe asthma, dupilumab treatment reduced the OCS dose by 70.1% from baseline, which was significantly higher compared to placebo treatment (41.9% reduction; OR, 3.25; 95% CI, 1.90–5.55; P < 0.001).74
Risk reduction by T2-targeted biologics in terms of annual severe exacerbation rates (compared to placebo) reportedly ranged from 32% to 70% (all statistically significant) in these trials.72,73,74 However, exacerbations still occurred. The annual severe exacerbation rates were 1.44 per year in the mepolizumab treatment group (vs. 2.12 in the placebo group),72 0.54 per year in the benralizumab treatment group (vs. 1.83 in the placebo group),73 and 0.649 in the dupilumab treatment group (vs. 1.597 in the placebo group).74 The mean improvement in the ACQ score by the use of these biologics ranged between −0.52 and −0.47 (compared to placebo; all statistically significant).72,73,74 However, their benefits on pre-bronchodilator FEV1 were weaker (mean improvement range: +112 to +220 mL from baseline ; statistical significance not consistent).72,73,74
While the effects of these new biologics have only been documented after 1 year of treatment, their long-term effects are unclear. Mepolizumab maintained its beneficial effects on reduction in exacerbations over a 4-year period, but did not prevent yearly decline in FEV1,75 but there was no placebo-controlled group to determine whether the decline in FEV1 observed over the 4 years of investigation is attributed to the inability of mepolizumab to interfere with the future risk of lung function decline in severe asthmatics.
Overall, new T2-targeted biologics are promising in reducing the risk of exacerbations especially for corticosteroid-dependent asthmatics where there is a significant reduction in maintenance OCS doses. Further progress in reducing future risks will come from research into T2-low-associated mechanisms,76 which can reduce the future risks listed in this article, particularly those associated with chronic airflow obstruction and decline in lung function.
CONCLUSION
Severe asthma is a life-threatening condition. In addition to its direct impact on daily life, it may also pose a substantial burden on future health outcomes. However, the future risk is not readily measurable in daily practice and may be poorly perceived by many patients and their physicians. Patients with severe asthma are at very high risk of developing drug side effects due to high-intensity treatment requirements for controlling asthma activity. Importantly, the increased risk of OCS-induced complications is observed even at very low-dose exposures to these agents. In addition, it is not clear whether long-term OCS therapy prevents future asthma progression. Thus, controlled severe asthma is not completely being well controlled in terms of future risk. Newly developed T2-targeted biologics significantly reduce the OCS maintenance dose and exacerbation risk, and also improve asthma control status in patients with OCS-dependent severe asthma. However, their benefits are still only partial in terms of the response rate. These findings indicate that significant but unmet clinical needs remain in patients with severe asthma, even when it appears to be under control with high-intensity treatment. Further studies are warranted to develop novel treatments in order to further reduce the future risks, particularly chronic airflow obstruction and lung function decline. A practical tool to address the future risks in these patients should also be developed.
Footnotes
Disclosure: There are no financial or other issues that might lead to conflict of interest.
