Key Points
Question
How are prehospital time and mortality associated in a physician-staffed trauma system?
Findings
The results of this cohort study from 2 French trauma registries demonstrate a linear association between total prehospital time and in-hospital all-cause mortality. The odds of death increased by 8% for each 10-minute increase in prehospital time.
Meaning
These findings call for a further streamlining of prehospital trauma care and the need to define the optimal intervention-to-time ratio.
This cohort study assesses the association of total prehospital time and in-hospital mortality in 2 prehospital, physician-staffed emergency medical systems in urban and rural France.
Abstract
Importance
The association between total prehospital time and mortality in physician-staffed trauma systems remains uncertain.
Objective
To describe the association of total prehospital time and in-hospital mortality in prehospital, physician-staffed trauma systems in France, with the hypothesis that total prehospital time is associated with increased mortality.
Design, Setting, and Participants
This cohort study was conducted from January 2009 to December 2016. Data for this study were derived from 2 distinct regional trauma registries in France (1 urban and 1 rural) that both have a physician-staffed emergency medical service. Consecutive adult trauma patients admitted to either of the regional trauma referral centers during the study period were included. Data analysis took place from March 2018 to September 2018.
Main Outcomes and Measures
The association between death and prehospital time was assessed with a multivariable model adjusted with confounders. Total prehospital time was the primary exposure variable, recorded as the time from the arrival of the physician-led prehospital care team on scene to the arrival at the hospital. The main outcome of interest was all-cause in-hospital mortality.
Results
A total of 10 216 patients were included (mean [SD] age, 41 [18] years; 7937 men [78.3%]) affected by predominantly nonpenetrating injuries (9265 [91.5%]), with a mean (SD) Injury Severity Score of 17 (14) points. Of the patients, 6737 (66.5%) had at least 1 body region with an Abbreviated Injury Scale score of 3 or more. A total of 1259 patients (12.4%) presented in shock (with systolic pressure <90 mm Hg) and 2724 (26.9%) with severe head injury (Abbreviated Injury Scale score ≥3 points). On unadjusted analysis, increasing prehospital times (in 30-minute categories) were associated with a markedly and constant increase in the risk of in-hospital death. The odds of death increased by 9% for each 10-minute increase in prehospital time (odds ratio, 1.09 [95% CI, 1.07-1.11]) and after adjustment by 4% (odds ratio, 1.04 [95% CI, 1.01-1.07]).
Conclusions and Relevance
In this study, an increase in total prehospital time was associated with increasing in-hospital all-cause mortality in trauma patients at a physician-staffed emergency medical system, after adjustment for case complexity. Prehospital time is a management objective in analogy to physiological targets. These findings plead for a further streamlining of prehospital trauma care and the need to define the optimal intervention-to-time ratio.
Introduction
The concept of time as essential determinant of outcome in the early care of trauma patients is a prevailing doctrine,1,2 captured in the term the golden hour of trauma.3,4 The concept of trauma as a time-sensitive condition has guided education and policy for decades in the international trauma community. Despite this cultural penetrance,5 evidence in favor remains elusive, and the concept is controversial.6,7,8,9,10
The concept of trauma as a time-sensitive health condition was developed and nurtured in a specific emergency medical system (EMS), mainly a paramedic-based system in North America. The international trauma community transposed this concept to diverse, specific settings, even if the respective context was different from that of the North American system.11 Data on system performance from physician-staffed EMS are far less abundant than data from EMS systems. On the one hand, physician-staffed EMS are thought to add complexity to a complex situation by performing more interventions that result in longer total prehospital time (TPT).12,13 On the other side, proponents of the physician-led critical care team advocate a more tailored provision of advanced prehospital critical care. The ensuing debate oscillates between dichotomous concepts such as scoop and run or stay and play.11,13,14 The reality is probably less easy to frame.
Based on this rationale and considering the comparative lack of data for physician-staffed EMS, it appeared justified to reconsider the association of prehospital total time with in-hospital mortality in a physician-staffed EMS. The objective was to describe the association of total prehospital time and in-hospital mortality in a large and representative cohort of trauma patients from 2 regional and very geographically distinct trauma systems in France (1 urban and 1 rural and mountainous). We hypothesized that a longer TPT is associated with a mortality increase in a physician-staffed EMS system.
Methods
This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. A checklist for this cohort study is provided in eTable 1 in the Supplement.
Ethical Approval
This is an observational study using data from 2 prospective multicenter regional trauma registries, the TraumaBase, from the Paris area, Île-de-France, and Trauma System of the Northern French Alps Emergency Network (Trauma System du Réseau Nord Alpin des Urgences [TRENAU]), from the Rhône-Alpes region. Both registries have obtained approval from the institutional review board (Comité de Protection des Personnes, Paris VI and Clermont-Ferrand), the Advisory Committee for Information Processing in Health Research (Comite Consultatif Pour le Traitement de l’Information en Matière de Recherche Dans le Domaine de la Santé, 11.305bis and 15.038bis), and from the National Data Protection Agency (Commission Nationale de l’Informatique et des Libertés 911461 and 915372), waiving the need for informed consent. Both registries use algorithms for consistency, coherence, and professional data monitoring. Data monitoring for the TraumaBase is assured by the Biostatistics Laboratory of Paris 7 and for the TRENAU registry by professional statisticians employed by the network.
