Abstract
Background
We assessed whether the risk of various psychotic disorders and non-psychotic bipolar disorder (including mania) varied by migrant status, a region of origin, or age-at-migration, hypothesizing that risk would only be elevated for psychotic disorders.
Methods
We established a prospective cohort of 1 796 257 Swedish residents born between 1982 and 1996, followed from their 15th birthday, or immigration to Sweden after age 15, until diagnosis, emigration, death, or end of 2011. Cox proportional hazards models were used to model hazard ratios by migration-related factors, adjusted for covariates.
Results
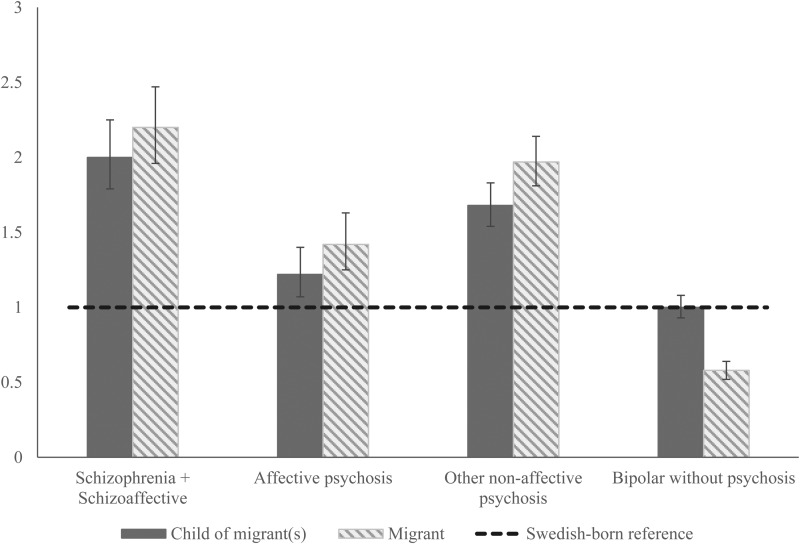
All psychotic disorders were elevated among migrants and their children compared with Swedish-born individuals, including schizophrenia and schizoaffective disorder (adjusted hazard ratio [aHR]migrants: 2.20, 95% CI 1.96–2.47; aHRchildren : 2.00, 95% CI 1.79–2.25), affective psychotic disorders (aHRmigrant1.42, 95% CI 1.25–1.63; aHRchildren: 1.22 95% CI 1.07–1.40), and other non-affective psychotic disorders (aHRmigrant: 1.97, 95% CI 1.81–2.14; aHRchildren: 1.68, 95% CI 1.54–1.83). For all psychotic disorders, risks were generally highest in migrants from Africa (i.e. aHRschizophrenia: 5.24, 95% CI 4.26–6.45) and elevated at most ages-of-migration. By contrast, risk of non-psychotic bipolar disorders was lower for migrants (aHR: 0.58, 95% CI 0.52–0.64) overall, and across all ages-of-migration except infancy (aHR: 1.20; 95% CI 1.01–1.42), while risk for their children was similar to the Swedish-born population (aHR: 1.00, 95% CI 0.93–1.08).
Conclusions
Increased risk of psychiatric disorders associated with migration and minority status may be specific to psychotic disorders, with exact risk dependent on the region of origin.
Key words: Bipolar disorder, epidemiology, mania, migration, psychotic disorders, schizophrenia
Background
The relationship between migration and schizophrenia risk is well-established (Ødegaard, 1932; Cantor-Graae and Selten, 2005; Fearon and Morgan, 2006; Bourque et al., 2011; Cantor-Graae and Pedersen, 2013; Close et al., 2016), and extends to children of migrants (Cantor-Graae and Selten, 2005; Bourque et al., 2011). The risk appears higher among visible minorities, such as the black Caribbean and African populations in the UK (Fearon et al., 2006; Kirkbride et al., 2012b), and is not explained by differences in age, sex, or socioeconomic position (Kirkbride et al., 2008). By contrast, elevated rates have not been consistently shown for bipolar disorder among migrants (Swinnen and Selten, 2007) or their children (Cantor-Graae and Pedersen, 2013; Pignon et al., 2017). Despite this, previous studies have rarely distinguished between bipolar disorders presenting with and without psychotic features. When restricted to those with psychosis, there is some evidence of higher rates of bipolar disorder in migrants and their children (Lloyd et al., 2005).
The impact of migration and social adversity on mental disorders also varies over the life course (Patel and Goodman, 2007), although only limited, equivocal research has investigated the role that age-at-migration may play in shaping risk (Veling et al., 2011; Pedersen and Cantor-Graae, 2012; Kirkbride et al., 2017b). For example, a Dutch study found the highest risk of psychotic disorders with infant migration (Veling et al., 2011), while a more recent British study found risk peaked with early childhood migration (Kirkbride et al., 2017b). Finally, a Danish study found no association between age-at-migration and schizophrenia (Pedersen and Cantor-Graae, 2012). No study to date has examined age-at-migration in relation to bipolar disorders, with or without psychosis.
To clarify these issues, we used national register data from Sweden, a country of 10 million people with a long history of immigration (OECD, 2017), to investigate whether migrant status, region of origin, and age-at-migration acted specifically on the risk of developing psychotic disorders, including schizophrenia, affective psychoses (i.e. bipolar disorder with psychotic symptoms or psychotic depression), or also extended to non-psychotic bipolar disorder and mania. Given the earlier research, we hypothesized that excess risk in migrant groups would be limited to psychotic disorders. Similarly, we hypothesized that migration during infancy and early childhood would increase psychosis risk, but not non-psychotic bipolar disorder and mania. These periods of the life course are marked by rapid social, neurobiological, and cognitive development, including maturation of the dopaminergic system in the prefrontal cortex during infancy (Rothmond et al., 2012; Selemon and Zecevic, 2015) and development of ‘theory of mind’ and general cognition during early childhood (Perner and Lang, 1999; Garety et al., 2001; Colvert et al., 2008). Migration during such periods may disrupt typical neurocognitive development, which subsequently increases psychosis risk. Whilst cognitive deficits have been observed in both schizophrenia and bipolar disorder, cognitive impairments in bipolar disorder appear less severe (Trotta et al., 2014), and other developmental abnormalities also show specificity towards psychotic disorders during this period (Reichenberg et al., 2002; Hill et al., 2013).
Methods
Study design and population
We used multiple national Swedish registers to identify all individuals born between 1982 and 1996, living in Sweden after their 15th birthday, including those who immigrated to Sweden. Cohort entry was age 15 years, or date of first immigration to Sweden, if later. Individuals were followed from cohort entry (earliest: 1 January 1997) until 31 December 2011, or exit from the cohort due to the diagnosis of a psychiatric disorder of interest (see below), emigration or death, whichever came sooner. The Cause of Death register was used to obtain the date of death and the Migration Register was used to record date of migration. Individuals who died emigrated for the final time, or who were diagnosed with a psychiatric outcome before age 15 were excluded.
