Abstract
Background
Provision of postpartum care can support new families in adapting to a new situation. We aimed to determine whether various determinants of socioeconomic status (SES) were associated with utilization of postpartum care. In addition, to stress the relevance of increasing postpartum care uptake among low SES-groups, an assessment of the potential (cost-)effectiveness of postpartum care is required.
Methods
National retrospective cohort study using linked routinely collected healthcare data from all registered singleton deliveries (2010–13) in the Netherlands. Small-for-gestational age and preterm babies were excluded. The associations between SES and postpartum care uptake, and between uptake and health care expenditure were studied using multivariable regression analyses.
Results
Of all 569 921 deliveries included, 1.2% did not receive postpartum care. Among women who did receive care, care duration was below the recommended minimum of 24 h in 15.3%. All indicators of low SES were independently associated with a lack in care uptake. Extremes of maternal age, single parenthood and being of non-Dutch origin were associated with reduced uptake independent of SES determinants. No uptake of postpartum care was associated with maternal healthcare expenses in the highest quartile: aOR 1.34 (95% CI 1.10–1.67). Uptake below the recommended amount was associated with higher maternal and infant healthcare expenses: aOR 1.09 (95% CI 1.03–1.18) and aOR 1.20 (95% CI 1.13–1.27), respectively.
Conclusion
Although uptake was generally high, low SES women less often received postpartum care, this being associated with higher subsequent healthcare expenses. Strategies to effectively reduce these substantial inequities in early life are urgently needed.
Introduction
The postpartum period is a critical transitional period not only for babies but also in the lives of new mothers.1 Adequate care provision during this period by skilled maternity care professionals enables an optimal start for the new family. A healthy start following childbirth may be of substantial short and long term benefit for maternal and child wellbeing, and as such has the potential to reduce healthcare associated costs.2,3
The uptake of healthcare overall and the incidence of adverse health outcomes during the postpartum period are closely linked to different determinants of one’s socioeconomic position; persons with a lower socioeconomic position tend to make less use of routine or preventive healthcare,4,5 and have a higher incidence of adverse health outcomes.3,6–10 Although a number of studies examined this relationship, the association between SES and use of postpartum care has not been investigated previously.
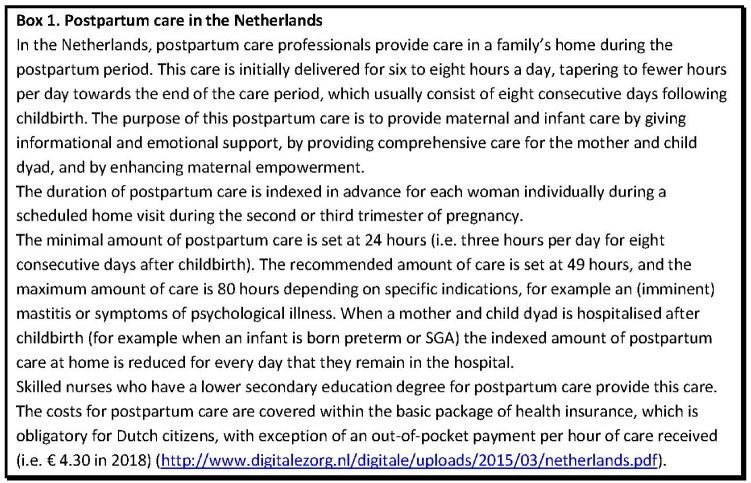
The strong position of primary care in the Netherlands, which includes easy access to postpartum care at home during the early postpartum period (figure 1), provides considerable potential to promote equity in maternal and infant health. This study seeks to describe the patterns of utilization of postpartum care services using a national population-based study, assessing: (i) whether different determinants of SES—represented by individual level, household level and area-level indicators—were associated with uptake of postpartum care and (ii) whether any inequalities translated in uptake of care translated into differences in subsequent healthcare expenditures for mother and child in the first year after childbirth, as an estimate of potential (cost-)effectiveness.
Figure 1.