Setting
The structure and triage in both trauma systems have been previously described.15,16 In summary, physician-staffed mobile intensive care units provide the prehospital care in both systems. A mobile intensive care unit team provides the equivalent of advanced trauma life support–based prehospital interventions (eg, sedation, prehospital anesthesia, advanced airway management, chest decompression). The TraumaBase in Île-de France covers an urban area of 4633.2 mi2 (12 000 km2) with a population of 12 million inhabitants and 15 million visitors per year. Almost exclusively, 8 physician-staffed EMS (Service Aide Medicale Urgente [SAMUs]) organized into 43 mobile intensive care units, 37 SAMUs, 6 Paris Fire Brigades (Brigade de Sapeurs de Pompiers), and 6 designated level I centers provide the trauma care; no lower-level care centers have been designated. The TRENAU area covers an area of 6949.8 mi2 (18 000 km2) in the Northern French Alps, with a population of 2 million inhabitants and a high seasonal variation (8 million tourists each year). Care in the TRENAU network is provided by 3 SAMUs and a total of 14 designated trauma hospitals, with 2 level I, 1 level II, and 11 level III centers. The TRENAU network uses specific management and triage guidelines.15 Within the Paris network, national triage17 and management guidelines apply, such as those for shock.18 At any given time, clinical management was left to the discretion of the responsible physician (prehospital or in-hospital). Both networks and registries are financially supported by the respective Regional Health Authorities (Agence Régionale de Santé) in Île-de-France and Rhône-Alpes.
Study Populations
All consecutive trauma patients triaged to 1 of the 6 regional, designated Paris level I trauma centers or 1 of the 14 centers participating in the TRENAU network were screened for inclusion. Patients who were not managed by a physician-staffed mobile unit or transported to a participating hospital (ie, recorded in the data set as death on scene or not transported) or transferred from a hospital outside of the respective system were not included. Only patients directly admitted to level I or level II centers (if in TRENAU) were included. The enhanced care teams in both systems are able to provide a full spectrum of advanced trauma life support care, including airway management with rapid sequence induction for intubation, sedation and analgesia, fluid therapy, vasoactive medication, fracture and dislocation reduction, chest decompression, hemorrhage control (eg, by tourniquets, splinting, compression), red blood cell concentrate transfusion, and other techniques. They currently do not provide thoracotomy or blood-component therapy other than red blood cell concentrates, which occur in less than 3% of cases in both systems.
We defined early critical prehospital trauma interventions as any of the following: prehospital intubation, vasopressor use, osmotherapy, and fluid resuscitation of more than 1000 mL. Shock was defined as a systolic arterial pressure less than 90 mm Hg.
eTable 1 in the Supplement provides the complete list of epidemiological, clinical (prehospital and in-hospital), physiological, and biological variables that were recorded for each patient. In brief, both data collections followed the revised version of the Utstein Template for Uniform Reporting of Data Following Major Trauma.19 Calculation of the 2005 version of Injury Severity Score (ISS) completed this information.
Exposure Variable and Outcome Criteria
Total prehospital time was the primary exposure variable, recorded as the time of arrival of the physician-led prehospital care-team on scene to the time of arrival at the hospital. Arrival on scene, leaving the scene, and arrival at the admitting hospital are systematically recorded in both registries based on prehospital intervention run sheets and/or dispatch center data; the exact timing of injury was not recorded in either registry.
The main outcome of interest was all-cause in-hospital mortality. Patients who died within 24 hours were retained in the analysis to minimize survivor bias. Cause-specific death, including death from bleeding and death from head injury, was considered the secondary end point. In both registries, the causes of death were based on a judgment by a physician reviewing all evidence at routine case closure. The physician performing case closure was not part of the working committee of this study.
Statistical Analysis
Sample Size
The retrospective nature of the study predetermines the sample size. A post hoc power calculation was performed using a 1-sample correlation Fisher z test. We used the regression coefficient of total prehospital time as an alternative hypothesis and a coefficient of 0 corresponding to the null hypothesis with no association with traumatic death.
Statistical Methods
Continuous variables were presented with means and SDs or with median and interquartile range when appropriate. Categorical variables were presented with frequencies and percentages.
The association between death and prehospital time was assessed graphically by plotting the risk of death on prehospital time. A generalized linear mixed model (GLMM) with random effect by registry and EMS system explored the association between death and prehospital time with a logit function. We assessed the departure of linearity in the association between death and time graphically and added the polynomial terms in the GLMM if needed (eTable 6 in the Supplement). Homogeneity between categories was tested using the χ2 test.
We fitted the best model according to likelihood ratio test and Akaike information criterion. In addition, a generalized additive model (GAM) assessed and explored the linearity of the association between death and time. The GAM is a flexible model of GLMM with a link function based on smoothing splines. The amount of smoothing is controlled by the number of equivalent degrees of freedom. We graphically assessed the smooth function to fix the equivalent degrees of freedom for prehospital time. We assessed the deviance variation that occurred depending on the use of the linear term or the smoothing term in the equation.