Outcomes
We linked participants to the National Patient Register to determine a psychiatric diagnosis in either inpatient or outpatient settings according to the International Classification of Diseases, 10th revision [ICD-10]. We studied four psychiatric outcomes: schizophrenia or schizoaffective disorder (F20.X, F25.X); affective psychotic disorders (F30.2, F31.2, F31.5, F32.3, F33.3), other non-affective psychotic disorders (F21.X-F24.X, F28.X- F29.X) and; bipolar disorder or manic symptoms without confirmed psychotic symptoms (F30.1, F30.8, F30.9, F31.0–31.1, F31.3–31.4, F31.6–31.9). For individuals who received diagnoses on multiple visits to in- or outpatient services, we adopted a hierarchal classification system, informed by clinical expertise (GL, CD, CM, AH) and consistent with earlier research (Björkenstam et al., 2013), as follows: schizophrenia or schizoaffective disorder, affective psychotic disorders, other non-affective psychotic disorders, and finally, non-psychotic bipolar disorder or mania; date of cohort exit was defined as the date at which they received this diagnosis.
Exposures
We defined migrant status according to information in the Total Population and Multi-Generational registers. Participants were classified as (i) migrants if they were born outside of Sweden; (ii) children of migrants if they were born in Sweden with one or both parents born outside of Sweden, and; (iii) Swedish-born if they were born in Sweden to two Swedish-born parents. The region of origin was defined by Statistics Sweden as Sweden, Finland, other Nordic countries, other European countries, Asia and Oceania, the Middle East, Africa, North America, South America, and unknown, based on country of birth. For migrants, we categorized age-at-first-migration into five groups: infancy (0–2 years), early childhood (3–6 years), middle childhood (7–12 years), adolescence (13–18 years) and early adulthood (19–29 years). We considered sex, current age, and follow-up period (see below) as a priori confounders. We also controlled for income in supplemental analyses, obtained from the Longitudinal Integration Database for Health Insurance and Labour Market Studies [LISA]. Since 1990, LISA has estimated total disposable family income from all sources each year (salary, wages, welfare, pensions), weighted for family size. As age 16 is the earliest an individual is included in the LISA, for most participants, we utilized information on their family income at age 15 via linkage to their parents, including adoptive parents where relevant. For migrants arriving in Sweden after age 15, we included their family income as first recorded in the LISA database. Where no income could be estimated, participants were excluded from these analyses (see below). We calculated income quintiles in each year for the entire population and assigned this value to participants in the year of their cohort entry. This method implicitly takes income inflation into account.
Statistical analysis
We first generated descriptive characteristics of the sample. Next, for each outcome, we investigated whether incidence varied by migrant status, region of origin, and age-at-migration using Cox proportional hazard regression. We estimated unadjusted and adjusted hazard ratios [aHR] and 95% confidence intervals [95% CI] for each exposure. To account for possible period effects (e.g., due to possible changes in health care services over the 14-year follow-up period), we split the data into 5-year bands of calendar time (1997–2001, 2002–2006, 2007–2011), modelled as a time-varying covariate. We also modelled age as a time-varying covariate (15–17, 18–20, 21–23, 24–26, 27–30 years), given risk of psychiatric disorders varies substantially by age (Hollander et al., 2016; Kirkbride et al., 2017a). The proportional hazards assumption was evaluated using Schoenfeld residuals and examination of log-log plots. We conducted two sensitivity analyses. First, because income may have been on the causal pathway between migration-related exposures and risk of psychiatric disorders, these adjustments were presented as sensitivity analyses, excluding those with missing information on this variable. Second, we included a washout period to exclude migrant participants diagnosed with an outcome of interest within 2 years of immigration to Sweden, who may have been prevalent cases. All modelling was conducted in Stata, version 13.
Results
We identified 1 796 257 individuals who contributed over 12.79 million person-years of follow-up (Table 1). Of these, 17.8% were migrants and 11.2% were children of migrants. In all, 15 423 individuals (0.9%) were diagnosed with an outcome of interest during follow-up, including 2172 individuals (0.1%) with schizophrenia or schizoaffective disorder, 2163 (0.1%) with an affective psychotic disorder, 4510 (0.3%) with another non-affective psychotic disorder, and 6295 (0.4%) with non-psychotic bipolar disorder. Among cases, the proportion of women diagnosed with a psychiatric disorder varied by migrant status (χ2 on 2 degrees of freedom [df]; p < 0.001), being highest amongst the Swedish-born population (59.2%) and lowest amongst migrants (45.0%). As expected, migrants with psychiatric diagnoses were more likely to be in the lowest income quintile (30.2%) compared to 5.3% of Swedish-born, and 8.6% of children of migrants (χ2 on 10 df; p < 0.001). Additional cohort characteristics are presented in Table 1.
Table 1.
Cohort characteristics by migrant status
| Swedish-born (n = 1 275 748) | Children of migrants (n = 200 407) | Migrants (n = 320 102) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cases | % | Total person-years | Cases | % | Total person-years | Cases | % | Total person-years | |
| Psychiatric diagnosis | |||||||||
| Schizophrenia + schizoaffective | 1333 | 0.1 | 9 802 814 | 368 | 0.2 | 1 403 948 | 471 | 0.2 | 1 631 366 |
| Affective psychotic disorders | 1532 | 0.1 | 9 802 240 | 259 | 0.1 | 1 404 455 | 372 | 0.1 | 1 631 982 |
| Other non-affective psychotic disorders | 2899 | 0.2 | 9 797 765 | 687 | 0.3 | 1 402 980 | 924 | 0.3 | 1 630 197 |
| Bipolar disorder without psychotic symptoms | 5130 | 0.4 | 9 793 959 | 724 | 0.4 | 1 403 407 | 441 | 0.1 | 1 632 041 |
| Sex | |||||||||
| Male | 4499 | 40.8 | 5 034 939 | 1017 | 48.2 | 720 336 | 1265 | 55.2 | 823 667 |
| Female | 6521 | 59.2 | 4 737 861 | 1094 | 51.8 | 678 348 | 1027 | 44.8 | 802 363 |
| Income | |||||||||
| Quintile 1 (Lowest) | 588 | 5.3 | 293 129 | 182 | 8.6 | 84 411 | 690 | 30.1 | 529 386 |
| Quintile 2 | 2021 | 18.3 | 1 212 372 | 431 | 20.4 | 228 359 | 300 | 13.1 | 192 003 |
| Quintile 3 | 2481 | 22.5 | 1 731 842 | 565 | 26.8 | 347 721 | 470 | 20.5 | 329 979 |
| Quintile 4 | 2985 | 27.1 | 3 011 696 | 485 | 23.0 | 374 611 | 381 | 16.6 | 270 114 |
| Quintile 5 (Highest) | 2932 | 26.6 | 3 517 217 | 436 | 20.7 | 358 555 | 278 | 12.1 | 169 106 |
| Unknown | 13 | 0.1 | 6544 | 12 | 0.6 | 5026 | 173 | 7.6 | 135 443 |
| Age-at-migration | |||||||||
| Swedish born | 11 020 | 100.0 | 9 772 800 | 2111 | 100.0 | 1 398 684 | |||
| Infancy (0–2) | 384 | 16.8 | 221 374 | ||||||
| Early childhood (3–6) | 436 | 19.0 | 297 272 | ||||||
| Middle childhood (7–12) | 539 | 23.5 | 394 417 | ||||||
| Adolescence (13–18) | 458 | 20.0 | 301 284 | ||||||
| Early adulthood (19–29) | 475 | 20.7 | 397 242 | ||||||
| Unknown | 0 | 0.0 | 14 441 | ||||||
| Region of origin | |||||||||
| Sweden | 11 020 | 100.0 | 9 772 800 | 2111 | 100.0 | 1 398 684 | |||
| Finland | 59 | 2.6 | 29 770 | ||||||
| Other Nordic | 83 | 3.6 | 54 832 | ||||||
| Europe | 582 | 25.4 | 522 376 | ||||||
| Asia + Oceania | 356 | 15.5 | 278 469 | ||||||
| Middle East | 560 | 24.4 | 441 042 | ||||||
| Africa | 400 | 17.5 | 161 752 | ||||||
| North America | 66 | 2.9 | 35 259 | ||||||
| South America | 185 | 8.1 | 101 726 | ||||||
| Unknown | 1 | 0.0 | 804 | ||||||
Risk of all psychotic disorders was elevated among migrants and their children compared with Swedish-born individuals, after adjustment for confounding. For example, risk of schizophrenia and schizoaffective disorder was approximately doubled in migrants (aHR: 2.20; 95% CI 1.96–2.47) and their children (aHR: 2.00; 95% CI 1.79–2.25), with similar results obtained for other non-affective psychotic disorders (Table 2). Risk of affective psychoses was also elevated amongst migrants (aHR: 1.42; 95% CI 1.25–1.63) and their children (aHR: 1.22; 95% CI 1.07–1.40), albeit to a lesser extent than for schizophrenia and other psychoses (Fig. 1). In contrast, migrants were at reduced risk of bipolar disorder without psychosis (aHR: 0.58, 95% CI 0.52–0.64) compared with the Swedish-born population, while the risk was equivocal for children of migrants (aHR: 1.00, 95% CI 0.93–1.08).
