Abstract
Background
Hospital staffing is usually reduced on weekends, potentially impacting inpatient care and postdischarge coordination of care for patients with acute decompensated heart failure (ADHF). However, investigations of in‐hospital mortality on the weekend versus weekday, and post‐hospital outcomes of weekend versus weekday discharge are scarce.
Methods and Results
Hospitalizations for ADHF were sampled by stratified design from 4 US areas by the Community Surveillance component of the ARIC (Atherosclerosis Risk in Communities) study. ADHF was classified by a standardized computer algorithm and physician review of the medical records. Discharges or deaths on Saturday, Sunday, or national holidays were considered to occur on the “weekend.” In‐hospital mortality was compared between hospitalizations ending on a weekend versus weekday. Post‐hospital (28‐day) mortality was compared among patients discharged alive on a weekend versus weekday. From 2005 to 2014, 39 699 weighted ADHF hospitalizations were identified (19% terminating on a weekend). Demographics, comorbidities, length of stay, and guideline‐directed therapies were similar for patients with hospitalizations ending on a weekend versus weekday. In‐hospital death doubled on the weekend compared with weekday (12% versus 6%) and was not attenuated by adjustment for potential confounders (odds ratio, 2.37; 95% CI, 1.93–2.91). There was no association between weekend discharge and 28‐day mortality among patients discharged alive.
Conclusions
The risk of in‐hospital death among patients admitted with ADHF appears to be doubled on the weekends when hospital staffing is usually reduced. However, among patients discharged alive, hospital discharge on a weekend is not adversely associated with mortality.
Keywords: acute heart failure, discharge, epidemiology, mortality
Subject Categories: Heart Failure, Mortality/Survival
Short abstract
See Editorial Mehta and Pandey
Clinical Perspective
What Is New?
Patients admitted with acute decompensated heart failure, have twice the in‐hospital mortality on weekend days compared with weekdays, but 28‐day post‐hospital mortality is similar, regardless of weekend versus weekday discharge.
The heightened risk of in‐hospital death on the weekend compared with weekdays is consistent for patients with heart failure who have reduced versus preserved ejection fraction or weekend versus weekday admission.
What Are the Clinical Implications?
It is crucial for health systems to continue developing care delivery models that allow for a consistent inpatient quality of care and availability of resources irrespective of day of the week.
Introduction
Heart failure (HF) is the third most common diagnosis for patient hospitalization, excluding maternal/neonatal stays.1 The “weekend effect,” worse patient outcomes following weekend admission, has been well‐described for many admission diagnoses.2, 3, 4, 5 This has been attributed to a variety of causes, including decreased availability of supervising physicians and subspecialty care on weekends, reduced nurse staffing, higher illness severity among patients admitted on weekends, and delays to diagnosis and therapeutic procedures.2, 6, 7, 8, 9, 10, 11 Outcomes of weekend versus weekday admission have also been described among patients admitted with acute decompensated HF (ADHF) in several large registries.12, 13, 14, 15
In contrast, there are no analyses of in‐hospital death on the weekend versus weekday for patients admitted for ADHF, and the existing data on post‐hospital outcomes by weekend or weekday discharge are both minimal and conflicting.13, 16 The Centers for Medicare and Medicaid Services prioritize in‐hospital mortality and 30‐day mortality as outcome metrics in the Hospital Quality Initiative.17 Examining inpatient mortality on the weekend versus weekday and post‐hospital outcomes following discharge on the weekend versus weekday in a large, geographically diverse sample of patients admitted with ADHF may suggest actionable areas for intervention. To meet this objective, we analyzed ADHF hospitalizations captured by the Community Surveillance component of the ARIC (Atherosclerosis Risk in Communities) study. We expected that patients would have worse in‐hospital outcomes on the weekend because of fewer available resources including diagnostic and therapeutic procedures and subspecialty care. Further, we anticipated that patients discharged alive on the weekends would have worse post‐hospital outcomes because of incomplete discharge instructions and scheduling of follow‐up care. Finally, we explored the possibility that associations between weekend discharge and mortality may be modified by HF type or by synergistic interaction with weekend admission.
Methods
Study Design and Population
The ARIC study's data and materials are publicly available.18, 19 Details of the Community Surveillance component of the ARIC study have been previously described.20 In short, admissions for ADHF from January 1, 2005, to December 31, 2014, were sampled by stratified design from 4 US communities: Washington County, Maryland; Forsyth County, North Carolina; Jackson, Mississippi; and selected suburbs of Minneapolis, Minnesota. All surveillance protocols were approved by local institutional review boards. Informed consent was not required, because all data were anonymized by redacting personal identifiers. Events from acute care hospitals for patients 55 years or older with a home address within an ARIC community were identified through discharge diagnoses and their associated International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) codes, which included the following: rheumatic heart disease (398.91), hypertensive heart disease with congestive HF (402.01, 402.11, 402.91), hypertensive heart disease and renal failure with congestive HF (404.01, 404.03, 404.11, 404.13, 409.91, 404.93), acute cor pulmonale (415), chronic pulmonary heart disease (416.9), other primary cardiomyopathies (425.4), congestive HF (428.x), acute edema of lung (518.4), and dyspnea and respiratory abnormalities (786.0x). Sampling fractions were assigned based on ICD‐9‐CM codes (428.x code, all other codes), ARIC center, sex, and race (white or black).
