Abstract
Background:
Excessive prescription of opioids has become a national problem. Providers must attempt to decrease the amount of opioids prescribed while still providing patients with adequate pain relief after surgery.
Hypothesis:
Implementing a standardized multimodal analgesic protocol will decrease the amount of opioids prescribed at the time of surgery as well as the total amount of opioids dispensed postoperatively.
Study Design:
Case series; Level of evidence, 4.
Methods:
Patients who had undergone meniscectomy, rotator cuff repair (RCR), or anterior cruciate ligament (ACL) reconstruction at our institution were identified by Current Procedural Terminology code 12 months prior to and 6 months after the initiation of a standardized multimodal postoperative pain protocol. Records were reviewed to extract demographic data, amount of opioids prescribed at the time of surgery, amount and frequency of opioid refills, and call-ins regarding pain medication or its side effects. A Wilcoxon rank-sum test was used to evaluate differences in opioid prescriptions between pre- and postprotocol, and significance was set to P < .05.
Results:
The mean amount of opioids prescribed at the time of surgery decreased from 63.5 to 22.3 pills (P < .0001) for meniscectomy, from 73.3 to 39.7 (P < .0001) for ACL reconstruction, and from 75.6 to 39.8 (P < .0001) for RCR. The percentage of patients receiving a refill of opioids during the postoperative period also decreased for all groups: from 13% to 4% (P = .0051) for meniscectomy, 29.2% to 11.4% (P = .0005) for ACL reconstruction, and 47.3% to 24.4% (P < .0001) for RCR. There was no significant difference in patient calls regarding pain medication or its side effects.
Conclusion:
Institution of a standardized multimodal analgesia protocol significantly decreased the amount of opioids dispensed after common arthroscopic procedures. This reduction in the amount of opioids given on the day of surgery did not result in an increased demand for refills. Our study also demonstrated that 20 opioid pills were adequate for patients undergoing meniscectomy and 40 pills were adequate for ACL reconstruction and RCR in the majority of cases. This protocol serves as a way for providers to decrease the amount of opioids dispensed after surgery while providing patients with alternatives for pain relief.
Keywords: opioid, meniscectomy, ACL reconstruction, rotator cuff repair, multimodal analgesia
The opioid epidemic in the United States has become a problem on an individual and societal level. The United States is responsible for >80% of the world’s consumption of narcotic pain medication.13 Studies have demonstrated that the main source of opioid pain medication being used for nonmedical purposes comes from a friend or relative who has received a prescription from a single provider.13 Leftover opioid pain medication after surgery falls into this pool and is subject to abuse. Other studies have shown that the majority of patients who undergo surgery have leftover opioid pain medication, and most do not know how to properly dispose of it.7
Orthopaedic surgeons are among the top surgical subspecialists prescribing opioid pain medication.23 Providers are challenged to balance providing patients with adequate pain control after surgery with avoiding the excessive prescription of opioid pain medication. However, the definition of “appropriate amount of opioids” is poorly defined and likely variable according to which surgical procedure is performed. Several studies have attempted to quantify how much narcotic pain medication patients take after particular orthopaedic procedures, but more of these studies are needed.10,15
In an attempt to decrease the amount of opioid pain mediation dispensed after outpatient arthroscopic procedures, we developed a multimodal analgesic regimen with our pharmacy team to provide patients with a limited amount of opioid pain medication and additional medications that address other facets of the pain pathway. The purpose of the current study was to investigate whether implementation of a multimodal analgesic regimen policy can decrease the amount of opioid pain medication dispensed to patients undergoing common arthroscopic procedures. We hypothesized that the institution of this policy (1) has decreased the initial amount of opioid pain medication prescribed after surgery as well as the total amount of opioid pain medication dispensed and (2) has not resulted in an increase of opioid refill demands.
