Abstract
Objective
To test relations between exposure to poverty, in the forms of family income and neighborhood deprivation, during three developmental stages, and children’s body mass index (BMI) in early adolescence.
Methods
Data came from a longitudinal sample of racially diverse, urban, low-income boys. Interactions between family income to needs and census-derived neighborhood deprivation at three developmental stages—early childhood (18 and 24 months), preschool-to-school entry (3.5 and 6 years), and school-age (8 and 10 years)—were tested in relation to BMI at age 11.
Results
There was a significant interaction whereby higher income predicted lower BMI only in the context of low levels of neighborhood deprivation in early childhood. In high-deprivation neighborhoods, higher income was associated with risk for overweight/obesity in early adolescence. This pattern was found to be specific to income and neighborhood deprivation measured in early childhood.
Conclusions
Findings have implications for policy relevant to obesity prevention. More research on associations between early exposure to poverty and later risk for obesity on low-income samples is warranted, as the relationship is likely complex and influenced by many different factors, including the family and neighborhood food environments and child health behaviors.
Keywords: obesity, at risk youth, disparities, health promotion and prevention, longitudinal research
Obesity is a public health concern that affects individuals across the lifespan in a variety of ways, from subjective report of physical (Doll, Petersen, & Stewart‐Brown, 2000) and psychological (Ul-Haq, Mackay, Fenwick, & Pell, 2013) well-being to greater risk for debilitating health problems, including cardiovascular disease and metabolic syndrome (Després & Lemieux, 2006). Poverty is a known risk factor for obesity in both childhood (Hernandez & Pressler, 2015) and adulthood (Senese, Almeida, Fath, Smith, & Loucks, 2009). The specific mechanisms driving the relationship between poverty and obesity remain unclear, but researchers hypothesize that several explanations are likely, including greater access and affordability of unhealthy foods (Drewnowski & Specter, 2004) and reduced space and resources for promoting physical activity (Sallis & Glanz, 2006).
Mechanisms in the association between poverty and obesity may occur at the level of the individual family and/or the broader neighborhood context where children reside. For example, a recent systematic review identified behaviors occurring primarily within children’s households, including nutritional practices (e.g., sugar-sweetened beverage intake) and sedentary behavior (e.g., more TV viewing and computer use) as possible mediators in the association between socio-economic position and child adiposity (Gebremariam, Lien, Nianogo, & Arah, 2017). On the other hand, in another recent systematic review addressing influences on child obesity risk at the neighborhood level, researchers concluded that convenience store access and vegetation in the community were associated with weight outcomes for low-income children of color (Johnson et al., 2019). Family income and neighborhood poverty are both likely to play a role in influencing children’s weight outcomes, perhaps through different mechanisms.
However, few studies have compared the relative influences of poverty at the family versus neighborhood level on child weight outcomes. Understanding whether the relationship between poverty and weight is driven primarily by family income, neighborhood deprivation, or a combination of these risk factors could have important implications for understanding basic processes and mechanisms, as well as identifying targets for prevention. Although income and neighborhood deprivation are moderately inter-correlated (Coley, Sims, Dearing, & Spielvogel, 2018) and poor families often live in low-income neighborhoods (Reardon, Fox, & Townsend, 2015), there is some evidence that each index of poverty measures distinct aspects of a child’s early environment (Leventhal & Brooks-Gunn, 2003), which may be especially relevant for children of color who are more likely to reside in low-income neighborhoods even when family income is relatively high (Intrator, Tannen, & Massey, 2016). Although there are several published studies that have tested relationships between family income and neighborhood deprivation in relation to child weight (Crespi, Wang, Seto, Mare, & Gee, 2015; Klebanov, Evans, & Brooks-Gunn, 2014; Rossen, 2014), more research is needed. Crespi et al. (2015) found some evidence that both family socioeconomic status (SES) and neighborhood poverty were associated with children’s body mass index (BMI) growth. As their study focused exclusively on girls, the relationship between family and neighborhood poverty and boys’ BMI is less clear.
Another notable gap in the literature is that many studies of the mechanisms in the association between child poverty and obesity are cross-sectional (e.g., Albaladejo et al., 2014; Dollman, Ridley, Magarey, Martin, & Hemphill, 2007; Hanson & Chen, 2006). Findings from longitudinal studies with long-term follow-up (Hernandez & Pressler, 2014; Ziol-Guest, Duncan, & Kalil, 2009) suggest that the association between exposure to poverty in childhood and later weight outcomes may endure well beyond childhood. Specifically, there is evidence to suggest that early childhood (i.e., age 0–5) is one of a few potentially “sensitive periods” during which child weight is particularly vulnerable to the effects of poverty. For example, Lee, Andrew, Gebremariam, Lumeng, and Lee (2014) found that exposure to poverty from birth to age 2 was significantly associated with obesity risk at age 15 even after accounting for exposure to poverty after age 2. In addition, Ziol-Guest et al. (2009) found that exposure to poverty prenatally and in the first year predicted BMI in adulthood (age 30–37), but later family income did not. Early childhood is theorized to be a sensitive period for later obesity based on the idea that feeding practices, including nutritional deprivation, in infancy and early childhood may modify metabolism (Hales & Barker, 2001) and appetite regulation, as well as the appetite regulatory system in the brain (McMillen, Adam, & Mühlhäusler, 2005).