Postpartum care in the Netherlands
Methods
We conducted a national population-based retrospective cohort study of women living in the Netherlands who delivered a live singleton baby between 1 January 2010 and 31 December 2013. Routinely collected healthcare and claims data were linked at the individual level across various national databases. First, we studied the association between different determinants of low SES and the uptake of postpartum care. Second, we studied the association between the uptake of postpartum care and healthcare expenditures for mother and child in the following year. We used the RECORD statement to guide reporting of our findings (Supplementary file S1).11
Study design and setting
Population-based retrospective cohort study from 1 January 2010 through 31 December 2013 using routinely collected healthcare data from Statistics Netherlands (translated Dutch name: ‘Central Bureau of Statistics’, abbreviation ‘CBS’).
Participants
All registered pregnancies among women living in the Netherlands who delivered a live singleton baby at 24 or more completed gestational weeks between 2010 and 2013.
Exposure variables
For the first part of this study, multiple determinants of SES including individual, household and area-level SES indicators constituted the exposures of interest. Disposable household income was used as an individual SES indicator, defined as the sum available from the household income for final consumption and savings (i.e. net income) and divided into quartiles. Mother’s highest educational qualification, based on the International Standard Classification of Education (ISCED) (http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf), was considered a second individual SES indicator. Three groups were considered: lower education (pre-primary, primary and lower secondary education), intermediate education (upper secondary education, post-secondary non-tertiary education) and higher education (first stage of tertiary education, second stage of tertiary education).
Home ownership was considered a household indicator of SES and was dichotomized into owner-occupiers and no-owners (i.e. renters and others).
Neighbourhood deprivation was considered an area-level SES indicator and was based on the Neighbourhood Deprivation Index (NDI) formulated by NIVEL in 2012.12 Deprivation was defined at an NDI of 5.5% (i.e. 885 000 people).
In the second part, the exposure was the uptake of any postpartum care, and—in a secondary analysis—the uptake of postpartum care above the recommended minimum (i.e. 24 h) among those who did receive postpartum care.
Covariates
Covariates were selected based on their association with the outcome variables or both the outcome and the exposure variables: maternal age, parity, country of origin, parenthood household status, level of urbanization and small-for-gestational age and preterm babies. Details are presented in Supplementary file S2.
Outcomes
Determinants of low SES and uptake of postpartum care
Uptake of postpartum care was derived from data regarding healthcare expenditures. Expenditures were provided per annum; therefore pregnancies from women who gave birth more than once within 1 year were excluded for all analysis. The amount of postpartum care was calculated by dividing the total postpartum care expenditures within 1 year by the eligible compensation per hour of care, which differed per year.13 Uptake of postpartum care was dichotomized into ‘No’, and ‘Yes’ (any amount of postpartum care). The secondary outcome was postpartum care uptake above the minimum (i.e. 24 h), as assessed among all women who did make use of postpartum care. The uptake of the minimum amount of care was dichotomized.
Uptake of postpartum care and healthcare expenditures
Annual total healthcare expenditures were obtained separately for mother and child. Quartiles of annual healthcare expenditures were formed for each and dichotomized into ‘low’ (expenses within the first three quartiles) and ‘high’ (expenses in the fourth quartile). Healthcare expenditure data were only available at an aggregated level per annum. We were therefore able to reliably evaluate health care costs in the year post-delivery only among those women delivering close to closing of the year. As such, we pragmatically considered total healthcare costs in the subsequent year following delivery in December a reasonable estimate of healthcare expenditure in the year post-delivery, and excluded deliveries in January to November from these analyses. Healthcare expenditures are subdivided based on a combination of diagnosis and treatment codes enabling us to exclude all healthcare expenses that were labelled as pregnancy-related. In addition, we excluded women with more than one pregnancy during the study period (i.e. 2010–13) because having consecutive pregnancies over a 2-year period could influence healthcare expenditures at the annual level.
