Key Points
Question
What were the trends in carbohydrate, fat, and protein intake among US adults from 1999 to 2016?
Findings
In this nationally representative serial cross-sectional study that included 43 996 adults, there were decreases in low-quality carbohydrates (primarily added sugar) and increases in high-quality carbohydrates (primarily whole grains), plant protein (primarily whole grains and nuts), and polyunsaturated fat. However, 42% of energy intake was still derived from low-quality carbohydrates and the intake of saturated fat remained above 10% of energy.
Meaning
The macronutrient composition of diet among US adults has improved, but continued high intake of low-quality carbohydrates and saturated fat remain.
Abstract
Importance
Changes in the economy, nutrition policies, and food processing methods can affect dietary macronutrient intake and diet quality. It is essential to evaluate trends in dietary intake, food sources, and diet quality to inform policy makers.
Objective
To investigate trends in dietary macronutrient intake, food sources, and diet quality among US adults.
Design, Setting, and Participants
Serial cross-sectional analysis of the US nationally representative 24-hour dietary recall data from 9 National Health and Nutrition Examination Survey cycles (1999-2016) among adults aged 20 years or older.
Exposure
Survey cycle.
Main Outcomes and Measures
Dietary intake of macronutrients and their subtypes, food sources, and the Healthy Eating Index 2015 (range, 0-100; higher scores indicate better diet quality; a minimal clinically important difference has not been defined).
Results
There were 43 996 respondents (weighted mean age, 46.9 years; 51.9% women). From 1999 to 2016, the estimated energy from total carbohydrates declined from 52.5% to 50.5% (difference, −2.02%; 95% CI, −2.41% to −1.63%), whereas that of total protein and total fat increased from 15.5% to 16.4% (difference, 0.82%; 95% CI, 0.67%-0.97%) and from 32.0% to 33.2% (difference, 1.20%; 95% CI, 0.84%-1.55%), respectively (all P < .001 for trend). Estimated energy from low-quality carbohydrates decreased by 3.25% (95% CI, 2.74%-3.75%; P < .001 for trend) from 45.1% to 41.8%. Increases were observed in estimated energy from high-quality carbohydrates (by 1.23% [95% CI, 0.84%-1.61%] from 7.42% to 8.65%), plant protein (by 0.38% [95% CI, 0.28%-0.49%] from 5.38% to 5.76%), saturated fatty acids (by 0.36% [95% CI, 0.20%-0.51%] from 11.5% to 11.9%), and polyunsaturated fatty acids (by 0.65% [95% CI, 0.56%-0.74%] from 7.58% to 8.23%) (all P < .001 for trend). The estimated overall Healthy Eating Index 2015 increased from 55.7 to 57.7 (difference, 2.01; 95% CI, 0.86-3.16; P < .001 for trend). Trends in high- and low-quality carbohydrates primarily reflected higher estimated energy from whole grains (0.65%) and reduced estimated energy from added sugars (−2.00%), respectively. Trends in plant protein were predominantly due to higher estimated intake of whole grains (0.12%) and nuts (0.09%).
Conclusions and Relevance
From 1999 to 2016, US adults experienced a significant decrease in percentage of energy intake from low-quality carbohydrates and significant increases in percentage of energy intake from high-quality carbohydrates, plant protein, and polyunsaturated fat. Despite improvements in macronutrient composition and diet quality, continued high intake of low-quality carbohydrates and saturated fat remained.
This national survey study uses NHANES data to characterize trends in dietary macronutrient intake, food sources, and diet quality among US adults from 1999 to 2016.
Introduction
Unhealthy diet is a major risk factor for noncommunicable diseases globally, including type 2 diabetes mellitus, cardiovascular disease, and certain types of cancer.1,2,3 In the United States, poor diet was estimated to be the leading cause of death and the third leading cause of disability-adjusted life-year loss.4 Consequently, evaluation of overall population trends in diet is important to identifying challenges and opportunities for improving the diet of all US adults.
The calorie demands of the human body are mainly supplied by 3 dietary macronutrients: carbohydrate, fat, and protein.5 As within-person variation in energy intake is small over extended periods, increases in consumption of one macronutrient often leads to decreases in another. In addition to the quantity, the food sources and types of macronutrients are also important in understanding their associations with disease risks.6,7,8,9,10 Changes in the economy, nutrition-related policies, and food processing methods can affect the macronutrient composition and diet quality at the population level. However, evidence is still limited in trends of macronutrient composition, their subtypes, and food sources.11,12,13
This report describes data from 9 consecutive cycles of the National Health and Nutrition Examination Survey (NHANES) to examine trends in dietary macronutrients intake, major food sources of carbohydrate and protein, and overall dietary quality among US adults from 1999 to 2016.
Methods
Study Design and Population
The NHANES study protocol was approved by the research ethics review board of the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention, and all participants provided written informed consent. NHANES has been a nationally representative cross-sectional study since 1999, conducted by the NCHS, that obtains information on health and nutritional status of the noninstitutionalized civilian population in the United States.14 The study design, protocol, and data collection methods have been reported.15 Information on race/ethnicity was self-reported by NHANES participants via standardized questionnaires according to categories provided by the NCHS (non-Hispanic white, non-Hispanic black, Mexican American, other Hispanic, or other). Mexican American and other Hispanic groups were combined to create the Hispanic group. This information was collected to report changes in macronutrient intake and diet quality by race/ethnicity.
For these analyses, the study population included adults aged 20 years or older who completed at least 1 valid dietary recall during the 9 cycles of NHANES from 1999-2000 through 2015-2016. A diet recall was considered valid when all relevant variables associated with the diet recall contained a value.16
Assessment of Food Groups and Nutrients
In NHANES, diet was assessed using 24-hour recalls. From 1999 to 2002, one 24-hour dietary recall was conducted in person in the NHANES Mobile Examination Center. Beginning in 2003, a second 24-hour recall was administered by a telephone interview approximately 3 to 10 days after the first recall.17 The 4-step “multiple-pass method” was used between 1999 and 2001, and the 5-step “automated multiple-pass method” was introduced beginning in 2002. The multiple-pass method is designed to enhance complete and accurate food recall and reduce respondent burden. The multiple-pass method included collecting a self-reported food list, probing for foods forgotten, collecting details of foods, and final probing for any other foods.18 A standard set of measuring guides (eg, rectangular grid, measuring cups and spoons, and bowls) were used to help the respondent report the volume and dimensions of food items consumed.19 All foods and beverages consumed during the previous 24 hours (midnight to midnight) were recorded. The dietary sampling weights were used to account for the complex study design (eg, oversampling of minorities), missing dietary data, and poststratification.20
To assess intake of major foods groups, the same definitions were used for the same food groups in the US Department of Agriculture (USDA) Food Patterns Equivalents Database and MyPyramid Equivalents Database across different survey cycles. Nutrients were estimated based on cycle-specific versions of the USDA Food and Nutrition Database for Dietary Studies. A multiple-step process was developed based on methods previously used to estimate protein sources in NHANES.21 The process included estimation for foods that contained ingredients totally assigned to specific sources, estimation for the other foods, and summing the amount of protein and carbohydrate from each source in all foods (see eAppendix in the Supplement). Food sources of fat were not investigated because they are similar to protein food sources, and existing evidence on fat is mostly based on types of fatty acids rather than on particular food sources.6
Outcomes
The primary outcomes were energy intake from the major macronutrients and their subtypes, food sources of carbohydrate and protein, and overall diet quality as assessed by the Healthy Eating Index (HEI) 2015. The subtypes of macronutrients included high- and low-quality carbohydrates, animal and plant protein, saturated fatty acids, monounsaturated fatty acids, and polyunsaturated fatty acids. Food sources constituting these subtypes are shown in eTable 1 in the Supplement.