ADHF Classification and Final Study Population
Eligible hospitalizations were abstracted by trained abstractors if there was any evidence of ADHF, new onset of HF symptoms, or mention by a physician that HF was the reason for hospitalization. Abstracted cases were independently classified by a computer algorithm and physicians of the ARIC Mortality and Morbidity Classification Committee into 1 of 5 prespecified definitions: definite ADHF, probable ADHF, chronic stable HF, HF unlikely, or unclassifiable HF.21 For the purposes of this analysis, hospitalizations were limited to patients classified with definite and probable ADHF. Transfers to or from another acute care hospital were excluded, as these would result in misclassification of weekend discharge status and confound length‐of‐stay assessments.
Weekend Classification
Discharge due to release from the hospital or death on Saturday, Sunday, or federal holidays was considered to occur on the “weekend.” The US Government Office of Personnel Management classifies New Year's Day, Martin Luther King Day, President's Day, Memorial Day, Independence Day, Labor Day, Columbus Day, Veterans Day, Thanksgiving Day, and Christmas Day as federal holidays.
Demographics, Medical History, and Hospital Procedures
Demographic and clinical data were abstracted from the medical record. Demographic data included age, sex, race, health insurance status, hospital, and year of admission. Clinical characteristics included smoking history, comorbidities (chronic obstructive pulmonary disease, coronary disease, diabetes mellitus, receipt of dialysis, chronic kidney disease, stroke, previous HF admission, and previous hospitalization for ADHF), and vital signs at admission. Laboratory values during the span of the hospitalization (eg, hemoglobin, sodium, serum urea nitrogen, and creatinine) were abstracted by recording the “worst” and “last” values in the hospital record. Glomerular filtration rate was estimated using the Chronic Kidney Disease Epidemiology Collaboration (CKD‐EPI) formula22 and the “last” reported creatinine value. We defined chronic kidney disease by an estimated glomerular filtration rate <60 mL/min per 1.73 m2, or receipt of hemodialysis.22 Medications taken before admission or during hospitalization (eg, angiotensin‐converting enzyme inhibitors, angiotensin II receptor blockers, β‐blockers, digitalis, aldosterone blockers, statins, hydralazine, and nitrates), and therapies during hospitalization, such as intravenous medications (diuretics and inotropes) and diagnostic procedures (eg, right heart catheterization and coronary angiography) were also abstracted. Ejection fraction (EF) was recorded from inpatient diagnostic echocardiograms, either during the inpatient stay or within 90 days of hospitalization. We considered an EF <50% to be evidence of HF with reduced EF and EF ≥50% to be HF with preserved EF. EF data were available for 25 383 (64%) patients.
Mortality
In‐hospital mortality was abstracted from the medical record. Deaths within 28 days of hospitalization were ascertained by the ARIC study by linking patient records with the National Death Index.
Statistical Analysis
All analyses were performed using SAS 9.4 Survey Procedures (SAS Institute). Analyses were weighted by the inverse of the sampling probability and accounted for the stratified sampling design.23 Demographics, clinical characteristics, length of stay, and mortality were compared between patients with weekend versus weekday discharge. Categorical variables were compared using Rao‐Scott χ2 tests. Continuous variables were compared using the difference in least square means from weighted linear regression. Odds ratios of in‐hospital mortality on the weekend versus weekday were analyzed using multivariable logistic regression. Adjusted hazards of 28‐day mortality were compared using multivariable Cox regression, with analyses limited to patients discharged alive. Modeling strategies were determined a priori. First, we constructed minimally adjusted models accounting for demographics (age, race, sex, year of admission, and hospital). Next, we examined models adjusted for demographics and routinely abstracted variables shown to differ in univariate comparisons of patients with hospitalizations terminating on the weekend versus weekday. Additionally, we adjusted for length of stay and intravenous inotrope administration, considering these to be indicators of HF severity. We also explored the possibility that associations may differ by HF type or by weekend versus weekday admission. This was accomplished by constructing stratified models and by testing multiplicative interaction.
Results
Of 39 699 (8500 unweighted) hospitalizations included in this analysis, 19% ended on the weekend. A small percentage of hospitalizations (2%) terminated on a federal holiday. The mean age of patients at admission was 76 years, 48% were men, and 66% were white. The majority of patients (96%) had health insurance. As shown in Figure 1, day of admission was unequally distributed (P<0.0001), as was day of discharge (P<0.0001). Monday was the most frequent day of admission (16%), while Friday was the most frequent day of discharge (19%). Saturday and Sunday were the least common discharge days (9% and 6%, respectively).