Data sources and linkage
The available data for this study were linked across different national registries by CBS using the unique citizen service number (BSN) or the identification number of the Dutch Population Register (Dutch: A-number). Linkage with this information is feasible in 98–100% of all procedures undertaken by CBS. Details about the individual-level linkage across various routinely collected datasets are presented in Supplementary file S2.
Potential for bias
The data in this study are based on routinely collected healthcare data. There was a reasonably high proportion of missing values in some registries that could have introduced different biases. We applied multiple imputation using chained equations to account for this missing data in baseline characteristics. Multiple predictor variables were included to inform the multiple imputation process, forming 10 datasets. Results across the sets were combined using Rubin’s Rules.14
Statistical methods
We analysed the two associations under study using logistic regression analysis.
Infants born preterm or SGA and their mothers tend to remain in the hospital during most of the time that the mothers would otherwise be amendable to receiving postpartum care in the home situation (figure 1). Therefore, we excluded deliveries with these outcomes for all analyses because postpartum care uptake would otherwise be underestimated due to prolonged hospital admission.
Determinants of low SES and the uptake of postpartum care
The association between various determinants of low SES and postpartum care uptake (first), and uptake above the minimum (second) was analysed. All indicators of SES as exposure variables, and the predefined covariates were included in the analysis to minimize potential confounding.
Uptake of postpartum care and healthcare expenditures
The second model analysed the association between postpartum care uptake and healthcare expenditures for mother and child. We accounted for all SES indicators and all covariates included in the first model.
Sensitivity analyses
Consecutive pregnancies within the same mother have more characteristics in common than pregnancies between women. To assess whether this dependency of data affected our findings, we reran the model that analyses the first association with additional accounting for clustering at the individual level.
To assess whether the multiple imputed data were biased, we reran the two models on complete cases only.
Accessibility of protocol and programming code
Upon request all programming codes and the study protocol are available with the principal investigator.
Details of ethics approval
According to Dutch law, formal ethical assessment of the study protocol was not needed as the study did not involve an intervention and data from CBS are anonymized [based on guidance from the Central Committee on Research Involving Human Subjects (WMO) and the Dutch Personal Data Protection Act].
CBS collects and produces population statistics, referred to as non-public microdata, for all registered Dutch citizens. Under strict conditions, these data are accessible for scientific research. The research board of CBS has reviewed and approved the study protocol (project number 7883).
Results
Participants
During the study period, 683 163 deliveries were registered with CBS. After applying the pre-specified exclusion criteria, the final sample included 569 921 deliveries (Supplementary figure S1). For investigation of the association between postpartum care uptake and healthcare expenditures, we additionally excluded deliveries in January through November, and consecutive pregnancies within individual women during the study period. The final sample for this analysis contained 44 458 deliveries (Supplementary figure S1).
Determinants of low SES and uptake of postpartum care
Univariable associations
Table 1 presents the descriptive statistics for the study sample, by uptake of postpartum care. Of all deliveries included, 1.2% did not receive any postpartum care. Data on the uptake of postpartum care were missing for 4.8% of all deliveries. Women who did not use postpartum care were more often: multiparous (67.9% vs. 54.2%), single parents (20.1% vs. 7.7%), born outside the Netherlands (2.9% vs. 0.6%) and they more often lived in deprived neighbourhoods (19.1% vs. 6.8%; table 1). Among women who did receive postpartum care, care duration was below the recommended minimum of 24 h in 15.3% (Supplementary table S1). These deliveries were also associated with indicators of low SES when compared with deliveries with postpartum care uptake above the minimum amount (Supplementary table S1).
Table 1.
