Summary
Background
Screening and treatment for syphilis among pregnant women is the primary means of prevention of congenital syphilis. Sentinel surveillance for syphilis can inform these prevention efforts.
Methods
We reviewed antenatal syphilis screening results to assess trends and to identify correlates of seropositivity among women attending antenatal care clinics in the Democratic Republic of Congo during 2011.
Results
Syphilis seropositivity among the 17,669 women attending the antenatal care clinics during 2011 was 4.2% (range 0.4%−16.9%). Syphilis seropositivity was significantly higher among women attending rural clinics (5.0%) as compared to urban clinics (3.0%) and those tested in antenatal care clinics in the provinces of Equateur (7.6%) and Orientale (7.7%) as compared to other provinces (p < 0.001). Based on the ANC syphilis seroprevalence and national pregnancy estimates, we estimate that approximately 128,591 pregnant women countrywide would have tested seropositive for syphilis during 2011. Over 85,000 adverse pregnancy outcomes would have resulted from these maternal infections, assuming prenatal syphilis diagnosis and treatment were not available.
Conclusion
The prevalence of syphilis was highest in rural areas, but exceeded 1% in every area, indicating a need to assure screening and treatment throughout Democratic Republic of Congo. These sentinel surveillance estimates can be used to guide national congenital syphilis prevention efforts.
Keywords: Syphilis, congenital syphilis, antenatal care, Democratic Republic of Congo, STD, STI
Background
It is estimated that nearly 1.4 million women with syphilis become pregnant each year worldwide, and most go undiagnosed and untreated.1 Meanwhile, mother-to-child transmission of syphilis, i.e. congenital syphilis (CS), continues to account for more than 300,000 stillbirths and infant deaths globally per year despite prevention efforts.1,2 In 2007, the World Health Organization (WHO) launched the Initiative for the Global Elimination of Congenital Syphilis.3 The elimination of CS is considered a Global Winnable Battle by the Centers for Disease Control and Prevention (CDC)4 in tandem with the prevention of mother-to-child transmission of HIV (PMTCT). A primary component of these global initiatives is the integration of syphilis screening and treatment into basic antenatal health services.3,5 In order for countries to adequately address the burden of maternal syphilis, regional estimates of maternal syphilis seropositivity are needed.3,6
Syphilis seroprevalence in sub-Saharan Africa varies by and within countries and subpopulations.2 Within the Democratic Republic of Congo (DRC), wide ranges of syphilis seroprevalence have been recently reported among various groups: pregnant women (0–4%)7–10; internally displaced women (0.4–4%)11; blood donors (1.1–54%)12; HIV-infected persons (7%)13; child soldiers (3%)14; and female sex workers (12%).15 Syphilis screening is included along with HIV screening for pregnant women attending clinics participating in the national antenatal screening program.8 These antenatal care (ANC) screening data can be used to provide syphilis seropositivity estimates that better represent the general population and to guide CS prevention efforts.
Since 2005, the DRC Ministry of Health has conducted sentinel surveillance testing for syphilis and HIV among pregnant women receiving pre-natal care at ANC clinics supported by the collaborative resource contributions of the US government (USG) and other partners.8,16 Using this existing sentinel surveillance system, we reviewed antenatal syphilis screening results and correlates of positivity among women tested in 40 clinics participating in the national antenatal clinic surveillance program during 2011. We assessed trends in syphilis seropositivity among women who attended selected ANC clinics included in the antenatal clinic surveillance program during survey years 2005, 2007, 2009, and 2011.
Methods
ANC clinics
ANC clinics participating in the DRC national surveillance program must meet the inclusion criteria of providing care to a minimum of 400 women during a 4-week period.8,16 Because approximately 70% of the population in DRC is rural, selection of clinics is based on the same proportion of urban and rural sites in order to approach representativeness in ANC results. There are 11 provinces in DRC. One or more ANC clinics are located in each province. We conducted detailed analysis of the 2011 ANC survey and trend analysis using data from 23 clinics that participated in the survey years 2005, 2007, 2009, and 2011.
During 2011, six of the 40 survey clinics were located in a health center, while the remaining 34 were located in a general hospital. Of the 40 clinics, 14 were located in an urban setting as defined by the government of DRC as having an estimated population of greater than 100,000 persons. The remaining 26 of these clinics were located in a rural setting (estimated population <100,000). Data from clinics located in each province were combined to generate province-level seropositivity.