Table 2.
Unadjusted and Adjusted hazard ratios by migrant status
| N | % | Unadjusted | Adjusteda | |||
|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | Hazard ratio | 95% CI | |||
| Schizophrenia + schizoaffective | ||||||
| Swedish born (reference) | 1333 | 61.4 | 1 | 1 | ||
| Children of migrants | 368 | 16.9 | 2.00 | 1.78–2.25 | 2.00 | 1.79–2.25 |
| Migrant | 471 | 21.7 | 2.43 | 2.19–2.70 | 2.20 | 1.96–2.47 |
| Affective psychotic disorders | ||||||
| Swedish born (reference) | 1532 | 70.8 | 1 | 1 | ||
| Children of migrants | 259 | 12.0 | 1.24 | 1.09–1.42 | 1.22 | 1.07–1.40 |
| Migrant | 372 | 17.2 | 1.58 | 1.40–1.77 | 1.42 | 1.25–1.63 |
| Other non-affective psychotic disorders | ||||||
| Swedish born (reference) | 2899 | 64.3 | 1 | 1 | ||
| Children of migrants | 687 | 15.2 | 1.70 | 1.56–1.84 | 1.68 | 1.54–1.83 |
| Migrant | 924 | 20.5 | 2.13 | 1.98–2.30 | 1.97 | 1.81–2.14 |
| Bipolar disorder without psychosis | ||||||
| Swedish born (reference) | 5130 | 81.5 | 1 | 1 | ||
| Children of migrants | 724 | 11.5 | 1.02 | 0.95–1.11 | 1.00 | 0.93–1.08 |
| Migrant | 441 | 7.0 | 0.59 | 0.53–0.65 | 0.58 | 0.52–0.64 |
95% CI, 95% confidence interval.
Adjusted for age, sex, and time period.
Fig. 1.
Risk of schizophrenia, schizoaffective, and bipolar disorders by migrant status, region of origin, and age-at-migration. A national cohort study of 1.8 million people. Adjusted hazard ratios by migrant status. 95% CI, 95% confidence interval. 1Adjusted for age, sex, and time period.
The excess risk of psychotic disorders in migrants persisted for participants from all regions of origin (Table 3). Thus, for schizophrenia and schizoaffective disorder, all migrants (except people of ‘other Nordic’ origin) were at increased risk, while other non-affective psychotic disorders were elevated for migrants from all regions of origin. For affective psychoses, migrants from Africa, South America, Asia & Oceania, and the Middle East were at increased risk. For all psychotic outcomes, risk was highest amongst migrants from Africa, including schizophrenia (aHR: 5.24, 95% CI 4.26–6.45), other non-affective psychoses (aHR: 4.39, 95% CI 3.77–5.10), and to a lesser degree, affective psychosis (aHR: 2.01, 95% CI 1.49–2.70). By contrast, migrants from Africa, Europe, the Middle East, Asia, and Oceania showed reduced risk of bipolar disorder without psychosis compared with the Swedish-born population (Table 3), and only migrants from Finland (aHR: 1.56, 95% CI 1.01–2.41) and North America (aHR: 1.69, 95% CI 1.15–2.50) had elevated risk.
Table 3.