References
- 1.Wenzel SE, Brillhart S, Nowack K. An invisible disease: severe asthma is more than just “bad asthma”. Eur Respir J. 2017;50:1701109. doi: 10.1183/13993003.01109-2017. [DOI] [PubMed] [Google Scholar]
- 2.Foster JM, McDonald VM, Guo M, Reddel HK. “I have lost in every facet of my life”: the hidden burden of severe asthma. Eur Respir J. 2017;50:1700765. doi: 10.1183/13993003.00765-2017. [DOI] [PubMed] [Google Scholar]
- 3.Eassey D, Reddel HK, Foster JM, Kirkpatrick S, Locock L, Ryan K, et al. “…I've said I wish I was dead, you'd be better off without me”: a systematic review of people's experiences of living with severe asthma. J Asthma. 2019;56:311–322. doi: 10.1080/02770903.2018.1452034. [DOI] [PubMed] [Google Scholar]
- 4.Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43:343–373. doi: 10.1183/09031936.00202013. [DOI] [PubMed] [Google Scholar]
- 5.Hyland ME, Whalley B, Jones RC, Masoli M. A qualitative study of the impact of severe asthma and its treatment showing that treatment burden is neglected in existing asthma assessment scales. Qual Life Res. 2015;24:631–639. doi: 10.1007/s11136-014-0801-x. [DOI] [PubMed] [Google Scholar]
- 6.Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB, et al. A new perspective on concepts of asthma severity and control. Eur Respir J. 2008;32:545–554. doi: 10.1183/09031936.00155307. [DOI] [PubMed] [Google Scholar]
- 7.Bateman ED, Bousquet J, Braunstein GL. Is overall asthma control being achieved? A hypothesis-generating study. Eur Respir J. 2001;17:589–595. doi: 10.1183/09031936.01.17405890. [DOI] [PubMed] [Google Scholar]
- 8.Papaioannou AI, Kostikas K, Zervas E, Kolilekas L, Papiris S, Gaga M. Control of asthma in real life: still a valuable goal? Eur Respir Rev. 2015;24:361–369. doi: 10.1183/16000617.00001615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hekking PP, Wener RR, Amelink M, Zwinderman AH, Bouvy ML, Bel EH. The prevalence of severe refractory asthma. J Allergy Clin Immunol. 2015;135:896–902. doi: 10.1016/j.jaci.2014.08.042. [DOI] [PubMed] [Google Scholar]
- 10.Mincheva R, Ekerljung L, Bossios A, Lundbäck B, Lötvall J. High prevalence of severe asthma in a large random population study. J Allergy Clin Immunol. 2018;141:2256–2264.e2. doi: 10.1016/j.jaci.2017.07.047. [DOI] [PubMed] [Google Scholar]
- 11.Chen S, Golam S, Myers J, Bly C, Smolen H, Xu X. Systematic literature review of the clinical, humanistic, and economic burden associated with asthma uncontrolled by GINA Steps 4 or 5 treatment. Curr Med Res Opin. 2018;34:2075–2088. doi: 10.1080/03007995.2018.1505352. [DOI] [PubMed] [Google Scholar]
- 12.Silkoff PE, Laviolette M, Singh D, FitzGerald JM, Kelsen S, Backer V, et al. Longitudinal stability of asthma characteristics and biomarkers from the Airways Disease Endotyping for Personalized Therapeutics (ADEPT) study. Respir Res. 2016;17:43. doi: 10.1186/s12931-016-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim MH, Kim SH, Park SY, Ban GY, Kim JH, Jung JW, et al. Characteristics of adult severe refractory asthma in Korea analyzed from the severe asthma registry. Allergy Asthma Immunol Res. 2019;11:43–54. doi: 10.4168/aair.2019.11.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hermosa JL, Sánchez CB, Rubio MC, Mínguez MM, Walther JL. Factors associated with the control of severe asthma. J Asthma. 2010;47:124–130. doi: 10.3109/02770900903518835. [DOI] [PubMed] [Google Scholar]