Descriptive statistics of all deliveries by uptake of postpartum care (yes, no, missing)
| Postpartum care uptake | ||||||||
|---|---|---|---|---|---|---|---|---|
| Total population | Yes | No | Missing | |||||
| n=569 921 | % | n=535 470 | % | n=6833 | % | n=27 618 | % | |
| Maternal age | ||||||||
| <20 | 6837 | 1.2 | 6231 | 1.2 | 237 | 3.5 | 369 | 1.3 |
| 20–40 | 552 753 | 97.0 | 519 882 | 97.1 | 6325 | 92.6 | 26 546 | 96.1 |
| >40 | 10 331 | 1.8 | 9357 | 1.7 | 271 | 4.0 | 703 | 2.5 |
| Parity | ||||||||
| Primiparous | 259 330 | 45.5 | 245 298 | 45.8 | 2196 | 32.1 | 11 836 | 42.9 |
| Multiparous | 310 591 | 54.5 | 290 172 | 54.2 | 4637 | 67.9 | 15 782 | 57.1 |
| Country of origin | ||||||||
| The Netherlands | 414 243 | 72.7 | 393 408 | 73.5 | 2544 | 37.2 | 18 291 | 66.2 |
| Morocco | 24 726 | 4.3 | 22 920 | 4.3 | 980 | 14.3 | 826 | 3.0 |
| Turkey | 18 985 | 3.3 | 17 989 | 3.4 | 515 | 7.5 | 481 | 1.7 |
| Suriname | 13 802 | 2.4 | 12 864 | 2.4 | 372 | 5.4 | 566 | 2.0 |
| Netherlands Antilles | 6503 | 1.1 | 5864 | 1.1 | 189 | 2.8 | 450 | 1.6 |
| Other Non-Western | 36 253 | 6.4 | 32 077 | 6.0 | 1216 | 17.8 | 2960 | 10.7 |
| Other Western | 55 409 | 9.7 | 50 348 | 9.4 | 1017 | 14.9 | 4044 | 14.6 |
| Parenthood status | ||||||||
| Single parent | 44 576 | 7.8 | 41 130 | 7.7 | 1377 | 20.2 | 2069 | 7.5 |
| Two parents | 521 140 | 91.4 | 491 138 | 91.7 | 5184 | 75.9 | 24 818 | 89.9 |
| Other | 4197 | 0.7 | 3195 | 0.6 | 272 | 4.0 | 730 | 2.6 |
| Missing | 8 | 0.0 | 7 | 0.0 | 0 | 0.0 | 1 | 0.0 |
| Urbanized area | ||||||||
| Yes | 163 610 | 28.7 | 155 696 | 29.1 | 1247 | 18.2 | 6667 | 24.1 |
| No | 406 311 | 71.3 | 379 774 | 70.9 | 5586 | 81.8 | 20 951 | 75.9 |
| SES indicators | ||||||||
| Education | ||||||||
| Lower education | 74 984 | 13.2 | 70 317 | 13.1 | 2052 | 30.0 | 2615 | 9.5 |
| Intermediate education | 163 305 | 28.7 | 156 371 | 29.2 | 1438 | 21.0 | 5496 | 19.9 |
| Higher education | 197 725 | 34.7 | 184 817 | 34.5 | 955 | 14.0 | 11 953 | 43.3 |
| Missing | 133 907 | 23.5 | 123 965 | 23.2 | 2388 | 34.9 | 7554 | 27.4 |
| Low-disposable income | ||||||||
| Yes | 131 290 | 23.0 | 122 207 | 22.8 | 3445 | 50.4 | 5638 | 20.4 |
| No | 416 580 | 73.1 | 393 035 | 73.4 | 2993 | 43.8 | 20 552 | 74.4 |
| Missing | 22 051 | 3.9 | 20 228 | 3.8 | 395 | 5.8 | 1428 | 5.2 |
| Home ownership | ||||||||
| No-owners | 146 307 | 25.7 | 135 846 | 25.4 | 3984 | 58.3 | 6477 | 23.5 |
| Owner-occupiers | 401 563 | 70.5 | 379 396 | 70.9 | 2454 | 35.9 | 19 713 | 71.4 |
| Missing | 22 051 | 3.9 | 20 228 | 3.8 | 395 | 5.8 | 1428 | 5.2 |
| Neighbourhood deprivation | ||||||||
| Yes | 39 526 | 6.9 | 36 248 | 6.8 | 1305 | 19.1 | 1973 | 7.1 |
| No | 530 395 | 93.1 | 499 222 | 93.2 | 5528 | 80.9 | 25 645 | 92.9 |
Values are presented as numbers and percentage.
