Key Points
Question
Is there an increase in mental health service use after bariatric surgery?
Findings
In this cohort study, over a 10-year study period, 1 in 6 patients undergoing bariatric surgery (16.7%) used at least 1 perioperative episode of a mental health service. Compared with before surgery, outpatient, emergency department, and inpatient psychiatric presentations were all significantly more common after surgery.
Meaning
The current professional bariatric surgery guidelines recommending preoperative psychological assessments and the deferment of surgery in patients with active psychiatric conditions may be either ineffectual or inconsistently adhered to, and patients should be routinely assessed and informed preoperatively about the potential associations of bariatric surgery with mental health outcomes.
Abstract
Importance
Obesity is associated with an increased prevalence of psychiatric disorders. The association of bariatric surgery with mental health outcomes is poorly understood.
Objective
To investigate the association of bariatric surgery with the incidence of outpatient, emergency department (ED), and inpatient mental health service use.
Design, Setting, and Participants
This statewide, mirror-image, longitudinal cohort study used data from Western Australian Department of Health Data Linkage Branch records from all patients undergoing index (ie, first) bariatric surgery in Western Australia over a 10-year period (January 2007-December 2016), with mean (SD) follow-up periods of 10.2 (2.9) years before and 5.2 (2.9) years after index bariatric surgery. The data analysis was performed between November 2018 and March 2019.
Exposures
Index bariatric surgery.
Main Outcomes and Measures
The incidence and predictors for mental health presentations, deliberate self-harm, and suicide in association with the timing of bariatric surgery.
Results
A total of 24 766 patients underwent index bariatric surgery; of these, the mean (SD) age was 42.5 (11.7) years and 19 144 (77.3%) were women. Use of at least 1 mental health service occurred in 3976 patients (16.1%), with 1401 patients (35.2%) presenting only before surgery, 1025 (25.8%) presenting before and after surgery, and 1550 patients (39.0%) presenting only after surgery. There was an increase in psychiatric illness presentations after bariatric surgery (outpatient clinic attendance: incidence rate ratio [IRR], 2.3; 95% CI, 2.3-2.4; ED attendance: IRR, 3.0; 95% CI, 2.8-3.2; psychiatric hospitalization: IRR, 3.0; 95% CI, 2.8-3.1). There was also a 5-fold increase in deliberate self-harm presentations to an ED after surgery (IRR, 4.7; 95% CI, 3.8-5.7), with 25 of 261 postoperatives deaths (9.6%) due to suicide. Complications after bariatric surgery requiring further surgical intervention and a history of mental health service provision before surgery were the most important associations with subsequent mental health presentations after surgery. Deliberate self-harm and mental and behavioral disorders due to psychoactive substance use before bariatric surgery were the main associations with subsequent deliberate self-harm or suicide after surgery.
Conclusions and Relevance
We observed an increase in mental health service presentations after bariatric surgery, particularly among those who had prior psychiatric illnesses or developed surgical complications requiring further surgery. These findings caution the hypothesis that weight reduction by bariatric surgery will improve mental health in patients with obesity.
This longitudinal cohort study examines the association of bariatric surgery with the incidence of outpatient, emergency department, and inpatient mental health service use in Western Australia.
Introduction
The association between excess weight gain and mental health is complex and likely involves many genetic, hormonal, social, and environmental factors. Obesity has been causally linked to body dissatisfaction, low self-esteem, and depression; conversely, psychiatric conditions are associated with the onset of weight gain.1,2,3 Individuals with obesity are often stigmatized, facing social exclusion and discrimination,4 while the codiagnoses of obesity and mental health appear to propagate physical illness.5 Given that obesity (31.3%) and psychiatric conditions (20.1%) are prevalent in Australia and many other countries,6 an effective weight loss strategy could affect these 2 major health issues for millions of people.
Bariatric surgery, first conceived in the 1950s, has become an increasingly common procedure in the last 2 decades, with a growing number of studies confirming its safety and long-term effectiveness in reducing body weight.7,8,9 However, several recent studies have highlighted a concern that bariatric surgery may exacerbate psychiatric conditions,3,10,11,12 especially deliberate self-harm (DSH) and suicide.13 In response to this, major professional bariatric societies currently recommend that potential surgical candidates should have either no active severe pyschopathology or drug dependency problems and/or have undergone psychological assessment before surgery.14,15,16,17 However, how bariatric surgery is associated with broader mental health outcomes remains poorly understood.
We hypothesized that bariatric surgery may exacerbate comorbid psychiatric conditions, resulting in an increased requirement for mental health services after surgery, including for those without prior psychiatric illnesses. This study assessed the incidence and risk factors for mental health service use after bariatric surgery, including psychiatric outpatient clinic (OPC) care and emergency department (ED) presentation or hospitalization, stratified by different types of psychiatric conditions.