Participant enrollment and eligibility
During the 4 weeks of the yearly ANC surveillance survey, pregnant women presenting for ANC were automatically enrolled in the ANC surveillance protocol if they met the following criteria: (1) between the ages of 15 and 49, (2) pregnancy confirmed by a health care provider, (3) first visit to receive ANC for the current pregnancy and no prior syphilis test during the current pregnancy, (4) residence within the catchment area of the site, (5) not referred to the ANC clinic by another health facility during her current pregnancy. All women were asked for consent to receive syphilis testing prior to serum collection.8
Survey data collection
All pregnant women completed a nurse-administered in-person interview using a standard 14-question survey at the time of their first pre-natal and screening visit. The de-identified results of this survey for years 2005, 2007, 2009, and 2011 were entered and maintained by the Kinshasa School of Public Health (KSPH) in Kinshasa and shared with the Kinshasa-based CDC office with permission from the DRC National AIDS Program (PNLS). Demographic and risk variables include clinic site, trimester of first pre-natal visit for testing, age, age of father of current pregnancy, number of prior pregnancies, age of first pregnancy, age at first sexual encounter, age of first sexual partner, educational status, marital status, occupation, and rural or urban residence.
Syphilis testing
During the 4 weeks of the yearly ANC survey period, serum samples for syphilis and HIV screening were obtained at the first pre-natal visit from women who attended the 40 pre-natal clinics included in this analysis. Syphilis testing was performed using the Determine Syphilis® test (Alere, UK) followed by a rapid plasma regain (RPR) (Cypress Diagnostics) test for those women who tested positive. Women testing positive with both tests were counted as seropositive and were referred for treatment. Samples were analyzed in local laboratories that met the national selection criteria to process ANC specimens.
Pregnant population estimates and syphilis projections
Estimates of the number of pregnant women by DRC province were obtained from the National Reproductive Health Program 2011 Annual Report.17 Syphilis seroprevalence estimates by province were multiplied by the estimated pregnant population in each province to estimate the pregnant population that would have been seropositive for syphilis. Projected adverse pregnancy outcomes (APO) associated with untreated syphilis were calculated by multiplying recently published WHO percentage estimates of APO attributable to syphilis among seropositive women.18
Data analysis
Data were imported into SPSS (V18, Chicago, IL) and SAS (V 9.2, Cary, NC) for analysis. Correlates of seropositivity for data collected during 2011 were identified using Chi square tests. Routinely collected demographic and behavioral variables were used for the analysis. The stepwise procedure was the method utilized to obtain adjusted odds ratios and to find measures of association for further investigation. Data from the prior years 2005, 2007, 2009, and 2011 were analyzed for trend and association by rural or urban setting. Seropositivity data from 23 ANC clinics were graphed by year and rural/urban status using Microsoft Excel for years 2005, 2007, 2009, and 2011.
Results
Demographics
There were 17,669 women seen for primary ANC in the 40 clinics participating in the ANC sentinel surveillance program during 2011. The median age at time of testing visit was 25 years; median age at first pregnancy was 18 years; and the median number of pregnancies was three. Sixty percent of the participants resided in a rural area. The majority of women (92%) presented for initial pre-natal care during the second (43%) or third (49%) trimester. HIV seropositivity was 3.55% overall (Table 1).
Table 1.
Correlates of syphilis positivity among pregnant women screened at 40 antenatal clinics in Democratic Republic of Congo (DRC), 2011.
| Variable | Total | Positive (%) | OR (95% CI) | AOR (95% CI) |
|---|---|---|---|---|