Multivariable associations
All indicators of low SES were consistently and strongly associated with no uptake of postpartum care after mutual adjustment (table 2). Similarly, among mothers who did receive postpartum care, low SES indicators were associated with care uptake below the minimum (table 2). Extremes of maternal age, single parenthood and being of non-Dutch origin were associated with reduced uptake of postpartum care independent of individual and area-level SES.
Table 2.
Multivariable models of the association between SES indicators and 1) postpartum care uptake and 2) uptake above the minimum (i.e. 24 h)
| Postpartum care uptake (n = 569 921) | Uptake above the minimum amount (n = 535 470) | |||
|---|---|---|---|---|
| aOR (95% CI) | P value | aOR (95% CI) | P value | |
| Covariates | ||||
| Maternal age | ||||
| <20 years | 0.70 (0.61–0.81) | <0.001 | 0.57 (0.54–0.60) | <0.001 |
| 20–40 years (ref) | 1 | 1 | ||
| >40 years | 0.53 (0.47–0.60) | <0.001 | 0.78 (0.73–0.82) | <0.001 |
| Parity | ||||
| Primiparous (ref) | 1 | 1 | ||
| Multiparous | 0.59 (0.55–0.62) | <0.001 | 0.99 (0.98–1.01) | 0.601 |
| Parenthood | ||||
| Single parent | 0.82 (0.76–0.88) | <0.001 | 0.82 (0.80–0.84) | <0.001 |
| Two parents (ref) | 1 | 1 | ||
| Other | 0.22 (0.19–0.25) | <0.001 | 0.40 (0.37–0.43) | <0.001 |
| Country of origin | ||||
| The Netherlands (ref) | 1 | 1 | ||
| Morocco | 0.37 (0.34–0.40) | <0.001 | 0.23 (0.22–0.24) | <0.001 |
| Turkey | 0.44 (0.40–0.49) | <0.001 | 0.26 (0.25–0.27) | <0.001 |
| Suriname | 0.46 (0.41–0.51) | <0.001 | 0.29 (0.28–0.30) | <0.001 |
| Net. Antilles | 0.50 (0.43–0.58) | <0.001 | 0.32 (0.30–0.34) | <0.001 |
| Other Non-Western | 0.40 (0.37–0.43) | <0.001 | 0.22 (0.22–0.23) | <0.001 |
| Other Western | 0.41 (0.41–0.48) | <0.001 | 0.41 (0.40–0.42) | <0.001 |
| SES indicators | ||||
| Individual | ||||
| Education | ||||
| Lower education | 0.62 (0.57–0.66) | <0.001 | 0.65 (0.64–0.67) | <0.001 |
| Inter. education (ref) | 1 | 1 | ||
| Higher education | 1.21 (1.12–1.32) | <0.001 | 1.39 (1.36–1.42) | <0.001 |
| Low-disposable income | ||||
| Yes | 0.72 (0.68–0.77) | <0.001 | 0.69 (0.68–0.71) | <0.001 |
| Household | ||||
| Home ownership | ||||
| No-owners | 0.55 (0.52–0.59) | <0.001 | 0.51 (0.50–0.52) | <0.001 |
| Owner-occupiers (ref) | 1 | 1 | ||
| Area-level | ||||
| Neighbourhood deprivation | ||||
| Yes | 0.80 (0.75–0.85) | <0.001 | 0.79 (0.77–0.81) | <0.001 |
Presented are adjusted odds ratios (aOR) and their 95% confidence intervals (95%CI). All p-values are two-sided. Results for the uptake of care and the minimum uptake of care are presented separately.
Sensitivity analyses
Consistent results were obtained in all sensitivity analyses for robustness checks, including those accounting for clustering of pregnancies at the individual level, and those analysing complete cases only (Supplementary table S2).
