Abstract
Background:
We determined the risk thresholds above which statin use would be more likely to provide a net benefit for people over the age of 75 years without history of cardiovascular disease (CVD).
Methods:
An exponential model was used to estimate the differences in expected benefit and harms in people treated with statins over a 10-year horizon versus not treated. The analysis was repeated 100,000 times to consider the statistical uncertainty and produce a distribution of the benefit–harm balance index from which we determined the 10-year CVD risk threshold where benefits outweighed the harms. We considered treatment estimates from trials and observational studies, baseline risks, patient preferences, and competing risks of non-CVD death, and statistical uncertainty.
Results:
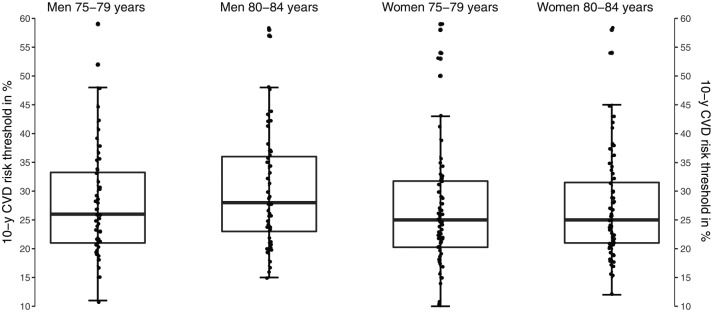
Based on average preferences, statins were more likely to provide a net benefit at a 10-year CVD risk of 24% and 25% for men aged 75–79 years and 80–84 years, respectively, and 21% for women in both age groups. However, these thresholds varied significantly depending on differences in individual patient preferences for the statin-related outcomes, with interquartile ranges of 21–33% and 23–36% for men aged 75–79 years and 80–84 years, respectively, as well as 20–32% and 21–32% for women aged 75–79 years and 80–84 years, respectively.
Conclusions:
Statins would more likely provide a net benefit for primary prevention in older people taking the average preferences if their CVD risk is well above 20%. However, the thresholds could be much higher or lower depending on preferences of individual patients, which suggests more emphasis should be placed on individual-based decision-making, instead of recommending statins for everyone based on a single or a small number of thresholds.
Keywords: benefit–harm balance, cardiovascular disease risk threshold, lipid-lowering drugs, primary CVD prevention, statins
Introduction
People over the age of 75 years, an age group that is increasing,1 are at a substantially increased risk of cardiovascular disease (CVD) and age-related morbidity and mortality compared with younger people.2 Primary preventive measures remain important in this age group, both in terms of lifestyle modification and drug treatment. Statins are the most widely used preventive drugs for CVD and are one of the most frequently used drug classes worldwide. However, their use is controversial in older people because there is significantly less evidence for this age group and the risk for statin-related harms increases with age, which could potentially offset their positive effects. The US Preventive Services Task Force concluded in a recent review that older people are underrepresented in trials and there is insufficient evidence to draw a robust conclusion about the balance of benefits and harms of statins for primary prevention in this age group.3,4 A limited amount of evidence from trials and observational studies has, however, become available recently that demonstrated the limited effects of statins for reducing CVD or all-cause mortality in individuals aged 75 years or older.5–7 These results raise the question in which age group the expected benefits of statins outweigh the expected harms.
A previous benefit–harm balance study found that in people aged 40–74 years, the 10-year CVD risk at which to initiate statins was between 14% and 22%, depending on age and sex, in order to achieve more benefits than harms from statin use.8 This is above the commonly used 7.5% or 10% 10-year CVD risk thresholds proposed to initiate statins for primary prevention in most guidelines issued by a number of different societies in cardiology;4,9 yet for most age groups, this figure is lower than the 20% proposed threshold in general or family medicine guidelines, including the German guideline.10 The study demonstrated that the benefit–harm balance of statins is less favorable with increasing age as the risks of experiencing harms increases proportionally more than the absolute reduction in CVD risk. Increased risk of harms including type 2 diabetes, cataracts, liver and kidney dysfunction, myopathy, and cognitive dysfunction– potential harms of statins– can be of increased concern for people over the age of 75 years because they potentially contribute to increased frailty and disability. However, neither the previous study nor any other analysis, to the best of the authors’ knowledge, assessed the benefit–harm balance of statins for this specific age group. In addition, the previous study did not assess the effect of different patient preferences on the benefit harm balance. Therefore, the current study aimed to assess the benefit–harm balance of low to moderate dose statins in adults over the age of 75 years for primary prevention of CVD, to determine baseline CVD risk thresholds above which a net benefit is achieved, on average, and to assess how the risk thresholds vary according to individual patient preferences.
Methods
Study design
We conducted a benefit–harm balance modeling study that included the following five standard steps.11 First, the exact question including the population of interest, intervention, comparator, and outcomes were specified. The population of interest were individuals aged 75 years or older with no prior history of CVD. The intervention was low to moderate dose statins compared with no statin use. The benefit outcome of interest was CVD (composite of unstable angina, myocardial infarction [MI], and ischemic stroke), and the potential harm outcomes included myopathy and muscle weakness, type 2 diabetes, renal and hepatic dysfunction, cancer, cognitive impairment, hemorrhagic stroke, digestive distress, and cataracts. The outcomes were selected based on our previous survey and trial reports.12,13 Second, a systematic approach was followed to identify and select the most valid and applicable evidence for the target population, as described previously and further described in the following.11 The three key input parameters in the model include relative effect estimates of statins on benefit and harm outcomes, baseline risks of outcomes (in people not using statins), and preference weighting for benefit and harm outcomes from a patient’s perspective. Third, the statistical analysis used was an exponential model to estimate the expected number of events for the benefit and harm outcomes in people using statins over a 10-year horizon versus not using statins, that also took into account patient preferences, competing risks, and statistical uncertainty to produce a single index indicating the benefit–harm balance. This method was first developed by Gail and colleagues14 from the National Cancer Institute (Gail/NCI) to assess the net benefit of tamoxifen in preventing breast cancer. We extended this approach to fit the research question, in particular to determine the risk thresholds above which the benefits of statins outweigh their harms (see the analysis).8 Fourth, sensitivity analyses were conducted to test alternative assumptions as described further below. Finally, the benefit–harm balance results were interpreted.
Parameters required for benefit–harm balance assessment
Treatment effect estimates
We searched for primary prevention trials specific to older people to derive the most valid, applicable, and precise evidence for the effects of statins on CVD. We also searched for large and high-quality observational studies in anticipation of scarce evidence from trials related to the target population. We could not identify a primary prevention trial that only included people aged 75 years or older. Two trials, the Study Assessing Goals in the Elderly (SAGE) and the pravastatin in elderly individuals at risk of vascular disease study (PROSPER), included people over the age of 65 years. However, SAGE was a secondary prevention trial and PROSPER was conducted in mixed primary and secondary prevention populations.15,16 We identified a recent and high-quality systematic review that provided the most valid and applicable estimates on the beneficial effects of statins for primary prevention of CVD in people over the age of 75 years, which pooled individual patient data from multiple trials.7 The majority of the data in this review primarily came from four trials,17 including the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial–Lipid-Lowering Trial (ALLHAT-LLT) that tested 40 mg/dl pravastatin daily versus placebo,18 the Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT-LLA) that evaluated 10 mg/dl atorvastatin daily versus placebo,19 the Justification for Use of Statins in Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER) that evaluated 20 mg/dl rosuvastatin daily compared with placebo,20 and the Heart Outcomes Prevention Evaluation (HOPE-3) trial that evaluated outcomes of 10 mg/dl rosuvastatin daily compared with placebo.21 The ALLHAT-LLT study had a higher proportion of patients with diabetes among those without prior CVD, but this trial contributed the least amount of data among the four trials (see the original publication17).
We did not find any trial that included only people over the age of 75 years that assessed the harm outcomes. The systematic review described above also did not report on harm outcomes except cancer, but the effect on cancer was for mixed populations.7,17 While a post hoc subgroup analysis of the JUPITER trial reported harm estimates for people aged 70–97 years,22 JUPITER evaluated moderate to high-dose rosuvastatin (20 mg/dl), which is unlikely to be used as a routine dose for primary prevention, particularly in older people. In addition, over 56% of the participants in the age group of 70–97 years were aged between 70 and 75 years,17 which was not our target population. Therefore, we did not consider this trial as the only input data for the analysis in order not to overestimate the risk of harms. We relied on the four trials that tested low, moderate, and moderate–high doses.18,19,21,22 Unfortunately, none of the studies reported on all of the harm outcomes consistently. This led to difficulties in including all harm outcomes in our analysis. We considered the harm outcomes if they were defined and measured consistently across the included trials. Finally, the included harm outcomes were renal impairment, diabetes, myopathy, and cancer. In addition, non-CVD mortality was included (i.e. deaths unrelated to statins) as a competing risk to take into account the increased death rates in older populations. If this was disregarded, it would overestimate the expected number of prevented or excess events.