Unadjusted and adjusted hazard ratios by region of origin
| N | % | Unadjusted | Adjusteda | |||
|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | Hazard ratio | 95% CI | |||
| Schizophrenia + schizoaffective | ||||||
| Swedish-born (reference) | 1333 | 61.4 | 1 | 1 | ||
| Finland | 7 | 0.3 | 2.26 | 1.07–4.75 | 1.90 | 0.90–4.02 |
| Other Nordic | 10 | 0.5 | 1.83 | 0.98–3.40 | 1.50 | 0.80–2.82 |
| Europe | 125 | 5.8 | 2.01 | 1.67–2.41 | 1.85 | 1.53–2.23 |
| Asia + Oceania | 61 | 2.8 | 1.92 | 1.48–2.49 | 1.72 | 1.32–2.25 |
| Middle East | 123 | 5.7 | 2.25 | 1.87–2.71 | 2.07 | 1.71–2.50 |
| Africa | 105 | 4.8 | 5.94 | 4.87–7.25 | 5.24 | 4.26–6.45 |
| North America | 11 | 0.5 | 2.77 | 1.53–5.02 | 2.44 | 1.34–4.43 |
| South America | 29 | 1.3 | 1.94 | 1.32–2.83 | 1.84 | 1.26–2.70 |
| Affective psychotic disorders | ||||||
| Swedish-born (reference) | 1532 | 70.8 | 1 | 1 | ||
| Finland | 6 | 0.3 | 1.58 | 0.71–3.52 | 1.35 | 0.60–3.03 |
| Other Nordic | 7 | 0.3 | 1.02 | 0.49–2.15 | 0.89 | 0.42–1.89 |
| Europe | 106 | 4.9 | 1.37 | 1.11–1.68 | 1.23 | 0.99–1.53 |
| Asia + Oceania | 71 | 3.3 | 1.76 | 1.37–2.25 | 1.53 | 1.18–1.99 |
| Middle East | 97 | 4.5 | 1.48 | 1.19–1.83 | 1.37 | 1.10–1.70 |
| Africa | 50 | 2.3 | 2.31 | 1.73–3.07 | 2.01 | 1.49–2.70 |
| North America | 7 | 0.3 | 1.49 | 0.71–3.13 | 1.36 | 0.64–2.86 |
| South America | 28 | 1.3 | 1.79 | 1.22–2.62 | 1.81 | 1.23–2.65 |
| Other non-affective psychotic disorders | ||||||
| Swedish-born (reference) | 2899 | 64.3 | 1 | 1 | ||
| Finland | 15 | 0.3 | 2.09 | 1.26–3.47 | 1.91 | 1.14–3.17 |
| Other Nordic | 22 | 0.5 | 1.56 | 1.00–2.42 | 1.36 | 0.87–2.12 |
| Europe | 225 | 5.0 | 1.60 | 1.40–1.84 | 1.50 | 1.30–1.72 |
| Asia + Oceania | 140 | 3.1 | 1.96 | 1.65–2.33 | 1.79 | 1.50–2.13 |
| Middle East | 240 | 5.3 | 2.00 | 1.75–2.28 | 1.88 | 1.64–2.16 |
| Africa | 198 | 4.4 | 4.89 | 4.23–5.65 | 4.39 | 3.77–5.10 |
| North America | 20 | 0.4 | 2.12 | 1.35–3.34 | 1.94 | 1.23–3.05 |
| South America | 64 | 1.4 | 2.13 | 1.66–2.73 | 2.12 | 1.65–2.72 |
| Bipolar disorder without psychosis | ||||||
| Swedish-born (reference) | 5130 | 81.5 | 1 | 1 | ||
| Finland | 21 | 0.3 | 1.73 | 1.13–2.66 | 1.56 | 1.01–2.41 |
| Other Nordic | 31 | 0.5 | 1.44 | 1.01–2.05 | 1.35 | 0.94–1.93 |
| Europe | 110 | 1.8 | 0.45 | 0.37–0.54 | 0.43 | 0.36–0.53 |
| Asia + Oceania | 79 | 1.3 | 0.63 | 0.50–0.79 | 0.60 | 0.47–0.75 |
| Middle East | 88 | 1.4 | 0.42 | 0.34–0.52 | 0.43 | 0.34–0.53 |
| Africa | 23 | 0.4 | 0.33 | 0.22–0.50 | 0.32 | 0.21–0.48 |
| North America | 26 | 0.4 | 1.68 | 1.14–2.47 | 1.69 | 1.15–2.50 |
| South America | 62 | 1.0 | 1.16 | 0.90–1.49 | 1.27 | 0.99–1.63 |
| Unknown | 1 | 0.0 | 3.73 | 0.52–26.46 | 3.27 | 0.46–23.27 |
95% CI, 95% confidence interval. There were no cases of schizophrenia/schizoaffective disorder, affective psychosis, or other non-affective psychosis among people of ‘unknown’ region of origin.
Adjusted for age, sex and time period.
Risks of all psychotic disorders were elevated across most ages-of-migration compared with the Swedish-born population (Table 4). For schizophrenia and schizoaffective disorder elevated risk was apparent across all ages-of-migration relative to the Swedish-born population, and was highest for those migrating in adolescence and early adulthood (aHRadolescence: 2.38, 95% CI 1.79–3.16; aHRearly adulthood: 2.77, 95% CI 1.64–4.69). For other non-affective psychotic disorders risk was elevated at all ages-of-migration, except early adulthood (aHR: 1.17; 95% CI 0.80–1.72). Risk of affective psychosis was elevated among those who migrated in infancy (aHR: 1.71, 95% CI 1.31–2.24), adolescence (aHR: 1.81, 95% CI 1.42–2.30) and early adulthood (aHR 2.05, 95% CI 1.20–3.52), but not childhood. In contrast, bipolar disorder without psychosis was associated with lower risks at all ages-of-migration, except during infancy (aHR: 1.20, 95% CI 1.01–1.42).
Table 4.
Unadjusted and adjusted hazard ratios by Age-At-Migration
| N | % | Unadjusted | Adjusted | |||
|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | Hazard ratioa | 95% CI | |||
| Schizophrenia + schizoaffective | ||||||
| Swedish born (reference) | 1333 | 61.4 | 1 | 1 | ||
| Infancy (0–2) | 49 | 2.3 | 1.57 | 1.17–2.09 | 1.57 | 1.18–2.09 |
| Early childhood (3–6) | 89 | 4.1 | 2.16 | 1.74–2.67 | 2.14 | 1.73–2.66 |
| Middle childhood (7–12) | 132 | 6.1 | 2.34 | 1.96–2.80 | 2.32 | 1.94–2.78 |
| Adolescence (13–18) | 105 | 4.8 | 2.97 | 2.43–3.62 | 2.76 | 2.23–3.41 |
| Early adulthood (19–29) | 96 | 4.4 | 3.56 | 2.88–4.41 | 2.77 | 1.64–4.69 |
| Affective psychotic disorders | ||||||
| Swedish born (reference) | 1532 | 70.8 | 1 | 1 | ||
| Infancy (0–2) | 58 | 2.7 | 1.69 | 1.30–2.21 | 1.71 | 1.31–2.24 |
| Early childhood (3–6) | 58 | 2.7 | 1.27 | 0.97–1.66 | 1.29 | 0.99–1.68 |
| Middle childhood (7–12) | 67 | 3.1 | 1.07 | 0.83–1.37 | 1.13 | 0.88–1.45 |
| Adolescence (13–18) | 87 | 4.0 | 1.89 | 1.51–2.38 | 1.81 | 1.42–2.30 |
| Early adulthood (19–29) | 102 | 4.7 | 2.34 | 1.90–2.89 | 2.05 | 1.20–3.52 |
| Other non-affective psychotic disorders | ||||||
| Swedish born (reference) | 2899 | 64.3 | 1 | 1 | ||
| Infancy (0–2) | 126 | 2.8 | 1.92 | 1.61–2.30 | 1.95 | 1.63–2.33 |
| Early childhood (3–6) | 191 | 4.2 | 2.16 | 1.86–2.50 | 2.15 | 1.85–2.49 |
| Middle childhood (7–12) | 210 | 4.7 | 1.76 | 1.52–2.02 | 1.82 | 1.58–2.10 |
| Adolescence (13–18) | 207 | 4.6 | 2.58 | 2.24–2.98 | 2.16 | 1.86–2.52 |
| Early adulthood (19–29) | 190 | 4.2 | 2.58 | 2.22–2.99 | 1.17 | 0.80–1.72 |
| Bipolar disorder without psychosis | ||||||
| Swedish born (reference) | 5130 | 81.5 | 1 | 1 | ||
| Infancy (0–2) | 141 | 2.2 | 1.19 | 1.00–1.40 | 1.20 | 1.01–1.42 |
| Early childhood (3–6) | 83 | 1.3 | 0.53 | 0.42–0.66 | 0.54 | 0.43–0.67 |
| Middle childhood (7–12) | 97 | 1.5 | 0.45 | 0.36–0.55 | 0.49 | 0.40–0.59 |
| Adolescence (13–18) | 43 | 0.7 | 0.31 | 0.23–0.42 | 0.27 | 0.20–0.37 |
| Early adulthood (19–29) | 77 | 1.2 | 0.68 | 0.55–0.86 | 0.35 | 0.20–0.61 |
95% CI, 95% confidence interval; Swedish-born reference category. Children of migrants excluded as results shown in Table 2.
