Abstract
Securing stable vascular access is an important clinical skill for the anaesthesiologist. Sick children, complex surgeries, chronic illnesses, multiple hospitalisations, and prolonged treatments can make vascular access challenging. A search was done in the English language literature using the keywords “paediatric,” “vascular access,” “venous access,” and “techniques” or “complications” in Pubmed, Embase, and Google scholar databases. Articles were screened and appropriate content was included. Intraosseous access is a lifesaving technique that can be performed even in hypovolaemic patients rapidly. Transillumination and near-infrared light improve visualisation of superficial veins in difficult access. Ultrasonography has become the standard of care in selecting the vessel, size of catheter, guide placement, and prevent complications. Fluoroscopy is used during insertion of long-term vascular access devices. This article reviews the various routes of access, their indications, most appropriate site, securing techniques, advantages, disadvantages, and complications associated with vascular access in children.
Key words: Paediatric, vascular access, vascular access complications, vascular access techniques, venous access
INTRODUCTION
Placing vascular access is considered a basic skill for anaesthesiologists.[1] Being considered experts in vascular access, anaesthesiologists receive referrals for difficult vascular access from other professionals. Hence, well versing with vascular access techniques including advanced vascular access is imperative. Obtaining vascular access in children may require multiple attempts and can be stressful for the child, the family as well as the care provider.[2] Small caliber veins, anatomical variations, along with child's anxiety, and withdrawal add to the difficulty of anaesthesiologist. This article provides overview of vascular access in children, their indications, techniques, advantages, disadvantages, and complications. Maintenance protocols for these vascular catheters are beyond the scope of this review.
OVERVIEW OF VASCULAR ACCESS
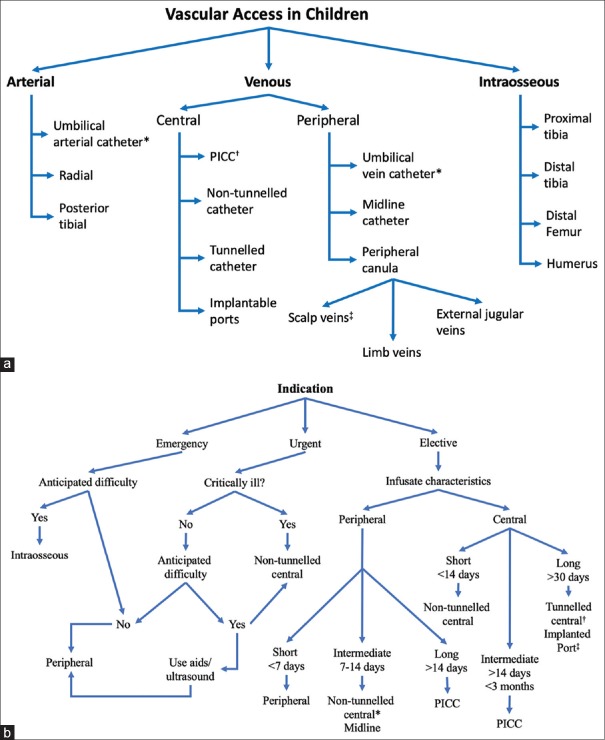
Vascular access can be venous, arterial, or intraosseous. Figure 1a depicts an overview of vascular access in children. Venous access is used in anaesthesia, resuscitation, critical care for fluid, and medication delivery. Arterial access is desired in major surgeries and critically ill children where blood pressure monitoring and blood gas sampling are needed. Intraosseous access is emergency access in arrest and peri-arrest scenarios.
Figure 1.
