Abstract
Trichosporon species are emerging opportunistic yeasts that cause life-threatening disseminated disease in severely immunocompromised patients. Trichosporon japonicum is a very rare cause of invasive trichosporonosis. We describe a case of Trichosporon japonicum fungemia in an immunocompetent patient with a transcutaneous biventricular assist device.
Keywords: antifungal therapy, MALDI TOF, Trichosporon japonicum, ventricular assist device
Trichosporon species are widely distributed in the environment and are regularly found on normal skin, particularly in the perigenital areas, and occasionally as part of the normal gastrointestinal or upper respiratory microbiome [1]. Invasive trichosporonosis is the most common non-Candida yeast infection in persistently neutropenic patients undergoing chemotherapy for hematological malignancies or after organ transplantation [1]. It is associated with 50%–80% mortality despite antifungal therapy. Trichosporon fungemia is difficult to diagnose and refractory to treatment, thus accounting for the associated high mortality [2].
Cases of fungemia caused by new species within the genus Trichosporon are becoming increasingly recognized. We report a case of Trichosporon japonicum fungemia in a patient with a transcutaneous biventricular assist device (BiVAD) and no known immunodeficiency.
CASE
A previously healthy, HIV-negative 18-year-old female presented with malaise, cough, nausea, and vomiting. The patient had severe hypotension and biventricular heart failure. She was taken to the operating room to initiate extracorporeal membrane oxygenation. Intraoperatively she developed ventricular fibrillation and had to be resuscitated. She underwent salvage cannulation of the right atrium and ascending aorta. It was then decided to proceed to insertion of a transcutaneous BiVAD. Dacron grafts were anastomosed to the ascending aorta and pulmonary artery, and 2 arterial cannulas were secured. A drainage cannula was implanted into the left ventricular apex. The sternum was left open due to perioperative bleeding. Myocardial biopsy showed focal mild hypertrophic changes and no viral inclusions.
On postoperative day 25, there was an increase in white blood cell count (15.5 ×109/L) and CRP (216 mg/L). β-1,3-D-glucan rose from <31 pg/mL to 80 pg/mL (<60 pg/mL [negative], 60–80 pg/mL [indeterminate], and >80 pg/mL [positive]). At the time, the patient was on antifungal prophylaxis with fluconazole. A point-of-care latex agglutination cryptococcal capsular polysaccharide antigen (CrAg) test was negative.
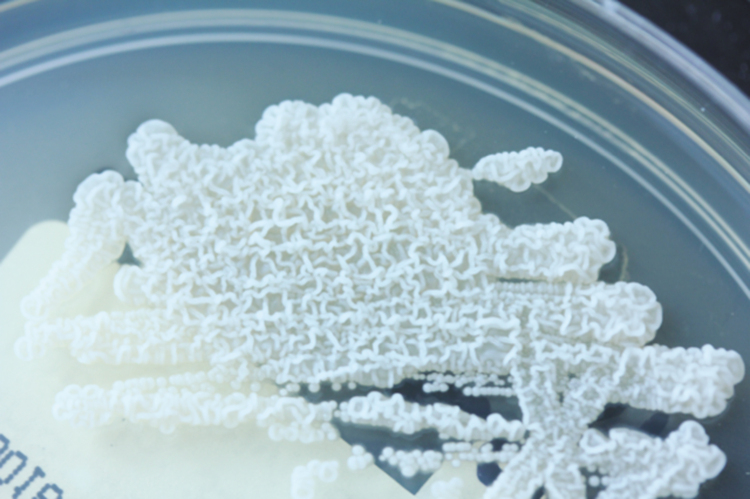
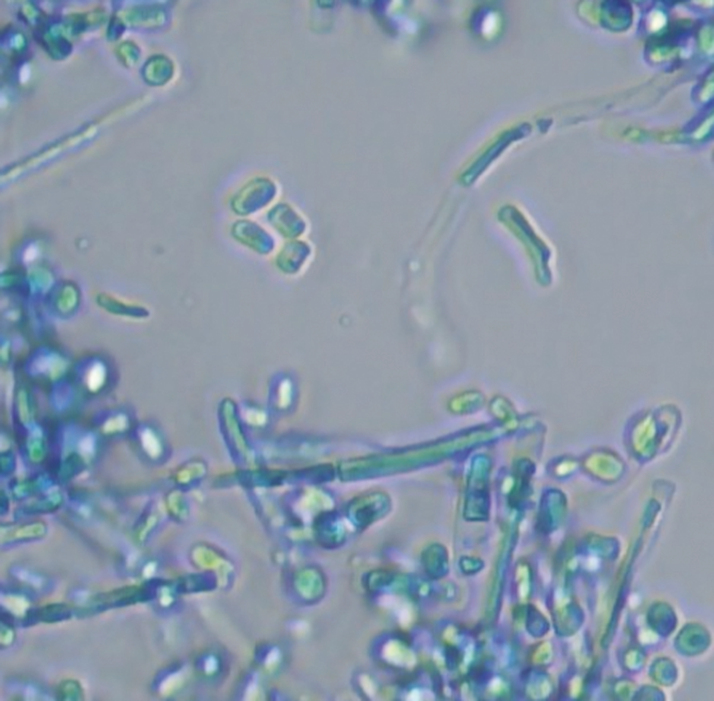
Two sets of blood cultures taken from central catheters were inoculated onto Sabouraud dextrose agar with chloramphenicol (Oxoid) and grew yeast after 2 days of incubation (Figure 1). A presumptive identification of Trichosporon was made via direct microscopy based on the appearance of the blastoconidia and arthroconidia (Figure 2). T. japonicum was identified by Matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) with a score value of 2.07. The identification of T. japonicum was further confirmed by polymerase chain reaction amplification of nuclear rRNA and large-subunit (28S) rRNA gene fragments with specific primers, ITS5 (5′ GGA AGT AAA AGT CGT AAC AAG G 3′) and ITS4 (5′ TCC TCC GCT TAT TGA TAT GC 3′), D1 (5′ GCA TAT CAA TAA GCG GAG GA 3′), and D2 (5′TTG GTC CGT GTT TCA AGA CG 3′), respectively.