To control for potential variables associated with case complexity, a GLMM and GAM model was applied in multivariable analysis to adjust for the confounders age, sex, severity of anatomic injury pattern (by ISS), systolic blood pressure, and Glasgow Coma Scale (GCS) score in a parsimonious method. These 5 variables are strongly correlated with prehospital interventions, such as airway management. The more severely a patient is in shock (by systolic blood pressure measurement) or the greater the likelihood of a traumatic brain injury (TBI) (as measured by the GCS), the more severely injured the patient is (per the ISS). The high injury load may trigger more interventions and longer prehospital times. In consequence, for the sake of simplicity and to avoid collinearity, the models did deliberately not include prehospital interventions.
Two-sided P values <.05 were considered significant. All statistical analyses were performed using Stata SE version 14.0 (StataCorp).
Missing Data
Multiple imputation of missing values to assess total prehospital time was not feasible. Several variables were not routinely collected in both registries (eg, distance between scene of injury and hospital, dispatching decision). Measurement errors in variables that are not routinely collected could lead to inappropriate assessments when applied to multiple imputation. Data were unlikely to be missing at random, and this could lead to a bias toward the null when applying multiple imputation. For this reason, a complete case analysis was performed. Comparability of patients with and without missing data on TPT were assessed in terms of demographic characteristics, prehospital condition, injury severity, and in-hospital death.
Results
In total, 6441 patients were screened for inclusion from January 2011 to December 2016 in the TraumaBase database and 8888 were screened for inclusion from the TRENAU database from January 2009 to December 2016. The main reason to exclude patients was missing data (eFigure 1 and eTable 2 in the Supplement). In total, 10 126 patients (5059 from TRENAU and 5067 from TraumaBase) were retained for complete case analysis.
Patients had a mean (SD) age of 41 (18) years, and most were men (7937 [78.3%]) affected by predominantly nonpenetrating injury (9265 [91.5%]), with a mean (SD) ISS of 17 (14) points. In 6737 patients (66.5%), at least 1 body region had an AIS score of 3 points or more. A total of 1259 patients (12.4%) presented in shock (systolic pressure <90 mm Hg), and 2724 (26.9%) presented with severe head injury (AIS ≥3 points; Table 1).
Table 1. Patient Characteristics According to Regional Database.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Total | Paris, Île-de-France (TraumaBase) | Northern French Alps (TRENAU) | |
| No. | 10 126 | 5067 | 5059 |
| Age, mean (SD), y | 41 (18) | 38 (17) | 42 (18) |
| Male sex | 7937 (78.3) | 3998 (78.9) | 3939 (77.9) |
| Penetrating injury | 861 (8.5) | 568 (11.2) | 293 (5.8) |
| Circumstances | |||
| Road traffic injury | 5598 (55.2) | 3014 (59.5) | 2549 (50.4) |
| Fall | 3053 (30.1) | 1231 (24.3) | 1805 (35.7) |
| Stabbing | 605 (5.9) | 399 (7.9) | 201 (4.0) |
| Gun shot | 250 (2.5) | 169 (3.3) | 80 (1.6) |
| Prehospital systolic blood pressure, mm Hg | |||
| Mean (SD) | 117 (32) | 109 (34) | 126 (2.5) |
| <90 mm Hg | 1259 (12.4) | 946 (18.7) | 313 (6.2) |
| Prehospital Glasgow Coma Scale score | |||
| 3-8 | 1518 (15.0) | 889 (17.5) | 629 (12.4) |
| 9-13 | 963 (9.5) | 517 (10.2) | 446 (8.8) |
| 13-15 | 7453 (73.6) | 3648 (72.0) | 3805 (75.2) |
| Injury Severity Score | |||
| Mean (SD) | 17 (14) | 18 (15) | 17 (13) |
| 0-15 | 5313 (52.5) | 2679 (52.9) | 2634 (52.1) |
| 16-24 | 2034 (20.1) | 1013 (20.0) | 1021 (20.2) |
| 25-34 | 1757 (17.4) | 818 (16.1) | 939 (18.6) |
| ≥35 | 966 (9.5) | 554 (10.9) | 412 (8.1) |
| Overall Abbreviated Injury Scale score ≥3 | 6737 (66.5) | 3302 (65.2) | 3435 (67.9) |
| Severe head injury (Abbreviated Injury Scale–head score ≥3) | 2724 (26.9) | 1346 (26.6) | 1378 (27.2) |
| Secondary transfer | |||
| In-hospital mortality | 968 (9.6) | 566 (11.2) | 402 (7.9) |
Abbreviation: TRENAU, Trauma System du Réseau Nord Alpin des Urgences.