Diet quality was assessed using the HEI-2015, which measures adherence to key recommendations in the 2015-2020 Dietary Guidelines for Americans.22 The foods and nutrients were represented on a density basis as amounts per 1000 kcal. The 9 adequacy components included total fruit, whole fruit, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant protein, and fatty acids. The 4 moderation components included refined grains, sodium, percentage of energy from added sugars, and percentage of energy from saturated fatty acids. The scoring method is described in eTable 2 in the Supplement. The total HEI-2015 score ranges from 0 (nonadherence) to 100 (perfect adherence). No minimal clinically important difference has been defined for the HEI-2015.
Secondary outcomes were trends in intakes of macronutrients and diet quality by major population subgroups, including age, sex, race/ethnicity, education, and income level.
Statistical Analysis
All analyses incorporated the dietary sample weights, stratification, and clustering of the complex sampling design to ensure nationally representative estimates. To correct for measurement error, the absolute intakes of nutrients in grams per day were adjusted for total energy intake to 2000 kcal/d using the residual method to minimize measurement error in dietary estimates.23 Additionally, the National Cancer Institute (NCI) method was applied to estimate the usual intake and distribution for all nutrients and food groups (eAppendix in the Supplement). The NCI method is preferred for estimating usual intake distribution from 24-hour diet recalls.24 Percentage of energy of a nutrient was computed as proportion of energy from the nutrient over total energy intake. For instance, for total carbohydrate, percentage of energy = (total carbohydrate [g] × 4 [kcal/g])/total energy intake (kcal) × 100. Total energy intake was estimated as the sum of energy from protein, carbohydrates, and fat. Weighted means and 95% confidence intervals were estimated for dietary macronutrients and the HEI-2015 by cycle. General linear regression was used to estimate trends by treating 2-year survey cycle as a continuous variable. Absolute differences in estimated means were calculated between 1999-2000 and 2015-2016 cycles. Because NHANES started collecting 2 dietary recalls with the 2003-2004 cycle, in sensitivity analyses, the absolute difference was calculated between the 2003-2004 and 2015-2016 cycles. Similar analyses were conducted using the estimates of energy-adjusted absolute intake in grams per day among the overall population. To evaluate potential differences in trends by population subgroups (age, sex, race/ethnicity, education, and income), a survey-weighted Wald F statistic was used to test for an interaction between 2-year survey cycle and demographic subgroups, and statistical significance was set at P = .001 (.05/5 [subgroups] × 9 [nutrients and diet quality]). To determine the degree to which observed trends were due to demographic shifts, additional analyses were performed adjusting for sociodemographic characteristics. Participants with missing data on education and income were excluded in the corresponding subgroup analyses and multivariable analysis. All data were analyzed using SAS version 9.4 (SAS Institute Inc), and statistical significance was set at a 2-tailed P < .05 for all primary analyses. Because of the potential for type I error due to multiple comparisons, findings for the primary and secondary outcomes not corrected for multiple comparisons should be interpreted as exploratory.
Results
Participant Characteristics
Between 1999 and 2016, 88.9% (44 013/49 512) of the NHANES respondents aged 20 years or older provided a single dietary recall. Of these, 70.2% (30 894/44 013) provided a second recall. Participants with invalid diet recalls (n = 17) were excluded.
A total of 43 996 US adults (weighted mean age, 46.9 years [SE, 0.19 years]; n = 22 796 [51.9%] women) were included in these analyses. From 1999 to 2016, the proportion of older adults (aged ≥65 years) increased from 18.0% to 21.1%, while the proportion of younger adults (aged 20-34 years) decreased from 30.0% to 27.8% (Table 1). The proportion who were non-Hispanic white declined from 69.8% to 64.4%, whereas the percentage of other races/ethnicities increased from 4.6% to 9.6%. The proportion of respondents with at least some college education increased from 49.1% to 65.3%.
Table 1. Sociodemographic Characteristics of US Adults by NHANES Survey Cycle, 1999 to 2016.
| Characteristics | No. of Participants (Weighted %)a | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1999-2000 (n = 4237) | 2001-2002 (n = 4744) | 2003-2004 (n = 4448) | 2005-2006 (n = 4520) | 2007-2008 (n = 5420) | 2009-2010 (n = 5762) | 2011-2012 (n = 4801) | 2013-2014 (n = 5047) | 2015-2016 (n = 5017) | |
| Age group, y | |||||||||
| 20-34 | 1136 (30.0) | 1320 (27.6) | 1207 (29.5) | 1378 (27.8) | 1260 (27.7) | 1442 (27.9) | 1317 (27.7) | 1321 (27.8) | 1273 (27.8) |
| 35-49 | 1035 (31.1) | 1258 (33.1) | 1044 (28.8) | 1141 (30.1) | 1369 (30.1) | 1522 (28.9) | 1178 (26.6) | 1322 (26.1) | 1244 (24.8) |
| 50-64 | 929 (20.8) | 1011 (22.4) | 901 (24.0) | 953 (24.1) | 1395 (25.6) | 1419 (25.8) | 1274 (28.1) | 1298 (27.4) | 1290 (26.3) |
| ≥65 | 1137 (18.0) | 1155 (16.9) | 1296 (17.7) | 1048 (18.0) | 1396 (16.6) | 1379 (17.4) | 1032 (17.6) | 1106 (18.6) | 1210 (21.1) |
| Sex | |||||||||
| Male | 1978 (47.8) | 2250 (48.2) | 2135 (48.1) | 2163 (48.0) | 2662 (47.1) | 2789 (48.2) | 2394 (48.7) | 2414 (48.5) | 2415 (48.1) |
| Female | 2259 (52.2) | 2494 (51.8) | 2313 (51.9) | 2357 (52.0) | 2758 (52.9) | 2973 (51.8) | 2407 (51.3) | 2633 (51.5) | 2602 (51.9) |
| Race/ethnicity | |||||||||
| Non-Hispanic white | 1891 (69.8) | 2494 (72.9) | 2391 (73.0) | 2276 (72.7) | 2548 (70.2) | 2786 (68.7) | 1842 (66.6) | 2233 (65.7) | 1711 (64.4) |
| Non-Hispanic black | 792 (10.8) | 890 (10.6) | 867 (11.2) | 1012 (11.5) | 1136 (11.3) | 1025 (11.4) | 1274 (11.5) | 1009 (11.4) | 1060 (11.0) |
| Hispanic | 1421 (14.8) | 1200 (12.3) | 1016 (10.8) | 1049 (10.6) | 1525 (13.2) | 1647 (13.6) | 932 (14.3) | 1125 (14.7) | 1543 (15.0) |
| Otherb | 133 (4.6) | 160 (4.1) | 174 (5.0) | 183 (5.2) | 211 (5.3) | 304 (6.3) | 753 (7.7) | 680 (8.2) | 703 (9.6) |
| Education levelc | |||||||||
| Less than high school graduate | 1633 (24.6) | 1421 (19.2) | 1288 (18.1) | 1234 (17.1) | 1665 (20.1) | 1634 (18.8) | 1102 (16.3) | 1028 (14.7) | 1150 (13.8) |
| High school graduate or GED | 957 (26.3) | 1110 (24.7) | 1111 (26.4) | 1093 (25.4) | 1341 (25.8) | 1316 (22.5) | 1008 (19.9) | 1141 (22.3) | 1108 (21.0) |
| Some college or above | 1633 (49.1) | 2207 (56.0) | 2043 (55.4) | 2191 (57.5) | 2410 (54.1) | 2799 (58.7) | 2688 (63.8) | 2875 (63.0) | 2757 (65.3) |
| Ratio of family income to poverty levelc,d | |||||||||
| <1.30 | 1106 (23.6) | 1190 (21.1) | 1209 (21.4) | 1115 (17.4) | 1498 (21.4) | 1746 (22.2) | 1564 (25.1) | 1592 (25.1) | 1429 (21.0) |
| 1.30-3.49 | 1397 (35.7) | 1723 (35.1) | 1676 (37.5) | 1703 (37.5) | 1921 (34.1) | 1973 (35.8) | 1530 (33.8) | 1615 (34.3) | 1826 (36.7) |
| ≥3.50 | 1137 (40.7) | 1516 (43.8) | 1326 (41.1) | 1507 (45.2) | 1516 (44.6) | 1509 (42.0) | 1340 (41.0) | 1479 (40.6) | 1282 (42.3) |
Abbreviations: GED, general equivalency diploma; NHANES, National Health and Nutrition Examination Survey.