Figure 1.
Trichosporon cultured on Sabouraud dextrose agar with chloramphenicol.
Figure 2.
Trichosporon cultured on Sabouraud dextrose agar with chloramphenicol. Note the rounded blastoconidia, arthroconidia because of hyphal fragmentation, and true hyphae.
The patient was commenced on caspofungin for treatment of fungemia. There was no evidence of disseminated infection. After identification of the organism as T. japonicum, she was switched to liposomal amphotericin B and flucytosine while awaiting antifungal susceptibility testing results. All catheters were removed. Three sets of blood cultures collected on day 30 yielded no growth.
On day 38, the device was explanted as the patient recovered from cardiac failure. The cannulas were removed, and the Dacron grafts were divided, oversewn, and tied. Culture of the removed left ventricular apex cuff and aortic cannula grew T. japonicum.
Antifungal susceptibilities became available. The minimum inhibitory concentration (MIC) values by the EUCAST method [3] were as follows: fluconazole (1 mg/L), itraconazole (0.125 mg/L), voriconazole (0.06 mg/L), amphotericin B (1 mg/L), micafungin (>4 mg/L), and flucytosine (8 mg/L). The minimum fungicidal concentration values of micafungin were >4 mg/L. The patient was switched to voriconazole on day 39, as fungemia developed while on fluconazole prophylaxis. She received 6 weeks of antifungal treatment after BiVAD explantation.
DISCUSSION
We report a case of BiVAD infection due to Trichosporon, an unusual fungal organism. The portal of entry of the fungus was presumably the central catheter. Candida spp. are the most common fungi causing VAD-related fungemia, which can be associated with high mortality rates [4, 5]. In 1998, a novel Trichosporon species was isolated from the air in Japan and was named T. japonicum [6]. The first genetically confirmed identification of T. japonicum from a clinical sample was reported from a fatal case of trichosporonosis in an 8-year old girl who had undergone bone marrow transplant for acute myelogenous leukemia [7]. Over 80% of the cases of trichosporonosis occur in patients with hematological malignancies with persistent neutropenia, neutrophil dysfunction, or with history of previous use of an echinocandin [8]. The majority of these cases are catheter-related, as in our case.
Molecular analysis is required, as currently available Vitek II yeast identification and API ID32C systems are not reliable for identification of all clinically relevant Trichosporon species [9]. A number of recent reports have demonstrated the utility of MALDI-TOF MS for the identification of Trichosporon species [10, 11]. In 1 study, a specific database composed of 18 reference strains plus 7 clinical isolates allowed the correct identification of 67 of the 68 clinical isolates (98.5%) [10]. Aspergillus galactomannan, Trichosporon beigelii, and T. dermatis share antigens with Cryptococcus, and a number of reports have demonstrated cross-reactivity in the cryptococcal antigen kit. Therefore, dual positivity in this test may be an indicator of invasive trichosporonosis; however, the sensitivity and specificity of this approach have not been defined [12]. Both Aspergillus galactomannan and CrAg were negative in our case.
