Abstract
Background:
The United Nations has declared the Syrian crisis as the worst humanitarian crisis of the twenty-first century. Pharmacists play a vital role in humanitarian aid and in delivering health advices for refugees. Many Syrian refugees are in need of psychosocial assessments.
Objective:
Objective of this study was to investigate the prevalence of post-traumatic stress disorder (PTSD), assessed by pharmacists among Syrian civilian refugees residing in Amman, Jordan.
Methods:
A cross-sectional study involving Syrian civilian refugees living in Amman, Jordan, was conducted using the published and validated Arabic version of the Harvard Trauma Questionnaire (HTQ). Pharmacists recruited civilian Syrian refugees and completed the HTQ. The questionnaire included 45 questions, with the first 16 questions (HTQ-16) intended to assess the trauma symptoms felt by refugees. Assessments were done by the pharmacists and refugees were categorized to suffer PTSD if their mean item score for the HTQ-16 scale was > 2.5.
Results:
Study participants (n=186; mean age 31.5 years; 51.3% males) had a HTQ-16 mean score of 2.35 (SD=0.53), with a range of 1.19 - 3.63. Over a third of participants (38.7%) were categorized as having PTSD. Males reported significantly worse PTSD symptoms (mean=2.42, SD=0.50) compared to females (mean=2.26, SD=0.57). Correlation between the mean item score for the HTQ-16 and characteristics of the study participants showed higher mean item score correlated with being a male, older in age, a smoker, and if trauma was experienced.
Conclusions:
Many Syrian civilian refugees living in Jordan suffer from PTSD. Male participants were found to be more affected by the severity of the disorder. Pharmacists are suitably situated to identify civilian Syrian refugees suffering from PTSD in dire need of help, paving the way for much needed healthcare resources to be delivered to this particular group of refugees.
Keywords: Pharmacists, Stress Disorders, Post-Traumatic, Stress, Psychological, Refugees, Altruism, Surveys and Questionnaires, Jordan, Syria
INTRODUCTION
According to the latest UN Refugee Agency’s annual Global Trends report, 68.5 million people across the world are forced out of their homeland.1 Escaping conflict and persecution led 25.4 million refugees to flee their countries, and it is developing countries that are most affected.1
The civil war in Syria, which started in March 2011, continues to account for the largest forcibly displaced population globally. As of the end of 2017, there were 12.6 million forcibly displaced Syrians, comprising around 6.3 million refugees, 146,700 asylum-seekers, and 6.2 million internally displaced people.1 The United Nations declared the Syrian crisis “the worst humanitarian crisis of the twenty-first century”; and as of September 2017, according to the latest statistics of UNHCR, there were 661,859 registered refugees in Jordan, of which 182,011 (27.5%) lived in the capital Amman.2
The 1951 Refugee Convention is a key legal document and defines a refugee as “someone who is unable or unwilling to return to their country of origin owing to a well-founded fear of being persecuted for reasons of race, religion, nationality, membership of a particular social group, or political opinion”.3 Refugees commonly experience physical and emotional traumas that predispose them to psychological disturbances prior to, and following resettlement.3,4 International studies show that refugees suffer from increased rates of short-term and long-term mental health problems.5-7 These studies have investigated the general effects of war and living life as a refugee, and shed light on mental health consequences claimed to affect refugees and their descendants for many years. Refugees commonly suffer from severe psychological distress, and many of them suffer from serious psychiatric and trauma-related problems.8 Post-traumatic stress disorder (PTSD) is the most common consequence of violence or life as a refugee.9 It has been defined as at least one month of recurrent, painful experiencing of a traumatic event, emotional numbing, or hyper-arousal, and avoidance of trauma-related memories.9 Approximately one out of three refugees suffers from PTSD or other trauma-related mental disorders.9-12
Services to which refugees have access following resettlement ideally should provide psychological, educational, financial, health, and social support for refugees. Such services need to provide integrated care and flexibility in responding to the diverse needs of heterogeneous refugee groups, in ways that align with their cultural beliefs and norms. In particular, the importance of developing culturally appropriate mental health services delivering psychosocial interventions for such marginalized populations has been highlighted in previous studies.13-15 Findings stated that working with individuals who are of refugee status presents healthcare professionals with challenges that distinguish refugees’ mental health needs from those of other populations. Such mental health services should aim to reduce the symptoms of psychological trauma and enhance the quality of refugees’ psychological and social wellbeing.16,17
Pharmacists play a vital role in humanitarian aid and in delivering health advice to refugees.18,19 Pharmacists are readily available and have a firm relationship with people in crises, hence can provide psychological and social needed support.20 Pharmacists working within a team of healthcare providers can deliver services for refugees with the potential to bridge the gap between differing healthcare professionals’ expertise.21
Many Syrian refugees were found to be in need of help and psychosocial assessments.22 However, studies investigating the effect of PTSD on Syrian refugees are scant, and little is known about the prevalence of this problem and its correlates. In light of this unique set of challenges, there is a need for current information on the mental health status of refugees, particularly the displaced Syrian refugees in Jordan.
The aim of this study was to investigate the prevalence, severity and factors associated with PTSD in the Syrian refugee population in Jordan, using a different approach to accessing this community through pharmacists working in Amman, Jordan.
METHODS
Study design and setting
A cross-sectional design was used. A convenience sample of Syrian refugees who reside in Amman, Jordan was approached. Inclusion criteria included: participants over 18 years of age, holding the Syrian nationality, officially of refugee status and willing to provide written informed consent. The exclusion criteria were: participants already diagnosed with a mental illness and/ or major psychiatric illness (such as dementia and depression); those with a history of taking psychotropic agents; and participants having major hearing or visual difficulties). Syrian refugees identified as living in selected areas in Amman (areas high in Syrian residents) were approached. In affluent socioeconomic areas, where refugees resided amongst the Jordanian locals, refugees were approached and recruited through universities (students) and workplaces. And, in lower-socioeconomic areas, Syrian refugees, who resided in designated areas and buildings, were also invited to participate when it was most appropriate for the researcher to approach them.