Percentages were adjusted for NHANES survey weights.
“Other” includes race/ethnicity other than non-Hispanic white, non-Hispanic black, and Hispanic, including multiracial.
Numbers may not sum to the total number of participants because of missing data (n=53 without education data; n=3571 without income data).
Represents the ratio of family income to the federal poverty threshold, adjusting for household size. A higher ratio indicates a higher level of income.
Total and Subtypes of Carbohydrate, Protein, and Fat Intake
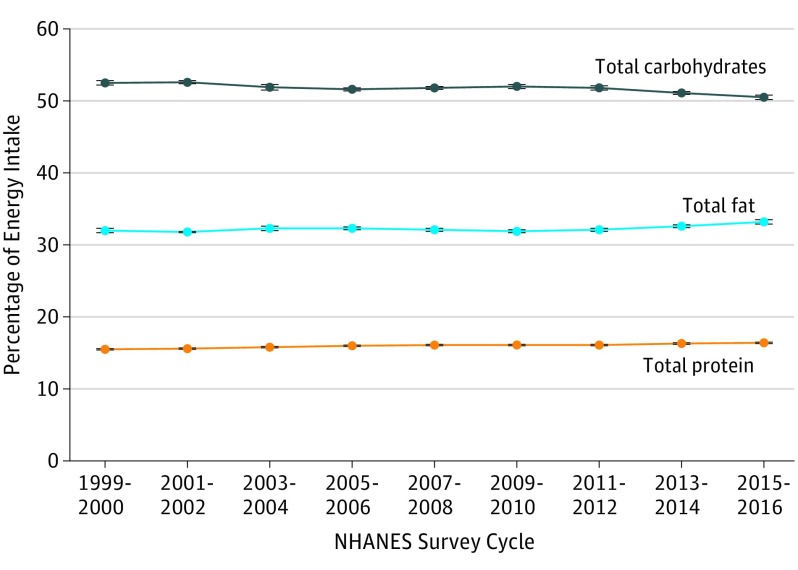
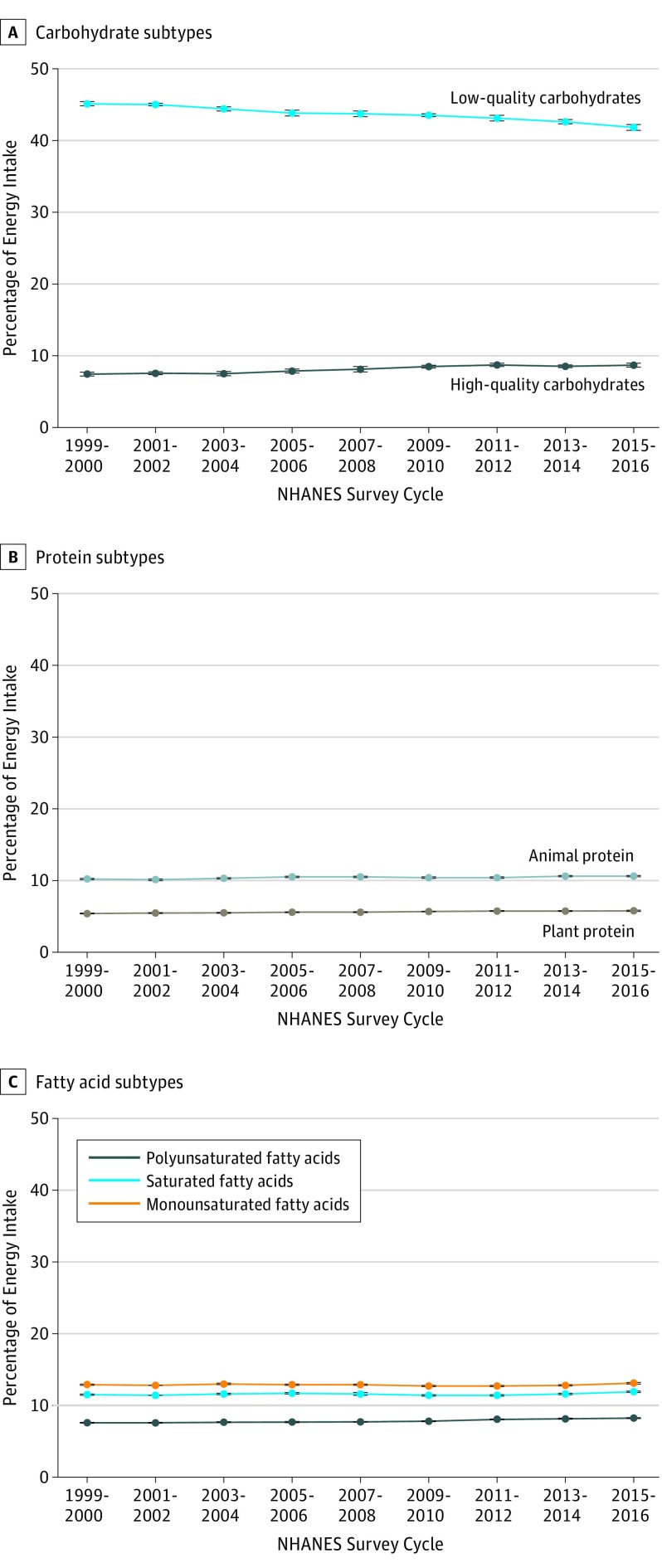
From 1999 to 2016, the estimated percentage of energy intake from total carbohydrates declined from 52.5% to 50.5% (difference, −2.02%; 95% CI, −2.41% to −1.63%; P < .001 for trend) (Figure 1 and eTable 3 in the Supplement). The estimated percentage of energy from high-quality carbohydrates increased from 7.42% to 8.65% (difference, 1.23%; 95% CI, 0.84%-1.61%; P < .001 for trend), whereas that from low-quality carbohydrates decreased from 45.1% to 41.8% (difference, −3.25%; 95% CI, −3.75% to −2.74%; P < .001 for trend) (Figure 2 and eTable 3). The estimated percentage of energy from total protein increased from 15.5% to 16.4% (difference, 0.82%; 95% CI, 0.67%-0.97%; P < .001 for trend) and that from total fat increased from 32.0% to 33.2% (difference, 1.20%; 95% CI, 0.84%-1.55%; P < .001 for trend). The increases in the estimated total protein energy intake were associated with increases in estimated intake from both animal protein (from 10.2% to 10.6%; difference, 0.44%; 95% CI, 0.33%-0.54; P < .001 for trend) and plant protein (from 5.38% to 5.76%; difference, 0.38%; 95% CI, 0.28%-0.49%; P < .001 for trend). The increases in the estimated intake of total fat were associated with increases in estimated energy intake from saturated fatty acids (from 11.5% to 11.9%; difference, 0.36%; 95% CI, 0.20%-0.51%; P < .001 for trend), monounsaturated fatty acids (from 12.9% to 13.1%; difference, 0.19%; 95% CI, 0.03%-0.36%; P < .001 for trend), and polyunsaturated fatty acids (from 7.58% to 8.23%; difference, 0.65%; 95% CI, 0.56%-0.74%; P < .001 for trend). Similar trends were observed when the macronutrients were evaluated by energy-adjusted absolute intake in grams per day (eTable 3 in the Supplement) and when trends were examined from 2003 to 2016 (eTable 4 in the Supplement). After excluding 3624 participants with missing data on education and income, adjusting for changes in the sociodemographic characteristics over time did not alter the results (eTable 5 in the Supplement).