(a and b) Overview of Vascular Access in Children. (a) depicts the types of vascular access. (* Only in neonates, † Peripherally inserted central catheter, and ‡ In neonates and infants).(b) depicts the decision tree for venous access in children. (* Non-tunneled central line preferred if critically ill or haemodynamic monitoring needed; † Tunneled central catheters preferred if wide bore access desired; ‡ Implanted ports preferred if wide bore access not necessary)
PLACEMENT OF VASCULAR ACCESS IN CHILDREN
Placement of vascular access in an awake child can be challenging. Reducing anxiety as well as pain is the goal. Parental presence and breastfeeding reduces anxiety.[3] Distraction techniques should be tailor-made depending on the age of the child. It can range from music, toys, balloons, puppets, bubbles, and books to cartoons, movies, video games, and electronic smart toys. Smartphones have shown to be useful distraction gadgets in 3–7 years age group.[4] Similarly, non-nutritive sucking, swaddling, and rocking have been found useful in neonates and infants.[5] Local anaesthesia creams containing a mixture of lignocaine with prilocaine or tetracaine - like Prilox® (Neon Laboratories Ltd. Mumbai, India) and Tetralid® (Ajanta Pharma Ltd. Mumbai, India) applied in occlusive dressings an hour prior can help reduce the pain of vascular access. Not more than 1 gm for infants <5 kg and 2 gm for 5–10 kg is recommended.[6] Oral sucrose has been shown to reduce procedural pain in neonates.[7] Sedation or general anaesthesia is required for central venous access. Vascular access should be taken over clean and healthy skin. Skin cleaning with 2% chlorhexidine in 70% alcohol is recommended for antisepsis. In preterm neonates and infants less than 2 months, 2% chlorhexidine is not approved for use by FDA due to skin absorption and irritation. However, 10% povidone-iodine or 0.5% chlorhexidine can be used in this age group.[8,9] Donning clean gloves for self-protection should be done for peripheral venous cannulation, whereas arterial, central, and long-term venous cannulations should be done under aseptic precautions. Use of transparent non-occlusive dressings over vascular cannulation allows monitoring for complications. Chlorhexidine impregnated dressings are preferred to reduce infective complications when longer dwell times are anticipated.[10] Antibiotic prophylaxis is not needed for vascular access except in implantable port placements, immunocompromised, and high-risk neonates.[11]
Aids and devices for vascular access placement
The difficulty of venous access in children can be predicted using difficult intravenous access (DIVA) score and appropriate aids or devices may be used for cannulation in such patients.[12] Simple techniques such as tourniquet, tapping over the vein, and local warming of the area can improve the success of peripheral venous access by local vasodilation. Local vasodilation can also be achieved by epidermal nitroglycerin, which is especially helpful after vasoconstricting effects of local anaesthetic cream.[13]
Transillumination technique facilitates the placement of peripheral venous cannula by highlighting the veins as light passes through the thin connective tissues in children <2 years. Light-emitting diodes are preferred over the regular light as they have greater transillumination power and lesser risk of burns.[14] Near-infrared devices help to identify the superficial veins that cannot be visualised or palpated. The haemoglobin in the blood absorbs the infrared light thus delineating veins. Multiple devices are available in the market with no significant benefit of one over the other.[15] A systematic review and meta-analysis performed of near-infrared light devices demonstrate their utility mainly in difficult vascular access situations.[16] Figure 2 impresses the effect of infrared and transillumination techniques in a patient with difficult venous access.
Figure 2.
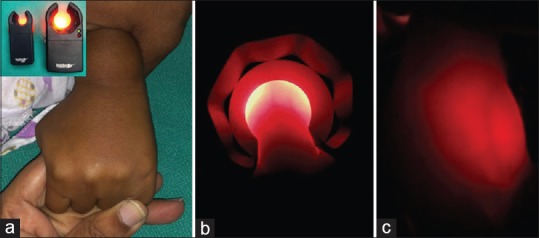
Techniques for difficult peripheral venous cannulation. (a) shows dorsum of hand with non-visible and non-palpable veins. Inset shows adult and paediatric infrared vein visualizing device. (b and c) show veins visualised by infrared and transillumination techniques, respectively
The role of ultrasound in all types of vascular access - peripheral, central, and arterial - is well established. However, ultrasound is expensive, requires training and competency. The availability and licensing requirements for ultrasound in our country limit its widespread use. International evidence-based recommendations on ultrasound-guided vascular access suggest using ultrasound not only to guide catheter placement but also to select the appropriate size of catheter, verify catheter tip placement, and rule out catheter-related complications.[17] Rapid central venous assessment approach is a standardised approach recommended before central venous catheterisation.[18] High frequency (5–18 Hz) linear array hockey-stick ultrasound probe with a small footprint of 25 mm is preferred. Echogenic needles have been tried to improve real time visualisation during placement with variable success.[19] The oblique-axis view for vascular cannulation is superior over long-axis and short-axis views, which have a lower success rate and higher mechanical complication rate, respectively.[20]
Radiological confirmation is desirable for all central venous accesses for verifying the direction of catheter and tip position. Fluoroscopy is recommended for long-term venous access such as PICC, tunneled catheters, and implantable ports.
TYPES OF VASCULAR ACCESS
Table 1 depicts the various methods of vascular access in children and compares the advantages, disadvantages, and the sizes of catheters used for the access. A brief description of each vascular access is also included. Figure 3 is a pictorial representation of the type-wise common locations of vascular access in children.
Table 1.