| Populationa | 17,669 | 739 (4.2) | ||
| Age group | ||||
| 15–29 | 12,609 | 463 (3.7) | 1.0 | 1.0 |
| 30–49 | 5060 | 276 (5.5) | 1.5 (1.3–1.8) | 1.4 (1.2–1.7) |
| Age at first pregnancy | ||||
| ≤19 years | 12,201 | 566 (4.6) | 1.5 (1.2–1.8) | 1.0 (0.9–1.3) |
| ≥20 years | 5435 | 173 (3.2) | 1.0 | 1.0 |
| Age at first sexual encountera | ||||
| ≤15 | 7559 | 399 (5.3) | 1.6 (1.4–1.9) | 1.3 (1.1–1.5) |
| ≥16 | 9984 | 334 (3.4) | 1.0 | 1.0 |
| Age group of first sexual partner | ||||
| ≤15–19 | 4816 | 262 (5.4) | 1.5 (1.3–1.8) | 1.3 (1.1–1.5) |
| ≥20 | 12,220 | 446 (3.7) | 1.0 | 1.0 |
| Age group of current partner | ||||
| ≤15–29 | 6560 | 223 (3.4) | 0.7 (0.6–0.8) | 1.0 |
| ≥30 | 10,834 | 506 (4.7) | 1.0 | 1.4 (1.1–1.8) |
| Lifetime pregnancies | ||||
| One | 4144 | 118 (2.8) | 0.6 (0.5–0.7) | 0.8 (0.6–1.0) |
| Two or more | 13,524 | 621 (4.6) | 1.0 | 1.0 |
| Trimester at testing | ||||
| First | 1379 | 62 (4.5) | 1.1 (0.8–1.4) | |
| Second | 7612 | 311 (4.0) | 1.0 (0.8–1.1) | |
| Third | 8676 | 366 (4.2) | 1.0 | |
| HIV test result | ||||
| Positive | 627 | 29 (4.6) | 1.1 (0.8–1.6) | |
| Negative | 17,042 | 710 (4.2) | 1.0 | |
| Education | ||||
| None | 1274 | 75 (5.9) | 3.8 (1.5–9.6) | 2.6 (1.0–6.7) |
| Some primary | 4572 | 248 (5.4) | 3.5 (1.4–8.6) | 1.9 (0.8–4.9) |
| Complete primary | 1313 | 58 (4.4) | 2.8 (1.1–7.1) | 1.9 (0.7–4.9) |
| Some secondary | 7913 | 297 (3.8) | 2.4 (1.0–5.8) | 1.9 (0.8–4.7) |
| Complete secondary | 2052 | 51 (2.5) | 1.6 (0.6–3.9) | 1.6 (0.6–4.1) |
| Some university | 312 | 5 (1.6) | 1.0 | 1.0 |
| Complete university | 233 | 5 (2.1) | 1.3 (0.4–4.7) | 1.3 (0.4–4.7) |
| Marital status | ||||
| Single | 915 | 26 (2.8) | 1.0 | 1.0 |
| Married (mono) | 11,322 | 452 (4.0) | 1.4 (1.0–2.1) | 1.1 (0.7–1.6) |
| Married (poly) | 2066 | 109 (5.3) | 1.9 (1.2–2.9) | 1.2 (0.7–1.9) |
| Non-married couple | 3147 | 145 (4.6) | 1.7 (1.1–2.5) | 1.3 (0.8–2.0) |
| Separated | 149 | 4 (2.7) | 0.9 (0.3–2.7) | 0.6 (0.2–1.9) |
| Divorced | 21 | 1 (4.8) | 1.7 (0.2–13.2) | 1.3 (0.2–10.2) |
| Widow | 45 | 2 (4.4) | 1.6 (0.4–6.9) | 0.9 (0.2–3.8) |
| Clinic location | ||||
| Urban | 7102 | 215 (3.0) | 1.0 | 1.0 |
| Rural | 10,567 | 524 (5.0) | 1.7 (1.4–2.0) | 1.6 (1.3–1.9) |
| Clinic Setting | ||||
| Health center | 2659 | 83 (3.1) | 0.7 (0.6–0.9) | 1.3 (0.9–1.5) |
| General hospital | 15,010 | 656 (4.4) | 1.0 | 1.0 |
| Province name | ||||
| BasCongo | 1327 | 16 (1.2) | 0.3 (0.2–0.4) | 0.4 (0.3–0.6) |
| Bandundu | 2703 | 54 (2.0) | 0.4 (0.3–0.6) | 0.3 (0.1–0.4) |
| Equateur | 2162 | 165 (7.6) | 1.8 (1.4–2.3) | 1.5 (1.1–2.0) |
| Kasai | 1309 | 51 (3.9) | 0.9 (0.6–1.2) | 0.9 (0.7–1.4) |
| Katanga | 2119 | 94 (4.4) | 1.0 | 1.0 |
| Kinshasa | 1840 | 41 (2.2) | 0.5 (0.3–0.7) | 0.5 (0.3–0.7) |
| Maniema | 859 | 26 (3.0) | 0.7 (0.4–1.0) | 0.5 (0.3–0.9) |
| North Kivu | 909 | 42 (4.6) | 1.0 (0.7–1.5) | 1.1 (0.8–1.7) |
| Occidental | 863 | 31 (3.6) | 0.8 (0.5–1.2) | 0.8 (0.5–1.3) |
| Orientale | 2658 | 205 (7.7) | 1.8 (1.4–2.3) | 1.7 (1.3–2.3) |
| South Kivu | 920 | 14 (1.5) | 0.3 (0.2–0.6) | 0.3 (0.2–0.6) |
OR = odds ratio; CI = confidence interval.
Age of first pregnancy (N = 17,636), age of first sex (N = 17,543), age of current partner (N = 17,394), marital status (N = 17,665).
Demographic correlates of syphilis seropositivity
Univariate correlates of syphilis seropositivity included: age (5.5%, 30–49 years versus 3.7%, 15–29 years), age of first pregnancy (4.6%, ≤19 years versus 3.2%, >20 years), age of first sexual encounter (5.3%, ≤15 years versus 3.4% ≥16 years), age of first sexual partner (5.4%, ≤15–19 years versus 3.7%, ≥20 years), age of the father of pregnancy (4.7%, ≥30 years versus 3.4% ≤15–29 years), number of pregnancies (4.6%, two or more pregnancies versus 2.8%, one pregnancy), and lower educational attainment. There was no association between HIV seropositivity and syphilis seropositivity (Table 1). In multivariate analysis controlling for univariate correlates, statistically significant associations remained for age (p=0.003), age of first sexual encounter (p=0.005), age of first sexual partner (p=0.009), and age of father of current pregnancy (p=0.001).