Moreover, we considered observational studies for some of the harm outcomes, in particular for diabetes and cancer,5,6 and consolidated them with the above trials.8 That is, while trials are often considered as the gold standard to provide reliable effect estimates because they are usually powered to detect efficacy (here reduction in CVD),23 observational studies are often more suitable to assess the harms of treatments.24 Therefore, we used the effect estimate for the reduction in CVD from trials only in the main analysis and performed a sensitivity analysis taking a combined effect for CVD reduction from more recently published large observational studies.5,6
Baseline risks
Baseline risks for the benefit and harm outcomes are required to estimate the absolute number of prevented or excess events. We searched for large registries and observational studies that provide real-world baseline risks for people aged 75 years or older, rather than taking rates from trials (control arm). The baseline risk for CVD to initiate statins is what we aimed to determine from this study. However, we took empirical age- and sex-specific baseline risks for the harm outcomes, including diabetes, cancer, and competing risk for non-CVD mortality for Switzerland from the Global Burden of Disease (GBD) estimates,25 and renal impairment and myopathy from the UK General Practitioner database (summarized in Table 1).26 We chose to take data from Switzerland for some of the baseline risks because the outcome preferences were elicited there and the outcome risks were moderate in Switzerland, therefore avoiding a number of extreme results. For the risks of renal impairment and myopathy, which were not available in the Swiss population, the rates from the UK did not represent extreme values because the source study only included moderate-to-severe cases (in addition, they were average, not age or sex specific rates).
Table 1.
Summary of input data.
| Outcomes | Treatment effect |
Preference |
Baseline rate in 10,000 people
per annum (95% CI) |
|||
|---|---|---|---|---|---|---|
| RR (95% CI) | Estimate (95% CI)§ | Men, 75–79 years old | Men, 80–84 years old | Women, 75–79 years old | Women, 80–84 years old | |
| CVD composite | 0.922 (0.773–1.099) | 0.645 (0.553–0.692) | NA | NA | NA | NA |
| Moderate/severe renal impairment | 1.332 (0.947–1.357) | 0.262 (0.242–0.293) | 7.4 (6.9–7.9) | 7.4 (6.9–7.9) | 6.0 (5.6–6.4) | 6.0 (5.6–6.4) |
| Type 2 diabetes‡ | 1.038 (0.935–1.152) | 0.378 (0.347–0.424) | 141 (103–182) | 116 (84–150) | 132 (98–168) | 109 (77–140) |
| Moderate/severe myopathy | 1.474 (0.413–5.260) | 0.255 (0.253–0.256) | 3.6 (3.4–3.9) | 3.6 (3.4–3.9) | 3.2 (2.9–3.5) | 3.2 (2.9–3.5) |
| All cancers‡ | 1.012 (0.932–0.100) | 0.859 (0.843–0.880) | 335 (299–377) | 372 (337–404) | 193 (176–212) | 213 (195–232) |
| Non-CVD mortality† | NA | NA | 197(185–210) | 361 (342–381) | 115 (108–124) | 218 (205–231) |
Competing risk.
Outcomes with convergent estimates from trials and observational studies (combined using inverse variance averaged weighting).8
Preferences measured as surface under cumulative ranking curve estimated from best–worst scaling survey.
CVD, cardiovascular disease; NA, not applicable; RR, risk ratio.
Outcome preferences
To balance the CVD events prevented by statin use against the excess number of harm events, outcomes need to be weighted according to their relative importance or patient preferences. We considered patient preferences from a best-minus-worst scaling (BWS) survey conducted in Switzerland to inform the choice of weightings on selected outcomes.12 We used both aggregated patient preferences so as to determine average risk thresholds as well as individual patient preferences in order to assess risk threshold variation.28 We used average preference weightings in the main analysis on a 0–1 scale estimated using the surface under the cumulative ranking curve (a network meta-analysis comparing the importance of outcomes).29 This method cannot estimate preferences for individuals. We calculated individual preference values (from 120 participants in the BWS survey) using best-minus-worst score (i.e., the number of times an outcome was selected as most worrisome minus the number of times it was selected as least worrisome across choice sets) and normalized them according to relative probabilities (Appendix Figure 1).
Of note, the preference for the benefit outcome was originally determined for each component of CVD events,12 not for CVD composite outcomes because of its wide range of manifestations that creates challenges when determining preferences from individual patients. We generated preference values for the CVD composite endpoint by taking into account the preference values of each CVD component and their frequency in the general populations (e.g., mild-to-moderate MIs were more frequent than severe or fatal MIs). The resulting preference for the composite CVD used in this analysis was equivalent to the weight of a moderate MI.
Subgroups
Our previous work highlighted different risk thresholds based on age and sex.8 Therefore, the risk thresholds in this analysis were determined for men and women aged 75–79 years and 80–84 years, separately taking the age and sex specific baseline risks and treatment effects into account. We did not include people aged 85 years or older in order to avoid inadequate conclusions because there was a very limited amount of evidence available for this age group.
Statistical analysis
The statistical analysis methods are briefly presented here, and the detailed methods are available in the literature.8 We calculated the expected number of prevented CVD events and excess harm events among 10,000 people treated with statins over a 10-year horizon versus an identical cohort not treated with statins. We calculated event numbers for men and women separately in different age groups, and at different 10-year baseline risks for CVD (1%, 2%, 3% etc.) until benefits outweighed harms. We weighted the differences in the expected number of prevented CVD events and excess harm events using the respective preference weightings and summed them across all outcomes to obtain a single benefit–harm balance index. We performed the analysis for 100,000 repetitions for each subgroup, considering the statistical uncertainty for each input parameter, to generate a distribution of the benefit–harm balance index. From this distribution, we calculated the probability that the index was positive for the different subgroups. Then, the defined net benefit was determined; i.e., the benefits outweighed harms, when the probability for the index being positive was at least 60%. This means that in 60% of the 100,000 repetitions, statins would be more likely to provide a net benefit compared with not taking statins. We defined net harm, or harms outweighed benefits, if the probability for the index being positive was less than 40%. Probabilities between 40% and 60% represented neither net benefit nor net harm.
Moreover, while it is important to estimate the clinical relevance of the thresholds, the absolute value of the benefit–harm balance index is difficult to interpret because it is a composite output of multiple parameters. In theory, the index can be interpreted as the number of prevented fatal CVD cases (with a maximum preference weight of 1.0) in 10,000 people treated with statins. However, we converted the index back into CVD composite outcome and moderate MI (i.e., dividing the index by the moderate MI preference weight), but preferred to report the prevented events equivalent to moderate MI with taking statins for the sake of effective communication (unlike CVD owing to its wide range of manifestations). We present these absolute events in 10,000 people with their uncertainty intervals based on the 5th and 95th percentiles derived from the respective distribution of benefit–harm balance index. This interpretation of the net prevented MI events should apply to the positive index only, not for the negative index where there would be no expected benefit. We performed all analyses using R version 3.3.2 (R Foundation for Statistical Computing).30
Sensitivity analyses
We determined the thresholds using an alternative assumption by taking all treatment effects from trials only (i.e. excluding observational studies for diabetes and cancer estimates). In addition, we ran the analysis with combined effect estimates of statins on CVD from trials (risk ratio, 0.922; 95% CI 0.773–1.099) and large and valid observational studies conducted from the database of the Catalan primary care system (hazard ratio 0.94; 95% CI 0.86–1.04) and French health care system database (hazard ratio 0.93; 95% CI 0.89–0.96).5,6 The hazard ratio was approximated to a risk ratio using a conversion equation.31
Ethics
This study was based on published and aggregated data for which no ethical approval was needed.
Results
Expected outcome events
The expected numbers of CVD and harm outcomes, with their uncertainty intervals in people treated with statins versus not treated are presented in Tables 2–5. The absolute expected prevented CVD events over 10 years of taking statins were higher in people at high risk of CVD, increasing from 6 in 10,000 people at a 1% 10-year baseline CVD risk to 153 in 10,000 people with a 25% 10-year baseline CVD risk. As a result, the magnitude of benefit increases across the risk spectrum, with people at higher risk deriving greater benefit. The expected number of harm events was assumed to be similar across the CVD risk spectrum. In 10,000 people taking statins daily for 10 years, the absolute expected excess risk of developing myopathy was 18 for men and 17 for women, and 12 in men and 10 in women for renal impairment, the same in both age groups. However, excess type 2 diabetes events were marginally different between the age groups (because of differences in baseline risks), with 44 per 10,000 men aged 75–79 years (35 events in ages 80–84 years) and 42 per 10,000 women aged 75–79 years (35 events in ages 80–84 years). Similarly, the expected number of cancer events was 32 per 10,000 men aged 75–79 years (33 events in ages 80–84 years) and 24 per 10,000 women aged 75–79 years (25 events in ages 80–84 years).
Table 2.