The median TPT was 73 (interquartile range [IQR], 54-100) minutes in the TraumaBase cohort and 60 (IQR, 45-80) minutes in the TRENAU cohort (eTable 3 in the Supplement). The median TPT was 65 (IQR, 49-90) minutes for the combined cohort, with 4067 of 10 126 cases (40.2%) presenting a TPT shorter than 60 minutes. Three-quarters of patients (7434 of 10 126 [73.4%]) were transported by land, and 9098 of 10 126 (89.8%) were admitted to a designated trauma center.
In addition, TPT increased with the number of prehospital interventions performed. Indeed, a TPT lower than 60 minutes involved intubation and vasopressor use in 537 of 4049 patients (13.3%) and 228 of 4047 patients (5.6%), respectively, whereas a TPT longer than 120 minutes involved intubation and vasopressor use in 458 of 994 patients (46.1%) and 185 of 994 patients (18.6%), respectively (eTable 4 in the Supplement). Characteristics of excluded patients were similar to those who were included in the analysis, except with a slight difference in the mechanism of injury (road traffic: included patients, 5598 of 10 126 [55.3%] vs excluded patients, 1551 of 3633 [42.7%]; falls: included patients, 3053 of 10 126 [30.2%] vs excluded patients, 1389 of 3633 [38.2%]).
Primary Outcome
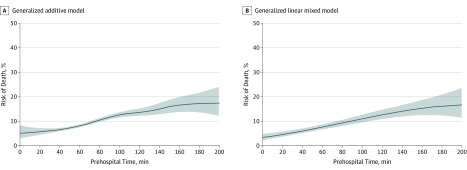
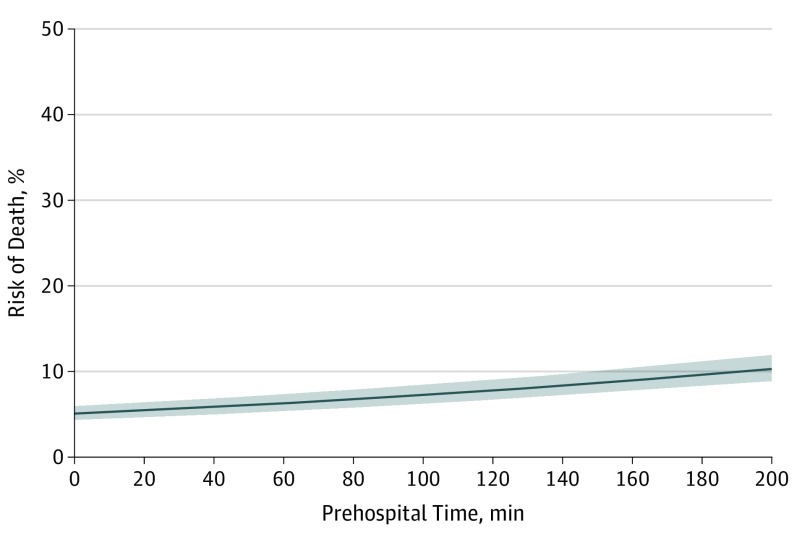
Unadjusted GLMM and GAM showed a significant, progressive increase of all-cause mortality with TPT (odds ratio [OR], 1.09 [95% CI, 1.07-1.11]; P < .001; Figure 1). Increasing 30-minute categories of TPT were associated with a markedly and constant increase in the risk of in-hospital death (total: 9.6% [95% CI, 9.0%-10.1%]; 0-29 minutes: 5.3% [95% CI, 3.6%-4.6%]; ≥180 minutes, 19.4% [95% CI, 13.3%-27.3%]; Table 2). Odds of death increased by 9% for each 10-minute increase in TPT (OR, 1.09 [95% CI, 1.07-1.11]; Table 3) and by 4% after adjustment for confounders (OR, 1.04 [95% CI, 1.01-1.07]; Figure 2; Table 3). The post hoc power calculation demonstrated a study power of 100%.
Figure 1. Unadjusted Models Representing the Risk of Death From All Causes, per Prehospital Time, Truncated at 200 Minutes.
A, Generalized additive model: area under the curve, 0.59 (95% CI, 0.57-0.61); internal overall calibration (expected over observed), 1.00 (95% CI, 0.94-1.06); and calibration slope, 1.03 (95% CI, 0.82-1.23). B, Generalized linear mixed model: area under the curve, 0.59 (95% CI, 0.57-0.61); internal overall calibration (expected over observed), 1.01 (95% CI, 0.94-1.07); and calibration slope, 0.99 (95% CI, 0.79-1.19). In both graphs, the shaded area represents the 95% CIs.