- 15.Díez JM, Barcina C, Muñoz M, Leal M. Control of persistent asthma in Spain: associated factors. J Asthma. 2008;45:740–746. doi: 10.1080/02770900802216783. [DOI] [PubMed] [Google Scholar]
- 16.Turktas H, Mungan D, Uysal MA, Oguzulgen K Turkish Asthma Control Survey Study Group. Determinants of asthma control in tertiary level in Turkey: a cross-sectional multicenter survey. J Asthma. 2010;47:557–562. doi: 10.3109/02770901003692777. [DOI] [PubMed] [Google Scholar]
- 17.Yii AC, Tan JH, Lapperre TS, Chan AK, Low SY, Ong TH, et al. Long-term future risk of severe exacerbations: distinct 5-year trajectories of problematic asthma. Allergy. 2017;72:1398–1405. doi: 10.1111/all.13159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Magnoni MS, Latorre M, Bettoncelli G, Sanchez-Herrero MG, Lopez A, Calvo E, et al. Asthma control in primary care: the results of an observational cross-sectional study in Italy and Spain. World Allergy Organ J. 2017;10:13. doi: 10.1186/s40413-017-0144-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chipps BE, Haselkorn T, Paknis B, Ortiz B, Bleecker ER, Kianifard F, et al. More than a decade follow-up in patients with severe or difficult-to-treat asthma: The Epidemiology and Natural History of Asthma: Outcomes and Treatment Regimens (TENOR) II. J Allergy Clin Immunol. 2018;141:1590–1597.e9. doi: 10.1016/j.jaci.2017.07.014. [DOI] [PubMed] [Google Scholar]
- 20.Chen H, Gould MK, Blanc PD, Miller DP, Kamath TV, Lee JH, et al. Asthma control, severity, and quality of life: quantifying the effect of uncontrolled disease. J Allergy Clin Immunol. 2007;120:396–402. doi: 10.1016/j.jaci.2007.04.040. [DOI] [PubMed] [Google Scholar]
- 21.Sullivan SD, Wenzel SE, Bresnahan BW, Zheng B, Lee JH, Pritchard M, et al. Association of control and risk of severe asthma-related events in severe or difficult-to-treat asthma patients. Allergy. 2007;62:655–660. doi: 10.1111/j.1398-9995.2007.01383.x. [DOI] [PubMed] [Google Scholar]
- 22.Meltzer EO, Busse WW, Wenzel SE, Belozeroff V, Weng HH, Feng J, et al. Use of the Asthma Control Questionnaire to predict future risk of asthma exacerbation. J Allergy Clin Immunol. 2011;127:167–172. doi: 10.1016/j.jaci.2010.08.042. [DOI] [PubMed] [Google Scholar]
- 23.Bateman ED, Reddel HK, Eriksson G, Peterson S, Östlund O, Sears MR, et al. Overall asthma control: the relationship between current control and future risk. J Allergy Clin Immunol. 2010;125:600–608. 608.e1–606. doi: 10.1016/j.jaci.2009.11.033. [DOI] [PubMed] [Google Scholar]
- 24.Haselkorn T, Fish JE, Zeiger RS, Szefler SJ, Miller DP, Chipps BE, et al. Consistently very poorly controlled asthma, as defined by the impairment domain of the Expert Panel Report 3 guidelines, increases risk for future severe asthma exacerbations in The Epidemiology and Natural History of Asthma: Outcomes and Treatment Regimens (TENOR) study. J Allergy Clin Immunol. 2009;124:895–902.e1-4. doi: 10.1016/j.jaci.2009.07.035. [DOI] [PubMed] [Google Scholar]
- 25.Fuhlbrigge A, Peden D, Apter AJ, Boushey HA, Camargo CA, Jr, Gern J, et al. Asthma outcomes: exacerbations. J Allergy Clin Immunol. 2012;129:S34–48. doi: 10.1016/j.jaci.2011.12.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McDonald VM, Hiles SA, Godbout K, Harvey ES, Marks GB, Hew M, et al. Treatable traits can be identified in a severe asthma registry and predict future exacerbations. Respirology. 2019;24:37–47. doi: 10.1111/resp.13389. [DOI] [PubMed] [Google Scholar]