Probability of net benefit and expected benefit and harm outcomes in 10 years per 10,000 men aged 75–79 years.
| 10-y CVD risk (%) | Probability of net benefit (%) | Net prevented moderate MI | Benefit-harm index | CVD |
Myopathy |
Diabetes type 2 |
Renal impairment |
Cancer |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No statin | Statin | No statin | Statin | No statin | Statin | No statin | Statin | No statin | Statin | ||||
| 1 | 39.12 | –73 (–475, 309) | –47 (–306, 199) | 91 (90, 91) | 84 (72, 97) | 33 (31, 34) | 51 (26, 87) | 1208 (955, 1495) | 1252 (976, 1568) | 67 (64, 70) | 79 (47, 122) | 2600 (2391, 2820) | 2632 (2281, 3010) |
| 2 | 40.41 | –66 (–470, 316) | –43 (–303, 204) | 182 (181, 182) | 168 (145, 194) | 33 (31, 34) | 51 (26, 87) | 1208 (956, 1494) | 1252 (974, 1569) | 67 (64, 70) | 79 (47, 122) | 2600 (2390, 2820) | 2631 (2280, 3010) |
| 3 | 41.58 | –60 (–466, 323) | –39 (–300, 208) | 272 (271, 274) | 252 (217, 291) | 33 (31, 34) | 51 (26, 88) | 1208 (957, 1494) | 1252 (977, 1567) | 67 (64, 70) | 79 (47, 123) | 2601 (2390, 2821) | 2633 (2282, 3010) |
| 4 | 42.57 | –54 (–459, 330) | –35 (–296, 213) | 363 (362, 365) | 337 (290, 388) | 33 (31, 34) | 51 (26, 87) | 1209 (957, 1496) | 1253 (976, 1568) | 67 (64, 70) | 79 (47, 123) | 2600 (2389, 2819) | 2632 (2281, 3009) |
| 5 | 44.04 | –47 (–456, 340) | –30 (–294, 219) | 454 (452, 456) | 421 (363, 484) | 33 (31, 34) | 51 (26, 88) | 1208 (956, 1495) | 1252 (975, 1570) | 67 (64, 70) | 79 (47, 123) | 2600 (2390, 2820) | 2632 (2279, 3012) |
| 6 | 44.92 | –42 (–452, 348) | –27 (–292, 224) | 545 (542, 548) | 506 (436, 582) | 33 (31, 34) | 51 (26, 88) | 1208 (955, 1496) | 1252 (976, 1570) | 67 (64, 70) | 79 (47, 122) | 2601 (2390, 2821) | 2633 (2282, 3010) |
| 7 | 45.81 | –33 (–447, 357) | –22 (–288, 230) | 636 (633, 639) | 590 (510, 678) | 33 (31, 34) | 51 (26, 87) | 1208 (956, 1495) | 1252 (975, 1569) | 67 (64, 70) | 79 (47, 123) | 2601 (2392, 2821) | 2633 (2282, 3011) |
| 8 | 47.09 | –28 (–441, 365) | –18 (–285, 235) | 727 (724, 731) | 675 (583, 774) | 33 (31, 34) | 51 (26, 87) | 1209 (956, 1493) | 1253 (976, 1567) | 67 (64, 70) | 79 (47, 123) | 2601 (2390, 2821) | 2633 (2281, 3010) |
| 9 | 47.66 | –20 (–436, 376) | –13 (–281, 242) | 818 (814, 822) | 760 (657, 871) | 33 (31, 34) | 51 (26, 88) | 1209 (958, 1494) | 1253 (977, 1568) | 67 (64, 70) | 79 (47, 122) | 2600 (2389, 2821) | 2631 (2281, 3007) |
| 10 | 48.86 | –15 (–436, 385) | –10 (–281, 248) | 909 (905, 914) | 845 (731, 968) | 33 (31, 34) | 52 (26, 88) | 1208 (955, 1493) | 1252 (976, 1565) | 67 (64, 70) | 79 (47, 122) | 2600 (2390, 2819) | 2632 (2282, 3006) |
| 11 | 50.15 | –9 (–435, 395) | –6 (–281, 255) | 1000 (995, 1005) | 929 (805, 1066) | 33 (31, 34) | 51 (26, 87) | 1208 (957, 1493) | 1252 (976, 1567) | 67 (64, 70) | 79 (47, 122) | 2600 (2389, 2820) | 2631 (2278, 3010) |
| 12 | 50.84 | –2 (–428, 407) | –1 (–276, 262) | 1092 (1086, 1097) | 1014 (878, 1162) | 33 (31, 34) | 51 (26, 88) | 1207 (956, 1494) | 1251 (975, 1567) | 67 (64, 70) | 79 (47, 122) | 2601 (2390, 2822) | 2632 (2281, 3009) |
| 13 | 51.51 | 2 (–433, 414) | 1 (–279, 267) | 1183 (1177, 1188) | 1100 (955, 1259) | 33 (31, 34) | 51 (26, 87) | 1208 (956, 1495) | 1252 (976, 1569) | 67 (64, 70) | 79 (47, 123) | 2600 (2390, 2820) | 2633 (2281, 3010) |
| 14 | 52.34 | 9 (–427, 424) | 6 (–275, 274) | 1274 (1268, 1280) | 1185 (1029, 1354) | 33 (31, 34) | 51 (26, 88) | 1208 (957, 1497) | 1252 (977, 1569) | 67 (64, 70) | 79 (47, 122) | 2600 (2388, 2821) | 2632 (2282, 3009) |
| 15 | 53.39 | 15 (–426, 433) | 10 (–275, 280) | 1365 (1358, 1372) | 1271 (1104, 1452) | 33 (31, 34) | 51 (26, 88) | 1207 (957, 1494) | 1251 (978, 1567) | 67 (64, 70) | 79 (47, 123) | 2600 (2390, 2819) | 2632 (2281, 3009) |
| 16 | 54.32 | 22 (–420, 447) | 14 (–271, 289) | 1456 (1449, 1463) | 1355 (1178, 1548) | 33 (31, 34) | 51 (26, 88) | 1208 (956, 1494) | 1252 (975, 1568) | 67 (64, 70) | 79 (47, 123) | 2600 (2391, 2820) | 2631 (2282, 3007) |
| 17 | 55.14 | 27 (–421, 456) | 18 (–272, 294) | 1548 (1540, 1555) | 1441 (1253, 1643) | 33 (31, 34) | 51 (26, 88) | 1208 (956, 1495) | 1252 (976, 1568) | 67 (64, 70) | 79 (47, 122) | 2601 (2390, 2822) | 2632 (2281, 3011) |
| 18 | 55.81 | 33 (–423, 465) | 21 (–273, 300) | 1639 (1631, 1647) | 1527 (1328, 1740) | 33 (31, 34) | 51 (26, 87) | 1207 (957, 1494) | 1252 (976, 1569) | 67 (64, 70) | 79 (47, 123) | 2600 (2388, 2819) | 2632 (2282, 3008) |
| 19 | 56.84 | 38 (–420, 479) | 24 (–271, 309) | 1731 (1722, 1739) | 1613 (1404, 1837) | 33 (31, 34) | 51 (26, 88) | 1208 (956, 1495) | 1252 (976, 1568) | 67 (64, 70) | 79 (47, 122) | 2600 (2389, 2820) | 2632 (2280, 3010) |
| 20 | 57.08 | 45 (–418, 487) | 29 (–269, 314) | 1822 (1813, 1831) | 1698 (1479, 1934) | 33 (31, 34) | 51 (26, 88) | 1208 (956, 1495) | 1251 (976, 1568) | 67 (64, 70) | 79 (47, 122) | 2601 (2391, 2820) | 2632 (2282, 3008) |
| 21 | 58.32 | 50 (–420, 499) | 32 (–271, 322) | 1914 (1904, 1923) | 1784 (1557, 2031) | 33 (31, 34) | 51 (26, 87) | 1208 (957, 1495) | 1252 (976, 1568) | 67 (64, 70) | 79 (47, 123) | 2601 (2389, 2823) | 2633 (2280, 3011) |
| 22 | 58.97 | 56 (–419, 510) | 36 (–270, 329) | 2005 (1995, 2014) | 1870 (1632, 2126) | 33 (31, 34) | 51 (26, 88) | 1208 (956, 1495) | 1252 (976, 1568) | 67 (64, 70) | 79 (47, 123) | 2600 (2389, 2820) | 2632 (2281, 3009) |
| 23 | 59.75 | 60 (–419, 518) | 39 (–270, 334) | 2097 (2087, 2106) | 1956 (1709, 2222) | 33 (31, 34) | 51 (26, 88) | 1208 (957, 1495) | 1252 (977, 1569) | 67 (64, 70) | 79 (47, 123) | 2600 (2390, 2821) | 2632 (2281, 3007) |
| 24 | 60.04 | 65 (–419, 531) | 42 (–270, 342) | 2188 (2178, 2199) | 2043 (1786, 2318) | 33 (31, 34) | 51 (26, 88) | 1208 (956, 1494) | 1252 (976, 1568) | 67 (64, 70) | 79 (47, 123) | 2600 (2389, 2819) | 2632 (2279, 3008) |
| 25 | 60.85 | 70 (–423, 542) | 45 (–273, 350) | 2280 (2269, 2291) | 2129 (1863, 2413) | 33 (31, 34) | 51 (26, 87) | 1207 (957, 1493) | 1252 (977, 1567) | 67 (64, 70) | 79 (47, 123) | 2601 (2392, 2820) | 2634 (2281, 3010) |
The intervals are 5th and 95th percentiles of the respective distribution. All estimates accounted for competing risk for non-CVD mortality. The expected events of the harm outcomes are expected to be the same across the CVD risk spectrum. The marginal variation across the CVD risk spectrum is due to statistical uncertainty and competing risk for non-CVD death.
CVD, cardiovascular disease.
Table 3.