Figure 1.
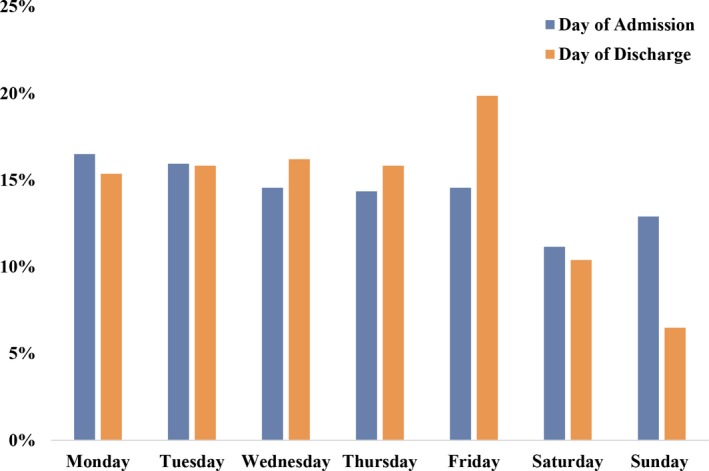
Frequency of admissions and discharges by day of week among patients hospitalized with acute decompensated heart failure. The Community Surveillance component of the Atherosclerosis Risk in Communities study, 2005–2014.
Patient demographics, comorbidities, laboratory values, HF classification, in‐hospital procedures, and receipt of intravenous inotropes, intravenous diuretics, and other evidence‐based therapies were largely comparable among hospitalizations ending on a weekend versus weekday (Table 1). However, patients who were discharged on a weekend were less frequently admitted on a weekend (20% versus 28%) and were less likely to have a history of stroke (18% versus 21%). Administration of β‐blockers was more common among patients discharged on the weekend (70% versus 66%), while administration of angiotensin II receptor blockers was less common (11% versus 14%). The overall mean length of stay was 8 days (11 days among patients dying in‐hospital) and did not differ for hospitalizations terminating on a weekend versus weekday.
Table 1.
Demographics and Clinical Characteristics of Patients With ADHF Hospitalizations Ending on a Weekend vs Weekday
| Weekenda Discharge (n=7494) No. (%) or Mean±SEM | Weekday Discharge (n=32 205) No. (%) or Mean±SEM | P Value | |
|---|---|---|---|
| Demographics | |||
| Age, y | 76±0.2 | 76±0.1 | 0.7 |
| Women | 3809 (51) | 17 120 (53) | 0.1 |
| White | 5150 (69) | 21 063 (65) | 0.02 |
| Health insurance | 7178 (96) | 31 121 (97) | 0.2 |
| Year of admission | 2010±0.01 | 2010±0.01 | 1.0 |
| Weekend admission | 1478 (20) | 9054 (28) | <0.0001 |
| Medical history | |||
| Ejection fractionb | 42%±0.6% | 43%±0.3% | 0.4 |
| HFrEF (EF <50%)b | 2559 (54) | 10 984 (53) | 0.5 |
| Hypertension | 6433 (86) | 27 650 (86) | 1.0 |
| Atrial fibrillation/flutter | 12 098 (38) | 2987 (40) | 0.1 |
| Chronic kidney diseasec | 4040 (72) | 17 441 (70) | 0.3 |
| COPD/bronchitis | 2673 (36) | 11 294 (35) | 0.7 |
| Myocardial infarction | 2036 (27) | 8012 (25) | 0.1 |
| Coronary heart disease | 4326 (58) | 18 105 (56) | 0.3 |
| Diabetes mellitus | 3525 (47) | 15 508 (48) | 0.5 |
| Dialysis | 524 (7) | 2252 (7) | 1 |
| Stroke/transient ischemic attack | 1344 (18) | 6833 (21) | 0.01 |
| Prior HF hospitalization | 2716 (36) | 11 288 (35) | 0.6 |
| Current smoking | 1001 (13) | 4085 (13) | 0.5 |
| Hospital vital signs and laboratory valuesd | |||
| Systolic BP, mm Hge | 141±0.9 | 142±0.5 | 0.3 |
| Diastolic BP, mm Hge | 76±0.5 | 78±0.3 | <0.0001 |
| B‐type natriuretic peptide, pg/dLf | 1320±53 | 1359±36 | <0.0001 |
| Hemoglobin, g/dL | 10.6±0.06 | 10.5±0.03 | 0.2 |
| Sodium, mEq/L | 136±0.1 | 136±0.06 | 0.5 |
| Serum urea nitrogen, mg/dL | 41±0.7 | 41±0.3 | 0.8 |
| Creatinine, mg/dL | 2.15±0.05 | 2.15±0.02 | 1.0 |
| Hospital procedures/intravenous medications | |||
| Right heart catheterization | 215 (3) | 895 (3) | 0.8 |
| Angiography | 948 (13) | 3781 (12) | 0.4 |
| Intravenous inotropes | 455 (6) | 1876 (6) | 0.7 |
| Intravenous diuretics | 5969 (80) | 25 736 (80) | 0.8 |
| Medications | |||
| ACE inhibitor | 2684 (36) | 11 552 (36) | 1.0 |
| Angiotensin receptor II blocker | 847 (11) | 4376 (14) | 0.03 |
| β‐Blocker | 5219 (70) | 21 322 (66) | 0.02 |
| Digitalis | 899 (12) | 4034 (12) | 0.6 |
| Diuretics | 5170 (69) | 21 996 (68) | 0.7 |
| Aldosterone blocker | 659 (9) | 2668 (8) | 0.6 |
| Nitrates | 2239 (30) | 9247 (29) | 0.4 |
| Hydralazine | 919 (12) | 3767 (12) | 0.6 |
| Length of stay, d | 8.1±1.5 | 8.1±0.2 | 1.0 |
The Community Surveillance component of the Atherosclerosis Risk in Communities Study, 2005–2014. ACE indicates angiotensin‐converting enzyme; ADHF, acute decompensated heart failure; COPD, chronic obstructive pulmonary disease; HF, heart failure; HFrEF, heart failure with reduced ejection fraction; SEM, standard error of the mean.