Regional seropositivity for syphilis and HIV co-infection
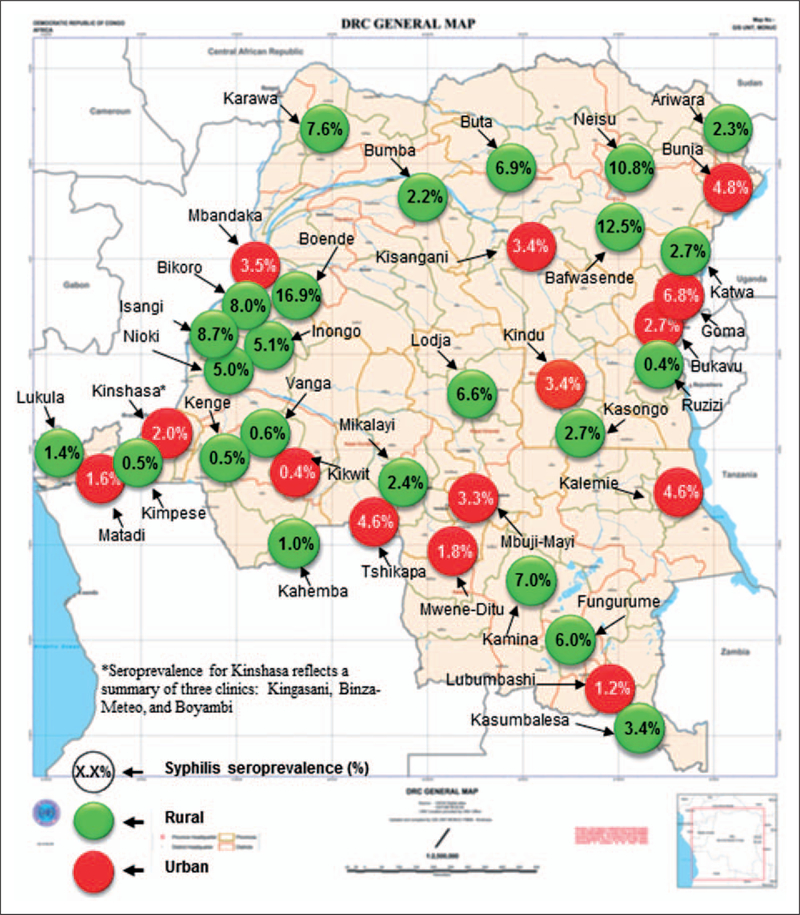
The overall syphilis seropositivity was 4.2% (739/17,669), (95% CI 3.9–4.5) (Table 1). The seropositivity for syphilis ranged from a low of 0.4% in Ruzizi to a high of 16.9% in Boende for 2011 (Figure 1). Women seen in rural clinics had a higher seropositivity (5%) as compared to those diagnosed in an urban setting (3%) (p<0.001) (Table 1). The provinces of Equateur (7.6%) and Orientale (7.7%) had a significantly higher seroprevalence than other sites (p<0.001). The provinces of Bas Congo (1.2%), Bandundu (2.0%), and South Kivu (1.5%) had significantly lower syphilis seroprevalence as compared to other clinic sites (p<0.001). In multivariate analyses controlling for demographic and behavioral correlates, province, and urban or rural clinic site, higher syphilis seropositivity remained associated with rural clinics and the provinces of Equateur and Orientale (p<0.001). The provinces of Bandundu, BasCongo, and South Kivu remained significantly associated with lower syphilis seropositivity (p<0.001). Of the 739 women seropositive for syphilis, 29 (4.6%) were seropositive for HIV (OR 1.1, 95% 0.8–1.6) (Table 1).
Figure 1.
Syphillis seroprevalence among women attending attenatal clinics in DRC, 2011 (N = 17,669).
Estimates of pregnant populations seropositive for syphilis and adverse pregnancy outcomes (APOs)
During 2011, an estimated 3,061,697 women were pregnant in DRC.19 Applying an overall estimated syphilis seroprevalence of 4.2% (95% CI 4.1–4.3), an estimated 128,591 of these pregnant women were seropositive for syphilis. Province-level estimates of pregnant women seropositive for syphilis are presented in Table 2. The province with the highest number of estimated pregnant women seropositive for syphilis was Orientale (N=30,204), followed by Equateur (N=28,052). The lowest number of pregnant women estimated to be syphilis seropositive were in BasCongo (N=1469) and South Kivu (N=3222). Using published estimates of adverse birth outcomes among pregnant women seropositive for syphilis,18 and assuming diagnosis and treatment were not available, a total of 85,513 pregnancies countrywide would have been affected by syphilis in 2011. The provinces of Equateur and Orientale had the highest APO estimates at 18,655 and 20,086, respectively (Table 2).