In addition, there is some more recent research suggesting that the effects of family and neighborhood poverty on weight outcomes may exert more or less influence based on children’s developmental status. Klebanov et al. (2014) found that family poverty was associated with higher BMI at age 2, while neighborhood poverty predicted greater BMI growth from age 2 to 6. The researchers speculated that neighborhoods may play a greater role in influencing children’s outcomes after age 2, when children gradually start to spend more time outside of the home. Supporting this hypothesis, Kravitz-Wirtz (2016) found that exposure to neighborhood deprivation during late childhood and adolescence, but not early childhood, was associated with later obesity in young adulthood.
However, interactive effects of poverty at the family versus neighborhood level have infrequently been tested in relation to child weight outcomes. Based on cumulative risk theory (Forehand, Biggar, & Kotchick, 1998), it would be expected that high levels of neighborhood deprivation might exacerbate the effect of low family income on child weight. However, sometimes individual and contextual effects interact in unexpected ways. For example, one cross-sectional, epidemiological study found that the combination of high neighborhood deprivation and greater family income was associated with higher rates of obesity among 2–18 year-old children (Rossen, 2014). The author noted that this counterintuitive finding could perhaps explain the “diminishing returns” that are evident for racial minorities. That is, while White children’s risk for obesity seems to decrease as family income increases, for Black children the evidence is more mixed (Wang & Zhang, 2006), perhaps because Black children are more likely to reside in disadvantaged communities at higher levels of income (Reardon et al., 2015).
Furthermore, a limitation of prior research is that few studies use primarily low-income samples when testing associations between income and weight, even though prior research suggests that this population is at greatest risk for poor health outcomes, including obesity. In past studies using large, representative samples, low-income children are compared to middle- and high-income children, with findings supporting the influence of socio-economic risk on children’s weight status (Bhargava, Jolliffe, & Howard, 2008; Kendzor, Caughy, & Owen, 2012). Therefore, it remains unclear the extent to which the relationship between income and/or neighborhood deprivation and children’s weight demonstrates the same pattern within exclusively low-income samples. In addition, despite an abundance of studies on poverty and antisocial behavior in males (e.g., Sitnick, Galán, & Shaw, 2019), there is a relative dearth of studies on low-income boys with respect to associations between poverty and weight. There is some evidence that neighborhoods affect obesity in boys and girls differently (Hsieh et al., 2015), with some research indicating that some facets of the neighborhood (e.g., park space) have stronger effect sizes for BMI in males versus females (Wolch et al., 2011).
Current Study
The current study is, to our knowledge, the first to test longitudinally the relationship between exposure to poverty and later weight, assessing poverty at the levels of both family income and neighborhood deprivation, and using a low-income sample. The study’s primary goal was to elucidate the independent and interactive effects of exposure to two different types of childhood poverty on weight outcomes for boys in early adolescence. Although the sample is not representative, it offers the ability to look at variation in both income and neighborhood deprivation within a cohort of low-income, urban families. These children, and specifically boys, are infrequently the focus of research on weight outcomes despite low-income children’s high risk of poor weight-related health outcomes in childhood through adulthood (Wells, Evans, Beavis, & Ong, 2010) and the increasing prevalence of obesity in boys versus girls (Fryar, Carroll, & Ogden, 2012). Another goal of the study was to determine whether exposure to poverty in early childhood, thought to be a “sensitive period” for a variety of later health outcomes (Shonkoff, Boyce, & McEwen, 2009), is a unique predictor of later weight, or whether poverty measured later in childhood has similar effects. Therefore, relationships were tested between family income and neighborhood deprivation measured during three distinct developmental periods of early childhood (1.5–2 years), preschool-to-school entry (3.5–6 years), and school-age (8–10 years), on BMI outcomes in early adolescence (age 11).
Hypotheses
Based on the idea that early childhood is a sensitive period for health outcomes (Lee et al., 2014; Ziol-Guest et al., 2009), it was hypothesized that family income would be a stronger predictor of BMI when it was measured in early childhood. It was also hypothesized that neighborhood deprivation would have a more robust relationship with BMI when it was measured later in childhood, based on neighborhood influences becoming more apparent as children age and begin to spend more time outside of the home (Oliver & Hayes, 2008).
In conceptualizing the interaction between family income and neighborhood poverty, it was predicted that BMI would be greatest at low levels of family income and high levels of neighborhood deprivation in early childhood, based on the theory that multiple risks have additive adverse effects on well-being (Rutter, 1979). However, as Rossen (2014) found that neighborhood deprivation was associated with greater risk of obesity for children above the poverty threshold, we also were interested in examining an alternative hypothesis where BMI would be greatest at high levels of neighborhood deprivation and relatively higher levels of family income.
Method
Participants
Study participants came from a longitudinal sample of 310 boys followed prospectively from age 18 months into young adulthood as part of a larger study, the Pitt Mother & Child Project, examining the developmental antecedents of antisocial behavior (Shaw, Hyde, & Brennan, 2012). Mother-son dyads were recruited from the Women, Infants, and Children Nutritional Supplement (WIC) program in the greater Pittsburgh area beginning in 1991 when children were between the ages of 6 and 17 months. In addition to being male and being a WIC participant, the latter to ensure low-income status, families were required to have another child living at home to increase family stress (i.e., raising more than one child at a time).
All of the mothers in the study provided informed consent for the study, which was reviewed and approved by the local IRB. The boys in the sample were racially diverse, with 53% European American, 36% African American, 5% biracial, and 6% another race (e.g., Asian American). Less than 1% of the sample identified as Hispanic American. Families were predominantly low-income, with an average per capita annual income of $2,892 and a mean Hollingshead SES score of 24.5, indicative of a working-class sample (Hollingshead, 1975).