- 27.Bel EH, Sousa A, Fleming L, Bush A, Chung KF, Versnel J, et al. Diagnosis and definition of severe refractory asthma: an international consensus statement from the Innovative Medicine Initiative (IMI) Thorax. 2011;66:910–917. doi: 10.1136/thx.2010.153643. [DOI] [PubMed] [Google Scholar]
- 28.Miller MK, Lee JH, Miller DP, Wenzel SE TENOR Study Group. Recent asthma exacerbations: a key predictor of future exacerbations. Respir Med. 2007;101:481–489. doi: 10.1016/j.rmed.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 29.Calhoun WJ, Haselkorn T, Mink DR, Miller DP, Dorenbaum A, Zeiger RS. Clinical burden and predictors of asthma exacerbations in patients on guideline-based steps 4–6 asthma therapy in the TENOR cohort. J Allergy Clin Immunol Pract. 2014;2:193–200. doi: 10.1016/j.jaip.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 30.Tanaka A, Uno T, Sato H, Jinno M, Hirai K, Miyata Y, et al. Predicting future risk of exacerbations in Japanese patients with adult asthma: a prospective 1-year follow up study. Allergol Int. 2017;66:568–573. doi: 10.1016/j.alit.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 31.Kang HR, Song HJ, Nam JH, Hong SH, Yang SY, Ju S, et al. Risk factors of asthma exacerbation based on asthma severity: a nationwide population-based observational study in South Korea. BMJ Open. 2018;8:e020825. doi: 10.1136/bmjopen-2017-020825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boer S, Sont JK, Loijmans RJ, Snoeck-Stroband JB, ter Riet G, Schermer TR, et al. Development and validation of personalized prediction to estimate future risk of severe exacerbations and uncontrolled asthma in patients with asthma, using clinical parameters and early treatment response. J Allergy Clin Immunol Pract. 2019;7:175–182.e5. doi: 10.1016/j.jaip.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Bloom CI, Palmer T, Feary J, Quint JK, Cullinan P. Exacerbation patterns in adults with asthma in England. a population-based study. Am J Respir Crit Care Med. 2019;199:446–453. doi: 10.1164/rccm.201808-1516OC. [DOI] [PubMed] [Google Scholar]
- 34.Patel M, Pilcher J, Reddel HK, Qi V, Mackey B, Tranquilino T, et al. Predictors of severe exacerbations, poor asthma control, and β-agonist overuse for patients with asthma. J Allergy Clin Immunol Pract. 2014;2:751–758. doi: 10.1016/j.jaip.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 35.Loymans RJ, Honkoop PJ, Termeer EH, Snoeck-Stroband JB, Assendelft WJ, Schermer TR, et al. Identifying patients at risk for severe exacerbations of asthma: development and external validation of a multivariable prediction model. Thorax. 2016;71:838–846. doi: 10.1136/thoraxjnl-2015-208138. [DOI] [PubMed] [Google Scholar]
- 36.Park HW, Song WJ, Kim SH, Park HK, Kim SH, Kwon YE, et al. Classification and implementation of asthma phenotypes in elderly patients. Ann Allergy Asthma Immunol. 2015;114:18–22. doi: 10.1016/j.anai.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 37.Bateman ED, Buhl R, O'Byrne PM, Humbert M, Reddel HK, Sears MR, et al. Development and validation of a novel risk score for asthma exacerbations: the risk score for exacerbations. J Allergy Clin Immunol. 2015;135:1457–1464.e4. doi: 10.1016/j.jaci.2014.08.015. [DOI] [PubMed] [Google Scholar]
- 38.Kupczyk M, ten Brinke A, Sterk PJ, Bel EH, Papi A, Chanez P, et al. Frequent exacerbators--a distinct phenotype of severe asthma. Clin Exp Allergy. 2014;44:212–221. doi: 10.1111/cea.12179. [DOI] [PubMed] [Google Scholar]