Probability of net benefit and expected benefit and harm outcomes in 10 years per 10,000 men aged 80–84 years.
| 10-y CVD risk (%) | Probability of net benefit (%) | Net prevented moderate MI | Benefit-harm index | CVD |
Myopathy |
Diabetes type 2 |
Renal impairment |
Cancer |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No statin | Statin | No statin | Statin | No statin | Statin | No statin | Statin | No statin | Statin | ||||
| 1 | 39.91 | –67 (–465, 314) | –43 (–300, 203) | 84 (83, 85) | 78 (67, 90) | 30 (29, 32) | 48 (24, 81) | 932 (731, 1163) | 967 (746, 1220) | 62 (59, 65) | 73 (43, 113) | 2637 (2472, 2810) | 2669 (2339, 3017) |
| 2 | 41.25 | –61 (–460, 321) | –39 (–297, 207) | 168 (167, 169) | 156 (134, 179) | 30 (29, 32) | 47 (24, 81) | 932 (731, 1164) | 967 (746, 1222) | 62 (59, 65) | 73 (43, 113) | 2638 (2472, 2809) | 2669 (2340, 3018) |
| 3 | 42.42 | –53 (–457, 328) | –34 (–295, 212) | 252 (250, 254) | 234 (201, 269) | 30 (29, 32) | 48 (24, 81) | 932 (732, 1164) | 967 (746, 1222) | 62 (59, 65) | 73 (43, 114) | 2637 (2471, 2809) | 2668 (2340, 3018) |
| 4 | 43.12 | –49 (–453, 335) | –31 (–292, 216) | 336 (334, 339) | 312 (269, 359) | 30 (29, 32) | 47 (24, 81) | 932 (731, 1163) | 967 (747, 1222) | 62 (59, 65) | 73 (43, 113) | 2638 (2471, 2808) | 2669 (2342, 3018) |
| 5 | 44.33 | –43 (–446, 340) | –28 (–288, 220) | 420 (417, 424) | 390 (336, 449) | 30 (29, 32) | 47 (24, 81) | 932 (732, 1163) | 967 (747, 1219) | 62 (59, 65) | 73 (43, 113) | 2637 (2471, 2808) | 2669 (2342, 3018) |
| 6 | 45.24 | –36 (–442, 350) | –23 (–285, 226) | 505 (501, 508) | 468 (404, 539) | 30 (29, 32) | 47 (24, 81) | 931 (732, 1161) | 966 (747, 1219) | 62 (59, 65) | 73 (44, 113) | 2637 (2471, 2811) | 2668 (2341, 3019) |
| 7 | 46.35 | –31 (–438, 357) | –20 (–283, 230) | 589 (584, 593) | 546 (471, 629) | 30 (29, 32) | 47 (24, 81) | 933 (732, 1164) | 967 (746, 1223) | 62 (59, 65) | 73 (43, 113) | 2637 (2471, 2809) | 2668 (2342, 3015) |
| 8 | 47.28 | –25 (–435, 364) | –16 (–280, 234) | 673 (668, 678) | 625 (539, 718) | 30 (29, 32) | 47 (24, 81) | 933 (732, 1165) | 968 (747, 1223) | 62 (59, 65) | 73 (43, 113) | 2638 (2470, 2809) | 2670 (2341, 3018) |
| 9 | 48.28 | –18 (–431, 374) | –12 (–278, 241) | 758 (752, 763) | 703 (608, 807) | 30 (29, 32) | 47 (24, 81) | 933 (730, 1165) | 967 (746, 1222) | 62 (59, 65) | 73 (43, 113) | 2637 (2472, 2809) | 2668 (2340, 3017) |
| 10 | 49.18 | –12 (–429, 384) | –8 (–277, 248) | 842 (836, 848) | 782 (676, 898) | 30 (29, 32) | 47 (24, 81) | 932 (731, 1163) | 966 (746, 1221) | 62 (59, 65) | 73 (43, 113) | 2637 (2471, 2808) | 2668 (2339, 3017) |
| 11 | 50.17 | –7 (–424, 392) | –4 (–273, 253) | 927 (920, 933) | 861 (744, 986) | 30 (29, 32) | 48 (24, 81) | 933 (732, 1163) | 968 (748, 1222) | 62 (59, 65) | 73 (43, 113) | 2637 (2471, 2808) | 2668 (2344, 3015) |
| 12 | 50.88 | –3 (–424, 396) | –2 (–274, 255) | 1011 (1004, 1019) | 940 (814, 1077) | 30 (29, 32) | 48 (24, 81) | 933 (732, 1163) | 967 (748, 1221) | 62 (59, 65) | 73 (43, 114) | 2638 (2472, 2809) | 2670 (2341, 3019) |
| 13 | 52.01 | 3 (–421, 408) | 2 (–272, 263) | 1096 (1088, 1104) | 1019 (883, 1166) | 30 (29, 32) | 47 (24, 81) | 933 (731, 1164) | 967 (747, 1221) | 62 (59, 65) | 73 (43, 113) | 2637 (2471, 2809) | 2669 (2342, 3016) |
| 14 | 52.84 | 10 (–419, 417) | 6 (–270, 269) | 1181 (1172, 1189) | 1098 (952, 1255) | 30 (29, 32) | 48 (24, 81) | 933 (731, 1163) | 967 (747, 1221) | 62 (59, 65) | 73 (44, 114) | 2638 (2471, 2809) | 2669 (2343, 3019) |
| 15 | 53.66 | 16 (–416, 429) | 10 (–269, 277) | 1265 (1256, 1275) | 1177 (1022, 1345) | 30 (29, 32) | 48 (24, 81) | 932 (731, 1163) | 967 (747, 1220) | 62 (59, 65) | 73 (43, 113) | 2637 (2471, 2809) | 2668 (2341, 3018) |
| 16 | 54.14 | 20 (–416, 438) | 13 (–268, 282) | 1350 (1340, 1360) | 1257 (1091, 1435) | 30 (29, 32) | 48 (24, 81) | 933 (732, 1164) | 968 (747, 1222) | 62 (59, 65) | 73 (43, 114) | 2637 (2471, 2810) | 2669 (2341, 3018) |
| 17 | 54.88 | 25 (–416, 448) | 16 (–269, 289) | 1435 (1424, 1446) | 1336 (1161, 1524) | 30 (29, 32) | 47 (24, 81) | 932 (732, 1163) | 967 (748, 1220) | 62 (59, 65) | 73 (43, 113) | 2637 (2471, 2808) | 2669 (2339, 3021) |
| 18 | 55.86 | 31 (–412, 456) | 20 (–266, 294) | 1520 (1509, 1531) | 1415 (1231, 1615) | 30 (29, 32) | 47 (24, 81) | 932 (732, 1163) | 967 (747, 1219) | 62 (59, 65) | 73 (43, 113) | 2637 (2470, 2808) | 2669 (2342, 3018) |
| 19 | 56.57 | 36 (–415, 470) | 23 (–268, 303) | 1605 (1593, 1617) | 1495 (1301, 1705) | 30 (29, 32) | 48 (24, 81) | 933 (731, 1165) | 967 (747, 1223) | 62 (59, 65) | 73 (44, 113) | 2638 (2472, 2810) | 2670 (2340, 3018) |
| 20 | 57.09 | 41 (–413, 476) | 26 (–267, 307) | 1690 (1678, 1702) | 1576 (1373, 1794) | 30 (29, 32) | 47 (24, 81) | 933 (732, 1164) | 968 (748, 1221) | 62 (59, 65) | 73 (43, 113) | 2637 (2470, 2809) | 2669 (2341, 3018) |
| 21 | 57.53 | 47 (–412, 484) | 30 (–266, 312) | 1775 (1762, 1788) | 1655 (1444, 1883) | 30 (29, 32) | 47 (24, 81) | 933 (731, 1165) | 968 (748, 1223) | 62 (59, 65) | 73 (43, 113) | 2637 (2471, 2809) | 2669 (2342, 3015) |
| 22 | 58.67 | 52 (–409, 496) | 34 (–264, 320) | 1861 (1847, 1874) | 1736 (1514, 1975) | 30 (29, 32) | 48 (24, 81) | 932 (730, 1164) | 967 (746, 1220) | 62 (59, 65) | 73 (43, 114) | 2638 (2471, 2809) | 2668 (2340, 3018) |
| 23 | 59.04 | 55 (–412, 504) | 36 (–266, 325) | 1946 (1932, 1960) | 1816 (1586, 2064) | 30 (29, 32) | 48 (24, 81) | 932 (731, 1162) | 967 (747, 1220) | 62 (59, 65) | 73 (43, 113) | 2637 (2471, 2810) | 2670 (2342, 3021) |
| 24 | 59.64 | 60 (–411, 515) | 40 (–265, 332) | 2031 (2016, 2046) | 1896 (1656, 2151) | 30 (29, 32) | 48 (24, 81) | 932 (731, 1163) | 967 (748, 1223) | 62 (59, 65) | 73 (43, 114) | 2637 (2470, 2808) | 2669 (2341, 3018) |
| 25 | 60.41 | 68 (–406, 527) | 44 (–262, 340) | 2117 (2101, 2132) | 1976 (1727, 2243) | 30 (29, 32) | 48 (24, 81) | 933 (733, 1162) | 968 (749, 1223) | 62 (59, 65) | 73 (43, 113) | 2638 (2472, 2810) | 2669 (2343, 3018) |
The intervals are 5th and 95th percentiles of the respective distribution. All estimates accounted for competing risk for non-CVD mortality. The expected events of the harm outcomes are expected to be the same across the CVD risk spectrum. The marginal variation across the CVD risk spectrum is due to statistical uncertainty and competing risk for non-CVD death.
CVD, cardiovascular disease.
Table 4.