In the current study, data from assessments occurring at age 1.5, 2, 3.5, 6, 8, 10, and 11, were used. Data were available for 310 families at the initial, age 1.5 assessment and 302 (97%) at the age 2 assessment. Retention was as follows for the following visits at child age 3.5, 6, 8, and 10, respectively: 294 (95%) at age 3.5, 286 (92%) at age 6, 253 (82%) at age 8, and 243 (78%) at age 10. While retention continued to be relatively high at the age 11 assessment (79%), participants with BMI data were limited to 183 at age 11 because the weight protocol was implemented mid-way through the assessment wave.
Measures
Family Income to Needs Ratio. Family income information was collected from mothers as part of a broader interview about socio-demographic characteristics when children were 18 and 24 months (early childhood), 3.5 and 6 years (preschool-to-school entry), and 8 and 10 years (school-age). For each developmental period, family income to needs was represented by the average monthly income to needs reported at the two assessments at each developmental period (e.g., average family income at 18 and 24 months for early childhood). Income to needs was calculated by dividing the total family income at each age by the U.S. census poverty threshold for the family size for each year (i.e., 1992, 1993, 1996, 1998, & 2000). Families were categorized as being “in poverty” when their income to needs was less than 100% of the federal poverty threshold. For descriptive purposes, families in the current study were categorized as “near-poor” when their income to needs was 100–175% of the federal poverty threshold and “not poor” when their income to needs was greater than 175% of the poverty threshold (Mahoney, Lord, & Carryl, 2005).
Neighborhood deprivation
Neighborhood deprivation was calculated using U.S. census data at the block group level to geocode participants’ addresses. A census block group is the smallest geographical unit available from the U.S. census, with a population of between 600 and 3,000 people. Neighborhood deprivation was assessed using the address provided at each assessment; the variable used in the current study was represented by the mean of the two values calculated for each developmental period (e.g., average score across 18- and 24-month assessments for early childhood). Data from the 1990 decennial census were used to compute the neighborhood deprivation variable assessments that occurred between 1990 and 1995 (i.e., when children were 18 months, 24 months, and 3.5 years), and 2,000 decennial census data were used for visits that took place in 1996 or after (i.e., when children were 6, 8, and 10 years). A composite variable of neighborhood deprivation was created by averaging six census block group level variables, as recommended by Wikström and Loeber (2000): median family income, percent of families with an income below the poverty line, percent of families receiving public assistance, percent of unemployed residents, percent single-mother households, and percent of residents with a bachelor’s degree or higher. The composite variable was then converted into a z-score. The z-score from the two assessments were averaged to represent the neighborhood deprivation variable used in analyses for each of the three developmental periods. This method of operationalizing neighborhood deprivation with census data has been used in a number of studies, most often to predict children’s behavior and conduct problems (Galán, Shaw, Dishion, & Wilson, 2017; Winslow & Shaw, 2007).
BMI. Examiners measured boys’ heights and weights at a laboratory assessment at age 11. Height and weight were measured using a Health O Meter 400 kiloliter beam physician scale (Jarden Corporation, Rye, NY) and recorded to the nearest inch and pound, respectively. BMI was calculated using the ratio of weight (kg) over height (m) squared and converted to normed z-scores (BMIz) based on the CDC’s age- and sex-specific growth charts (Kuczmarski et al., 2000). Age 11 BMI values were converted into gender- and age-based percentiles for descriptive purposes, but BMIz was used as the outcome in all analyses.
Child birth weight. Child birth weight was obtained from birth records at the time of the 18-month assessment. Birth weight was included as a covariate to account for the possibility that the relationship between early exposure to poverty and child BMIz was accounted for by child birth weight, as family poverty is an established correlate of birth weight (Luo, Wilkins, & Kramer, 2006), and birth weight may predict later BMI (Singhal, Wells, Cole, Fewtrell, & Lucas, 2003).
Covariates. Selected covariates were included in analyses to account for potentially confounding variables in the relationship between early poverty and BMIz. These included target child’s birth weight, target child race, and maternal education. Maternal education was operationalized using the average of all six assessments.
Data Analytic Strategy
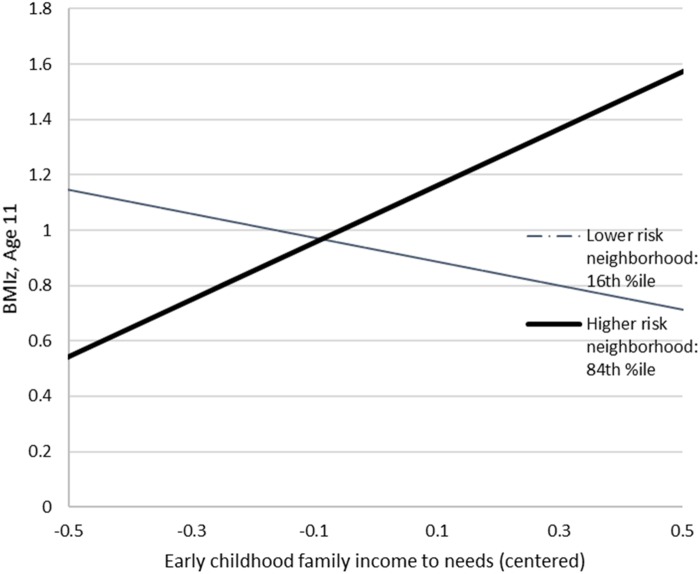
Multiple regression analyses were computed in Mplus (Muthén & Muthén, 2004) to test for associations and interactions between family income and neighborhood deprivation at each developmental period and early adolescent BMIz. All continuous variables were mean-centered to more easily interpret regression coefficients. Covariates were entered first, followed by the family income and neighborhood deprivation variables for early childhood, preschool-age, and school-age, followed by the interaction terms for early childhood, preschool-age, and school-age income x neighborhood deprivation, in a stepwise fashion. In the case of a significant interaction, the pattern of the interaction was probed by plotting the lines for family income at low (the 16th percentile) and high (the 84th percentile) levels of neighborhood deprivation (Cohen, Cohen, West, & Aiken, 2013). T-tests were conducted to determine whether the simple slope of either line was significantly different from zero.