Figure 1. Trends in Estimated Percentage of Energy Intake From Total Carbohydrates, Protein, and Fat Among US Adults Aged 20 Years or Older by NHANES Survey Cycle From 1999-2000 to 2015-2016.
NHANES indicates National Health and Nutrition Examination Survey. Data were adjusted for NHANES survey weights to be nationally representative. Error bars indicate 95% CIs. P < .001 for trend for all (decrease for total carbohydrates; increase for total protein and total fat).
Figure 2. Trends in Estimated Percentage of Energy Intake From Subtypes of Carbohydrates, Protein, and Fat Among US Adults Aged 20 Years or Older by NHANES Survey Cycle From 1999-2000 to 2015-2016.
NHANES indicates National Health and Nutrition Examination Survey. Data were adjusted for NHANES survey weights to be nationally representative. Error bars indicate 95% CIs. P < .001 for trend for all (decrease for low-quality carbohydrates; increase for all others).
Carbohydrate and Protein Intake by Food Sources
From 1999 to 2016, increases in the estimated percentage of energy intake from high-quality carbohydrates were associated with increases in estimated carbohydrate intake from whole grains (from 2.00% to 2.65%; difference, 0.65%; 95% CI, 0.50%-0.79%; P < .001 for trend) and whole fruit (from 2.87% to 3.21%; difference, 0.34%; 95% CI, 0.13%-0.55%; P = .002 for trend) (Table 2). The declines in the estimated energy intake from low-quality carbohydrates were associated with decreases in estimated carbohydrate intake from added sugar (from 16.4% to 14.4%; difference, −2.00%; 95% CI, −2.68% to −1.33%; P < .001 for trend) and fruit juice (from 3.93% to 2.81%; difference, −1.12%; 95% CI, −1.39% to −0.84%; P < .001 for trend). The increases in the estimated energy intake from animal protein were associated with increases in estimated protein intake derived from poultry (from 2.38% to 2.54%; difference, 0.15%; 95% CI, 0.07%-0.24%; P < .001 for trend) and eggs (from 0.70% to 0.80%; difference, 0.10%; 95% CI, 0.08%-0.13%; P < .001 for trend). The increases in estimated energy intake from plant protein were associated with increases in estimated protein intake from whole grains (from 0.38% to 0.50%; difference, 0.12%; 95% CI, 0.09%-0.15%; P < .001 for trend), nuts (from 0.36% to 0.45%; difference, 0.09%; 95% CI, 0.05%-0.13%; P < .001 for trend), and soy (from 0.12% to 0.19%; difference, 0.07%; 95% CI, 0.04%-0.10%; P < .001 for trend). Similar trends were found in evaluation of food sources by energy-adjusted absolute intake in grams per day (eTable 6 in the Supplement).
Table 2. Trends in Estimated Percentage of Energy Intake From Carbohydrates and Protein From Different Sources Among Adults Aged 20 Years or Older by NHANES Survey Cycle, 1999 to 2016.
| Estimated Energy Intake, Survey-Weighted Mean % (95% CI)a | Difference, 2015-2016 vs 1999-2000 (95% CI)b | P Value for Trend | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1999-2000 (n = 4237) | 2001-2002 (n = 4744) | 2003-2004 (n = 4448) | 2005-2006 (n = 4520) | 2007-2008 (n = 5420) | 2009-2010 (n = 5762) | 2011-2012 (n = 4801) | 2013-2014 (n = 5047) | 2015-2016 (n = 5017) | |||
| Carbohydrates | |||||||||||
| High-quality sources | |||||||||||
| Whole grains | 2.00 (1.93-2.08) | 2.15 (2.08-2.23) | 2.09 (1.99-2.18) | 2.28 (2.17-2.39) | 2.32 (2.18-2.45) | 2.47 (2.39-2.55) | 2.60 (2.48-2.72) | 2.56 (2.48-2.64) | 2.65 (2.53-2.77) | 0.65 (0.50 to 0.79) | <.001 |
| Whole fruits | 2.87 (2.72-3.03) | 2.89 (2.80-2.98) | 2.86 (2.69-3.03) | 3.03 (2.89-3.17) | 3.19 (3.01-3.37) | 3.34 (3.25-3.43) | 3.30 (3.17-3.43) | 3.19 (3.07-3.32) | 3.21 (3.06-3.36) | 0.34 (0.13 to 0.55) | <.001 |
| Nonstarchy vegetables | 1.67 (1.63-1.70) | 1.67 (1.64-1.69) | 1.70 (1.66-1.74) | 1.71 (1.67-1.76) | 1.71 (1.67-1.75) | 1.75 (1.72-1.79) | 1.84 (1.80-1.88) | 1.81 (1.78-1.84) | 1.81 (1.77-1.85) | 0.14 (0.08 to 0.20) | <.001 |
| Legumes | 0.88 (0.82-0.94) | 0.84 (0.79-0.89) | 0.83 (0.77-0.89) | 0.82 (0.77-0.88) | 0.87 (0.81-0.93) | 0.90 (0.83-0.97) | 0.96 (0.90-1.02) | 0.94 (0.90-0.99) | 0.98 (0.93-1.03) | 0.10 (0.02 to 0.18) | <.001 |
| Low-quality sources | |||||||||||
| Refined grains | 15.2 (15.0-15.5) | 15.3 (15.1-15.5) | 15.1 (14.9-15.3) | 15.1 (14.9-15.3) | 15.3 (15.1-15.5) | 15.5 (15.3-15.8) | 15.9 (15.7-16.1) | 15.9 (15.7-16.0) | 15.9 (15.6-16.2) | 0.69 (0.31 to 1.07) | <.001 |
| Fruit juice | 3.93 (3.70-4.15) | 3.93 (3.76-4.10) | 3.84 (3.55-4.13) | 3.64 (3.43-3.85) | 3.45 (3.25-3.65) | 3.48 (3.35-3.61) | 3.33 (3.02-3.63) | 2.87 (2.74-2.99) | 2.81 (2.65-2.98) | −1.12 (−1.39 to −0.84) | <.001 |
| Potato | 2.49 (2.42-2.55) | 2.49 (2.45-2.53) | 2.51 (2.44-2.58) | 2.51 (2.43-2.58) | 2.53 (2.46-2.60) | 2.49 (2.44-2.54) | 2.45 (2.40-2.49) | 2.47 (2.43-2.51) | 2.50 (2.46-2.55) | 0.02 (−0.06 to 0.10) | .47 |