Comparison of different vascular accesses
| Type of access | Common sites | Catheter sizes | Dwell time | Advantages | Disadvantages |
|---|---|---|---|---|---|
| Peripheral venous access | Dorsum of hand and leg, antecubital, great saphenous vein, external jugular, scalp veins | 26 G, 24 G (neonates) 22 G (infants) 20 G (children) |
Short termUp to 5 days | Simple, cost effective, minimal complications | Short term, can’t withdraw blood |
| Midline access | Deep veins of arm or forearm | 24 G (neonates) 22 G (infants) 20 G (children) |
Intermediate-termUp to 14 days | Longer dwell time, ease of insertion, no radiological confirmation needed | Can’t withdraw blood, only peripherally compatible solutions can be used |
| PICC (peripheral inserted central catheter) access | Basillic vein, brachial vein, cephalic vein (size of catheter <one-third of vein diameter) | 1 Fr (neonates) 2 Fr (infants) 3 Fr (smaller children) 4 Fr (older children) |
Intermediate-term Few weeks to few months* |
Blood sampling possible, patient can be sent home | Needs training and expertise, radiological confirmation needed, device care patient training required |
| Non-tunneled central venous access | Internal jugular, subclavian, and femoral veins | 3 Fr (neonates) 4 Fr (infants) 5 Fr (smaller children) 7 Fr (older children) |
Short term 1-2 weeks |
Multiple lumens, CVP monitoring, hyperosmolar, and irritant drugs | Limited duration use due to the risk of infection, Patient cannot be sent home |
| Tunneled central venous access (Hickmann’s/Broviac) | Subclavian vein, internal jugular veins (right side preferably) | 4.2 Fr Broviac (infants) 6.6 Fr Broviac (smaller children) 7 Fr Hickman’s (smaller children) 9 Fr Hickman’s (older children) |
Long term 1-6 months |
Blood sampling possible, high rate of infusion and blood draw possible | Needs training and expertise, radiological confirmation needed, costly device, device care patient training required, needs surgical removal |
| Implantable port access | Subclavian vein, internal jugular | 4 Fr (infants) 5.5 Fr (smaller children) 7 Fr (older children) |
Long term >3 months to few years | Longevity of access, least chances of infection, preserves body image | Elaborate placement technique, costly device, needs surgical removal |
| Intra-osseous access | Proximal tibia, distal tibia, distal femur, proximal humerus | 15 G needles 15 mm (3 - 39 kg) 25 mm (> 40 kg) 45 mm (> 40 kg and excessive soft tissue) |
Emergency access <24 hours | Useful in emergency settings, quick access, requires less skill and training than central venous access | Require simple training |
| Arterial access | Radial artery, ulnar artery, femoral artery, Posterior tibial | 24 G (neonates) 24 G or 22 G (infants) 22 G or 20 G (children) |
Short term Up to 7 days |
Beat to beat blood pressure monitoring, blood gas sampling | Arterial injury, arterial occlusion |
| Umbilical access (venous and arterial) | Umbilical cord | 3.5 Fr for low birth weight babies, 5 Fr for term neonates | Short term Up to 7 days |
Useful in emergency settings, easy access, frequent blood sampling | Requires simple training |
G - Gauge; Fr – French; *Up to a year if catheter is viable
Figure 3.
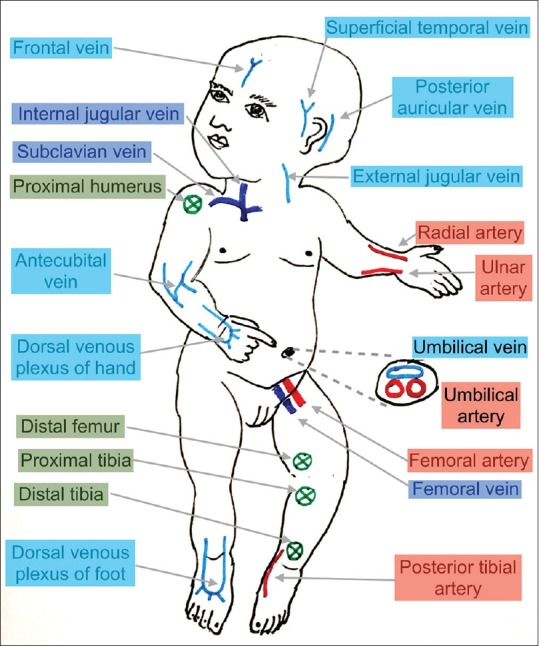
Common vascular access locations for peripheral venous access (light blue), central venous access (dark blue), arterial access (red), and intraosseous access (green)
I. Peripheral venous access
Peripheral venous access is the most common vascular access, and veins in the dorsal venous plexus of the hand are preferred. One should be well-versed with venous anatomy and common sites for cannulation in children [Figure 3]. Veins on the leg should be avoided as they promote the immobilisation of the child. Care should be taken while accessing antecubital fossa veins to avoid inadvertent arterial cannulation. The external jugular vein is available as additional wide bore access in case of unexpected intraoperative haemorrhage. Collapsed vein, loose skin, and shallow angle of penetration add to the challenges of cannulating this vein. Scalp veins can be accessed in the neonatal or infant age group when adequate peripheral access is not available. DIVA score is useful in predicting difficult peripheral vascular access using four variables – vein visibility, palpability, age, and prior neonatal intensive care stay[12] but requires adequate external validation. It is recommended to use the smallest size of the peripheral cannula that is required to serve the purpose, except in the emergency and unstable patients, where a larger cannula can be selected. Stabilizing the vein and stretching the skin help to prevent rolling of the vein. The catheter is entered at an angle of 10–25° till give-way feel and backflow is visible, after which the angle of insertion can be further dropped till the catheter can be threaded in the vein. Once placed, the cannula and the limb need to be supported with a splint to avoid dislodgement during child's activity. Care must be taken to avoid ischaemia and pressure injuries.