Missing Data and Selective Attrition Effects
Multiple regression analysis was computed in Mplus (Muthén & Muthén, 2004) using full information maximum likelihood estimation to handle missing data. Analyses were conducted with the full sample (N = 310). To examine possible selective attrition effects, analyses were conducted to determine whether those for whom BMI data were available at age 11 (N = 183) differed on any study variables at baseline. Of the eight independent sample t-tests conducted, none were found to be significant.
Results
Descriptive Statistics
Means, standard deviations, and ranges for all study variables are presented in Table I. In early childhood, 68.4% of the sample had an income to needs ratio of less than 100% (i.e., the U.S. government’s poverty threshold), 26.5% were categorized as “near-poor,” with an income to needs ratio of between 100% and 175%, and 5.1% were “not poor” (i.e., reported an income to needs ratio of greater than 175%). By school-age (average income to needs when children were 8 and 10 years), 40.5% of families were living in poverty according to the federal threshold, with 31.2% in the “near-poor” income range and 28.3% categorized as “not poor.” At age 11, 43.7% of the sample was overweight or obese (at or above the 85th percentile) and 24% obese (at or above the 95th percentile).
Table I.
Descriptives of Study Variables
| Variable | Mean (SD) | Range |
|---|---|---|
| Family income to needs, 18 & 24M (n = 310) | .83 (.5) | .11–2.95 |
| Family income to needs, 3.5 & 6 yr (n = 296) | 1.04 (.7) | .24–4.00 |
| Family income to needs, 8 & 10 yr (n = 269) | 1.39 (.9) | 2.15–5.23 |
| Maternal education, average (n = 310) | 12.79 (1.4) | 8.0–17.3 |
| Census-derived neighborhood deprivation, z-score, 18 & 24M (n = 301) | .38 (1.2) | −2.04–3.10 |
| Census-derived neighborhood deprivation, z-score, 3.5 & 6 yr (n = 301) | .30 (.9) | −1.45–2.76 |
| Census-derived neighborhood deprivation, z-score, 8 & 10 yr (n = 267) | .18 (.7) | −1.06–2.58 |
| Child birth weight, pounds (n = 261) | 7.33 (1.3) | 2.0–10.7 |
| Age 11 BMI (n = 183) | 20.68 (4.6) | 13.5–34.8 |
| Age 11 BMIz (n = 183) | .76 (1.1) | −2.62–2.55 |
Correlations among study variables appear in Table II. Income to needs was moderately negatively correlated with census-derived neighborhood deprivation measure at the same time (with r’s ranging from −.30 to −.39). Child race was highly correlated with census-derived neighborhood deprivation in early childhood (r = .67), with African American children much more likely to live in high-deprivation neighborhoods.
Table II.
Correlations among Study Variables
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Family income to needs, 18 & 24M | – | |||||||||
| 2. Family income to needs, 3 & 6 yrs | .61* | – | ||||||||
| 3. Family income to needs, 8 & 10 yrs | .50* | .74* | – | |||||||
| 4. Maternal education | .32* | .23* | .32* | – | ||||||
| 5. Census neighb. dep., 18 & 24M | −.39* | −.37* | −.31* | −.14* | – | |||||
| 6. Census neighb. dep., 3 & 6 | −.37* | −.39* | −.36* | −.18* | .80* | – | ||||
| 7. Census neighb. dep., 8 & 10 | −.28* | −.28* | −.30* | −.20* | .51* | .72* | – | |||
| 8. Child birth weight | .06 | .06 | .06 | .07 | −.18* | −.20* | −.12† | – | ||
| 9. Child is African American | −.33* | −.31* | −.30* | −.05 | .67* | .66* | .53* | −.21* | – | |
| 10. Age 11 BMIz | −.09 | −.07 | −.18* | −.04 | −.01 | .04 | .04 | −.05 | .06 | – |
Denotes significance at p < .05.
Denotes significance at p <. 10.
Interactions of Family Income and Neighborhood Poverty in Predicting Weight
Covariates, income and neighborhood deprivation at each developmental stage, and terms representing the statistical interactions between family income and neighborhood deprivation at all three developmental stages were all entered simultaneously into the regression. Income to needs at school-age was found to have a significant, negative association with age 11 BMIz (β = −.20, p < .05; 95% CI β = −.46 to −.02). None of the covariates, nor neighborhood deprivation at any developmental stage, were significantly associated with child BMIz. There was, however, a significant interaction between family income and neighborhood deprivation in early childhood (β = .25, p < .05; 95% CI β =.06–.45) in predicting child BMIz at age 11 (see Table III). The interactions between family income and neighborhood deprivation in the preschool and school-age periods were not significant. The total variance accounted for by all independent variables in predicting child BMIz was r2 = .15, p < .05.
Table III.