Table 2. Primary and Secondary Outcomes According to Prehospital Time.
| Total Prehospital Time, mina | Total, No. | Overall In-Hospital Death | Death Attributable to Head Injury | Death Attributable to Bleeding | |||
|---|---|---|---|---|---|---|---|
| Patients, No. | % (95% CI) | Patients, No. | % (95% CI) | Patients, No. | % (95% CI) | ||
| 0-29 | 514 | 27 | 5.3 (3.6-7.6) | 13 | 2.5 (1.5-4.3) | 8 | 1.6 (0.8-3.1) |
| 30-59 | 3535 | 244 | 6.9 (6.1-7.8) | 129 | 3.7 (3.1-4.3) | 53 | 1.5 (1.1-2.0) |
| 60-89 | 3459 | 344 | 9.9 (9.0-11.0) | 179 | 5.2 (4.5-6.0) | 63 | 1.8 (1.4-2.3) |
| 90-119 | 1624 | 208 | 12.8 (11.3-14.5) | 109 | 6.7 (5.6-8.0) | 36 | 2.2 (1.6-3.1) |
| 120-179 | 870 | 121 | 13.9 (11.8-16.4) | 55 | 6.3 (4.9-8.1) | 19 | 2.2 (1.4-3.4) |
| ≥180 | 124 | 24 | 19.4 (13.3-27.3) | 16 | 12.9 (8.0-20.0) | 3 | 2.4 (0.8-7.2) |
| Total | 10 126 | 968 | 9.6 (9.0-10.1) | 501 | 5.0 (4.5-5.4) | 182 | 1.8 (1.5-2.1) |
| P value for homogeneity test | NA | NA | <.001 | NA | <.001 | NA | .467 |
Abbreviation: NA, not available.
Total prehospital time, arrival of the physician-led prehospital care team on scene to arrival at the hospital.
Table 3. Association Between Outcome and Prehospital Timea.
| Death by Type | Odds Ratio by Generalized Linear Mixed Model (95% CI)b | P Value |
|---|---|---|
| Univariable Analysis | ||
| Overall death | 1.09 (1.07-1.11) | <.001 |
| Death attributable to head injury | 1.09 (1.06-1.11) | <.001 |
| Death attributable to bleeding | 1.04 (1.00-1.09) | .04 |
| Multivariable Analysis | ||
| Overall death | 1.04 (1.01-1.07) | .002 |
| Death attributable to head injury | 1.03 (1.00-1.07) | .15 |
| Death attributable to bleeding | 1.00 (0.99-1.02) | .24 |
Generalized linear model with random effect by registry and emergency medical system; adjustment for individual confounders as logarithmic function (prehospital time, age, systolic blood pressure, Injury Severity Score, and Glasgow Coma Scale score).
Odds ratio for increase of 10 minutes in prehospital time.
Figure 2. Adjusted Association Between Death and Prehospital Time.
Multivariable generalized linear mixed model representing the risk of death from all causes according to prehospital time, adjusted for individual confounder as logarithmic function (age, systolic blood pressure, Glasgow Coma Score scale, and Injury Severity Score): area under the curve, 0.96 (95% CI, 0.95-0.96); internal overall calibration (expected over observed), 1.00 (95% CI, 0.96-1.04); and calibration slope, 1.00 (95% CI, 0.94-1.06). The full model is presented in eTable 5 in the Supplement. The shaded area represents the 95% CIs.
Secondary Outcomes
Increasing 30-minute categories of TPT were associated with a progressive and constant increase in the risk of death attributable to head injury (total: 5.0% [95% CI, 4.5%-5.4%]; 0-29 minutes: 2.5% [95% CI, 1.5%-4.3%]; ≥180 minutes, 12.9% [95% CI, 8.0%-20.0%]; Table 2). This association was also observed, although less markedly, when considering death from bleeding (total: 1.8% [95% CI, 1.5%-2.1%]; 0-29 minutes: 1.6% [95% CI, 0.8%-3.1%]; ≥180 minutes, 2.4% [95% CI, 0.8%-7.2%]; Table 2). Unadjusted odds of death attributable to head injury increased by 9% for each 10-minute increase in TPT (OR, 1.09 [95% CI, 1.07-1.11]), while unadjusted OR of death attributable to bleeding increased by 4% (1.04 [95% CI, 1.01-1.07]; Table 3). When adjusting for confounders, the association of TPT with in-hospital death attributable to head and bleeding injury showed a nonsignificant increase (Table 3).
Discussion
The main finding of this study is that longer TPT is independently associated with increasing all-cause in-hospital mortality in a physician-staffed trauma system. To the best of our knowledge, this is the first study reporting such an association in a physician-staffed EMS in Europe.
The increase of mortality with increasing TPT appears to be common sense. However, existing comparative data on TPT and mortality in physician-staffed EMSs are limited and conflicting.20,21 Although time would be considered an independent exposure variable, it remains invariably dependent on exposure variables, such as physiology, severity of injury, and prehospital interventions. Concordantly, it was justifiable to assume that TPT could only be the result of multifactorial complexity, thereby challenging its independent association with outcome. Nevertheless, by accounting for complexity (ie, age, ISS, GCS score, and shock), time remained an independent exposure variable corroborating studies conducted in North America,22 although other studies suggest that a physician-led team exerts a positive influence on outcome,12,22 even when TPT is longer.
