Abstract
The transcription factor nuclear factor-κB (NFκB) is an ubiquitously expressed inducible regulator of a broad range of genes and plays a pivotal role in cell death and survival pathways. Three models of brain tolerance (ischemic, epileptic, and polyunsaturated fatty acid-induced preconditioning), known to confer resistance to neurons against ischemia or status epilepticus, were used to determine whether NFκB mediated the late preconditioning. A sublethal 3 min ischemia, a dose of 5 mg/kg kainic acid (KA5) or 500 nmol of linolenic acid (LIN500) led to a rapid increase of NFκB DNA-binding activity and nuclear translocation of p65 and p50 subunits of NFκB in neurons. Pretreatment with the NFκB inhibitor diethyldithiocarbamate or κB decoy DNA blocked the increased DNA-binding activity and the nuclear translocation of NFκB and abolished the neuroprotective effects of different delayed preconditionings against severe ischemia or epilepsy. The inhibition of NFκB observed in rats preconditioned with 3 min ischemia, KA5 or LIN500 treatments compared with ischemic or epileptic controls was correlated with the prevention of the inducible degradation of the inhibitory protein IκBα. Preconditioning probably inhibits the activation of NFκB by interfering with a pathway that leads to the direct transcriptional activation of IκBα by NFκB itself. The present work provides evidence that activation of NFκB is a crucial step in the signal transduction pathway that underlies the development of brain tolerance and may open new strategies in the prevention of cerebral diseases, such as ischemia or epilepsy.
Keywords: NFκB, brain preconditioning, ischemia, kainic acid, excitotoxicity, polyunsaturated fatty acids
Noxious stimuli applied at doses close to but below the threshold of cell injury induce adaptative responses that protect the brain against additional stress from the same (tolerance) or other (cross-tolerance) stimuli. Among different stresses, hypoxia (Gidday et al., 1994), ischemia (Kitagawa et al., 1990; Kirino et al., 1991; Liu et al., 1992; Simon et al., 1993;Glazier et al., 1994; Heurteaux et al., 1995; Matsushima and Hakim, 1995; Toyoda et al., 1997), seizures (Plamondon et al., 1999), anoxia (Perez-Pinzon et al., 1996), spreading depression (Kawahara et al., 1994; Matsushima et al., 1996), heat (Chopp et al., 1989; Kitagawa et al., 1991b), oxidative stress (Ohtsuki et al., 1992), polyunsaturated fatty acids (PUFAs) treatment (our unpublished data), and inhibitors of oxidative phosphorylation (Riepe et al., 1997) induce tolerance to subsequent cerebral (focal or global) ischemia. Similarly, kainic acid (KA)- or bicuculline-induced seizures and hippocampal kindling reduce the injurious impact of a second epileptic challenge (Kelly and McIntyre, 1994; Sasahira et al., 1995;Plamondon et al., 1999). The existence of early and delayed phases of preconditioning against brain injuries is now as well established as it is in cardiac preconditioning (Millar et al., 1996). Clearly, the first phase occurs within minutes and is transient (Perez-Pinzon et al., 1997), whereas the delayed phase takes hours to become apparent and lasts for days (Kitagawa et al., 1990; Kirino et al., 1991). Recent studies show that the initial signals responsible for triggering the development of both preconditionings involve the opening of ATP-sensitive K+ channels (KATP channels) via the activation of adenosine A1 receptors (Heurteaux et al., 1995; Reshef et al., 1998a,b; Plamondon et al., 1999; Blondeau et al., 2000). However, delayed preconditioning requires de novo synthesis of proteins, promoting neuronal survival, including heat shock protein 70 (Kitagawa et al., 1990, 1991a; Liu et al., 1993; Nishi et al., 1993; Simon et al., 1993; Blondeau et al., 2000), Bcl-2 (Shimazaki et al., 1994), and superoxide dismutase (MnSOD) (Toyoda et al., 1997). It seems likely that the signaling pathway of late preconditioning would include the activation of transcription factors that drive the expression of proteins responsible for neuroprotection.
One of the transcription factors that could activate gene expression in response to epileptic or ischemic preconditioning is the nuclear factor-κB (NFκB). This oxidative responsive transcription factor plays a pivotal role in neuronal survival and plasticity (for review, see Mattson et al., 2000). NFκB is activated by various intercellular signals, including cytokines, neurotrophic factors, and neurotransmitters. Oxidative stress and elevation of intracellular calcium levels are particularly important inducers of NFκB activation. Stimulation of glutamate receptors and membrane depolarization lead to activation of NFκB in hippocampal pyramidal neurons and cerebellar granule neurons (Guerrini et al., 1995;Kaltschmidt et al., 1995). NFκB activity is increased in neurons and glial cells in both neurodegenerative disorders (Hunot et al., 1997;Kaltschmidt et al., 1997; Lukiw and Bazan, 1998) and models of stroke, cardiac arrest, or epilepsy (Rong and Baudry, 1996; Clemens et al., 1997; Gabriel et al., 1999). The involvement of NFκB in the inhibition of apoptosis is now well established (Mattson et al., 2000). NFκB plays a central role in the induction of neuroprotective antiapoptotic gene products, such as MnSOD and Bcl-2 that are known to contribute to ischemic tolerance (Toyoda et al., 1997). NFκB is made up of two prototypical subunits of 50 kDa (p50) and 65 kDa (p65; RelA) that belong to the Rel family. The most usual form of NFκB is a heterodimer of p65 and p50, which normally exists in the cytoplasm in a dormant form bound to one of a member of inhibitory proteins called IκBα, IκBβ, IκBε, p105, and p100 (for review, seeVerma et al., 1995; Baeuerle and Baltimore, 1996). During activation, NFκB dissociates from Iκβ and translocates as a p50/p65 dimer to the nucleus as a result of the complete proteolytic degradation of Iκβ proteins or the partial degradation of p105 and p100 precursors. Phosphorylation by a protein kinase complex Iκβ kinase and ubiquitination of Iκβ are necessary for dissociation of Iκβ from the transcription dimer, which binds to consensus κβ sequences in the enhancer region of κβ-responsive genes and then can initiate gene transcription (Chen et al., 1995; Verma et al., 1995; Baeuerle and Baltimore, 1996).
The purpose of the present study is to test the hypothesis that the delayed preconditioning is mediated by NFκB and to characterize the mechanisms that trigger the translocation of NFκB during preconditioning in three models of brain tolerance (ischemic, epileptic, and polyunsaturated fatty acid-induced preconditioning) known to confer resistance to hippocampal neurons against neuronal injury associated with ischemia or status epilepticus.
MATERIALS AND METHODS
Animals. Experiments were performed on male Wistar rats weighing 250–300 gm (Charles River Laboratories, St. Aubin, France). The animals, maintained on a 12 hr light/dark cycle, were given food and water ad libitum. They were acclimatized for at least 1 week before drug treatments or surgery. All animal experiments were performed in accordance with NIH Guide for the Care and Use of Laboratory Animals. All efforts were made to minimize the number of animals used and their suffering.
Preconditioning procedures. Two different paradigms of brain injury were used: the four-vessel occlusion model of transient global forebrain ischemia (Pulsinelli and Brierley, 1979) and KA-induced (seizure-mediated) excitotoxic damage (Lothman and Collins, 1981) to hippocampal neurons. Vehicle-injected or sham-operated rats were used as negative controls for ischemia and epilepsy. Preconditioned groups were as follows. Ischemic preconditioned rats received a 3 min sublethal global ischemia (I3) before severe 6 min ischemia (I6); KA5-preconditioned animals were intraperitoneally injected with a 5 mg/kg dose of KA 3 d before a second KA7.5 challenge (7.5 mg/kg). PUFA-preconditioned rats were intravenously injected with linolenic acid (LIN500, 500 nmol/kg body weight) 3 d before KA7.5 injection or 6 min ischemia. Vehicle-injected or sham-operated animals treated 3 d before KA7.5 injection or 6 min ischemia were used as controls for the preconditioned groups. Rats were killed at 1, 24, and 72 hr after the last treatment (n = 6 per time per group).
Transient complete forebrain ischemia. Transient complete forebrain ischemia was performed by four-vessel occlusion as described previously (Pulsinelli and Brierley, 1979; Heurteaux et al., 1995). Briefly, rats were deeply anesthetized by inhalation of 2% halothane mixed with 30% oxygen and 70% nitrous oxide. The vertebral arteries were irreversibly occluded by electrocoagulation, and a small-diameter silicon tubing was looped around the carotid arteries to facilitate subsequent occlusion. On the following day, both carotid arteries were clamped with microvascular clamps for 3 or 6 min in awake and spontaneously ventilating animals. Rats lost their righting reflex within 1 min of carotid clamping. Cessation of electroencephalographic activity was confirmed during ischemic insults. Heartbeat, arterial blood pressure, and core temperature were continuously monitored during surgery, ischemia, and drug administration. The body temperature of rats was supported with a heating blanket during and in the hours after surgery, ischemia, and reperfusion. No difference in body temperature, heartbeat, and arterial blood pressure has been seen among the different groups.
Drug treatments. All drugs were freshly mixed on the day of experimentation. KA (Sigma, St. Louis, MO) was dissolved in NaCl 0.9% solution and injected intraperitoneally (5 and 7.5 mg/kg, i.p.). All rats that were treated with KA exhibited seizures within the first hour after injection. LIN was first dissolved in ethanol at a molar concentration and then diluted in NaCl 0.9% solution to reach a final concentration of 500 μm. LIN500 (500 nmol/kg body weight, i.v.) was injected 3 d before KA (7.5 mg/kg, i.p.) injection or 6 min ischemia. The pH of the different solutions was adjusted to 7.0. The diethyldithiocarbamate (DTTC) (Sigma) was dissolved in NaCl 0.9% solution and injected intraperitoneally (150 mg/kg, i.p.) 15 min before LIN500 or KA5 administration or sublethal 3 min ischemia.