Interactions between Family Income and Neighborhood Poverty in Predicting Early Adolescent BMIz
| Variable | BMIz (Age 11) | |
|---|---|---|
| B (SE) | β (p) | |
|
| ||
| Child race—African American | .03 (.2) | .02 (.89) |
| Child race—Other (i.e., not African American or White) | −.33 (.3) | −.08 (.20) |
| Birth weight | .00 (.0) | −.04 (.55) |
| Maternal education | .00 (.1) | .00 (.95) |
| Family income to needs—early childhood | .13 (.2) | .06 (.59) |
| Neighborhood deprivation—early childhood | .05 (.1) | .05 (.72) |
| Family income to needs—preschool age | .33 (.2) | .20 (.11) |
| Neighborhood deprivation—preschool age | .07 (.2) | .14 (.38) |
| Family income to needs—school age | −.30 (.1) | −.24 (.03)* |
| Neighborhood deprivation—school age | −.10 (.2) | −.07 (.56) |
| Income to needs x neighborhood deprivation—early | .58 (.2) | .25 (.01)* |
| Income to needs x neighborhood deprivation—preschool | .36 (.2) | .19 (.13) |
| Income to needs x neighborhood deprivation—school | .05 (.2) | .03 (.78) |
Denotes significance at p < .05.
To understand the pattern of the interaction in early childhood for BMIz, the effect of family income on BMIz was calculated at low (the 16th percentile) and high (the 84th percentile) levels of neighborhood deprivation. In the context of low neighborhood deprivation, early childhood family income had the expected, inverse relationship with BMI at age 11 (i.e., lower income associated with higher BMIz). In the context of high levels of neighborhood deprivation, however, higher income predicted higher BMIz (see Figure 1). The simple slope of the line plotted for family income at low levels of neighborhood deprivation (at the 16th percentile of neighborhood deprivation) was not significantly different from zero (t = −1.81, p = .07). The simple slope for family income at high levels of neighborhood deprivation was significantly different from zero at the 84th percentile of neighborhood deprivation (t = 3.0, p < .01). Analyses of regions of significance suggested that simple slopes of the lines plotted for family income were significantly different from 0 at or below the 12th percentile (t = −1.98, p < .05) and at or above the 80th percentile (t = 1.97, p < .05) of neighborhood deprivation.
Figure 1.
Interaction between family income and neighborhood deprivation in relation to age 11 BMIz.
Discussion
The current study expands upon the current literature on the relationship between childhood exposure to poverty and risk for obesity in early adolescence. Our results indicate that two moderately related aspects of early childhood poverty, family income, and neighborhood deprivation, may predict children’s weight years later.
The current study found that within a predominantly low-income sample, early childhood family income appeared to be protective against children’s risk for overweight in early adolescence when families resided in low-deprivation neighborhoods. However, in the context of higher levels of neighborhood deprivation, higher family income (i.e., being “near-poor” as opposed to poor) was a risk factor for higher BMIz in early adolescence. Children with low family income and high neighborhood deprivation were found to be relatively protected from high BMIz. Conversely, those youths with a combination of higher income/high neighborhood deprivation and low income/low neighborhood deprivation were found to be most at risk for higher weight at age 11.
Our findings also suggested that the interaction between exposure to neighborhood deprivation and family income in predicting later weight may be specific to early childhood. The current study did not find evidence to support the hypothesis that family income would be a stronger predictor of BMIz in early childhood and neighborhood deprivation would have a stronger association at school-age. In fact, family income at school-age (when children were 8 and 10 years old) was found to have a significant, negative association with BMIz, while there was no relationship found for school-age neighborhood deprivation.
Although findings from many prior studies support the hypothesis that childhood poverty is a potent risk factor for obesity (Senese et al., 2009; Hernandez & Pressler, 2015), others have found that this relationship may be weaker for certain populations, including males and African Americans (Fradkin et al., 2015; Lee, Harris, & Gordon-Larsen, 2009). The current study builds upon recent efforts that focus on specific populations (i.e., low-income, racially diverse, male youth) and underscores the importance of examining multiple components of poverty and their interactions in relation to later health outcomes, rather than focusing on only one component of poverty. Regarding the former, our study’s all-male, predominantly low-income sample is novel, as the majority of prior research has tested these relationships using representative samples.
The finding that the combination of high neighborhood deprivation and higher family income is associated wither higher rates of obesity, while unexpected, is consistent with findings from Rossen (2014), who used a much larger sample. There is some additional research to support that children from “near-poor” families may be more at risk for obesity than children from families below the poverty threshold (Kimbro, Brooks-Gunn, & McLanahan, 2011; Mahoney et al., 2005), though the current study found that only in the context of greater neighborhood deprivation was being “near poor” a greater risk for obesity than being below the poverty threshold.
Perhaps those “near-poor” families with relatively higher incomes living in more deprived neighborhoods might still have limited access to healthy foods because of greater physical distance to grocery stores containing more varied and nutritious food options. Their higher incomes might only go so far in contexts where physical access and proximity to food is still limited (i.e., living in food deserts; Larson, Story, & Nelson, 2009; Richardson, Boone-Heinonen, Popkin, & Gordon-Larsen, 2012). In addition, neighborhood poverty is associated with greater availability of fast-food restaurants and convenience stores (i.e., “food swamps”; Hilmers, Hilmers, & Dave, 2012; Richardson et al., 2012), which have been found to predict child obesity (Cobb et al., 2015). Perhaps such obesogenic characteristics of the neighborhood food environment are associated with greater risk for obesity, but only for those families with at least some financial means to access them.