Ethics approval was obtained from the Faculty of Pharmacy, Applied Science Private University Ethics Committee and from the Jordanian Ministry of Health. Data collection occurred between January and October, 2014.
Those who agreed to participate in the study and provided written informed consent, were informed that the information they provided would help to offer them better care and would not affect their treatment programs, and that they may find some of the questions discomforting or embarrassing, in which case they were free not to answer, and if they did answer; their responses to the questions would be kept confidential if so requested. All transcripts were de-identified by giving each a code to ensure confidentiality.
Face-to-face interviews using a structured questionnaire based on the objectives of the study were utilized to collect the data. These interviews were conducted by three trained pharmacists who attended a 2-day training program concerning the study purpose, questionnaire, protocol, and strategies for conducting interviews.
A pilot study with 15 participants was conducted with the attendance of one of the principal researchers to assure uniformity in interviewing skills among the three pharmacists. No changes to the questionnaires were made after the pilot study. The principal researcher consulted a psychologist about what to do in case serious cases of PTSD were identified.
Instrument
The Arabic version of the Harvard Trauma Questionnaire (HTQ) was used in this study, derived from the Diagnostic and Statistical Manual of Mental Disorder Text Revision (DSM-IV TR) published by the American Psychology Association (APA, 1987, 1994), to assess the trauma symptoms felt by refugees who had experienced painful or horrific events in their lives.23-25 The HTQ consists of four parts, of which Part 1 (42 questions) explores trauma events and Part IV (45 questions) explores trauma symptoms. This version was validated among Iraqi refugees in the United State by Shoeb, Weinstein, and Mollica in 2007.26
To answer the aim of this study, a three-section questionnaire was used to collect data; Section 1 included information related to socio-demographic characteristics (i.e. age, gender, occupation, and educational level), personal characteristics (i.e. residential status (high/ low socioeconomic), smoking, medical history) and trauma-related questions (i.e. experience of trauma, cause of the trauma).
Section 2 included nine closed questions selected from Part 1 of the HTQ.23 These nine questions were related to the trauma events experienced by the refugees. Participants were instructed to answer them with ‘yes’ or ‘no’ with reference to their past suffering and symptoms.
Section 3 included all questions found in the Part IV of the HTQ.23 The first 16 questions (HTQ-16) of this version assess the trauma symptoms felt by refugees who had experienced painful or horrific events in their lives. The items represent the criteria for the intrusion/ re-experiencing, avoidance/ numbing, and hypervigilance/ arousal symptom clusters (i.e. “Recurrent thoughts/ memories” and “hard to concentrate”). The next set of PTSD symptom items were culture-specific items. Each item was assessed using a level of agreement with four possible categories of responses ranging from: ‘1’ = “Not at all”, to ‘4’ = ‘extremely’.
The mean item score is obtained by summing the individual item scores and then dividing by the number of items, yielding a mean item score for the scale. The cut-off scores proposed by Mollica and colleagues (2004) was used and the standard cut-off score of 2.5 on the Harvard Trauma indicated probable PTSD.26
Scoring the trauma symptoms part of the HTQ Section IV was planned to take between 5 to 10 minutes, which included calculating the mean item score for the first HTQ-16, and the full symptom scale (HTQ-45).
Data analysis
Descriptive statistics were calculated for the demographics of the sample (age, gender, education, marital status, residential status) and for their health characteristics (smoking, trauma experiences and exposure to TV). Categorical variables (such as gender) were presented as percentages and number of cases. The mean and standard deviation (SD) were calculated for quantitative variables. Statistical comparisons between different groups were carried out by using Chi square test and independent t-test; p values ≤0.05 were considered significant. Relationships between the mean item score for the HTQ-16 and the full symptom scale among Syrian refugees and their characteristics were examined using Pearson’s correlation coefficient for continuous variables; Epsilon squared, and Glass rank bi-serial for categorical variables. In order to determine associations of PTSD for the refugees, a binary logistic regression analysis was performed. The dependent variable was refugees having been symptomatic of PTSD (having HTQ-16 and the full symptom scale mean score of >2.5 or not). Variables included in the model were: age, gender, educational level, marital status, residential status, smoking, watching TV, experienced a trauma and the kind of trauma.
RESULTS
A total sample of 186 participants completed the questionnaire. The mean age of participants was 32.65 years (SD=13.90), and 53.2% of study participants were males. Half the participants (50.0%) reported having a bachelor’s degree level of education and 44.0% of them were married. Regardless of the type of trauma, 88.2% of the participants reported having suffered trauma. Most patients (86.5%) reported TV watching. Table 1 presents information on these characteristics.
Table 1. Socio-demographic and clinical characteristics of the study participants according to the scores on HTQ-16 and the full symptom scale* (n= 186).
