Key Points
Mice with Adamts13−/− or a heterozygous cfh mutation (ie, chfW1206R) do not develop spontaneous TMA.
However, mice carrying Adamts13−/−cfhW1206R or cfhR1206R develop TMA with a significantly increased mortality rate.
Abstract
Severe deficiency of plasma ADAMTS13 activity is the primary cause of thrombotic thrombocytopenic purpura (TTP) whereas overwhelming activation of complement via an alternative pathway results in atypical hemolytic uremic syndrome (aHUS), the prototypes of thrombotic microangiopathy (TMA). However, clinical and pathogenic distinctions between TTP and aHUS are often quite challenging. Clinical reports have suggested that complement activation may play a role in the development of TTP, which is caused by severe deficiency of plasma ADAMTS13 activity. However, the experimental evidence to support this hypothesis is still lacking. Here, we show that mice with either Adamts13−/− or a heterozygous mutation of complement factor H (cfh) at amino acid residue of 1206 (ie, cfhW/R) alone remain asymptomatic despite the presence of occasional microvascular thrombi in various organ tissues. However, mice carrying both Adamts13−/− and cfhW/R exhibit thrombocytopenia, low haptoglobin, increased fragmentation of erythrocytes in peripheral blood smear, increased plasma levels of lactate dehydrogenase activity, blood urea nitrogen, and creatinine, as well as an increased mortality rate, consistent with the development of TMA. Moreover, mice with a homozygous mutation of cfh (ie, cfhR/R) with or without Adamts13−/− developed severe TMA. The mortality rate in mice with Adamts13−/−cfhR/R was significantly higher than that in mice with cfhR/R alone. Histological and immunohistochemical analyses demonstrated the presence of disseminated platelet-rich thrombi in terminal arterioles and capillaries of major organ tissues in these mice that were either euthanized or died. Together, our results support a synergistic effect of severe ADAMTS13 deficiency and complement activation in pathogenesis of TMA in mice.
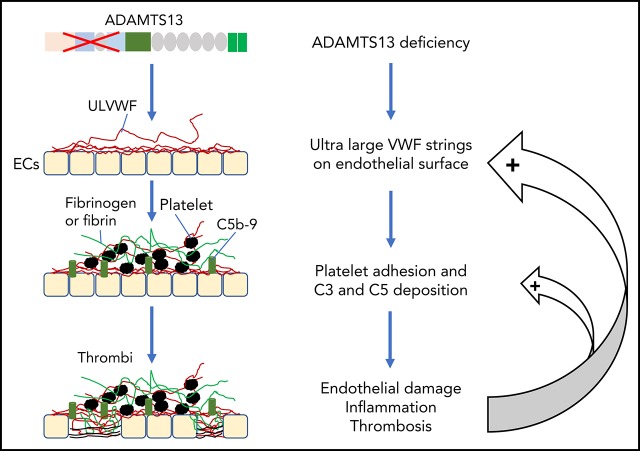
Visual Abstract
Introduction
Thrombotic microangiopathy (TMA) is a heterogeneous group of thrombotic disorders characterized by severe thrombocytopenia and microangiopathic hemolytic anemia with various degrees of terminal organ injury.1-3 TMA may develop following infection with Shiga toxin–producing Escherichia coli (STEC), resulting in hemolytic uremic syndrome (HUS), known as STEC-HUS.4,5 TMA may also be caused by the lack of a plasma metalloprotease ADAMTS13 activity, rendering it incapable of cleaving ultra-large von Willebrand factor (ULVWF) released from activated or injured endothelial cells. This type of TMA is known as thrombotic thrombocytopenic purpura (TTP).6-9 Furthermore, TMA may be caused by uncontrolled activation of the complement system, most commonly via its alternative complement pathway. This type of TMA is referred to as atypical HUS (aHUS).10,11
STEC-HUS, commonly seen in children under 5 years of age, accounts for 90% of all cases of HUS, resulting primarily from E coli O157 infection.5,12,13 Upon infection with STEC, Shiga toxin A and B are produced in the gut and then enter into the circulation where they trigger acute inflammation, release of ULVWF, and loss of thrombomodulin on the endothelial surface, resulting in a prothrombotic state.14-16 aHUS, seen in both children and adults, is primarily caused by excessive activation of the complement system via its alternative pathway. This may take place when the function of complement-regulatory proteins is compromised, such as in cases with mutations in complement factor H (CFH),17,18 factor I (CFI),17,19 and membrane cofactor protein (MCP),17,20,21 as well as thrombomodulin22 or when a mutation in C323,24 or factor B (CFB)25,26 occurs, which results in resistance to inhibition by the complement-regulatory proteins.
In humans, the disease penetrance for aHUS with a known heterozygous mutation in CFH (or CFI) is only 50%27; in mice, a heterozygous mutation of cfh at the amino acid residue of 1206 (ie, cfhW/R), which corresponds to the CFH mutation (W/R) at the amino acid residue of 1183 in patients with aHUS,28 does not result in a symptomatic aHUS as we previously reported.29 This suggests that additional environmental or genetic factors may be necessary to trigger the onset and result in progression of aHUS.
Approximately 95% of TTP cases are caused by acquired autoantibodies against ADAMTS13 protease8,30; only less than 5% of TTP cases are caused by inherited mutations in ADAMTS13.7,31,32 Similar to aHUS, some children with hereditary deficiency of ADAMTS13 develop their first acute episode early in life, but others may develop their first episode of TTP in adulthood, usually triggered by infections or pregnancy.31,32 In almost every case of TTP, there are evidences of neutrophil and complement activation, indicated by the marked elevation of plasma levels of human neutrophil peptides (HNPs),33 DNA, myeloperoxidase,34 histone-DNA complexes,33 Bb, C3a, C3b, C5a, and sC5b-9.33,35-38 Some patients with refractory TTP caused by severe ADAMTS13 deficiency appeared to respond to treatment with eculizumab,39-41 a monoclonal antibody against complement C5, which is shown to block the formation of terminal membrane attack complexes. These results allow us to hypothesize that there may be a synergy between ADAMTS13 deficiency and complement activation in pathogenesis of TMA.
To test this hypothesis, we took advantage of 2 existing mouse lines, Adamts13−/− (Motto et al42) and cfhW/R (Ueda et al29), to generate a new strain of mice with a combined mutation in Adamts13 and cfh. Our results demonstrate that mice with either Adamts13−/− or cfhW/R remain asymptomatic, but mice with cfhW/R in the Adamts13−/− background exhibit thrombocytopenia, elevated lactate dehydrogenase (LDH) and creatinine, and as well, an increased mortality rate, consistent with the development of TMA. Additionally, mice with cfhR/R on top of Adamts13−/− exhibit more severe organ damage and increased mortality than cfhR/R alone. Our results suggest a synergistic effect of severe ADATMS13 deficiency and complement activation in the pathogenesis of TMA. These findings may provide a rationale for a more targeted therapeutic intervention in patients with refractory TMA.
Methods
Animals
All animal experimental protocols were approved by the institutional animal care and use committee at the University of Alabama at Birmingham. All mutant mice were derived from wild-type (wt) C57BL/6J. Adamts13−/− mice (kindly provided by David Ginsburg, University of Michigan, Ann Arbor, MI)42 were bred with mice carrying a heterozygous cfh mutation (cfh; ie, cfhW/R)29 to generate heterozygous mutations in both Adamts13 and cfh (ie, Adamts13+/−cfhW/R) mice. These mice were then bred to generate mice with various combinations of Adamts13 and cfh mutations (ie, Adamts13−/−cfhW/R and Adamts13−/−cfhR/R). These mice were then compared phenotypically with the age- and sex-matched control mice (eg, wt, Adamts13−/−, cfhW/R, and cfhR/R) in the same genetic background.