Children from low-income families living in low-deprivation neighborhoods were also found to be at risk for higher BMIz than children from low-income families living in high-deprivation neighborhoods. Although children from low-income families living in neighborhoods with relatively low deprivation might reside closer to sources of healthy food (e.g., supermarkets, farmers’ markets) than in high-poverty neighborhoods, their financial constraints might limit their ability to purchase high-quality foods. Research suggests that the addition of a full-service grocery store in a neighborhood may not influence low-income families’ consumption of fruits and vegetables (Dubowitz et al., 2015; Elbel et al., 2015).
Findings from the current study could have important implications for policies intended to help low-income families. It could be that in the context of high-poverty neighborhoods, policies that lead to increased income for very low-income families could be associated with higher risk for child overweight. Interestingly, participation in the Supplemental Nutrition Assistance Program (SNAP) has been found to be associated with higher BMI for adolescents (Leung, Tester, Rimm, & Willett, 2017); perhaps neighborhood quality is an important moderator of the association between SNAP participation and BMI.
The literature would benefit from further study of the relationship between neighborhood deprivation, family income, and obesity while pursuing possible mechanisms involved in driving such interactions, such as structural (e.g., proximity to food stores) and social (e.g., neighborhood violence, cohesiveness) aspects of families’ ecologies. A recent systematic review of neighborhood risk factors for obesity in low-income Black and Hispanic children concluded that there is a paucity of research in this area (Johnson et al., 2019); thus, future studies must prioritize examining specific risk factors at the neighborhood level (e.g., food environment, neighborhood greenspace, violence and crime in the neighborhood).
Limitations
Limitations of the current study include the relatively small sample size and the absence of a complete dataset for age 11 BMI. Future studies testing similar hypotheses would also benefit from assessing weight outcomes as growth in BMI across childhood. Another limitation was that we were unable to account for several covariates that would have been beneficial to include (e.g., maternal BMI, whether families received food stamp benefits and if so how much, family composition of the child’s home, daycare attendance) as these data were no collected in the current study. Also, the current study was limited to males; thus, findings may not be generalizable to females or youth from higher-SES urban, rural, or suburban communities. As some research suggests that there may be important sex differences in the relationship between poverty and obesity, with a stronger association usually found for females (Le Meyer, Zane, Cho, & Takeuchi, 2009; Zhang & Wang, 2004), there is a need for more studies involving urban, low-income females. Last, although the current study attempted to disambiguate the influence of two different aspects of children’s experience of poverty, it did not examine the specific characteristics of family or neighborhood poverty that would be expected to drive the associations with child weight (e.g., children’s diet, the neighborhood food environment, neighborhood greenspace). Further unpacking the findings of the current study would be a logical next step for future research and could help inform specific targets of child obesity prevention.
Conclusions
As the pattern of findings in the current study was unexpected, further research is necessary to determine whether the results can be replicated with other samples, both low-income and representative of the national income spectrum. Our findings highlight the importance of considering two components of poverty—neighborhood deprivation and family income—with respect to children’s health outcomes. In spite of the aforementioned limitations, the current study provides support to a growing literature on the association between early childhood exposure to poverty and detrimental health outcomes including, but not limited to, obesity.
Funding
This work was supported by the National Institute of Mental Health (grant numbers 50907, 01666); and the National Institute on Drug Abuse (grant numbers 25630, 26222) to D.S.
References
- Albaladejo R., Villanueva R., Navalpotro L., Ortega P., Astasio P., Regidor E. (2014). Risk behaviors and sports facilities do not explain socioeconomic differences in childhood obesity: A cross-sectional study. BMC Public Health, 14, 1181.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhargava A., Jolliffe D., Howard L. L. (2008). Socio-economic, behavioural and environmental factors predicted body weights and household food insecurity scores in the Early Childhood Longitudinal Study-Kindergarten. British Journal of Nutrition, 100, 438–444. [DOI] [PubMed] [Google Scholar]
- Cobb L. K., Appel L. J., Franco M., Jones‐Smith J. C., Nur A., Anderson C. A. (2015). The relationship of the local food environment with obesity: A systematic review of methods, study quality, and results. Obesity, 23, 1331–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J., Cohen P., West S. G., Aiken L.S. (2013). Applied multiple regression/correlation analysis for the behavioral sciences. Mahway, NJ: Routledge. [Google Scholar]
- Coley R. L., Sims J., Dearing E., Spielvogel B. (2018). Locating economic risks for adolescent mental and behavioral health: Poverty and affluence in families, neighborhoods, and schools. Child Development, 89, 360–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crespi C. M., Wang M. C., Seto E., Mare R., Gee G. (2015). Associations of family and neighborhood socioeconomic characteristics with longitudinal adiposity patterns in a biracial cohort of adolescent girls. Biodemography and Social Biology, 61, 81–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Després J.-P., Lemieux I. (2006). Abdominal obesity and metabolic syndrome. Nature, 444, 881.. [DOI] [PubMed] [Google Scholar]
- Doll H. A., Petersen S. E., Stewart‐Brown S. L. (2000). Obesity and physical and emotional well‐being: Associations between body mass index, chronic illness, and the physical and mental components of the SF‐36 questionnaire. Obesity Research, 8, 160–170. [DOI] [PubMed] [Google Scholar]
- Dollman, J., Ridley, K., Magarey, A., Martin, M., & Hemphill, E. (2007). Dietary intake, physical activity and TV viewing as mediators of the association of socioeconomic status with body composition: a cross-sectional analysis of Australian youth. International Journal of Obesity, 31, 45. [DOI] [PubMed] [Google Scholar]
- Drewnowski A., Specter S. E. (2004). Poverty and obesity: The role of energy density and energy costs. The American Journal of Clinical Nutrition, 79, 6–16. [DOI] [PubMed] [Google Scholar]