Table 2.
Estimates of pregnant women seropositive for syphilis by province, Democratic Republic of Congo (DRC) 2011.
| Province | 2011 Estimated pregnanciesa | Syphilis seroprevalence in women attending ANC (%) (95% CI) | Estimated pregnant women seropositive for syphilis | Projected number (range) of adverse pregnancy outcomes assuming unavailability of diagnosis and treatmentb | |
|---|---|---|---|---|---|
| Country total | 3,061,697 | 4.2 (4.1–4.3) | 128,591 | 85,513 | (68,668–105,187) |
| BasCongo | 122,440 | 1.2 (0.7–1.8) | 1469 | 977 | (784–1201) |
| Bandundu | 312,096 | 2.0 (1.7–2.3) | 6241 | 4150 | (3333–5105) |
| Equateur | 369,108 | 7.6 (7.3–7.9) | 28,052 | 18,655 | (14,980–22,947) |
| Kasai | 316,846 | 3.9 (3.4–4.2) | 12,357 | 8217 | (6599–10,108) |
| Katanga | 358,905 | 4.4 (4.1–4.7) | 15,792 | 10,502 | (10,568–12,918) |
| Kinshasa | 343,464 | 2.6 (2.3–2.9) | 8930 | 5938 | (4769–7305) |
| Maniema | 294,786 | 3.0 (2.7–3.4) | 8844 | 5881 | (4722–7234) |
| North Kivu | 84,760 | 4.6 (4.0–5.2) | 3899 | 2593 | (2082–3189) |
| Occidental | 252,242 | 3.6 (3.2–4.0) | 9080 | 4849 | (6018–7427) |
| Orientale | 392,264 | 7.7 (7.4–8.0) | 30,204 | 20,086 | (16,129–24,707) |
| South Kivu | 214,786 | 1.5 (1.1–1.9) | 3222 | 2143 | (1721–2636) |
| Provincial total | 128,090 | 85,180 | (68,400–104,778) | ||
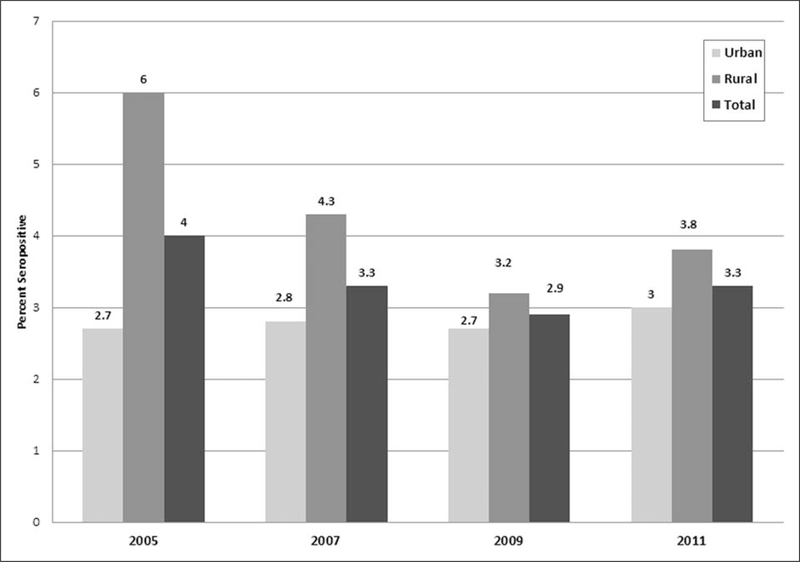
Trends in ANC syphilis seropositivity 2005–2011
Among the 23 clinics originally included in the 2005 ANC surveillance survey and retained in the ANC clinic program during 2007, 2009, and 2011, overall seropositivity remained stable (p=0.2 for trend) with a decline from 4% in 2005 to 2% in 2007 (67% decline) but an increase during 2009 to 2.9% and 2011 to 3.3%. Significant differences in syphilis seropositivity were noted by rural versus urban status with rural areas having higher seropositivity than urban for each of the four years studied (p<0.05 for urban versus rural all years) (Figure 2).
Figure 2.
Syphillis seropositivity among women tested in antenatal clinics in DRC, urban versus rural setting.
p< 0.05 for all years comparing urban versus rural clinic setting, p= 0.2 for trend between years. N=23 consistent clinics for each year.