| Characteristics n (%) | Asymptomatic PTSD | Symptomatic PTSD | Total | Test statistics |
|---|---|---|---|---|
| Age (Years) | chi-square=8.96 p < 0.01 | |||
| Youth (18-24) | 55 (21.0) | 21 (79.0) | 76 (41.0) | |
| Adult (25- 64) | 60 (56.6) | 46 (43.4) | 106 (57.0) | |
| Senior (≥ 65) | 3 (75.0) | 1 (25.0) | 4 (2.00) | |
| Gender | chi-square=0.304 p= 0.58 | |||
| Females | 57 (65.5) | 30 (34.5) | 87 (46.8) | |
| Males | 61 (61.6) | 38 (38.4) | 99 (53.2) | |
| Education | chi-square=12.92 p = 0.012 | |||
| Not educated | 17(85.0) | 3(15.0) | 20 (10.8) | |
| Elementary or less | 14 (43.7) | 18 (56.3) | 32 (17.2) | |
| Secondary | 21 (55.3) | 17 (44.7) | 38 (20.0) | |
| Bachelor’s degree | 63 (76.8) | 30 (32.2) | 93 (50.0) | |
| Postgraduate degree | 0 (0.00) | 3 (100.0) | 3 (1.0) | |
| Marital status | chi-square=7.57 p = 0.56 | |||
| Single | 28 (34.1) | 54 (65.9) | 82 (44.0) | |
| Married | 31 (76.8) | 51 (76.8) | 82 (44.0) | |
| Divorced/ Widowed | 15 (0.00) | 8 (0.00) | 23 (12.0) | |
| Residential status | chi-square=0.051 p = 0.82 | |||
| Urban | 45 (36.0) | 80 (64.0) | 125 (67.2) | |
| Rural | 23 (37.7) | 38 (62.3) | 61 (32.8) | |
| Smoking status | chi-square=12.0 p = 0.002 | |||
| Yes | 28 (58.3) | 20 (41.7) | 48 (25.8) | |
| Ex-smoker | 2 (18.2) | 9 (81.8) | 11 (5.9) | |
| Never | 38 (30.0) | 89 (70.0) | 127 (68.3) | |
| Medical history | chi-square=3.57 p = 0.059 | |||
| No | 68 (37.8) | 112 (62.2) | 180 (96.7) | |
| Yes | 0 (00.0) | 6 (100.0) | 6 (03.0) | |
| Experiencing trauma | chi-square=11.03 p = 0.001 | |||
| No | 1 (4.54) | 21 (95.45) | 22 (11.8) | |
| Yes | 67 (40.9) | 97 (59.1) | 164 (88.2) | |
| Kind of trauma | chi-square=0.180 p = 0.671 | |||
| Social | 2 (28.6) | 5 (71.4) | 7 (4.30) | |
| War | 95 (60.5) | 62 (39.5) | 157 (95.7) | |
| Watching TV | chi-square=0.420 p = 0.517 | |||
| No | 4 (16.0) | 21 (84.0) | 25 (13.4) | |
| Yes | 60 (37.3) | 101 (62.7) | 161 (86.5) |
Total scores >2.5 in HTQ-16 and the full symptom scale were considered symptomatic of PTSD
Completing the trauma symptoms part of the HTQ (HTQ-45) with the refugees took from 3.45 to 7.0 minutes. The mean item score for the HTQ-16 was 2.35 (SD=0.53) with a range of 1.19 - 3.63, and 38.7% categorized to have PTSD (mean item score for the HTQ-16 and the full symptom scale >2.5). Independent t-tests were performed to assess if the mean item score for the HTQ-16 and the full symptom scale differed significantly for female compared with male participants. The analysis revealed that the mean item score for the HTQ-16 differed significantly, t (184) = -2.161, p=0.032. Overall, females were found to experience less PTSD than males (HTQ-16 mean item score for females= 2.26, SD=0.57 and males=2.42, SD=0.50).
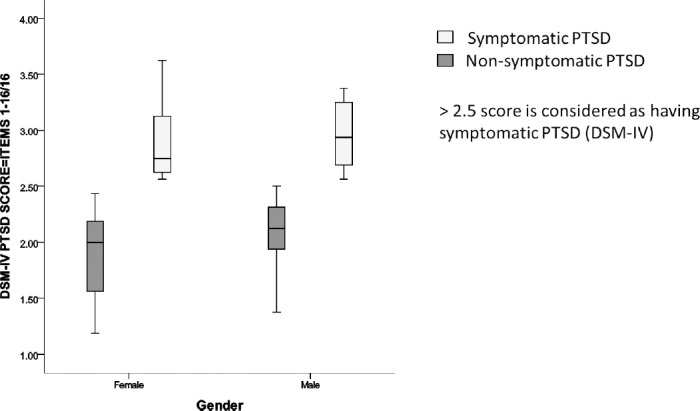
Regarding the full symptom scale, the mean item score for the HTQ-45 was 2.33 (SD=0.47; range 1.1 - 3.24), and 31.2 % were categorized to have PTSD (mean item score for the full symptom scale >2.5). Median scores and IQR for the mean item score for the HTQ-16 and full symptom scale based on gender are presented in Figure 1 and Figure 2, respectively.
Figure 1. Proportion of respondents (n= 186) with symptomatic versus non-symptomatic post traumatic stress disorder (the mean item score for the HTQ-16) showing gender differences.
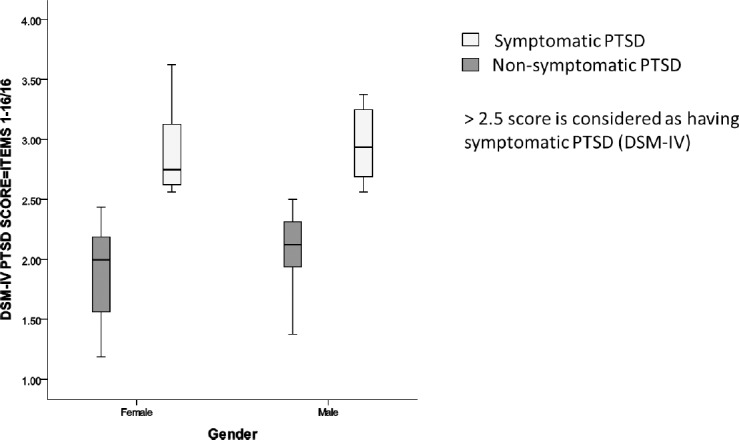
Figure 2. Proportion of respondents (n= 186) with symptomatic versus non-symptomatic post traumatic stress disorder (the mean item score for the HTQ-16) showing gender differences.
Trauma assessment involving the nine trauma assessment questions (Section 2) was performed based on gender-specific differences (Table 2). The analysis showed more than 50% of participants suffered ill-health without access to medical assistance whilst in Syria. However, compared to their residence in Jordan, only 24.0% of both genders reported to have had no access to medical assistance. Many participants reported having witnessed someone being physically harmed (e.g. beating and knifing), however significantly more males (36.4%) experienced torture. Comparisons based on gender for the rest of the questions are presented in Table 2.