- Dubowitz T., Ghosh-Dastidar M., Cohen D. A., Beckman R., Steiner E. D., Hunter G. P., Collins R. L. (2015). Changes in diet after introduction of a full service supermarket in a food desert. Health Affairs (Project Hope), 34, 1858.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbel B., Moran A., Dixon L. B., Kiszko K., Cantor J., Abrams C., Mijanovich T. (2015). Assessment of a government-subsidized supermarket in a high-need area on household food availability and children’s dietary intakes. Public Health Nutrition, 18, 2881–2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forehand R., Biggar H., Kotchick B. A. (1998). Cumulative risk across family stressors: Short-and long-term effects for adolescents. Journal of Abnormal Child Psychology, 26, 119–128. [DOI] [PubMed] [Google Scholar]
- Fradkin C., Wallander J. L., Elliott M. N., Tortolero S., Cuccaro P., Schuster M. A. (2015). Associations between socioeconomic status and obesity in diverse, young adolescents: Variation across race/ethnicity and gender. Health Psychology, 34, 1.. [DOI] [PubMed] [Google Scholar]
- Fryar C. D., Carroll M. D., Ogden C. L. (2012). Prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2009–2010. National Center for Health Statistics, 1960, 1–5. [Google Scholar]
- Galán C. A., Shaw D. S., Dishion T. J., Wilson M. N. (2017). Neighborhood deprivation during early childhood and conduct problems in middle childhood: Mediation by aggressive response generation. Journal of Abnormal Child Psychology, 45, 935–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebremariam M., Lien N., Nianogo R., Arah O. (2017). Mediators of socioeconomic differences in adiposity among youth: A systematic review. Obesity Reviews, 18, 880–898. [DOI] [PubMed] [Google Scholar]
- Hales C. N., Barker D. J. (2001). The thrifty phenotype hypothesis. British Medical Bulletin, 60, 5–20. [DOI] [PubMed] [Google Scholar]
- Hanson M. D., Chen E. (2006). Socioeconomic status, race, and body mass index: The mediating role of physical activity and sedentary behaviors during adolescence. Journal of Pediatric Psychology, 32, 250–259. [DOI] [PubMed] [Google Scholar]
- Hernandez D. C., Pressler E. (2014). Accumulation of childhood poverty on young adult overweight or obese status: Race/ethnicity and gender disparities. Journal of Epidemiology and Community Health, 68, 478–484. [DOI] [PubMed] [Google Scholar]
- Hernandez D. C., Pressler E. (2015). Gender disparities among the association between cumulative family-level stress & adolescent weight status. Preventive Medicine, 73, 60–66. [DOI] [PubMed] [Google Scholar]
- Hilmers A., Hilmers D. C., Dave J. (2012). Neighborhood disparities in access to healthy foods and their effects on environmental justice. American Journal of Public Health, 102, 1644–1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead A. B. (1975). Four factor index of social status. Unpublished manuscript. Retrieved from https://artlesstanzim.files.wordpress.com/2014/05/hollinghead-four-factors-2.pdf
- Hsieh S., Klassen A. C., Curriero F. C., Caulfield L. E., Cheskin L. J., Davis J. N., Spruijt-Metz D. (2015). Built environment associations with adiposity parameters among overweight and obese Hispanic youth. Preventive Medicine Reports, 2, 406–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intrator J., Tannen J., Massey D. S. (2016). Segregation by race and income in the United States 1970–2010. Social Science Research, 60, 45–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K. A., Showell N. N., Flessa S., Janssen M., Reid N., Cheskin L. J., Thornton R. L. (2019). Do neighborhoods matter? A systematic review of modifiable risk factors for obesity among low socio-economic status Black and Hispanic children. Childhood Obesity, 15, 71–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendzor D. E., Caughy M. O., Owen M. T. (2012). Family income trajectory during childhood is associated with adiposity in adolescence: A latent class growth analysis. BMC Public Health, 12, 611.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbro R. T., Brooks-Gunn J., McLanahan S. (2011). Young children in urban areas: Links among neighborhood characteristics, weight status, outdoor play, and television watching. Social Science & Medicine, 72, 668–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klebanov P. K., Evans G. W., Brooks-Gunn J. (2014). Poverty, ethnicity, and risk of obesity among low birth weight infants. Journal of Applied Developmental Psychology, 35, 245–253. [Google Scholar]
- Kravitz-Wirtz N. (2016). Temporal effects of child and adolescent exposure to neighborhood disadvantage on black/white disparities in young adult obesity. Journal of Adolescent Health, 58, 551–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski R., Ogden C., Grummer-Strawn L., Flegal K., Guo S., Wei R., Johnson C. (2000). CDC growth charts: United States. Advance Data, 314, 1–27. [PubMed] [Google Scholar]
- Larson N. I., Story M. T., Nelson M. C. (2009). Neighborhood environments: Disparities in access to healthy foods in the US. American Journal of Preventive Medicine, 36, 74–81.e10. [DOI] [PubMed] [Google Scholar]
- Le Meyer O., Zane N., Cho Y. I., Takeuchi D. T. (2009). Use of specialty mental health services by Asian Americans with psychiatric disorders. Journal of Consulting and Clinical Psychology, 77, 1000.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H., Andrew M., Gebremariam A., Lumeng J. C., Lee J. M. (2014). Longitudinal associations between poverty and obesity from birth through adolescence. American Journal of Public Health, 104, e70–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H., Harris K. M., Gordon-Larsen P. (2009). Life course perspectives on the links between poverty and obesity during the transition to young adulthood. Population Research and Policy Review, 28, 505.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung C. W., Tester J. M., Rimm E. B., Willett W. C. (2017). SNAP participation and diet-sensitive cardiometabolic risk factors in adolescents. American Journal of Preventive Medicine, 52, S127–S137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal T., Brooks-Gunn J. (2003). Children and youth in neighborhood contexts. Current Directions in Psychological Science, 12, 27–31. [Google Scholar]
- Luo Z.-C., Wilkins R., Kramer M. S. (2006). Effect of neighbourhood income and maternal education on birth outcomes: A population-based study. Canadian Medical Association Journal, 174, 1415–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney J. L., Lord H., Carryl E. (2005). Afterschool program participation and the development of child obesity and peer acceptance. Applied Developmental Science, 9, 202–215. [Google Scholar]
- McMillen I. C., Adam C. L., Mühlhäusler B. S. (2005). Early origins of obesity: Programming the appetite regulatory system. The Journal of Physiology, 565, 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. (2004). Mplus user's guide: Statistical analysis with latent variables: User's guide. Los Angeles, CA: Muthén & Muthén.