| Other starchy vegetable | 0.58 (0.57-0.60) | 0.59 (0.58-0.60) | 0.59 (0.58-0.61) | 0.61 (0.59-0.64) | 0.61 (0.60-0.63) | 0.60 (0.59-0.61) | 0.59 (0.58-0.61) | 0.59 (0.58-0.60) | 0.59 (0.58-0.61) | 0.01 (−0.01 to 0.03) | .10 |
| Added sugar | 16.4 (15.8-16.9) | 16.1 (15.8-16.5) | 15.6 (15.2-16.1) | 15.0 (14.6-15.4) | 15.1 (14.6-15.6) | 14.9 (14.6-15.1) | 14.8 (14.4-15.1) | 14.7 (14.4-15.0) | 14.4 (13.9-14.8) | −2.00 (−2.68 to −1.33) | <.001 |
| Other sourcesc | 6.46 (6.39-6.53) | 6.61 (6.53-6.70) | 6.78 (6.63-6.93) | 6.96 (6.86-7.06) | 6.69 (6.56-6.81) | 6.51 (6.44-6.59) | 6.03 (5.91-6.15) | 6.06 (5.94-6.17) | 5.61 (5.49-5.73) | −0.85 (−0.99 to −0.71) | <.001 |
| Protein | |||||||||||
| Animal sources | |||||||||||
| Unprocessed red meat | 2.70 (2.67-2.73) | 2.66 (2.62-2.70) | 2.73 (2.68-2.77) | 2.74 (2.69-2.78) | 2.74 (2.69-2.79) | 2.72 (2.67-2.76) | 2.73 (2.67-2.79) | 2.73 (2.70-2.76) | 2.75 (2.70-2.79) | 0.05 (−0.01 to 0.10) | .09 |
| Processed meat | 1.10 (1.07-1.12) | 1.11 (1.09-1.13) | 1.13 (1.09-1.17) | 1.14 (1.10-1.18) | 1.12 (1.10-1.15) | 1.11 (1.08-1.15) | 1.11 (1.08-1.13) | 1.11 (1.08-1.14) | 1.11 (1.09-1.13) | 0.01 (−0.02 to 0.05) | .76 |
| Poultry | 2.38 (2.34-2.43) | 2.36 (2.32-2.41) | 2.39 (2.33-2.45) | 2.44 (2.39-2.50) | 2.50 (2.43-2.57) | 2.47 (2.40-2.54) | 2.46 (2.39-2.54) | 2.54 (2.49-2.59) | 2.54 (2.46-2.61) | 0.15 (0.07 to 0.24) | <.001 |
| Seafood | 0.75 (0.73-0.77) | 0.73 (0.72-0.75) | 0.76 (0.73-0.79) | 0.78 (0.75-0.81) | 0.78 (0.75-0.81) | 0.79 (0.77-0.82) | 0.80 (0.77-0.83) | 0.81 (0.77-0.85) | 0.81 (0.77-0.84) | 0.06 (0.02 to 0.10) | <.001 |
| Dairy | 2.54 (2.50-2.57) | 2.55 (2.51-2.59) | 2.55 (2.48-2.63) | 2.61 (2.55-2.66) | 2.57 (2.49-2.66) | 2.60 (2.56-2.63) | 2.50 (2.43-2.57) | 2.58 (2.53-2.64) | 2.60 (2.51-2.69) | 0.06 (−0.03 to 0.16) | .10 |
| Eggs | 0.70 (0.69-0.71) | 0.69 (0.68-0.71) | 0.70 (0.67-0.72) | 0.74 (0.72-0.76) | 0.75 (0.73-0.77) | 0.75 (0.72-0.77) | 0.75 (0.74-0.77) | 0.78 (0.77-0.80) | 0.80 (0.78-0.82) | 0.10 (0.08 to 0.13) | <.001 |
| Other animal sourcesd | 0.01 (0.01-0.01) | 0.01 (0.01-0.01) | 0.01 (0.01-0.01) | 0.01 (0.01-0.01) | 0.01 (0.00-0.01) | 0.01 (0.01-0.01) | 0.01 (0.01-0.01) | 0.01 (0.01-0.01) | 0.01 (0.01-0.01) | 0.00 (0.00 to 0.00) | <.001 |
| Plant sources | |||||||||||
| Whole grains | 0.38 (0.37-0.40) | 0.41 (0.40-0.43) | 0.40 (0.38-0.42) | 0.44 (0.42-0.46) | 0.45 (0.42-0.48) | 0.47 (0.46-0.49) | 0.52 (0.49-0.55) | 0.51 (0.49-0.53) | 0.50 (0.48-0.53) | 0.12 (0.09 to 0.15) | <.001 |
| Refined grains | 2.65 (2.62-2.68) | 2.68 (2.66-2.71) | 2.68 (2.66-2.71) | 2.67 (2.64-2.69) | 2.68 (2.66-2.71) | 2.69 (2.67-2.72) | 2.70 (2.67-2.72) | 2.69 (2.67-2.71) | 2.67 (2.63-2.70) | 0.02 (−0.03 to 0.06) | .33 |
| Nuts | 0.36 (0.34-0.38) | 0.37 (0.36-0.38) | 0.39 (0.37-0.41) | 0.40 (0.39-0.42) | 0.39 (0.37-0.41) | 0.41 (0.39-0.43) | 0.43 (0.41-0.45) | 0.44 (0.42-0.47) | 0.45 (0.42-0.49) | 0.09 (0.05 to 0.13) | <.001 |
| Legumes | 0.31 (0.29-0.33) | 0.29 (0.28-0.31) | 0.29 (0.27-0.31) | 0.29 (0.27-0.31) | 0.31 (0.29-0.32) | 0.31 (0.29-0.33) | 0.33 (0.31-0.35) | 0.33 (0.31-0.34) | 0.34 (0.32-0.36) | 0.04 (0.01 to 0.06) | <.001 |
| Soy | 0.12 (0.10-0.13) | 0.12 (0.11-0.13) | 0.15 (0.13-0.16) | 0.15 (0.13-0.17) | 0.15 (0.14-0.17) | 0.16 (0.15-0.17) | 0.15 (0.13-0.16) | 0.15 (0.14-0.17) | 0.19 (0.17-0.22) | 0.07 (0.04 to 0.10) | <.001 |
| Other plant sourcese | 1.55 (1.54-1.57) | 1.57 (1.56-1.59) | 1.59 (1.57-1.60) | 1.62 (1.59-1.65) | 1.60 (1.59-1.62) | 1.63 (1.61-1.65) | 1.62 (1.59-1.65) | 1.61 (1.58-1.64) | 1.60 (1.57-1.64) | 0.05 (0.01 to 0.09) | <.001 |
Abbreviation: NHANES, National Health and Nutrition Examination Survey.
Data were adjusted for NHANES survey weights to be nationally representative.
Values may not equal the difference between the beginning and ending estimates because of rounding.
Residual carbohydrates not from individual food groups (eg, dairy foods).
Residual animal protein not from individual food groups (eg, insects).
Residual plant protein not from individual food groups (eg, fruits and vegetables).
Healthy Eating Index 2015
From 1999 to 2016, the estimated mean of the HEI-2015 increased from 55.7 to 57.7 (difference, 2.01; 95% CI, 0.86-3.16; P < .001 for trend) (Table 3). The largest increase in the estimated component scores was observed for added sugar (from 5.68 to 6.84; difference, 1.17; 95% CI, 0.88-1.45; P < .001 for trend), indicating reduced consumption of sugar. The largest decrease was observed for sodium (from 4.39 to 3.83; difference, −0.56; 95% CI, −0.72 to −0.39; P< .001 for trend), corresponding to increased sodium consumption. No statistically significant trends were observed for component scores for fruit, dairy, and refined grains.