Discussion
This analysis of DRC antenatal clinic syphilis screening results demonstrates moderate to high syphilis seroprevalence (4.2%) and geographic variations, with higher percentages seen among women in rural areas and those in the provinces of and Equateur and Orientale. Among this population of women participating in the ANC clinic survey, the majority received syphilis testing during the second and third trimester. HIV co-infection was uncommon and lower educational status portended a greater risk of syphilis seropositivity. Syphilis seropositivity was related to older age at the time of current pregnancy and younger age of first sexual encounter. Provincial-level seroprevalence estimates and number of pregnancies estimated to be affected by syphilis were high but will allow for resource projections to guide expanded syphilis screening and treatment programs. This is the first study to analyze national DRC ANC syphilis screening data for correlates of seropositivity. These findings have important implications for integrated CS prevention efforts linked to early ANC in regions of high syphilis seroprevalence.
The seroprevalence of syphilis among women seen at ANC in DRC was moderately high but relatively stable during 2005–2011. Higher seropositivity among rural regions suggests associations with poverty, lower education, and limited access to health care or to facilities with laboratory capacity.5 Overall, syphilis seroprevalence estimates among pregnant women in DRC are comparable to previously reported combined estimates among pregnant women from west and Central Africa (3.5%)19 but are higher than those reported in some of the countries bordering DRC such as Burundi (1.4%), Sudan (2.2%), Rwanda (1.5%) and lower than those in others Zambia (5%), Central African Republic (CAR) (10%), and Tanzania (4.4%), suggesting possible differences in screening and treatment access, risk, and disease prevalence.9,10 The DRC provinces of Equateur and Orientale which border CAR had significantly higher syphilis seropositivity. These same provinces are home to many internally displaced women that have since returned from conflict zones. In comparison to women living in longstanding river-dwelling communities, internally displaced women in DRC are at higher risk of being seropositive for syphilis (0.4 versus 4.0%) and having experienced gender-based violence.11
The optimal timing of syphilis screening as part of ANC is during the first trimester of pregnancy such that treatment can be provided in time to prevent perinatal complications including stillbirth, neonatal death, low birth weight, premature birth, and congenital deformities.3,5,20 The majority of women in this sample presented for ANC and were tested during the second (43%) and third (49%) trimesters limiting the opportunity for early treatment. In addition to lives saved through prevention,20 maternal screening for syphilis has been shown to be highly cost effective.21 Rapid point-of-care testing for syphilis has been consistently demonstrated to substantially reduce syphilis burden among tested populations through access to immediate treatment21,22 and bordering countries of Uganda and Zambia have now integrated rapid syphilis testing into ANC programs.22 DRC does not currently employ a rapid point-of-care test for syphilis thus, treatment is not available until and unless the woman returns for her test results. Injectable penicillin, for treatment of women testing positive for syphilis during the 4-week ANC survey, is administered as a one-time dose of 2.4 MU according to DRC national treatment guidelines.23 Penicillin is provided at no charge to the ANC clinics in DRC through USG funding during the 4-week survey period and though stock-outs are rare, clinics may impose a charge for administration, thus limiting treatment for some impoverished women. Syphilis screening and treatment services at these clinics may or may not be available during the remainder of the year; and if available may incur additional cost to pregnant women.
HIV prevalence among pregnant women attending ANC clinics in DRC has been decreasing during 2001–20118 and higher HIV prevalence is seen in urban areas. Previous studies differ with respect to associations with HIV status and syphilis seropositivity among pregnant women in sub-Saharan Africa.24,25 HIV/syphilis co-infection was rare among pregnant women testing positive for syphilis in this sample and we did not find an association between syphilis and HIV seropositivity.
Older age at ANC presentation and younger age at first sex suggest cumulative sexual risk among syphilis seropositive pregnant women in this sample. Lower educational attainment was associated with syphilis seropositivity in univariate analysis and has been reported previously as associated with syphilis.26 These findings are similar to other reports24–26 and may be valuable in promoting education of women regarding STD risks associated with younger age of sexual initiation and promoting the availability of rapid STD tests of low complexity allowing broader access to diagnosis and treatment among young female populations.
