Abstract
Schistosomiasis infection is a major cause of morbidity and mortality in endemic areas. Developed countries have declared that schistosomiasis has been eradicated; however, residents of these countries may travel and stay in endemic areas and the number of foreign travelers is increasing in the recent years. Thus, schistosomiasis is regarded as an imported infection. Ultrasonography and serum antibody titer tests are well established as diagnostic methods for schistosomiasis. However, a definitive diagnosis cannot be obtained using these tests in some cases. We herein report a case in which schistosomiasis was confirmed based on laparoscopic liver biopsy without a definitive diagnosis by blood test, fecal examination, or imaging.
Keywords: laparoscopic liver biopsy, outside transmission areas, schistosomiasis, travelers, infection
Introduction
Schistosomiasis is a parasitic infection caused by trematodes of the genus Schistosoma that is acquired upon contact with freshwater bodies contaminated with larvae of these parasites. Approximately >200 million people are infected by schistosomes worldwide. Infection causes either the urinary or intestinal form of the disease, resulting in >200 thousand deaths per year, mostly in Sub-Saharan Africa (1,2). Imported schistosomiasis in migrants and travelers returning from endemic areas has been defined as a “hidden epidemic” in receiving developed countries (3). It is pathologically caused by eggs released by female parasites residing in the venous plexus draining the large intestine, which are then trapped in the bowel wall and the liver (4). Morbidity and mortality due to advanced hepatic involvement resulting in liver fibrosis and portal hypertension are well recognized and described (5). A standardized protocol for evaluating and grading hepatic schistosomiasis using ultrasonography (US) was issued by the World Health Organization in 2000 and was evaluated for usability and usefulness (6). However, in some cases a definitive diagnosis cannot be obtained using US and a schistosomiasis serum antibody titer test.
To our knowledge, this is the first case of schistosomiasis confirmed using laparoscopic liver biopsy without a definitive diagnosis by blood test, fecal egg examination, or abdominal imaging.
Case Report
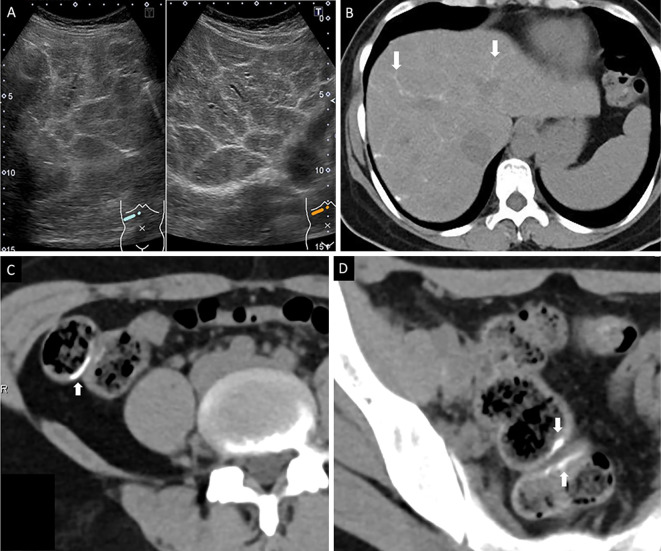
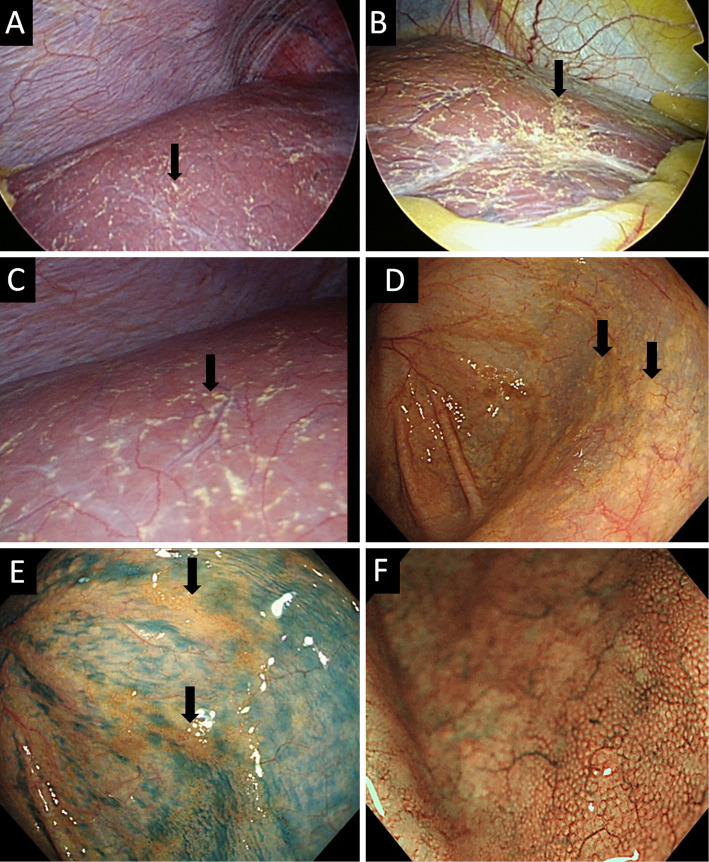
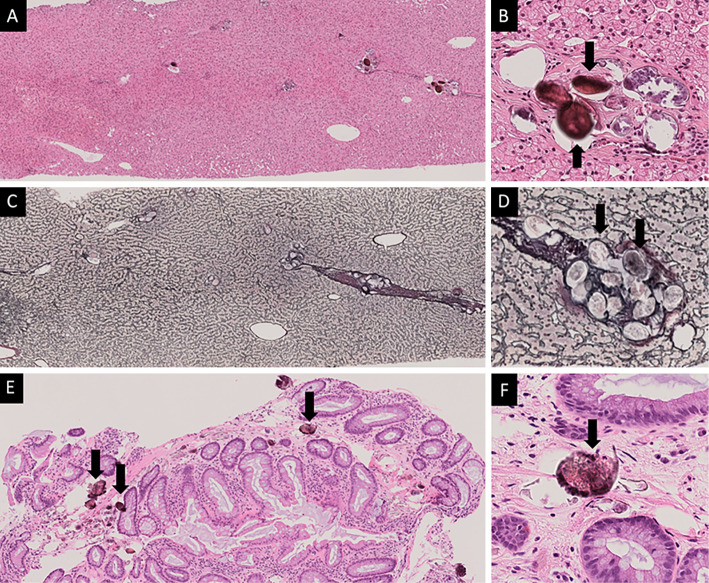