II. Midline access
Midline access is peripheral venous access useful in prolonged antibiotic treatments. The midline catheter - Seldipur Smartmidline® (Vygon, Ecouen, France) - about 6 to 12 cm long, is inserted in deep veins of the arm under ultrasound guidance. Alternatively, a long peripheral cannula can be placed in mid-arm veins. Although currently underutilised, this seems promising access for children undergoing surgery, where a single venous cannula can suffice the duration of care.[21]
III. Peripherally inserted central catheter access
Peripherally inserted central catheter (PICC) access is an intermediate-term vascular access inserted in one of the deep arm veins – basilic, brachial, or cephalic - with the tip lying in the junction of superior vena cava and right atrium. In older children, ultrasound-guided Seldinger technique using sheath over dilator is used for placement e.g., POLY PER-Q-CATH® (Bard Access systems Inc., UT 84116, USA). In neonates, cubital or saphenous veins are cannulated using sheath over needle apparatus e.g., Polyurethane Epicutaneous-Cave catheter® (Vygon, Ecouen, France). It is a central line and can be used for blood sampling if catheter size more than 3 Fr. Valved PICCs e.g., GROSHONG® (Bard Access systems Inc., UT 84116, USA) have the same incidence of catheter occlusions as compared to open-ended PICCs but have the advantage of avoiding heparin for flushing.[22] Power-injectable PICCs like POWERPICC® (Bard Access systems Inc., UT 84116, USA) are designed to withstand the higher pressures of computed tomography contrast infusion and are preferred in oncological patients who may require frequent scans.[23]
IV. Non-tunneled central venous access
The common indications for central venous access are vasopressors use, parenteral nutrition, chemotherapy, and poor peripheral venous access. It is contraindicated in local infections, severe coagulation, or platelet abnormalities without correction.
Principles of cannulation
Seldinger technique is the safest method of central venous cannulation. Use of ultrasound is highly recommended to increase the success rate as well as decrease the complications.[24] The ideal tip location of the central venous catheter is near the superior vena cava and right atrium junction. Any other position has a higher chance of vessel injury, thrombosis, or arrhythmias. Various techniques to confirm tip location include electrocardiographic, ultrasound–guided, and radiological assistance. Electrocardiographic needs special equipment, ultrasound-guided needs additional personnel, and radiological is associated with radiation hazard. Hence, the choice may be personal according to the setup. Measuring the distance between entry point to the sternal angle is a reliable landmark guided technique.[25] The internal jugular vein is preferred for low complications and ease of ultrasound guidance. The subclavian vein is alternatively preferred being a non-collapsible vein with fixed landmarks, more comfort, and low infection rates. Femoral vein is less preferred owing to a higher risk of infections. The overall catheter-related infection rates for neonatal central lines are significantly higher than adult central lines.[26]
Internal jugular vein cannulation technique: Ultrasound guided cannulation is the standard of care. The landmark guided internal jugular vein (IJV) cannulation is described using an anterior, central, or posterior approach. In children, the higher anterior approach is preferred by many to reduce the chances of pneumothorax. The needle enters from the medial edge of sternocleidomastoid at the level of the thyroid cartilage and is directed toward the ipsilateral nipple. Simulated Valsalva in a ventilated patient, pressure on liver, and Trendelenburg position help to increase IJV size during cannulation. Head should be turned slightly to the contralateral side. Excessive head rotation in children can collapse the IJV and also bring it too close to the carotid artery. Owing to low-pressure compressible IJV, there is a possibility of a counter puncture in children and aspiration should be done while withdrawing the needle. There is a higher risk of vertebral artery puncture in younger children, owing to its proximity[27]
Subclavian vein cannulation technique: The technique of placement is similar to adults, with puncture point at the junction of medial two-third and lateral one-third of the clavicle, and the needle pointing toward the sternal notch, just below the clavicle. The chances of malposition are higher with subclavian than that of the internal jugular vein. Ultrasound guidance for the subclavian vein is difficult because of the clavicle overlapping the vein. Instead, the brachiocephalic vein is well accessible for ultrasound-guided cannulation and can be considered in neonates and infants[28]
Femoral vein cannulation technique: Femoral vein cannulation is similar to that in adults, with the puncture point medial to the palpable femoral artery, and 1–2 cm below the inguinal ligament. Ultrasound-guided cannulation is considered the best practice.[29]
V. Tunneled central venous access