Administration of κB decoy DNA. As reported previously (Smith-Swintosky et al., 1994; Yu et al., 1999), double-stranded κB decoy DNA was prepared by annealing complementary single-stranded oligonucleotides of the following sequences: 5′-GAGGGGACTTTCCCT-3′ and 5′-AGGGAAAGTCCCCTC-3′. Control DNA with a scrambled sequence was prepared by annealing oligonucleotides of the following sequences: 5′-GATGCGTCTGTCGCA-3′ and 5′-TGCGACAGACGC1ATC-3′. Stocks of double-stranded DNA were prepared at a concentration of 2 mm in saline. κB decoy and control scrambled DNA (60 μg) were infused intracerebroventricularly at a rate of 0.5 μl/min for 20 min (two injections at 24 and 2 hr before sublethal 3 min ischemia or KA or LIN500 treatment) via a stainless steel cannula (23 gauge) stereotaxically implanted with a Kopf stereotaxic apparatus (David Kopf Instruments, Tujunga, CA) into the right lateral ventricle (dorsoventral, − 3.6 mm below the cortical surface; mediolateral, +1.4 mm from bregma; and anteroposterior, − 0.8 mm from bregma) (Smith-Swintosky et al., 1994; Yu et al., 1999).
Histological procedures. At the end of the experiment, animals were killed at designated time points, and brains were frozen quickly in isopentane at −40°C. Coronal sections (10 μm) were cut on cryostat (Leica, Nussloch, Germany) and post-fixed by immersion in 4% paraformaldehyde–10−2m PBS for 30 min. Slides were then dehydrated in ethanol baths (50, 70, and 100%), air dried, and stored at −70°C until use. For each brain studied (n = 6 per time point and treatment), two sections were placed on 3-aminopropylethoxysilane-coated slides, and 10 slides (randomly chosen) per rat were stained with cresyl violet. The neuronal density of hippocampal CA1 subfield, known to be the most vulnerable to ischemia, was determined by the method of Kirino (1982) on coronal sections of the dorsal hippocampus corresponding to brain sections located between 3.14 and 4.16 mm posterior to bregma (Paxinos and Watson, 1986). The total linear length of the CA1 sector was measured using a digitizer. The number of living neurons in the stratum pyramidale within the CA1 subfield was counted using a Leica Aristoplan photomicroscope at a magnification of 400×. Neurons that had shrunken cell bodies with surrounding empty spaces were excluded. The neuronal density of CA1 sector, i.e., the number of intact pyramidal cells per 1 mm linear length of the CA1 stratum pyramidale observed in each 10 μm section, was quantified. Thus, a mean value for each hippocampal CA1 substructure was obtained from 10 bilateral measurements on two sections per slide and 10 slides per rat, for the six animals in each of experimental group. The neuronal density for a given animal represents the average of both right and left hippocampal neuronal cell densities. Neuronal density values were expressed as mean ± SEM. Data analysis was performed by two-factor (experimental condition and brain region) ANOVA, followed by Tukey's w test for multiple comparisons. A probability <5% was considered statistically significant.
Preparation of nuclear and cytosolic extracts. Nuclear and cytosolic extracts from hippocampi were prepared according to the method reported previously with some modifications (Dignam et al., 1983). Briefly, after being removed from storage at −70°C, hippocampi (n = 6 per experimental group) were homogenized in four volumes of ice-cold lysis buffer containing 10 mm HEPES, pH 7.9, 1.5 mmMgCl2, 10 mm KCl, 1% NP-40, 0.5 mm dithiothreitol, and protease inhibitor cocktail on ice using a Dounce homogenizer. After 10 min at room temperature, homogenates were centrifuged at 6000 ×g for 5 min at 4°C. The supernatant was taken as the crude cytosolic fraction. The pellet was resuspended in 10 vol of cold washing buffer (20 mm HEPES, pH 7.9, 25% glycerol, 420 mm NaCl, 1.5 mm MgCl2, 0.2 mm EDTA, 0.5 mmdithiothreitol, and protease inhibitor cocktail). After 30 min at 4°C, under continuous gentle mixing, the extracted nuclear proteins were collected by centrifugation at 12,500 × g for 30 min at 4°C. The supernatant was dialyzed 1 hr at 4°C against 10 mm Tris, 10 mmMgCl2, 100 mm KCl, 1 mm EDTA, 1 mmdithiothreitol, and protease inhibitor cocktail. This dialyzed supernatant was again centrifuged at 50,000 × g for 30 min at 4°C. The pellet resuspended in 20 mmHEPES, pH 7.9, 50 mm KCl, 0.2 mm EDTA, 0.2 mmdithiothreitol, and protease inhibitor cocktail was aliquoted and stored at −70°C until use.
The crude cytosolic fractions were mixed with vol cytosolic extraction buffer (0.3 m HEPES, pH 7.9, 0.03 mmMgCl2, 1.4 M KCl, 0.5 mmdithiothreitol, and protease inhibitor cocktail) and centrifuged at 100,000 × g for 1 hr at 4°C. The supernatant was dialyzed, centrifuged, aliquoted, and stored at −70°C as described above. Protein concentrations of the final nuclear and cytosolic fractions were determined by using Bradford's method (Bradford, 1976). Aliquots of the nuclear and cytosolic extracts were stored at −70°C for gel shifts, supershift assays, and Western blottings.
Electrophoretic mobility shift assay. The gel-shift assay was performed using a commercial DNA-binding protein detection system (Promega, Charbonniéres, France), as described by the manufacturer. Briefly, double-stranded oligonucleotide containing the κB consensus sequence (5′-AGTTGAGGGGACTTTCCCAGGC-3′) was end-labeled using [γ-32P]ATP (6000 Ci/mmol; ICN Biochemicals, Orsay, France) and T4 polynucleotide kinase and was purified by centrifugation through a G-25 spin column (Amersham Pharmacia Biotech, Saclay, France). DNA binding was performed in 20 μl reaction containing a 20 μg aliquot of extracted nuclear protein, 10 mm HEPES, pH 7.9, 50 mm KCl, 0.2 mm EDTA, 2.5 mm DTT, 10% glycerol, and 0.05% NP-40. After 10 min of incubation on ice, 3 × 10−4cpm of labeled probe was added to the reaction, and the mixture was incubated for 20 min at 37°C. Then, protein–DNA complexes were resolved by electrophoresis through 4 or 7% native polyacrylamide gels (37.5:1 acrylamide/bisacrylamide) in buffer containing 5 mm Tris, pH 8.3, and 38 mmglycine for 4 hr at 150 V. Gels were dried, autoradiographed on a Bas-1500 phosphorimager (Fujifilm, Tokyo, Japan) for 4 hr, and exposed to x-ray film (X-Omat; Eastman Kodak, Le Pontet, France) using intensifier screens at room temperature for 3 d. The specificity of the identified κ-binding proteins in the nuclear extracts was determined by adding a 50-fold excess of unlabeled competitor to 20 μg of nuclear extract before incubation with the binding mixture containing buffer and labeled probe. The transcription factor AP2 consensus oligonucleotide (5′-GATCGAACTGACCGCCCG CGGCCCGT-3′) was used as the unlabeled nonspecific competitor. To ensure consistency in the data analysis, the nuclear and cytosolic extracts of different experimental groups were run on the same gel.
To measure total NFκB activity in the cytosol, cytosolic extracts (20 μg) were treated after the DNA-binding reaction with deoxycholate (DOC) at a final concentration of 0.5% for 5 min on ice, followed by incubation in 1% NP-40 for 30 min at room temperature to release NFκB from IκB.
For gel supershift experiments, the oligonucleotide–nuclear protein binding reaction was followed by incubating the mixture overnight at 4°C with 1 μg of either anti-p50 or anti-p65 antibodies (Santa Cruz Biotechnology, Tebu, France) separately or together. Electrophoretic mobility shift assay (EMSA) was then performed as described above.
All radioactive gels were quantified by densitometry using a Bas-1500 phosphorimaging system (Fujifilm) and TINA software. Data are expressed as mean ± SEM (n = 6). Data analysis was performed by two-factor ANOVA, followed by Tukey'sw test for multiple comparisons. A probability <5% was considered statistically significant.
Western blotting. Proteins in the nuclear and cytosolic extracts (20 μg) were separated by SDS-PAGE on 10% SDS-PAGE gels for 1 hr at 100 mA. Proteins were transferred onto nitrocellulose membrane (Hybond-C) in blotting buffer (156 mmTris, 1 m glycine, and PBS) for 2 hr at 50 mA and blocked with 4% skim milk (Regilait) in PBS for 2 hr at room temperature. The blotted membrane was incubated for 4 hr at room temperature with the rabbit polyclonal anti-NFκB p65 antibody (AB1604, diluted 1:2000; Chemicon, Euromedex, Mundolsheim, France) and overnight at 4°C with the mouse monoclonal antibody raised against the active form of NFκB (MAB3026, diluted 1:150; Chemicon) or the rabbit polyclonal anti-IκBα antibody (sc-847, diluted 1:500; Santa Cruz Biotechnology). After washing with 0.1% Tween 20–PBS (four times, 15 min each), the blots were incubated for 1 hr at room temperature with goat anti-rabbit IgG coupled to horseradish peroxidase (diluted 1:15,000; Jackson ImmunoResearch, Interchim, Montluson, France) and then washed again in 0.1% Tween 20–PBS. Fluorography was performed on Kodak X-Omat AR film using Western blotting detection reagents (Pierce, Rockford, IL) following the enhanced chemiluminescence technique. To ensure consistency in the data analysis, the nuclear and cytosolic extracts of the same sample were run on the same gel (n = 6). In each blot, α-tubulin was used as an internal control for the loading of protein level (data not shown).
Immunohistochemistry. Frozen sections (10 μm) were post-fixed with acetone for 10 min at −20°C. Sections were then immersed in 0.3% H2O2–methanol for 30 min, permeabilized in 0.3% Tween 20–PBS for 15 min, treated for 10 min in a microwave oven in 0.1 m citrate buffer, pH 6.0, and blocked with 1% horse–goat serum (Vector Laboratories, Burlingame, CA) for 4 hr at room temperature. Sections were then incubated with the mouse monoclonal antibody raised against the active form of NFκB (MAB3026, diluted 1:150; Chemicon) overnight at 4°C. After the primary incubation and three rinses in 1× PBS, sections were then incubated in biotinylated horse anti-mouse IgG or biotinylated goat anti-rabbit IgG (diluted 1:1000; Jackson ImmunoResearch) for 2 hr. NFκB labeling was compared with immunohistochemical stainings obtained with the monoclonal mouse antibody against the neuron-specific nuclear protein NeuN (neuronal nuclei) (MAB377, diluted 1:250; Chemicon), the rabbit anti-cow glial fibrillary acidic protein (GFAP) marker of astrocytes (clone V9, diluted 1:250; Dako, Trappes, France), the monoclonal mouse anti-vimentin (Z0334, diluted 1:50; Dako), and the monoclonal mouse anti-RT1B directed against the Class II major histocompatibility complex (MRC OX6, diluted 1:50; Biosource International, Cliniscience Montrouge, France), markers of activated microglia. Immunohistochemical expressions were visualized by DAB–DAB-Ni staining using the VectaStain ABC kit (Vector Laboratories). All sections were washed in distilled water and mounted with Entellan. For double labeling, the monoclonal mouse antibody against NeuN (MAB377, diluted 1:250; Chemicon) and the rabbit polyclonal anti-NFκ-B p65 subunit antibody (AB1604, diluted 1:150; Chemicon) were used and detected with the Alexa Fluor 488 goat–horse anti-rabbit–anti-mouse IgG antibodies (diluted 1:1000; Molecular Probes, Interchim, Montluson, France). Sections were analyzed using a laser-scanning confocal microscope (Leitz, Wetzlar, Germany).