Table 3. Trends in Estimated Healthy Eating Index (HEI) 2015 Total and Component Scores Among Adults Aged 20 Years or Older by NHANES Survey Cycle, 1999 to 2016.
| HEI-2015 Scores | Survey-Weighted Mean (95% CI)a | Difference, 2015-2016 vs 1999-2000 (95% CI)b | P Value for Trend | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1999-2000 (n = 4237) | 2001-2002 (n = 4744) | 2003-2004 (n = 4448) | 2005-2006 (n = 4520) | 2007-2008 (n = 5420) | 2009-2010 (n = 5762) | 2011-2012 (n = 4801) | 2013-2014 (n = 5047) | 2015-2016 (n = 5017) | |||
| Total score (0-100) | 55.7 (54.8-56.6) | 56.2 (55.6-56.7) | 55.4 (54.6-56.1) | 56.6 (56.0-57.2) | 56.9 (56.0-57.8) | 57.6 (57.2-58.0) | 58.2 (57.6-58.7) | 57.8 (57.3-58.2) | 57.7 (57.0-58.5) | 2.01 (0.86 to 3.16) | <.001 |
| Component scores | |||||||||||
| Adequacy components | |||||||||||
| Total vegetables (0-5) | 3.52 (3.48-3.55) | 3.50 (3.46-3.54) | 3.54 (3.51-3.58) | 3.59 (3.53-3.65) | 3.60 (3.56-3.64) | 3.58 (3.55-3.61) | 3.60 (3.56-3.64) | 3.55 (3.50-3.59) | 3.60 (3.55-3.64) | 0.08 (0.02 to 0.14) | <.001 |
| Greens and beans (0-5) | 2.60 (2.51-2.70) | 2.55 (2.47-2.62) | 2.48 (2.40-2.56) | 2.69 (2.58-2.80) | 2.73 (2.62-2.84) | 2.75 (2.67-2.82) | 2.85 (2.77-2.93) | 2.88 (2.79-2.96) | 2.95 (2.87-3.03) | 0.35 (0.22 to 0.47) | <.001 |
| Total fruits (0-5) | 2.80 (2.67-2.93) | 2.86 (2.78-2.95) | 2.75 (2.60-2.90) | 2.80 (2.71-2.89) | 2.82 (2.69-2.94) | 2.91 (2.86-2.96) | 2.86 (2.79-2.93) | 2.77 (2.68-2.85) | 2.77 (2.66-2.87) | −0.03 (−0.20 to 0.14) | .07 |
| Whole fruits (0-5) | 3.11 (2.99-3.23) | 3.16 (3.09-3.23) | 3.00 (2.86-3.14) | 3.11 (3.01-3.20) | 3.20 (3.08-3.32) | 3.26 (3.21-3.31) | 3.26 (3.17-3.36) | 3.24 (3.15-3.32) | 3.25 (3.13-3.37) | 0.14 (−0.03 to 0.31) | .006 |
| Whole grains (0-10) | 2.24 (2.17-2.32) | 2.42 (2.34-2.51) | 2.32 (2.22-2.41) | 2.53 (2.43-2.62) | 2.55 (2.44-2.65) | 2.74 (2.67-2.81) | 2.86 (2.74-2.98) | 2.81 (2.74-2.88) | 2.81 (2.68-2.94) | 0.56 (0.41 to 0.72) | <.001 |
| Total dairy (0-10) | 5.64 (5.54-5.74) | 5.58 (5.50-5.66) | 5.57 (5.42-5.73) | 5.78 (5.68-5.88) | 5.72 (5.55-5.88) | 5.89 (5.81-5.97) | 5.67 (5.53-5.81) | 5.71 (5.61-5.82) | 5.59 (5.42-5.76) | −0.06 (−0.25 to 0.14) | <.001 |
| Total protein foods (0-5) | 4.90 (4.89-4.92) | 4.90 (4.89-4.92) | 4.87 (4.85-4.90) | 4.90 (4.88-4.91) | 4.90 (4.89-4.92) | 4.90 (4.88-4.91) | 4.91 (4.89-4.93) | 4.91 (4.90-4.92) | 4.93 (4.92-4.94) | 0.02 (0.01 to 0.04) | <.001 |
| Seafood and plant protein (0-5) | 4.11 (4.04-4.17) | 3.98 (3.94-4.03) | 3.81 (3.75-3.88) | 4.14 (4.07-4.20) | 4.19 (4.11-4.27) | 4.20 (4.13-4.26) | 4.28 (4.23-4.32) | 4.29 (4.25-4.33) | 4.33 (4.28-4.38) | 0.23 (0.14 to 0.31) | <.001 |
| (PUFAs + MUFAs)/SFAs (0-10) | 4.56 (4.47-4.65) | 4.62 (4.53-4.70) | 4.63 (4.57-4.70) | 4.47 (4.39-4.56) | 4.63 (4.48-4.77) | 4.72 (4.61-4.82) | 4.95 (4.83-5.06) | 4.81 (4.71-4.90) | 4.74 (4.63-4.86) | 0.18 (0.04 to 0.33) | <.001 |
| Moderation components | |||||||||||
| Sodium (0-10) | 4.39 (4.29-4.49) | 4.55 (4.47-4.63) | 4.35 (4.23-4.47) | 4.18 (4.04-4.32) | 4.16 (4.07-4.25) | 3.80 (3.70-3.90) | 3.92 (3.85-3.98) | 3.89 (3.78-4.00) | 3.83 (3.70-3.96) | −0.56 (−0.72 to −0.39) | <.001 |
| Refined grains (0-10) | 6.18 (6.06-6.29) | 6.14 (6.04-6.25) | 6.04 (5.93-6.14) | 6.24 (6.12-6.35) | 6.18 (6.05-6.32) | 6.25 (6.10-6.40) | 6.27 (6.12-6.43) | 6.30 (6.17-6.43) | 6.38 (6.18-6.57) | 0.20 (−0.03 to 0.42) | .03 |
| Saturated fat (0-10) | 5.97 (5.82-6.12) | 6.10 (6.01-6.19) | 5.85 (5.68-6.02) | 5.77 (5.68-5.86) | 5.91 (5.76-6.05) | 6.13 (6.00-6.26) | 6.20 (6.05-6.35) | 5.98 (5.85-6.10) | 5.69 (5.57-5.82) | −0.27 (−0.47 to −0.08) | <.001 |
| Added sugars (0-10) | 5.68 (5.44-5.91) | 5.80 (5.61-5.98) | 6.14 (5.92-6.36) | 6.39 (6.22-6.57) | 6.31 (6.09-6.53) | 6.48 (6.37-6.59) | 6.55 (6.40-6.71) | 6.65 (6.53-6.77) | 6.84 (6.69-7.00) | 1.17 (0.88 to 1.45) | <.001 |
Abbreviations: MUFAs, monounsaturated fatty acids; NHANES, National Health and Nutrition Examination Survey; PUFAs, polyunsaturated fatty acids; SFAs, saturated fatty acids.
Data were adjusted for NHANES survey weights to be nationally representative. Higher scores indicate greater adherence to the 2015 Dietary Guidelines for Americans.
Values may not equal the difference between the beginning and ending estimates because of rounding.