Genotyping
All phenotypical data were collected prior to the genotyping or blinded with the genotypes. Genotyping for Adamts13 was performed by polymerase chain reaction amplification with 4 pairs of primers according to the strategy described previously.42,43 For cfh genotyping, Sanger sequencing was performed in the amplified polymerase chain reaction product (forward primer, ATTGACCAGCTACAGACAGTATCA; reverse primer, CATGCATGTGCCTTTCTAA-ACA).
CBCs and erythrocyte morphology analysis
Whole blood was collected via retro-orbital sinus into a heparin-coated capillary tube and anticoagulated with 0.32% sodium citrate. Complete blood counts (CBCs) were performed using a Hemavet 950FS analyzer (Drew Scientific, Miami Lakes, FL).43 Additionally, a thin blood smear was prepared for each sample and fixed in methanol, and stained with Wright-Giemsa stain (Sigma-Aldrich, St. Louis, MO).
Assay for plasma haptoglobin
Plasma haptoglobin was determined using a murine-specific haptoglobin enzyme-linked immunosorbent assay (ELISA) (Abcam, Cambridge, MA).44
Assays for plasma blood urea nitrogen, creatinine, and LDH
Plasma urea nitrogen was determined using a urea nitrogen colorimetric detection assay (Invitrogen, Frederick, MD). Plasma creatinine was determined using a creatinine colorimetric assay (Sigma-Aldrich).45 Plasma LDH levels were determined using an LDH activity assay (Sigma-Aldrich).46 All assays were performed on plasma according to the manufacturers’ instructions.
Assay for plasma soluble C5b-9 complexes
Plasma soluble C5-9 complexes (sC5b-9) levels were determined using the High Sensitivity sC5-9 ELISA kit according to the manufacturer’s recommendation (Aviva Systems Biology, San Diego, CA).
Plasma VWF antigen and multimer analysis
Murine plasma von Willebrand factor (VWF) antigen levels were quantified by an in-house ELISA as described previously.29 Plasma VWF multimers were determined by western blotting following electrophoresis on 1% agarose gel and capillary transferring to membrane. The western blot was performed with a rabbit anti-human VWF immunoglobulin G (IgG; Dako, Glostrup, Denmark) as the primary antibody and IRDye800-labeled goat anti-rabbit IgG (LI-COR Biosciences, Lincoln, NE) as the secondary antibody.47
Histology and immunohistochemical studies
Major organ tissues were harvested from mice of various genotypes when they died or when they were euthanized at the age of ∼2 months. The tissues (brain, heart, intestine, kidney, liver, and lung) were fixed in 4% paraformaldehyde in phosphate-buffered saline and were then paraffin-embedded. Thin sections (6 µm) were prepared using a microtome and stained with hematoxylin and eosin (H&E). Additionally, the adjacent sections were used for immunohistochemical staining for VWF, glycoprotein IIb/IIIa (GPIIb/IIIa), and fibrinogen using a rabbit anti-human VWF IgG (Dako), a mouse anti-human GPIIb/IIIa antibody (a gift from Heyu Ni, University of Toronto, Toronto, ON, Canada), and a rabbit anti-human fibrinogen IgG (Dako), respectively, followed by the peroxidase-conjugated secondary antibody and color reaction with 3,3′-diaminobenzidine/H2O2. Digital images were taken using a Carl Zeiss Axioplan light microscope (Göttingen, Germany) at magnification of ×200.
Statistical analysis
All data were expressed as the median in a box-whisker plot (minimum to maximum values) or as the mean ± a standard deviation (SD). The Mann-Whitney U test was used for comparison between 2 groups. A 1-sample Student t test between proportions was performed to determine whether there was a statistically significant difference between the expected percentage and the observed percentage of certain genotype using MedCalc software (Ostend, Belgium). P < .05 was considered to be statistically significant. The death of affected mice was monitored daily for 180 days. A Kaplan-Meier survival plot and statistical analysis were performed using GraphPad Prism 7 (GraphPad, La Jolla, CA).
Results
Distribution of various genotypes in mice
Table 1 shows the expected and the observed distribution of mice with various genotypes at 4 weeks of age after crossing Adamts13−/−cfhW/W with Adamts13−/−cfhW/R or Adamts13−/−cfhW/R with Adamts13−/−cfhW/R mice. As shown, the percentage of mice with Adamts13−/−cfhW/R (37.5%) was significantly lower than the expected percentage of 50% (P = .01) (Table 1, top panel). Additionally, as the percentage of Adamts13−/−cfhW/W mice was significantly higher (P = .01) than the expected percentage of 25% based on the Mendelian distribution, the percentage of mice with the Adamts13−/−cfhW/R (45.2%) and Adamts13−/−cfhR/R (22.3%) genotype was also modestly lower than the expected 50% and 25%, respectively (Table 1, bottom panel). However, these differences were not statistically significant. These results suggest that only a small subset of mice carrying the heterozygous or homozygous mutation in cfh on top of Adamts13−/− may be lethal in utero or expire shortly after birth.
Table 1.
Expected and obtained distribution of mice with various genotypes
| Genotype | N | Expected, % | Observed, % |
|---|---|---|---|
| a13−/−cfhW/W × a13−/−cfhW/R | |||
| a13−/−cfhW/W | 60 | 50 | 62.5* |
| a13−/−cfhW/R | 36 | 50 | 37.5* |
| a13−/−cfhW/R × a13−/−cfhW/R | |||
| a13−/−cfhW/W | 64 | 25 | 32.5 |
| a13−/−cfhW/R | 89 | 50 | 45.2 |
| a13−/−cfhR/R | 44 | 25 | 22.3 |
A Student t test was performed for comparing the difference between the percent observed and expected. The null hypothesis value (percentage expected) is based on the Mendelian distribution.
a13−/−, Adamts13 null; cfh, complement factor H; cfhW/W, cfhW/R, and cfhR/R represent wild-type, heterozygous, and homozygous mutations in the gene encoding cfh at the position of 1206.
P < .05.