Methods
Study Design and Setting
This was a population-based, retrospective, longitudinal, mirror-image cohort study including all patients who underwent index (ie, first) elective bariatric surgery in private and public health care institutions during a 10-year period between 2007 and 2016 in Western Australia. The start point of the studied period was chosen based on the rapid increase in bariatric procedures from 24.4 bariatric surgical procedures per 100 000 person-years in 2004 to 94.4 bariatric surgical procedures per 100 000 person-years by 2007.18 The longitudinal, mirror-image design allowed for an incidence comparison between mental health use before and after bariatric surgery while minimizing the confounding association of important patient characteristics, such as sex and medical comorbidities. Comorbid data were collected from January 2002, guaranteeing a minimum 5-year preoperative observation period, with a final censor date of June 1, 2017, unless the patients died earlier, ensuring a minimum postoperative follow-up observation period of 5 months for all study patients after their index bariatric surgery. Western Australia had a population of 2.39 million in 2011, comprising 10.4% of the total Australian population with an emigration rate of less than 1.2%.19
Data Sources
The Western Australian Department of Health Data Linkage Branch systematically links and updates the administrative private and public health care data for the entire state of Western Australia by merging data from 8 independent statewide data registries, including the birth records, private and public hospitalization data, cancer registry, ED presentations, public OPC and inpatient psychiatric services data, death registry, midwives’ notifications, and the Western Australian electoral roll.20,21 In this study, patients who had their index bariatric surgery in Western Australia were first identified from the private and public hospitalization data set. Their corresponding mental health data were obtained through the ED presentation data set and the inpatient and public OPC mental health services data sets. The medical comorbidities and survival data were obtained from the private and public hospitalization data set and death registry, respectively. The accuracy of this process has previously been validated,21 with successful completion of multiple population-based studies.9,18 The incidence of suicide in the study cohort was compared with the general population in Western Australia using data from the Western Australia Mental Health Commission.22 Ethics approval, including a waiver of consent, was obtained from the authors’ home institution, St John of God Subiaco Hospital, and the Western Australian Department of Health Human Research ethics committees before the deidentified data, with diagnoses, procedures, and causes of death coded according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) system, was released to the study investigators.
Participants
In this study, only patients who had their index bariatric surgery in Western Australia during the study period were included. The presence or absence and also the incidence of mental health use requiring psychiatric OPC or ED attendance and hospitalization before and after the index bariatric surgical hospitalization were determined.
Patients were identified using a preexisting Data Linkage Branch “bariatric panel” of ICD-10 procedural codes (eTable 1 in the Supplement). Before July 2013 there were limited procedure-specific codes for bariatric surgery in Australia making the distinction between certain types of bariatric surgery difficult. The codes were expanded after July 2013 to better define specific bariatric procedures. Psychiatric illnesses in this study were identified and grouped using the following ICD-10 codes and are listed in eTable 2 in the Supplement.
Patients were excluded if they had bariatric surgery before January 2007 or their first bariatric surgery during the study period was already a bariatric revision procedure, indicating that bariatric surgery captured during the study period was preceded by another bariatric surgery performed before 2007 or outside Western Australia. Missing psychiatric diagnostic data occurred for 174 hospitalizations and OPC presentations (<1%) and 9064 (36.6%) for ED presentations.
Variables and Outcomes
The primary outcome was the incidence of mental health service use, including psychiatric OPC attendance, ED presentations with a psychiatric diagnosis, and inpatient hospitalizations because of a psychiatric disorder before and after each index bariatric surgery. Secondary outcomes were the incidence of patients presenting to the ED for suicidal ideation or DSH and incidence of completed suicide after bariatric surgery.
Statistical Analysis
The incidence of psychiatric OPC or ED presentations and hospitalizations was reported as the number of events per 10 000 patient years. The difference in incidence rates of these psychiatric presentations before and after surgery was reported as incidence rate ratios (IRRs) and its statistical significance was analyzed using the Wilcoxon signed rank test. The mirror-image design was used to minimize confounding, and IRR was used to account for the variable follow-up periods before and after surgery for each patient. Because suicide was a rare occurrence, suicide rates were reported in number of events per 100 000 person-years with subsequent sex standardization.
A multivariable logistic regression was used to assess the determinants of postoperative mental health service use, DSH, and suicide after bariatric surgery. These multivariate models initially included biologically plausible risk factors for mental health service use in addition to the calendar year of the index procedure and follow-up duration. Covariates with a P value of more than .25 were then removed in a stepwise fashion, starting with covariates with the largest P value, to generate a parsimony model to improve the precision of the results. The strength of the predictors was reflected by the magnitude of the adjusted odds ratio (aOR) for ordinal dependent variables and a linear regression for continuous dependent variables. Imputation was not used to replace missing data. All statistical tests were 2-tailed and performed using SPSS, version 23.0 (IBM Corp). Statistical significance was set at P < .05.