Trichosporon species show variable susceptibility to amphotericin B, flucytosine, fluconazole, and itraconazole. Also, Trichosporon breakthrough fungemias in patients on echinocandin prophylaxis have been reported due to high MICs [13, 14]. Voriconazole is the preferred treatment for invasive trichosporonosis due to its excellent in vitro activity and studies reporting good clinical outcomes [12]. In fungemia, voriconazole or an amphotericin B-triazole combination regimen, plus early recovery from neutropenia or removal of central venous catheters, are associated with a favorable outcome [2]. In contrast, history of antimicrobial use, bacterial bloodstream co-infection, prophylactic/empirical antifungal therapy, and use of amphotericin B for treatment are associated with poor prognosis [2]. It is important to note that our patient developed T. japonicum fungemia while on fluconazole prophylaxis.
This represents a rare case of T. japonicum infection in a patient with a transcutaneous BiVAD.
Acknowledgments
We thank Dr. Lily Novark-Frazer and Samuel Hill for help with the genotyping of the isolate.
Potential conflicts of interest. Felix Bongomin acted as consultant for and received honoraria from Gilead Sciences. Paschalis Vergidis received honoraria from Pfizer for lectures. Akaninyene Otu, Giorgio Calisti, Malcolm D. Richardson, James Barnard, and Rajamiyer Venkateswaran have nothing to disclose. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Castano G, Mada PK.. Trichosporonosis. StatPearls; 2018. [PubMed] [Google Scholar]
- 2. Liao Y, Lu X, Yang S, et al. Epidemiology and outcome of Trichosporon fungemia: a review of 185 reported cases from 1975 to 2014. Open Forum Infect Dis 2015; 2(4):ofv141. doi: 10.1093/ofid/ofv141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters, version 8.1 2017. Available at: http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/AFST/Clinical_breakpoints/Antifungal_breakpoints_v_8.1_March_2017.pdf. Accessed 1 May 2019.
- 4. Aslam S, Hernandez M, Thornby J, et al. Risk factors and outcomes of fungal ventricular-assist device infections. Clin Infect Dis 2010; 50:664–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Koval CE, Rakita R; AST Infectious Diseases Community of Practice Ventricular assist device related infections and solid organ transplantation. Am J Transplant 2013; 13(Suppl 4):348–54. [DOI] [PubMed] [Google Scholar]
- 6. Sugita T, Nakase T. Trichosporon japonicum sp. nov. isolated from the air. Int J Syst Bacteriol 1998; 48 Pt 4:1425–9. [DOI] [PubMed] [Google Scholar]
- 7. Ağirbasli H, Bilgen H, Ozcan SK, et al. Two possible cases of Trichosporon infections in bone-marrow-transplanted children: the first case of T. japonicum isolated from clinical specimens. Jpn J Infect Dis 2008; 61:130–2. [PubMed] [Google Scholar]
- 8. Álvarez-Uría A, Muñoz P, Vena A, et al. Fungaemia caused by rare yeasts: incidence, clinical characteristics and outcome over 10 years. J Antimicrob Chemother 2018; 73:823–5. [DOI] [PubMed] [Google Scholar]
- 9. Taj-Aldeen SJ, Al-Ansari N, El Shafei S, et al. Molecular identification and susceptibility of Trichosporon species isolated from clinical specimens in Qatar: isolation of Trichosporon dohaense Taj-Aldeen, Meis & Boekhout sp. nov. J Clin Microbiol 2009; 47:1791–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. de Almeida Júnior JN, Figueiredo DSY, Toubas D, et al. Usefulness of matrix-assisted laser desorption ionisation–time-of-flight mass spectrometry for identifying clinical Trichosporon isolates. Clin Microbiol Infect 2014; 20:784–90. [DOI] [PubMed] [Google Scholar]
- 11. de Almeida JN, Favero Gimenes VM, Francisco EC, et al. Evaluating and improving Vitek MS for identification of clinically relevant species of trichosporon and the closely related genera Cutaneotrichosporon and Apiotrichum. J Clin Microbiol 2017; 55:2439–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Arendrup MC, Boekhout T, Akova M, et al. ; European Society of Clinical Microbiology and Infectious Diseases Fungal Infection Study Group; European Confederation of Medical Mycology ESCMID and ECMM joint clinical guidelines for the diagnosis and management of rare invasive yeast infections. Clin Microbiol Infect 2014; 20(Suppl 3):76–98. [DOI] [PubMed] [Google Scholar]
- 13. Matsue K, Uryu H, Koseki M, et al. Breakthrough trichosporonosis in patients with hematologic malignancies receiving micafungin. Clin Infect Dis 2006; 42:753–7. [DOI] [PubMed] [Google Scholar]
- 14. Goodman D, Pamer E, Jakubowski A, et al. Breakthrough trichosporonosis in a bone marrow transplant recipient receiving caspofungin acetate. Clin Infect Dis 2002; 35:E35–6. [DOI] [PubMed] [Google Scholar]