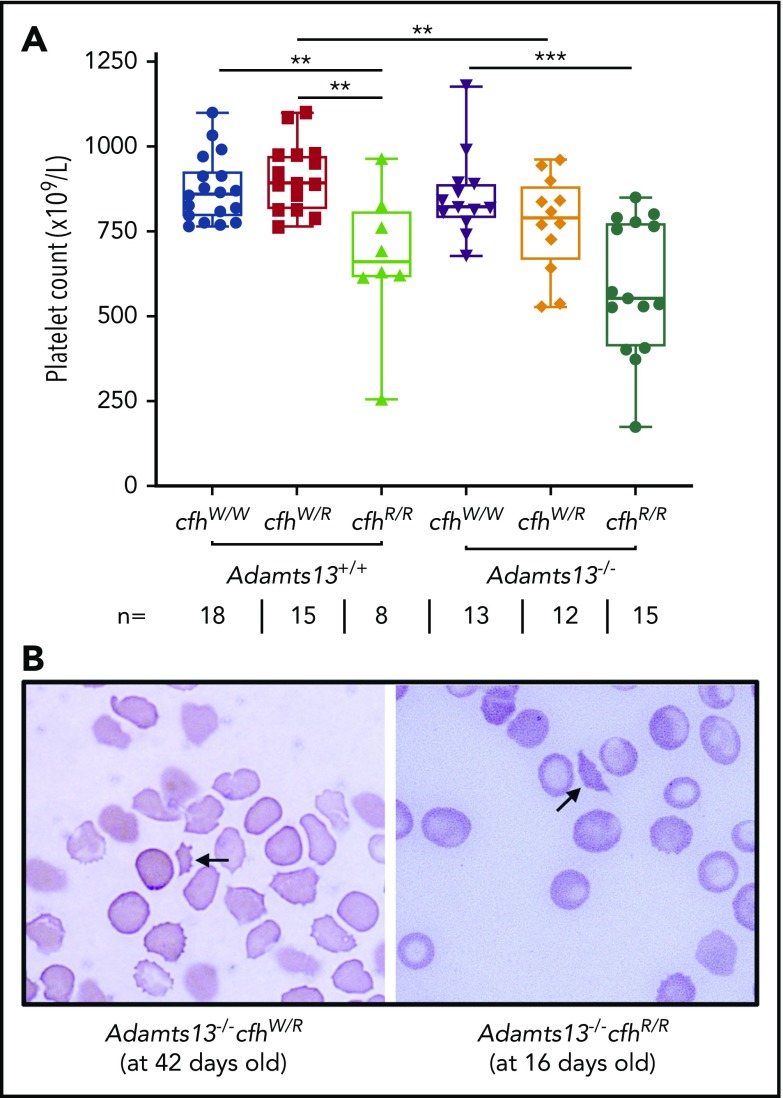
Platelet counts in mice with various genotypes
A CBC was performed in each of the adult mice who survived to the age of 2 to 3 months. Platelet counts have been shown to be the most sensitive marker for the diagnosis of TMA in mice.43,48 As shown, there were significantly lower median platelet counts in mice with cfhR/R (662 × 109/L) than in those with cfhW/R (893 × 109/L) (P = .0018) and in wt mice (861 × 109/L) (P = .0042) (Figure 1A). Similarly, there were significantly lower median platelet counts in mice with Adamts13−/−cfhW/R (791 × 109/L) or Adamts13−/−cfhR/R (553 × 109/L) than in mice with cfhW/R (893 × 109/L) or Adamts13−/− (821 × 109/L) (Figure 1A). However, there was no statistically significant difference in the median platelet counts between the cfhR/R mice (662 × 109/L) and the Adamts13−/−cfhR/R mice (553 × 109/L) (Figure 1A). Peripheral blood smears with Wright-Giemsa stain showed the presence of fragmented red blood cells (or schistocytes) in Adamts13−/−cfhW/R, cfhR/R, and Adamts13−/−cfhR/R mice (Figure 1B), but not in any wt control mice or in those carrying Adamts13−/− or cfhW/R (not shown). These results demonstrate that mice with either cfhW/R or Adamts13−/− alone remain asymptomatic, but mice with Adamts13−/−cfhW/R , cfhR/R, or Adamts13−/−cfhR/R develop symptomatic and laboratory-confirmed TMA.
Figure 1.
Platelet counts and schistocytes in theperipheral blood smear from mice with various genotypes. (A) Platelet counts in mice with various genotypes are shown as the dots in the box-whisker plots. Each dot represents the platelet count of an individual mouse. The box spans the interquartile range. The top and bottom lines outside of the box represent the maximal and minimal values, respectively. The Mann-Whitney U test was performed to compare the difference of platelet counts in wt or Adamts13−/− with each of the other experimental groups. **P < .01 and ***P < .005, respectively. The number (n =) of mice with each genotype is shown below the graph. (B) Blood smear reveals the red blood cell morphology. The arrow indicates the fragmentated red blood cells (or schistocytes) in the background of other red blood cells from Adamts13−/−cfhW/R at the age of 42 days and Adamts13−/−cfhR/R at the age of 16 days. Wright-Giemsa stain; original magnification ×200.
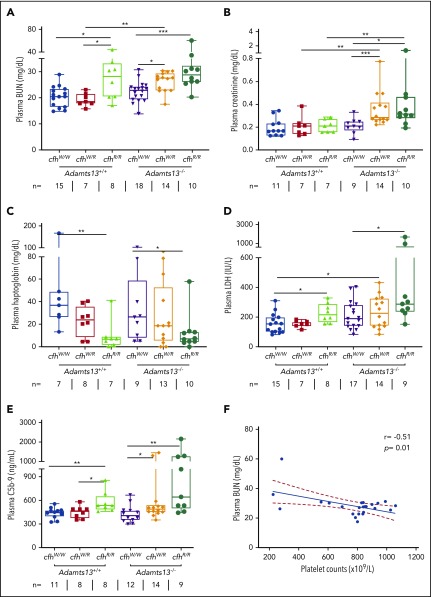
Plasma levels of BUN, creatinine, and LDH in mice with various genotypes
To assess the potential organ damage resulting from TMA, we determined plasma levels of blood urea nitrogen (BUN), creatinine, and LDH in mice with various genotypes at the age of ∼2.5 months (or 10 weeks). As shown, the median levels of plasma BUN increased significantly in mice with Adamts13−/−cfhW/R (27.5 mg/dL), cfhR/R (28.2 mg/dL), and Adamts13−/−cfhR/R (28.9 mg/dL) when compared with the levels in wt mice (20.5 mg/dL) or in those carrying Adamts13−/− alone (23.0 mg/dL) (Figure 2A). Interestingly, the median levels of plasma creatinine were only significantly elevated in mice with Adamts13−/−cfhW/R (0.28 mg/dL) and Adamts13−/−cfhR/R (0.31 mg/dL), but not in those with any other genotype (Figure 2B). There was a statistically significant correlation between platelet counts and plasma BUN levels in mice with Adamts13−/−cfhW/R or Adamts13−/−cfhR/R mice (P = .01) (Figure 2F). However, no correlation between platelet counts and plasma creatinine levels was detected in mice with any genotype (not shown). These results suggest that plasma BUN levels may be a more sensitive and reliable marker for assessing the overall renal functions in mice, consistent with results reported previously.29
Figure 2.
Plasma BUN, creatinine, haptoglobin, and LDH in mice with various genotypes. Box-whisker and dot plots show the median, interquartile, minimum to maximum, and each individual value of plasma BUN (A), creatinine (B), haptoglobin (C), and LDH (D), as well as sC5b-9 (E) in mice at the age of 2 to 3 months with various genotypes. The Mann-Whitney U test was performed to compare the difference in each biomarker between the wt or Adamts13−/− and each of the other experimental groups. (E) A negative correlation was detected between BUN and sC5b-9 in plasma of Adamts13−/−cfhW/R and Adamts13−/−cfhR/R mice. *P < .05, **P < .01, and ***P < .001, respectively. The number of mice (n =) from each genotype tested is shown under each graph. (F) Pearson correlation coefficient (r = −0.51, P = .01) between platelet counts and plasma BUN levels was determined using Prism 7 software.
To assess the degree of hemolysis, we determined the plasma levels of haptoglobin, which binds free hemoglobin and results in accelerated clearance from circulation during hemolysis.49-51 As shown, the median plasma haptoglobin levels in mice with cfhR/R (6.9 mg/dL; P = .007) or Adamts13−/−cfhR/R (7.2 mg/dL; P = .03) were significantly lower than those in wt (36.9 mg/dL) or Adamts13−/− (26.5 mg/dL). However, there was no statistically significant difference in the median haptoglobin levels between the cfhR/R mice and the Adamts13−/−cfhR/R mice or between the cfhW/R and Adamts13−/−cfhW/R groups (Figure 2C). These results suggest that complement overactivation may be the primary driving force causing hemolysis.
To assess the degree of overall organ damage, plasma levels of LDH were also determined. High LDH is predictive for more severe disease52 and a higher mortality rate in patients with TTP.53 As shown, there was a significant increase in the median plasma levels of LDH in mice with cfhR/R (216.6 U/L; P = .02), Adamts13−/−cfhW/R (229.2 U/L; P = .04), and Adamts13−/−cfhR/R (283.3 U/L; P = .001) when compared with those in wt mice (153.1 U/L). The highest plasma levels of LDH were detected in mice with Adamts13−/−cfhR/R (Figure 2D). These results indicate that the most severe organ damage occurs in mice with a combined abnormality (ie, severe ADAMTS13 deficiency and a homozygous mutation in cfh).