Results
Patient Characteristics
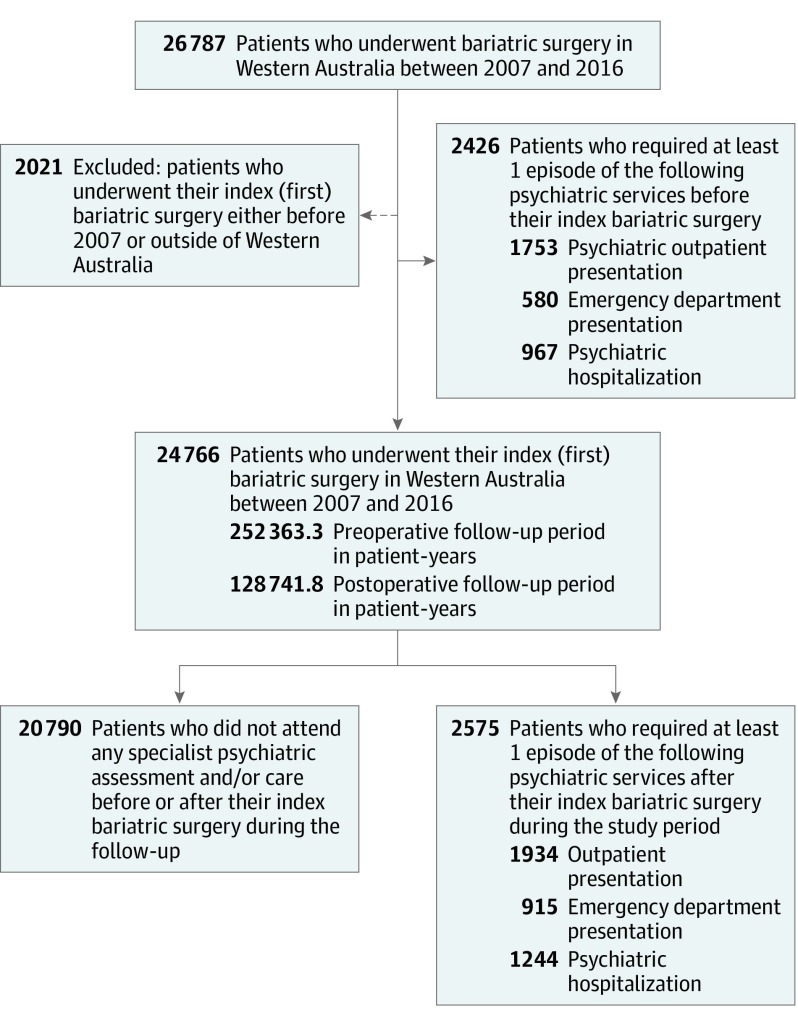
Of the 26 787 patients who underwent any bariatric surgical procedure in Western Australia between 2007 and 2016, 24 766 (92.5%) had their index bariatric surgery during the study period (Figure). The mean (SD) age of patients at the time of their index bariatric surgery was 42.5 (11.7) years and 19 144 (77.3%) were women. Most of the index bariatric surgery was performed in a private metropolitan hospital (22 515 [90.9%]); only 1886 bariatric procedures (7.6%) were performed in a rural hospital. The total follow-up time for the whole cohort was 252 363.3 patient-years before surgery (mean [SD] 10.2 [2.9] years per patient) and 128 741.8 patient-years after surgery (mean [SD] 5.2 [2.9] years per patient). A total of 5001 study patients (20.2%) had 1 or more subsequent bariatric procedures after their index bariatric surgery during the study period.
Figure. Mental Health Service Use Matrix Before and After Index Bariatric Surgery.
Patients often used more than 1 mental health service.
Overview of Mental Health Service Use
During the study period, 3976 patients (16.1%) presented on at least 1 occasion to a psychiatric service; of these, 1401 (35.2%) attended such services only in the preoperative period, 1025 (25.8%) attended psychiatric services before and after index bariatric surgery, and 1550 (6.9% of all patients who did not have any documented psychiatric illness before surgery) first attended a psychiatric service only after surgery. Overall, approximately 2575 patients (10%) required at least 1 episode of mental health services after their surgery. Table 1 outlines the number of patients who used different types of mental health services either before, after, or before and after surgery. There was a significant increase in the number of patients who underwent bariatric surgery who attended, one form or another, a mental health service after surgery compared with before surgery (39% vs 35.2%; Wilcoxon signed rank test: P = .006).
Table 1. Number of Patients Among 24 766 Participants Who Attended Different Modes of Psychiatric Services Before and After Their Index Bariatric Surgery Between 2007 and 2016.
| Characteristic | No. (%) | |||
|---|---|---|---|---|
| Patients With Their Only Psychiatric Presentations Before Index Bariatric Surgery | Patients With Psychiatric Presentations Before and After Index Bariatric Surgery | Patients With Their First Psychiatric Presentations After Index Bariatric Surgery | No. of Patients With Psychiatric Presentations | |
| Psychiatric outpatient clinic presentationsa | 1026 (34.7) | 727 (24.5) | 1207 (40.8) | 2960 (100) |
| Emergency department psychiatric presentationsa | 472 (34.0) | 108 (7.8) | 807 (58.2) | 1387 (100) |
| Hospitalizations for a psychiatric diagnosisa | 596 (32.4) | 371 (20.2) | 873 (47.4) | 1840 (100) |
| Any form of psychiatric servicesb | 1401c (35.2) | 1025 (25.8) | 1550c (39.0) | 3976 (100) |
Percentages refer to the proportion of patients presenting for psychiatric review based on setting (ie, outpatient, emergency department, or inpatient).
Patients using more than 1 mode of mental health service are only counted once.
Wilcoxon signed rank test comparing isolated preindex bariatric surgery psychiatric presentations (column 1) against patients with their first psychiatric presentations after index bariatric surgery (column 3), P = .006.
Incidence of Different Mental Health Conditions Requiring Mental Health Services
We observed an increase in the incidence of mental health service use across all 3 major types of mental health services and for all psychiatric conditions (IRR ranged between 1.3 and 7.7). Table 2 outlines the number of patients with different types of psychiatric conditions and the associated incidence of mental health use before and after their index bariatric surgery and then stratifies them by the 3 major types of mental health service (psychiatric OPC, ED attendance, or psychiatric inpatient hospitalization). To minimize confounding from changes in practice, regression toward the mean, confounding by indication, or bias from aging, we conducted 2 sensitivity analyses. Restricting our analysis to either the central years of 2009 and 2010 or to patients with a maximum 24-month follow-up (eTable 3 in the Supplement) did not change the association between bariatric surgery and increased postoperative mental health service use.