The association of TPT and mortality implies that time is an independent exposure that should be a management objective. Observed TPT were comparable with other European physician-staffed EMSs13,23,24 but longer than in paramedic-staffed EMS.25 A propensity-matched analysis reported that critical prehospital interventions were associated with a decrease in mortality without affecting TPT.14 Clinicians constantly negotiate a trade-off between safely performing crucial interventions and limiting time on scene. The answer to this challenge may not be dichotomic concepts such as scoop and run, stay and play, or play and run. Instead, we suggest framing this challenge as a ratio between time spent on scene and interventions performed to meet the patient's critical needs. This ratio is specific to every case and prehospital situation. We suggest to call this the intervention-to-time ratio. This ratio implies that the time every prehospital intervention required must be tailored to each patient and counterbalanced by its potential gain in survival. A recent cohort study of trunk trauma5 revealed increased mortality in patients in shock with incompressible trunk trauma, long before any definitive hemorrhage control is possible; hence the advocacy of some people in favor of very advanced prehospital resuscitation and hemorrhage control, such as resuscitative endovascular balloon occlusion of the aorta, which carries the risk of prolonging scene time. The TPT stems from aspects crucial to prehospital care other than resuscitation, including extrication, communication with command or dispatch and the receiving center, and transport time.26 The whole process needs streamlining to keep TPT as short and safe as possible, to only address the targeted and individualized essential needs of each patient that are of benefit to that patient.
When looking at the specific causes of death, the adjusted model (Table 3; Figure 2) showed a nonsignificant association of time with hemorrhage-associated mortality. The critical association of time and trauma hemorrhage was recently observed, demonstrating peak mortality from hemorrhage at 37 minutes.27 This circumstance might have reduced the size of the association with death by hemorrhage in the model. Both registries only include patients who arrived alive at the hospital. Ball et al28 indicated that with shorter TPT, more patients arrived alive but then died subsequently. Future studies need to address this question and include all patients deceased on scene.
In opposition to previous reports,29 the adjusted model did not show a significant association of TPT and TBI-induced mortality. Affirmation of TBI as the cause of death is difficult since patients with head injuries commonly have other confounding causes of death (eg, hemorrhage, thoracic trauma). Moreover, a substantial proportion of patients with TBI ultimately die after withdrawal of treatment and are registered as such, which may have biased the true proportion of death attributable to TBI.
This study has several strengths. Data were extracted from 2 established registries with robust data management. These data were collected from 2 geographically and structurally distinct regions with different trauma systems. The TRENAU system qualifies as inclusive, with 3 designated levels of care.16 The Paris system tends to be exclusive, with 6 designated level I centers absorbing the most regional trauma cases.17 These characteristics apply to other European EMS, supporting the external validity and generalizability of the observations made. Thus, the present model appears robust and generalizable. As eFigure 2 in the Supplement illustrates, mortality retains a coherent and consistent association to well-documented variables and confounders.
Limitations
This study carries a number of limitations linked to its design. Based on a prospective data collection and with adequate control of potential confounders, it appeared appropriate, however, to examine the hypothesis in a sufficiently large real-world cohort. A physician closing the case determined the cause of death, and a subjective bias cannot be excluded, which is in analogy to most existing registries, unless postmortem computed tomographic scans and/or systematic autopsies become standard. Only patients who arrived alive in the hospital were included in the study, a feature shared with most established trauma registries that may have reduced the sign of the association of hemorrhage-induced mortality and time. The choice of adjustment variables may seem arbitrary and the number of variables limited. However, the adjustment aimed to compensate for case complexity and case mix in a simple but robust way. Patients with shock (as indicated by systolic blood pressure <90 mm Hg) and/or TBI (low GCS scores) and high injury load (high ISS) and elderly patients account for the greater part of this complexity, since they may require prehospital resuscitation. Hence, the models did not include any specific prehospital interventions, because they are well correlated and share a high collinearity with any of the 4 adjustment variables in the model and are part of the so-called causal pathway.
Prehospital interventions in France focus on advanced airway management, fluid and vasoactive therapy, and simple hemostatic measures (eTable 4 in the Supplement). At the time of the study, blood product use was rare, and advanced surgical techniques were exceptional.
We decided to perform complete case analysis instead of performing multiple imputation. We cannot exclude that exclusion of observations led to selection bias. Multiple imputation is not always superior to complete case analysis; in particular, if missing data are not missing at random, imputation may generate a bias toward the null.30 In this study, it seems inappropriate to impute data on prehospital time without precise geographical location, because ambulances in France are currently not systematically equipped with geographic positioning systems.
Missing data led to the exclusion of 23% of patients from both registries. However, apart from a slight difference in the mechanism of injury, patients who were excluded shared the characteristics and severity of injury similar to the patients who were included. This study included cases from a large urban and a rural, mountainous area, supporting the generalizability of the results to most of European and mature trauma systems. A cluster effect cannot be excluded. The use of a mixed model with a random effect should however control for this bias. These results may less apply to very remote isolated regions and or systems with a higher incidence of penetrating injury.