Adjusted for age, sex, and time period, baseline Swedish-born.
These associations were partially attenuated following adjustment for income, but this did not substantially alter our findings (online Supplementary Tables S1–S3). A sensitivity analysis excluding possible prevalent cases in migrants (diagnosed within 2 calendar years of immigration) did not change the pattern of our results (online Supplementary Tables S4–S6). Schoenfeld tests and examination of log-log residual plots revealed no evidence of departure from proportionality across our main exposures for schizophrenia or affective psychosis (online Supplementary Table S7). These tests did suggest a departure from proportionality for our other two outcomes, but log-log residual plots revealed these effects were small and the departure from a zero-slope was negligible (online Supplementary Fig. S1).
Discussion
Principal findings
This is the first longitudinal study to investigate how migrant status, region of origin, and age-at-migration affect the risk of schizophrenia, schizoaffective disorder, affective psychotic disorders, other non-affective psychotic disorders, and non-psychotic bipolar disorder. We discovered distinct signatures of risk, which varied according to the presence or absence of psychosis. Thus, migration-related exposures substantially increased the risk of psychotic disorders, albeit with more attenuated effect sizes for affective psychoses. In contrast, non-psychotic bipolar disorder showed a markedly different pattern, with generally lower risks across our three migration-related exposures compared with the Swedish-born population. Our results were impervious to adjustment for income and were unlikely to be explained by prevalent cases amongst migrants, or by age, sex, or period effects.
Strengths and limitations
We used to register data from a nationwide cohort of nearly 1.8 million people, with nearly complete coverage, and virtually no loss-to-follow-up. Clinical recording of schizophrenia spectrum disorders is known to be highly complete in the registers with good validity (Dalman et al., 2002; Hollander et al., 2016), although this requires demonstrating for bipolar disorders. We limited our follow-up period to 1997–2011 when ICD-10 was the sole diagnostic classification system used in Sweden. This avoided major changes in diagnostic practice over the cohort period and allowed us to distinguish between bipolar disorders with and without psychosis for the first time in this population. Our decision to use a hierarchical diagnostic classification did not bias findings; similar results were obtained when we classified participants by their first or final diagnosis in the registers (data available from authors). To account for possible changes in case ascertainment over time, including the introduction of more outpatient services in Sweden after 1997, we included calendar time to control for period effects. There was no evidence of a violation of proportional hazards across our three migration-related exposures for schizophrenia or affective psychosis. Departures from proportionality for other outcomes were small, and were likely driven by our large sample size, and would likely have had trivial effects on the interpretation of our results.
We have no reason to believe that our estimates of the incidence of bipolar disorder and affective psychosis are not valid, however, unlike non-affective psychosis, these disorders still require validation in the Swedish registry data. In our sample, psychosis was only diagnosed in 25.6% of those with bipolar disorder/mania, which is lower than previous lifetime estimates between 50 and 61% (Goodwin and Jamison, 1990; Dunayevich and Keck, 2000). This may reflect the young age of our sample, meaning that some people diagnosed with bipolar disorder without psychosis for the first time in our study may eventually go onto experience an episode of psychosis. Alternatively, bipolar disorder with psychosis may be under-diagnosed in Sweden. Nonetheless, the overall incidence of affective psychosis in our sample (15.9, 95% CI 15.2–16.6) was higher than reported in previous studies (Kirkbride et al., 2006), favouring the former explanation than one of under-diagnosis. For all migration exposures, elevated risk of schizophrenia and schizoaffective disorders was of the order of magnitude higher than for affective psychosis. For children of migrants (although not migrants) the confidence intervals around the elevated risk of affective psychosis narrowly overlapped those for the non-significant difference in risk of bipolar disorder without psychosis between children of migrants and the Swedish-born populations; we cannot, therefore, exclude the possibility that our findings have partially arisen from chance, although the consistency and pattern of our results suggest this is unlikely; nevertheless, further, large studies are required to replicate our results.
In our study, case participants were based on contact with mental health services, which may have led to some underestimation of the true incidence of psychiatric disorders within the population, although register-based approaches appear to lead to more complete case ascertainment than first contact designs (Hogerzeil et al., 2014). Nevertheless, if migrants and their children had differential treatment-seeking behaviours compared with Swedish-born individuals, differential ascertainment bias could have affected our results. Research from the Netherlands has demonstrated a larger gap between mental health care need and service use among migrants compared with native Dutch (Koopmans et al., 2012). Despite the universal availability of health care in Sweden, such differences in help-seeking may have conservatively biased our estimates of risk amongst some migrants, particularly for less severe phenotypes such as bipolar disorder without psychosis for which people may be less likely to seek mental health care. Nevertheless, our findings for bipolar disorders without psychosis are in line with previous studies which have not consistently found elevated risk in migrants or their children (Swinnen and Selten, 2007; Cantor-Graae and Pedersen, 2013; Pignon et al., 2017).
Our sensitivity analyses suggested our results were not due to confounding by income. Nevertheless, our income covariate was differentially missing by migrant status (7.4% in migrants, 0.5% in their children, 0.1% in the Swedish-born), which may have introduced bias vis-à-vis residual confounding; from the available data, however, any confounding effect appeared modest, and income may lie on the causal pathway between migration and mental health, making adjustment inappropriate.
Further sensitivity analyses suggested our results were unlikely to be attributable to prevalent cases amongst migrants, arguing against selective migration, consistent with previous observations (Selten et al., 2002; van der Ven et al., 2014). Migration is a cognitively-demanding process, requiring effective planning skills, which would be inconsistent with premorbid cognitive defects experienced by people who go onto develop psychosis (Rosenthal et al., 1974; Cannon et al., 2000; van der Ven et al., 2014).
Comparison with the previous literature
Our results are consistent with previous research demonstrating an increased risk of schizophrenia-spectrum disorders among migrants and their children (Lloyd et al., 2005; Coid et al., 2008; Cantor-Graae and Pedersen, 2013). Some studies have also shown an increased risk of affective psychosis in migrants and their children (Lloyd et al., 2005; Coid et al., 2008). Our results also mirror the wider literature, which has shown that region of origin has a significant impact on psychosis risk (Kirkbride et al., 2012a; Pedersen and Cantor-Graae, 2012), notably amongst visible minority populations (Fearon et al., 2006; Coid et al., 2008; Kirkbride et al., 2012a).