Table 2. Incidence Rate Ratios for Different Psychiatric Diagnoses Requiring Either Outpatient, ED, or Hospitalization Services Before and After Index Bariatric Surgerya Between 2007 and 2016b Among 24 766 Patients.
| Psychiatric Diagnosis or Symptomatic Presentation | Before Index Bariatric Surgery | After Index Bariatric Surgery | Incidence Rate Ratio (95% CI)c | ||||
|---|---|---|---|---|---|---|---|
| Patients, No. | Presentations or Hospitalization, No. | Presentation Rate, per 10 000 Patient-Years | Patients, No. | Presentations or Hospitalization, No. | Presentation Rate, per 10 000 Patient-Years | ||
| Outpatient Clinic Presentationsd | |||||||
| Organic disorders | 10 | 80 | 3.2 | 21 | 315 | 24.5 | 7.7 (6.0-9.9) |
| Mental and behavioral disorders due to psychoactive substance use | 55 | 364 | 14.4 | 77 | 824 | 64.0 | 4.4 (3.9-5.0) |
| Schizophrenia-like disorders | 76 | 6640 | 263.1 | 89 | 8235 | 639.7 | 2.4 (2.4-2.5) |
| Mood disorders | 564 | 16 396 | 649.7 | 639 | 18 727 | 1455.0 | 2.2 (2.2-2.3) |
| Neurotic disorders | 316 | 5450 | 216.0 | 418 | 7533 | 585.1 | 2.7 (2.6-2.8) |
| Behavioral disorders | 49 | 901 | 35.7 | 30 | 608 | 47.2 | 1.3 (1.2-1.5) |
| Personality disorders | 130 | 8584 | 340.1 | 185 | 9230 | 716.9 | 2.1 (2.0-2.2) |
| Psychological development disorders | 0 | 0 | 0.0 | 2 | 41 | 3.2 | Not able to be estimated |
| Unspecified disorders | 25 | 854 | 33.8 | 19 | 705 | 54.8 | 1.6 (1.5-1.8) |
| Psychiatric evaluation/examination | 51 | 370 | 14.7 | 49 | 758 | 58.9 | 4.0 (3.5-4.5) |
| No recorded diagnosis | 734 | 2088 | 82.7 | 809 | 2874 | 223.2 | 2.7 (2.6-2.8) |
| Total | 1753e | 41 727 | 1653.0 | 1934e | 49 850 | 3872.0 | 2.3 (2.3-2.4) |
| ED Presentationsf | |||||||
| Drug and alcohol overdoses | 289 | 515 | 20.4 | 399 | 589 | 45.8 | 2.2 (2.0-2.5) |
| Psychotic disorders | 19 | 32 | 1.3 | 33 | 49 | 3.8 | 3.0 (1.9-4.7) |
| Mood disorders | 107 | 134 | 5.3 | 133 | 156 | 12.1 | 2.3 (1.8-2.9) |
| Neurotic disorders | 59 | 67 | 2.7 | 136 | 170 | 13.2 | 5.0 (3.7-6.6) |
| Behavioral disorders | 92 | 130 | 5.2 | 138 | 180 | 14.0 | 2.7 (2.2-3.4) |
| Personality disorders | 35 | 35 | 1.4 | 66 | 68 | 5.3 | 3.8 (2.5-5.7) |
| Deliberate self-harm | 73 | 115 | 4.6 | 117 | 162 | 12.6 | 2.8 (2.2-3.5) |
| Suicidal ideation | 85 | 119 | 4.7 | 258 | 425 | 33.0 | 7.0 (5.7-8.6) |
| Nonspecific psychiatric | 60 | 85 | 3.4 | 80 | 100 | 7.8 | 2.3 (1.7-3.1) |
| Requesting psychiatric review | 44 | 58 | 2.3 | 59 | 79 | 6.1 | 2.7 (1.9-3.7) |
| Total | 580e | 1290 | 51.1 | 915e | 1978 | 153.6 | 3.0 (2.8-3.2) |
| Hospitalizationsc | |||||||
| Mental and behavioral disorders due to psychoactive substance use | 202 | 438 | 17 | 405 | 1017 | 79 | 4.6 (4.1-5.1) |
| Schizophrenia-like disorders | 62 | 189 | 7 | 76 | 319 | 25 | 3.3 (2.8-4.0) |
| Mood disorders | 621 | 1710 | 68 | 765 | 2431 | 189 | 2.8 (2.6-3.0) |
| Neurotic disorders | 539 | 1111 | 44 | 728 | 1578 | 123 | 2.8 (2.6-3.0) |
| Behavioral disorders | 21 | 28 | 1 | 41 | 62 | 5 | 4.3 (2.8-6.8) |
| Personality disorders | 142 | 516 | 2 | 193 | 605 | 47 | 2.3 (2.0-2.6) |
| Total | 967e | 3992 | 158 | 1244e | 6012 | 467 | 3.0 (2.8-3.1) |
Abbreviation: ED, emergency department.
Index bariatric surgery refers to the original bariatric surgery occurring between 2007 and 2016.
Follow-up periods: 252 363.3 patient-years before index bariatric cases and 128 741.8 patient-years after index bariatric surgery.
Comparison made between prior and post–bariatric surgery psychiatric presentation or hospitalization rates.
Based on International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes.
Patients with multiple psychiatric presentations are only counted once.
Based on the Department of Health Emergency Department Information System.
There was an increasing trend of outpatient mental health services use after the first bariatric surgery for those who did not have any psychiatric health history in recent years (7.9-16.0 new patients per 1000 patient-years), whereas the incidence of psychiatric ED presentations and hospitalizations appeared to be relatively stable across the 10-year period (eFigure in the Supplement).