Probability of net benefit and expected benefit and harm outcomes in 10 years per 10,000 women aged 75–79 years.
| 10-y CVD risk (%) | Probability of net benefit (%) | Net prevented moderate MI | Benefit-harm index | CVD |
Myopathy |
Diabetes type 2 |
Renal impairment |
Cancer |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No statin | Statin | No statin | Statin | No statin | Statin | No statin | Statin | No statin | Statin | ||||
| 1 | 39.42 | –60 (–397, 253) | –39 (–256, 163) | 92 (92, 92) | 85 (73, 98) | 29 (27, 32) | 46 (24, 79) | 1146 (917, 1407) | 1188 (936, 1479) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1721 (1462, 2000) |
| 2 | 40.91 | –54 (–391, 262) | –35 (–252, 169) | 184 (183, 184) | 170 (146, 196) | 29 (27, 32) | 46 (24, 79) | 1146 (916, 1407) | 1188 (935, 1477) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1721 (1464, 2000) |
| 3 | 41.91 | –47 (–388, 267) | –30 (–250, 172) | 276 (275, 276) | 255 (220, 294) | 29 (27, 32) | 46 (24, 79) | 1146 (917, 1406) | 1188 (936, 1476) | 55 (52, 58) | 65 (38, 101) | 1696 (1578, 1820) | 1721 (1465, 2001) |
| 4 | 43.3 | –42 (–384, 276) | –27 (–248, 178) | 367 (366, 369) | 341 (294, 392) | 29 (27, 32) | 46 (24, 79) | 1146 (916, 1407) | 1188 (934, 1478) | 55 (52, 58) | 65 (39, 101) | 1697 (1578, 1820) | 1721 (1464, 2003) |
| 5 | 44.46 | –34 (–374, 284) | –22 (–241, 183) | 459 (458, 461) | 426 (367, 490) | 29 (27, 32) | 46 (24, 79) | 1146 (918, 1405) | 1188 (936, 1477) | 55 (52, 58) | 65 (38, 101) | 1696 (1578, 1820) | 1720 (1465, 2000) |
| 6 | 45.89 | –29 (–374, 295) | –19 (–241, 190) | 551 (549, 553) | 511 (441, 588) | 29 (27, 32) | 46 (24, 79) | 1146 (916, 1408) | 1188 (934, 1477) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1722 (1466, 2002) |
| 7 | 47.22 | –22 (–369, 304) | –14 (–238, 196) | 643 (641, 645) | 597 (515, 686) | 29 (27, 32) | 46 (24, 79) | 1146 (917, 1408) | 1189 (935, 1479) | 55 (52, 58) | 65 (38, 101) | 1697 (1579, 1820) | 1721 (1463, 2001) |
| 8 | 48.4 | –16 (–367, 315) | –10 (–237, 203) | 735 (733, 738) | 682 (590, 784) | 29 (27, 32) | 46 (24, 79) | 1147 (918, 1408) | 1189 (937, 1478) | 55 (52, 58) | 65 (39, 101) | 1697 (1577, 1821) | 1722 (1465, 2001) |
| 9 | 49.32 | –8 (–364, 321) | –5 (–235, 207) | 827 (825, 830) | 768 (665, 881) | 29 (27, 32) | 46 (24, 79) | 1146 (916, 1405) | 1188 (936, 1478) | 55 (52, 58) | 65 (39, 101) | 1697 (1577, 1820) | 1721 (1463, 2001) |
| 10 | 50.5 | –5 (–363, 332) | –3 (–234, 214) | 919 (916, 922) | 855 (739, 979) | 29 (27, 32) | 46 (24, 79) | 1146 (916, 1405) | 1188 (935, 1477) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1821) | 1722 (1465, 2001) |
| 11 | 51.67 | 5 (–355, 344) | 3 (–229, 222) | 1012 (1008, 1015) | 940 (814, 1078) | 29 (27, 32) | 46 (24, 79) | 1146 (917, 1407) | 1188 (934, 1479) | 55 (52, 58) | 65 (39, 100) | 1697 (1579, 1820) | 1720 (1463, 1999) |
| 12 | 52.75 | 9 (–357, 353) | 6 (–230, 228) | 1104 (1100, 1107) | 1025 (889, 1174) | 29 (27, 32) | 46 (24, 79) | 1145 (915, 1405) | 1187 (934, 1476) | 55 (52, 58) | 65 (38, 101) | 1696 (1577, 1820) | 1721 (1465, 2000) |
| 13 | 53.54 | 16 (–353, 366) | 10 (–228, 236) | 1196 (1192, 1200) | 1112 (964, 1272) | 29 (27, 32) | 46 (24, 79) | 1147 (917, 1408) | 1189 (937, 1477) | 55 (52, 58) | 65 (38, 100) | 1697 (1578, 1820) | 1721 (1464, 2001) |
| 14 | 54.73 | 22 (–355, 377) | 14 (–229, 243) | 1288 (1284, 1292) | 1198 (1040, 1369) | 29 (27, 32) | 46 (24, 79) | 1147 (917, 1405) | 1188 (936, 1475) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1821) | 1721 (1465, 2002) |
| 15 | 55.51 | 28 (–353, 388) | 18 (–228, 250) | 1380 (1376, 1385) | 1284 (1115, 1467) | 29 (27, 32) | 46 (24, 79) | 1146 (917, 1406) | 1188 (936, 1476) | 55 (52, 58) | 65 (38, 101) | 1696 (1578, 1820) | 1721 (1465, 1999) |
| 16 | 56.67 | 34 (–352, 398) | 22 (–227, 257) | 1473 (1468, 1477) | 1371 (1192, 1565) | 29 (27, 32) | 46 (24, 79) | 1146 (916, 1405) | 1188 (935, 1476) | 55 (52, 58) | 65 (38, 100) | 1697 (1579, 1820) | 1721 (1464, 2002) |
| 17 | 57.45 | 39 (–355, 411) | 25 (–229, 265) | 1565 (1560, 1570) | 1457 (1267, 1664) | 29 (27, 32) | 46 (24, 79) | 1147 (917, 1406) | 1189 (936, 1478) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1722 (1465, 2003) |
| 18 | 58.54 | 47 (–350, 422) | 30 (–226, 272) | 1657 (1652, 1662) | 1543 (1344, 1759) | 29 (27, 32) | 46 (24, 79) | 1146 (916, 1407) | 1188 (934, 1477) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1721 (1464, 2000) |
| 19 | 58.68 | 51 (–352, 433) | 33 (–227, 279) | 1750 (1744, 1755) | 1631 (1420, 1856) | 29 (27, 32) | 46 (24, 79) | 1146 (916, 1406) | 1188 (935, 1477) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1720 (1465, 2000) |
| 20 | 59.66 | 56 (–352, 445) | 36 (–227, 287) | 1842 (1836, 1848) | 1717 (1496, 1954) | 29 (27, 32) | 46 (24, 79) | 1147 (916, 1408) | 1189 (936, 1480) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1722 (1465, 2000) |
| 21 | 60.34 | 62 (–352, 456) | 40 (–227, 294) | 1934 (1928, 1940) | 1804 (1573, 2052) | 29 (27, 32) | 46 (24, 79) | 1147 (918, 1406) | 1189 (937, 1478) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1721 (1464, 2001) |
| 22 | 61.2 | 68 (–357, 468) | 44 (–230, 302) | 2027 (2020, 2033) | 1891 (1651, 2150) | 29 (27, 32) | 46 (24, 79) | 1146 (917, 1406) | 1188 (936, 1476) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1721 (1465, 2001) |
| 23 | 61.74 | 74 (–353, 479) | 48 (–228, 309) | 2119 (2113, 2126) | 1978 (1729, 2247) | 29 (27, 32) | 46 (24, 79) | 1146 (916, 1404) | 1188 (935, 1476) | 55 (52, 58) | 65 (39, 101) | 1697 (1578, 1820) | 1721 (1464, 2000) |
| 24 | 62.36 | 78 (–353, 491) | 50 (–228, 317) | 2212 (2205, 2219) | 2066 (1806, 2342) | 29 (27, 32) | 46 (24, 79) | 1147 (918, 1407) | 1189 (935, 1479) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1722 (1466, 2001) |
| 25 | 63.02 | 85 (–355, 504) | 55 (–229, 325) | 2305 (2297, 2312) | 2152 (1883, 2441) | 29 (27, 32) | 46 (24, 79) | 1145 (916, 1405) | 1188 (935, 1476) | 55 (52, 58) | 65 (38, 101) | 1697 (1578, 1820) | 1720 (1463, 2002) |
The intervals are 5th and 95th percentiles of the respective distribution. All estimates accounted for competing risk for non-CVD mortality. The expected events of the harm outcomes are expected to be the same across the CVD risk spectrum. The marginal variation across the CVD risk spectrum is due to statistical uncertainty and competing risk for non-CVD death.
CVD, cardiovascular disease.
Table 5.