Table 2. Proportion of participants answering ‘yes’ to each of the 9-trauma assessment questions in Part 2 of the Questionnaire (n = 186).
| Proportion of patients who answered with ‘yes’ | Female n= 87 | Male n= 99 | chi-square | p-value |
|---|---|---|---|---|
| 1.Have you suffered from ill health without access to medical care or medicine during your stay in your country?** | 43 (49.4) | 60 (60.8) | 2.34 | 0.126 |
| 2.Have you suffered ill health without access to medical care or medicine during your stay in Jordan? | 21 (24.1) | 24 (24.2) | 0.00 | 0.987 |
| 3.Have you seen massive execution of civilians?* | 21 (24.1) | 37 (37.3) | 3.78 | 0.052 |
| 4.Have you been exposed to combat situation (explosions, artillery fire, shelling) or landmine?** | 50 (57.5) | 61 (61.6) | 0.33 | 0.565 |
| 5.Have you got serious physical injury from combat situation or landmine?** | 32 (36.8) | 44 (44.4) | 1.23 | 0.289 |
| 6.Have you been\ witnessed someone being physically harmed (beating, knifing, etc.)? | 49 (56.6) | 58 (58.6) | 0.10 | 0.565 |
| 7.Have you witnessed sexual abuse or rape?** | 16 (18.3) | 25 (25.2) | 1.27 | 0.260 |
| 8.Have you been kidnapped/ taken as a hostage?** | 12 (13.8) | 19 (19.1) | 1.10 | 0.294 |
| 9.Have you been tortured (while in captivity have you received deliberate and systematic infliction of physical and/ or mental suffering)?** | 4 (4.5) | 36 (36.4) | 27.7 | <0.001 |
Significantly correlated with the scores on HTQ-16 and the full symptom scale (p< 0.05).
Significantly correlated with the scores on HTQ-16 and the full symptom scale (p< 0.001).
Table 3 presents the correlation between the mean item score for the HTQ-16, the full symptom scale and characteristics of the study participants. Participants were more likely to have higher mean item score if they were males, older, smokers, and experienced trauma. However, no significant correlations were found between depression categories and the remainder of patients’ characteristics, including watching TV.
Table 3. Correlations between mean item score for the HTQ-16, the full symptom scale and patients’ characteristics (n = 186).
| mean item score for the full symptom scale | mean item score for the HTQ-16 | |||
|---|---|---|---|---|
| r | p-value | r | p-value | |
| Age (years) | 0.349 | <0.001 | 0.273 | <0.001 |
| Gender (F=0, M=1) | 0.145 | 0.049 | 0.145 | 0 .049 |
| Educational level | -0.137 | 0.063 | -0.166 | 0.150 |
| Marital status (single= 1, married=2, widowed or divorced=3) | -0.107 | 0.155 | -0.115 | 0.124 |
| Residential status (rural=1, urban=2) | -0.037 | 0.616 | -0.036 | 0.612 |
| Smoker (0=smoker, 1=ex-smoker, 2=never) | 0.330 | <0.001 | 0.257 | <0.001 |
| Experienced a trauma (0= no, 1= yes) | 0.298 | <0.001 | 0.402 | <0.001 |
| Kind of trauma (0= war, 1=social, 3= economical, 4= others, 5= none) | -0.035 | 0.488 | -0.075 | 0.342 |
| Watching TV (no=1, yes=2) | 0.060 | 0.429 | 0.104 | 0.171 |
The model resulting from the binary logistic regression analysis explained between 12.3% (Cox and Snell R-square) and 18.6% (Nagelkerke R-square) of variance in whether participants had mean scores on HTQ-16 and the full symptom scale > 2.5, therefore classified to have PTSD. The variables ‘smoker’, and ‘experienced trauma’ made a unique statistically significant contribution to the model (chi-square (df 4)=25.05, p<0.001). Online appendix summarizes the raw score logistic regression coefficient, Wald statistics and the estimated odds ratio for symptomatic PTSD compared with asymptomatic along with 95%CI.
DISCUSSION
Refugees are vulnerable and share similar experiences regardless of the country they come from, or the culture they belong to.27,28 Several reports have mentioned that mental and social health problems (e.g. the inability to adapt comfortably to different social situations or to form satisfying interpersonal relationships with others) were the most common problems experienced amongst refugees.11,12 With the Syrian refugees currently constituting 20.0% of Jordan’s population, studies investigating their current state, needs and safe settlement in the country are urgently needed.29 Previous literature investigating the effect of trauma and the factors that contribute to PTSD were more focused on military personnel, despite the fact that larger numbers of refugees suffered from the problem.30 This current study sheds light on the prevalence and severity of PTSD in Syrian refugees in Jordan. Understanding the gender difference helps pave the way towards allocating appropriate services/resources for the management of the refugees’ health.