Methods
The study was approved by our institutional review board, determined to be Health Insurance Portability and Accountability Act (HIPAA) compliant. A multimodal analgesic protocol was developed, and decisions about the amount of opioid pills to prescribe were made per consensus between providers and pharmacists at our institution. This regimen utilized scheduled acetaminophen, anti-inflammatories, and gabapentin during the first 2 weeks after surgery, starting on postoperative day zero. Aspirin was included in the regimen with meloxicam for its antiplatelet function. Although both are nonsteroidal anti-inflammatories, meloxicam is a selective COX-2 inhibitor and was chosen to decrease the risk of gastrointestinal complications. A limited number of opioid pills (oxycodone, 5-mg tablets) were prescribed: either 20 pills for patients who underwent arthroscopy without soft tissue repair or reconstruction or 40 pills for patients who had any soft tissue repair or reconstruction (Table 1). If a patient had an allergy to oxycodone, an alternative opioid was prescribed. If a patient had any contraindication for the use of anti-inflammatories (eg, renal insufficiency, peptic ulcer disease), these were also omitted from their home-going regimen.
TABLE 1.
Standardized Multimodal Analgesic Protocol to Guide Prescribing Habits After Outpatient Arthroscopic Surgerya
| Scheduled | ||
| Acetaminophen | 650 mg q4H | 14 d |
| Meloxicam | 15 mg daily | 14 d |
| Gabapentin | 300 mg TID | 14 d |
| Aspirin | 325 mg daily | 14 d |
| PRN | ||
| Oxycodone | 5 mg q4H PRN | 20 tablets for no repairb |
| 40 tablets for repairc |
aPRN, as needed; q4H, every 4 hours; TID, 3 times daily.
bNo repair included shoulder, elbow, or knee arthroscopy.
cRepair included any ligament, labral, tendon, meniscal, or cartilage repair or reconstruction.
The care team members involved in the study educated patients and families prior to surgery about appropriate use of pain medication after surgery. Although this was not a formal education plan, our physicians, physician assistants, and nurses counseled patients to use opioid pain medications only as needed and to discontinue their usage as soon as possible, as it has been shown that preoperative education can significantly decrease opioid use.20 Providers were instructed to adhere to the policy when writing postoperative prescriptions. Prior to instituting this pain control regimen, the number of prescribed opioid pain medications after surgical procedures was relatively random and based on the prescribing provider’s preference. Alternative forms of analgesia other than opioids were not routinely prescribed at the time of surgery prior to the protocol but were encouraged. Cryotherapy was encouraged in the postoperative period.
We retrospectively compared the records of patients who had undergone arthroscopic meniscectomy, rotator cuff repair (RCR), and anterior cruciate ligament (ACL) reconstruction 12 months prior to versus 6 months after the implementation of the multimodal analgesic protocol. Medical record numbers of patients were gathered according to the following codes, per Current Procedural Terminology, fourth edition–Healthcare Common Procedure Coding System (CPT 4–HCPCS): 29880 or 29881 for meniscectomy; 29888 for ACL reconstruction; and 23410, 24312, or 29827 for RCR. Records were reviewed to ensure that the primary procedure was one of the 3 listed here, and patients who had additional procedures in the same setting were excluded.
Demographic data were extracted from the patient record and included age, sex, body mass index, smoking status, preoperative opioid use, and American Society of Anesthesiologists score (Table 2). The initial amount and type of opioid pain medication prescribed after surgery were recorded. Any additional refills or refill requests were also documented. Records were screened for documentation of patient calls to the provider’s care team regarding side effects, pain control concerns, and refill requests.
TABLE 2.