Weekend=Saturday, Sunday, or national holiday.
Ejection fraction (EF) limited to 25 383 (64%) patients with available echocardiography abstractions.
Chronic kidney disease defined by estimated glomerular filtration rate <60 mL/min per 1.73 m2 or receipt of hemodialysis; among 30 609 patients with available creatinine data abstractions.
Laboratory results are the worst reported values from the hospitalization.
Blood pressures (BPs) on admission.
Data not available for 50% of patients.
In total, there were 2816 (7%) in‐hospital deaths. Demographic, diagnostic, and clinical characteristics of patients who died in‐hospital on the weekend versus weekday are shown in Table S1. The incidence of in‐hospital death was twice as high on the weekend (12% versus 6%; P<0.0001), with a similar pattern observed among subgroups stratified by HF type and by weekend versus weekday admission (Figure 2). However, the incidence of in‐hospital death did not differ by weekend or weekday admission (7% versus 7%). After adjusting for demographics, patients had twice the odds of in‐hospital death on the weekend (odds ratio, 2.37; 95% CI, 1.93–2.91) (Figure 3. Similar adjusted associations were observed in patients with HF with reduced EF and HF with preserved EF, with no suggestion of statistical interaction (P for interaction=0.4). However, there was a trend toward higher in‐hospital mortality on the weekend for patients admitted on a weekend as opposed to a weekday (P for interaction=0.2). The increased odds of in‐hospital death on the weekend versus weekday was consistent in models with additional adjustments for stroke, diastolic blood pressure, angiotensin II receptor blockers, β‐blockers, length of stay, and intravenous inotropes (Table 2). There was no difference in the adjusted odds of in‐hospital death by weekend versus weekday admission (Table S2).
Figure 2.
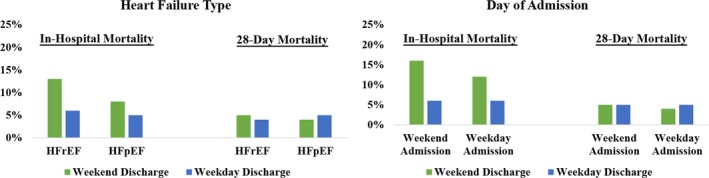
Incidence* of in‐hospital and 28‐day mortality among patients with acute decompensated heart failure hospitalizations ending on a weekday vs weekend, stratified by heart failure type and admission on a weekend vs weekday. The Community Surveillance component of the Atherosclerosis Risk in Communities study, 2005–2014. *Heart failure type limited to patients with available echocardiography, and 28‐day mortality limited to patients discharged alive. HFpEF indicates heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction.
Figure 3.
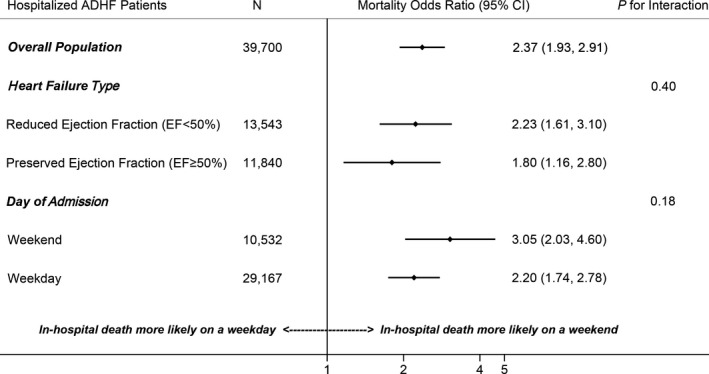
Adjusted odds ratios of in‐hospital mortality among patients with acute decompensated heart failure (ADHF) hospitalizations ending on a weekend vs weekday. The Community Surveillance component of the Atherosclerosis Risk in Communities study, 2005–2014. Models adjusted for age, race, sex, year of admission, and hospital.
