We report patient-to-patient transmission of Enterobacter hormaechei isolates with reduced susceptibility to ceftazidime-avibactam due to production of KPC-40, a variant of KPC-3 with a two-amino-acid insertion in the Ω-loop region (L167_E168dup). The index patient had received a prolonged course of ceftazidime-avibactam therapy, whereas the second patient had not received the agent and still became colonized with the KPC-40-producing strain.
KEYWORDS: Enterobacter cloacae complex, avibactam, omega loop
ABSTRACT
We report patient-to-patient transmission of Enterobacter hormaechei isolates with reduced susceptibility to ceftazidime-avibactam due to production of KPC-40, a variant of KPC-3 with a two-amino-acid insertion in the Ω-loop region (L167_E168dup). The index patient had received a prolonged course of ceftazidime-avibactam therapy, whereas the second patient had not received the agent and still became colonized with the KPC-40-producing strain. The complex dynamics of KPC (Klebsiella pneumoniae carbapenemase) described here highlight several key diagnostic and therapeutic considerations.
TEXT
KPC (Klebsiella pneumoniae carbapenemase)-producing Enterobacteriales strains are endemic in hospitals in certain regions of the United States. While Klebsiella pneumoniae is the predominant species, KPC is increasingly produced by other Gram-negative species due to the spread of KPC enzymes carried on mobile genetic elements (1, 2). Mortality from infections caused by these organisms has been high but has improved significantly with the advent of newer β-lactam–β-lactamase combinations, including ceftazidime-avibactam, which possess activity against KPC-producing Enterobacteriales (3). However, use of ceftazidime-avibactam has been associated with emergence of resistance in K. pneumoniae isolates, which usually occurs through mutations in the blaKPC gene (4). Here, we report development of a novel KPC variant conferring ceftazidime-avibactam resistance in Enterobacter hormaechei, a common member of the Enterobacter cloacae complex, with subsequent patient-to-patient transmission.
The first patient (patient B) was a 69-year-old man who was admitted to the transplant intensive care unit of a hospital in the midwestern United States in 2016 for a liver transplant. Three months later, the patient was identified as a carrier of carbapenem-resistant K. pneumoniae (strain 01140-2) (5). He received two courses of ceftazidime-avibactam (14 and 33 days) in late 2016 and was transferred to a rehabilitation unit in early 2017. One week after transfer, carbapenem-resistant E. hormaechei (strain 04408-5) was identified from a rectal screening culture. On the same day, carbapenem-resistant K. pneumoniae (strain 04409-2) and E. hormaechei (strain 04409-1) isolates were identified from the rectal screening culture of a second patient (patient H) who was staying in the same rehabilitation unit. Patient H, a 63-year-old woman, did not develop infection and did not receive any antibiotic, including ceftazidime-avibactam, during her stay in the hospital. The two patients overlapped for 5 days in the rehabilitation unit.
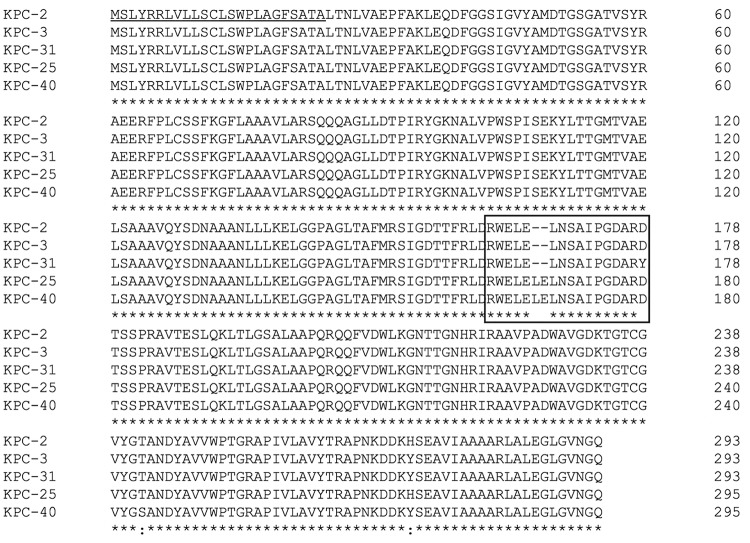