Conclusions
This study demonstrates an independent association of in-hospital, all-cause mortality in trauma with total prehospital time in a physician-staffed EMS in France, even after adjustment for case complexity. These results imply that prehospital time management should become a management objective. Both findings plead for further streamlining of prehospital trauma care and the need to define the optimal intervention-to-time ratio.
eTable 1. Complete list of collected variables
eTable 2. Characteristics of patients excluded for analysis and missing data
eTable 3. Transportation mode and time according to regional database.
eTable 4. Pre-hospital Interventions and Total Pre-hospital Time
eTable 5. Generalized Linear Mixed Model with primary outcome all-causes of death.
eTable 6. Generalized Linear Mixed Model with primary outcome all-causes of death.
eFigure 1. Flowchart of study
eFigure 2. Adjusted Generalized Additive Model for individual confounders as logarithmic function (prehospital time, age, systolic blood pressure, Injury Severity Score, GCS); the y-axis represents the functional risk of death
References
- 1.Sampalis JS, Lavoie A, Williams JI, Mulder DS, Kalina M. Impact of on-site care, prehospital time, and level of in-hospital care on survival in severely injured patients. J Trauma. 1993;34(2):252-261. doi: 10.1097/00005373-199302000-00014 [DOI] [PubMed] [Google Scholar]
- 2.Sampalis JS, Denis R, Lavoie A, et al. . Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46(4):565-579. doi: 10.1097/00005373-199904000-00004 [DOI] [PubMed] [Google Scholar]
- 3.Boyd DR, Cowley RA. Comprehensive regional trauma/emergency medical services (EMS) delivery systems: the United States experience. World J Surg. 1983;7(1):149-157. doi: 10.1007/BF01655923 [DOI] [PubMed] [Google Scholar]
- 4.Rogers FB, Rittenhouse KJ, Gross BW. The golden hour in trauma: dogma or medical folklore? Injury. 2015;46(4):525-527. doi: 10.1016/j.injury.2014.08.043 [DOI] [PubMed] [Google Scholar]
- 5.Alarhayem AQ, Myers JG, Dent D, et al. . Time is the enemy: mortality in trauma patients with hemorrhage from torso injury occurs long before the “golden hour”. Am J Surg. 2016;212(6):1101-1105. doi: 10.1016/j.amjsurg.2016.08.018 [DOI] [PubMed] [Google Scholar]
- 6.Pepe PE, Wyatt CH, Bickell WH, Bailey ML, Mattox KL. The relationship between total prehospital time and outcome in hypotensive victims of penetrating injuries. Ann Emerg Med. 1987;16(3):293-297. doi: 10.1016/S0196-0644(87)80174-9 [DOI] [PubMed] [Google Scholar]
- 7.Pons PT, Markovchick VJ. Eight minutes or less: does the ambulance response time guideline impact trauma patient outcome? J Emerg Med. 2002;23(1):43-48. doi: 10.1016/S0736-4679(02)00460-2 [DOI] [PubMed] [Google Scholar]
- 8.Lerner EB, Billittier AJ, Dorn JM, Wu Y-WB. Is total out-of-hospital time a significant predictor of trauma patient mortality? Acad Emerg Med. 2003;10(9):949-954. doi: 10.1197/S1069-6563(03)00313-0 [DOI] [PubMed] [Google Scholar]
- 9.Newgard CD, Meier EN, Bulger EM, et al. ; ROC Investigators . Revisiting the “golden hour”: an evaluation of out-of-hospital time in shock and traumatic brain injury. Ann Emerg Med. 2015;66(1):30-41, 41.e1-41.e3. doi: 10.1016/j.annemergmed.2014.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kotwal RS, Howard JT, Orman JA, et al. . The effect of a golden hour policy on the morbidity and mortality of combat casualties. JAMA Surg. 2016;151(1):15-24. doi: 10.1001/jamasurg.2015.3104 [DOI] [PubMed] [Google Scholar]
- 11.Haas B, Nathens AB. Pro/con debate: is the scoop and run approach the best approach to trauma services organization? Crit Care. 2008;12(5):224. doi: 10.1186/cc6980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yeguiayan J-M, Garrigue D, Binquet C, et al. ; French Intensive Care Recorded In Severe Trauma Study Group . Medical pre-hospital management reduces mortality in severe blunt trauma: a prospective epidemiological study. Crit Care. 2011;15(1):R34. doi: 10.1186/cc9982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wyen H, Lefering R, Maegele M, et al. ; TraumaRegister DGU . The golden hour of shock—how time is running out: prehospital time intervals in Germany–a multivariate analysis of 15,103 patients from the TraumaRegister DGU(R). Emerg Med J. 2013;30(12):1048-1055. doi: 10.1136/emermed-2012-201962 [DOI] [PubMed] [Google Scholar]
- 14.Meizoso JP, Valle EJ, Allen CJ, et al. . Decreased mortality after prehospital interventions in severely injured trauma patients. J Trauma Acute Care Surg. 2015;79(2):227-231. doi: 10.1097/TA.0000000000000748 [DOI] [PubMed] [Google Scholar]