Table 2.
Crude, Minimally Adjusted, and Fully Adjusted ORs of In‐Hospital Death on a Weekend vs Weekday Among Patients Admitted With ADHF
| Subgroup | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| All patients | 2.29 (1.88–2.80) | 2.37 (1.93–2.91) | 2.46 (1.99–3.04) | 2.49 (2.0–3.10) |
| HFrEFa (EF <50%) | 2.10 (1.53–2.89) | 2.23 (1.61–3.10) | 2.39 (1.69–3.38) | 2.50 (1.01–1.05) |
| HFpEFa (EF ≥50%) | 1.71 (1.10–2.64) | 1.80 (1.16–2.81) | 1.75 (1.11–2.74) | 2.63 (2.00–2.44) |
| Weekend admission | 3.07 (2.05–4.60) | 3.05 (2.02–4.60) | 3.00 (1.94–4.63) | 2.84 (1.80–4.50) |
| Weekday admission | 2.11 (1.68–2.65) | 2.20 (1.74–2.78) | 2.36 (1.85–3.01) | 2.44 (1.90–3.13) |
The Community Surveillance component of the Atherosclerosis Risk in Communities study, 2005–2014. Model 1=crude. Model 2=adjusted for demographics (age, race, sex, year of admission, and hospital code). Model 3=adjusted for demographics, history of stroke, diastolic blood pressure at admission, and receipt of angiotensin II receptor blockers and β‐blockers during hospitalization. Model 4=adjusted for demographics, history of stroke, diastolic blood pressure at admission, receipt of angiotensin II receptor blockers and β‐blockers during hospitalization, and disease severity as indicated by length of stay and receipt of intravenous inotropes. ADHF indicates acute decompensated heart failure; EF, ejection fraction; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; OR, odds ratio.
Classification of heart failure type limited to 25 383 patients (64%) with available echocardiography abstractions.
Among patients discharged alive, a total of 1868 (5%) deaths occurred by 28 days of hospitalization. Clinical characteristics of patients discharged alive on the weekend versus weekday are shown in Table S3 and are largely comparable. As shown in Figure 4, a similar distribution of discharge days was observed when comparing 28‐day fatalities with 28‐day survivors (P=0.3). Sunday was the least common discharge day (6% of discharges for both groups), followed by Saturday (9% and 10%). The incidence of 28‐day mortality did not differ among patients with a weekend versus weekday discharge (5% for each). After adjustment for demographics and surrogate markers for disease severity (length of stay and intravenous inotropes), no significant difference in 28‐day mortality was noted among patients discharged alive on the weekend versus weekday (hazard ratio, 0.86; 95% CI, 0.62–1.19).
Figure 4.
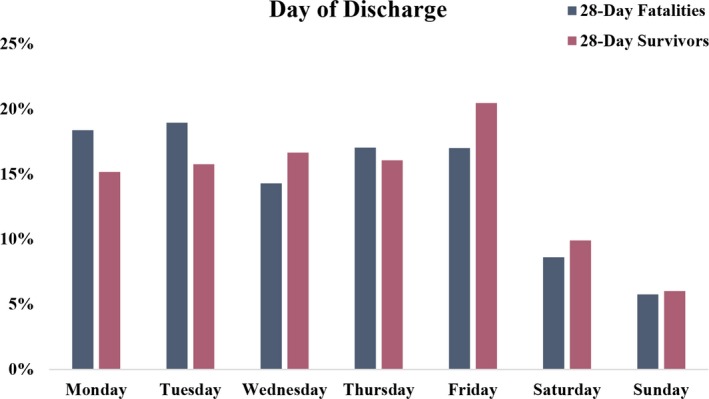
Distributions of discharge days among patients hospitalized with acute decompensated heart failure who were discharged alive, stratified by those who died or survived by 28 days of hospitalization. The Community Surveillance component of the Atherosclerosis Risk in Communities study, 2005–2014.
Discussion
We conducted this investigation to examine whether mortality differs among patients with ADHF hospitalizations ending on the weekend versus weekday. Among 39 699 hospitalizations, a greater incidence of in‐hospital deaths occurred on the weekend, irrespective of HF type, with a trend toward greater in‐hospital mortality among patients also admitted on the weekend. The association remained significant after adjusting for hospital‐ and patient‐level factors. However, no difference in 28‐day mortality was observed among patients discharged alive on a weekend versus weekday. To our knowledge, this is the first examination of mortality outcomes and their relation to hospitalizations ending on a weekend versus weekday in a population‐based sample of patients classified with ADHF by physician validation.