Hickman and Broviac are tunneled catheters that are used when large bore access is required for longer duration treatments such as chemotherapy, plasmapheresis, and bone marrow transplantation. The catheters have a Dacron cuff that helps sealing of the subcutaneous tract from the exit point to the vessel puncture, thus reducing infections. Special care and precautions required for handling the catheter should be taught to the patient's family. The right subclavian vein is usually preferred for tunneled catheters due to the ease of placement. However, it can be placed in subclavian or internal jugular of either side. Vessel puncture is done using Seldinger technique, and the catheter is tunneled subcutaneously away from the vessel entry point in inferomedial direction at least 8–10 cm away such that the Dacron cuff lies 3–4 cm inside the newer exit point. Details regarding the placement technique can be read elsewhere.[30]
VI. Implantable port access
Implantable ports are preferred when vascular access is required intermittently for longer duration treatments, such as chemotherapy, enzyme replacement therapy, and long-term parenteral nutrition. Port is placed under the skin and is accessed with Huber tip needles. It has a port body with silicone diaphragm that can withstand more than 1000 punctures, connected to a silicone or polyurethane catheter, which is placed in the central vein. The IJV or subclavian access of the central vein is taken and port pocket is created on the anterior part of the chest, under the clavicle. The catheter is then railroaded into the port pocket. The wound is closed in two layers after achieving haemostasis. Details regarding the placement technique can be read elsewhere.[30] Ports preserve body image and allow a shower or swim, unlike tunneled catheters.
VII. Intraosseous access
Intraosseous access is emergency access that all anaesthesiologists should learn. In peri-arrest situations, if the peripheral access cannot be secured in 1 min, intraosseous needle should be placed.[31] EZ-IO® (Teleflex Incorporated, USA) 15 G (15 mm and 25 mm) needles are available with powered gun to aid the placement. In case of non-availability of those, a wide bore needle with a trocar or bone marrow needle may be used. Intraosseous access is temporary access and should not be maintained for longer than 24 h. The most preferred site is proximal or distal tibia. If the selected bone is fractured or has a prior failed intraosseous attempt, it should not be used for intraosseous access. The needle is screwed perpendicularly down, away from the growth plate, till loss of resistance is felt and the needle grips to the bone. Inability to aspirate marrow does not refute correct placement, but saline flush should not cause local swelling. The needle support device is available with EZ-IO® access.
VIII. Arterial access
This is indicated for invasive blood pressure monitoring and frequent arterial blood gas analysis. In neonates, the umbilical artery can be used. In children, radial artery, femoral artery, and posterior tibial artery are commonly used. Role of modified Allen's test before radial artery cannulation is controversial.[32] Ultrasound guidance for radial artery cannulation improves the success rate and reduces complications as compared with palpation or Doppler auditory assistance.[33]
IX. Umbilical access
Umbilical venous access is indicated in neonatal resuscitation, exchange transfusion, central venous pressure monitoring, fluid, and medication infusion when peripheral venous access is unavailable. Both umbilical venous and arterial access cannot be used in omphalitis, peritonitis, and necrotizing enterocolitis. Under aseptic precautions, thin-walled single umbilical vein at 12'oclock position in the umbilical cord stump is identified. An umbilical tape is applied around the base of the umbilical cord; umbilical vein is dilated with artery forceps and catheterised with gentle caudal stretch up to 4–5 cm. Free backflow of blood is verified and catheter secured to the umbilical cord with tapes. If central venous monitoring is desirable, it is pushed 10–12 cm deep and the position of the tip confirmed radiologically. Two-third of the distance from shoulder to umbilicus correlates with correct placement of tip of the catheter in inferior vena cava just below the right atrium.[34]
Umbilical arterial access is performed for arterial blood pressure monitoring, blood gases sampling, and exchange transfusions in neonates. Placement technique is similar to umbilical vein except that one of two thick-walled umbilical arteries is selected. The catheter is flushed with heparinised saline to avoid inadvertent air bubbles. The umbilical artery is opened with the tip of the curved artery forceps with steady pressure and catheterised without undue pressure. Lignocaine 2% may be trickled to break the arterial spasm. The high position of umbilical artery catheter - between thoracic vertebrae T6 and T9 - is preferred over the low position - between lumbar vertebrae L3 and L4. The formula used to calculate the insertion depth in centimeters is 9+ (3 × weight in Kg).[35] The radiological position of tip of the catheter should be between the 6th and 9th thoracic vertebrae on chest X-ray.