Determinants of Requiring Mental Health Services Before Bariatric Surgery in Those Without Any Prior Mental Health Condition
Table 3 outlines the factors for patients who required different types of mental health services for the first time after bariatric surgery. A prior preoperative presentation to one type of psychiatric service was the strongest predictor for requiring other types of psychiatric services after surgery (aOR ranged between 1.62 and 3.73). Apart from young age, surgical complications after the index bariatric surgery requiring further surgical interventions was the only factor consistently associated with an increased risk of requiring, in one form or another, mental health services after surgery (aOR ranged between 1.23 and 1.45). In a secondary analysis using a linear regression to assess the determinants associated with an increasing number of first-time psychiatric presentations after bariatric surgery, patient age, prior presentation to an alternative mental health service, and reoperation for bariatric complications were all significant risk factors for requiring more psychiatric services after the index bariatric surgery (eTable 4 in the Supplement).
Table 3. Multivariate Logistic Regression With Backward Elimination Showing Factors Associated With First-Time Mental Health Presentations Following Index Bariatric Surgery Between 2007 and 2016a.
| Characteristic | OR (95% CI) | ||
|---|---|---|---|
| First-Time Psychiatric OPC Presentation After Bariatric Surgery (n = 1207) | First-Time Psychiatric ED Presentation After Bariatric Surgery (n = 807) | First-Time Psychiatric Hospitalization After Bariatric Surgery (n = 873) | |
| Demographics | |||
| Age, per year | 0.97 (0.96-0.98) | 0.97 (0.96-0.97) | 0.99 (0.98-0.99) |
| Sex, male | Excluded P > .25 | 1.27 (1.06-1.52) | 1.22 (1.03-1.44) |
| Private health insurance | 1.49 (1.29-1.72) | 1.40 (1.17-1.67) | 1.14 (0.96-1.36) |
| Charlson comorbidity score ≥1 | 1.19 (1.00-1.42) | Excluded P > .25 | 1.21 (1.00-1.47) |
| Index surgery undertaken at a rural hospital | Excluded P > .25 | 1.34 (1.03-1.74) | Excluded P > .25 |
| SEIFA LGA IRSD 2011 disadvantage score, per increasing decileb | 0.95 (0.93-0.98) | 1.06 (1.02-1.10) | 1.06 (1.02-1.09) |
| Preoperative psychiatric history | |||
| Pre–index surgery psychiatric OPC presentation | NA | 2.97 (2.41-3.67) | 2.60 (2.13-3.17) |
| Pre–index surgery psychiatric ED presentation | 1.58 (1.15-2.17) | NA | 2.83 (2.09-3.82) |
| Pre–index surgery psychiatric hospitalization | 1.62 (1.28-2.07) | 3.73 (2.95-4.71) | NA |
| Surgical factors | |||
| Index surgery, gastric bandc | 1.26 (0.82-1.93) | 1.18 (0.71-1.98) | 1.13 (0.68-1.90) |
| Index surgery, sleeve gastrectomyc | 1.65 (1.15-2.37) | 1.38 (0.88-2.16) | 1.32 (0.85-2.06) |
| Index surgery, bypass procedurec | 1.95 (0.98-3.87) | 1.02 (0.34-3.00) | 3.02 (1.50-6.06) |
| Repeated bariatric surgery, obesity onlyd | 1.38 (0.99-1.90) | 0.62 (0.36-1.06) | 1.62 (1.13-2.33) |
| Repeated bariatric surgery, complication onlyd | 1.23 (1.03-1.47) | 1.43 (1.17-1.75) | 1.45 (1.19-1.76) |
| Repeated bariatric surgery, complication and obesityd | 1.18 (0.97-1.44) | 1.07 (0.84-1.37) | 1.56 (1.26-1.94) |
Abbreviations: ED, emergency department; IRSD, The Index of Relative Socio-Economic Disadvantage, LGA, local government area; NA, not applicable; OPC, outpatient clinic; OR, odds ratio; SEIFA, Socio-Economic Indexes for Areas.
Total cohort size = 24 766 patients undergoing bariatric surgery with the multivariate logistic regression adjusted for year of surgery and duration of follow-up.
The IRSD is a general socioeconomic index that summarizes a range of information about the economic and social conditions of people and households within an area. This index includes only measures of relative disadvantage, with lower scores equating with increasing disadvantage. The average IRSD equals 1000 and roughly two-thirds of the scores lie between 900 and 1100.
When compared with the remaining bariatric surgery group of restrictive procedures.
When compared with patients not requiring repeated bariatric procedures.
Determinants of Deliberate Self-harm, Suicidal Ideation, and Suicide After Bariatric Surgery
A total of 333 patients undergoing bariatric surgery presented to an ED with DSH or suicidal ideation after their index bariatric surgery, and the incidence rate of these psychiatric conditions was significantly higher after surgery compared with before surgery (IRR, 4.7; 95% CI, 3.8-5.7). Patients who were younger (aOR, 0.95 per year increment; 95% CI, 0.94-0.96), with a higher socioeconomic status (aOR, 1.06; 95% CI, 1.00-1.13), who had DSH or suicidal ideation, mental and behavioral disorders due to psychoactive substance use or mood disorders before their index bariatric surgery, and had a sleeve gastrectomy (aOR, 2.03; 95% CI, 1.00-4.11) or a bypass procedure (aOR, 3.62; 95% CI, 1.12-11.76) as their index bariatric procedure were significantly associated with an increased risk of DSH or suicidal ideation after their first bariatric surgery (Table 4).