PTSD is a common psychiatric condition in primary care patients. In the general population, a national sample of 5877 people in the USA, aged 15 to 54 years, showed a 7.8% estimated lifetime prevalence of PTSD.31 However, among special populations, such as veterans of Iraq and Afghanistan wars, 58.2% of 238,098 veterans who received a health care service in the USA were diagnosed with PTSD.32 As for PTSD diagnosis among refugees, a report by the US Committee for Refugees demonstrated a wide variation in the prevalence of the symptoms of PTSD (4-86%).33 This study revealed the prevalence of PTSD amongst adult refugees in Jordan to be 35.0%. The identified proportion falls within the wide range of prevalence identified earlier, but is well below the upper ranges (86.0%).33 Immigration-related stressors such as language difficulties and cultural differences are not found in the Middle East region, which could have played a role in keeping that proportion at the lower rate. Moreover, religious beliefs and family ties in the Arabic region provide a network of healing, again, neutralizing some war effects and keeping PTSD proportion at the lower rate.33
Although exposure to war-related violence does not necessarily lead to PTSD, the incidence of PTSD has been known to increase in populations exposed to war.31 A study conducted in Canada in the year 2011 emphasized that the prevalence of common mental health problems increased for refugees who had severe exposure to previous violence, as they have higher rates of trauma-related disorders, including PTSD.34 Also, time does not seem to resolve the problem; individuals who have experienced great levels of trauma have a greater risk of developing psychological disorders long after resettlement.35 A study conducted in Netherlands showed an unchanged high prevalence of PTSD (16.3% in 2003 and 15.2% in 2010) amongst refugees, attributable in part to the late onset of PTSD symptoms and the low use of mental healthcare services.36
The World Health Organization (WHO) defined health in its broader sense in the 1948 constitution as “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity”.37 Fear of stigma, unawareness of mental illness, lack of appropriate services that suit people’s needs all form barriers to accessing mental healthcare, contributing to people not seeking treatment in time.38 It is important to note that people with PTSD are more than twice as likely to experience non-psychiatric medical conditions as those without PTSD, even when adjusting for other factors such as age, socioeconomic status, and major depression.39 In addition, mental health assessment is not easy, with certain factors preventing accurate assessment, including high patient volume, the presence of multiple family members within the room, and natural hesitancy to discuss extremely sensitive matters.40 Findings indicate that refugees would stand to benefit from long-term contact with mental health and social work teams, thus further interventional research in this area is called for.40
Many factors affect PTSD development and severity amongst refugees. It has been reported that psychological distress is exacerbated by both environmental conditions (financial stress, poor housing, lack of employment) and psychosocial outcomes (loss of role, poor social support and reduced activity), which are themselves stressors.41 Length of time following exposure to war and trauma could also play a role. A study in Jordan conducted in six different areas in the country, indicated that there are significant effects of gender, marital status and educational level on PTSD symptoms of Syrian refugees.27 Another study conducted in the northern part of Jordan showed that there are differences among the Syrian refugees in the extent and degree of PTSD; revealing that females, higher educated or married participants showed more symptoms of PTSD than males and females who were less educated or single.28
The significant association identified in this study between trauma and PTSD in symptomatic refugees is consistent with previous findings, where individuals with higher rates of trauma were shown to have correspondingly more severe mental health symptoms, including PTSD.42 Another factor associated with more severe PTSD symptoms was smoking. A study conducted in the USA in 2012 suggested that certain PTSD symptoms may uniquely be associated with particular indicators of smoking behavior.43,44
Longer hours of watching TV showed no association with PTSD, unlike many previous findings.45,46 A study conducted in Pakistan in 2009 showed high rate of PTSD symptoms by TV viewers, confirming the association between watching TV and PTSD.45 PTSD symptoms have also been related to the type of TV show watched by affected people. A study conducted in the USA revealed that three to five days following the 2001 September 11 attacks, people reported watching an average of eight hours of television a day related to the attacks. Those who watched the most coverage, and for 12 or more hours, had more substantial stress reactions and 3.4-fold increased risk of new-onset PTSD.46 On the other hand, it is likely that having access to a TV could be associated with being more settled and having a better income as a refugee, so watching TV for long hours may not really be a concern for Syrian refugees.
Results of this study showed a relatively high proportion of participants (60.8% males; 49.4% females) reporting having ill health without access to medical aid or medicines after the war during their stay in Syria, with the proportion decreasing significantly after their settlement in Jordan (24.2% males; 24.1% females). It is important to note here that refugee’s ill health usually differ from the host countries’ population health pattern, hence, healthcare professionals are advised to collaborate in investigating and improving healthcare among refugees.47 A study conducted on 756 Syrian refugees from six different cities in Jordan in 2016 examining the impact of chronic diseases and availability of medications for PTSD, showed that PTSD was comorbid with chronic diseases in more than half of the participants.48
Gender differences also play a role in manifestation of mental illnesses.39 This study pointed to gender as a contributing factor to the experience of PTSD; results appear to suggest that there is a variation in the prevalence rate of PTSD, with males having significantly worse PTSD symptoms than females. Males reporting greater trauma experiences in the Syrian conflict, such as seeing mass execution of civilians and being tortured whilst in captivity, could be linked to the higher reported PTSD levels. Exposure to torture has been shown to account for higher rates of reported prevalence of PTSD and depression.35 Interestingly our results differ from previous studies conducted in this area, where female Syrian refugees were found to suffer more PTSD symptoms than males.49 Another study reported that both genders involved in the Syrian conflict were equally affected by the war, as the rates of depression did not differ between both genders.50
Many studies have been conducted in the geographical area surrounding Syria, shedding light on the psychological impact of war on the Syrian refugees for adults, women and children.13,40,51 The need for psychological and mental health services was emphasized in all studies.
In addition, since many refugees have PTSD which often goes under-diagnosed because of the many competing priorities experienced by refugee communities, it would be valuable if refugees with PTSD could be identified more readily. Pharmacists can be engaged in this field, forming a link between refugees and mental health specialists. Pharmacists are accessible primary care providers for refugees in Jordan, ideally positioned to screen for refugees with PTSD, referring those in need of care to healthcare specialists. Pharmacists can perform this role through their presence in the community pharmacy, an accessible health care facility to the public, where pharmacists are available to provide personalized advice about health and medicine on a walk-in basis, without the need for a costly appointment.52 Pharmacists can also be engaged in new services targeting refugees, such as the successful, previously trialled, specialized medication management review service delivered to Syrian refugees in Jordan’.53 Most importantly, pharmacists need to be resourced to provide helpful information about services they could access and brief information about PTSD, clarifying how much their engagement is helpful. It took the pharmacists an average of 5 minutes to complete the survey with each refugee, indicating the feasibility of this assessment. Engaging pharmacists with refugees can create new and needed services that can be delivered by pharmacists not only in the Middle East, but wherever refugees reside. This is in line with the WHO recommendations supporting the implementation of the recently published report by the High-Level Commission on Health Employment and Economic Growth established by United Nations Secretary in March 2016 calling for “ambitious solutions to ensure that the world has the right number of jobs for health workers with the right skills and in the right places to deliver universal health coverage”.54,55
Limitations
Limitations of this study involved the sampling strategy, which was minimized as much as possible by having a clear stringent protocol followed by the investigators when interviewing the refugees. Although the study presents a unique approach to research in the Middle East, it is challenging to draw conclusive deductions for the recruited study sample, and generalization of the results are restricted to the refugees residing in Amman, Jordan. The in-person interview aspect of this study could have made some participants uncomfortable sharing their personal mental health. The pharmacists conducting the interviews in this study were of both genders. Female refugees could have been more open when a female pharmacist interviewed them versus a male pharmacist. Such gender differences of the pharmacist may have influenced the females comfort level when speaking about their mental health, which could have affected the results.