- 39.Song WJ, Sintobin I, Sohn KH, Kang MG, Park HK, Jo EJ, et al. Staphylococcal enterotoxin IgE sensitization in late-onset severe eosinophilic asthma in the elderly. Clin Exp Allergy. 2016;46:411–421. doi: 10.1111/cea.12652. [DOI] [PubMed] [Google Scholar]
- 40.Bloom CI, Nissen F, Douglas IJ, Smeeth L, Cullinan P, Quint JK. Exacerbation risk and characterisation of the UK's asthma population from infants to old age. Thorax. 2018;73:313–320. doi: 10.1136/thoraxjnl-2017-210650. [DOI] [PubMed] [Google Scholar]
- 41.Mukherjee M, Nair P. Autoimmune responses in severe asthma. Allergy Asthma Immunol Res. 2018;10:428–447. doi: 10.4168/aair.2018.10.5.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pavord ID, Korn S, Howarth P, Bleecker ER, Buhl R, Keene ON, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380:651–659. doi: 10.1016/S0140-6736(12)60988-X. [DOI] [PubMed] [Google Scholar]
- 43.Ortega HG, Yancey SW, Mayer B, Gunsoy NB, Keene ON, Bleecker ER, et al. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: a secondary analysis of the DREAM and MENSA studies. Lancet Respir Med. 2016;4:549–556. doi: 10.1016/S2213-2600(16)30031-5. [DOI] [PubMed] [Google Scholar]
- 44.Hanania NA, Wenzel S, Rosén K, Hsieh HJ, Mosesova S, Choy DF, et al. Exploring the effects of omalizumab in allergic asthma: an analysis of biomarkers in the EXTRA study. Am J Respir Crit Care Med. 2013;187:804–811. doi: 10.1164/rccm.201208-1414OC. [DOI] [PubMed] [Google Scholar]
- 45.Wenzel S, Swanson B, Teper A, Hamilton J, Izuhara K, Ohta S, et al. Dupilumab reduces severe exacerbations in periostin-high and periostin-low asthma patients. Eur Respir J. 2016;48:OA1798 [Google Scholar]
- 46.Newby C, Agbetile J, Hargadon B, Monteiro W, Green R, Pavord I, et al. Lung function decline and variable airway inflammatory pattern: longitudinal analysis of severe asthma. J Allergy Clin Immunol. 2014;134:287–294. doi: 10.1016/j.jaci.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 47.American Thoracic Society. Proceedings of the ATS workshop on refractory asthma: current understanding, recommendations, and unanswered questions. Am J Respir Crit Care Med. 2000;162:2341–2351. doi: 10.1164/ajrccm.162.6.ats9-00. [DOI] [PubMed] [Google Scholar]
- 48.Matsunaga K, Akamatsu K, Miyatake A, Ichinose M. Natural history and risk factors of obstructive changes over a 10-year period in severe asthma. Respir Med. 2013;107:355–360. doi: 10.1016/j.rmed.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 49.Almeida PC, Ponte EV, Souza-Machado A, Cruz AA. Longitudinal trends in clinical characteristics and lung function of patients with severe asthma under treatment in Brazil. BMC Pulm Med. 2016;16:141. doi: 10.1186/s12890-016-0302-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fardet L, Petersen I, Nazareth I. Prevalence of long-term oral glucocorticoid prescriptions in the UK over the past 20 years. Rheumatology (Oxford) 2011;50:1982–1990. doi: 10.1093/rheumatology/ker017. [DOI] [PubMed] [Google Scholar]
- 51.van Staa TP, Leufkens HG, Abenhaim L, Begaud B, Zhang B, Cooper C. Use of oral corticosteroids in the United Kingdom. QJM. 2000;93:105–111. doi: 10.1093/qjmed/93.2.105. [DOI] [PubMed] [Google Scholar]
- 52.Overman RA, Yeh JY, Deal CL. Prevalence of oral glucocorticoid usage in the United States: a general population perspective. Arthritis Care Res (Hoboken) 2013;65:294–298. doi: 10.1002/acr.21796. [DOI] [PubMed] [Google Scholar]