Demographic Data of Pre- and Postprotocol Cohorts for Each Procedure Studieda
| Meniscectomy | ACL Reconstruction | RCR | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre (n = 283) | Post (n = 126) | P Value | Pre (n = 199) | Post (n = 105) | P Value | Pre (n = 184) | Post (n = 115) | P Value | |
| Mean age, y | 40.1 | 41.9 | .324 | 26.1 | 28.5 | .246 | 53 | 52.2 | .954 |
| Mean BMI | 30.1 | 31.6 | .294 | 27 | 27.7 | .274 | 31 | 31.7 | .524 |
| Female, % | 43.1 | 36.5 | .21 | 41.2 | 42.9 | .781 | 34.8 | 35.7 | .878 |
| Smokers, % | 14.5 | 15.1 | .876 | 12.6 | 17.1 | .276 | 23.4 | 22.6 | .879 |
| Preoperative opiate use, n (%) | 43 (15.2) | 17 (13.5) | .653 | 27 (13.6) | 13 (12.4) | .771 | 51 (27.7) | 36 (31.3) | .507 |
| Mean ASA score | 1.67 | 1.72 | .42 | 1.33 | 1.46 | .081 | 1.98 | 1.97 | .807 |
aACL, anterior cruciate ligament; ASA, American Society of Anesthesiologists; BMI, body mass index; Post, postprotocol; Pre, preprotocol; RCR, rotator cuff repair.
Univariate analysis was carried out to detect statistically significant differences in opioid prescriptions at the time of surgery and after surgery, as well as differences in demographic data among the cohorts of patients (Table 2). A Wilcoxon rank-sum test was used for continuous variables, and chi-square or Fisher exact test was used for categorical variables. Significance was set at P < .05.
Results
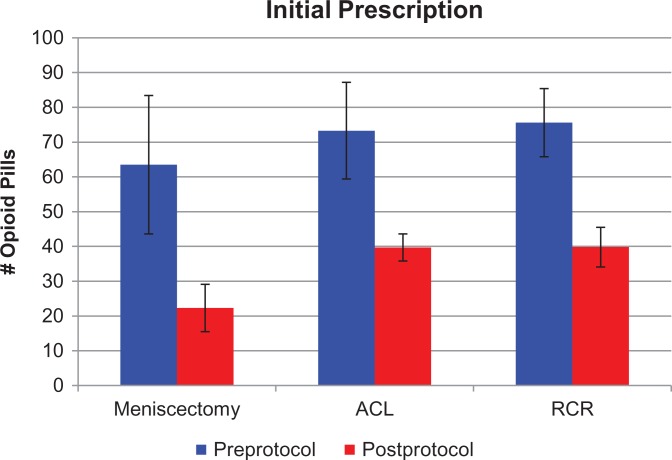
There was no statistically significant difference in patient age, body mass index, sex, American Society of Anesthesiologists score, preoperative opioid use, or smoking status between the pre- and postprotocol cohorts. There was a statistically significant decrease in the amount of opioid pills prescribed at the time of surgery for all 3 surgery types. The mean amount of opioid pills prescribed on the day of surgery decreased by 64.9%, from 63.5 pills (range, 15-80) to 22.3 (range, 10-40; P < .0001) for meniscectomy; by 45.8%, from 73.3 (range, 15-80) to 39.7 (range, 14-45; P < .0001) for ACL reconstruction; and by 47.4%, from 75.6 (range, 20-90) to 39.8 (range, 0-60; P < .0001) for RCR (Figure 1 and Table 3). Differences from the protocol in the mean amount of pills prescribed (ie, 22.3 vs 20 pills; 39.7 and 39.8 vs 40 pills) were likely secondary to protocol deviation among the prescribing providers. Prior to the protocol’s institution, the most common opioid prescribed was oxycodone/acetaminophen pills (5 mg/325 mg), followed by hydrocodone/acetaminophen pills (5 mg/325 mg).
Figure 1.
Mean number of opioid pills prescribed at the time of surgery after meniscectomy, anterior cruciate ligament (ACL) reconstruction, and rotator cuff repair (RCR) before and after institution of the standardized multimodal analgesic protocol. Error bars represent 1 SD.
TABLE 3.
