Abstract
Postural tachycardia syndrome (POTS) can cause orthostatic headache. However, it is difficult to differentiate POTS from spontaneous intracranial hypotension (SIH) caused by cerebrospinal fluid (CSF) leaks. We herein report a 53-year-old woman who presented with SIH associated with POTS. A cervicothoracic and lumbar epidural blood patch rapidly improved not only the headache but also the orthostatic tachycardia, suggesting POTS secondary to SIH. This case suggests that a CSF leak can cause secondary POTS. Therefore, POTS should be considered in patients with orthostatic headaches, even in the presence of a CSF leak.
Keywords: orthostatic headache, spontaneous intracranial hypotension, postural tachycardia syndrome, cerebrospinal fluid-blood gradient
Introduction
Most orthostatic headaches are caused by intracranial hypotension following cerebrospinal fluid (CSF) leaks (1), although postural tachycardia syndrome (POTS), a form of dysautonomia, is also causative (2). POTS is defined as a >30-beats per min (bpm) increase in heart rate, or an absolute heart rate >120 bpm, within 10 minutes from the supine position in the absence of hypotension, arrhythmias, sympathomimetic drugs or other condition (3). However, it is difficult to differentiate POTS from spontaneous intracranial hypotension (SIH), which may show positional tachycardia to compensate for intracranial hypotension (4). At present, these disorders are considered distinct entities.
We herein report a case of SIH associated with POTS.
Case Report
A 53-year-old woman suddenly developed an explosive headache while picking mandarins. The severe headache spontaneously subsided after several hours, but dull occipital pain with intermittent throbbing continued, and she was admitted to our hospital. She had a history of menstrual-related migraine without aura and severe cough for two weeks. As physical and radiological examination findings were unremarkable, loxoprofen was prescribed.
A week later, she felt gradual worsening of holocephalic headaches. Sitting upright worsened her headache, lightheadedness, and neck pain. Her symptoms were more severe in the evening than at other times of day. Repeated brain magnetic resonance imaging and cisternography findings were normal. As SIH was clinically suspected, conservative treatment with saline infusion was started. Theophylline (100 mg per day) was initiated, but it exacerbated her lightheadedness. Active standing tests showed a significant heart rate increase (68 bpm during supine position, 109 bpm during standing), while her blood pressure was 122/78 mmHg in the spine position and 129/77 mmHg while standing. These findings were consistent with POTS (3). Elastic compression stockings and an increase in salt and fluid intake slightly reduced her headache symptoms, although excessive tachycardia on standing continued.
One month later, the patient developed bilateral tinnitus, and an audiogram revealed especially low-frequency bilateral hearing loss. Gadolinium-enhanced brain magnetic resonance imaging revealed diffuse dural enhancement (Fig. 1). To determine the leakage point, 111In-diethylenetriamine pentaacetic acid cisternography was performed. The cerebral spinal fluid (CSF) opening pressure was 0 mmH2O. Appearance of the tracer in the urinary bladder was confirmed as early as 30 minutes after injection, and the majority of the tracer had disappeared by 24 hours (Fig. 2). At 1 and 3 hours, CSF leaks were suspected in the cervical areas (Fig. 2, arrows). Based on these findings, the patient was diagnosed with SIH. A cervicothoracic (C7/Th7) and lumbar (L1/2) epidural blood patch was performed. Active standing tests the following day showed a postural increase of 24 bpm (heart rate: from 78 to 102 bpm) on standing without orthostatic hypotension, suggesting an improvement in POTS. One week after the procedure, the patient was free from headache. Two months after the procedure, the patient did not show postural tachycardia and remained free from headache, and she had returned to her job and previous level of physical activity.
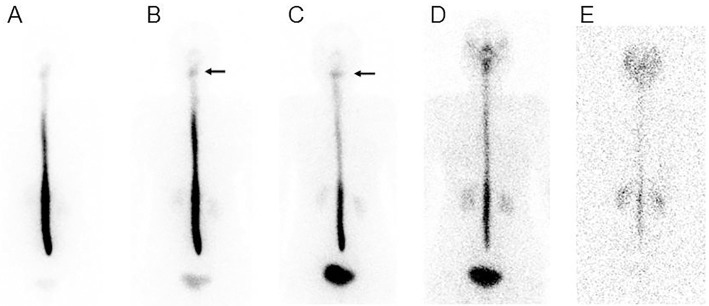
Figure 1.
T1-weighted magnetic resonance imaging with contrast enhancement. Thickening and enhancement of the dura were noted.