COMPLICATIONS OF VASCULAR ACCESS
A complete discussion on the complications of vascular access is beyond the scope of this article. Common complications encountered with the respective accesses are compiled in Table 2. Early complications occur during placement and can be avoided by following safe placement techniques. Late complications could be infective or mechanical. Aseptic precautions during placement, hand hygiene, and non-touch techniques during maintenance care help to reduce the infective complications.
Table 2.
Common complications of vascular access
| Early | Late |
|---|---|
| Complications of peripheral venous access | |
| Bleeding | Thrombophlebitis |
| Hematoma | Extravasation |
| Complications of central venous access | |
| Arrhythmia | Bloodstream infection |
| Injury to adjacent structures | Catheter occlusion |
| Pneumothorax | Vein thrombosis |
| Malposition | Catheter damage |
| Air embolisation | Vein perforation |
| Complications of arterial access | |
| Bleeding | Distal ischaemia |
| Hematoma | Aneurysm |
| Injury to adjacent structures | Arterial thrombosis |
| Complications of intraosseous access | |
| Hematoma | Cellulitis |
| Extravasation | Compartment syndrome |
| Bone fracture | Osteomyelitis |
| Complications of umbilical access | |
| Vessel perforation | Infection |
| Malposition | Vessel thrombosis |
| False tract | Catheter damage |
DECISION TREE FOR VENOUS ACCESS IN CHILDREN
The choice of venous access depends on the indication, infusate characteristics, and the anticipated duration of the access. Selection of venous access depending on infusate characteristics is depicted in Table 3. Patient factors such as - a chubby child, thrombophlebitis, and multiple hospitalisations - may also affect the choice because of limited peripheral venous access. We recommend the venous access placement decision tree shown in Figure 1b in children excluding infants and neonates.
Table 3.
Selection of venous access based on infusate properties
| Infusate property | Central venous access | Peripheral venous access |
|---|---|---|
| pH | < 5 and >9 | between 5 and 9 |
| Osmolarity | >600 mOsm/L | < 600 mOsm/L |
| Final dextrose concentration | > 10% | < 10% |
| Tonicity | Hypo/hypertonic | Isotonic |
| Irritant, Vesicant | Yes | No |
FUTURE DIRECTIONS
Safety in paediatric vascular access can be increased by incorporating evidence-based protocols in placement and maintenance care. Attempts should be made to improve the quality and homogeneity of data generated in literature. This can be achieved by forming a global paediatric vascular access registry to report practices and outcomes.[36] Similarly, a multidisciplinary vascular access team can be considered for a comprehensive approach within each hospital. Such teams seem promising in improving care and reducing vascular access-related complications.[37] Anaesthesiologists have the right skill set and should lead vascular access teams.
SUMMARY
Paediatric vascular access can be challenging. Denying or delaying treatment due to lack of vascular access is unacceptable. Anaesthesiologists should gain the knowledge of various vascular access types and devices. Right choice of vascular access at the right time can save lives.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bodenham Chair A, Babu S, Bennett J, Binks R, Fee P, Fox B, et al. Association of Anaesthetists of Great Britain and Ireland: Safe vascular access 2016. Anaesthesia. 2016;71:573–85. doi: 10.1111/anae.13360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lininger RA. Pediatric peripheral i.v. insertion success rates. Pediatr Nurs. 2003;29:351–4. [PubMed] [Google Scholar]
- 3.Harrison D, Reszel J, Bueno M, Sampson M, Shah VS, Taddio A, et al. Breastfeeding for procedural pain in infants beyond the neonatal period. Cochrane Database Syst Rev. 2016;10:CD011248. doi: 10.1002/14651858.CD011248.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuo HC, Pan HH, Creedy DK, Tsao Y. Distraction-based interventions for children undergoing venipuncture procedures: A randomized controlled study. Clin Nurs Res. 2018;27:467–82. doi: 10.1177/1054773816686262. [DOI] [PubMed] [Google Scholar]
- 5.Pillai Riddell RR, Racine NM, Gennis HG, Turcotte K, Uman LS, Horton RE, et al. Non-pharmacological management of infant and young child procedural pain. Cochrane Database Syst Rev. 2015;12:CD006275. doi: 10.1002/14651858.CD006275.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.EMLA, Oraqix (lidocaine/prilocaine) dosing, indications, interactions, adverse effects, and more [Internet] [Last accessed on 2019 Jul 25]. Available from: https://reference.medscape.com/drug/emla-oraqix-lidocaine-prilocaine-343663 .