- 53.Sarnes E, Crofford L, Watson M, Dennis G, Kan H, Bass D. Incidence and US costs of corticosteroid-associated adverse events: a systematic literature review. Clin Ther. 2011;33:1413–1432. doi: 10.1016/j.clinthera.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 54.Rice JB, White AG, Scarpati LM, Wan G, Nelson WW. Long-term systemic corticosteroid exposure: a systematic literature review. Clin Ther. 2017;39:2216–2229. doi: 10.1016/j.clinthera.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 55.Lefebvre P, Duh MS, Lafeuille MH, Gozalo L, Desai U, Robitaille MN, et al. Acute and chronic systemic corticosteroid-related complications in patients with severe asthma. J Allergy Clin Immunol. 2015;136:1488–1495. doi: 10.1016/j.jaci.2015.07.046. [DOI] [PubMed] [Google Scholar]
- 56.Dalal AA, Duh MS, Gozalo L, Robitaille MN, Albers F, Yancey S, et al. Dose-response relationship between long-term systemic corticosteroid use and related complications in patients with severe asthma. J Manag Care Spec Pharm. 2016;22:833–847. doi: 10.18553/jmcp.2016.22.7.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sullivan PW, Ghushchyan VH, Globe G, Schatz M. Oral corticosteroid exposure and adverse effects in asthmatic patients. J Allergy Clin Immunol. 2018;141:110–116.e7. doi: 10.1016/j.jaci.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 58.Sweeney J, Patterson CC, Menzies-Gow A, Niven RM, Mansur AH, Bucknall C, et al. Comorbidity in severe asthma requiring systemic corticosteroid therapy: cross-sectional data from the Optimum Patient Care Research Database and the British Thoracic Difficult Asthma Registry. Thorax. 2016;71:339–346. doi: 10.1136/thoraxjnl-2015-207630. [DOI] [PubMed] [Google Scholar]
- 59.Barry LE, O'Neill C, Patterson C, Sweeney J, Price D, Heaney LG. Age and sex associations with systemic corticosteroid-induced morbidity in asthma. J Allergy Clin Immunol Pract. 2018;6:2014–2023.e2. doi: 10.1016/j.jaip.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 60.Bloechliger M, Reinau D, Spoendlin J, Chang SC, Kuhlbusch K, Heaney LG, et al. Adverse events profile of oral corticosteroids among asthma patients in the UK: cohort study with a nested case-control analysis. Respir Res. 2018;19:75. doi: 10.1186/s12931-018-0742-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Daugherty J, Lin X, Baxter R, Suruki R, Bradford E. The impact of long-term systemic glucocorticoid use in severe asthma: a UK retrospective cohort analysis. J Asthma. 2018;55:651–658. doi: 10.1080/02770903.2017.1353612. [DOI] [PubMed] [Google Scholar]
- 62.Price DB, Trudo F, Voorham J, Xu X, Kerkhof M, Ling Zhi Jie J, et al. Adverse outcomes from initiation of systemic corticosteroids for asthma: long-term observational study. J Asthma Allergy. 2018;11:193–204. doi: 10.2147/JAA.S176026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Heffler E, Madeira LN, Ferrando M, Puggioni F, Racca F, Malvezzi L, et al. Inhaled corticosteroids safety and adverse effects in patients with asthma. J Allergy Clin Immunol Pract. 2018;6:776–781. doi: 10.1016/j.jaip.2018.01.025. [DOI] [PubMed] [Google Scholar]
- 64.Wong CA, Walsh LJ, Smith CJ, Wisniewski AF, Lewis SA, Hubbard R, et al. Inhaled corticosteroid use and bone-mineral density in patients with asthma. Lancet. 2000;355:1399–1403. doi: 10.1016/S0140-6736(00)02138-3. [DOI] [PubMed] [Google Scholar]