Probability of net benefit and expected benefit and harm outcomes in 10 years per 10,000 women aged 80–84 years.
| 10-y CVD risk (%) | Probability of net benefit (%) | Net prevented moderate MI | Benefit-harm index | CVD |
Myopathy |
Diabetes type 2 |
Renal impairment |
Cancer |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No statin | Statin | No statin | Statin | No statin | Statin | No statin | Statin | No statin | Statin | ||||
| 1 | 40.9 | –57 (–436, 291) | –37 (–281, 188) | 90 (89, 90) | 83 (72, 96) | 29 (27, 31) | 45 (23, 77) | 938 (730, 1177) | 973 (747, 1237) | 54 (51, 57) | 63 (38, 98) | 1731 (1620, 1847) | 1756 (1477, 2061) |
| 2 | 41.87 | –53 (–431, 298) | –34 (–278, 192) | 180 (179, 181) | 167 (143, 192) | 29 (27, 31) | 45 (23, 77) | 939 (731, 1179) | 974 (747, 1238) | 54 (51, 57) | 64 (38, 99) | 1731 (1620, 1846) | 1758 (1479, 2064) |
| 3 | 42.85 | –47 (–426, 304) | –30 (–275, 196) | 270 (268, 271) | 250 (215, 288) | 29 (27, 31) | 45 (23, 77) | 939 (731, 1177) | 974 (747, 1236) | 54 (51, 57) | 64 (38, 98) | 1731 (1621, 1847) | 1758 (1480, 2063) |
| 4 | 43.96 | –39 (–422, 313) | –25 (–272, 202) | 360 (358, 362) | 334 (287, 384) | 29 (27, 31) | 45 (23, 77) | 938 (730, 1176) | 973 (747, 1236) | 54 (51, 57) | 64 (38, 99) | 1731 (1620, 1848) | 1757 (1478, 2064) |
| 5 | 45.22 | –33 (–417, 319) | –21 (–269, 206) | 450 (447, 452) | 417 (360, 480) | 29 (27, 31) | 45 (23, 78) | 939 (731, 1177) | 974 (747, 1236) | 54 (51, 57) | 64 (38, 99) | 1731 (1620, 1847) | 1758 (1479, 2064) |
| 6 | 46.47 | –26 (–411, 330) | –17 (–265, 213) | 540 (537, 543) | 501 (432, 576) | 29 (27, 31) | 45 (23, 77) | 938 (730, 1177) | 973 (747, 1237) | 54 (51, 57) | 64 (38, 99) | 1731 (1620, 1847) | 1757 (1479, 2063) |
| 7 | 47.51 | –20 (–406, 336) | –13 (–262, 217) | 630 (626, 633) | 584 (504, 672) | 29 (27, 31) | 45 (23, 78) | 939 (734, 1178) | 974 (749, 1236) | 54 (51, 57) | 63 (38, 98) | 1732 (1621, 1848) | 1758 (1480, 2062) |
| 8 | 48.61 | –12 (–403, 349) | –8 (–260, 225) | 720 (716, 724) | 669 (578, 768) | 29 (27, 31) | 45 (23, 77) | 938 (732, 1176) | 973 (748, 1236) | 54 (51, 57) | 64 (38, 98) | 1731 (1620, 1847) | 1756 (1477, 2060) |
| 9 | 49.74 | –6 (–400, 357) | –4 (–258, 230) | 810 (806, 815) | 752 (650, 862) | 29 (27, 31) | 45 (23, 77) | 939 (731, 1176) | 974 (748, 1237) | 54 (51, 57) | 64 (38, 98) | 1731 (1620, 1846) | 1757 (1479, 2062) |
| 10 | 51.19 | 0 (–395, 367) | 0 (–255, 237) | 900 (896, 905) | 836 (723, 959) | 29 (27, 31) | 45 (23, 77) | 939 (731, 1178) | 974 (747, 1237) | 54 (51, 57) | 64 (38, 98) | 1731 (1620, 1847) | 1757 (1477, 2063) |
| 11 | 52.01 | 5 (–394, 377) | 3 (–254, 243) | 991 (985, 996) | 920 (797, 1055) | 29 (27, 31) | 45 (23, 77) | 938 (732, 1177) | 973 (747, 1235) | 54 (51, 57) | 64 (38, 98) | 1732 (1621, 1847) | 1757 (1480, 2062) |
| 12 | 53.08 | 9 (–394, 388) | 6 (–254, 250) | 1081 (1075, 1087) | 1004 (870, 1150) | 29 (27, 31) | 45 (23, 77) | 939 (732, 1177) | 974 (748, 1236) | 54 (51, 57) | 64 (37, 99) | 1731 (1620, 1846) | 1758 (1478, 2064) |
| 13 | 54.01 | 17 (–391, 398) | 11 (–252, 257) | 1171 (1165, 1177) | 1089 (944, 1247) | 29 (27, 31) | 45 (23, 77) | 939 (732, 1179) | 974 (747, 1238) | 54 (51, 57) | 64 (37, 99) | 1732 (1620, 1847) | 1757 (1480, 2063) |
| 14 | 54.58 | 23 (–389, 406) | 15 (–251, 262) | 1262 (1255, 1268) | 1173 (1019, 1341) | 29 (27, 31) | 45 (23, 78) | 938 (731, 1177) | 973 (747, 1235) | 54 (51, 57) | 64 (38, 99) | 1731 (1620, 1847) | 1757 (1477, 2062) |
| 15 | 55.69 | 29 (–388, 417) | 19 (–250, 269) | 1352 (1345, 1359) | 1258 (1091, 1436) | 29 (27, 31) | 45 (23, 77) | 939 (733, 1177) | 975 (749, 1235) | 54 (51, 57) | 63 (38, 99) | 1732 (1620, 1847) | 1757 (1480, 2062) |
| 16 | 56.40 | 36 (–381, 428) | 23 (–246, 276) | 1442 (1435, 1450) | 1343 (1165, 1534) | 29 (27, 31) | 45 (23, 77) | 939 (733, 1176) | 974 (749, 1235) | 54 (51, 57) | 64 (38, 98) | 1731 (1620, 1847) | 1757 (1479, 2061) |
| 17 | 57.44 | 40 (–386, 439) | 26 (–249, 283) | 1533 (1525, 1541) | 1427 (1240, 1628) | 29 (27, 31) | 45 (23, 77) | 938 (731, 1178) | 973 (747, 1235) | 54 (51, 57) | 64 (38, 99) | 1731 (1619, 1848) | 1758 (1479, 2063) |
| 18 | 58.03 | 47 (–383, 448) | 30 (–247, 289) | 1623 (1615, 1632) | 1512 (1316, 1722) | 29 (27, 31) | 45 (23, 77) | 939 (732, 1176) | 973 (747, 1235) | 54 (51, 57) | 64 (38, 98) | 1732 (1620, 1847) | 1758 (1478, 2065) |
| 19 | 58.63 | 50 (–388, 460) | 32 (–250, 297) | 1714 (1705, 1723) | 1598 (1391, 1820) | 29 (27, 31) | 45 (23, 77) | 939 (732, 1177) | 974 (749, 1236) | 54 (51, 57) | 64 (38, 98) | 1731 (1620, 1847) | 1758 (1478, 2065) |
| 20 | 59.6 | 57 (–384, 470) | 37 (–248, 303) | 1805 (1795, 1814) | 1682 (1465, 1915) | 29 (27, 31) | 45 (23, 77) | 938 (730, 1176) | 973 (746, 1235) | 54 (51, 57) | 64 (38, 98) | 1731 (1619, 1847) | 1757 (1480, 2062) |
| 21 | 60.19 | 64 (–383, 484) | 41 (–247, 312) | 1895 (1885, 1905) | 1767 (1541, 2010) | 29 (27, 31) | 45 (23, 77) | 938 (731, 1177) | 973 (747, 1235) | 54 (51, 57) | 64 (38, 98) | 1731 (1621, 1847) | 1757 (1479, 2062) |
| 22 | 60.82 | 68 (–388, 493) | 44 (–250, 318) | 1986 (1976, 1996) | 1853 (1618, 2107) | 29 (27, 31) | 45 (23, 77) | 939 (732, 1179) | 975 (748, 1238) | 54 (51, 57) | 64 (38, 98) | 1731 (1619, 1847) | 1757 (1477, 2063) |
| 23 | 61.40 | 71 (–386, 504) | 46 (–249, 325) | 2077 (2066, 2087) | 1938 (1693, 2202) | 29 (27, 31) | 45 (23, 77) | 938 (731, 1176) | 973 (747, 1235) | 54 (51, 57) | 64 (38, 98) | 1732 (1620, 1847) | 1758 (1480, 2064) |
| 24 | 61.99 | 79 (–384, 516) | 51 (–248, 333) | 2168 (2156, 2179) | 2023 (1768, 2301) | 29 (27, 31) | 45 (23, 77) | 939 (732, 1177) | 974 (748, 1236) | 54 (51, 57) | 64 (38, 99) | 1731 (1620, 1847) | 1757 (1478, 2063) |
| 25 | 62.60 | 84 (–383, 529) | 54 (–247, 341) | 2258 (2247, 2270) | 2109 (1846, 2392) | 29 (27, 31) | 45 (23, 77) | 939 (732, 1178) | 974 (748, 1235) | 54 (51, 57) | 64 (38, 98) | 1731 (1620, 1847) | 1757 (1478, 2061) |
The intervals are 5th and 95th percentiles of the respective distribution. All estimates accounted for competing risk for non-CVD mortality. The expected events of the harm outcomes are expected to be the same across the CVD risk spectrum. The marginal variation across the CVD risk spectrum is due to statistical uncertainty and competing risk for non-CVD death.
CVD, cardiovascular disease.