RESULTS
Effect of preconditioning on NFκB DNA-binding activity and subcellular localization of p65 and p50 subunits (Western blotting and immunohistochemistry)
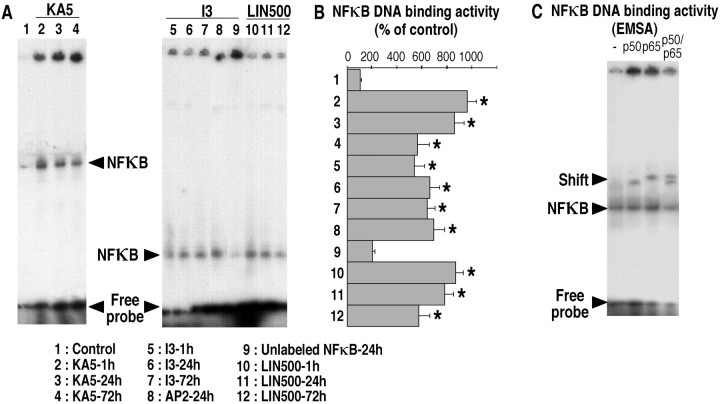
Figure 1 demonstrates that the three different preconditioning stimuli (sublethal 3 min ischemia, KA5 treatment, or LIN500 treatment) were associated with activation of NFκB. The gel-shift analysis (EMSA) of NFκB DNA-binding proteins at 1, 24, and 72 hr after ischemia or after treatment in hippocampal nuclear extracts from rats subjected to 3 min ischemia or injected with KA5 or LIN500 was compared with that obtained from controls (sham-operated or vehicle-injected). As illustrated in Figure 1,A and B, each preconditioning stimulus induced an intense NFκB DNA-binding activity as early as 1 hr after sublethal ischemia, KA5 treatment, or LIN500 treatment in pooled nuclear hippocampal tissue. Figure 1B summarizes the quantification of NFκB binding activity in nuclear extracts from the complete set of rats. For the three preconditioning stimuli, the increase in NFκB DNA-binding activity in the nuclear fraction varied from 5.4- to 9.7-fold compared with respective control groups. The specificity of the NFκB binding was demonstrated by a competitive experiment using unlabeled NFκB oligonucleotide probe and nonspecific transcription factor AP2 oligoprobe and performed on nuclear extracts from rats submitted to 3 min ischemia or treated with LIN500 or KA5. Competition assays using excess of nonradiolabeled NFκB-specific oligoprobe extinguished the specific retarded NFκB band, whereas the nonspecific competitor AP2 oligoprobe has no effect. Furthermore, supershift assays showed that the NFκB complex was composed predominantly of p65/p50 heterodimers under all conditions. Figure1C gives one example of supershift assay obtained with a preconditioning induced by a sublethal 3 min ischemia. Figure1C shows the marked slowing down of the migration of the NFκB–oligonucleotide complex (supershift) after the addition of specific anti-p50 and p65 antibodies to the EMSA reaction mixture. A combination of anti-p65 and anti-p50 antibodies caused additional gel retardation and reduced the NFκB DNA band (Fig. 1C). Similar results were obtained with KA5 or LIN500 treatment preconditioning stimulus (data not shown).
Fig. 1.
EMSA showing the time course of increased NFκB DNA-binding activity induced by the three different preconditionings (3 min ischemia, KA5 treatment, and LIN500 treatment).A, Representative gel shifts analysis showing NFκB DNA-binding activity in nuclear protein extracts from hippocampi of control rats (lane 1) or rats submitted to 3 min ischemia (lanes 5–9) or treated with KA5 (lanes 2–4) or LIN500 (lanes 10–12) and obtained at 1, 24, and 72 hr after the different preconditionings. NFκB DNA-binding activity was assayed as described in Materials and Methods. Competition assays of NFκB DNA-binding activity was performed in the presence of 50-fold excess of unlabeled competitor NFκB (lane 9) and nonspecific competitor AP2 (lane 8) consensus oligonucleotides. The shifted bands of specific NFκB DNA complexes are indicated by thearrowheads. The right andleft gels correspond to 4 and 7% polyacrylamide gels, respectively. B, Quantification of NFκB DNA-binding activity in the different experimental groups. The specific shifted bands were quantified using a phosphorimaging system as described in Materials and Methods. The values are expressed as a percentage of control. No significant differences were found between vehicle-injected and sham-operated rats, and values of these groups were pooled and termed control. Data represent the mean ± SEM values. Data are representative of six separate experiments in each group (n = 6). *p < 0.05 indicates statistical significance when compared with control.C, Supershift analysis of NFκB binding proteins present in nuclear extracts 24 hr after 3 min ischemia. The binding activity assay was performed in the presence of anti-p65 antibodies, anti-p50 antibodies, a combination of both, or no antibody. Thearrowheads indicate the bands of specific NFκB–DNA complexes, which were supershifted by anti-p65 antibodies, anti-p50 antibodies, or by their combination.
Figure 2 depicts the induction of NFκB protein in the hippocampus after the three types of preconditioning assessed using Western blot analysis (Fig. 2A–C) and immunohistochemistry (Fig. 3). Figure2A–C shows representative Western blotting analysis of the p65 (Fig. 2A,B) and p50 (Fig. 2C) content in cytosolic and nuclear extracts from rats subjected to 3 min ischemia or injected with 5 mg/kg KA or 500 nmol/kg LIN taken at serial times after sublethal or drug treatments. The p65 and p50 subunits of NFκB were rich in the cytosolic fractions from sham-operated or vehicle-injected rats but undetectable in the nuclear extracts. In contrast, the protein levels of p65 and p50 in the three preconditioned groups were significantly enhanced in the nuclear fraction and concurrently decreased in the cytosol as early as 1 hr, indicating a rapid translocation of these NFκB subunits from the cytosol to the nucleus.
Fig. 2.
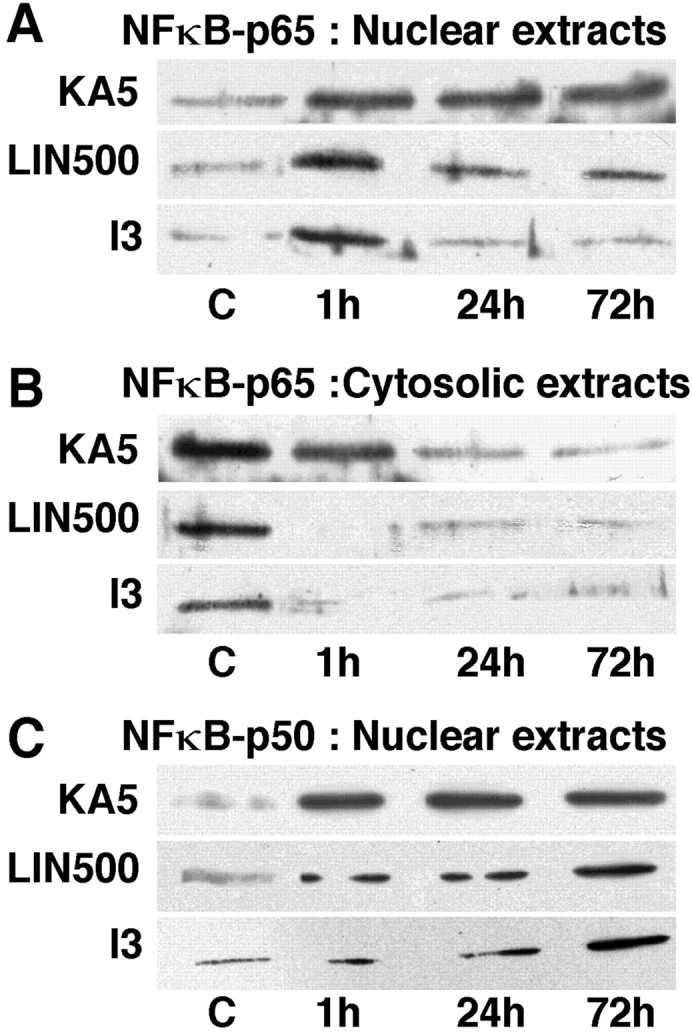
Representative Western blotting analysis of p65 and p50 subunits of NFκB in nuclear (A,C) and cytosolic (B) extracts from hippocampi of control rats (C) or rats submitted to 3 min ischemia (I3) or treated with KA5 or LIN500 and obtained at 1, 24, and 72 hr after the different preconditionings.
Fig. 3.