Comparisons with previous findings with respect to age-at-migration and psychotic disorders require careful attention. In one study (Veling et al., 2011), the highest risk of non-affective psychoses amongst migrants relative to the background population was associated with migration during infancy, with risk declining thereafter, such that adulthood migration was not associated with differences in risk. Two further studies (Anderson et al., 2015; Kirkbride et al., 2017b) found some evidence that elevated psychosis risk peaked with migration during adolescence relative to the background population, consistent with our observations for non-affective psychotic disorders. Nevertheless, in all these studies, including our own, overlapping confidence intervals for risks at different ages-of-migration mean these findings are also consistent with those reported by Cantor-Graae and Pedersen and Pedersen (2003) in Denmark, who found no statistically significant differences in psychosis risk by age-of-migration, when migration at birth provided the reference category. In our study, the only robust differences in risk by age-of-migration occurred for bipolar disorder without psychosis, never previously examined, where risks were elevated with infant migration, but significantly reduced at all other ages of migration, relative to the Swedish-born population.
Meaning of findings
The different signatures of risk we observed between psychotic and non-psychotic disorders with respect to migration suggest that exposure to adversities related to migration and minority status could act specifically on psychotic rather than affective pathways. Emerging research supports the hypothesis that psychotic and non-psychotic bipolar disorder may have distinct neurodevelopmental origins (Murray et al., 2004; Maggioni et al., 2017). For example, structural magnetic resonance imaging has revealed that non-psychotic bipolar disorders do not show deficits in cortical grey matter volume, in contrast to affective psychosis and other psychotic disorders (Maggioni et al., 2017). Moreover, schizophrenia (Green, 2006) and bipolar disorder with psychosis (Glahn et al., 2007; Bora et al., 2010; Hill et al., 2013) also appear to share premorbid cognitive deficits, not consistently observed for non-psychotic affective disorders (Reichenberg et al., 2002; Trotta et al., 2014). These deficits could contribute to a plausible pathway, through which repeated exposure to social adversities, including migration, leads to psychotic symptoms via increased stress reactivity (Bentall et al., 2014). Individuals who develop non-psychotic bipolar disorder may not experience comparable premorbid cognitive deficits (Goodwin et al., 2008; MacCabe et al., 2010; Vreeker et al., 2016). However, the evidence remains equivocal, as a recent meta-analysis did not find different trajectories of cognitive functioning between schizophrenia and bipolar disorder (Bora and Özerdem, 2017), though did not differentiate between those with and without psychosis in the latter.
Repeated exposure to factors associated with migration – including social disadvantage, trauma or discrimination experienced prior to, during, or following migration – may also prime individuals to expect a greater level of threat from the environment (Reininghaus et al., 2016). Such processes may sensitize neurobiological pathways relevant to psychosis, including dysregulation of the mesolimbic dopaminergic system (Kapur, 2003), particularly amongst those with impaired neurocognition, who may be more prone to errors in salience appraisal of irrelevant or benign environmental stimuli (Kapur, 2003; Roiser et al., 2009). Given the absence of similar neurocognitive impairments in non-psychotic bipolar disorder (Kapur, 2003; Roiser et al., 2009), such psychological and biological mechanisms may partially underlie the observed differences between psychotic and non-psychotic disorders.
We should also give credence to another possible explanation of our results: misdiagnosis. It has been suggested that higher rates of psychotic disorders in some ethnic minority groups are due to diagnostic bias, with people from the majority group less likely to receive a stigmatizing diagnosis such as schizophrenia compared with bipolar disorder (Schwartz and Blankenship, 2014). Although we did not have data on ethnicity in our study, migrants from regions where they were most likely to be visible minorities in Sweden (i.e. Africa, the Middle East, Asia & Oceania) were more likely to be diagnosed with a psychotic disorder, and less likely to be diagnosed with bipolar disorder without psychosis than Swedish-born participants. Together with the finding that only migrants from Nordic countries or North America were more likely to be diagnosed with the non-psychotic bipolar disorder than the Swedish-born population, this is consistent with the misdiagnosis hypothesis. Nonetheless, our data do not entirely support this explanation. Finnish, other Nordic and European, and North America migrants were also all at increased risk of psychotic disorders, to a similar extent to groups from the Middle East, Asia, and South America. Furthermore, in our data, European migrants were also less likely to be diagnosed with the non-psychotic bipolar disorder, which does not readily fit with the hypothesis that people of white ethnicities are likely to receive less stigmatizing (non-psychotic) diagnoses instead of psychotic ones. In general, the misdiagnosis hypothesis is not borne out by other available evidence (Lewis et al., 1990; Hickling et al., 1999; Selten et al., 2010; Zandi et al., 2010), and previous epidemiological studies – with some blinding of diagnosticians to ethnicity – have demonstrated elevated rates of psychotic disorders persist in several black and minority ethnic groups (Fearon et al., 2006).
Conclusion
The shared patterns of risk across three categories of psychotic disorders with respect to various migration-related exposures suggest that migration may act specifically on psychotic rather than affective pathways to disorder. This provides potentially important clues to the aetiology of serious mental illnesses and should galvanise efforts to identify the exact social, environmental, and biological determinants of this preventable, gross inequality experienced by migrant and minority populations (Kirkbride, 2017).
Acknowledgements
This work was supported by a Sir Henry Dale Fellowship jointly funded by the Wellcome Trust and the Royal Society (grant number: 101272/Z/13/Z to JBK), by Mental Health Research UK (to JBK/JD), UCLH NIHR Biomedical Research Centre, and by a UCL Overseas Research Scholarship (to JD).
Author ORCIDs
Jennifer Dykxhoorn 0000-0001-6391-8626.
Conflict of interest
Ms. Dykxhoorn, Dr Hollander, Prof. Magnusson, Prof. Lewis, Prof. Dalman, and Dr Kirkbride report no competing interests.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291718003227.