Trends in Population Subgroups
Participants with missing data on education (n = 53) and income (n = 3571) were excluded in the corresponding subgroup analyses. Between 1999 and 2016, there were significant declines in estimated percentage of energy intake from low-quality carbohydrates and increases in estimated percentage of energy intake from high-quality carbohydrates, plant and animal protein, and polyunsaturated fatty acids across all population subgroups (P < .05 for trend for all) (eTables 7-9 in the Supplement). Greater changes in low-quality carbohydrates and polyunsaturated fatty acids were observed among younger vs older individuals and among those with a higher vs lower level of education or income (P < .001 for interaction for all). For example, changes in estimated percentage of energy from low-quality carbohydrates and polyunsaturated fatty acids were greater among individuals with the highest level of income (−3.89% [95% CI, −4.67% to −3.11%] and 0.76% [95% CI, 0.57%-0.95%], respectively) than among those with the lowest level of income (−2.46% [95% CI, −3.11% to −1.82%] and 0.49% [95% CI, 0.35%-0.63%], respectively) (P < .001 for interaction for all). For the HEI-2015, greater increases in estimated total score were observed among younger vs older individuals and among those with a higher vs lower level of income (P < .001 for interaction for all) (eTable 10 in the Supplement).
Discussion
From 1999 to 2016, the macronutrient composition of the diet of US adults improved, with declines in low-quality carbohydrates (primarily added sugar) and increases in high-quality carbohydrates (primarily whole grains), plant protein (primarily whole grains and nuts), and polyunsaturated fatty acids, accompanied by improvements in overall diet quality as assessed by the HEI-2015. However, proportions of energy intake from low-quality carbohydrates remained high, while saturated fat intake remained above the recommended level.
The decreasing trend in total carbohydrate intake (from 52% to 50% of energy) and increasing trend in total fat intake (from 32% to 33%) in the past 18 years partly reversed the trends observed between 1971 and 2000, when the energy intake from carbohydrates increased from 42%-45% to 49%-52% while intake from total fat decreased from 36%-37% to 32%.12,13 These opposing trends could be due to dietary guidelines prior to 2000 that recommended low-fat diets,25 which was associated with decreased intake of total fat and increased intake of refined grains and added sugar. After 2000, shifts in scientific evidence and dietary guidelines promoted health benefits of healthy fats and plant sources of protein and the harms of low-quality carbohydrates.26,27 At the same time, the growing popularity of specific diet patterns such as Atkins, paleo, low-carbohydrate, and vegan/vegetarian diets may have contributed to changes in recent trends.
Several improvements in macronutrient composition and diet quality were identified. From 1999 to 2016, consistent with concurrent dietary guidance, US adults decreased intake of added sugar and increased consumption of whole grains, poultry, and nuts.26,27 The overall diet quality as measured by the HEI-2015 improved as well, consistent with previous studies evaluating other diet quality scores such as the Alternative Healthy Eating Index 2010 and the American Heart Association Diet Score.28,29 However, the improvement in the HEI-2015 was small in magnitude and of uncertain clinical importance. Despite observed improvements, important dietary challenges remained. First, US adults still consumed a disproportionally high energy intake from low-quality carbohydrates. The majority of the low-quality carbohydrate energy intake represented carbohydrates from refined grains, fruit juice, and potatoes (21.2% of intake), followed by added sugars in foods and beverages (14.4% of intake). Second, protein intake was mostly derived from animal foods such as unprocessed red meat and processed meat, whereas protein intake from seafood and plant sources such as whole grains, nuts, and legumes remained a much smaller percentage of energy intake. Previous studies showed that red meat and processed meat were associated with poorer health outcomes.9,30,31 Third, saturated fat intake remained above the Dietary Guidelines for Americans recommended level of 10% of energy intake.26 Fourth, US adults with low income and educational attainment experienced a smaller improvement in macronutrient composition and did not improve the overall diet quality in the past 18 years. Further interventions should focus on minimizing these differences.
This study’s strengths included use of the most recent dietary data from NHANES, thereby facilitating evaluation of trends in the past 18 years, investigation of the trends of macronutrients by quality and food sources, and examination of potential differences by sociodemographic subgroups.
Limitations
This study has several limitations. First, self-reported dietary 24-hour recall data are subject to measurement error due to large day-to-day variations in food intake. However, the NCI method was applied to reduce measurement error and improve estimates of usual intake. Second, changes in dietary databases and dietary assessment methods over the study period may affect estimated trends in macronutrient intake. Still, the same protocols were followed to derive each macronutrient from different foods across all cycles. The sensitivity analyses restricted to cycles using the same dietary database and assessment method showed results similar to the main analyses. Third, a multiple-step process was developed to estimate food sources of protein and carbohydrate, but this method requires further replication and validation. Fourth, the cross-sectional nature of the NHANES survey precluded conclusions on how demographic shifts contributed to these trends. Fifth, participants with missing data on education or income were excluded, which may affect the generalizability of these findings. Sixth, no data were available on associations of these dietary changes with population outcomes.
Conclusions
From 1999 to 2016, US adults experienced a significant decrease in percentage of energy intake from low-quality carbohydrates and significant increases in percentage of energy intake from high-quality carbohydrates, plant protein, and polyunsaturated fat. Despite improvements in macronutrient composition and diet quality, continued high intake of low-quality carbohydrates and saturated fat remained.
eAppendix. Supplemental Methods
eTable 1. Dietary Components Classified as Food Sources of Carbohydrate and Protein
eTable 2. Healthy Eating Index-2015 Components, Component Points, and Standards for Scoring
eTable 3. Trends in Estimated Percent Energy (%E) and Absolute Intake (g/d) of Total and Subtypes of Macronutrients Among US Adults ≥20 Years by NHANES Survey Cycle, 1999-2016
eTable 4. Trends in Estimated Percent Energy (%E) and Absolute Intake (g/d) of Total and Subtypes of Macronutrients Among US Adults ≥20 Years by NHANES Survey Cycle, 2003-2016
eTable 5. Trends in Estimated Percent Energy (%E) and Absolute Intake (g/d) of Total and Subtypes of Macronutrients, After Adjustment for Age, Sex, Race/Ethnicity, Education, and Income Among US Adults ≥20 Years by NHANES Survey Cycle, 1999-2016
eTable 6. Trends in Estimated Absolute Intake of Carbohydrate and Protein From Different Sources (g/d) Among Adults ≥20 Years by NHANES Survey Cycle, 1999-2016
eTable 7. Trends in Estimated Percent Energy (%E) From High- and Low-Quality Carbohydrate by Age Group, Sex, Race/Ethnicity, Education, and Income, 1999-2016
eTable 8. Trends in Estimated Percent Energy (%E) From Animal and Plant Protein by Age Group, Sex, Race/Ethnicity, Education, and Income, 1999-2016
eTable 9. Trends in Estimated Percent Energy (%E) From Saturated Fatty Acids, Monounsaturated Fatty Acids, and Polyunsaturated Fatty Acids by Age Group, Sex, Race/Ethnicity, Education, and Income, 1999-2016
eTable 10. Trends in Estimated Healthy Eating Index-2015 by Age Group, Sex, Race/Ethnicity, Education, and Income, 1999-2016