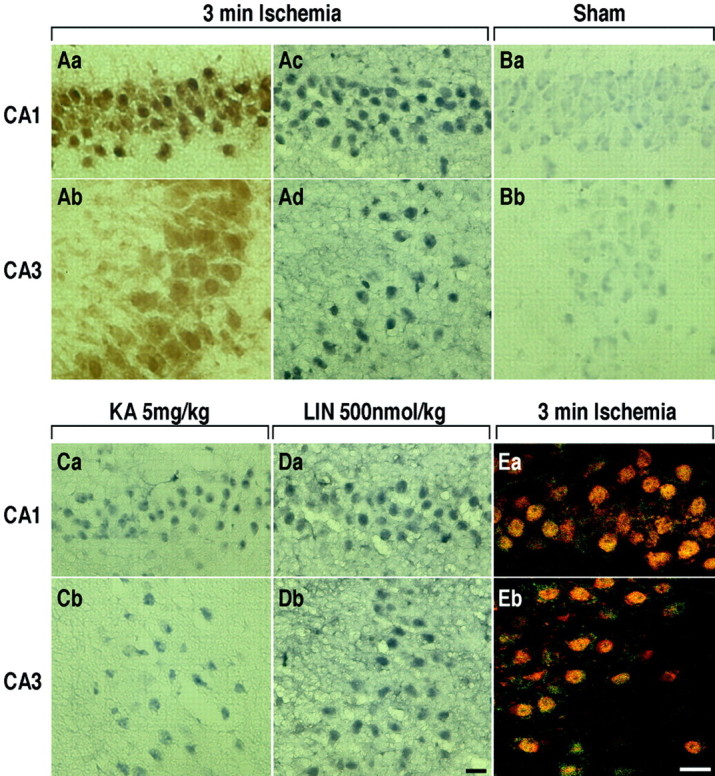
Representative immunohistochemical staining of the active form of NFκB protein in hippocampal CA1 and CA3 substructures of rats killed 24 hr after each of preconditioning stimuli.Aa–Ad, 3 min ischemia. Ba,Bb, Sham-surgery. Ca, Cb, KA5 treatment. Da, Db, LIN500 treatment.Aa, Ab, Immunohistochemical staining of NeuN protein within CA1 and CA3 pyramidal cells after sublethal ischemia. E, Colocalization of NFκB-p65 and the neuron-specific nuclear protein NeuN (neuronal nuclei) within CA1 (Ea) and CA3 (Eb) pyramidal cells. Brain sections were immunostained with antibodies against the p65 subunit of NFκB (green) and NeuN (red) for double-labeling. Scale bars, 20 μm.
Immunostaining using a monoclonal antibody raised against the active form of NFκB performed at 24 hr after each of different preconditioning triggers (short ischemia, KA5 treatment, or LIN500 treatment) was performed to determine the cellular identity of the increase in NFκB activity associated with preconditioning visualized above by gel shift and Western blotting analysis (Figs. 1,2A–C). Immunoreactivity for the activated form of NFκB was not detectable in either sham-operated (Fig.3Ba,Bb) or vehicle-injected (data not shown) hippocampus. Sublethal 3 min ischemia (Fig.3Ac,Ad), KA5 treatment (Fig.3Ca,Cb), or LIN500 treatment (Fig.3Da,Db) induced a strong immunoreactivity for NFκB in CA1 and CA3 pyramidal cell layers (Fig.3Ac,Ad,Ca,Cb,Da,Db), hilar neurons, and dentate gyrus (data not shown) 24 hr after preconditioning stimulus. The extent and intensity of immunoreactivity appeared similar in three treatments. According to morphological criteria, the positive cells seemed to be neurons. Immunohistochemical observations with GFAP and vimentin antibodies excluded astrocytes and microglia as main sources of NFκB activation in the three models of preconditioning tested (data not shown). Immunostainings obtained with the antibody raised against the neuron-specific nuclear protein NeuN (Fig. 3Aa,Ab) provided evidence that the immunoreactivity for the active form of NFκB was predominant in the nucleus. Double labeling with antibodies against the neuron-specific nuclear protein NeuN and the NFκB-p65 subunit indicated nuclear colocalization (Fig. 3Ea,Eb).
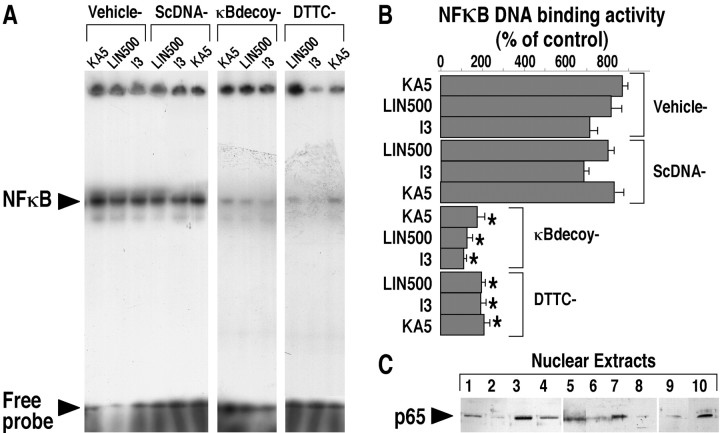
Effects of κB decoy DNA and DTTC on NFκB DNA-binding activity and subcellular localization of p65 subunit
κB decoy DNA and DTTC have been shown to block NFκB DNA-binding activity in different systems (Schreck et al., 1992;Smith-Swintosky et al., 1994; Yu et al., 1999). In the present study, double-stranded κB decoy DNA or control double-stranded DNA with a scrambled sequence was injected intracerebroventricularly (two injections at 24 and 2 hr before 3 min ischemia, KA5 treatment, or LIN500 treatment), and rats were killed 1 hr after the preconditioning stimulus. As illustrated in Figure 4,A and B, the gel-shift analysis of NFκB shows that the increase in NFκB DNA-binding activity induced by each preconditioning was suppressed in hippocampus of rats injected with κB decoy DNA but was unaffected in animals injected with control scrambled DNA. Figure 4B summarizes the quantification of NFκB DNA-binding activity in nuclear extracts from the complete set of rats. For the three preconditioning stimuli, the decrease in NFκB DNA-binding activity in the nuclear fraction varied from 4.8- to 6.0-fold compared with respective control groups (KA5, LIN500, or I3). The remaining NFκB DNA-binding activity corresponded to that of negative controls (vehicle-injected or sham-operated rats). Administration of κB decoy DNA prevented the decrease in p65 content in the cytosolic extracts (data not shown) and its increase induced by sublethal ischemia (I3) or LIN500 treatment in the nuclear extracts analyzed 24 hr after the preconditioning stimulus (Fig. 4C). A similar result was obtained with KA5 treatment preconditioning stimulus (data not shown).
Fig. 4.
Electrophoretic mobility shift assay (A, B) and Western blotting analysis of p65 subunit of NFκB (C) showing the effect of intracerebroventricular administration of κB decoy DNA or intraperitoneal injection of DTTC on the increased NFκB DNA-binding activity induced by the three different preconditionings (3 min ischemia, KA5 treatment, and LIN500 treatments). A, Representative gel shift analysis showing NFκB DNA-binding activity in hippocampal nuclear extracts isolated from rats that had received intracerebroventricular injections of vehicle, 60 μg of κB decoy DNA (κBdecoy), 60 μg of scrambled control DNA (ScDNA), or intraperitoneal injection of DTTC (150 mg/kg) before sublethal ischemia (I3) or administration of either KA5 or LIN500. Rats were killed 1 hr (for κB decoy or scrambled control DNA) or 24 hr (for DTTC) after each type of preconditioning. NFκB activity was assayed as described in Materials and Methods. The shifted band of specific NFκB DNA complexes is indicated by the arrowhead. B, Quantification of NFκB DNA-binding activity in the different experimental groups. The specific shifted bands were quantified using a phosphorimaging system as described in Materials and Methods. Values are expressed as a percentage of control. Results are expressed as mean ± SEM. Data are representative of six separate experiments in each group (n = 6). *p < 0.05 indicates statistical significance when compared with vehicle-injected rats. C, Representative Western blotting analysis of p65 subunit of NFκB in hippocampal nuclear extracts isolated from rats that had received intracerebroventricular injections of vehicle, 60 μg of κB decoy DNA (κBdecoy), 60 μg of scrambled control DNA (ScDNA) or intraperitoneal DTTC injection (150 mg/kg) before I3 or LIN500. Rats were killed 24 hr after the conditioning stimulus. The position of p65 is indicated by thearrowhead. 1, Vehicle; 2, DTTC–LIN500; 3, LIN500; 4, Sham-operated; 5, I3; 6, DTTC–I3;7, scrambled control DNA–LIN500; 8, κB decoy DNA–LIN500; 9, κB decoy DNA–I3;10, scrambled control DNA–I3.
In the same manner, administration of DTTC (150 mg/kg, i.p.) 15 min before 3 min ischemia, KA5 treatment, or LIN500 treatment significantly blocked the increase in NFκB DNA-binding activity in the nuclear fraction of hippocampi analyzed 24 hr after sublethal ischemia or drug treatment (KA5 or LIN500) (Fig.4A,B). Analysis of extracts from rats pretreated with DTTC and then exposed to the different preconditioning stimuli showed a greatly reduced level of p65 content in nuclear fraction compared with hippocampi submitted to 3 min ischemia or injected with LIN500 in the absence of DTTC (Fig.4C). A similar result was obtained with KA5 treatment preconditioning stimulus (data not shown).
Effects of κB decoy DNA and DTTC treatment on the hippocampal ischemic tolerance induced by the different preconditionings
The effects of κB decoy DNA and DTTC treatment on brain tolerance were assessed by analysis of the neuronal degeneration in CA1 substructure of rats killed 7 d after the second ischemia. Figure5, A and C, shows representative photomicrographs of the CA1 sector in the different groups, and Figure 5, B and D, reports the quantitative analysis of neuronal cell density in the respective experimental groups. As expected, control (sham-operated or vehicle-injected) rats did not show neurodegeneration (Fig.5Aa). In contrast, typical cell death appeared in pyramidal neurons of CA1 substructure after 6 min ischemia (Fig.5Ab,Cb). Compared with control rats (Fig.5Ba,Da), 21% of CA1 pyramidal cells only survived (Fig. 5Bb,Db). Preconditioning with sublethal 3 min ischemia (Fig. 5Ac) or LIN500 injection (Fig. 5Cc) 3 d before 6 min ischemia totally prevented neuronal death induced by severe ischemia. In these preconditioned groups, 99 and 95% of CA1 cells were preserved, respectively (Fig.5Bc,Dc). However, the intracerebroventricular administration of κB decoy DNA before each preconditioning stimulus (3 min ischemia or LIN500 treatment) abolished the ischemic tolerance and markedly enhanced the hippocampal neurodegeneration (Fig.5Ad,Cd) compared with rats that were injected with scrambled control DNA before preconditioning (Fig.5Ae,Ce). The injection of κB decoy DNA alone did not induce any damage in hippocampus (Fig.5Cg,Dg). In the same manner, the intraperitoneal injection of DTTC before 3 min ischemia (Fig. 5Af) or LIN500 treatment (Fig. 5Cf) blocked the ischemic tolerance induced by each preconditioning. Quantitative analysis of neuronal damage in CA1 substructure confirmed the marked enhancement of CA1 pyramidal cell degeneration in rats injected with κB decoy DNA before each preconditioning stimulus (Fig.5Bd,Dd) compared with rats submitted to 6 min ischemia (Fig. 5Bb,Db). Seventy and 75% of CA1 pyramidal neurons were destroyed in rats injected with κB decoy DNA before sublethal 3 min ischemia (Fig. 5Bd) or LIN500 injection (Fig. 5Dd), respectively. Similar results were obtained with epileptic tolerance (data not shown). Together, these data show that the treatment with κB decoy DNA or DTTC prevented the neuroprotective effects of late preconditionings (sublethal ischemia, LIN500 treatment, or KA5 treatment) against ischemia or epilepsy and that the blockade of NFκB activation was deleterious in the three models of brain tolerance used in that work.