click here to view supplementary material
References
- Anderson KK, Cheng J, Susser E, McKenzie KJ and Kurdyak P (2015) Incidence of psychotic disorders among first-generation immigrants and refugees in Ontario. Canadian Medical Association Journal 187, E279–E286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentall RP, De Sousa P, Varese F, Wickham S, Sitko K, Haarmans M and Read J (2014) From adversity to psychosis: pathways and mechanisms from specific adversities to specific symptoms. Social Psychiatry and Psychiatric Epidemiology 49, 1011–1022. [DOI] [PubMed] [Google Scholar]
- Björkenstam E, Björkenstam C, Hjern A, Reutfors J and Bodén R (2013) A five year diagnostic follow-up of 1840 patients after a first episode non-schizophrenia and non-affective psychosis. Schizophrenia Research 150, 205–210. [DOI] [PubMed] [Google Scholar]
- Bora E and Özerdem A (2017) Meta-analysis of longitudinal studies of cognition in bipolar disorder: comparison with healthy controls and schizophrenia. Psychological Medicine 47, 2753–2766. [DOI] [PubMed] [Google Scholar]
- Bora E, Yücel M and Pantelis C (2010) Cognitive impairment in affective psychoses: a meta-analysis. Schizophrenia Bulletin 36, 112–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourque F, van der Ven E and Malla A (2011) A meta-analysis of the risk for psychotic disorders among first- and second-generation immigrants. Psychological Medicine 41, 897–910. [DOI] [PubMed] [Google Scholar]
- Cannon TD, Bearden CE, Hollister JM, Rosso IM, Sanchez LE and Hadley T (2000) Childhood cognitive functioning in schizophrenia patients and their unaffected siblings: a prospective cohort study. Schizophrenia Bulletin 26, 379–393. [DOI] [PubMed] [Google Scholar]
- Cantor-Graae E and Pedersen CB (2013) Full spectrum of psychiatric disorders related to foreign migration. JAMA Psychiatry 70, 427. [DOI] [PubMed] [Google Scholar]
- Cantor-Graae E and Selten J-PP (2005) Schizophrenia and migration: a meta-analysis and review. American Journal of Psychiatry 162, 12–24. [DOI] [PubMed] [Google Scholar]
- Close C, Kouvonen A, Bosqui T, Patel K, O'Reilly D and Donnelly M (2016) The mental health and wellbeing of first generation migrants: a systematic-narrative review of reviews. Globalization and Health 12, 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coid JW, Kirkbride JB, Barker D, Cowden F, Stamps R, Yang M and Jones PB (2008) Raised incidence rates of all psychoses among migrant groups: findings from the East London first episode psychosis study. Archives of General Psychiatry 65, 1250–1258. [DOI] [PubMed] [Google Scholar]
- Colvert E, Rutter M, Kreppner J, Beckett C, Castle J, Groothues C, Hawkins A, Stevens S and Sonuga-Barke EJS (2008) Do theory of mind and executive function deficits underlie the adverse outcomes associated with profound early deprivation?: Findings from the English and Romanian Adoptees Study. Journal of Abnormal Child Psychology 36, 1057–1068. [DOI] [PubMed] [Google Scholar]
- Dalman C, Broms J, Cullberg J and Allebeck P (2002) Young cases of schizophrenia identified in a national inpatient register. Social Psychiatry and Psychiatric Epidemiology 37, 527–531. [DOI] [PubMed] [Google Scholar]
- Dunayevich E and Keck PE (2000) Prevalence and description of psychotic features in bipolar mania. Current Psychiatry Reports 2, 286–290. [DOI] [PubMed] [Google Scholar]
- Fearon P and Morgan C (2006) Environmental factors in schizophrenia: the role of migrant studies. Schizophrenia Bulletin 32, 405–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fearon P, Kirkbride JB, Morgan C, Dazzan P, Morgan K, Lloyd T, Hutchinson G, Tarrant J, Fung WLA, Holloway J, Mallett R, Harrison G, Leff J, Jones PB and Murray RM (2006) Incidence of schizophrenia and other psychoses in ethnic minority groups: results from the MRC AESOP Study. Psychological Medicine 36, 1541–1550. [DOI] [PubMed] [Google Scholar]
- Garety P, Kuipers E, Fowler D, Freeman D and Bebbington P (2001) A cognitive model of the positive symptoms of psychosis. Psychological Medicine 31, 189–195. [DOI] [PubMed] [Google Scholar]
- Glahn DC, Bearden CE, Barguil M, Barrett J, Reichenberg A, Bowden CL, Soares JC and Velligan DI (2007) The neurocognitive signature of psychotic bipolar disorder. Biological Psychiatry 62, 910–916. [DOI] [PubMed] [Google Scholar]
- Goodwin F and Jamison K (1990) Manic Depressive Illness. New York: Oxford University Press. [Google Scholar]
- Goodwin GM, Martinez-Aran A, Glahn DC and Vieta E (2008) Cognitive impairment in bipolar disorder: neurodevelopment or neurodegeneration? An ECNP expert meeting report. European Neuropsychopharmacology 18, 787–793. [DOI] [PubMed] [Google Scholar]
- Green MF (2006) Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. Journal of Clinical Psychiatry 67, 3–8. [PubMed] [Google Scholar]
- Hickling FW, Mckenzie K, Mullen R and Murray R (1999) A Jamaican psychiatrist evaluates diagnoses at a London psychiatric hospital. British Journal of Psychiatry 175, 283–285. [DOI] [PubMed] [Google Scholar]
- Hill S, Reilly J, Keefe R, Gold J, Bishop J, Gershon E, Tamminga C, Pearlson G, Keshavan M and Sweeney J (2013) Neuropsychological impairments in schizophrenia and psychotic bipolar disorder: findings from the Bipolar and Schizophrenia Network on Intermediate Phenotypes (B-SNIP) Study. The American Journal of Psychiatry 170, 1275–1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogerzeil SJ, van Hemert AM, Rosendaal FR, Susser E and Hoek HW (2014) Direct comparison of first-contact versus longitudinal register-based case finding in the same population: early evidence that the incidence of schizophrenia may be three times higher than commonly reported. Psychological Medicine 44, 3481–3490. [DOI] [PubMed] [Google Scholar]
- Hollander A-C, Dal H, Lewis G, Magnusson C, Kirkbride JB and Dalman C (2016) Refugee migration and risk of schizophrenia and other non-affective psychoses: cohort study of 1.3 million people in Sweden. BMJ 352, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapur S (2003) Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. American Journal of Psychiatry 160, 13–23. [DOI] [PubMed] [Google Scholar]
- Kirkbride JB (2017) Migration and psychosis: our smoking lung? World Psychiatry 16, 119–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkbride JB, Fearon P, Morgan C, Dazzan P, Morgan K, Tarrant J, Lloyd T, Holloway J, Hutchinson G, Leff JP, Mallett RM, Harrison GL, Murray RM and Jones PB (2006) Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings from 3-center AESOP study. Archives of General Psychiatry 63, 250–258. [DOI] [PubMed] [Google Scholar]
- Kirkbride JB, Barker D, Cowden F, Stamps R, Yang M, Jones PB and Coid JW (2008) Psychoses, ethnicity and socio-economic status. British Journal of Psychiatry 193, 18–24. [DOI] [PubMed] [Google Scholar]
- Kirkbride JB, Errazuriz A, Croudace T, Morgan C, Jackson D, McCrone P, Murray R and Jones P (2012a) Systematic Review of the Incidence and Prevalence of Schizophrenia and Other Psychoses in England. London: Department of Health Policy Research Programme. [Google Scholar]