- 65.Choi YJ, Lee HY, Yoon D, Kim A, Shin YS, Park HS, et al. Trabecular bone score is more sensitive to asthma severity and glucocorticoid treatment than bone mineral density in asthmatics. Allergy Asthma Immunol Res. 2019;11:343–356. doi: 10.4168/aair.2019.11.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Weatherall M, James K, Clay J, Perrin K, Masoli M, Wijesinghe M, et al. Dose-response relationship for risk of non-vertebral fracture with inhaled corticosteroids. Clin Exp Allergy. 2008;38:1451–1458. doi: 10.1111/j.1365-2222.2008.03029.x. [DOI] [PubMed] [Google Scholar]
- 67.Garbe E, Suissa S, LeLorier J. Association of inhaled corticosteroid use with cataract extraction in elderly patients. JAMA. 1998;280:539–543. doi: 10.1001/jama.280.6.539. [DOI] [PubMed] [Google Scholar]
- 68.Bourdin A, Molinari N, Vachier I, Pahus L, Suehs C, Chanez P. Mortality: a neglected outcome in OCS-treated severe asthma. Eur Respir J. 2017;50:1701486. doi: 10.1183/13993003.01486-2017. [DOI] [PubMed] [Google Scholar]
- 69.Bourdin A, Fabry-Vendrand C, Ostinelli J, Ait-Yahia M, Darnal E, Bouee S, et al. The burden of severe asthma in France: a case-control study using a medical claims database. J Allergy Clin Immunol Pract. 2019;7:1477–1487. doi: 10.1016/j.jaip.2018.12.029. [DOI] [PubMed] [Google Scholar]
- 70.Fernandes AG, Souza-Machado C, Coelho RC, Franco PA, Esquivel RM, Souza-Machado A, et al. Risk factors for death in patients with severe asthma. J Bras Pneumol. 2014;40:364–372. doi: 10.1590/S1806-37132014000400003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fajt ML, Wenzel SE. Development of new therapies for severe asthma. Allergy Asthma Immunol Res. 2017;9:3–14. doi: 10.4168/aair.2017.9.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bel EH, Wenzel SE, Thompson PJ, Prazma CM, Keene ON, Yancey SW, et al. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N Engl J Med. 2014;371:1189–1197. doi: 10.1056/NEJMoa1403291. [DOI] [PubMed] [Google Scholar]
- 73.Nair P, Wenzel S, Rabe KF, Bourdin A, Lugogo NL, Kuna P, et al. Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N Engl J Med. 2017;376:2448–2458. doi: 10.1056/NEJMoa1703501. [DOI] [PubMed] [Google Scholar]
- 74.Rabe KF, Nair P, Brusselle G, Maspero JF, Castro M, Sher L, et al. Efficacy and safety of dupilumab in glucocorticoid-dependent severe asthma. N Engl J Med. 2018;378:2475–2485. doi: 10.1056/NEJMoa1804093. [DOI] [PubMed] [Google Scholar]
- 75.Khatri S, Moore W, Gibson PG, Leigh R, Bourdin A, Maspero J, et al. Assessment of the long-term safety of mepolizumab and durability of clinical response in patients with severe eosinophilic asthma. J Allergy Clin Immunol. 2019;143:1742–1751.e7. doi: 10.1016/j.jaci.2018.09.033. [DOI] [PubMed] [Google Scholar]
- 76.Chung KF, Adcock IM. Precision medicine for the discovery of treatable mechanisms in severe asthma. Allergy. 2019 doi: 10.1111/all.13771. [DOI] [PubMed] [Google Scholar]
- 77.Zazzali JL, Broder MS, Omachi TA, Chang E, Sun GH, Raimundo K. Risk of corticosteroid-related adverse events in asthma patients with high oral corticosteroid use. Allergy Asthma Proc. 2015;36:268–274. doi: 10.2500/aap.2015.36.3863. [DOI] [PubMed] [Google Scholar]
- 78.Lefebvre P, Duh MS, Lafeuille MH, Gozalo L, Desai U, Robitaille MN, et al. Burden of systemic glucocorticoid-related complications in severe asthma. Curr Med Res Opin. 2017;33:57–65. doi: 10.1080/03007995.2016.1233101. [DOI] [PubMed] [Google Scholar]