- Oliver L. N., Hayes M. V. (2008). Effects of neighbourhood income on reported body mass index: An eight year longitudinal study of Canadian children. BMC Public Health, 8, 16.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon S. F., Fox L., Townsend J. (2015). Neighborhood income composition by household race and income, 1990–2009. The Annals of the American Academy of Political and Social Science, 660, 78–97. [Google Scholar]
- Richardson A. S., Boone-Heinonen J., Popkin B. M., Gordon-Larsen P. (2012). Are neighbourhood food resources distributed inequitably by income and race in the USA? Epidemiological findings across the urban spectrum. BMJ Open, 2, e000698.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen L. M. (2014). Neighbourhood economic deprivation explains racial/ethnic disparities in overweight and obesity among children and adolescents in the USA. Journal of Epidemiology and Community Health, 68, 123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M. (1979). Protective factors in children's responses to stress and disadvantage. Annals of the Academy of Medicine, Singapore, 8, 324.. [PubMed] [Google Scholar]
- Sallis J. F., Glanz K. (2006). The role of built environments in physical activity, eating, and obesity in childhood. The Future of Children, 16, 89–108. [DOI] [PubMed] [Google Scholar]
- Senese L. C., Almeida N. D., Fath A. K., Smith B. T., Loucks E. B. (2009). Associations between childhood socioeconomic position and adulthood obesity. Epidemiologic Reviews, 31, 21–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw D. S., Hyde L. W., Brennan L. M. (2012). Early predictors of boys' antisocial trajectories. Development and Psychopathology, 24, 871–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff J. P., Boyce W. T., McEwen B. S. (2009). Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. JAMA, 301, 2252–2259. [DOI] [PubMed] [Google Scholar]
- Singhal A., Wells J., Cole T. J., Fewtrell M., Lucas A. (2003). Programming of lean body mass: A link between birth weight, obesity, and cardiovascular disease? The American Journal of Clinical Nutrition, 77, 726–730. [DOI] [PubMed] [Google Scholar]
- Sitnick S. L., Galán C. A., Shaw D. S. (2019). Early childhood predictors of boys’ antisocial and violent behavior in early adulthood. Infant Mental Health Journal, 40, 67–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ul-Haq Z., Mackay D. F., Fenwick E., Pell J. P. (2013). Meta-analysis of the association between body mass index and health-related quality of life among children and adolescents, assessed using the pediatric quality of life inventory index. The Journal of Pediatrics, 162, 280–286. e281. [DOI] [PubMed] [Google Scholar]
- Wang Y., Zhang Q. (2006). Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. The American Journal of Clinical Nutrition, 84, 707–716. [DOI] [PubMed] [Google Scholar]
- Wells N. M., Evans G. W., Beavis A., Ong A. D. (2010). Early childhood poverty, cumulative risk exposure, and body mass index trajectories through young adulthood. American Journal of Public Health, 100, 2507–2512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wikström P. O. H., Loeber R. (2000). Do disadvantaged neighborhoods cause well‐adjusted children to become adolescent delinquents? A study of male juvenile serious offending, individual risk and protective factors, and neighborhood context. Criminology, 38, 1109 [Google Scholar]
- Winslow E. B., Shaw D. S. (2007). Impact of neighborhood disadvantage on overt behavior problems during early childhood. Aggressive Behavior: Official Journal of the International Society for Research on Aggression, 33, 207–219. [DOI] [PubMed] [Google Scholar]
- Wolch J., Jerrett M., Reynolds K., McConnell R., Chang R., Dahmann N., Berhane K. (2011). Childhood obesity and proximity to urban parks and recreational resources: A longitudinal cohort study. Health & Place, 17, 207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Q., Wang Y. (2004). Socioeconomic inequality of obesity in the United States: Do gender, age, and ethnicity matter? Social Science & Medicine, 58, 1171–1180. [DOI] [PubMed] [Google Scholar]
- Ziol-Guest K. M., Duncan G. J., Kalil A. (2009). Early childhood poverty and adult body mass index. American Journal of Public Health, 99, 527–532. [DOI] [PMC free article] [PubMed] [Google Scholar]