Fig. 5.
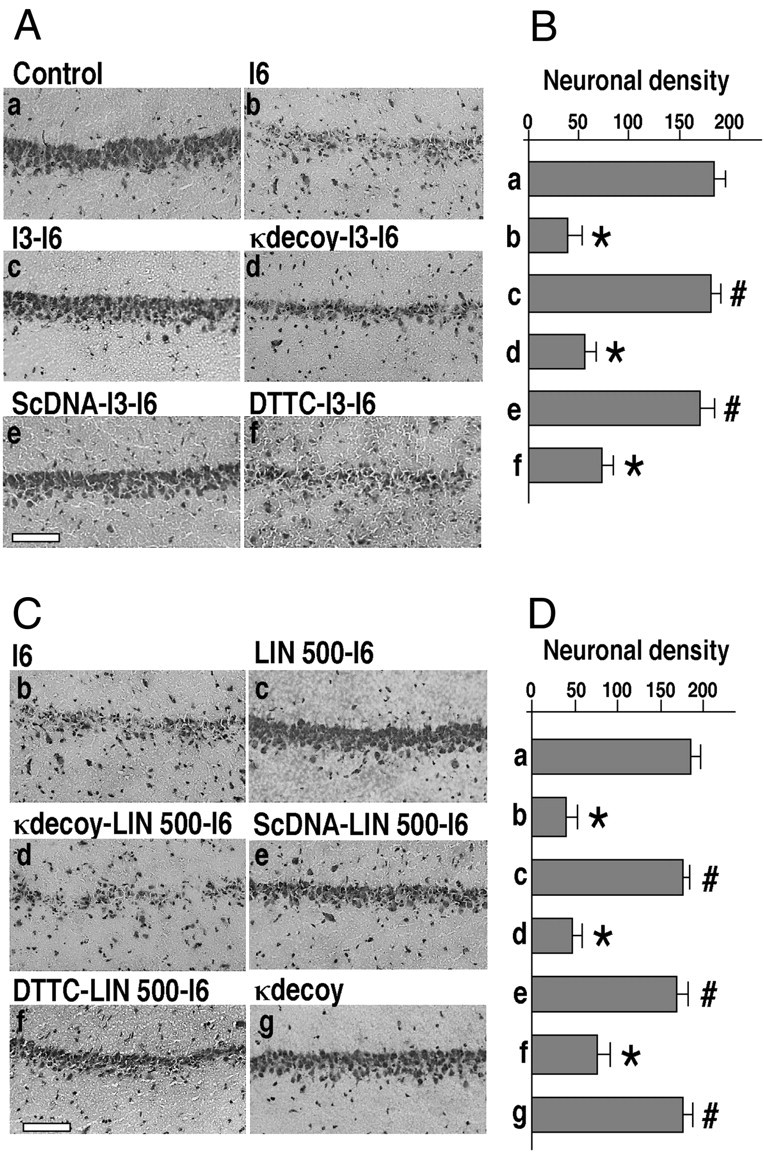
Effect of κB decoy DNA, scrambled control DNA, and DTTC injections on the ischemic tolerance induced by brief ischemia or LIN500 treatment. A, C, Representative photomicrographs highlighting morphological changes in CA1 subfield of cresyl violet-stained hippocampal sections 7 d after severe 6 min ischemia in the different experimental groups. I6corresponds to rats submitted to 6 min ischemia. I3-I6corresponds to rats submitted to 3 min ischemia 3 d before 6 min ischemia. κdecoy I3-I6 or ScDNA I3-I6corresponds to rats that, respectively, had received intracerebroventricular injections of 60 μg of κB decoy DNA or scrambled control DNA at 24 and 2 hr before 3 min ischemia. DTTC I3-I6 corresponds to rats that had received an intraperitoneal injection of DTTC (150 mg/kg) 30 min before 3 min ischemia. Rats were killed 7 d after 6 min ischemia. Scale bar, 100 μm.B, D, Quantification of neuronal density in the hippocampal CA1 pyramidal layer of different experimental groups. Results are expressed as mean ± SEM (n = 6) and represent neuronal densities assessed in cresyl violet-stained sections per 1 mm linear length of CA1 pyramidal layer. A mean value for each CA1 substructure was obtained from 10 bilateral measurements on two sections per slide and 10 slides per animal (n = 6) in each of the experimental groups. Differences were considered statistically significant whenp < 0.05 (Tukey's test). * indicates significantly different from control (sham-operated animals). # indicates significantly different from ischemic animals (6 min).
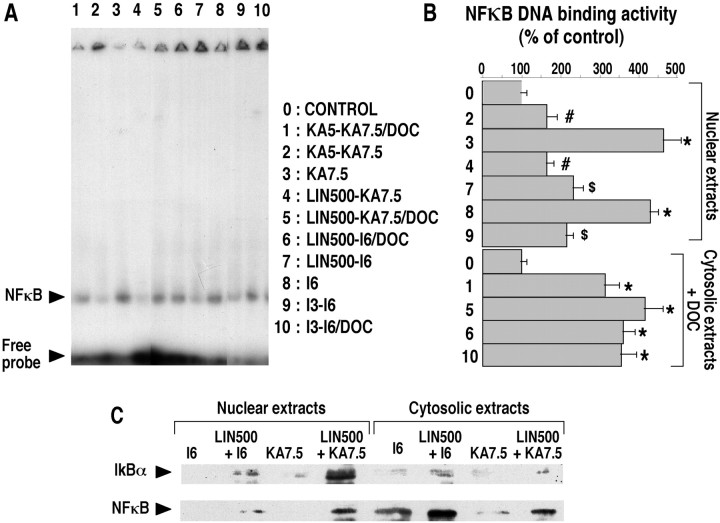
Changes in NFκB DNA-binding activity and subcellular localization of IκBα and the active form of p65 in the different groups of preconditioned brains
Electrophoretic mobility shift assays revealed that NFκB DNA-binding activity was decreased in nuclear extracts of rats preconditioned with 3 min ischemia, KA5 treatment, or LIN500 treatment compared with rats submitted to 6 min ischemia or treated with 7.5 mg/kg KA (Fig. 6A). Treatment with DOC, which dissociates the cytosolic NFκB–IκB complex, allowing the detection of inactive NFκB, restored NFκB DNA-binding activity in preconditioned hippocampi (Fig.6A). This indicated that NFκB was present but not active in preconditioned rats. Figure 6B summarizes the quantification of NFκB DNA-binding activity in nuclear and cytosolic extracts from the complete set of rats. For the three preconditioned groups, the NFκB DNA-binding activity in nuclear extracts decreased 44–65% compared with respective positive controls. The restoring of the NFκB DNA-binding activity after DOC treatment in cytosolic extracts reached 90% compared with positive controls (Fig. 6B). A possible mediator of the inhibitory action of preconditioning on NFκB activation is IκB, encoded by the immediate early gene MAD-3 (Haskill et al., 1991). IκB degradation is enhanced by various NFκB inducers, which also cause new synthesis of IκBα by an inducible autoregulatory pathway (Sun et al., 1993). The effect of preconditioning on IκBα and NFκB metabolism was examined by immunoblotting with antibodies to IκBα and active form of NFκB, which recognizes the heterotetrameric protein, consisting of the two p50 and two p65 subunits. Analysis of nuclear and cytosolic extracts of control, ischemic, or epileptic rats revealed that the loss of IκBα correlated with translocation of NFκB from the cytoplasm to the nucleus (Fig. 6C). Severe ischemia and KA treatment (7.5 mg/kg) led to the disappearance of IκBα and to the presence of the active form of NFκB in cytosolic extracts. In contrast, the amount of IκBα protein was notably increased in nuclear extracts of rats preconditioned with LIN500 treatment (LIN500-I6 or LIN500-KA7.5) and submitted to severe 6 min ischemia or KA7.5 treatment 3 d later (Fig. 6C). A similar result was obtained with rats preconditioned with 3 min ischemia or KA5 treatment (data not shown). The profile of preconditioning-induced IκBα and of the accumulation of the active form of NFκB paralleled that of the inhibition of NFκB DNA-binding activity. Preconditioning with 3 min ischemia, KA5 or LIN500 treatment resulted in retention of p65 in cytoplasm (data not shown).
Fig. 6.
Changes in NFκB DNA-binding activity and subcellular localization of IκBα and active form of NFκB in the different groups of preconditioned brains. A, Representative gel shifts analysis showing NFκB DNA-binding activity in hippocampal nuclear and cytosolic extracts isolated from rats preconditioned with 3 min ischemia (I3-I6), KA5 treatment (KA5-KA7.5), or LIN500 treatment (LIN500-I6 or LIN500-KA7.5) and submitted to 6 min ischemia or KA7.5 treatment 3 d later. Rats were killed 24 hr after the last treatment. Cytosolic extracts were analyzed by EMSA with DOC treatment after binding as described in Materials and Methods. The shifted band of specific NFκB–DNA complexes is indicated by the arrowhead. B, Quantification of NFκB DNA-binding activity in the different experimental groups. The specific shifted bands were quantified using a phosphorimaging system as described in Materials and Methods. The values are expressed as a percentage of control. No significant differences were found between saline-injected and sham-operated rats, and values of these groups were pooled and termed control. Results are expressed as mean ± SEM. Data are representative of six separate experiments in each group (n = 6). Differences were considered statistically significant whenp < 0.05 (Tukey's test). * indicates significantly different from control (saline-injected or sham-operated animals). # indicates significantly different from KA7.5-injected animals. $ indicates significantly different from ischemic animals (6 min). C, Representative Western blotting analysis of IκBα and active form of NFκB in hippocampal nuclear and cytosolic extracts isolated from ischemic (I6) and epileptic (KA7.5) rats and rats preconditioned with LIN500 treatment (LIN500-I6 orLIN500-KA7.5) and submitted to severe 6 min ischemia or KA7.5 treatment 3 d later. Rats were killed 24 hr after the last treatment. The positions of IκBα and active form of NFκB are indicated by the arrowheads.