CVD risk thresholds and absolute net benefit events
Weighting the prevented CVD events against the harm outcomes yielded the benefit–harm index (Tables 2–5). Based on the average preference values, statins were more likely (with a probability of 60% or above) to provide a net benefit for older people at baseline 10-year CVD risk threshold of 24% and 25% in men aged 75–79 years and 80–84 years, respectively. The threshold for women was 21% for both age groups (Tables 2–5). In other words, older people with baseline CVD risk lower than those thresholds were not likely to obtain a net benefit from taking statins. The corresponding absolute net prevented events at the determined thresholds, expressed in terms of moderate MI events, were 65 (5th and 95th percentiles, –419 to 531) in 10,000 men aged 75–79 years and 68 (5th and 95th percentiles, –406 to 527) in men aged 80–84 years. These events were similar in women; that is, taking statins daily for 10 years would prevent 62 events equivalent to moderate MI (5thand 95the percentiles, –352 to 456) in 10,000 women aged 75–79 years and 64 (5th and 95th percentiles, –383 to 484) in 10,000 women aged 80–84 years with a baseline CVD risks of 21% (Tables 2–5).
Preference-sensitivity of thresholds
The thresholds varied by individual preferences regardless of whether we took estimates from trials only or combined effect from observational studies. For each set of preference values derived from the 120 BWS survey respondents, we repeated the entire analyses and, therefore, derived 120 estimates of the benefit–harm balance indices and risk thresholds for the net benefit for each subgroup. The thresholds ranged from 11% to 59% 10-year CVD risk in men and from 10% to 59% 10-year CVD risk in women (Figure 1). The interquartile ranges (IQRs) of the thresholds in men were between 21% and 33% for ages 75–79 years and between 23% and 36% for ages 80–84 years. The corresponding IQRs in women were between 20% and 32% for ages 75–79 years and between 21% and 32% for ages 80–84 years. A number of individual’s preference values resulted in even higher thresholds. For example, 10 out of 120 people in each of the two age groups had very low preference values for CVD but higher values for the harm outcomes resulting in higher-risk thresholds or no net benefit at all. In addition, the opposite was true with individuals giving increased weight to CVD than to harm outcomes, which resulted in very low-risk thresholds.
Figure 1.
The 10-year CVD risk threshold variation taking preferences of CVD and statin-related harm outcomes taken from individuals.
A small fixed noise was added to the threshold points in the figure for visibility. CVD, cardiovascular disease.
Sensitivity analyses
In the main analysis, the estimates for the risk of diabetes and cancer were consolidated from both trials and observational studies. Rejecting the treatment estimates for these two outcomes from observational studies, statins showed net benefit at 23% and 21% 10-year CVD risk thresholds for men aged 75–79 years and 80–84 years, respectively, and 21% and 19% 10-year CVD risk for women aged 75–79 years and 80–84 years, respectively. The thresholds were slightly lower than those in the main analysis. This can be explained because cancer incidence was dropped from this analysis as a harm outcome as there was no treatment effect in the included trial data. In addition, the risk decreases for diabetes with age in the general population, particularly over the age of 75 years, resulted in lower absolute excess risk and, therefore, affected the thresholds toward lower values in the older age group (80–84 years) than the younger age group (75–79 years), which was in contrast to the main analysis.
In addition, another sensitivity analysis in which we used combined effect estimates for CVD from trials and observational studies, instead of from trials only, revealed slightly higher thresholds than the main analysis with 27% and 28% 10-year CVD risk for men aged 75–79 years and 80–84 years, respectively, and 24% for both age groups in women. Risk thresholds remained preference-sensitive across all analyses.
Discussion
This study found that in a primary prevention population aged 75 years or older and with moderate baseline harm risks, statin use is more likely to provide a net benefit if the baseline CVD risk is at least 24% in men and 21% in women. However, when taking into account variation in preferences for benefit and harm outcomes between individuals, the thresholds for a net benefit may be significantly increased or decreased on an individual level. This indicates that the benefit–harm balance of statins is highly preference-sensitive and that the average risk thresholds derived in this study can only give a limited amount of guidance, and patient-centered decision-making needs to take individual preferences into account.
Guideline developers have understandably been hesitant to make recommendations on the prescription of statins as a primary preventive measure for people over the age of 75 years because of the limited number of randomized controlled trial data available for this age group. With the recent data from a meta-analysis of individual patient data from trials and two large observational studies, there is now an increased amount of evidence on the effects of statins on CVD in this population.5–7 The smaller observed treatment effect of statins on CVD in people over the age of 75 years of only 8% relative risk reduction, as compared with 24–26% in younger adults,7,13 is an important reason why the 10-year CVD risk thresholds for an overall beneficial effect is quite high and well above risk thresholds recommended by a number of guidelines.9,32,33
Despite the recently available evidence on the effect of statins on CVD in older people,7 it is probable that additional evidence will change the current estimates of the benefit–harm balance (e.g., the ongoing STAREE trial in the elderly may provide further evidence).34 It is likely that the thresholds could be even higher because we did not include some of the harm outcomes in our analysis owing to a lack of evidence (i.e., hepatic dysfunction, cataracts, cognitive loss, and gastrointestinal problems).7,13 To overcome the limited amount of data, we combined evidence from observational studies with the trial data on diabetes and cancer.23 If only the trial data are relied on and the observational data are excluded, the thresholds showed slightly lower risk thresholds because no effect of statins on cancer was observed in the included trials. In addition, because the absolute treatment effects as well as the benefit–harm balance are highly dependent on the baseline risks, using more valid and precise baseline risks in the model could change the benefit–harm balance estimates.11 Finally, it is also possible that additional preference-elicitation surveys could obtain different average weightings for older people for the outcomes depending how the decisional context is framed and depending on the methods used to determine preferences and the age of the population studied.
Our work demonstrates that individual preferences have a substantially greater effect on the benefit–harm balance than specific additional pieces of evidence. This has important implications for guideline developers. Despite the official endorsement for considering patient preferences, guidelines commonly issue only a single or few recommendations that are independent of patient preferences, values, and context.35 However, even the most valid and largest trials or observational studies will not be conclusive as to whether the intervention will be worthwhile for an individual patient unless the perspectives of patients are considered, including their preferences. We had the opportunity to consider combinations of preferences from 120 people and estimate the benefit–harm balance for each combination. As can be expected, the benefit–harm balance of statins for primary prevention in older people varied dramatically across the combinations of preferences. As a consequence, a one-size-fits-all recommendation is not appropriate for such a preference-sensitive decision, and according to the guidance of the GRADE Working Group, strong recommendations should not be issued either for or against statins in such a situation.36 Depending on the context in which the recommendations are developed (i.e., considering specific population baseline risks or other factors), weak recommendations for statins could be issued for older people at 10-year CVD above 21% or 24%. These recommendations should acknowledge that depending on the individual’s preferences, this threshold could be significantly lower or higher. Tailoring recommendations to individual patients could be supported by using decision aids that consider individual patient baseline risks and preferences.
Prescribing statins to older people needs further careful handling because simply focusing on the total absolute risk could lead to overtreatment. Older people could easily meet the risk thresholds just because of their age, which is a strong independent, but nonmodifiable risk factor.37 Instead, it is important to assess the modifiability of the underlying risk factors, including cholesterol levels, diabetes, hypertension, smoking, and vascular inflammation because statins do not have any benefit otherwise.6 Nevertheless, how diabetes predicts CVD in people taking statins is not clear from the current literature; that is, studies show that statin therapy reduces the risk for CVD but it could increase blood sugar as an adverse effect and, therefore, increase the risk for CVD where the effects may cancel each other out.5,6,15 We did not determine a risk threshold specifically for diabetes patients because considering such heterogeneous evidence in the analysis could be misleading. Our findings could apply to all people regardless of whether they have diabetes. However, it should be noted that patients with diabetes would still have an increased chance of being recommended for statins because diabetes strongly increases the baseline CVD risk score.
An important limitation of this study was that we could not consider all prespecified harm outcomes, as noted previously. In addition, obtaining valid, applicable, and precise effect estimates of the harm outcomes that were included was a challenge. Some of the estimates that were extrapolated from trials could have included people younger than 75 years. However, the extrapolation was more likely to overestimate the net benefit in older people because it is expected that the harm outcomes are generally increased in older people because of frailty, comorbidities, and polypharmacy and drug–drug interactions. In addition, the generalizability of the thresholds to other countries should be further investigated taking into consideration country-specific outcome risks. An additional limitation is that we took the preferences from empirical research that included people mostly younger than 75 years.12 We can only speculate what the results in this older age group would be but it is possible that, as older people might not live long enough to receive long-term benefits, they would worry more about harm outcomes than younger people since the harm outcomes could affect their quality of life in the short term. This might have overestimated the net benefit. However, in the BWS survey there was no association between age and preferences. A strength of the survey is that preferences were elicited using lay descriptions that were constructed based on the clinical features, treatment options, and prognosis of the outcomes. As a result, the preferences were similar across the socioeconomically disparate environments of Switzerland and Ethiopia.12 In addition, the GBD study also found similar preferences across several, quite different countries.38 However, treatment preferences might vary depending on other factors that were not captured in the lay descriptions of our preference-eliciting survey, such as costs or access to care. Therefore, country-specific preference values may be required if consideration of such factors is warranted. However, it is probable that preferences vary between individuals in different countries and, most importantly, this study revealed that individual treatment thresholds are preference-sensitive and, thus, might differ notably from average population-level preferences
In conclusion, this study has demonstrated that the benefits of statins would be more likely to outweigh their harm in primary CVD prevention if the 10-year risk of people over the age of 75 years is higher than 20%. However, these thresholds assume average preferences in a population. This study further demonstrated that the benefit–harm balance is highly dependent on individual preferences for benefit and harm outcomes. As a consequence, guidelines should continue to be cautious when making population-level recommendations and should support individual decision-making taking into account individual modifiable risks and, probably most importantly, individual preferences.