eReferences
References
- 1.GBD 2016 Risk Factors Collaborators Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1345-1422. doi: 10.1016/S0140-6736(17)32366-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pan A, Lin X, Hemler E, Hu FB. Diet and cardiovascular disease: advances and challenges in population-based studies. Cell Metab. 2018;27(3):489-496. doi: 10.1016/j.cmet.2018.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet. 2014;383(9933):1999-2007. doi: 10.1016/S0140-6736(14)60613-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mokdad AH, Ballestros K, Echko M, et al. ; US Burden of Disease Collaborators . The state of US health, 1990-2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444-1472. doi: 10.1001/jama.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trumbo P, Schlicker S, Yates AA, Poos M; Food and Nutrition Board of the Institute of Medicine, the National Academies . Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc. 2002;102(11):1621-1630. doi: 10.1016/S0002-8223(02)90346-9 [DOI] [PubMed] [Google Scholar]
- 6.Sacks FM, Lichtenstein AH, Wu JHY, et al. ; American Heart Association . Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2017;136(3):e1-e23. doi: 10.1161/CIR.0000000000000510 [DOI] [PubMed] [Google Scholar]
- 7.Bernstein AM, Sun Q, Hu FB, Stampfer MJ, Manson JE, Willett WC. Major dietary protein sources and risk of coronary heart disease in women. Circulation. 2010;122(9):876-883. doi: 10.1161/CIRCULATIONAHA.109.915165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ludwig DS, Hu FB, Tappy L, Brand-Miller J. Dietary carbohydrates: role of quality and quantity in chronic disease. BMJ. 2018;361:k2340. doi: 10.1136/bmj.k2340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song M, Fung TT, Hu FB, et al. . Association of animal and plant protein intake with all-cause and cause-specific mortality. JAMA Intern Med. 2016;176(10):1453-1463. doi: 10.1001/jamainternmed.2016.4182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet. 2019;393(10170):434-445. doi: 10.1016/S0140-6736(18)31809-9 [DOI] [PubMed] [Google Scholar]
- 11.Berryman CE, Lieberman HR, Fulgoni VL III, Pasiakos SM. Protein intake trends and conformity with the dietary reference intakes in the United States: analysis of the National Health and Nutrition Examination Survey, 2001-2014. Am J Clin Nutr. 2018;108(2):405-413. doi: 10.1093/ajcn/nqy088 [DOI] [PubMed] [Google Scholar]
- 12.Cohen E, Cragg M, deFonseka J, Hite A, Rosenberg M, Zhou B. Statistical review of US macronutrient consumption data, 1965-2011: Americans have been following dietary guidelines, coincident with the rise in obesity. Nutrition. 2015;31(5):727-732. doi: 10.1016/j.nut.2015.02.007 [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention Trends in intake of energy and macronutrients—United States, 1971-2000. MMWR Morb Mortal Wkly Rep. 2004;53(4):80-82. [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention About the National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed June 2, 2019.
- 15.Centers for Disease Control and Prevention National Health and Nutrition Examination Survey response rates and population totals. https://wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx. Accessed June 2, 2019.
- 16.Centers for Disease Control and Prevention Information about dietary variables in National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/tutorials/dietary/AdditionalResources/Info_DietaryVariables.htm. Accessed June 2, 2019.
- 17.Moshfegh AJ, Rhodes DG, Baer DJ, et al. . The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88(2):324-332. doi: 10.1093/ajcn/88.2.324 [DOI] [PubMed] [Google Scholar]
- 18.Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J Nutr. 2006;136(10):2594-2599. doi: 10.1093/jn/136.10.2594 [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention National Health and Nutrition Examination Survey: measuring guides for the dietary recall interview. https://www.cdc.gov/nchs/nhanes/measuring_guides_dri/measuringguides.htm. Accessed June 2, 2019.
- 20.Centers for Disease Control and Prevention Key concepts about the NHANES sample weights. https://www.cdc.gov/nchs/tutorials/nhanes/SurveyDesign/SampleDesign/Info1.htm. Accessed June 2, 2019.
- 21.Pasiakos SM, Agarwal S, Lieberman HR, Fulgoni VL III. Sources and amounts of animal, dairy, and plant protein intake of US adults in 2007-2010. Nutrients. 2015;7(8):7058-7069. doi: 10.3390/nu7085322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reedy J, Lerman JL, Krebs-Smith SM, et al. . Evaluation of the Healthy Eating Index–2015. J Acad Nutr Diet. 2018;118(9):1622-1633. doi: 10.1016/j.jand.2018.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Willett WC. Nutritional Epidemiology. 3rd ed. Oxford, England: Oxford University Press; 2013. [Google Scholar]
- 24.Tooze JA, Midthune D, Dodd KW, et al. . A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc. 2006;106(10):1575-1587. doi: 10.1016/j.jada.2006.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.La Berge AF. How the ideology of low fat conquered America. J Hist Med Allied Sci. 2008;63(2):139-177. doi: 10.1093/jhmas/jrn001 [DOI] [PubMed] [Google Scholar]
- 26.US Department of Health and Human Services; US Department of Agriculture 2015-2020 Dietary Guidelines for Americans. 8th ed. December 2015. https://health.gov/dietaryguidelines/2015/guidelines/. Accessed June 2, 2019.
- 27.Lloyd-Jones DM, Hong Y, Labarthe D, et al. ; American Heart Association Strategic Planning Task Force and Statistics Committee . Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586-613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 28.Wang DD, Leung CW, Li Y, et al. . Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174(10):1587-1595. doi: 10.1001/jamainternmed.2014.3422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary intake among US adults, 1999-2012. JAMA. 2016;315(23):2542-2553. doi: 10.1001/jama.2016.7491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelemen LE, Kushi LH, Jacobs DR Jr, Cerhan JR. Associations of dietary protein with disease and mortality in a prospective study of postmenopausal women. Am J Epidemiol. 2005;161(3):239-249. doi: 10.1093/aje/kwi038 [DOI] [PubMed] [Google Scholar]
- 31.Farvid MS, Cho E, Chen WY, Eliassen AH, Willett WC. Dietary protein sources in early adulthood and breast cancer incidence: prospective cohort study. BMJ. 2014;348:g3437. doi: 10.1136/bmj.g3437 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Supplemental Methods
eTable 1. Dietary Components Classified as Food Sources of Carbohydrate and Protein
eTable 2. Healthy Eating Index-2015 Components, Component Points, and Standards for Scoring
eTable 3. Trends in Estimated Percent Energy (%E) and Absolute Intake (g/d) of Total and Subtypes of Macronutrients Among US Adults ≥20 Years by NHANES Survey Cycle, 1999-2016
eTable 4. Trends in Estimated Percent Energy (%E) and Absolute Intake (g/d) of Total and Subtypes of Macronutrients Among US Adults ≥20 Years by NHANES Survey Cycle, 2003-2016
eTable 5. Trends in Estimated Percent Energy (%E) and Absolute Intake (g/d) of Total and Subtypes of Macronutrients, After Adjustment for Age, Sex, Race/Ethnicity, Education, and Income Among US Adults ≥20 Years by NHANES Survey Cycle, 1999-2016
eTable 6. Trends in Estimated Absolute Intake of Carbohydrate and Protein From Different Sources (g/d) Among Adults ≥20 Years by NHANES Survey Cycle, 1999-2016
eTable 7. Trends in Estimated Percent Energy (%E) From High- and Low-Quality Carbohydrate by Age Group, Sex, Race/Ethnicity, Education, and Income, 1999-2016
eTable 8. Trends in Estimated Percent Energy (%E) From Animal and Plant Protein by Age Group, Sex, Race/Ethnicity, Education, and Income, 1999-2016
eTable 9. Trends in Estimated Percent Energy (%E) From Saturated Fatty Acids, Monounsaturated Fatty Acids, and Polyunsaturated Fatty Acids by Age Group, Sex, Race/Ethnicity, Education, and Income, 1999-2016
eTable 10. Trends in Estimated Healthy Eating Index-2015 by Age Group, Sex, Race/Ethnicity, Education, and Income, 1999-2016
eReferences