Table 4. Logistic Regression Showing Risk Factors for 333 Patients Who Underwent Bariatric Surgery Presenting to an ED With Suicidal Ideation or DSH After Their Index Bariatric Procedure Between 2007 and 2016a.
| Characteristic | Univariate OR (95% CI) | P Value | Multivariate OR (95% CI)b | P Value |
|---|---|---|---|---|
| Demographics | ||||
| Age, per year | 0.95 (0.94-0.96) | <.001 | 0.95 (0.94-0.96) | <.001 |
| Sex, male | 0.89 (0.68-1.17) | .40 | NAc | NA |
| Private insurance | 1.57 (1.21-2.03) | .001 | 1.46 (1.12-1.92) | .06 |
| Charlson comorbidity index >0 | 1.23 (0.93-1.64) | .15 | 1.35 (0.98-1.85) | .07 |
| Index bariatric surgery undertaken at a rural hospital | 1.09 (0.74-1.62) | .66 | NAc | NA |
| SEIFA LGA IRSD, per increasing deciled | 1.05 (0.99-1.11) | .10 | 1.06 (1.00-1.13) | .04 |
| Preoperative psychiatric history | ||||
| Prior ED presentation with DSH or suicidal ideation | 14.58 (9.12-23.29) | <.001 | 4.84 (2.74-8.54) | <.001 |
| Prior hospitalization, DSHe | 16.55 (11.63-23.54) | <.001 | 2.42 (1.50-3.91) | <.001 |
| Prior hospitalization, mental disorders due to psychoactive substance usee | 15.74 (10.58-23.42) | <.001 | 2.75 (1.65-4.57) | <.001 |
| Prior hospitalization, mood disorderse | 12.88 (9.82-16.89) | <.001 | 5.89 (4.07-8.50) | <.001 |
| Surgical factors | ||||
| Type of operation, gastric bandf | 1.71 (0.79 -3.67) | .17 | 1.58 (0.71-3.52) | .26 |
| Type of operation, gastric sleevef | 1.64 (0.83-3.22) | .15 | 2.03 (1.00-4.11) | .05 |
| Type of operation, gastric bypassf | 2.82 (0.92-8.66) | .07 | 3.62 (1.12-11.76) | .03 |
| Repeated surgery, obesityg | 0.84 (0.39-1.80) | .65 | 0.68 (0.31-1.51) | .34 |
| Repeated surgery, complicationsg | 1.50 (1.11-2.03) | .09 | 1.30 (0.94-1.79) | .11 |
| Repeated surgery, obesity and complicationsg | 1.02 (0.69-1.52) | .91 | 0.77 (0.51-1.16) | .21 |
Abbreviations: DSH, deliberate self-harm; ED, emergency department; IRSD, Index of Relative Socio-Economic Disadvantage; LGA, local government area; NA, not applicable; OR, odds ratio; SEIFA, Socio-Economic Indexes for Areas.
Index procedure is when the original bariatric surgery occurred between 2007 and 2016. Total cohort size = 24 766 patients who underwent bariatric surgery.
Multivariate logistic regression adjusted for year of surgery and duration of follow-up.
Excluded in stepwise backward elimination.
The IRSD is a general socioeconomic index that summarizes a range of information about the economic and social conditions of people and households within an area. It includes only measures of relative disadvantage with lower deciles equating with increasing disadvantage.
Using International Statistical Classification of Diseases and Related Health Problems, Tenth Revision classifications.
When compared with the remaining bariatric surgery group of restrictive procedures.
When compared with patients not requiring repeated bariatric procedures.
Of 261 deaths recorded during the follow-up period after surgery, 25 patients (9.6%) committed suicide (95% CI, 6.0%-13.2%). The suicide rate after index bariatric surgery was 19.4 deaths per 100 000 patient-years. Women accounted for 15 suicides (15.0 deaths per 100 000 patient-years) and men for 10 suicides (35.1 deaths per 100 000 patient-years). The overall, male, and female standardized suicidal rates of the cohort were higher than the corresponding suicidal rates of the general population (13.5 per 100 000 person years), male (19.8 per 100 000 person years), and female (7.2 per 100 000 person years) suicide rates in Western Australia, respectively. Hospitalization because of a DSH (aOR, 5.34; 95% CI, 1.22-23.34) and mental and behavioral disorders due to psychoactive substance use (aOR, 4.69; 95% CI, 1.03-21.30) before patients’ index bariatric surgery were the only 2 factors significantly associated with an increased risk of suicide after surgery (eTable 5 in the Supplement).
Discussion
Although shown to be an effective method in achieving weight loss, controversy remains whether bariatric surgery may increase the risk of adverse mental health outcomes, including DSH.3,11,12,13,23 In this population-based statewide cohort study, we found that 1 in 6 patients (16.7%) had used at least 1 episode of a mental health service during the study period, with approximately 1 in 10 (10%) of all patients doing so after their first bariatric surgery. Mental health service use across 3 major types of mental health provisions increased significantly, and this remained consistent across all major psychiatric conditions. Furthermore, ED presentations because of DSH or suicidal ideation were also significantly increased after index bariatric surgery, with the overall suicide rate accounting for 10% of all deaths among patients who underwent bariatric surgery. These findings have important implications and require further discussion.
Potentially, some Australian bariatric surgeons may not be completely aware of, or hesitant to follow, the available guidelines that exist regarding the perioperative assessment of, and recommendations for, patients with prior psychiatric illness, instead believing that any successful reduction in body weight may outweigh any possible mental health harms.4,5 Our findings question this latter belief and support the peer-reviewed guidelines published by the American Society of Metabolic and Bariatric Surgery surrounding careful patient selection.16 In most cases, it would be recommended that patients with an active or recent history of severe psychopathology, compulsive behaviors, DSH, suicidal ideation, or mental and behavioral disorders due to psychoactive substance use be excluded or have their bariatric surgery postponed until the active psychiatric issues have been treated with a period of mental health stability.16 It therefore remains incumbent on all health care clinicians to integrate and communicate an agreed multidisciplinary, perioperative plan in patients with complex psychiatric conditions that prioritizes the ready postoperative access to mental health services.