The K. pneumoniae isolates from patients B and H were sequenced on the Illumina NextSeq platform (GenBank accession no. QRBQ00000000.1 and QRBO00000000.1). Comparative analysis showed that both isolates belonged to sequence type (ST) 258, and there were only two core genome single-nucleotide polymorphisms (SNPs) that separated the isolates from one another, as assessed by Snippy (https://github.com/tseemann/snippy). Comparative genome analysis of the E. hormaechei isolates from each patient showed that they both belonged to ST407 and had one core genome SNP that separated them from one another (GenBank accession no. QRBS00000000.1 and QRBR00000000.1). ST258 is the globally epidemic K. pneumoniae lineage that is often associated with KPC production (6), and E. hormaechei ST407 has been associated with production of the CTX-M-15 β-lactamase but not KPC (7). All four strains were blaKPC positive by PCR (8). Examination of KPC sequences from the Illumina data showed that the K. pneumoniae isolate from patient B carried blaKPC encoding KPC-31 (GenBank accession no. NG_055494.1), whereas the K. pneumoniae isolate from patient H carried blaKPC encoding KPC-3. KPC-31 has an aspartic acid-to-tyrosine (D179Y) substitution at position 179 in the Ω-loop of KPC-3, which is known to confer resistance to ceftazidime-avibactam (Fig. 1) (4). The two E. hormaechei isolates, on the other hand, carried blaKPC encoding KPC-40 (GenBank accession no. WP_115470049.1), which contains a duplication of leucine and glutamic acid residues between positions 168 and 169 (L167_E168dup), also located in the Ω-loop of the KPC enzyme. This duplication is seen in KPC-25 (GenBank accession no. NG_051167.1) as well, but its phenotype has not yet been reported. KPC-40 has a threonine-to-serine substitution at position 237 (T237S) located in the oxyanion hole compared with KPC-3. Previous site-saturation mutagenesis experiments suggested that this substitution specifically maintains kinetic activities of the KPC enzyme against β-lactams, including carbapenems (9).
FIG 1.
Alignment of relevant KPC variants. KPC-31 and KPC-40 confer reduced susceptibility to ceftazidime-avibactam and susceptibility to meropenem. The phenotype conferred by KPC-25 is not known. The signal peptide is underlined, and the Ω-loop region is boxed.
MICs of representative antimicrobial agents were obtained by broth microdilution using Sensititre GNX2F plates (Thermo). Ceftazidime-avibactam MICs were obtained by manual broth microdilution. The two E. hormaechei isolates producing KPC-40 showed reduced susceptibility to ceftazidime-avibactam and collateral susceptibility to carbapenems (Table 1).
TABLE 1.
MICs of the KPC-producing strains
| Antimicrobial agent | MIC (μg/ml) in: |
|||
|---|---|---|---|---|
| Patient B for: |
Patient H for: |
|||
| K. pneumoniae 01140-2 (KPC-31, ST258) | E. hormaechei 04408-5 (KPC-40, ST407) | K. pneumoniae 04409-2 (KPC-31, ST258) | E. hormaechei 04409-1 (KPC-40, ST407) | |
| Ceftazidime-avibactama | 64 | 16 | 4 | 8 |
| Ertapenem | >4 | 4 | >4 | 2 |
| Imipenem | >8 | ≤1 | >8 | ≤1 |
| Meropenem | >8 | ≤1 | >8 | ≤1 |
| Cefotaxime | >32 | >32 | >32 | >32 |
| Ceftazidime | >16 | >16 | >16 | >16 |
| Cefepime | >16 | 8 | >16 | 8 |
| Aztreonam | >16 | >16 | >16 | >16 |
| Piperacillin-tazobactam | >64/4 | >64/4 | >64/4 | >64/4 |
| Ciprofloxacin | >2 | ≤0.25 | >2 | ≤0.25 |
| Levofloxacin | >8 | ≤1 | >8 | ≤1 |
| Gentamicin | ≤1 | ≤1 | ≤1 | ≤1 |
| Amikacin | 16 | ≤4 | 16 | ≤4 |
| Tobramycin | >8 | ≤1 | >8 | ≤1 |
| Doxycycline | >16 | 16 | >16 | 16 |
| Tigecycline | 1 | 2 | 1 | 2 |
| Colistin | ≤0.25 | ≤0.25 | ≤0.25 | ≤0.25 |
The breakpoint for ceftazidime-avibactam approved by the Clinical and Laboratory Standards Institute is ≤8/4 μg/ml for susceptible and ≥16/4 μg/ml for resistance.