To assess the status of complement activation in vivo, plasma levels of the soluble terminal complement complex (sC5b-9) were determined in mice with various genotypes. Serum or plasma sC5-9 has been shown to be a reliable marker of complement activation in patients with aHUS54,55 and TTP.36,53,56 The median plasma levels of sC5b-9 in cfhR/R mice (536.6 ng/mL) were significantly higher than those in cfhW/R (461.5 ng/mL; P = .03) or cfhW/W (449.4 ng/mL; P = .005) mice. Moreover, the median plasma levels of sC5b-9 in mice with Adamts13−/−cfhW/R (491.4 ng/mL; P = .04) or Adamts13−/−cfhR/R (644.0 ng/mL; P = .003) were also significantly higher than those in Adamts13−/− mice (406.9 ng/mL). These results suggest that there is more complement activation in mice with a combined abnormality (a mutation in cfh and Adamts13−/−) than in those with a mutation in either cfh or Adamts13 alone.
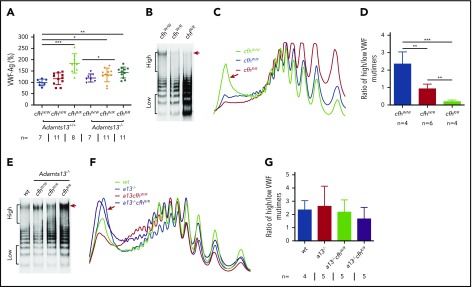
Plasma VWF antigen and multimers in mice with various genotypes
VWF plays an essential role in pathogenesis of TTP.2,6,57 However, the role of VWF in pathogenesis of aHUS is less well understood.4 Our results showed that plasma levels of VWF antigen (the mean ± SD) were dramatically increased in mice with cfhR/R (183.7% ± 42.4%; P = .0003), Adamts13−/−cfhW/R (132.7% ± 30.4%; P = .02), and Adamts13−/−cfhR/R (143.5% ± 24.1%; P = .0019) compared with those in wt mice (99.5% ± 14.5%) (Figure 3A). No significant difference in plasma VWF antigen levels was detected between Adamts13−/− and wt groups. Interestingly, plasma VWF multimer analysis revealed that the increase of plasma VWF antigen in the cfhR/R mice was primarily attributed by the increase of small to medium sizes of VWF multimers. Few or no ULVWF multimers were detected in mice with cfhW/R or cfhR/R when normal plasma ADAMTS13 activity was present (Figure 3B-D). This may be due to the increase in degradation, proteolysis, or consumption of ULVWF in the ongoing thrombosis. In the absence of ADAMTS13 activity, however, the newly released ULVWF may remain anchored on the endothelial surface. However, there was no significant change in the ratio of high- to low-molecular-weight VWF multimers in mice with Adamts13−/−cfhW/R or Adamts13−/−cfhR/R compared with that in Adamts13−/− or wt mice (Figure 3E-G). These results indicate that there may be cross talk between ADAMTS13, VWF, and complement activation that regulates endothelial function and thrombus formation.
Figure 3.
Plasma VWF antigen and multimer distribution in mice with various genotypes. (A) Plasma levels of VWF antigen in mice with various genotypes. Dots and horizontal lines represent the individual, the mean values, and ± SD. The Mann-Whitney U test was performed to compare the difference of VWF antigen between the wt or Adamts13−/− mice with each of the other experimental groups. Representative images of (B,E) VWF multimers, (C,F) densitometric scanning, and (D,G) the ratios of high to low molecular VWF forms, respectively, in mice with various genotypes. The data in panels D and G are the mean ± SD. Mann-Whitney U analysis was performed to determine the statistical significance among various groups. *P < .05, **P < .01, and ***P < .005, respectively.
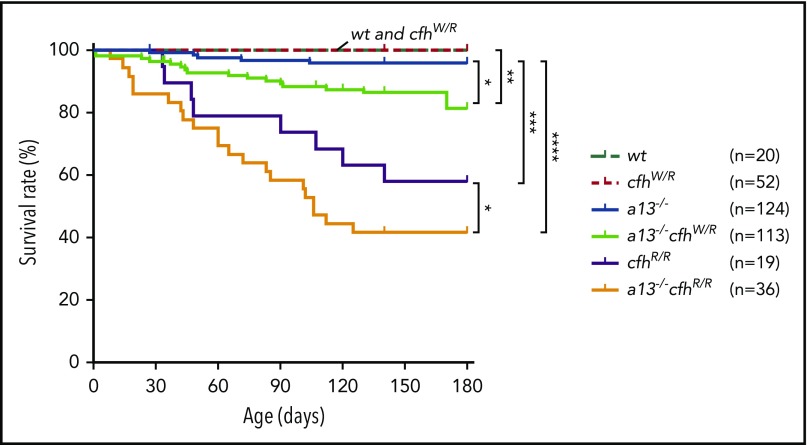
Kaplan-Meier survival analysis in mice with various genotypes
Mice carrying Adamts13−/− or cfhW/R alone were viable, fertile, and largely asymptomatic. There was a small increase in the mortality rate in Adamts13−/− mice (4%) compared with wt (0%) or cfhW/R (0%) mice. However, the mortality rate in mice with Adamts13−/−cfhW/R (14.2%) was significantly higher than that in mice with Adamts13−/− or cfhW/R alone. Likewise, the mortality rate in mice with Adamts13−/−cfhR/R (58.3%) was dramatically increased compared with that in mice with Adamts13−/− (4%) or cfhR/R (42.1%) alone (Figure 4). These results suggest that individuals carrying either cfhW/R or cfhR/R on top of severe ADAMTS13 deficiency may have significantly higher mortality rates than those carrying a single gene mutation. This is at least the case in mice.
Figure 4.
Kaplan-Meier survival analysis of mice with various genotypes. The mortality rate (percentage) was determined for 6 months in mice with various genotypes. The log-rank (Mantel-Cox) test was used to compare the difference in the mortality rate between the control group (wt or cfhW/R) and each of other genotypes. *P < .05, **P < .01, ***P < .005, and ****P < .0001, respectively. a13−/−, Adamts13−/−; cfhW/R and cfhR/R are the heterozygous and homozygous mutations, respectively.
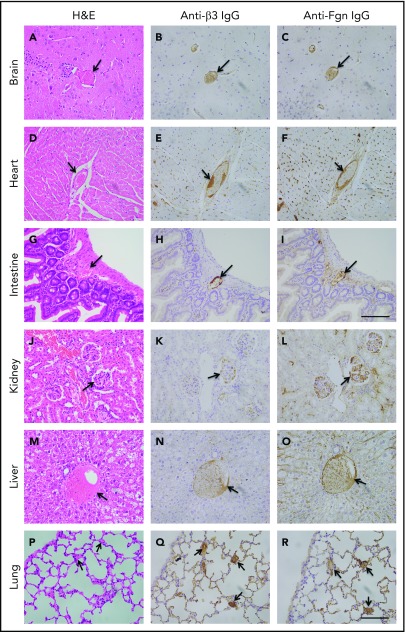
Histology and immunohistochemical analysis of major tissues in mice with various genotypes
To determine the extent of microvascular thromboses and thrombus compositions, we performed H&E histology analysis and immunohistochemistry on tissue sections from brain, heart, lung, liver, and kidney, etc. As shown, the occlusive microvascular thrombi stained with H&E (Figure 5, left column) and antibodies against platelet integrin β3 (Figure 5, middle column) or fibrinogen (Figure 5, right column) were present in all tissues examined except for spleen obtained from mice with Adamts13−/−cfhW/R (Figure 5) but more prominent in the tissues from mice with cfhR/R or Adamts13−/−cfhR/R (not shown). Occasional microvascular thrombi (1-2 thrombi per 10 high-power fields) were also detected in the brain, heart, kidney, and intestine in the asymptomatic mice (n = 3) with Adatms13−/− or cfhW/R alone (not shown). No occlusive thrombus was detected in any organ tissue in the wt mice. All control slides without the primary antibody were stained negative. These results suggest that silent thrombi may occur in the asymptomatic mice carrying Adamts13−/− or cfhW/R, but disseminated occlusive thrombi are only present in mice with Adamts13−/−cfhW/R, cfhR/R, and Adamts13−/−cfhR/R, which is confirmatory for TMA in these mice.