APOs among women as a result of untreated syphilis have been recently estimated to occur in up to 66.5% (range 53%–82%) of pregnant women seropositive for syphilis.18 Using these estimates, projections of women seropositive for syphilis and APOs associated with untreated maternal syphilis in DRC provide valuable information to guide services and resources in the direction of CS elimination. Of the eleven provinces in DRC, Equateur and Orientale were most heavily affected by higher syphilis seropositivity. These were also the provinces with the highest estimated number of pregnant women in DRC; together representing 25% of the total for 2011. Given higher affected population projections in these specific provinces of DRC, efforts to expand services may prioritize these areas in order to match service needs with available resources. Services to consider might include rapid syphilis testing at the first ANC visit (integrated with HIV testing) and, for women testing positive, prompt treatment with injectable penicillin during the same clinic encounter. Available rapid syphilis tests are simple and inexpensive and have been proven feasible for primary health care workers to conduct even at clinics lacking electricity or running water.27
We reviewed data collected from the DRC ANC clinic survey to provide estimates and projections of the magnitude of the issue of syphilis seropositivity among pregnant women. The interpretation of these findings should take into account the following limitations. The population of women included in this ANC clinic surveillance program may not be representative of the pregnant population of DRC. In 2011, the DRC Reproductive Health Program (DRCRHP) estimated 3,061,697 pregnancies occurring countrywide.17 Our sample represented a small proportion (0.6%) of this total. Thus, generalization of these data should be done with caution. DRC is estimated to be 70% rural and the DRCRHP estimated that 76% of pregnant women accessed pre-natal care in 2011.17 Clinics and laboratories participating in this surveillance program are able to collect and perform specimen analysis using moderate complexity systems and may not represent the ANC available to most pregnant women in DRC. Access to care for pregnant women residing in rural areas may be limited by geographical distance, poverty, and conflict.5,11 Syphilis seropositivity does not necessarily indicate active syphilis infection, and may be an indicator of previously treated syphilis; although this evaluation included confirmatory RPR testing, false positives are assumed to be low. Projections of APOs may be overestimates as some women in DRC may have benefitted from diagnosis and treatment. Finally, information on maternal receipt of treatment, pregnancy outcomes, and infant treatment were not collected, thus, the effect of the screening program in preventing infant transmission could not be ascertained.
DRC’s current health planning priorities and commitment of international partners offers several opportunities for strengthening antenatal syphilis control. Both the US President’s Emergency Plan for AIDS Relief (PEPFAR) and Global Fund are supporting the DRC efforts to strengthen the national vision for PMTCT of HIV and syphilis. The number of clinics participating in ANC surveillance increased from 23 in 2005 to 40 in 201128 and is expected to increase to 60 clinics in 2013.29 By 2014, PEPFAR estimates that PMTCT services with integrated syphilis screening and treatment will be provided to approximately 1.2 million pregnant women.29 Because antenatal syphilis screening and treatment is integrated into ANC, these new PMTCT programs will help boost the coverage of antenatal syphilis testing and treatment. Data from this expanded testing program will further inform program planning, surveillance, prevention, and treatment efforts. CS prevention efforts in DRC would benefit from further study to evaluate screening coverage, treatment completion rates, and birth outcomes among pregnant women diagnosed with syphilis in ANC clinics in order to identify targets for service improvement and resource allocation.
Study approval
This study protocol was reviewed and designated as routine disease surveillance/not human subjects research by the Ethics/IRB committee of the Kinshasa School of Public Health and CDC for each of the years included in this study.
Acknowledgments
Funding
This research received no specific grant from any funding agency in the public, commercial, or not for profit sectors.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent views of the Centers for Disease Control and Prevention.
References
- 1.Newman L, et al. Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. PLoS Med 2013; 10: e1001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Sexual and Reproductive Health. Over a million pregnant women infected with syphilis worldwide, http://www.who.int/reproductive-health/topics/rtis/syphilis/pregnancy/en/ (accessed August 14, 2013).
- 3.World Health Organization. Methods for surveillance and monitoring of congenital syphilis elimination within existing systems, http://whqlibdoc.who.int/publications/2011/9789241503020_eng.pdf (2011, accessed 8 January 2013).
- 4.Centers for Disease Control and Prevention. Winnable battles. Mother-to-child transmission of HIV and syphilis globally, http://www.cdc.gov/winnablebattles/Mother-to-ChildTransmission (accesssed 8 January 2013).