Although it would have been useful to extrapolate socioeconomic factors in the analysis by questioning the participants about their income, this question was left optional due to the refusal of many participants to respond to such questioning. The questionnaire (HTQ) used for the Syrian refugees (non-Western population) in this study to assess their mental health problems is an internationally validated questionnaire.24 The questionnaire was translated and validated in the Arabic language and was found useful when used across different cultures and populations.23,25,33 Yet, to adapt the HTQ to the Syrian refugee context for a better understanding of the situation, researchers can benefit from investigating the effects of trauma on the Middle Eastern populations in general, and on Syrians in particular.
CONCLUSIONS
Civilian Syrian refugees interviewed by pharmacists in Jordan showed a high incidence of PTSD. The prevalence rate of Syrian refugees in Jordan who report symptoms of PTSD on DSM-IV score was 35%. More males than females were found to be affected by the disorder. Many refugees have suffered different types of traumas, mainly exposure to combat situation and being or witnessing someone physically harmed. More males were tortured and witnessed massive execution of civilians than females. Having experienced previous trauma, being older in age, a smoker or a male showed significant association with PTSD severity. Results of this study highlight the ability of pharmacists to identify refugees with PTSD in need of dire help, directing needed resources to treat civilian refugees affected by PTSD. Further research exploring PTSD for refugee children residing in the countries surrounding Syria is needed. Longitudinal studies are called for, considering that individuals who have experienced great levels of trauma have a greater risk of developing psychological disorders years after resettlement.35 Future studies could also investigate if less intensive training with a shorter questionnaire could be enough for pharmacists to take on this role.
Data availability
The datasets generated during or analyzed during the current study are available from the corresponding author on reasonable request.
ACKNOWLEDGMENTS
The authors are grateful to the Applied Science Private University, Amman, Jordan, for the full financial support granted to this research project. The authors wish to thank the refugees who participated in this study; Doctor Mohammed Basheti and Aboud Foude for their valuable contribution in the study.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
FUNDING
This work was supported by the Applied Science Private University, Amman, Jordan [grant number: DRGS-2017-2018-7].
Contributor Information
Iman A. Basheti, Professor in Clinical Pharmacy. Department of Clinical Pharmacy, Faculty of Pharmacy, Applied Science Private University. Amman (Jordan). dr_iman@asu.edu.jo
Shahnaz M. Ayasrah, Department of Applied Science/Nursing, Al-Balqa Applied University a. Al-Salt (Jordan). shahnazhamdan@bau.edu.jo
Mariam M. Basheti, Faculty of Pharmacy, Jordan University of Science and Technology. Irbid (Jordan). mariabasheti@hotmail.com
Judeh Mahfuz, Professor in human resource management. Applied Science Private University. Amman (Jordan). mahfouz@asu.edu.jo.
Betty Chaar., Associate Professor in pharmacy practice. School of Pharmacy, Faculty of Medicine and Health, University of Sydney. Sydney, NSW a (Australia). betty.chaar@sydney.edu.au.
References
- 1. [accesed Feb 3 2019];Global Trends forced displacement in 2017. https://www.unhcr.org/5b27be547.pdf .
- 2. [accesed Sep 3 2018];United Nations population Fund regional situation report for the Syrian crisis. https://www.unfpa.org/sites/default/files/resource-pdf/UNFPA_Regional_Situation_Report_for_the_Syria_Crisis_-_Issue_72_-_August.pdf .
- 3.Robjant K, Fazel M. The emerging evidence for Narrative Exposure Therapy:a review. Clin Psychol Rev. 2010;30(8):1030–1039. doi: 10.1016/j.cpr.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Neuner F, Onyut PL, Ertl V, Odenwald M, Schauer E, Elbert T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement:a randomized controlled trial. J Consult Clin Psychol. 2008;76(4):686–694. doi: 10.1037/0022-006X.76.4.686. [DOI] [PubMed] [Google Scholar]
- 5.Porter M, Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons:a meta-analysis. JAMA. 2005;294(5):602–612. doi: 10.1001/jama.294.5.602. [DOI] [PubMed] [Google Scholar]
- 6.Schweitzer R, Melville F, Steel Z, Lacherez P. Trauma, post-migration living difficulties, and social support as predictors of psychological adjustment in resettled Sudanese refugees. Aust N Z J Psychiatry. 2006;40(2):179–187. doi: 10.1080/j.1440-1614.2006.01766.x. [DOI] [PubMed] [Google Scholar]
- 7.Laban CJ, Gernaat HB, Komproe IH, van der Tweel I, De Jong JT. Postmigration living problems and common psychiatric disorders in Iraqi asylum seekers in the Netherlands. J Nerv Ment Dis. 2005;193(12):825–832. doi: 10.1097/01.nmd.0000188977.44657.1d. [DOI] [PubMed] [Google Scholar]
- 8.Strijk PJ, van Meijel B, Gamel CJ. Health and social needs of traumatized refugees and asylum seekers:an exploratory study. Perspect Psychiatr Care. 2011;47(1):48–55. doi: 10.1111/j.1744-6163.2010.00270.x. [DOI] [PubMed] [Google Scholar]
- 9.Norredam M, Garcia-Lopez A, Keiding N, Krasnik A. Risk of mental disorders in refugees and native Danes:a register-based retrospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2009;44(12):1023–1029. doi: 10.1007/s00127-009-0024-6. [DOI] [PubMed] [Google Scholar]
- 10.Carta MG, Moro MF, Bass J. War traumas in the Mediterranean area. Int J Soc Psychiatry. 2015;61(1):33–38. doi: 10.1177/0020764014535754. [DOI] [PubMed] [Google Scholar]