Figure 5.
Histology and immunohistochemical analysis of microvascular thrombosis in mouse tissues. Representative images of major organ tissues from Adamts13−/−cfhW/R at the age of 3 months being euthanized, including brain (A-C), heart (D-F), intestine (G-I), kidney (J-L), liver (M-O), and lung (P-R), stained with H&E (left column), anti-β3 IgG (middle column), and anti-fibrinogen (Fgn) IgG (right column) as described in “Methods.” Arrow indicates the presence of occlusive and platelet-rich microvascular thrombus. Scale bar, 100 μm.
Discussion
The present study demonstrates a potential synergistic role of severe ADAMTS13 deficiency and overactivation of complement system in a murine model of TMA. As we and others have previously reported, mice with only cfhW/R (Ueda et al29) or Adamts13−/− (Motto et al42 and Jin et al48) are asymptomatic with no thrombocytopenia or elevated LDH except for occasional thrombi on tissue examination. However, mice with cfhR/R or Adamts13−/−cfhW/R develop symtomatic TMA, indicated by low platelet counts, low haptoglobin, increased fragmentation of red blood cells, and increased LDH, BUN, and creatinine. Disseminated microvascular thrombi are present in nearly all organ tissues in these mice, further confirming the diagnosis. Moreover, mice with Adamts13−/−cfhW/R or Adamts13−/−cfhR/R have an increased mortality rate when compared with those carrying cfhW/R or cfhR/R or Adamts13−/− alone. Together, these results demonstrate a potential synergistic, albeit detrimental, effect of severe ADAMTS13 deficiency and heightened complement activation in the onset, progression, and outcome of TMA in mice.
TTP/HUS was historically considered to be 1 complicated syndrome.58,59 With the discovery of ADAMTS13,7,60-62 TTP is now recognized as a distinct entity, primarily resulting from autoantibodies against ADAMTS13.8,49,53,63,64 An IgG-type autoantibody binds ADAMTS13 and inhibits its activity in >95% of TTP cases.8,30,49,65-68 Therapeutic plasma exchange (TPE) plus corticosteroids and rituximab has been the mainstay of treatment of such an immune-mediated TTP (iTTP).69,70 TPE is thought to remove autoantibodies while replenishing the missing or inhibited ADAMTS13 enzyme.8,71 The clinical course in each patient is quite different with some responding to therapy rapidly and completely while others respond to the therapy slowly and unevenly or not at all.72-74 However, the mortality rate in patients with iTTP remains as high as 10% to 20%.33,75 In those who survive the acute episode, ∼40% of patients may experience an exacerbation and/or relapses despite all proper therapeutics given.33,75,76 With the introduction of caplacizumab, an anti-VWF A1 nanobody, the exacerbation rate has significantly reduced during TPE and after the discontinuation of TPE.76,77 In any case, the heterogeneity in disease severity and responses to therapies suggest the presence of other disease modifiers in the pathogenesis of TTP.
Noris et al reported the presence of a heterozygous mutation in CFH (S890I) in a patient with congenital (cTTP) who has renal failure.78 Chapin et al also reported the presence of heterozygous mutations in CFH in 4 cases with ticlopidine-induced TTP in whom there was severe deficiency of plasma ADAMTS13 resulting from an autoantibody against ADAMTS13.79 More recently, studies have demonstrated that elevated serum or plasma markers of complement activation via an alternative pathway are prevalent in patients with both cTTP and iTTP.35-38,56,80,81 Conversely, some pediatric patients with aHUS were found to have a partial82 or even severe deficiency of plasma ADAMTS13 activity,83 although these patients with severe plasma ADAMTS13 deficiency in the absence of anti-ADAMTS13 IgG would have been diagnosed as cTTP rather than aHUS today.70,84 Together, these findings suggest that complement activation and partial or severe deficiency of plasma ADAMTS13 activity could coexist in patients with a clinical diagnosis of aHUS or TTP.
The associations between ADAMTS13, VWF, and complement components or regulators have been studied in vitro. Turner and Moake demonstrate that C3, CFB, CFD, C5, CFH, and CFI are able to attach to the newly released ULVWF strings on the endothelial surface in the amount required for assembly of the alternative pathway components into active complexes.85 Additionally, small VWF multimers are shown to act as a cofactor mediating the CFI-dependent degradation of C3b, thereby inhibiting complement activation, whereas ULVWF multimers do not have such an inhibitory activity toward complement activation, thus, they may promote complement activation.86 When ADAMTS13 is present, the newly released endothelial ULVWF multimers are rapidly and efficiently removed from the cell surface. This will not only reduce platelet adhesion and aggregation but also eliminate the complement component assembly and activation on the injured or activated endothelium. When ADAMTS13 is absent, endothelial ULVWF strings may serve as a template for assembling complement components, which leads to overactivation of complement in situ, resulting in endothelium damage and thrombus formation.
The interaction between CFH and VWF remains elusive. One report demonstrates that CFH may function as a disulfide reductase, which reduces the size of VWF multimers under shear.87 Other reports show that CFH may bind VWF and inhibit88 or enhance its proteolytic cleavage by ADAMTS13.89 Our own unpublished data are consistent with the latter under shear (W.C. and X.L.Z, unpublished results, 14 July 2019). Plasma ADAMTS13 activity in mice with cfhR/R increases by 50% as we previously reported.29 This may at least partially explain the reduction of VWF multimer size in mice with cfhR/R. However, a marked increase of plasma VWF antigen in these mice suggests complement-mediated activation and damage to vascular endothelium. The degree of endothelial injury may be more severe in mice with Adamts13−/−cfhR/R than with cfhR/R based on the increased levels of plasma sC5b-9 and the increased mortality rate in the double mutant mice, despite lower plasma VWF antigen concentrations in these mice. Without a functional ADAMTS13, the released ULVWF in Adamts13−/−cfhR/R mice may remain anchored on the endothelial surface, which promotes activation of complement components and thrombus formation. We conclude that severe deficiency of plasma ADAMTS13 activity and heightened activation of the complement system may play a synergistic, albeit detrimental, role in the onset, progression, and outcomes of TMA in mice.
Acknowledgments
The authors thank David Ginsburg for providing us with Adamts13−/− mice and Dezhi (Annie) Wang at the Core Research Laboratory, Department of Pathology, University of Alabama at Birmingham (Birmingham, AL) for technical support in performing histology and immunohistochemistry. The authors appreciate the gift of mouse anti-human GPIIb/IIIa antibodies from Heyu Ni at the University of Toronto (Toronto, ON, Canada). The authors thank Nicole K. Kocher at the Department of Pathology, University of Alabama at Birmingham for proofreading the manuscript.
This work was partially supported by grants from the National Institutes of Health, National Heart, Lung, and Blood Institute (HL126724) (X.L.Z.), the Answering TTP Foundation (X.L.Z.), and the postdoctoral fellowship grant (18POST33960098) from the American Heart Association (L.Z.).