Supplemental Material
Supplemental material, Supplementary_material for Net benefit of statins for primary prevention of cardiovascular disease in people 75 years or older: a benefit–harm balance modeling study by Henock G. Yebyo, Hélène E. Aschmann, Dominik Menges, Cynthia M. Boyd and Milo A. Puhan in Therapeutic Advances in Chronic Disease
Footnotes
Author contribution: HGY and MAP conceptualized the study. HGY performed the statistical analysis and wrote the original draft. All authors interpreted critically revised manuscript and approved the final version.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Henock G. Yebyo  https://orcid.org/0000-0001-5400-2448
https://orcid.org/0000-0001-5400-2448
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Henock G. Yebyo, Epidemiology, Biostatistics & Prevention Institute, University of Zurich, Hirschengraben 84, Zurich, CH-8001, Switzerland.
Hélène E. Aschmann, Department of Epidemiology; Epidemiology, Biostatistics and Prevention Institute, University of Zurich, Zurich, Switzerland
Dominik Menges, Department of Epidemiology; Epidemiology, Biostatistics and Prevention Institute, University of Zurich, Zurich, Switzerland.
Cynthia M. Boyd, The Johns Hopkins University, School of Medicine, Baltimore, MD, USA
Milo A. Puhan, Department of Epidemiology; Epidemiology, Biostatistics and Prevention Institute, University of Zurich, Zurich, Switzerland
References
- 1. United Nations. World aging population 2017. New York: United Nations, 2017. DOI: 10.1049/el:20000788. [DOI] [Google Scholar]
- 2. Marrugat J, Sala J, Manresa JM, et al. Acute myocardial infarction population incidence and in-hospital management factors associated to 28-day case-fatality in the 65 year and older. Eur J Epidemiol 2004; 19: 231–237. [DOI] [PubMed] [Google Scholar]
- 3. Konrat C, Boutron I, Trinquart L, et al. Underrepresentation of elderly people in randomised controlled trials. The example of trials of 4 widely prescribed drugs. PLoS One 2012; 7: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Statin use for the primary prevention of cardiovascular disease in adults. JAMA 2016; 316: 1997. [DOI] [PubMed] [Google Scholar]
- 5. Ramos R, Comas-Cufí M, Martí-Lluch R, et al. Statins for primary prevention of cardiovascular events and mortality in old and very old adults with and without type 2 diabetes: Retrospective cohort study. BMJ 2018; 362: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bezin J, Moore N, Mansiaux Y, et al. Real-life benefits of statins for cardiovascular prevention in elderly subjects: a population-based cohort study. Am J Med 2019; 132: 740–748. [DOI] [PubMed] [Google Scholar]
- 7. Armitage J, Baigent C, Barnes E, et al. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet 2019; 393: 407–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yebyo HG, Aschmann HE, Puhan MA. Finding the balance between benefits and harms when using statins for primary prevention of cardiovascular disease: a modeling study. Ann Intern Med 2019; 170: 1–10. [DOI] [PubMed] [Google Scholar]
- 9. National Institute for Health and Care Excellence. Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease, http://www.nice.org.uk/guidance/cg181/documents/lipid-modification-update-draft-full-guideline2 (2014, accessed 1 June 2019). [PubMed]
- 10. Ludt S, Angelow A, Baum E, et al. DEGAM Leitlinie S3: Hausärztliche Risikoberatung zur kardiovaskulären Prävention. Berlin, https://www.awmf.org/uploads/tx_szleitlinien/053-024l_S3_Hausaerztliche_Risikoberat_kardiovask_Praevention_2018-09.pdf (2017, accessed May 24, 2019). [Google Scholar]
- 11. Fain KM, Yu T, Li T, et al. Evidence selection for a prescription drug’s benefit-harm assessment: challenges and recommendations. J Clin Epidemiol 2016; 74: 151–157. [DOI] [PubMed] [Google Scholar]
- 12. Yebyo HG, Aschmann HE, Yu T, et al. Should statin guidelines consider patient preferences? Eliciting preferences of benefit and harm outcomes of statins for primary prevention of cardiovascular disease in the sub-Saharan African and European contexts. BMC Cardiovasc Disord 2018; 18: 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yebyo HG, Aschmann HE, Kaufmann M, et al. Comparative effectiveness and safety of statins as a class and of specific statins for primary prevention of cardiovascular disease: a systematic review, meta-analysis, and network meta-analysis of randomized trials with 94,283 participants. Am Heart J 2019; 210: 18–28. [DOI] [PubMed] [Google Scholar]
- 14. Gail MH, Costantino JP, Bryant J, et al. Weighing the risks and benefits of tamoxifen treatment for preventing breast cancer. J Natl Cancer Inst 2004; 11: 53–56. [DOI] [PubMed] [Google Scholar]
- 15. Ford I, Twomey C, Jukema JW, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet 2002; 360: 1623–1630. [DOI] [PubMed] [Google Scholar]
- 16. Deedwania P, Stone PH, Bairey Merz CN, et al. Effects of intensive versus moderate lipid-lowering therapy on myocardial ischemia in older patients with coronary heart disease. Circulation 2007; 115: 700–707. [DOI] [PubMed] [Google Scholar]
- 17. Armitage J, Baigent C, Barnes E, et al. Supplementary appendix. Lancet 2019; 393(Suppl.): s1–S11. [Google Scholar]
- 18. ALLHAT. Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care. JAMA 2002; 288. [DOI] [PubMed] [Google Scholar]
- 19. Sever PS, Dahlöf B, Poulter NR, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet 2017; 361: 1149–1158. [DOI] [PubMed] [Google Scholar]
- 20. Suwijn SR, Boel JA, Post B, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein Paul. N Engl J Med 2008; 359: 315–324. [DOI] [PubMed] [Google Scholar]
- 21. Yusuf S, Bosch J, Dagenais G, et al. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med 2016; 374: 2021–2031. [DOI] [PubMed] [Google Scholar]
- 22. Glynn RJ, Koenig W, Nordestgaard BG, et al. Rosuvastatin for primary prevention in older persons with elevated C-reactive protein and low to average low-density lipoprotein cholesterol levels: Exploratory analysis of a randomized trial. Ann Intern Med 2010; 152: 488–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Seruga B, Templeton AJ, Emilio F, et al. Under-reporting of harm in clinical trials. Lancet Oncol 2016; 17: e209–e219. [DOI] [PubMed] [Google Scholar]
- 24. Vandenbroucke JP. What is the best evidence for determining harms of medical treatment? CMAJ 2006; 174: 645–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Global Burden of Disease. GBD health data exchange, http://ghdx.healthdata.org/gbd-results-tool (2017, accessed 14 February 2019).
- 26. Hippisley-Cox J, Coupland C. Unintended effects of statins in men and women in England and Wales: Population based cohort study using the QResearch database. BMJ 2010; 340: 1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Han BH, Sutin D, Williamson JD, et al. Effect of statin treatment vs usual care on primary cardiovascular prevention among older adults: the ALLHAT-LLT randomized clinical trial. JAMA Intern Med 2017; 177: 955–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bennett WL, Aschmann HE, Puhan MA, et al. A benefit–harm analysis of adding basal insulin vs. sulfonylurea to metformin to manage type II diabetes mellitus in people with multiple chronic conditions. J Clin Epidemiol 2019; 113: 92–100. [DOI] [PubMed] [Google Scholar]
- 29. Salanti G, Ades AE, Ioannidis JPA. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 2011; 64: 163–171. [DOI] [PubMed] [Google Scholar]
- 30. R Core Team. R: a language and environment for statistical computing, https://www.r-project.org/ (2016, accessed 1 June 2019).
- 31. Shor E, Roelfs D, Vang ZM. The ‘Hispanic mortality paradox’ revisited: Meta-analysis and meta-regression of life-course differentials in Latin American and Caribbean immigrants’ mortality. Soc Sci Med 2017; 186: 20–33. [DOI] [PubMed] [Google Scholar]
- 32. Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Statin Use for the primary prevention of cardiovascular disease in adults. JAMA 2016; 316: 1997–2007. [DOI] [PubMed] [Google Scholar]
- 33. Robinson JG. Overview of the 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. Future Cardiol 2014; 10: 149–152. [DOI] [PubMed] [Google Scholar]
- 34. ClinicalTrials.gov. A clinical trial of Statin therapy for reducing events in the elderly (STAREE), https://clinicaltrials.gov/ct2/show/NCT02099123 (accessed 8 August 2019).
- 35. Barrett B, Ricco J, Wallace M, et al. Communicating statin evidence to support shared decision-making. BMC Fam Pract 2016; 17: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hultcrantz M, Rind D, Akl EA, et al. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol 2017; 87: 4–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mortensen MB, Nordestgaard BG. Comparison of five major guidelines for statin use in primary prevention in a contemporary general population. Ann Intern Med 2018; 168: 85. [DOI] [PubMed] [Google Scholar]
- 38. Salomon JA, Vos T, Hogan DR, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2129–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_material for Net benefit of statins for primary prevention of cardiovascular disease in people 75 years or older: a benefit–harm balance modeling study by Henock G. Yebyo, Hélène E. Aschmann, Dominik Menges, Cynthia M. Boyd and Milo A. Puhan in Therapeutic Advances in Chronic Disease