- 15.Bouzat P, Ageron F-X, Brun J, et al. ; TRENAU group . A regional trauma system to optimize the pre-hospital triage of trauma patients. Crit Care. 2015;19:111. doi: 10.1186/s13054-015-0835-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamada SR, Gauss T, Duchateau F-X, et al. . Evaluation of the performance of French physician-staffed emergency medical service in the triage of major trauma patients. J Trauma Acute Care Surg. 2014;76(6):1476-1483. doi: 10.1097/TA.0000000000000239 [DOI] [PubMed] [Google Scholar]
- 17.Riou B, Thicoïpé M, Atain-Kouadio P. Comment Évaluer la Gravité? in SAMU de France. Actualités en Réanimation Préhospitalière: le Traumatisé Grave. Paris, France: SFEM Éditions, 2003; 115-128. [Google Scholar]
- 18.Duranteau J, Asehnoune K, Pierre S, Ozier Y, Leone M, Lefrant J-Y. Recommandations sur la réanimation du choc hémorragique. Anesthésie & Réanimation. 2015;1(1):62-74. doi: 10.1016/j.anrea.2014.12.007 [DOI] [Google Scholar]
- 19.Ringdal KG, Coats TJ, Lefering R, et al. ; Utstein TCD expert panel . The Utstein template for uniform reporting of data following major trauma: a joint revision by SCANTEM, TARN, DGU-TR and RITG. Scand J Trauma Resusc Emerg Med. 2008;16:7. doi: 10.1186/1757-7241-16-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harmsen AMK, Giannakopoulos GF, Moerbeek PR, Jansma EP, Bonjer HJ, Bloemers FW. The influence of prehospital time on trauma patients outcome: a systematic review. Injury. 2015;46(4):602-609. doi: 10.1016/j.injury.2015.01.008 [DOI] [PubMed] [Google Scholar]
- 21.Jung K, Huh Y, Lee JC, et al. . Reduced mortality by physician-staffed HEMS dispatch for adult blunt trauma patients in Korea. J Korean Med Sci. 2016;31(10):1656-1661. doi: 10.3346/jkms.2016.31.10.1656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fukuda T, Ohashi-Fukuda N, Kondo Y, Hayashida K, Kukita I. Association of prehospital advanced life support by physician with survival after out-of-hospital cardiac arrest with blunt trauma following traffic collisions: japanese registry-based study. JAMA Surg. 2018;153(6):e180674. doi: 10.1001/jamasurg.2018.0674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Funder KS, Petersen JA, Steinmetz J. On-scene time and outcome after penetrating trauma: an observational study. Emerg Med J. 2011;28(9):797-801. doi: 10.1136/emj.2010.097535 [DOI] [PubMed] [Google Scholar]
- 24.Timm A, Maegele M, Lefering R, Wendt K, Wyen H; TraumaRegister DGU(®) . Pre-hospital rescue times and actions in severe trauma. a comparison between two trauma systems: Germany and the Netherlands. Injury. 2014;45(suppl 3):S43-S52. doi: 10.1016/j.injury.2014.08.017 [DOI] [PubMed] [Google Scholar]
- 25.Ruelas OS, Tschautscher CF, Lohse CM, Sztajnkrycer MD. Analysis of prehospital scene times and interventions on mortality outcomes in a national cohort of penetrating and blunt trauma patients. Prehosp Emerg Care. 2018;22(6):691-697. doi: 10.1080/10903127.2018.1448494 [DOI] [PubMed] [Google Scholar]
- 26.Brown JB, Rosengart MR, Forsythe RM, et al. . Not all prehospital time is equal: Influence of scene time on mortality. J Trauma Acute Care Surg. 2016;81(1):93-100. doi: 10.1097/TA.0000000000000999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oyeniyi BT, Fox EE, Scerbo M, Tomasek JS, Wade CE, Holcomb JB. Trends in 1029 trauma deaths at a level 1 trauma center: Impact of a bleeding control bundle of care. Injury. 2017;48(1):5-12. doi: 10.1016/j.injury.2016.10.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ball CG, Williams BH, Tallah C, Salomone JP, Feliciano DV. The impact of shorter prehospital transport times on outcomes in patients with abdominal vascular injuries. J Trauma Manag Outcomes. 2013;7(1):11. doi: 10.1186/1752-2897-7-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dinh MM, Bein K, Roncal S, Byrne CM, Petchell J, Brennan J. Redefining the golden hour for severe head injury in an urban setting: the effect of prehospital arrival times on patient outcomes. Injury. 2013;44(5):606-610. doi: 10.1016/j.injury.2012.01.011 [DOI] [PubMed] [Google Scholar]
- 30.White IR, Carlin JB. Bias and efficiency of multiple imputation compared with complete-case analysis for missing covariate values. Stat Med. 2010;29(28):2920-2931. doi: 10.1002/sim.3944 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Complete list of collected variables
eTable 2. Characteristics of patients excluded for analysis and missing data
eTable 3. Transportation mode and time according to regional database.
eTable 4. Pre-hospital Interventions and Total Pre-hospital Time
eTable 5. Generalized Linear Mixed Model with primary outcome all-causes of death.
eTable 6. Generalized Linear Mixed Model with primary outcome all-causes of death.
eFigure 1. Flowchart of study
eFigure 2. Adjusted Generalized Additive Model for individual confounders as logarithmic function (prehospital time, age, systolic blood pressure, Injury Severity Score, GCS); the y-axis represents the functional risk of death