Footnotes
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: L.Z. and X.L.Z. designed research, performed experiments, analyzed the results, and wrote the manuscript; D.Z, and W.C. performed some experiments and analyzed the data; W.-C.S. provided critical reagents; and all authors reviewed and approved the final version of the manuscript.
Conflict-of-interest disclosure: X.L.Z. is a speaker for Alexion, is a consultant/speaker for Sanofi, is the founder of Clotsolution, and received research support from Takeda for a clinical trial using recombinant ADAMTS13. The remaining authors declare no competing financial interests.
Correspondence: X. Long Zheng, Division of Laboratory Medicine, Department of Pathology, The University of Alabama at Birmingham, 619 19th St S, Birmingham, AL 35243; e-mail: xzheng@uabmc.edu.
REFERENCES
- 1.Zheng XL, Sadler JE. Pathogenesis of thrombotic microangiopathies. Annu Rev Pathol. 2008;3:249-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moake JL. Thrombotic thrombocytopenic purpura: the systemic clumping “plague”. Annu Rev Med. 2002;53:75-88. [DOI] [PubMed] [Google Scholar]
- 3.Lämmle B, Kremer Hovinga JA, Alberio L. Thrombotic thrombocytopenic purpura. J Thromb Haemost. 2005;3(8):1663-1675. [DOI] [PubMed] [Google Scholar]
- 4.Noris M, Mescia F, Remuzzi G. STEC-HUS, atypical HUS and TTP are all diseases of complement activation. Nat Rev Nephrol. 2012;8(11):622-633. [DOI] [PubMed] [Google Scholar]
- 5.Espié E, Grimont F, Mariani-Kurkdjian P, et al. Surveillance of hemolytic uremic syndrome in children less than 15 years of age, a system to monitor O157 and non-O157 Shiga toxin-producing Escherichia coli infections in France, 1996-2006. Pediatr Infect Dis J. 2008;27(7):595-601. [DOI] [PubMed] [Google Scholar]
- 6.Zheng XL. ADAMTS13 and von Willebrand factor in thrombotic thrombocytopenic purpura. Annu Rev Med. 2015;66:211-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levy GG, Nichols WC, Lian EC, et al. Mutations in a member of the ADAMTS gene family cause thrombotic thrombocytopenic purpura. Nature. 2001;413(6855):488-494. [DOI] [PubMed] [Google Scholar]
- 8.Tsai HM, Lian EC. Antibodies to von Willebrand factor-cleaving protease in acute thrombotic thrombocytopenic purpura. N Engl J Med. 1998;339(22):1585-1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Furlan M, Robles R, Galbusera M, et al. von Willebrand factor-cleaving protease in thrombotic thrombocytopenic purpura and the hemolytic-uremic syndrome. N Engl J Med. 1998;339(22):1578-1584. [DOI] [PubMed] [Google Scholar]
- 10.Afshar-Kharghan V. Atypical hemolytic uremic syndrome. Hematology Am Soc Hematol Educ Program. 2016;2016:217-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kavanagh D, Goodship TH, Richards A. Atypical hemolytic uremic syndrome. Semin Nephrol. 2013;33(6):508-530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scheiring J, Andreoli SP, Zimmerhackl LB. Treatment and outcome of Shiga-toxin-associated hemolytic uremic syndrome (HUS). Pediatr Nephrol. 2008;23(10):1749-1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ake JA, Jelacic S, Ciol MA, et al. Relative nephroprotection during Escherichia coli O157:H7 infections: association with intravenous volume expansion. Pediatrics. 2005;115(6):e673-e680. [DOI] [PubMed] [Google Scholar]
- 14.Liu F, Huang J, Sadler JE. Shiga toxin (Stx)1B and Stx2B induce von Willebrand factor secretion from human umbilical vein endothelial cells through different signaling pathways. Blood. 2011;118(12):3392-3398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keir LS, Marks SD, Kim JJ. Shigatoxin-associated hemolytic uremic syndrome: current molecular mechanisms and future therapies. Drug Des Devel Ther. 2012;6:195-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang J, Motto DG, Bundle DR, Sadler JE. Shiga toxin B subunits induce VWF secretion by human endothelial cells and thrombotic microangiopathy in ADAMTS13-deficient mice. Blood. 2010;116(18):3653-3659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bresin E, Rurali E, Caprioli J, et al. ; European Working Party on Complement Genetics in Renal Diseases . Combined complement gene mutations in atypical hemolytic uremic syndrome influence clinical phenotype. J Am Soc Nephrol. 2013;24(3):475-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fremeaux-Bacchi V, Fakhouri F, Garnier A, et al. Genetics and outcome of atypical hemolytic uremic syndrome: a nationwide French series comparing children and adults. Clin J Am Soc Nephrol. 2013;8(4):554-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bienaime F, Dragon-Durey MA, Regnier CH, et al. Mutations in components of complement influence the outcome of factor I-associated atypical hemolytic uremic syndrome. Kidney Int. 2010;77(4):339-349. [DOI] [PubMed] [Google Scholar]
- 20.Provaznikova D, Rittich S, Malina M, et al. Manifestation of atypical hemolytic uremic syndrome caused by novel mutations in MCP. Pediatr Nephrol. 2012;27(1):73-81. [DOI] [PubMed] [Google Scholar]
- 21.Fremeaux-Bacchi V, Moulton EA, Kavanagh D, et al. Genetic and functional analyses of membrane cofactor protein (CD46) mutations in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2006;17(7):2017-2025. [DOI] [PubMed] [Google Scholar]
- 22.Delvaeye M, Noris M, De Vriese A, et al. Thrombomodulin mutations in atypical hemolytic-uremic syndrome. N Engl J Med. 2009;361(4):345-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sartz L, Olin AI, Kristoffersson AC, et al. A novel C3 mutation causing increased formation of the C3 convertase in familial atypical hemolytic uremic syndrome. J Immunol. 2012;188(4):2030-2037. [DOI] [PubMed] [Google Scholar]
- 24.Frémeaux-Bacchi V, Miller EC, Liszewski MK, et al. Mutations in complement C3 predispose to development of atypical hemolytic uremic syndrome. Blood. 2008;112(13):4948-4952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goicoechea de Jorge E, Harris CL, Esparza-Gordillo J, et al. Gain-of-function mutations in complement factor B are associated with atypical hemolytic uremic syndrome [published correction appears in Proc Natl Acad Sci USA. 2007;104(25):10749]. Proc Natl Acad Sci USA. 2007;104(1):240-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Funato M, Uemura O, Ushijima K, et al. A complement factor B mutation in a large kindred with atypical hemolytic uremic syndrome. J Clin Immunol. 2014;34(6):691-695. [DOI] [PubMed] [Google Scholar]
- 27.Kavanagh D, Richards A, Atkinson J. Complement regulatory genes and hemolytic uremic syndromes. Annu Rev Med. 2008;59:293-309. [DOI] [PubMed] [Google Scholar]
- 28.Loirat C, Frémeaux-Bacchi V. Atypical hemolytic uremic syndrome. Orphanet J Rare Dis. 2011;6:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ueda Y, Mohammed I, Song D, et al. Murine systemic thrombophilia and hemolytic uremic syndrome from a factor H point mutation. Blood. 2017;129(9):1184-1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zheng XL, Wu HM, Shang D, et al. Multiple domains of ADAMTS13 are targeted by autoantibodies against ADAMTS13 in patients with acquired idiopathic thrombotic thrombocytopenic purpura. Haematologica. 2010;95(9):1555-1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Dorland HA, Mansouri Taleghani M, Sakai K, et al. ; Hereditary TTP Registry . The International Hereditary Thrombotic Thrombocytopenic Purpura Registry: key findings at enrolment until 2017 [published online ahead of print 21 February 2019]. Haematologica. doi:10.3324/haematol.2019.216796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fujimura Y, Kokame K, Yagi H, et al. Hereditary deficiency of ADAMTS13 activity: Upshaw-Schulman syndrome In: Rodgers GM, ed. ADAMTS13 Biology and Disease, Cham, Switzerland: Springer; 2015:73-90. [Google Scholar]