Psychiatric conditions requiring different forms of mental health services were not uncommon in this study, including those without any prior documented psychiatric illnesses (1550 of 22 340 patients [6.9%]). An absence of well-documented psychiatric conditions before bariatric surgery does not therefore imply that these patients are not at risk of developing serious mental health conditions after surgery. Whether using a preoperative psychological assessment, as recommended by the current guidelines, can identify those at risk and improve their mental health outcomes, to our knowledge, remains scientifically unproven. Because surgical complications were associated with an increased incidence of mental health service use, mental health outcomes should thus be incorporated as one of the outcomes in future randomized clinical trials comparing the effectiveness of different types of bariatric procedures.
The heterogenous etiology of mental health disorders also means that the effect of bariatric surgery is unlikely to be uniform across different psychiatric diagnostic groupings. Perioperative analgesic and sedative drugs may potentiate the risk for organic disorders, whereas postoperative complications, such as sepsis, may precipitate or exacerbate anxiety, depression, or cognitive decline.24 With the increasing recognition that beyond the anatomical changes of bariatric surgery there are hormonal and microbiota changes that may partially contribute to mental health outcomes after surgery25,26,27; adequately powered randomized clinical trials are required to assess whether hormonal or microbiota optimization can improve patient-centered outcomes across diverse psychiatric conditions.
Strengths and Limitations
The strengths in this study lie in the robust source of the data and the ability to consider multiple modes of mental health presentations in the analysis. The limitations in this study include the possibility that some of the patients may have had mild mental health conditions that were solely managed by their family physicians or private psychiatrists and were not captured by this study. Alternatively, increased service use may represent greater scrutiny and closer follow-up in the postoperative period. This study was also beholden to the specifics of large administrational databases not explicitly designed for individual studies. As such, the data set relies on diagnostic coding rather than a criterion standard mental health diagnostic instrument and is devoid of useful variables, such as height and weight, and subject to a change in the Australian bariatric procedural codes in July 2013. Caution also needs to be exercised when assessing the suicide data in isolation. The absence of a control group and the relatively low overall incidence of suicide have limited our ability to determine the true risk and all the potential risk factors. Finally, we acknowledge that although our study used a state-wide administrational database, it was not a nation-wide study and we further caution the generalization of our findings to alternative health care systems and regions.
Conclusions
Over a mean (SD) follow-up period of 5 (2.9) years, 1 in 10 patients (10%) who underwent bariatric surgery used at least 1 episode of mental health care after bariatric surgery. We confirmed that prior psychiatric conditions were a major risk factor for requiring mental health services after bariatric surgery. Approximately 7% of the patients who did not have any prior documented psychiatric illnesses required some form of psychiatric services after surgery. Suicides accounted for about 10% of all deaths. Our findings question the hypothesis that weight reduction by bariatric surgery will improve mental health in patients with obesity.
eFigure. First Time Patients Presenting to Mental Health Services Following Index Bariatric Surgery: Rates per 1000 patient years follow up
eTable 1. International Classification of Diseases (ICD-10) Bariatric Surgery Codes
eTable 2. International Classification of Diseases 10th Version (ICD-10) Mental and Behavioural Disorder Codes
eTable 3. Sub-group analysis: The Incidence Risk Ratios for Different Psychiatric Diagnoses Requiring Either Outpatient, Emergency Department or Hospitalization Services Before and After Index Bariatric Surgery
eTable 4. Multivariate Linear Regression with Stepwise Elimination Showing Factors Associated with the Number of Mental Health Presentations for Patients Presenting for the First-Time Following Index Bariatric Surgery Between 2007 and 2016
eTable 5. Multivariate Logistic Regression Showing the Risk Factors for 25 Bariatric Patients Who Committed Suicide Out of 261 Deaths After Index Bariatric Procedure
References
- 1.Scott KM, McGee MA, Wells JE, Oakley Browne MA. Obesity and mental disorders in the adult general population. J Psychosom Res. 2008;64(1):97-105. doi: 10.1016/j.jpsychores.2007.09.006 [DOI] [PubMed] [Google Scholar]
- 2.Wardle J, Cooke L. The impact of obesity on psychological well-being. Best Pract Res Clin Endocrinol Metab. 2005;19(3):421-440. doi: 10.1016/j.beem.2005.04.006 [DOI] [PubMed] [Google Scholar]
- 3.Kubik JF, Gill RS, Laffin M, Karmali S. The impact of bariatric surgery on psychological health. J Obes. 2013;2013:837989. doi: 10.1155/2013/837989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9(12):788-805. doi: 10.1038/oby.2001.108 [DOI] [PubMed] [Google Scholar]
- 5.Romain AJ, Marleau J, Baillot A. Impact of obesity and mood disorders on physical comorbidities, psychological well-being, health behaviours and use of health services. J Affect Disord. 2018;225:381-388. doi: 10.1016/j.jad.2017.08.065 [DOI] [PubMed] [Google Scholar]
- 6.Australian Bureau of Statistics National health survey: first results, 2017-18. http://www.abs.gov.au/ausstats/abs@.nsf/mf/4364.0.55.001. Accessed February 8, 2019.