- 11.Bogic M, Njoku A, Priebe S. Long-term mental health of war-refugees:a systematic literature review. BMC Int Health Hum Rights. 2015;15:15. doi: 10.1186/s12914-015-0064-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries:a systematic review. Lancet. 2005;365(9467):1309–1314. doi: 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- 13.Basheti IA, Qunaibi EA, Malas R. Psychological impact of life as refugees:a pilot study on a Syrian camp in Jordan. Trop J Pharm Res. 2014;14(9):1695–1701. doi: 10.4314/tjpr.v14i9.22. [DOI] [Google Scholar]
- 14.Redwood-Campbell L, Fowler N, Kaczorowski J, Molinaro E, Robinson S, Howard M, Jafarpour M. How are new refugees doing in Canada?Comparison of the health and settlement of the Kosovars and Czech Roma. Can J Public Health. 2003;94(5):381–385. doi: 10.1007/BF03403567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knaevelsrud C, Stammel N, Olff M. Traumatized refugees:identifying needs and facing challenges for mental health care. Eur J Psychotraumatol. 2017;8(sup 2):1388103. doi: 10.1080/20008198.2017.1388103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Newman L. Seeking asylum-trauma, mental health, and human rights:an Australian perspective. J Trauma Dissociation. 2013;14(2):213–223. doi: 10.1080/15299732.2013.724342. [DOI] [PubMed] [Google Scholar]
- 17.Weinstein N, Khabbaz F, Legate N. Enhancing need satisfaction to reduce psychological distress in Syrian refugees. J Consult Clin Psychol. 2016;84(7):645–650. doi: 10.1037/ccp0000095. [DOI] [PubMed] [Google Scholar]
- 18.Bussieres JF, St-Arnaud C, Schunck C, Lamarre D, Jouberton F. The role of the pharmacist in humanitarian aid in Bosnia-Herzegovina:the experience of Pharmaciens Sans Frontieres. Ann Pharmacother. 2000;34(1):112–118. doi: 10.1345/aph.19157. [DOI] [PubMed] [Google Scholar]
- 19.Kay M, Wijayanayaka S, Cook H, Hollingworth S. Understanding quality use of medicines in refugee communities in Australian primary care:a qualitative study. Br J Gen Pract. 2016;66(647):e397–e409. doi: 10.3399/bjgp16X685249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hassali MA, Dawood OT, AL-Tamimi SK, Saleem F. Role of Pharmacists in Health Based Non-Governmental Organizations (NGO):Prospects and Future Directions. Pharm Anal Acta. 2016;7(2):467–471. doi: 10.4172/2153-2435.1000467. [DOI] [Google Scholar]
- 21.Nies MA, Lim WY, Fanning K, Tavanier S. Importance of Interprofessional Healthcare for Vulnerable Refugee Populations. J Immigr Minor Health. 2016;18(5):941–943. doi: 10.1007/s10903-016-0424-0. [DOI] [PubMed] [Google Scholar]
- 22.El Chammay R, Ammar W. Syrian crisis and mental health system reform in Lebanon. Lancet. 2014;384(9942):494. doi: 10.1016/S0140-6736(14)61329-5. [DOI] [PubMed] [Google Scholar]
- 23.Kleijn WC, Hovens JE, Rodenburg JJ. Posttraumatic stress symptoms in refugees:assessments with the Harvard Trauma Questionnaire and the Hopkins symptom Checklist-25 in different languages. Psychol Rep. 2001;88(2):527–532. doi: 10.2466/pr0.2001.88.2.527. [DOI] [PubMed] [Google Scholar]
- 24.Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Ment Dis. 1992;180(2):111–116. [PubMed] [Google Scholar]
- 25.Rasmussen A, Verkuilen J, Ho E, Fan Y. Posttraumatic stress disorder among refugees:Measurement invariance of Harvard Trauma Questionnaire scores across global regions and response patterns. Psychol Assess. 2015;27(4):1160–1170. doi: 10.1037/pas0000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mollica RF, McDonald LS, Massagli MP, Silove DM. Measuring Trauma, Measuring Torture:Instructions and Guidance on the Utilization of the Harvard Program in Refugee Trauma's Versions of The Hopkins Symptom Checklist-25 (HSCL-25) &The Harvard Trauma Questionnaire (HTQ) Cambridge, MA: Harvard Program in Refugee Trauma; 2004. [Google Scholar]
- 27.El-Khatib Z, Scales D, Vearey J, Forsberg BC. Syrian refugees, between rocky crisis in Syria and hard inaccessibility to healthcare services in Lebanon and Jordan. Confl Health. 2013;7(1):18. doi: 10.1186/1752-1505-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eckstein B. Primary care for refugees. Am Fam Physician. 2011;83(4):429–436. [PubMed] [Google Scholar]
- 29.Murshidi MM. Syrian Refugees Constitute 20% of Jordan's Population. Am J Public Health. 2016;106(5):e18. doi: 10.2105/AJPH.2016.303117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Neuner F, Schauer M, Klaschik C, Karunakara U, Elbert T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an african refugee settlement. J Consult Clin Psychol. 2004;72(4):579–587. doi: 10.1037/0022-006X.72.4.579. [DOI] [PubMed] [Google Scholar]
- 31.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 32.Seal KH, Maguen S, Cohen B, Gima KS, Metzler TJ, Ren L, Bertenthal D, Marmar CR. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. J Trauma Stress. 2010;23(1):5–16. doi: 10.1002/jts.20493. [DOI] [PubMed] [Google Scholar]
- 33.Shoeb M, Weinstein H, Mollica R. The Harvard trauma questionnaire:adapting a cross-cultural instrument for measuring torture, trauma and posttraumatic stress disorder in Iraqi refugees. Int J Soc Psychiatry. 2007;53(5):447–463. doi: 10.1177/0020764007078362. [DOI] [PubMed] [Google Scholar]
- 34.Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder AG, Guzder J, Hassan G, Rousseau C, Pottie K Canadian Collaboration for Immigrant and Refugee Health (CCIRH) Common mental health problems in immigrants and refugees:general approach in primary care. CMAJ. 2011;183(12):E959–E967. doi: 10.1503/cmaj.090292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement:a systematic review and meta-analysis. JAMA. 2009;302(5):537–549. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- 36.Lamkaddem M, Stronks K, Deville WD, Olff M, Gerritsen AA, Essink-Bot ML. Course of post-traumatic stress disorder and health care utilisation among resettled refugees in the Netherlands. BMC Psychiatry. 2014;14:90. doi: 10.1186/1471-244X-14-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grad FP. [Dec 5;2017 ];Bulletin of the World Health Organization. http://www.who.int/bulletin/archives/80(12)981.pdf .