- 33.Staley EM, Cao WJ, Pham HP, et al. Clinical factors and biomarkers predict outcome in patients with immune-mediated thrombotic thrombocytopenic purpura. Haematologica. 2019;104(1):166-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fuchs TA, Kremer Hovinga JA, Schatzberg D, Wagner DD, Lämmle B. Circulating DNA and myeloperoxidase indicate disease activity in patients with thrombotic microangiopathies. Blood. 2012;120(6):1157-1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cao W, Pham HP, Williams LA, et al. Human neutrophil peptides and complement factor Bb in pathogenesis of acquired thrombotic thrombocytopenic purpura. Haematologica. 2016;101(11):1319-1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tati R, Kristoffersson AC, Ståhl AL, et al. Complement activation associated with ADAMTS13 deficiency in human and murine thrombotic microangiopathy. J Immunol. 2013;191(5):2184-2193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Réti M, Farkas P, Csuka D, et al. Complement activation in thrombotic thrombocytopenic purpura. J Thromb Haemost. 2012;10(5):791-798. [DOI] [PubMed] [Google Scholar]
- 38.Westwood JP, Langley K, Heelas E, Machin SJ, Scully M. Complement and cytokine response in acute thrombotic thrombocytopenic purpura. Br J Haematol. 2014;164(6):858-866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vigna E, Petrungaro A, Perri A, et al. Efficacy of eculizumab in severe ADAMTS13-deficient thrombotic thrombocytopenic purpura (TTP) refractory to standard therapies. Transfus Apheresis Sci. 2018;57(2):247-249. [DOI] [PubMed] [Google Scholar]
- 40.Pecoraro C, Ferretti AV, Rurali E, Galbusera M, Noris M, Remuzzi G. Treatment of congenital thrombotic thrombocytopenic purpura with eculizumab. Am J Kidney Dis. 2015;66(6):1067-1070. [DOI] [PubMed] [Google Scholar]
- 41.Tsai E, Chapin J, Laurence JC, Tsai HM. Use of eculizumab in the treatment of a case of refractory, ADAMTS13-deficient thrombotic thrombocytopenic purpura: additional data and clinical follow-up. Br J Haematol. 2013;162(4):558-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Motto DG, Chauhan AK, Zhu G, et al. Shigatoxin triggers thrombotic thrombocytopenic purpura in genetically susceptible ADAMTS13-deficient mice. J Clin Invest. 2005;115(10):2752-2761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pickens B, Mao Y, Li D, et al. Platelet-delivered ADAMTS13 inhibits arterial thrombosis and prevents thrombotic thrombocytopenic purpura in murine models. Blood. 2015;125(21):3326-3334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Murphy S, Dowling P, Zweyer M, et al. Proteomic profiling of mdx-4cv serum reveals highly elevated levels of the inflammation-induced plasma marker haptoglobin in muscular dystrophy. Int J Mol Med. 2017;39(6):1357-1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Drotningsvik A, Midttun Ø, McCann A, Ueland PM, Høgøy I, Gudbrandsen OA. Dietary intake of cod protein beneficially affects concentrations of urinary markers of kidney function and results in lower urinary loss of amino acids in obese Zucker fa/fa rats. Br J Nutr. 2018;120(7):740-750. [DOI] [PubMed] [Google Scholar]
- 46.Holmgren G, Synnergren J, Bogestål Y, et al. Identification of novel biomarkers for doxorubicin-induced toxicity in human cardiomyocytes derived from pluripotent stem cells. Toxicology. 2015;328:102-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xiao J, Jin SY, Xue J, Sorvillo N, Voorberg J, Zheng XL. Essential domains of a disintegrin and metalloprotease with thrombospondin type 1 repeats-13 metalloprotease required for modulation of arterial thrombosis. Arterioscler Thromb Vasc Biol. 2011;31(10):2261-2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jin SY, Xiao J, Bao J, et al. AAV-mediated expression of an ADAMTS13 variant prevents shigatoxin-induced thrombotic thrombocytopenic purpura. Blood. 2013;121(19):3825-3829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Casina VC, Hu W, Mao JH, et al. High-resolution epitope mapping by HX MS reveals the pathogenic mechanism and a possible therapy for autoimmune TTP syndrome. Proc Natl Acad Sci USA. 2015;112(31):9620-9625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thielemans L, Layton DM, Shovlin CL. Low serum haptoglobin and blood films suggest intravascular hemolysis contributes to severe anemia in hereditary hemorrhagic telangiectasia. Haematologica. 2019;104(4):e127-e130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Anderton R. Hemolysis and haptoglobin levels [letter]. N Engl J Med. 1971;284(18):1044. [DOI] [PubMed] [Google Scholar]
- 52.Benhamou Y, Assié C, Boelle PY, et al. ; Thrombotic Microangiopathies Reference Center . Development and validation of a predictive model for death in acquired severe ADAMTS13 deficiency-associated idiopathic thrombotic thrombocytopenic purpura: the French TMA Reference Center experience. Haematologica. 2012;97(8):1181-1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Staley EM, Cao W, Pham HP, et al. Clinical factors and biomarkers predict outcome in patients with immune-mediated thrombotic thrombocytopenic purpura. Haematologica. 2019;104(1):166-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Prüfer F, Scheiring J, Sautter S, et al. Terminal complement complex (C5b-9) in children with recurrent hemolytic uremic syndrome. Semin Thromb Hemost. 2006;32(2):121-127. [DOI] [PubMed] [Google Scholar]
- 55.Riedl M, Hofer J, Giner T, et al. Novel biomarker and easy to perform ELISA for monitoring complement inhibition in patients with atypical hemolytic uremic syndrome treated with eculizumab. J Immunol Methods. 2016;435:60-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cataland SR, Holers VM, Geyer S, Yang S, Wu HM. Biomarkers of terminal complement activation confirm the diagnosis of aHUS and differentiate aHUS from TTP. Blood. 2014;123(24):3733-3738. [DOI] [PubMed] [Google Scholar]
- 57.Moake JL, Rudy CK, Troll JH, et al. Unusually large plasma factor VIII:von Willebrand factor multimers in chronic relapsing thrombotic thrombocytopenic purpura. N Engl J Med. 1982;307(23):1432-1435. [DOI] [PubMed] [Google Scholar]
- 58.Dervenoulas J, Tsirigotis P, Bollas G, et al. Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome (TTP/HUS): treatment outcome, relapses, prognostic factors. A single-center experience of 48 cases. Ann Hematol. 2000;79(2):66-72. [DOI] [PubMed] [Google Scholar]
- 59.Kakishita E. Pathophysiology and treatment of thrombotic thrombocytopenic purpura/hemolytic uremic syndrome (TTP/HUS). Int J Hematol. 2000;71(4):320-327. [PubMed] [Google Scholar]