- 7.Stevens B, Yamada J, Ohlsson A, Haliburton S, Shorkey A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst Rev. 2016;7:CD001069. doi: 10.1002/14651858.CD001069.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paternoster M, Niola M, Graziano V. Avoiding chlorhexidine burns in preterm infants. J ObstetGynecol Neonatal Nurs. 2017;46:267–71. doi: 10.1016/j.jogn.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Linder N, Prince S, Barzilai A, Keller N, Klinger G, Shalit I, et al. Disinfection with 10% povidone-iodine versus 0.5% chlorhexidine gluconate in 70% isopropanol in the neonatal intensive care unit. Acta Paediatr. 2004;93:205–10. doi: 10.1080/08035250310008159. [DOI] [PubMed] [Google Scholar]
- 10.Ullman AJ, Cooke ML, Mitchell M, Lin F, New K, Long DA, et al. Dressing and securement for central venous access devices (CVADs): A Cochrane systematic review. Int J Nurs Stud. 2016;59:177–96. doi: 10.1016/j.ijnurstu.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 11.Rupp SM, Apfelbaum JL, Blitt C, Caplan RA, Connis RT, Domino KB, et al. Practice guidelines for central venous access: A report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology. 2012;116:539–73. doi: 10.1097/ALN.0b013e31823c9569. [DOI] [PubMed] [Google Scholar]
- 12.Yen K, Riegert A, Gorelick MH. Derivation of the DIVA score: A clinical prediction rule for the identification of children with difficult intravenous access. Pediatr Emerg Care. 2008;24:143–7. doi: 10.1097/PEC.0b013e3181666f32. [DOI] [PubMed] [Google Scholar]
- 13.Andrew M, Barker D, Laing R. The use of glyceryl trinitrate ointment with EMLA cream for i.v. cannulation in children undergoing routine surgery. Anaesth Intensive Care. 2002;30:321–5. doi: 10.1177/0310057X0203000309. [DOI] [PubMed] [Google Scholar]
- 14.Hosokawa K, Kato H, Kishi C, Kato Y, Shime N. Transillumination by light-emitting diode facilitates peripheral venous cannulations in infants and small children. Acta Anaesthesiol Scand. 2010;54:957–61. doi: 10.1111/j.1399-6576.2010.02270.x. [DOI] [PubMed] [Google Scholar]
- 15.de Graaff JC, Cuper NJ, Mungra RA, Vlaardingerbroek K, Numan SC, Kalkman CJ. Near-infrared light to aid peripheral intravenous cannulation in children: A cluster randomised clinical trial of three devices. Anaesthesia. 2013;68:835–45. doi: 10.1111/anae.12294. [DOI] [PubMed] [Google Scholar]
- 16.Park JM, Kim MJ, Yim HW, Lee WC, Jeong H, Kim NJ. Utility of near-infrared light devices for pediatric peripheral intravenous cannulation: A systematic review and meta-analysis. Eur J Pediatr. 2016;175:1975–88. doi: 10.1007/s00431-016-2796-5. [DOI] [PubMed] [Google Scholar]
- 17.Lamperti M, Bodenham AR, Pittiruti M, Blaivas M, Augoustides JG, Elbarbary M, et al. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med. 2012;38:1105–17. doi: 10.1007/s00134-012-2597-x. [DOI] [PubMed] [Google Scholar]
- 18.Spencer TR, Pittiruti M. Rapid Central Vein Assessment (RaCeVA): A systematic, standardized approach for ultrasound assessment before central venous catheterization. J Vasc Access. 2019;20:239–49. doi: 10.1177/1129729818804718. [DOI] [PubMed] [Google Scholar]
- 19.Crum T, Adhikari S, Lander L, Blaivas M. Do echo-enhanced needles make a difference in sonographically guided vascular access? J Ultrasound Med. 2014;33:623–8. doi: 10.7863/ultra.33.4.623. [DOI] [PubMed] [Google Scholar]
- 20.Batllori M, Urra M, Uriarte E, Romero C, Pueyo J, Lopez-Olaondo L, et al. Randomized comparison of three transducer orientation approaches for ultrasound guided internal jugular venous cannulation. Br J Anaesth. 2016;116:370–6. doi: 10.1093/bja/aev399. [DOI] [PubMed] [Google Scholar]
- 21.Pacilli M, Bradshaw CJ, Clarke SA. Use of 8-cm 22G-long peripheral cannulas in pediatric patients. J Vasc Access. 2018;19:496–500. doi: 10.1177/1129729818761278. [DOI] [PubMed] [Google Scholar]