Pre- and Postprotocol Results by Procedurea
| Meniscectomy | ACL Reconstruction | RCR | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | P Value | Pre | Post | P Value | Pre | Post | P Value | |
| No. of pills prescribedb | 63.5 ± 19.9 | 22.3 ± 6.8 | <.0001 | 73.3 ± 13.9 | 39.7 ± 3.9 | <.0001 | 75.6 ± 9.8 | 39.8 ± 5.7 | <.0001 |
| Patients receiving refill,c % | 13.00 | 4.00 | .0051 | 29.20 | 11.40 | .0005 | 47.30 | 24.40 | <.0001 |
| Call-ins,d % | 3.50 | 4.00 | .7827 | 19.60 | 14.30 | .2492 | 10.87 | 5.20 | .0915 |
aACL, anterior cruciate ligament; Post, postprotocol; Pre, preprotocol; RCR, rotator cuff repair.
bMean ± SD.
cPercentage of patients receiving a refill of opioid medication.
dPercentage of patients calling the clinic for refills of their pain medication for each procedure.
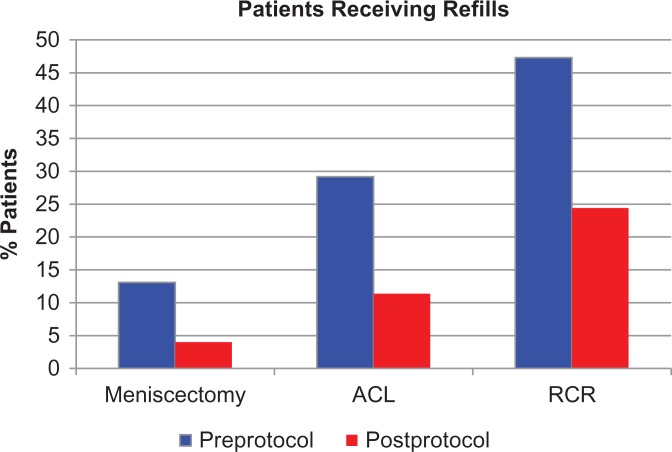
The percentage of patients receiving a refill of narcotics in the postoperative period also decreased for all groups: 13% (37 of 284) to 4% (5 of 125; P = .0051) in the meniscectomy group, 29.2% (59 of 199) to 11.4% (12 of 105; P = .0005) in the ACL reconstruction group, and 47.3% (87 of 184) to 24.4% (28 of 114; P < .0001) in the RCR group (Figure 2). There was no significant difference in the number of patients calling into the clinic after surgery regarding their pain medication before and after institution of our protocol; reasons for these calls included refill requests and side effects of the medication. Among our internal records, we did not observe any complications with the use of anti-inflammatories, such as gastrointestinal bleeding or wound-healing issues. Results are summarized in Table 3.
Figure 2.
Percentage of patients receiving a refill in the postoperative period following meniscectomy, anterior cruciate ligament (ACL) reconstruction, and rotator cuff repair (RCR) before and after pain protocol initiation.
Discussion
This study demonstrates that the implementation of a standardized multimodal analgesic regimen significantly decreased the amount of opioid pain medication prescribed in the postoperative period after common arthroscopic procedures. Remarkably, we observed a decrease in refills despite lowering the number of opioid pills prescribed after surgery. In this study, we come closer to defining what an appropriate amount of opioid pain mediation is after meniscectomy, RCR, and ACL reconstruction. In the face of the opioid epidemic, this protocol serves as an example of a way in which providers can decrease the amount of opioid pain medication dispensed to patients after surgery, resulting in fewer excess pills available for misuse.
The excessive prescription of narcotic pain medication in the United States has become a national crisis, as there has been a rapid increase in opioid consumption over the past decade. The timing of this increase correlates with the campaign of pain as the fifth vital sign.16 With increasing emphasis on patient satisfaction and patient-reported outcomes, providers are pressured to adequately treat a patient’s pain. It is of utmost importance that providers attempt to decrease the amount of opioid pain medication dispensed after surgery while still providing patients with adequate pain control.