- Kirkbride JB, Errazuriz A, Croudace TJ, Morgan C, Jackson D, Boydell J, Murray RM and Jones PB (2012b) Incidence of schizophrenia and other psychoses in England, 1950-2009: a systematic review and meta-analyses. PloS ONE 7, e31660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkbride JB, Hameed Y, Ankireddypalli G, Ioannidis K, Crane CM, Nasir M, Kabacs N, Metastasio A, Jenkins O, Espandian A, Spyridi S, Ralevic D, Siddabattuni S, Walden B, Adeoye A, Perez J and Jones PB (2017a) The epidemiology of first-episode psychosis in early intervention in psychosis services: Findings From the Social Epidemiology of Psychoses in East Anglia [SEPEA] Study. American Journal of Psychiatry 147, 143–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkbride JB, Hameed Y, Ioannidis K, Ankireddypalli G, Crane CM, Nasir M, Kabacs N, Metastasio A, Jenkins O, Espandian A, Spyridi S, Ralevic D, Siddabattuni S, Walden B, Adeoye A, Perez J and Jones PB (2017b) Ethnic minority status, age-at-immigration and psychosis risk in rural environments: evidence from the SEPEA Study. Schizophrenia Bulletin 43, 1251–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopmans GT, Uiters E, Devillé W and Foets M (2012) The use of outpatient mental health care services of migrants vis-à-vis Dutch natives: equal access? International Journal of Social Psychiatry 59, 342–350. [DOI] [PubMed] [Google Scholar]
- Lewis G, Croft-Jeffreys C and David A (1990) Are British psychiatrists racist? British Journal of Psychiatry 157, 410–415. [DOI] [PubMed] [Google Scholar]
- Lloyd T, Kennedy N, Fearon P, Kirkbride J, Mallett R, Leff J, Holloway J, Harrison G, Dazzan P, Morgan K, Murray RM and Jones PB (2005) Incidence of bipolar affective disorder in three UK cities: results from the ÆSOP study. British Journal of Psychiatry 186, 126–131. [DOI] [PubMed] [Google Scholar]
- MacCabe JH, Lambe MP, Cnattingius S, Sham PC, David AS, Reichenberg A, Murray RM and Hultman CM (2010) Excellent school performance at age 16 and risk of adult bipolar disorder: national cohort study. British Journal of Psychiatry 196, 109–115. [DOI] [PubMed] [Google Scholar]
- Maggioni E, Altamura AC and Brambilla P (2017) Exploring the neuroanatomical bases of psychotic features in bipolar disorder. Epidemiology and Psychiatric Sciences 26, 358–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray RM, Sham P, Van Os J, Zanelli J, Cannon M and McDonald C (2004) A developmental model for similarities and dissimilarities between schizophrenia and bipolar disorder. Schizophrenia Research 71, 405–416. [DOI] [PubMed] [Google Scholar]
- Ødegaard Ø (1932) Emigration and insanity. Acta Psychiatrica Neurologica (Supp.), 4, 1–206. [Google Scholar]
- OECD (2017) Foreign-born employment (indicator). doi: 10.1787/05428726-en (Accessed on 12 November 2017). [DOI]
- Patel V and Goodman A (2007) Researching protective and promotive factors in mental health. International Journal of Epidemiology 36, 703–707. [DOI] [PubMed] [Google Scholar]
- Pedersen CB and Cantor-Graae E (2012) Age at migration and risk of schizophrenia among immigrants in Denmark: a 25-year incidence study. The American Journal of Psychiatry 169, 1117–1118. [DOI] [PubMed] [Google Scholar]
- Perner J and Lang B (1999) Development of theory of mind and executive control. Trends in Cognitive Science 3, 337–344. [DOI] [PubMed] [Google Scholar]
- Pignon B, Alexis Geoffroy P, Thomas P, Roelandt JL, Rolland B, Morgan C, Vaiva G and Amad A (2017) Prevalence and clinical severity of mood disorders among first-, second- and third-generation migrants. Journal of Affective Disorders 210, 174–180. [DOI] [PubMed] [Google Scholar]
- Reichenberg A, Weiser M, Rabinowitz J, Caspi A, Schmeidler J, Mark M, Kaplan Z and Davidson M (2002) A population-based cohort study of premorbid intellectual, language, and behavioral functioning in patients with schizophrenia, schizoaffective disorder, and nonpsychotic bipolar disorder. Psychiatry: Interpersonal and Biological Processes 159, 2027–2035. [DOI] [PubMed] [Google Scholar]
- Reininghaus U, Kempton MJ, Valmaggia L, Craig TKJ, Garety P, Onyejiaka A, Gayer-Anderson C, So SH, Hubbard K, Beards S, Dazzan P, Pariante C, Mondelli V, Fisher HL, Mills JG, Viechtbauer W, McGuire P, van Os J, Murray RM, Wykes T, Myin-Germeys I and Morgan C (2016) Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: an experience sampling study. Schizophrenia Bulletin 42, sbv190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roiser JP, Stephan KE, den Ouden HEM, Barnes TRE, Friston KJ and Joyce EM (2009) Do patients with schizophrenia exhibit aberrant salience? Psychological medicine 39, 199–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal D, Goldberg I, Jacobsen B, Wender P, Kety S, Schulsinger F and Eldred C (1974) Migration, heredity, and schizophrenia. Psychiatry 37, 321–339. [DOI] [PubMed] [Google Scholar]
- Rothmond DA, Weickert CS and Webster MJ (2012) Developmental changes in human dopamine neurotransmission: cortical receptors and terminators. BMC Neuroscience 13, 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz RC and Blankenship DM (2014) Racial disparities in psychotic disorder diagnosis: a review of empirical literature. World Journal of Psychiatry 4, 133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selemon LD and Zecevic N (2015) Schizophrenia: a tale of two critical periods for prefrontal cortical development. Translational Psychiatry 5, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selten JP, Cantor-Graae E, Slaets J and Kahn RS (2002) Ødegaard's selection hypothesis revisited: schizophrenia in Surinamese immigrants to the Netherlands. American Journal of Psychiatry 159, 669–671. [DOI] [PubMed] [Google Scholar]
- Selten JP, Laan W, Veen ND, Blom JD, Veling W and Hoek HW (2010) Incidence of schizophrenia among Moroccan immigrants to the Netherlands. Schizophrenia Research 124, 240–241. [DOI] [PubMed] [Google Scholar]
- Swinnen S and Selten J-P (2007) Mood disorders and migration. British Journal of Psychiatry 190, 6–10. [DOI] [PubMed] [Google Scholar]
- Trotta A, Murray RM and MacCabe JH (2014) Do premorbid and post-onset cognitive functioning differ between schizophrenia and bipolar disorder? A systematic review and meta-analysis. Psychological Medicine 45, 381–394. [DOI] [PubMed] [Google Scholar]
- van der Ven E, Dalman C, Wicks S, Allebeck P, Magnusson C, van Os J and Selten JP (2015) Testing Ødegaard's selective migration hypothesis: a longitudinal cohort study of risk factors for non-affective psychotic disorders among prospective emigrants. Psychological Medicine 45, 727–34. [DOI] [PubMed] [Google Scholar]
- Veling W, Hoek HW, Selten J-P and Susser E (2011) Age at migration and future risk of psychotic disorders among immigrants in the Netherlands: a 7-year incidence study. The American Journal of Psychiatry 168, 1278–1285. [DOI] [PubMed] [Google Scholar]
- Vreeker A, Boks MPM, Abramovic L, Verkooijen S, van Bergen AH, Hillegers MHJ, Spijker AT, Hoencamp E, Regeer EJ, Riemersma-Van der Lek RF, Stevens AWMM, Schulte PFJ, Vonk R, Hoekstra R, van Beveren NJM, Kupka RW, Brouwer RM, Bearden CE, MacCabe JH and Ophoff RA (2016) High educational performance is a distinctive feature of bipolar disorder: a study on cognition in bipolar disorder, schizophrenia patients, relatives and controls. Psychological Medicine 46, 807–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandi T, Havenaar JM, Smits M, Limburg-Okken AG, van Es H, Cahn W, Algra A, Kahn RS and van den Brink W (2010) First contact incidence of psychotic disorders among native Dutch and Moroccan immigrants in the Netherlands: influence of diagnostic bias. Schizophrenia Research 119, 27–33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0033291718003227.
click here to view supplementary material