To determine the impact of the L167_E168dup variant observed in KPC-40, isogenic mutants of KPC-3 and KPC-40 were constructed. The blaKPC genes were amplified with primers KPC_P2_fwd_SpeI (5′-CCGACTAGTAAAATTCCAAACCCGAATGATCC-3′) and KPC_rev_EcoRI (5′-CCGGAATTCTTACTGCCCGTTGACGCCCAAT-3′) and cloned into pBCSK(-) (Agilent, Santa Clara, CA). Escherichia coli TOP10 cells were transformed with each construct, and transformants were selected using ampicillin 50 μg/ml and chloramphenicol 30 μg/ml. The blaKPC sequences in the transformants were confirmed by Sanger sequencing. As expected, production of KPC-40 conferred reduced ceftazidime-avibactam susceptibility with an MIC of 64 μg/ml, compared with an MIC of 1 μg/ml observed with production of KPC-3 (the MIC of the recipient with an empty vector was 0.25 μg/ml). We also generated a transformant carrying blaKPC that encoded L167_E168dup but not T237S. This transformant had a ceftazidime-avibactam MIC of 8 μg/ml, which confirmed the role of the L167_E168dup variant in reduced ceftazidime-avibactam susceptibility, although the concomitant T237S substitution was necessary for resistance. Certain disruptions of the Ω-loop are known to increase the flexibility of the structure, leading to improved binding of ceftazidime to the enzyme-active site (10).
The complete sequence of the plasmid carrying blaKPC-40 in E. hormaechei 04408-5 was determined by sequencing its genome on the MinION platform (Oxford Nanopore Technologies, Oxford Science Park, UK). Hybrid assembly of Illumina and MinION reads was performed using Unicycler v0.4.6 with default parameters (11). The resulting plasmid, p04408-5-KPC40, was 55,076 bp in size and carried the N replicon (GenBank accession no. MK862125). p04408-5-KPC40 was highly similar to pKm38_N (GenBank accession no. KY128483.1), a 69-kb N plasmid encoding KPC-2 and harbored by Klebsiella michiganensis strain Km97_38 isolated in 1997 (12). However, in addition to the differences in the blaKPC gene, a 17-kb region upstream of blaKPC-2 containing resistance genes aac(6’)-Ib, aadA1, blaOXA-9, blaTEM-1, strB, strA, and sul2 in pKm38_N was replaced by a 3.5-kb section containing a Tn3-family transposon Tn5403; and, as a result, p04408-5-KPC40 only carried blaKPC-40 and dfrA14 resistance genes.
Likewise, the blaKPC genes encoding KPC-3, KPC-31, and KPC-40 across the studied strains were all carried on N plasmids based on PCR of E. coli transformant strains, suggesting a likely shared origin (5). We speculate that KPC-31 (K. pneumoniae strain 01140-2) and KPC-40 (E. hormaechei strain 04408-5) evolved from KPC-3 under selective pressure from prolonged ceftazidime-avibactam therapy in patient B, and the E. hormaechei strain was then transmitted to patient H (E. hormaechei strain 04409-1). As for the K. pneumoniae 04409-2 strain in patient H, it is equally plausible that KPC-31 reverted to KPC-3 in the absence of ceftazidime-avibactam exposure or that patient B harbored a mixed population of K. pneumoniae isolates producing both KPC-3 and KPC-31, the former of which was acquired by patient H.
The complex dynamics of KPC described here highlight several key diagnostic and therapeutic considerations at a time when active screening for KPC-producing Enterobacteriales isolates is increasingly utilized, and ceftazidime-avibactam is considered the standard of care for the treatment of infections caused by these organisms. Ceftazidime-avibactam susceptibility should always be tested when the agent is used, but the risk of resistance increases when KPC-producing strains are isolated from a patient with previous exposure to this agent or when such strains are expected yet reported as extended-spectrum β-lactamase producers (13). Furthermore, in the setting of possible hospital transmission, such organisms recovered from patients who have not been exposed to ceftazidime-avibactam should also be tested for susceptibility to this agent when its use is considered.
ACKNOWLEDGMENTS
We thank Daniel Evans, Daniel Snyder, and Vaughn Cooper for assistance with genome sequencing.
D.V.T. was supported by the University of Pittsburgh Department of Medicine and by grant R00EY028222 from the National Institutes of Health. R.K.S. was supported by grants K08AI114883 and R03AI144636 from the National Institutes of Health. Y.D. was supported by research grants R01AI104895 and R21AI135522 from the National Institutes of Health.