Despite similar demographics, comorbidities, admission vital signs, and laboratory values, in‐hospital mortality was more frequent on the weekend than on weekdays. Higher in‐hospital mortality on the weekend has been reported for other conditions, such as chronic obstructive pulmonary disease and pneumonia.24, 25 A potential factor contributing to weekend in‐hospital mortality may be handovers of care. Handovers of care are frequently inconsistent on the weekends, likely because of an increased number of team transitions and decreased compliance with the handover structure itself.26 Several hospital systems have implemented quality initiatives to improve weekend handovers, leading to increased utilization and provider satisfaction with the handover tool.27, 28, 29, 30 Unfortunately, these interventions did not evaluate patient outcomes. Regardless, since improved handovers have been shown to reduce medical errors, focused initiatives concentrating on weekend handovers may lead to better in‐hospital outcomes on the weekend.31
We hypothesized that patients discharged on the weekend would have worse post‐hospital outcomes due to incomplete discharge instructions and scheduling of follow‐up care. On the contrary, no difference in 28‐day mortality was observed among patients with weekend versus weekday discharge. A possible explanation may be that patients discharged on the weekend were healthier, reflecting physician comfort with discharging lower‐risk patients on the weekend. Comorbidities, admission vital signs, and length of stay were comparable among patients discharged alive on the weekend versus weekday. Based on these available data, patients discharged on the weekend did not appear to be lower risk. However, there are many factors such as social support and a relationship with a primary care physician that we were unable to account for. Friday was the most frequent day of discharge. This likely reflects provider and patient preference to discharge before the weekend. Despite this, no significant difference in 28‐day mortality was observed by day of discharge or by weekend versus weekday discharge.
Previous reports of postdischarge mortality for patients with HF discharged on the weekend versus weekday have been conflicting. Consistent with our results, the OPTIMIZE‐HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure) registry observed no difference in 60‐ or 90‐day mortality among patients discharged on the weekend versus weekday.13 Conversely, McAlister et al16 reported a significantly lower 30‐day mortality for patients with HF discharged on a weekday, despite older age and greater comorbidities compared with patients with weekend discharges. However, this analysis was sourced from administrative claims databases with cases determined by unadjudicated International Classification of Diseases, Ninth Revision (ICD‐9) codes. Further, information concerning admission vital signs, laboratory results, ejection fraction, in‐hospital diagnosis, and treatment were lacking.
Providers are often hesitant to discharge patients on the weekend because of concern that coordination of follow‐up care may be inadequate. However, an analysis of the California's Office of Statewide Health Planning and Development database reported no difference in readmissions among patients hospitalized with pneumonia, myocardial infarction, and HF who were discharged on the weekend versus weekday.32 Given this and the similar 28‐day mortality among weekend and weekday discharges observed in the ARIC Community Surveillance, the hesitancy to discharge patients on the weekend is perhaps unfounded.
Multiple studies have examined outcomes of weekend versus weekday admission for patients hospitalized with ADHF. In an analysis from the GWTG‐HF (Get With the Guidelines—Heart Failure) registry, a higher incidence of in‐hospital mortality was observed for patients admitted with ADHF on the weekend.12 In support of this, a recent analysis from the Einstein Medical Center and Agency for Healthcare Research and Quality (AHRQ) Nationwide Inpatient Sample reported significantly higher in‐hospital mortality for patients admitted with ADHF on the weekend.15 Conversely, the OPTIMIZE‐HF registry reported no difference in in‐hospital mortality among patients admitted on the weekend compared with weekday.13 Similar to the results from the present study showing no difference in in‐hospital mortality by weekend versus weekday admission, no difference in in‐hospital mortality was observed for patients with HF with reduced EF who were admitted on a weekend versus weekday in a previous analysis from ARIC Community Surveillance.33 In these previous reports, in‐hospital death did not necessarily occur on the day of admission. Should patient condition worsen after day of admission, resources present at the time of decompensation may be similarly relevant as to those available on the day of admission. Thus, it is important to examine in‐hospital mortality of patients with ADHF by day of death, rather than solely by day of admission, because decreased availability of resources, including specialist and nursing availability, are known to be associated with increased weekend mortality.2, 6, 7, 8, 9, 10, 11
Study Limitations and Strengths
Our analysis from ARIC Community Surveillance has several limitations. This was an observational study and was based on data available in the hospital record. We were unable to consider hospital readmissions, an important postdischarge outcome, or cause‐specific mortality. Federal holidays were considered to occur on the “weekend,” but observation of federal holidays may differ by hospital. However, only 2% of hospitalizations in this analysis terminated on a federal holiday. Our analysis also has several noteworthy strengths. The Community Surveillance component of the ARIC study represents 4 geographically diverse regions of the United States. Rather than relying solely on ICD‐9 codes, ADHF hospitalizations were classified by a standardized computer algorithm and physician review. Clinical data were collected by certified abstractors following standardized protocols, and mortality outcomes were ascertained by linking records with the National Death Index.