DISCUSSION
Many different mechanisms have been proposed to be involved in the development of brain tolerance, including adenosine receptor stimulation, KATP channel opening, and delayed expression of neuroprotective genes. However, little is known on the nature of events occurring between the early opening of KATP channels through adenosine receptors and the induction of neuroprotective genes within the time window of protection-promoting neuronal survival. The switching “on–off” of gene expression is the province of transcription factors, which operate singly or in association with other proteins. The present work provides the first demonstration of the key role of the NFκB transcription factor in the signal transduction cascade of brain tolerance. The NFκB proteins are a family of inducible transcription factors that activate a variety of cellular genes involved in control of the inflammatory response and in regulating cellular growth (Mattson et al., 2000). The NFκB signaling pathway is a major determinant in the control of neuronal death and/or cell survival. Although NFκB activation occurs in neurons after brain injury, its role in the injury outcome remains unclear. The assumption that NFκB is contributing to neuronal cell death is documented by many papers reporting increased NFκB activity under pathological conditions in which neurons were dying (Grilli et al., 1996; Clemens et al., 1997). However, subsequentin vitro studies provide evidence that the activation of NFκB can protect neurons against amyloid β-peptide toxicity (Barger et al., 1995) and excitotoxic or oxidative stress (Goodman and Mattson, 1996; Mattson et al., 1997). Previous studies, in which injury-induced NFκB activity was suppressed by gene deletion of the p50 subunit (Yu et al., 1999) or administration of κB decoy DNA (Mattson et al., 1997; Yu et al., 1999) or pharmacological agents (Taglialatela et al., 1997; Maggirwar et al., 1998), strongly support a neuroprotective role for NFκB activation. NFκB consists of a p50 and p65/RelA complex that is trapped in the cytoplasm by an inhibitory protein IκBα (Verma et al., 1995; Baeuerle and Baltimore, 1996). As long as IκBα is bound to the p50/p65 complex, its translocation to the nucleus is prevented. Activation of NFκB consists of phosphorylation or degradation of IκBα from the complex in the cytoplasm, and during activation NFκB is translocated to the nucleus of the cell (Chen et al., 1995; Verma et al., 1995; Baeuerle and Baltimore, 1996).
Results reported in this paper demonstrate that, in the three models of brain tolerance studied (ischemic, epileptic, and polyunsaturated fatty acid-induced preconditionings), the activation of NFκB was required for the development of late cerebral preconditioning against severe ischemia or epilepsy. The three different inducers of preconditioning (sublethal 3 min ischemia, KA5 treatment, or LIN500 treatment) induced rapid activation of NFκB, as evidenced by its increased DNA-binding activity and nuclear translocation. The gel-shift analyses revealed that DNA-binding activity increased as early as 1 hr after sublethal ischemia, KA5 treatment, or LIN500 treatment, and the shifted band consisted of p50/p65 heterodimers. The presence of active NFκB was confirmed by nuclear localization of p50 and p65 subunits in Western blots of hippocampal extracts as early as 1 hr after each preconditioning stimulus, indicating a rapid translocation of NFκB subunits from cytosol to the nucleus. Immunohistochemical analyses using p65 antibodies revealed that, 24 hr after each of preconditioning stimuli, NFκB activation occurred in the pyramidal neurons and not in the glial cells. Pretreatment with the NFκB inhibitor DTTC or κB decoy DNA blocked the increased DNA-binding activity and the nuclear translocation of NFκB and, at the same time, abolished the neuroprotective effects of different delayed preconditionings against severe ischemia or epilepsy. Previous studies have shown that κB decoy DNA can block activation of κB-responsive genes, greatly increase the vulnerability of neurons to different insults, and promote neuronal cell death (Mattson et al., 1997; Yu et al., 1999). Dithiocarbamates, such as DTTC, have also been reported to be potent inhibitors of NFκB activation in various cell types (Schreck et al., 1992; Sherman et al., 1993; Ziegler-Heitbrock et al., 1993). Together, these results indicate that activation of NFκB is an essential mechanism whereby sublethal ischemia, KA5 treatment, or LIN500 treatment results in delayed neuroprotection.
The present work also provides evidence that the inhibition of NFκB observed in rats preconditioned with 3 min ischemia, KA5 treatment, or LIN500 treatment compared with ischemic or epileptic controls was correlated with the prevention of the inducible degradation of IκBα. Treatment of preconditioned extracts with the detergent DOC, which revealed as much DNA-binding activity in the different preconditioned hippocampi as in the controls, indicated that NFκB was present but not active in the preconditioned extracts. The preconditioning also prevented the release of NFκB from IκBα after a severe ischemic or epileptic insult. The phosphorylation and degradation of IκBα is necessary for the activation of NFκB and its subsequent appearance in the nucleus (Chen et al., 1995; Verma et al., 1995; Baeuerle and Baltimore, 1996). Therefore, on activation of NFκB, IκBα concentrations decrease. Immunoblotting with an antibody raised against IκBα reveals that the amount of IκBα protein increased in the preconditioned hippocampi compared with ischemic or epileptic cytosolic extracts. An interesting observation is the presence of IκBα protein and the active form of NFκB in the nuclear hippocampi of rats preconditioned with 3 min ischemia, KA5 treatment, or LIN500 treatment compared with ischemic or epileptic controls, in which IκBα protein was absent. The increase in IκBα abundance in preconditioned rats is probably the result of increased IκBα synthesis. This result strongly suggests that the inhibition of NFκB activation induced by preconditioning is mediated by induction of the IκBα inhibitory protein, which traps activated NFκB in inactive cytoplasmic complexes. In accordance with previous work, demonstrating the direct transcriptional activation of IκBα by NFκB itself (Scott et al., 1993; Sun et al., 1993; Chiao et al., 1994), IκBα probably newly synthetized after the activation of NFκB by preconditioning stimulus will bind free cytoplasmic NFκB and inactivate its potential nuclear translocation. Furthermore, excess IκBα translocates to the nucleus by an unknown mechanism, in which, as shown in vitro, it can sequester free NFκB (p65), promote net dissociation of DNA-bound NFκB, and thereby terminate its activity (Arenzana-Seisdedos et al., 1995). This nuclear NFκB–IκBα complex may be transported back to the cytoplasm or degraded in the nucleus. Recently, it has been shown that immunosuppression by glucocorticoids may be the direct outcome of the inhibition of NFκB activity through induction of IκBα synthesis (Auphan et al., 1995; Scheinman et al., 1995). It is not excluded that such a mechanism is also involved in the anti-inflammatory response and neuroprotection induced by sodium salicylate and aspirin (Kopp and Ghosh, 1994; Grilli et al., 1996).
In conclusion, these findings demonstrate that the transcription factor NFκB is indeed at the crossing of neuronal cell death and survival pathways and is a crucial component of the signal transduction cascade of cerebral preconditioning. This paper shows that (1) the three preconditioning protocols induce a rapid neuroprotective activation of NFκB in hippocampus, (2) the increases in NFκB DNA-activity determined by gel shift and Western blot analysis specifically reflect increases in hippocampal neurons, (3) preconditioning the brain with sublethal ischemia, KA5 treatment, or LIN500 treatment inhibits the activation of NFκB after the second injury and renders the brain more resistant to a subsequent potentially lethal ischemic or epileptic insult, and (4) the inhibition of NFκB is mediated by induction of the IκBα inhibitory protein, which traps activated NFκB in inactive cytoplasmic complexes. The cellular mechanisms whereby the three preconditioning treatments activate NFκB remains to be identified. Nitric oxide and free hydroxyl radicals are potential candidates for the role of NFκB activators. Not only they are known to activate NFκB but they are also known to be involved in brain and heart tolerance (Bolli et al., 1997; Centeno et al., 1999; Xuan et al., 1999; Rauca et al., 2000). The neuroprotection induced by activation of NFκB in hippocampal neurons related to induction of MnSOD (Mattson et al., 1997) and the increase of MnSOD activity in brain tolerance (Toyoda et al., 1997) strongly support the link between NFκB and oxidative stress in cerebral preconditioning. Together, these results strongly suggest that, whatever the type of preconditioning, the initial signals elicited by the conditioning stimulus are transduced into protective changes via an NFκB-dependent mechanism. The crucial involvement of this transcription factor in brain tolerance may open new ways in the search of therapeutic strategies.
Footnotes
This work was supported by the Centre National de la Recherche Scientifique, the Association Française contre les Myopathies, and the Conseil Regional (Provence-Alpes-Cote-d'Azur). We are grateful to G. Jarretou, F. Aguila, and V. Lopez for technical assistance.
Correspondence should be addressed to Prof. M. Lazdunski, Institut de Pharmacologie Moléculaire et Cellulaire, Centre National de la Recherche Scientifique, Unité Mixte de Recherche 6097, 660 route des Lucioles, Sophia Antipolis, 06560 Valbonne, France. E-mail:ipmc@ipmc.cnrs.fr.