- 38.Donnelly TT, Hwang JJ, Este D, Ewashen C, Adair C, Clinton M. If I was going to kill myself, I wouldn't be calling you. I am asking for help:challenges influencing immigrant and refugee women's mental health. Issues Ment Health Nurs. 2011;32(5):279–290. doi: 10.3109/01612840.2010.550383. [DOI] [PubMed] [Google Scholar]
- 39.Kimerling R. An investigation of sex differences in nonpsychiatric morbidity associated with posttraumatic stress disorder. J Am Med Womens Assoc (1972) 2004;59(1):43–47. [PubMed] [Google Scholar]
- 40.Abbott KL, Woods CA, Halim DA, Qureshi HA. Pediatric care during a short-term medical mission to a Syrian refugee camp in Northern Jordan. Avicenna J Med. 2017;7(4):176–181. doi: 10.4103/ajm.AJM_100_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wells R, Steel Z, Abo-Hilal M, Hassan AH, Lawsin C. Psychosocial concerns reported by Syrian refugees living in Jordan:systematic review of unpublished needs assessments. Br J Psychiatry. 2016;209(2):99–106. doi: 10.1192/bjp.bp.115.165084. [DOI] [PubMed] [Google Scholar]
- 42.Carlson EB, Rosser-Hogan R. Trauma experiences, posttraumatic stress, dissociation, and depression in Cambodian refugees. Am J Psychiatry. 1991;148(11):1548–1551. doi: 10.1176/ajp.148.11.1548. [DOI] [PubMed] [Google Scholar]
- 43.Gwozdziewycz N, Mehl-Madrona L. Meta-analysis of the use of narrative exposure therapy for the effects of trauma among refugee populations. Perm J. 2013;17(1):70–76. doi: 10.7812/TPP/12-058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Greenberg JB, Ameringer KJ, Trujillo MA, Sun P, Sussman S, Brightman M, Pitts SR, Leventhal AM. Associations between posttraumatic stress disorder symptom clusters and cigarette smoking. Psychol Addict Behav. 2012;26(1):89–98. doi: 10.1037/a0024328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Naeem F, Taj R, Khan A, Ayub M. Can watching traumatic events on TV cause PTSD symptoms?Evidence from Pakistan. Acta Psychiatr Scand. 2012;126(1):79–80. doi: 10.1111/j.1600-0447.2012.01876.x. [DOI] [PubMed] [Google Scholar]
- 46.Bernstein KT, Ahern J, Tracy M, Boscarino JA, Vlahov D, Galea S. Television watching and the risk of incident probable posttraumatic stress disorder:a prospective evaluation. J Nerv Ment Dis. 2007;195(1):41–47. doi: 10.1097/01.nmd.0000244784.36745.a5. [DOI] [PubMed] [Google Scholar]
- 47.Hebebrand J, Anagnostopoulos D, Eliez S, Linse H, Pejovic-Milovancevic M, Klasen H. A first assessment of the needs of young refugees arriving in Europe:what mental health professionals need to know. Eur Child Adolesc Psychiatry. 2016;25(1):1–6. doi: 10.1007/s00787-015-0807-0. [DOI] [PubMed] [Google Scholar]
- 48.Al-Smadi AM, Halaseh HJ, Gammoh OS, Ashour AF, Gharaibeh B, Khoury LS. Do chronic diseases and availability of medications predict post-traumatic stress disorder (PTSD) among Syrian refugees in Jordan? Pak J Nutr. 2016;15(10):936–941. [Google Scholar]
- 49.Al-Shagran H, Khasawneh OM, Ahmed AK, Jarrah AM. Post-traumatic stress disorder of Syrian refugees in Jordan. Int J Lib Arts Soc Sci. 2015;3(3):36–48. [Google Scholar]
- 50.Naja WJ, Aoun MP, El Khoury EL, Abdallah FJ, Haddad RS. Prevalence of depression in Syrian refugees and the influence of religiosity. Compr Psychiatry. 2016;68:78–85. doi: 10.1016/j.comppsych.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 51.Samari G. Syrian Refugee Women's Health in Lebanon, Turkey, and Jordan and Recommendations for Improved Practice. World Med Health Policy. 2017;9(2):255–274. doi: 10.1002/wmh3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Klepser ME, Adams AJ, Srnis P, Mazzucco M, Klepser D. U.S. community pharmacies as CLIA-waived facilities:Prevalence, dispersion, and impact on patient access to testing. Res Social Adm Pharm. 2016;12(4):614–621. doi: 10.1016/j.sapharm.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 53.Al Alawneh M, Nuaimi N, Basheti IA. Pharmacists in humanitarian crisis settings:Assessing the impact of pharmacist-delivered home medication management review service to Syrian refugees in Jordan. Res Social Adm Pharm. 2019;15(2):164–172. doi: 10.1016/j.sapharm.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 54.World Health Organization 2017. Seventieth World Health Assembly. Provisional agenda item 13.1. Human resources for health and implementation of the outcomes of the United Nations'High Level Commission on Health Employment and Economic Growth. [Feb 4;2018 ];World Health Assembly Journal. http://apps.who.int/gb/ebwha/pdf_files/WHA70'/A70_18-en.pdf?ua=1 .
- 55.World Health Organization. [Feb 4;2018 ];High-Level Commission on Health Employment and Economic Growth. Working for health and growth:investing in the health workforce. Report of the High-Level Commission on Health Employment and Economic Growth. http://apps.who.int/iris/bitstream/10665/250047/1/9789241511308-eng.pdf .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during or analyzed during the current study are available from the corresponding author on reasonable request.