Uptake of postpartum care and healthcare expenditures
Univariable associations
Descriptive statistics for the subgroup of 44 458 deliveries in December, were similar to those of all deliveries (Supplementary table S3). The prevalence of low SES indicators increased steadily across the four quartiles of maternal healthcare expenditure, with the highest quartile having the highest prevalence of low SES indicators: lowest educational level 23.0% in the highest quartile vs. 17.3% across the other quartiles, low disposable income 30.0% vs. 25.2%, no home-ownership 34.4% vs. 27.7% and living in a deprived neighbourhood 9.0% vs. 7.1% (Supplementary table S3). This tendency was not seen across the four quartiles of infant healthcare expenditure, were the prevalence of low maternal SES indicators in the highest quartile was comparable with the prevalence across the other quartiles (data not presented). The percentage of women who did not receive postpartum care was highest in the fourth quartile of maternal healthcare expenses (2.1% in the highest quartile vs. 1.2% across the other quartiles; Supplementary table S3).
Multivariable associations
Not receiving postpartum care, or having postpartum care uptake below the minimum, was associated with a significantly higher odds of having maternal healthcare expenditure within the highest quartile in the year following child birth: aOR 1.34; 95% CI 1.10–1.67; P 0.004, and aOR 1.09; 95% CI 1.03–1.18; P 0.005, respectively (table 3). Deliveries followed by postpartum care uptake below the minimum were in addition associated with infant healthcare expenditure within the highest quartile in the first year after birth (aOR 1.20; 95% CI 1.13–1.27; P < 0.001) (table 3).
Table 3.
Multivariable model of the association between the uptake of postpartum care and the lack in uptake and maternal and infant healthcare expenses within the highest quartile
| Maternal health care expenditures highest quartile | Infant health care expenditures highest quartile | |||
|---|---|---|---|---|
| aOR (95% CI) | P value | aOR (95% CI) | P value | |
| Primary analyses | ||||
| Maternity care uptake (n=44 458) | ||||
| No | 1.34 (1.10–1.67) | 0.004 | 1.12 (0.94–1.35) | 0.205 |
| Yes (ref) | 1 | 1 | ||
| Maternity care >24 h (n=41 583) | ||||
| No | 1.09 (1.03–1.18) | 0.005 | 1.20 (1.13–1.27) | <0.001 |
| Yes (ref) | 1 | 1 | ||
Presented are adjusted odds ratios (aOR) and their 95% confidence intervals (95%CI). All p-values are two-sided. Results are presented separately for maternal and infant healthcare expenditures, adjusted for maternal age, parity, country of origin, parenthood status, and all indicators of SES (i.e. educational level, disposable income, home ownership, and neighborhood poverty)
Sensitivity analyses
The association between no uptake of postpartum care and maternal healthcare expenses during the first year after childbirth was consistent in the sensitivity analysis using complete cases only [aOR 1.54 (95% CI 1.23–1.92; P < 0.001)].
Discussion
Using a national linked dataset of over half a million singleton pregnancies, we found that all indicators of low SES were associated with no uptake of postpartum care and with uptake of care below the recommended minimum. This lack of postpartum care uptake was associated with higher healthcare expenses in the first year after childbirth. For the first time, we demonstrate that postpartum care may be a cost-effective tool but is least provided to those who are most likely to benefit from it.
Strengths of this study include the very large and nationally representative sample and the use of a unique individual-level linkage across various routinely collected datasets of relevant medical and socioeconomic data. The relationship between low SES and lack of uptake of postpartum care was highly consistent across the various SES indicators. Although at the population level the proportion of women not receiving postpartum care is very small, we have shown that these women represent a marginalized group and may therefore benefit from efforts to improve their care.
In addition, associations between low SES and postpartum care uptake as well as between postpartum care uptake and subsequent healthcare expenditure showed a dose-response association. The largest differences were present between women who did not receive postpartum care and those who received care above the minimum amount. The findings of both analyses were furthermore highly robust in sensitivity analyses. In the absence of major changes to the system used for indicating the amount of postpartum care and of the health care insurance system in the Netherlands, the data used in this study (from 2010 to 2013) may be considered generalizable to the current day.