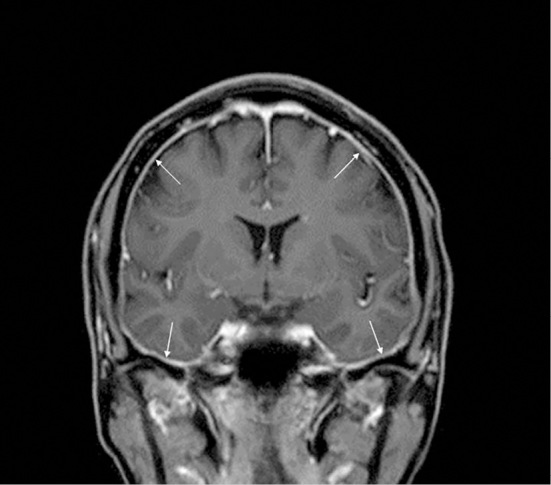
Figure 2.
111In-DTPA cisternogram at 30 min (A) and 1 (B), 3 (C), 6 (D), and 24 h (E). RI began to accumulate in the bladder as early as 30 min after intrathecal injection, suggesting a cerebrospinal fluid leak from the intrathecal space. At 1 and 3 h, the marked accumulation of the tracer was observed at the cervical areas (arrows). At 24 h, there were very low levels of the tracer in the intrathecal space.
Discussion
We herein report a patient with SIH associated with POTS. As theophylline exacerbated her lightheadedness, we performed autonomic testing, despite the potential for increasing the CSF production (5,6). We considered that POTS was secondary to SIH in this case, as her orthostatic tachycardia promptly improved after an epidural blood patch.
SIH is traditionally attributed to occult CSF leak (7). However, Franzini et al. proposed that a reduced inferior vena cava pressure could cause epidural hypotension via over-drainage of venous blood from the epidural spinal network and CSF (8). This concept is supported by the fact that a ‘lumbar’ epidural patch is effective, even if a CSF leak is shown in the cervical area (8). As such, reducing the inferior vena cava pressure may decrease the venous return and cause a compensatory rise in the heart rate when standing upright (9). Thus, there is potential for SIH patients to exhibit POTS.
SIH and POTS may have a common pathophysiology. In 1938, Schaltenbrand, using the term ‘aliquorrhea’, described orthostatic headache associated with low CSF pressure (10). This later came to be known as SIH. He reasoned that aliquorrhea syndrome resulted from the disturbance of the choroid plexus, possibly of vasomotor origin (10). Dysautonomia may thus underlie both SIH and POTS.
Although the present case might have merely developed secondary POTS as a result of deconditioning due to SIH, it is feasible to consider that a CSF leak caused secondary POTS. Although there are few reports on the co-occurrence of SIH and POTS, POTS should be suspected in patients with orthostatic headaches even in the presence of a CSF leak. Further studies examining the pathological mechanisms of SIH and POTS are warranted.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Mokri B. Spontaneous cerebrospinal fluid leaks: from intracranial hypotension to cerebrospinal fluid hypovolemia-evolution of a concept. Mayo Clin Proc 74: 1113-1123, 1999. [DOI] [PubMed] [Google Scholar]
- 2. Mokri B, Low PA. Orthostatic headaches without CSF leak in postural tachycardia syndrome. Neurology 61: 980-982, 2003. [DOI] [PubMed] [Google Scholar]
- 3. Freeman R, Wieling W, Axelrod FB, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton Neurosci 161: 46-48, 2011. [DOI] [PubMed] [Google Scholar]
- 4. Schievink WI, Deline CR. Headache secondary to intracranial hypotension. Curr Pain Headache Rep 18: 457, 2014. [DOI] [PubMed] [Google Scholar]
- 5. Feuerstein TJ, Zeides A. Theophylline relieves headache following lumbar puncture. Placebo-controlled, double-blind pilot study. Klin Wochenschr 64: 216-218, 1986. [DOI] [PubMed] [Google Scholar]
- 6. Han ME, Kim HJ, Lee YS, et al. Regulation of cerebrospinal fluid production by caffeine consumption. BMC Neurosci 10: 110, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rahman M, Bidari SS, Quisling RG, Friedman WA. Spontaneous intracranial hypotension: dilemmas in diagnosis. Neurosurgery 69: 4-14, 2011. [DOI] [PubMed] [Google Scholar]
- 8. Franzini A, Messina G, Nazzi V, et al. Spontaneous intracranial hypotension syndrome: a novel speculative physiopathological hypothesis and a novel patch method in a series of 28 consecutive patients. J Neurosurg 112: 300-306, 2010. [DOI] [PubMed] [Google Scholar]
- 9. Mathias CJ, Low DA, Iodice V, Owens AP, Kirbis M, Grahame R. Postural tachycardia syndrome-current experience and concepts. Nat Rev Neurol 8: 22-34, 2011. [DOI] [PubMed] [Google Scholar]
- 10. Schaltenbrand.. Normal and pathological physiology of the cerebrospinal fluid circulation. Lancet 1: 805-808, 1953. [DOI] [PubMed] [Google Scholar]