The patient was a 39-year-old woman from the Philippines who had migrated to Japan approximately 15 years previously. Six years previously, during her most recent trip to the Philippines, she performed agricultural work in paddy fields. She was admitted to our hospital because of fever and fatigue that persisted for more than 1 month. A blood test during her visit to our hospital revealed an abnormal liver function (total bilirubin, 0.5 mg/dL; aspartate aminotransferase, 60 U/L; alanine aminotransferase, 75 U/L; and gamma-glutamyl transferase, 65 U/L). US and computed tomography (CT) showed calcification along the hepatic limbus and portal vein (Fig. 1A and B) as well as in the ascending colon (Fig. 1C), sigmoid colon, and rectal wall (Fig. 1D). Schistosomiasis was therefore suspected. Table shows the blood test findings upon admission. A fecal inspection revealed no parasite eggs, and her schistosomiasis parasite egg antibody level was 0.135 (positive cut-off value, 0.200; negative cut-off value, <0.100). Thus, the antibody test was not definitively negative and was considered to be borderline positive. Hepatic angiography was performed; no findings suggestive of portal hypertension were noted and the hepatic venous pressure gradient was 1.8 mmHg. A liver stiffness measurement performed using a FibroscanⓇ device showed a value of 3.8 kPa. Based on the previously reported cut-off value for chronic liver disease (7), there were no findings consistent with the development of liver fibrosis. Thus, schistosomiasis was suspected based on her life history and the imaging findings. However, although the US findings were typical of schistosomiasis, fecal and serological examinations did not provide sufficient evidence for a diagnosis. A laparoscopic liver biopsy was therefore performed. The laparoscopic liver biopsy revealed yellow nodules on the liver surface that were suspected to be parasite eggs (Fig. 2A-C). In addition, although the fecal examination revealed no parasite eggs, colonoscopy showed widespread yellow granular areas from the cecum to the rectum, which was consistent with the laparoscopy findings (Fig. 2D-F). The examination of the liver biopsy specimen revealed parasite eggs in the portal region, mild inflammation around the portal vein, and no expansion of the portal region or fibrosis (Fig. 3A-D). The examination of the colon biopsy specimen revealed numerous calcifications in the lamina propria that were suspected to be insect eggs (Fig. 3E and F). Thus, the patient was diagnosed with schistosomiasis based on the confirmed presence of parasite eggs in the liver tissue. Praziquantel (40 mg/kg/day) was immediately administered. After starting the treatment, her symptoms improved, and her transaminase level normalized after 4 weeks.