Several studies in the orthopaedic literature have demonstrated that patients often have unused opioid pain medicine after surgery.8,9,14 These leftover pills fall into the most common source of abused pills—those obtained from friends and relatives who have been provided with a prescription from a single provider.13 Our study demonstrated that 20 opioid pills were adequate for the majority of patients undergoing meniscectomy and 40 opioid pills were adequate for most patients undergoing ACL reconstruction or RCR.
Few studies in the sports medicine literature have had the primary objective of quantifying the amount of opioids prescribed after particular procedures.25,26 Most data on opioid consumption come from studies that record its use as a surrogate for pain control as a secondary measure during the first few postoperative days.11,17 In a recent prospective study, Wojahn et al26 assessed opioid consumption after outpatient knee arthroscopy and demonstrated that patients took a median of 7 pills. They also demonstrated that meniscal repair predicted higher opioid consumption as compared with partial meniscectomy, loose body removal, debridement, or chondroplasty. These results suggest that the number of opioids given in the current protocol could be further decreased. More prospective studies like this one are needed to help create guidelines for responsible opioid-prescribing practices.
Multimodal analgesia refers to the use of ≥2 types of pain-relieving interventions with different mechanisms of action. There are multiple studies investigating the impact of multimodal analgesia on opioid consumption in the perioperative period.18,22,24 However, most of these studies implement alternative analgesic modalities preoperatively, such as an anti-inflammatory,4,21 neuropathic medicines,1,2 or regional anesthesia.5,12 Few studies have investigated a multimodal regimen prescribed in the postoperative period beyond the first few days after surgery.3
Two studies in the hand and upper extremity literature implemented a postoperative protocol and were successful in reducing the amount of opioids dispensed after surgery.6,19 Stanek et al19 utilized guidelines for upper extremity surgical procedures, including regional anesthesia, scheduled ibuprofen, Tylenol (acetaminophen), and recommendations on the amount of opioids to prescribe for particular procedures. Earp et al6 instituted a procedure-specific protocol with tiered amounts of opioids scaled for procedure type. Both author groups found that after implementation of a protocol, there was a significant decrease in the amount of opioid pain medication prescribed after procedures.
There are several limitations to our current study. First, owing to the retrospective nature of this study, we were not able to determine the ultimate cause of the decrease in opioid prescriptions after initiation of the protocol—whether it be secondary to the alternative scheduled analgesics prescribed at the time of surgery, increased awareness of prescribing habits with implementation of a protocol among providers, or the preoperative counseling provided to the patients regarding the appropriate use of opioid pain medication. Second, we were only able to report how many opioid pills were prescribed, and we did not have information about how many were consumed. Therefore, we cannot make recommendations regarding the appropriate amount of opioids to prescribe for these procedures from this study, but we can conclude that the amount used in the protocol was an adequate upper limit for the majority of our patients. Additionally, we do not know whether patients obtained opioid refills from a provider outside our institution. The state in which the study was performed does have an opioid registry; however, retrospective research does not fall within its acceptable use policy. We also did not report patient-reported outcomes or patient satisfaction with this new pain regimen or quantify side effects reported from the medications, although it is encouraging that there was no significant increase in refills received or calls to the clinic. Finally, the patients were grouped into procedure type according to CPT code. Although charts were reviewed to ensure that the primary procedure was meniscectomy, ACL reconstruction, or RCR, details about graft type or additional minor procedures during the case were not taken into account.
Conclusion
After implementation of a standardized multimodal analgesic protocol, we noted a significant decrease in the amount of opioid medication dispensed after common arthroscopic procedures without increases in refills received in the weeks following surgery. This study also demonstrates that 20 opioid pills were adequate for the majority of patients undergoing meniscectomy and 40 opioid pills were adequate for the majority of patients undergoing ACL reconstruction or RCR in the majority of cases. Further studies are warranted, as the appropriate number of opioid medications for these procedures can likely be further decreased. In the face of the opioid epidemic in the United States, this protocol serves as an example of a way for providers to decrease the amount of opioid pills dispensed after surgery while providing patients with alternative means of pain control.