Conclusions
Patients admitted with ADHF appear to have heightened risk of in‐hospital death on the weekends. Future studies should focus on in‐hospital death by day of discharge instead of solely by day of admission. Further, analyses of hospital resources should be conducted across many hospitals nationally to elucidate the specific reasons for this greater in‐hospital mortality on the weekends for patients admitted with ADHF.
Sources of Funding
Dr. Mounsey is supported by the Howard Holderness Distinguished Medical Scholars Program. The ARIC study has been funded in whole or in part with federal funds from the National Heart, Lung, and Blood Institute; National Institutes of Health; and the Department of Health and Human Services, under contract numbers (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700005I, HHSN268201700004I).
Disclosures
None.
Supporting information
Table S1. Demographics and Clinical Characteristics of Patients Admitted With ADHF and Dying In‐Hospital on a Weekend vs Weekday
Table S2. Demographics and Clinical Characteristics of Patients Admitted With ADHF and Discharged Alive on a Weekend vs Weekday
Table S3. Crude, Minimally Adjusted, and Fully Adjusted Odds Ratios of In‐Hospital Death Among Patients Admitted on the Weekend and Weekday With ADHF
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions.
(J Am Heart Assoc. 2019;8:e011631 DOI: 10.1161/JAHA.118.011631.)
References
- 1. HCUP Fast Stats. Rockville, MD: Agency for Healthcare Research and Quality; 2017. [Google Scholar]
- 2. Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–668. [DOI] [PubMed] [Google Scholar]
- 3. Magid DJ, Wang Y, Herrin J, McNamara RL, Bradley EH, Curtis JP, Pollack CV, French WJ, Blaney ME, Krumholz HM. Relationship between time of day, day of week, timeliness of reperfusion, and in‐hospital mortality for patients with acute ST‐segment elevation myocardial infarction. JAMA. 2005;294:803–812. [DOI] [PubMed] [Google Scholar]
- 4. Sorita A, Ahmed A, Starr SR, Thompson KM, Reed DA, Prokop L, Shah ND, Murad MH, Ting HH. Off‐hour presentation and outcomes in patients with acute myocardial infarction: systematic review and meta‐analysis. BMJ. 2014;348:f7393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fang J, Saposnik G, Silver FL, Kapral MK; Investigators of the Registry of the Canadian Stroke Network . Association between weekend hospital presentation and stroke fatality. Neurology. 2010;75:1589–1596. [DOI] [PubMed] [Google Scholar]
- 6. Deshmukh A, Pant S, Kumar G, Bursac Z, Paydak H, Mehta JL. Comparison of outcomes of weekend versus weekday admissions for atrial fibrillation. Am J Cardiol. 2012;110:208–211. [DOI] [PubMed] [Google Scholar]
- 7. Morton B, Nagaraja S, Collins A, Pennington SH, Blakey JD. A retrospective evaluation of critical care blood culture yield—do support services contribute to the “weekend effect”? PLoS One. 2015;10:e0141361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364:1037–1045. [DOI] [PubMed] [Google Scholar]
- 9. Walker AS, Mason A, Quan TP, Fawcett NJ, Watkinson P, Llewelyn M, Stoesser N, Finney J, Davies J, Wyllie DH, Crook DW, Peto TEA. Mortality risks associated with emergency admissions during weekends and public holidays: an analysis of electronic health records. Lancet. 2017;390:62–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151–2162. [DOI] [PubMed] [Google Scholar]
- 11. Wilcox ME, Chong CA, Niven DJ, Rubenfeld GD, Rowan KM, Wunsch H, Fan E. Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta‐analyses. Crit Care Med. 2013;41:2253–2274. [DOI] [PubMed] [Google Scholar]
- 12. Horwich TB, Hernandez AF, Liang L, Albert NM, Labresh KA, Yancy CW, Fonarow GC; Get With Guidelines Steering Committee and Hospitals . Weekend hospital admission and discharge for heart failure: association with quality of care and clinical outcomes. Am Heart J. 2009;158:451–458. [DOI] [PubMed] [Google Scholar]
- 13. Fonarow GC, Abraham WT, Albert NM, Stough WG, Gheorghiade M, Greenberg BH, O'Connor CM, Nunez E, Yancy CW, Young JB. Day of admission and clinical outcomes for patients hospitalized for heart failure: findings from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE‐HF). Circ Heart Fail. 2008;1:50–57. [DOI] [PubMed] [Google Scholar]
- 14. Hamaguchi S, Kinugawa S, Tsuchihashi‐Makaya M, Goto D, Tsutsui H. Weekend versus weekday hospital admission and outcomes during hospitalization for patients due to worsening heart failure: a report from Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE‐CARD). Heart Vessels. 2014;29:328–335. [DOI] [PubMed] [Google Scholar]
- 15. Shah M, Patnaik S, Patel B, Arora S, Patel N, Lahewala S, Figueredo VM, Martinez MW, Jacobs L. The day of the week and acute heart failure admissions: relationship with acute myocardial infarction, 30‐day readmission rate and in‐hospital mortality. Int J Cardiol. 2017;249:292–300. [DOI] [PubMed] [Google Scholar]
- 16. McAlister FA, Au AG, Majumdar SR, Youngson E, Padwal RS. Postdischarge outcomes in heart failure are better for teaching hospitals and weekday discharges. Circ Heart Fail. 2013;6:922–929. [DOI] [PubMed] [Google Scholar]
- 17. Outcome Measures—Centers for Medicare & Medicaid Services. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures.html. Accessed May 7, 2018.