REFERENCES
- 1.Arenzana-Seisdedos F, Thompson J, Rodriguez MS, Bachelerie F, Thomas D, Hay RT. Inducible nuclear expression of newly synthesized I kappa B alpha negatively regulates DNA-binding and transcriptional activities of NF-kappa B. Mol Cell Biol. 1995;15:2689–2696. doi: 10.1128/mcb.15.5.2689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Auphan N, DiDonato JA, Rosette C, Helmberg A, Karin M. Immunosuppression by glucocorticoids: inhibition of NF-kappa B activity through induction of I kappa B synthesis. Science. 1995;270:286–290. doi: 10.1126/science.270.5234.286. [DOI] [PubMed] [Google Scholar]
- 3.Baeuerle PA, Baltimore D. NF-kappa B: ten years after. Cell. 1996;87:13–20. doi: 10.1016/s0092-8674(00)81318-5. [DOI] [PubMed] [Google Scholar]
- 4.Barger SW, Horster D, Furukawa K, Goodman Y, Krieglstein J, Mattson MP. Tumor necrosis factors alpha and beta protect neurons against amyloid beta-peptide toxicity: evidence for involvement of a kappa B-binding factor and attenuation of peroxide and Ca2+ accumulation. Proc Natl Acad Sci USA. 1995;92:9328–9332. doi: 10.1073/pnas.92.20.9328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blondeau N, Plamondon H, Richelme C, Heurteaux C, Lazdunski M. KATP channel openers, adenosine agonists and epileptic preconditioning are stress signals inducing hippocampal neuroprotection. Neuroscience. 2000;100:465–474. doi: 10.1016/s0306-4522(00)00304-3. [DOI] [PubMed] [Google Scholar]
- 6.Bolli R, Manchikalapudi S, Tang XL, Takano H, Qiu Y, Guo Y, Zhang Q, Jadoon AK. The protective effect of late preconditioning against myocardial stunning in conscious rabbits is mediated by nitric oxide synthase. Evidence that nitric oxide acts both as a trigger and as a mediator of the late phase of ischemic preconditioning. Circ Res. 1997;81:1094–1107. doi: 10.1161/01.res.81.6.1094. [DOI] [PubMed] [Google Scholar]
- 7.Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1006/abio.1976.9999. [DOI] [PubMed] [Google Scholar]
- 8.Centeno JM, Orti M, Salom JB, Sick TJ, Perez-Pinzon MA. Nitric oxide is involved in anoxic preconditioning neuroprotection in rat hippocampal slices. Brain Res. 1999;836:62–69. doi: 10.1016/s0006-8993(99)01610-8. [DOI] [PubMed] [Google Scholar]
- 9.Chen Z, Hagler J, Palombella VJ, Melandri F, Scherer D, Ballard D, Maniatis T. Signal-induced site-specific phosphorylation targets I kappa B alpha to the ubiquitin-proteasome pathway. Genes Dev. 1995;9:1586–1597. doi: 10.1101/gad.9.13.1586. [DOI] [PubMed] [Google Scholar]
- 10.Chiao PJ, Miyamoto S, Verma IM. Autoregulation of I kappa B alpha activity. Proc Natl Acad Sci USA. 1994;91:28–32. doi: 10.1073/pnas.91.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chopp M, Chen H, Ho KL, Dereski MO, Brown E, Hetzel FW, Welch KMA. Transient hyperthermia protects against subsequent forebrain ischemic cell damage in the rat. Neurology. 1989;39:1396–1398. doi: 10.1212/wnl.39.10.1396. [DOI] [PubMed] [Google Scholar]
- 12.Clemens JA, Stephenson DT, Smalstig EB, Dixon EP, Little SP. Global ischemia activates nuclear factor-kappa B in forebrain neurons of rats. Stroke. 1997;28:1073–1081. doi: 10.1161/01.str.28.5.1073. [DOI] [PubMed] [Google Scholar]
- 13.Dignam JD, Lebovitz RM, Roeder RG. Accurate transcription initiation by RNA polymerase II in a soluble extract from isolated mammalian nuclei. Nucleic Acids Res. 1983;11:1475–1489. doi: 10.1093/nar/11.5.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gabriel C, Justicia C, Camins A, Planas AM. Activation of nuclear factor-kappa B in the rat brain after transient focal ischemia. Brain Res Mol Brain Res. 1999;65:61–69. doi: 10.1016/s0169-328x(98)00330-1. [DOI] [PubMed] [Google Scholar]
- 15.Gidday JM, Fitzgibbons JC, Shah AR, Park TS. Neuroprotection from ischemic brain injury by hypoxic preconditioning in the neonatal rat. Neurosci Lett. 1994;168:221–224. doi: 10.1016/0304-3940(94)90455-3. [DOI] [PubMed] [Google Scholar]
- 16.Glazier SS, O'Rourke DM, Graham DI, Welsh FA. Induction of ischemic tolerance following brief focal ischemia in rat brain. J Cereb Blood Flow Metab. 1994;14:545–553. doi: 10.1038/jcbfm.1994.68. [DOI] [PubMed] [Google Scholar]
- 17.Goodman Y, Mattson MP. Ceramide protects hippocampal neurons against excitotoxic and oxidative insults, and amyloid beta-peptide toxicity. J Neurochem. 1996;66:869–872. doi: 10.1046/j.1471-4159.1996.66020869.x. [DOI] [PubMed] [Google Scholar]
- 18.Grilli M, Pizzi M, Memo M, Spano P. Neuroprotection by aspirin and sodium salicylate through blockade of NF-kappa B activation. Science. 1996;274:1383–1385. doi: 10.1126/science.274.5291.1383. [DOI] [PubMed] [Google Scholar]
- 19.Guerrini L, Blasi F, Denis-Donini S. Synaptic activation of NF-kappa B by glutamate in cerebellar granule neurons in vitro. Proc Natl Acad Sci USA. 1995;92:9077–9081. doi: 10.1073/pnas.92.20.9077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haskill S, Beg AA, Tompkins SM, Morris JS, Yurochko AD, Sampson-Johannes A, Mondal K, Ralph P, Baldwin AS. Characterization of an immediate-early gene induced in adherent monocytes that encodes Iκβ-like activity. Cell. 1991;65:1281–1289. doi: 10.1016/0092-8674(91)90022-q. [DOI] [PubMed] [Google Scholar]
- 21.Heurteaux C, Lauritzen I, Widmann C, Lazdunski M. Essential role of adenosine, adenosine A1 receptors and KATP channels in cerebral ischemic preconditioning. Proc Natl Acad Sci USA. 1995;92:4666–4670. doi: 10.1073/pnas.92.10.4666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hunot S, Brugg B, Ricard D, Michel PP, Muriel MP, Ruberg M, Faucheux BA, Agid Y, Hirsch EC. Nuclear translocation of NF-kappa B is increased in dopaminergic neurons of patients with Parkinson disease. Proc Natl Acad Sci USA. 1997;94:7531–7536. doi: 10.1073/pnas.94.14.7531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaltschmidt B, Uherek M, Volk B, Baeuerle PA, Kaltschmidt C. Transcription factor NF-kappa B is activated in primary neurons by amyloid beta peptides and in neurons surrounding early plaques from patients with Alzheimer disease. Proc Natl Acad Sci USA. 1997;94:2642–2647. doi: 10.1073/pnas.94.6.2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaltschmidt C, Kaltschmidt B, Baeuerle PA. Stimulation of ionotropic glutamate receptors activates transcription factor NF-kappa B in primary neurons. Proc Natl Acad Sci USA. 1995;92:9618–9622. doi: 10.1073/pnas.92.21.9618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kawahara N, Reutzler CA, Klatzo I. A delayed effect of spreading depression on brain tissue associated with protection against ischemic neuronal damage. Brain Pathol [Suppl] 1994;4:5098. [Google Scholar]
- 26.Kelly ME, McIntyre DC. Hippocampal kindling protects several structures from the neuronal damage from kainic acid-induced status epilepticus. Brain Res. 1994;634:245–256. doi: 10.1016/0006-8993(94)91927-5. [DOI] [PubMed] [Google Scholar]
- 27.Kirino T. Delayed neuronal death in the gerbil hippocampus following ischemia. Brain Res. 1982;239:57–69. doi: 10.1016/0006-8993(82)90833-2. [DOI] [PubMed] [Google Scholar]
- 28.Kirino T, Tsujita Y, Tamura A. Induced tolerance to ischemia in gerbil hippocampal neurons. J Cereb Blood Flow Metab. 1991;11:299–307. doi: 10.1038/jcbfm.1991.62. [DOI] [PubMed] [Google Scholar]
- 29.Kitagawa K, Matsumoto M, Tagaya M, Hata R, Ueda H, Niinobe M, Handa N, Fukunaga R, Kimura K, Mikoshiba K, Kamada T. “Ischemic tolerance” phenomenon found in the brain. Brain Res. 1990;528:21–24. doi: 10.1016/0006-8993(90)90189-i. [DOI] [PubMed] [Google Scholar]
- 30.Kitagawa K, Matsumoto M, Kuwabara K, Tagaya M, Ohtsuki T, Hata R, Ueda H, Handa N, Kimura K, Kamada T. “Ischemic tolerance” phenomenon detected in various brain regions. Brain Res. 1991a;561:203–211. doi: 10.1016/0006-8993(91)91596-s. [DOI] [PubMed] [Google Scholar]
- 31.Kitagawa K, Matsumoto M, Tagaya M, Kuwabara K, Hata R, Handa N, Fukunaga R, Kimura K, Kamada T. Hyperthermia-induced neuronal protection against ischemic injury in gerbils. J Cereb Blood Flow Metab. 1991b;11:449–452. doi: 10.1038/jcbfm.1991.86. [DOI] [PubMed] [Google Scholar]
- 32.Kopp E, Ghosh S. Inhibition of NF-kappa B by sodium salicylate and aspirin. Science. 1994;265:956–959. doi: 10.1126/science.8052854. [DOI] [PubMed] [Google Scholar]
- 33.Liu Y, Kato H, Nakata N, Kogure K. Protection of rat hippocampus against ischemic neuronal damage by pretreatment with sublethal ischemia. Brain Res. 1992;586:121–124. doi: 10.1016/0006-8993(92)91380-w. [DOI] [PubMed] [Google Scholar]
- 34.Liu Y, Kato H, Nakata N, Kogure K. Temporal profile of heat shock protein 70 synthesis in ischemic tolerance induced by preconditioning ischemia in rat hippocampus. Neuroscience. 1993;56:921–927. doi: 10.1016/0306-4522(93)90138-6. [DOI] [PubMed] [Google Scholar]
- 35.Lothman EW, Collins RC. Kainic acid induced limbic seizures: metabolic, behavioral, electroencephalographic and neuropathological correlates. Brain Res. 1981;218:299–318. doi: 10.1016/0006-8993(81)91308-1. [DOI] [PubMed] [Google Scholar]