Acknowledgment
The authors acknowledge Lee Kral, PharmD, for collaboration in developing the multimodal analgesia protocol and Natalie Glass, PhD, for her statistical contributions.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: R.W.W. has received educational support from Arthrex and Smith & Nephew and hospitality payments from Medical Device Business Systems. M.B. has received speaking fees from Arthrex. B.R.W. has received educational support from Arthrex and Smith & Nephew and consulting fees and royalties from ConMed Linvatec. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Iowa (study No. 201801724).
References
- 1. Adam F, Menigaux C, Sessler DI, Chauvin M. A single preoperative dose of gabapentin (800 milligrams) does not augment postoperative analgesia in patients given interscalene brachial plexus blocks for arthroscopic shoulder surgery. Anesth Analg. 2006;103(5):1278–1282. [DOI] [PubMed] [Google Scholar]
- 2. Bang SR, Yu SK, Kim TH. Can gabapentin help reduce postoperative pain in arthroscopic rotator cuff repair? A prospective, randomized, double-blind study. Arthroscopy. 2010;26(9):S106–S111. [DOI] [PubMed] [Google Scholar]
- 3. Brown DW, Curry CM, Ruterbories LM, Avery FL, Anson PS. Evaluation of pain after arthroscopically assisted anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25(2):182–186. [DOI] [PubMed] [Google Scholar]
- 4. Dahl V, Dybvik T, Steen T, Aune AK, Rosenlund EK, Raeder JC. Ibuprofen vs acetaminophen vs ibuprofen and acetaminophen after arthroscopically assisted anterior cruciate ligament reconstruction. Eur J Anaesthesiol. 2004;21(6):471–475. [DOI] [PubMed] [Google Scholar]
- 5. DeMarco JR, Componovo R, Barfield WR, Liles L, Nietert P. Efficacy of augmenting a subacromial continuous-infusion pump with a preoperative interscalene block in outpatient arthroscopic shoulder surgery: a prospective, randomized, blinded, and placebo-controlled study. Arthroscopy. 2011;27(5):603–610. [DOI] [PubMed] [Google Scholar]
- 6. Earp BE, Silver JA, Mora AN, Blazar PE. Implementing a postoperative opioid-prescribing protocol significantly reduces the total morphine milligram equivalents prescribed. J Bone Joint Surg Am. 2018;100(19):1698–1703. [DOI] [PubMed] [Google Scholar]
- 7. Feinberg AE, Chesney TR, Srikandarajah S, Acuna SA, McLeod RS. Opioid use after discharge in postoperative patients: a systematic review. Ann Surg. 2018;267(6):1056–1062. [DOI] [PubMed] [Google Scholar]
- 8. Kim N, Matzon JL, Abboudi J, et al. A prospective evaluation of opioid utilization after upper-extremity surgical procedures: identifying consumption patterns and determining prescribing guidelines. J Bone Joint Surg Am. 2016;98(20):e89. [DOI] [PubMed] [Google Scholar]
- 9. Kumar K, Gulotta LV, Dines JS, et al. Unused opioid pills after outpatient shoulder surgeries given current perioperative prescribing habits. Am J Sports Med. 2017;45(3):636–641. [DOI] [PubMed] [Google Scholar]
- 10. Lovecchio F, Derman P, Stepan J, et al. Support for safer opioid prescribing practices: a catalog of published use after orthopaedic surgery. J Bone Joint Surg Am. 2017;99(22):1945–1955. [DOI] [PubMed] [Google Scholar]
- 11. Lubowitz JH, Schwartzberg R, Smith P. Randomized controlled trial comparing all-inside anterior cruciate ligament reconstruction technique with anterior cruciate ligament reconstruction with a full tibial tunnel. Arthroscopy. 2013;29(7):1195–1200. [DOI] [PubMed] [Google Scholar]