Our study also has limitations. First, some of the national registries from Statistics Netherlands have a reasonably high percentage of missing values. For example, the percentage of missing values on a woman’s highest educational qualification was as high as 30%. Upward educational-attainment biases could have influenced the registered data. To minimize bias within the imputed data, we had all SES indicators and outcome variables inform the imputation process. Sensitivity analyses on complete cases only showed similar results to the main analyses, supporting validity of the imputation and robustness of the findings. Second, we lacked information on medical conditions of women and infants. Having a medical condition that requires inpatient treatment could directly affect the uptake of postpartum care, as this care is provided only in the primary care setting (i.e. at home or in a primary care birth center). A third limitation is that the provided postpartum care is expressed in total expense rather than days of care received, making derivation necessary. In addition, we did not have information on the number of days spent in the hospital prior to receiving postpartum care, which may have biased our findings. Somewhat related to this point is that healthcare expenditures were only available at the annual level. We pragmatically addressed this by only assessing deliveries in December when exploring the association between postpartum care uptake and healthcare expenditure. Although this substantially reduced sample size, statistically significant and clinically relevant associations were still observed.
Our findings stress the need to further explore how equity in care uptake may be promoted. Obstetric healthcare providers should include the social determinants of health in their medical records, and in the referral to postpartum care organizations.2,15–17 Provision of postpartum care should be tailored according to these determinants to reach poor and other marginalized subpopulations.18,19 When striving to reduce inequalities in uptake of postpartum care additional determinants, besides those related to a person’s SES, should be considered. For example, our results showed that immigrant populations were less likely to receive postpartum care, even when accounting for SES indicators (table 2). This suggests that interventions targeting high-risk groups to increase postpartum care uptake should consider ethnic background in addition to SES-related factors. Cultural factors are likely to explain at least part of this inequity, but this requires further study. Mixed-methods research is needed to assess the facilitators and barriers to receiving postpartum care among low-SES women and those with an immigrant background.
Our results are in line with those observed in other reports; there is a consistent inequity in primary care provision, where more care is provided to the well-off, who need it less, than to the more disadvantaged.2,4,5,16–18,20 In the Netherlands, a possible barrier to postpartum care uptake is the additional co-payment required for each hour of care. To ensure equitable, universal coverage, policy-makers and health insurers should consider waiving this co-payment, particularly for low SES groups. Furthermore, our study provides evidence to suggest that postpartum care may help reduce subsequent healthcare expenditure, providing an additional incentive for stakeholders to invest in increasing the uptake of care. There is a need to further assess whether explicit resource allocation and priority setting to those in greatest need, perhaps in conjunction with approaches to reduce unnecessary care provision resulting in the over-payment in other sectors may help improve cost-effectiveness of postpartum care provision.
Given the observational nature of this study it is important that findings are reproduced in other settings or using different methodological approaches (i.e. prospective or randomized studies). Future research should focus on further analysing the (cost-)effectiveness of postpartum care; not only its effectiveness in achieving equity in care provision but also its ability to prevent illness and associated healthcare needs. An in-depth economic evaluation taking into account all expenses made by postpartum care organizations and the potential benefits (e.g. health benefits or value-based health measures) gained by mothers and their children could strengthen a renewed allocation for care provision.
Supplementary Material
Acknowledgements
We acknowledge Statistics Netherlands for assistance with project management. We further acknowledge that data are based on the authors’ calculations using data files from Statistics Netherlands.
Funding
This work was supported by ZonMW (The Netherlands Organization for Health Research and Development), research grant number 50-52000-98-173. The study protocol has undergone peer review by the funding body. J.V.B. is supported by personal fellowships from the Netherlands Lung Foundation and Erasmus MC. The funding sources had no role in study design, data collection and analysis, decision to publish or preparation of the article.
Conflicts of interest: None declared.
Key points
Women of low socioeconomic status are much less likely to receive postpartum care and low uptake of postpartum care is associated with higher health care expenditure after childbirth.