- 18. Atherosclerosis Risk in Communities Study Description | Atherosclerosis Risk in Communities. Available at: https://www2.cscc.unc.edu/aric/. Accessed October 31, 2018.
- 19. BioLINCC—Biologic Specimen and Data Repository Information Coordinating Center. Available at: https://biolincc.nhlbi.nih.gov/home/. Accessed October 31, 2018.
- 20. White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, Higgins M, Williams OD, Tyroler HA. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49:223–233. [DOI] [PubMed] [Google Scholar]
- 21. Rosamond WD, Chang PP, Baggett C, Johnson A, Bertoni AG, Shahar E, Deswal A, Heiss G, Chambless LE. Classification of heart failure in the Atherosclerosis Risk in Communities (ARIC) study: a comparison of diagnostic criteria. Circ Heart Fail. 2012;5:152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AH, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD‐EPI (Chronic Kidney Disease Epidemiology Collaboration) . A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mansournia MA, Altman DG. Inverse probability weighting. BMJ. 2016;352:i189. [DOI] [PubMed] [Google Scholar]
- 24. Suissa S, Dell'Aniello S, Suissa D, Ernst P. Friday and weekend hospital stays: effects on mortality. Eur Respir J. 2014;44:627–633. [DOI] [PubMed] [Google Scholar]
- 25. Ambrosi E, De Togni S, Guarnier A, Barelli P, Zambiasi P, Allegrini E, Bazoli L, Casson P, Marin M, Padovan M, Picogna M, Taddia P, Salmaso D, Chiari P, Frison T, Marognolli O, Canzan F, Saiani L, Palese A. In‐hospital elderly mortality and associated factors in 12 Italian acute medical units: findings from an exploratory longitudinal study. Aging Clin Exp Res. 2017;29:517–527. [DOI] [PubMed] [Google Scholar]
- 26. Govier M, Medcalf P. Living for the weekend: electronic documentation improves patient handover. Clin Med. 2012;12:124–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Patel R, Thiagarajan P. Structured approach in improving weekend handovers in a medical high dependency unit. BMJ Qual Improv Rep. 2014;3:(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Michael E, Patel C. Improving medical handover at the weekend: a quality improvement project. BMJ Qual Improv Rep. 2015;4:(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Martin R, Huddart M, Garbett C, Storr W, Watts O, Gupta S. Improving the written medical handover. BMJ Open Qual. 2018;7:e000278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Boyer M, Tappenden J, Peter M. Improving weekend out of hours surgical handover (WOOSH). BMJ Qual Improv Rep. 2016;5:(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Starmer AJ, Spector ND, Srivastava R, West DC, Rosenbluth G, Allen AD, Noble EL, Tse LL, Dalal AK, Keohane CA, Lipsitz SR, Rothschild JM, Wien MF, Yoon CS, Zigmont KR, Wilson KM, O'Toole JK, Solan LG, Aylor M, Bismilla Z, Coffey M, Mahant S, Blankenburg RL, Destino LA, Everhart JL, Patel SJ, Bale JF, Spackman JB, Stevenson AT, Calaman S, Cole FS, Balmer DF, Hepps JH, Lopreiato JO, Yu CE, Sectish TC, Landrigan CP; I‐PASS Study Group . Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371:1803–1812. [DOI] [PubMed] [Google Scholar]
- 32. Cloyd JM, Chen JC, Ma Y, Rhoads KF. Is weekend discharge associated with hospital readmission? J Hosp Med. 2015;10:731–737. [DOI] [PubMed] [Google Scholar]
- 33. Mounsey L, Chang P, Sueta C, Matsushita K, Russell S, Miler E, Caughey M. Outcomes of weekend versus weekday admission for acute decompensated heart failure in patients with reduced ejection fraction: the Atherosclerosis Risk in Communities Surveillance Study. J Am Coll Cardiol. 2018;71:A836. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Demographics and Clinical Characteristics of Patients Admitted With ADHF and Dying In‐Hospital on a Weekend vs Weekday
Table S2. Demographics and Clinical Characteristics of Patients Admitted With ADHF and Discharged Alive on a Weekend vs Weekday
Table S3. Crude, Minimally Adjusted, and Fully Adjusted Odds Ratios of In‐Hospital Death Among Patients Admitted on the Weekend and Weekday With ADHF