- 7.Chang S-H, Stoll CRT, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149(3):275-287. doi: 10.1001/jamasurg.2013.3654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flum DR, Belle SH, King WC, et al. ; Longitudinal Assessment of Bariatric Surgery (LABS) Consortium . Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361(5):445-454. doi: 10.1056/NEJMoa0901836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morgan DJ, Ho KM, Armstrong J, Litton E. Long-term clinical outcomes and health care utilization after bariatric surgery: a population-based study. Ann Surg. 2015;262(1):86-92. doi: 10.1097/SLA.0000000000000972 [DOI] [PubMed] [Google Scholar]
- 10.Dawes AJ, Maggard-Gibbons M, Maher AR, et al. Mental health conditions among patients seeking and undergoing bariatric surgery: a meta-analysis. JAMA. 2016;315(2):150-163. doi: 10.1001/jama.2015.18118 [DOI] [PubMed] [Google Scholar]
- 11.Szmulewicz A, Wanis KN, Gripper A, et al. Mental health quality of life after bariatric surgery: a systematic review and meta-analysis of randomized clinical trials. Clin Obes. 2019;9(1):e12290. doi: 10.1111/cob.12290 [DOI] [PubMed] [Google Scholar]
- 12.Morgan DJ, Ho KM. Incidence and risk factors for deliberate self-harm, mental illness, and suicide following bariatric surgery: a state-wide population-based linked-data cohort study. Ann Surg. 2017;265(2):244-252. doi: 10.1097/SLA.0000000000001891 [DOI] [PubMed] [Google Scholar]
- 13.Bhatti JA, Nathens AB, Thiruchelvam D, Grantcharov T, Goldstein BI, Redelmeier DA. Self-harm emergencies after bariatric surgery: a population-based cohort study. JAMA Surg. 2016;151(3):226-232. doi: 10.1001/jamasurg.2015.3414 [DOI] [PubMed] [Google Scholar]
- 14.International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) Are you a candidate? https://www.ifso.com/are-you-a-candidate/. Accessed March 17, 2019.
- 15.Australian New Zealand Metabolic Obesity Surgery Society Am I a candidate? https://anzmoss.com.au/obesity/am-i-a-candidate/. Accessed April 12, 2019.
- 16.American Society of Metabolic and Bariatric Surgery Recommendations for the presurgical psychosocial evaluation of bariatric surgery patients. https://asmbs.org/app/uploads/2016/06/2016-Psych-Guidelines-published.pdf. Accessed March 2019. [DOI] [PubMed]
- 17.The National Institute for Health and Care Excellence Obesity: identification, assessment and management. https://www.nice.org.uk/guidance/cg189/chapter/1-Recommendations#assessment. Accessed April 12, 2019. [PubMed]
- 18.Smith FJ, Holman CDJ, Moorin RE, Fletcher DR. Incidence of bariatric surgery and postoperative outcomes: a population-based analysis in Western Australia. Med J Aust. 2008;189(4):198-202. [DOI] [PubMed] [Google Scholar]
- 19.The Australian Bureau of Statistics Australian historical population statistics. http://www.abs.gov.au/AUSSTATS/abs@.nsf/mf/3105.0.65.001. Accessed January 26, 2019.
- 20.Western Australian Department of Health Data linkage Western Australia [database]. http://www.datalinkage-wa.org.au/. Accessed November 12, 2018.
- 21.Holman CDJ, Bass AJ, Rouse IL, Hobbs MS. Population-based linkage of health records in Western Australia: development of a health services research linked database. Aust N Z J Public Health. 1999;23(5):453-459. doi: 10.1111/j.1467-842X.1999.tb01297.x [DOI] [PubMed] [Google Scholar]
- 22.Government of Western Australia Mental Health Commission Suicide prevention 2020. https://www.mhc.wa.gov.au/media/1220/suicide-prevention-2020-strategy-final.pdf. Accessed February 12, 2019.
- 23.Müller A, Claes L, Smits D, Schag K, de Zwaan M. Lifetime self-harm behaviors are not more prevalent in bariatric surgery candidates than in community controls with obesity. Obes Facts. 2018;11(2):109-115. doi: 10.1159/000486484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prescott HC, Costa DK. Improving long-term outcomes after sepsis. Crit Care Clin. 2018;34(1):175-188. doi: 10.1016/j.ccc.2017.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dimitriadis GK, Randeva MS, Miras AD. Potential hormone mechanisms of bariatric surgery. Curr Obes Rep. 2017;6(3):253-265. doi: 10.1007/s13679-017-0276-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota’s effect on mental health: the gut-brain axis. Clin Pract. 2017;7(4):987. doi: 10.4081/cp.2017.987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tabasi M, Ashrafian F, Khezerloo JK, et al. Changes in gut microbiota and hormones after bariatric surgery: a bench-to-bedside review. Obes Surg. 2019;29(5):1663-1674. doi: 10.1007/s11695-019-03779-7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. First Time Patients Presenting to Mental Health Services Following Index Bariatric Surgery: Rates per 1000 patient years follow up
eTable 1. International Classification of Diseases (ICD-10) Bariatric Surgery Codes
eTable 2. International Classification of Diseases 10th Version (ICD-10) Mental and Behavioural Disorder Codes
eTable 3. Sub-group analysis: The Incidence Risk Ratios for Different Psychiatric Diagnoses Requiring Either Outpatient, Emergency Department or Hospitalization Services Before and After Index Bariatric Surgery
eTable 4. Multivariate Linear Regression with Stepwise Elimination Showing Factors Associated with the Number of Mental Health Presentations for Patients Presenting for the First-Time Following Index Bariatric Surgery Between 2007 and 2016
eTable 5. Multivariate Logistic Regression Showing the Risk Factors for 25 Bariatric Patients Who Committed Suicide Out of 261 Deaths After Index Bariatric Procedure