- 36.Lukiw WJ, Bazan NG. Strong nuclear factor-kappa B-DNA binding parallels cyclooxygenase-2 gene transcription in aging and in sporadic Alzheimer's disease superior temporal lobe neocortex. J Neurosci Res. 1998;53:583–592. doi: 10.1002/(SICI)1097-4547(19980901)53:5<583::AID-JNR8>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 37.Maggirwar SB, Sarmiere PD, Dewhurst S, Freeman RS. Nerve growth factor-dependent activation of NF-kappa B contributes to survival of sympathetic neurons. J Neurosci. 1998;18:10356–10365. doi: 10.1523/JNEUROSCI.18-24-10356.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matsushima K, Hakim AM. Transient forebrain ischemia protects against subsequent focal cerebral ischemia without changing cerebral perfusion. Stroke. 1995;26:1047–1052. doi: 10.1161/01.str.26.6.1047. [DOI] [PubMed] [Google Scholar]
- 39.Matsushima K, Hogan MJ, Hakim AM. Cortical spreading depression protects against subsequent focal cerebral ischemia in rats. J Cereb Blood Flow Metab. 1996;16:221–226. doi: 10.1097/00004647-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Mattson MP, Goodman Y, Luo H, Fu W, Furukawa K. Activation of NF-kappa B protects hippocampal neurons against oxidative stress-induced apoptosis: evidence for induction of manganese superoxide dismutase and suppression of peroxynitrite production and protein tyrosine nitration. J Neurosci Res. 1997;49:681–697. doi: 10.1002/(SICI)1097-4547(19970915)49:6<681::AID-JNR3>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 41.Mattson MP, Culmsee C, Yu Z, Camandola S. Roles of nuclear factor kappa B in neuronal survival and plasticity. J Neurochem. 2000;74:443–456. doi: 10.1046/j.1471-4159.2000.740443.x. [DOI] [PubMed] [Google Scholar]
- 42.Millar CGM, Baxter GF, Thiemermann C. Protection of the myocardium by ischaemic preconditioning: mechanisms and therapeutic implications. Pharmacol Ther. 1996;69:143–151. doi: 10.1016/0163-7258(95)02055-1. [DOI] [PubMed] [Google Scholar]
- 43.Nishi S, Taki W, Uemura Y, Higashi T, Kikuchi H, Kudoh H, Satoh M, Nagata K. Ischemic tolerance due to the induction of HSP70 in a rat ischemic recirculation model. Brain Res. 1993;615:281–288. doi: 10.1016/0006-8993(93)90039-p. [DOI] [PubMed] [Google Scholar]
- 44.Ohtsuki T, Matsumoto M, Kuwabara K, Kitagawa K, Suzuki K, Taniguchi N, Kamada T. Influence of oxidative stress on induced tolerance to ischemia in gerbil hippocampal neurons. Brain Res. 1992;599:246–252. doi: 10.1016/0006-8993(92)90398-s. [DOI] [PubMed] [Google Scholar]
- 45.Paxinos G, Watson C. The rat brain in stereotaxic coordinates. Academic; San Diego: 1986. [DOI] [PubMed] [Google Scholar]
- 46.Perez-Pinzon MA, Mumford PL, Rosenthal M, Sick TJ. Anoxic preconditioning in hippocampal slices: role of adenosine. Neuroscience. 1996;75:687–694. doi: 10.1016/0306-4522(96)00311-9. [DOI] [PubMed] [Google Scholar]
- 47.Perez-Pinzon MA, Xu GP, Dietrich WD, Rosenthal M, Sick TJ. Rapid preconditioning protects rats against ischemic neuronal damage after 3 but not 7 days of reperfusion following global cerebral ischemia. J Cereb Blood Flow Metab. 1997;17:175–182. doi: 10.1097/00004647-199702000-00007. [DOI] [PubMed] [Google Scholar]
- 48.Plamondon H, Blondeau N, Heurteaux C, Lazdunski M. Mutually protective actions of kainic acid epileptic preconditioning and sublethal global ischemia on hippocampal neuronal death: involvement of adenosine A1 receptors and KATP channels. J Cereb Blood Flow Metab. 1999;19:1296–1308. doi: 10.1097/00004647-199912000-00002. [DOI] [PubMed] [Google Scholar]
- 49.Pulsinelli WA, Brierley JB. A new model of bilateral hemispheric ischemia in the unanesthetized rat. Stroke. 1979;10:267–272. doi: 10.1161/01.str.10.3.267. [DOI] [PubMed] [Google Scholar]
- 50.Rauca C, Zerbe R, Jantze H, Krug M. The importance of free hydroxyl radicals to hypoxia preconditioning. Brain Res. 2000;868:147–149. doi: 10.1016/s0006-8993(00)02388-x. [DOI] [PubMed] [Google Scholar]
- 51.Reshef A, Sperling O, Zoref-Shani E. Adenosine-induced preconditioning of rat neuronal cultures against ischemia-reperfusion injury. Adv Exp Med Biol. 1998a;431:365–368. doi: 10.1007/978-1-4615-5381-6_72. [DOI] [PubMed] [Google Scholar]
- 52.Reshef A, Sperling O, Zoref-Shani E. Opening of ATP-sensitive potassium channels by cromakalim confers tolerance against chemical ischemia in rat neuronal cultures. Neurosci Lett. 1998b;250:111–114. doi: 10.1016/s0304-3940(98)00458-3. [DOI] [PubMed] [Google Scholar]
- 53.Riepe MW, Esclaire F, Kasischke K, Schreiber S, Nakase H, Kempski O, Ludolph AC, Dirnagl U, Hugon J. Increased hypoxic tolerance by chemical inhibition of oxidative phosphorylation: “chemical preconditioning.”. J Cereb Blood Flow Metab. 1997;17:257–264. doi: 10.1097/00004647-199703000-00002. [DOI] [PubMed] [Google Scholar]
- 54.Rong Y, Baudry M. Seizure activity results in a rapid induction of nuclear factor-kappa B in adult but not juvenile rat limbic structures. J Neurochem. 1996;67:662–668. doi: 10.1046/j.1471-4159.1996.67020662.x. [DOI] [PubMed] [Google Scholar]
- 55.Sasahira M, Lowry T, Simon RP, Greenberg DA. Epileptic tolerance: previous seizures protect against seizure-induced neuronal injury. Neurosci Lett. 1995;185:95–98. doi: 10.1016/0304-3940(94)11233-9. [DOI] [PubMed] [Google Scholar]
- 56.Scheinman RI, Cogswell PC, Lofquist AK, Baldwin AS., Jr Role of transcriptional activation of I kappa B alpha in mediation of immunosuppression by glucocorticoids. Science. 1995;270:283–286. doi: 10.1126/science.270.5234.283. [DOI] [PubMed] [Google Scholar]
- 57.Schreck R, Meier B, Mannel DN, Droge W, Baeuerle PA. Dithiocarbamates as potent inhibitors of nuclear factor kappa B activation in intact cells. J Exp Med. 1992;175:1181–1194. doi: 10.1084/jem.175.5.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Scott ML, Fujita T, Liou HC, Nolan GP, Baltimore D. The p65 subunit of NF-kappa B regulates I kappa B by two distinct mechanisms. Genes Dev. 1993;7:1266–1276. doi: 10.1101/gad.7.7a.1266. [DOI] [PubMed] [Google Scholar]
- 59.Sherman MP, Aeberhard EE, Wong VZ, Griscavage JM, Ignarro LJ. Pyrrolidine dithiocarbamate inhibits induction of nitric oxide synthase activity in rat alveolar macrophages. Biochem Biophys Res Commun. 1993;191:1301–1308. doi: 10.1006/bbrc.1993.1359. [DOI] [PubMed] [Google Scholar]
- 60.Shimazaki K, Ishida A, Kawai N. Increase in bcl-2 oncoprotein and the tolerance to ischemia-induced neuronal death in the gerbil hippocampus. Neurosci Res. 1994;20:95–99. doi: 10.1016/0168-0102(94)90026-4. [DOI] [PubMed] [Google Scholar]
- 61.Simon RP, Niiro M, Gwinn R. Prior ischemic stress protects against experimental stroke. Neurosci Lett. 1993;163:135–137. doi: 10.1016/0304-3940(93)90364-q. [DOI] [PubMed] [Google Scholar]
- 62.Smith-Swintosky VL, Pettigrew LC, Craddock SD, Culwell AR, Rydel RE, Mattson MP. Secreted forms of beta-amyloid precursor protein protect against ischemic brain injury. J Neurochem. 1994;63:781–784. doi: 10.1046/j.1471-4159.1994.63020781.x. [DOI] [PubMed] [Google Scholar]
- 63.Sun SC, Ganchi PA, Ballard DW, Greene WC. NF-kappa B controls expression of inhibitor I kappa B alpha: evidence for an inducible autoregulatory pathway. Science. 1993;259:1912–1915. doi: 10.1126/science.8096091. [DOI] [PubMed] [Google Scholar]
- 64.Taglialatela G, Robinson R, Perez-Polo JR. Inhibition of nuclear factor kappa B (NFkappa B) activity induces nerve growth factor-resistant apoptosis in PC12 cells. J Neurosci Res. 1997;47:155–162. [PubMed] [Google Scholar]
- 65.Toyoda T, Kassell NF, Lee KS. Induction of ischemic tolerance and antioxidant activity by brief focal ischemia. NeuroReport. 1997;8:847–851. doi: 10.1097/00001756-199703030-00008. [DOI] [PubMed] [Google Scholar]
- 66.Verma IM, Stevenson JK, Schwarz EM, Van Antwerp D, Miyamoto S. Rel/NF-kappa B/I kappa B family: intimate tales of association and dissociation. Genes Dev. 1995;9:2723–2735. doi: 10.1101/gad.9.22.2723. [DOI] [PubMed] [Google Scholar]
- 67.Xuan YT, Tang XL, Banerjee S, Takano H, Li RC, Han H, Qiu Y, Li JJ, Bolli R. Nuclear factor-kappa B plays an essential role in the late phase of ischemic preconditioning in conscious rabbits. Circ Res. 1999;84:1095–1109. doi: 10.1161/01.res.84.9.1095. [DOI] [PubMed] [Google Scholar]
- 68.Yu Z, Zhou D, Bruce-Keller AJ, Kindy MS, Mattson MP. Lack of the p50-subunit of nuclear factor-kappa B increases the vulnerability of hippocampal neurons to excitotoxic injury. J Neurosci. 1999;19:8856–8865. doi: 10.1523/JNEUROSCI.19-20-08856.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ziegler-Heitbrock HW, Sternsdorf T, Liese J, Belohradsky B, Weber C, Wedel A, Schreck R, Bauerle P, Strobel M. Pyrrolidine dithiocarbamate inhibits NF-kappa B mobilization and TNF production in human monocytes. J Immunol. 1993;151:6986–6993. [PubMed] [Google Scholar]