- 12. Malik T, Mass D, Cohn S. Postoperative analgesia in a prolonged continuous interscalene block versus single-shot block in outpatient arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy. 2016;32(8):1544–1550. [DOI] [PubMed] [Google Scholar]
- 13. Manchikanti L, Singh A. Therapeutic opioids: a ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain Physician. 2008;11(2):S63–S88. [PubMed] [Google Scholar]
- 14. Rodgers J, Cunningham K, Fitzgerald K, Finnerty E. Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am. 2012;37(4):645–650. [DOI] [PubMed] [Google Scholar]
- 15. Sabatino MJ, Kunkel ST, Ramkumar DB, Keeney BJ, Jevsevar DS. Excess opioid medication and variation in prescribing patterns following common orthopaedic procedures. J Bone Joint Surg Am. 2018;100(3):180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sandlin D. The new Joint Commission Accreditation of Healthcare Organizations’ requirements for pain assessment and treatment: a pain in the assessment? J Perianesth Nurs. 2000;15(3):182–184. [DOI] [PubMed] [Google Scholar]
- 17. Schwartzberg RS, Reuss BL, Rust R. Efficacy of continuous subacromial bupivacaine infusion for pain control after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2013;22(10):1320–1324. [DOI] [PubMed] [Google Scholar]
- 18. Secrist ES, Freedman KB, Ciccotti MG, Mazur DW, Hammoud S. Pain management after outpatient anterior cruciate ligament reconstruction: a systematic review of randomized controlled trials. Am J Sports Med. 2016;44(9):2435–2447. [DOI] [PubMed] [Google Scholar]
- 19. Stanek JJ, Renslow MA, Kalliainen LK. The effect of an educational program on opioid prescription patterns in hand surgery: a quality improvement program. J Hand Surg Am. 2015;40(2):341–346. [DOI] [PubMed] [Google Scholar]
- 20. Syed UAM, Aleem AW, Wowkanech C, et al. Neer Award 2018. The effect of preoperative education on opioid consumption in patients undergoing arthroscopic rotator cuff repair: a prospective, randomized clinical trial. J Shoulder Elbow Surg. 2018;27(6):962–967. [DOI] [PubMed] [Google Scholar]
- 21. Toivonen J, Pitko VM, Rosenberg PH. Etoricoxib pre-medication combined with intra-operative subacromial block for pain after arthroscopic acromioplasty. Acta Anaesthesiol Scand. 2007;51(3):316–321. [DOI] [PubMed] [Google Scholar]
- 22. Uquillas CA, Capogna BM, Rossy WH, Mahure SA, Rokito AS. Postoperative pain control after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25(7):1204–1213. [DOI] [PubMed] [Google Scholar]
- 23. Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SR. Characteristics of opioid prescriptions in 2009. JAMA. 2011;305(13):1299–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Warrender WJ, Syed UAM, Hammoud S, et al. Pain management after outpatient shoulder arthroscopy: a systematic review of randomized controlled trials. Am J Sports Med. 2017;45(7):1676–1686. [DOI] [PubMed] [Google Scholar]
- 25. Welton KL, Kraeutler MJ, McCarty EC, Vidal AF, Bravman JT. Current pain prescribing habits for common shoulder operations: a survey of the American Shoulder and Elbow Surgeons membership. J Shoulder Elbow Surg. 2018;27(6):S76–S81. [DOI] [PubMed] [Google Scholar]
- 26. Wojahn RD, Bogunovic L, Brophy RH, et al. Opioid consumption after knee arthroscopy. J Bone Joint Surg Am. 2018;100(19):1629–1636. [DOI] [PubMed] [Google Scholar]