- 60.Zheng X, Chung D, Takayama TK, Majerus EM, Sadler JE, Fujikawa K. Structure of von Willebrand factor-cleaving protease (ADAMTS13), a metalloprotease involved in thrombotic thrombocytopenic purpura. J Biol Chem. 2001;276(44):41059-41063. [DOI] [PubMed] [Google Scholar]
- 61.Gerritsen HE, Robles R, Lämmle B, Furlan M. Partial amino acid sequence of purified von Willebrand factor-cleaving protease. Blood. 2001;98(6):1654-1661. [DOI] [PubMed] [Google Scholar]
- 62.Plaimauer B, Zimmermann K, Völkel D, et al. Cloning, expression, and functional characterization of the von Willebrand factor-cleaving protease (ADAMTS13). Blood. 2002;100(10):3626-3632. [DOI] [PubMed] [Google Scholar]
- 63.Rieger M, Mannucci PM, Kremer Hovinga JA, et al. ADAMTS13 autoantibodies in patients with thrombotic microangiopathies and other immunomediated diseases. Blood. 2005;106(4):1262-1267. [DOI] [PubMed] [Google Scholar]
- 64.Furlan M, Robles R, Solenthaler M, Lämmle B. Acquired deficiency of von Willebrand factor-cleaving protease in a patient with thrombotic thrombocytopenic purpura. Blood. 1998;91(8):2839-2846. [PubMed] [Google Scholar]
- 65.Pos W, Crawley JT, Fijnheer R, Voorberg J, Lane DA, Luken BM. An autoantibody epitope comprising residues R660, Y661, and Y665 in the ADAMTS13 spacer domain identifies a binding site for the A2 domain of VWF. Blood. 2010;115(8):1640-1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Luken BM, Kaijen PH, Turenhout EA, et al. Multiple B-cell clones producing antibodies directed to the spacer and disintegrin/thrombospondin type-1 repeat 1 (TSP1) of ADAMTS13 in a patient with acquired thrombotic thrombocytopenic purpura. J Thromb Haemost. 2006;4(11):2355-2364. [DOI] [PubMed] [Google Scholar]
- 67.Luken BM, Turenhout EA, Kaijen PH, et al. Amino acid regions 572-579 and 657-666 of the spacer domain of ADAMTS13 provide a common antigenic core required for binding of antibodies in patients with acquired TTP. Thromb Haemost. 2006;96(3):295-301. [DOI] [PubMed] [Google Scholar]
- 68.Luken BM, Turenhout EA, Hulstein JJ, Van Mourik JA, Fijnheer R, Voorberg J. The spacer domain of ADAMTS13 contains a major binding site for antibodies in patients with thrombotic thrombocytopenic purpura. Thromb Haemost. 2005;93(2):267-274. [DOI] [PubMed] [Google Scholar]
- 69.Crawley JT, Scully MA. Thrombotic thrombocytopenic purpura: basic pathophysiology and therapeutic strategies. Hematology Am Soc Hematol Educ Program. 2013;2013:292-299. [DOI] [PubMed] [Google Scholar]
- 70.Saha M, McDaniel JK, Zheng XL. Thrombotic thrombocytopenic purpura: pathogenesis, diagnosis and potential novel therapeutics. J Thromb Haemost. 2017;15(10):1889-1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rock GA, Shumak KH, Buskard NA, et al. ; Canadian Apheresis Study Group . Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. N Engl J Med. 1991;325(6):393-397. [DOI] [PubMed] [Google Scholar]
- 72.Zheng XL, Kaufman RM, Goodnough LT, Sadler JE. Effect of plasma exchange on plasma ADAMTS13 metalloprotease activity, inhibitor level, and clinical outcome in patients with idiopathic and nonidiopathic thrombotic thrombocytopenic purpura. Blood. 2004;103(11):4043-4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bell WR, Braine HG, Ness PM, Kickler TS. Improved survival in thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Clinical experience in 108 patients. N Engl J Med. 1991;325(6):398-403. [DOI] [PubMed] [Google Scholar]
- 74.Clark WF, Rock GA, Buskard N, et al. Therapeutic plasma exchange: an update from the Canadian Apheresis Group. Ann Intern Med. 1999;131(6):453-462. [DOI] [PubMed] [Google Scholar]
- 75.Kremer Hovinga JA, Vesely SK, Terrell DR, Lämmle B, George JN. Survival and relapse in patients with thrombotic thrombocytopenic purpura. Blood. 2010;115(8):1500-1511, quiz 1662. [DOI] [PubMed] [Google Scholar]
- 76.Peyvandi F, Scully M, Kremer Hovinga JA, et al. Caplacizumab reduces the frequency of major thromboembolic events, exacerbations and death in patients with acquired thrombotic thrombocytopenic purpura. J Thromb Haemost. 2017;15(7):1448-1452. [DOI] [PubMed] [Google Scholar]
- 77.Peyvandi F, Scully M, Kremer Hovinga JA, et al. ; TITAN Investigators . Caplacizumab for acquired thrombotic thrombocytopenic purpura. N Engl J Med. 2016;374(6):511-522. [DOI] [PubMed] [Google Scholar]
- 78.Noris M, Bucchioni S, Galbusera M, et al. ; International Registry of Recurrent and Familial HUS/TTP . Complement factor H mutation in familial thrombotic thrombocytopenic purpura with ADAMTS13 deficiency and renal involvement. J Am Soc Nephrol. 2005;16(5):1177-1183. [DOI] [PubMed] [Google Scholar]
- 79.Chapin J, Eyler S, Smith R, Tsai HM, Laurence J. Complement factor H mutations are present in ADAMTS13-deficient, ticlopidine-associated thrombotic microangiopathies. Blood. 2013;121(19):4012-4013. [DOI] [PubMed] [Google Scholar]
- 80.Itami H, Hara S, Matsumoto M, et al. Complement activation associated with ADAMTS13 deficiency may contribute to the characteristic glomerular manifestations in Upshaw-Schulman syndrome. Thromb Res. 2018;170:148-155. [DOI] [PubMed] [Google Scholar]
- 81.Hu XH, Bao J, Ueda Y, et al. Complement activation may trigger the onset of thrombotic thrombocytopenic purpura in patients with severe ADAMTS13 deficiency [abstract]. Blood. 2014;124(21). Abstract 600. [Google Scholar]
- 82.Feng S, Eyler SJ, Zhang Y, et al. Partial ADAMTS13 deficiency in atypical hemolytic uremic syndrome. Blood. 2013;122(8):1487-1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Veyradier A, Obert B, Haddad E, et al. Severe deficiency of the specific von Willebrand factor-cleaving protease (ADAMTS 13) activity in a subgroup of children with atypical hemolytic uremic syndrome [published correction appears in J Pediatr. 2003;142(6):616]. J Pediatr. 2003;142(3):310-317. [DOI] [PubMed] [Google Scholar]
- 84.Scully M, Cataland S, Coppo P, et al. ; International Working Group for Thrombotic Thrombocytopenic Purpura . Consensus on the standardization of terminology in thrombotic thrombocytopenic purpura and related thrombotic microangiopathies. J Thromb Haemost. 2017;15(2):312-322. [DOI] [PubMed] [Google Scholar]
- 85.Turner NA, Moake J. Assembly and activation of alternative complement components on endothelial cell-anchored ultra-large von Willebrand factor links complement and hemostasis-thrombosis. PLoS One. 2013;8(3):e59372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Feng S, Liang X, Kroll MH, Chung DW, Afshar-Kharghan V. von Willebrand factor is a cofactor in complement regulation. Blood. 2015;125(6):1034-1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nolasco L, Nolasco J, Feng S, Afshar-Kharghan V, Moake J. Human complement factor H is a reductase for large soluble von Willebrand factor multimers--brief report. Arterioscler Thromb Vasc Biol. 2013;33(11):2524-2528. [DOI] [PubMed] [Google Scholar]
- 88.Rayes J, Roumenina LT, Dimitrov JD, et al. The interaction between factor H and VWF increases factor H cofactor activity and regulates VWF prothrombotic status. Blood. 2014;123(1):121-125. [DOI] [PubMed] [Google Scholar]
- 89.Feng S, Liang X, Cruz MA, et al. The interaction between factor H and von Willebrand factor. PLoS One. 2013;8(8):e73715. [DOI] [PMC free article] [PubMed] [Google Scholar]