Substantial inequities in postpartum care provision according to immigration status furthermore exist.
Interventions to increase postpartum care uptake among those who are most likely to benefit may help reduce health inequalities and subsequent healthcare costs.
References
- 1. Shaw E, Levitt C, Wong S, et al. Systematic review of the literature on postpartum care: effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health. Birth 2006;33:210–20. [DOI] [PubMed] [Google Scholar]
- 2. Marmot M, Friel S, Bell R, et al. Commission on social determinants of H. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 2008;372:1661–9. [DOI] [PubMed] [Google Scholar]
- 3. Pillas D, Marmot M, Naicker K, et al. Social inequalities in early childhood health and development: a European-wide systematic review. Pediatr Res 2014;76:418–24. [DOI] [PubMed] [Google Scholar]
- 4. Ahmed S, Creanga AA, Gillespie DG, Tsui AO. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS One 2010;5:e11190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lindquist A, Kurinczuk JJ, Redshaw M, Knight M. Experiences, utilisation and outcomes of maternity care in England among women from different socio-economic groups: findings from the 2010 National Maternity Survey. BJOG 2015;122:1610–7. [DOI] [PubMed] [Google Scholar]
- 6. Gray R, Bonellie SR, Chalmers J, et al. Social inequalities in preterm birth in Scotland 1980-2003: findings from an area-based measure of deprivation. Bjog 2008;115:82–90. [DOI] [PubMed] [Google Scholar]
- 7. Poeran J, Maas AF, Birnie E, et al. Social deprivation and adverse perinatal outcomes among Western and non-Western pregnant women in a Dutch urban population. Soc Sci Med 2013;83:42–9. [DOI] [PubMed] [Google Scholar]
- 8. Chauvel L, Leist AK. Socioeconomic hierarchy and health gradient in Europe: the role of income inequality and of social origins. Int J Equity Health 2015;14:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Currie J, Lin W. Chipping away at health: more on the relationship between income and child health. Health Aff (Millwood) 2007;26:331–44. [DOI] [PubMed] [Google Scholar]
- 10. Mackenbach JP. The persistence of health inequalities in modern welfare states: the explanation of a paradox. Soc Sci Med 2012;75:761–9. [DOI] [PubMed] [Google Scholar]
- 11. Benchimol EI, Smeeth L, Guttmann A, et al. [The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement]. Z Evid Fortbild Qual Gesundhwes 2016;115-116:33–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Devillé WW. Herijking stedelijke achterstandsgebieden. Available at: https://www.nivel.nl/sites/default/files/bestanden/Rapport-Herijking-achterstandsgebieden-2012.pdf, 2012.
- 13. Autoriteit NZ. Available at: https://www.nza.nl/english, 2012.
- 14. Roysten P. Multiple imputation of missing values. Stata J 2004;3:227–41. [Google Scholar]
- 15. Gottlieb L, Sandel M, Adler NE. Collecting and applying data on social determinants of health in health care settings. JAMA Intern Med 2013;173:1017–20. [DOI] [PubMed] [Google Scholar]
- 16. Heiman HA. Beyond health care: the role of social determinants in promoting health and health equity. The Henry J Kaiser Family Foundation; 2015; Issue brief. Available at: http://files.kff.org/attachment/issue-brief-beyond-health-care. [Google Scholar]
- 17. ACOG Committee Opinion No. 729: Importance of social determinants of health and cultural awareness in the delivery of reproductive health care. Obstet Gynecol 2018;131:e43–8. [DOI] [PubMed] [Google Scholar]
- 18. Blas E, Gilson L, Kelly MP, et al. Addressing social determinants of health inequities: what can the state and civil society do? Lancet 2008;372:1684–9. [DOI] [PubMed] [Google Scholar]
- 19. Victora CG, Barreto ML, do Carmo Leal M, et al. Health conditions and health-policy innovations in Brazil: the way forward. Lancet 2011;377:2042–53. [DOI] [PubMed] [Google Scholar]
- 20. Hart JT. The inverse care law. Lancet 1971;1:405–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.