Figure 1.
The abdominal ultrasonography (US) and computed tomography (CT) findings. (A) US (B-mode) revealed a network calcification pattern (white arrows). (B) Non-contrast computed tomography showed calcification along the liver vessel. (C) CT showed calcification in the ascending colon. (D) CT showed calcification in the rectal wall.
Table.
Patient Characteristics.
| White blood cell count | 6,700 | /µL | AST | 27 | U/L | IgG | 1,240 | mg/dL | |||||
| Neutrophils | 63.2 | % | ALT | 63 | U/L | IgA | 252 | mg/dL | |||||
| Lymphocyte | 28.9 | % | LDH | 204 | U/L | IgM | 55 | mg/dL | |||||
| Monocyte | 4.3 | % | ALP | 246 | U/L | IgE | 1,000 | mg/dL | |||||
| Eosinophil | 3.3 | % | GGT | 56 | U/L | HBsAg | Negative | ||||||
| Hemoglobin | 12.4 | g/dL | Ammonia | 24 | µg/dL | Anti-HBc | Negative | ||||||
| Platelet count | 27.7×104 | /μL | BUN | 8 | mg/dL | Anti-HCV | Negative | ||||||
| Prothrombin time | 102 | % | Creatinine | 0.48 | mg/dL | Fecal parasite egg | Negative | ||||||
| Total protein | 6.5 | g/dL | Na | 140 | mEq/L | Schistosomiasis parasite egg antibody | 0.135 | ||||||
| Serum albumin | 3.9 | g/dL | K | 4.7 | mEq/L | ||||||||
| Total bilirubin | 0.4 | mg/dL | Cl | 104 | mEq/L | ||||||||
AST: aspartate aminotransferase, ALT: alanine aminotransferase, LDH: lactate dehydrogenase, ALP: alkaline phosphatase, GGT: gamma-glutamyl transferase, BUN: blood urea nitrogen, Na: sodium, K: potassium, CL: chlorine, IgG: Immunoglobulin G, IgA: Immunoglobulin A, IgM: Immunoglobulin M, IgE: Immunoglobulin E, HBsAg: hepatitis B surface antigen, Anti-HBc: hepatitis B core antibody, Anti-HCV: hepatitis C virus antibody
Figure 2.
The laparoscopic and endoscopic findings. (A) A distant view of the right liver lobe. Yellowish-tinged nodules (black arrows) that were suspected to be parasite eggs were seen diffusely on the liver surface. (B) A distant view of the left liver lobe. Yellow nodules that were suspected to be parasite eggs were seen (black arrow). (C) A proximal view of the right liver lobe. Yellow nodules that were suspected to be parasite eggs were seen (black arrow). (D) The ascending colon. As with laparoscopy, endoscopy revealed that the yellow granular parts were interspersed (black arrow). (E) After spraying indigo carmine, a yellow nodule could be clearly observed (black arrow). The mucosal surface was normal. (F) Narrow band imaging (NBI).
Figure 3.
The pathological examination of the liver and colon specimens. A-D show the findings of the pathological examination of the liver specimen. A and B show Hematoxylin and Eosin staining sections. C and D show silver impregnation-stained sections. (A) Inflammation around the portal vein was mild. No interface hepatitis was noted. (B) A parasite egg was observed in the portal region (black arrow). (C) No portal region expansion or fibrosis were seen. (D) A high-power view of the portal region. Parasite eggs were clearly observed in the portal vein (black arrow). E and F show the findings of the pathological examination of the colon specimen. (E) An image of the biopsy specimen obtained from the ascending colon. Calcification of the mucosal lamina propria (black arrow). No granulomas were observed. (F) A high-power image of the lamina propria. Parasite eggs were clearly observed in the lamina propria (black arrow).