REFERENCES
- 1.Ahn C, Syed A, Hu F, O’Hara JA, Rivera JI, Doi Y. 2014. Microbiological features of KPC-producing Enterobacter isolates identified in a U.S. hospital system. Diagn Microbiol Infect Dis 80:154–158. doi: 10.1016/j.diagmicrobio.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chavda KD, Chen L, Fouts DE, Sutton G, Brinkac L, Jenkins SG, Bonomo RA, Adams MD, Kreiswirth BN. 2016. Comprehensive genome analysis of carbapenemase-producing Enterobacter spp.: new insights into phylogeny, population structure, and resistance mechanisms. mBio 7:e02093-16. doi: 10.1128/mBio.02093-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Duin D, Lok JJ, Earley M, Cober E, Richter SS, Perez F, Salata RA, Kalayjian RC, Watkins RR, Doi Y, Kaye KS, Fowler VG, Paterson DL, Bonomo RA, Evans S, Antibacterial Resistance Leadership Group. 2018. Colistin versus ceftazidime-avibactam in the treatment of infections due to carbapenem-resistant Enterobacteriaceae. Clin Infect Dis 66:163–171. doi: 10.1093/cid/cix783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shields RK, Chen L, Cheng S, Chavda KD, Press EG, Snyder A, Pandey R, 2017. Emergence of ceftazidime-avibactam resistance due to plasmid-borne blaKPC-3 mutations during treatment of carbapenem-resistant Klebsiella pneumoniae infections. Antimicrob Agents Chemother 61:e02097-16. doi: 10.1128/AAC.02097-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reeme AE, Bowler SL, Buchan BW, Graham MB, Behrens E, Singh S, Hong JC, Arvan J, Hyke JW, Palen L, Savage S, Seliger H, Huerta S, Ledeboer NA, Kotay S, Mathers AJ, Cooper VS, Mustapha MM, Mettus RT, Doi Y, Munoz-Price LS. 2019. Use of a cohorting-unit and systematic surveillance cultures to control a Klebsiella pneumoniae carbapenemase (KPC)-producing Enterobacteriaceae outbreak. Infect Control Hosp Epidemiol 40:767–773. doi: 10.1017/ice.2019.99. [DOI] [PubMed] [Google Scholar]
- 6.Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos GL, Cormican M, Cornaglia G, Garau J, Gniadkowski M, Hayden MK, Kumarasamy K, Livermore DM, Maya JJ, Nordmann P, Patel JB, Paterson DL, Pitout J, Villegas MV, Wang H, Woodford N, Quinn JP. 2013. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis 13:785–796. doi: 10.1016/S1473-3099(13)70190-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Piekarska K, Zacharczuk K, Wolkowicz T, Wolaniuk N, Rzeczkowska M, Gierczynski R. 2019. Emergence of Enterobacteriaceae co-producing CTX-M-15, ArmA and PMQR in Poland. Adv Clin Exp Med 28:249–254. doi: 10.17219/acem/94165. [DOI] [PubMed] [Google Scholar]
- 8.Doi Y, Potoski BA, Adams-Haduch JM, Sidjabat HE, Pasculle AW, Paterson DL. 2008. Simple disk-based method for detection of Klebsiella pneumoniae carbapenemase-type β-lactamase by use of a boronic acid compound. J Clin Microbiol 46:4083–4086. doi: 10.1128/JCM.01408-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Papp-Wallace KM, Taracila M, Hornick JM, Hujer AM, Hujer KM, Distler AM, Endimiani A, Bonomo RA. 2010. Substrate selectivity and a novel role in inhibitor discrimination by residue 237 in the KPC-2 β-lactamase. Antimicrob Agents Chemother 54:2867–2877. doi: 10.1128/AAC.00197-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barnes MD, Winkler ML, Taracila MA, Page MG, Desarbre E, Kreiswirth BN, Shields RK, Nguyen MH, Clancy C, Spellberg B, Papp-Wallace KM, Bonomo RA. 2017. Klebsiella pneumoniae carbapenemase-2 (KPC-2), substitutions at Ambler position AspCLXXIX, and resistance to ceftazidime-avibactam: unique antibiotic-resistant phenotypes emerge from β-lactamase protein engineering. mBio 8:e00528-17. doi: 10.1128/mBio.00528-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wick RR, Judd LM, Gorrie CL, Holt KE. 2017. Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput Biol 13:e1005595. doi: 10.1371/journal.pcbi.1005595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eilertson B, Chen L, Chavda KD, Kreiswirth BN. 2017. Genomic characterization of two KPC-producing Klebsiella isolates collected in 1997 in New York City. Antimicrob Agents Chemother 61:e02458-16. doi: 10.1128/AAC.02458-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haidar G, Clancy CJ, Shields RK, Hao B, Cheng S, Nguyen MH. 2017. Mutations in blaKPC-3 that confer ceftazidime-avibactam resistance encode novel KPC-3 variants that function as extended-spectrum β-lactamases. Antimicrob Agents Chemother 61:e02534-16. doi: 10.1128/AAC.02534-16. [DOI] [PMC free article] [PubMed] [Google Scholar]