- 22.Johnston AJ, Streater CT, Noorani R, Crofts JL, Del Mundo AB, Parker RA. The effect of peripherally inserted central catheter (PICC) valve technology on catheter occlusion rates--the 'ELeCTRiC' study. J Vasc Access. 2012;13:421–5. doi: 10.5301/jva.5000071. [DOI] [PubMed] [Google Scholar]
- 23.Xu B, Zhang J, Tang S, Hou J, Ma M. Comparison of two types of cathetersthrough femoral vein catheterization in patients with lung cancer undergoing chemotherapy: A retrospective study. J Vasc Access. 2018;19:651–7. doi: 10.1177/1129729818769227. [DOI] [PubMed] [Google Scholar]
- 24.Lau CS, Chamberlain RS. Ultrasound-guided central venous catheter placement increases success rates in pediatric patients: A meta-analysis. Pediatr Res. 2016;80:178–84. doi: 10.1038/pr.2016.74. [DOI] [PubMed] [Google Scholar]
- 25.Chaskar V, Karnik PP, Dave NM, Garasia M. Comparative study of three methods for depth of central venous catheter placement in children: An observational pilot study. Turk J Anaesthesiol Reanim. 2018;46:116–20. doi: 10.5152/TJAR.2018.32748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leblebicioglu H, Erben N, Rosenthal VD, Atasay B, Erbay A, Unal S, et al. International Nosocomial Infection Control Consortium (INICC) national report on device-associated infection rates in 19 cities of Turkey, data summary for 2003-2012. Ann Clin Microbiol Antimicrob. 2014;13:51. doi: 10.1186/s12941-014-0051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jung CW, Jalilov G, Song IK, Kim EH, Kim HS, Kim JT, et al. Position and relative size of the vertebral artery according to age: Implications for internal jugular vein access. Paediatr Anaesth. 2017;27:997–1002. doi: 10.1111/pan.13209. [DOI] [PubMed] [Google Scholar]
- 28.Breschan C, Graf G, Jost R, Stettner H, Feigl G, Neuwersch S, et al. A Retrospective Analysis of the Clinical Effectiveness of Supraclavicular, Ultrasound-guided Brachiocephalic Vein Cannulations in Preterm Infants. Anesthesiology. 2018;128:38–43. doi: 10.1097/ALN.0000000000001871. [DOI] [PubMed] [Google Scholar]
- 29.Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015;1:CD011447. doi: 10.1002/14651858.CD011447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Naik V, Rao K, Rayani B, Subrahmanyam M, Subrahmanyam R. Long-term venous access devices and anaesthesiologists. Update in Anaesthesia [Internet] 2019;33:62–9. [Google Scholar]
- 31.Monsieurs KG, Nolan JP, Bossaert LL, Greif R, Maconochie IK, Nikolaou NI, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1.Executive summary. Resuscitation. 2015;95:1–80. doi: 10.1016/j.resuscitation.2015.07.038. [DOI] [PubMed] [Google Scholar]
- 32.Romeu-Bordas Ó, Ballesteros-Peña S. Reliability and validity of the modified Allen test: A systematic review and metanalysis. Emergencias. 2017;29:126–35. [PubMed] [Google Scholar]
- 33.Aouad-Maroun M, Raphael CK, Sayyid SK, Farah F, Akl EA. Ultrasound-guided arterial cannulation for paediatrics. Cochrane Database Syst Rev. 2016;9:CD011364. doi: 10.1002/14651858.CD011364.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Magnan JP. Umbilical Vein Catheterization Technique [Internet] [Last accessed on 2019 Jun 10]. Available from: https://emedicine.medscape.com/article/80469-technique .
- 35.Shukla H, Ferrara A. Rapid estimation of insertional length of umbilical catheters in newborns. Am J Dis Child. 1986;140:786–8. doi: 10.1001/archpedi.1986.02140220068034. [DOI] [PubMed] [Google Scholar]
- 36.Schults JA, Rickard CM, Kleidon T, Hughes R, Macfarlane F, Hung J, et al. Building a global, pediatric vascular access registry: A scoping review of trial outcomes and quality indicators to inform evidence-based practice. Worldviews Evid Based Nurs. 2019;16:51–9. doi: 10.1111/wvn.12339. [DOI] [PubMed] [Google Scholar]
- 37.Legemaat MM, Jongerden IP, van Rens RM, Zielman M, van den Hoogen A. Effect of a vascular access team on central line-associated bloodstream infections in infants admitted to a neonatal intensive care unit: A systematic review. Int J Nurs Stud. 2015;52:1003–10. doi: 10.1016/j.ijnurstu.2014.11.010. [DOI] [PubMed] [Google Scholar]