Discussion
Schistosomiasis usually causes acute serum abnormalities, associated with the onset of egg laying by the female parasite (approximately 5 weeks post-infection) and granuloma formation around the eggs trapped in the liver and intestinal wall (8). Schistosomiasis is associated with hepatosplenomegaly and leukocytosis with eosinophilia; this phase of infection is often asymptomatic, but symptoms include fever, nausea, headache, irritating cough, and in extreme cases, diarrhea accompanied with blood, mucus, and necrotic material. These symptoms, if present, last from a few weeks to several months (8). In Japan, schistosomiasis was once prevalent in certain areas including the Kofu Basin, Kyushu, and Shizuoka; however, there have been no new cases since 1978, and a declaration of eradication was issued. However, the number of Japanese people traveling to and staying in endemic areas and foreign visitors to Japan have increased in recent years. Thus, the significance of schistosomiasis as an imported infectious disease has been recognized (9).
In patients with schistosomiasis, US and CT typically show characteristic findings, including a “network pattern of calcification” on US and a “turtle-back” pattern on non-contrast CT (10). In this case, intrahepatic calcification was observed on US and CT. The differential diagnoses include various diseases that cause intrahepatic calcification (e.g., past liver injury, hepatic tuberculosis, parasite, and bleeding). Schistosomiasis was suspected because of these imaging findings and the patient's life history. However, a fecal examination and blood test did not lead to a definite diagnosis. The presence of egg nodules and parasite eggs in the liver tissues was confirmed by performing a laparoscopic liver biopsy, which was useful for making a definitive diagnosis of schistosomiasis. We herein report the case in which schistosomiasis was diagnosed based on the findings of a laparoscopic examination when a fecal examination and blood test results were negative.
In conclusion, laparoscopic liver biopsy is useful for the diagnosis of schistosomiasis when the results of fecal and serological examinations are inconclusive.
The authors state that they have no Conflict of Interest (COI).
References
- 1. WHO.. Schistosomiasis and soil-transmitted helminthiases: number of people treated in 2016. Wkly Epidemiol Rec 92: 749-760, 2017. [PubMed] [Google Scholar]
- 2. Steinmann P, Keiser J, Bos R, Tanner M, Utzinger J. Schistosomiasis and water resources development: systematic review, meta-analysis, and estimates of people at risk. Lancet Infect Dis 6: 411-425, 2006. [DOI] [PubMed] [Google Scholar]
- 3. Beltrame A, Buonfrate D, Gobbi F, et al. . The hidden epidemic of schistosomiasis in recent African immigrants and asylum seekers to Italy. Eur J Epidemiol 32: 733-735, 2017. [DOI] [PubMed] [Google Scholar]
- 4. Colley DG, Bustinduy AL, Secor WE, King CH. Human schistosomiasis. Lancet 383: 2253-2264, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van der Werf MJ, de Vlas SJ, Brooker S, et al. . Quantification of clinical morbidity associated with schistosome infection in sub-Saharan Africa. Acta Trop 86: 125-139, 2003. [DOI] [PubMed] [Google Scholar]
- 6. el Scheich T, Holtfreter MC, Ekamp H, et al. . The WHO ultrasonography protocol for assessing hepatic morbidity due to Schistosoma mansoni. Acceptance and evolution over 12 years. Parasitol Res 113: 3915-3925, 2014. [DOI] [PubMed] [Google Scholar]
- 7. Ferraioli G, Filice C, Castera L, et al. . WFUMB guidelines and recommendations for clinical use of ultrasound elastography: part 3: liver. Ultrasound Med Biol 41: 1161-1179, 2015. [DOI] [PubMed] [Google Scholar]
- 8. Ishii A, Tsuji M, Tada I. History of Katayama disease: schistosomiasis japonica in Katayama district, Hiroshima, Japan. Parasitol Int 52: 313-319, 2003. [DOI] [PubMed] [Google Scholar]
- 9. Machida K, Yamada T, Shimura E, et al. . Schistosomiasis japonica in a patient who emigrated from China: a case report. Nippon Shokakibyo Gakkai Zasshi 115: 1094-1100, 2018(in Japanese, Abstract in English). [DOI] [PubMed] [Google Scholar]
- 10. Cheung H, Lai YM, Loke TK, et al. . The imaging diagnosis of hepatic schistosomiasis japonicum sequelae. Clin Radiol 51: 51-55, 1996. [DOI] [PubMed] [Google Scholar]