- 5.Kamb ML, Newman LM, Riley PL, et al. A road map for the global elimination of congenital syphilis. Obstet Gynecol Int 2010; 2010: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newman L, Hawkes S, Kamb M, et al. Challenges in global estimates of syphilis in pregnancy. Sex Transm Inf 2011; 87: S4.1. [Google Scholar]
- 7.Kinoshita-Moleka R, Smith JS, Atibu J, et al. Low prevalence of HIV and other selected sexually transmitted infections in 2004 in pregnant women from Kinshasa, the Democratic Republic of the Congo. Epidemiol Infect 2008; 136: 1290–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sentinel Surveillance of HIV/AIDS among pregnant women attending antenatal care clinics in the Democratic Republic of Congo. National Program of AIDS Control (PNLS), Ministry of Public Health: Democratic Republic of Congo, 2011, pp.1–70. [Google Scholar]
- 9.Global HIV/AIDS Response – Epidemic update and health sector progress towards universal access – Progress Report 2011. World Health Organization, 2011, pp.176–178. [Google Scholar]
- 10.Towards Universal Access – Scaling up priority HIV/AIDS interventions in the health sector – Progress Report 2010. World; Health Organization, 2010, pp.112–113. [Google Scholar]
- 11.Kim AA, Malele F, Kaiser R, et al. HIV infection among internally displaced women and women residing in river populations along the Congo River, Democratic Republic of Congo. AIDS Behav 2009; 13: 914–920. [DOI] [PubMed] [Google Scholar]
- 12.Batina A, Kabemba S and Malengela R. [Infectious markers among blood donors in Democratic Republic of Congo (DRC)]. Rev Med Brux 2007; 28: 145–149. [PubMed] [Google Scholar]
- 13.Tu D, Kos N, Culbert H, et al. Syndromic STI control and rates of hepatitis B and syphilis co-infection (with HIV) in Bukavu, Democratic Republic of Congo (DRC): Medicin sans Frontieres (MSF) program implementation in the context of chronic war and a failing healthcare system. Abstract ThPeC7369. The XV International AIDS Conference, Bangkok, Thailand, 11–16 July 2004. [Google Scholar]
- 14.Senga RK and Lutala PM. High prevalence of syphilis among demobilized child soldiers in Eastern Congo: a cross-sectional study. Confl Health 2011; 5: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vandepitte JM, Malele F, Kivuvu DM, et al. HIV and other sexually transmitted infections among female sex workers in Kinshasa, Democratic Republic of Congo, in 2002. Sex Transm Dis 2007; 34: 203–208. [DOI] [PubMed] [Google Scholar]
- 16.Guidelines for conducting HIV sentinel serosurveys among pregnant women and other groups. UNAIDS/WHO Working Group on Global HIV/AIDS and STI Surveillance, 2003, pp.1–77. [Google Scholar]
- 17.Programme National de Sante de la Reproduction, Rapport Annuel 2011. Republique Democratique du Congo Ministere de la Sante Publique, 2011; p.13. [Google Scholar]
- 18.Gomez GB, Kamb ML, Newman LM, et al. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ 2013; 91: 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chico RM, Mayaud P, Ariti C, et al. Prevalence of malaria and sexually transmitted and reproductive tract infections in pregnancy in sub-Saharan Africa: a systematic review. JAMA 2012; 307: 2079–2086. [DOI] [PubMed] [Google Scholar]
- 20.Blencowe H, Cousens S, Kamb M, et al. Lives Saved Tool supplement detection and treatment of syphilis in pregnancy to reduce syphilis related stillbirths and neonatal mortality. BMC Public Health 2011; 11: S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schackman BR, Neukermans CP, Nerette Fontain SN, et al. Cost-effectiveness of rapid syphilis screening in prenatal HIV testing programs in Haiti. PloS Med 2007; 4: 937–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Strasser S, Bitarakwate E, Gill M, et al. Syphilis testing within prevention of mother-to-child transmission of HIV programs in Uganda and Zambia: a field acceptability and feasibility study. J Acquir Immune Defic Syndr 2012; 61: e40–e46. [DOI] [PubMed] [Google Scholar]
- 23.Guide National de Prise en Charge des Infections Sexuellement Transmissibles Selon l’Approche Syndromique. Republique Democratique du Congo, Ministere de la Sante, Programme Nationa de Lutte Contre le SIDA and IST (PNLS), 2006, p.40. [Google Scholar]
- 24.Lubiganon P, Piaggio G, Villar J, et al. The epidemiology of syphilis in pregnancy. Int J STD AIDS 2002; 13: 486–494. [DOI] [PubMed] [Google Scholar]
- 25.Todd J, Munguti K, Grosskurth H, et al. Risk factors for active syphilis and TPHA seroconversion in rural African populations. Sex Transm Inf 2001; 77: 37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McDermott J, Steketee R, Larsen A, et al. Sypihlis-associated perinatal and infant mortality in rural Malawi. Bull World Health Organ 1993; 71: 773–780. [PMC free article] [PubMed] [Google Scholar]
- 27.Mabey DC, Sollis KA, Kelly HA, et al. Point-of-care tests to strengthen health systems and save newborn lives: the case of syphilis. Plos Med 2012; 9: E1001233.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Democratic Republic of the Congo. Operational Plan Report FY2011. US President’s Emergency Plan for AIDS Relief (PEPFAR). 1–80, http://www.pepfar.gov/documents/organization/199727.pdf (accessed 28 March 2013).
- 29.Plan d’élimination de la transmission du VIH de la mère à l’enfant et du maintien des mères en vie: 2012–2017 (2012). Programme National Multisectoriel de Lutte contre le SIDA. République Démocratique du Congo. [Google Scholar]