Abstract
Background
Septal haematomas causing left ventricular or biventricular outflow obstruction are rare but known complications of chronic total occlusion (CTO) percutaneous coronary intervention (PCI) and can be life-threatening.
Case summary
In this case, we describe the formation of a septal haematoma during retrograde CTO PCI. The patient was initially managed conservatively but became progressively unstable, for which she underwent coiling of the inflow and outflow of the septal perforator. Despite coiling, she developed near complete right ventricular outflow obstruction (based on echocardiography). She was successfully managed with a percutaneous right ventricle assist device, with subsequent resolution of the outflow obstruction.
Discussion
Septal haematomas with resultant outflow obstruction have been uniformly fatal. In our case, the use of a percutaneous right ventricle assist device was life-saving.
Keywords: Case report, Chronic total occlusion, Percutaneous coronary intervention, Septal haematoma, Outflow obstruction
Learning points
Septal haematomas are rare but known complications from chronic total occlusion percutaneous coronary intervention.
While the vast majority of septal haematomas can be treated conservatively, they can progress to cause haemodynamic compromise.
The use of percutaneous ventricular assist devices can be life-saving in such situations.
Introduction
Percutaneous coronary intervention (PCI) of a chronic total occlusion (CTO) is amongst one of the most technically demanding procedures. Retrograde techniques have allowed for an increase in CTO crossing rates, with success rates greater than 90%1,2 but have also resulted in slightly increased complication rates.1–3 One known complication is the development of septal haematomas, which can result in life-threatening outflow obstruction.4–6
The typical mechanism of septal haematoma formation is from laceration of a septal artery, which was utilized for collateral crossing during retrograde CTO PCI.7 While the vast majority of septal haematomas can be managed conservatively, a few can grow large enough to affect the outflow of either or both ventricles.6 Other consequences include ventricular septal defect,4 cardiac tamponade (dry),8 and coronary-ventricular fistulas.9
Herein, we describe the life-saving management of a patient with a septal haematoma with isolated right ventricular outflow obstruction using a right ventricular assist device.
Timeline
| Initial procedure | Successful chronic total occlusion percutaneous coronary intervention performed but with septal haematoma formation, which was treated conservatively. |
| 4 h post-procedure | Worsening haemodynamics prompting repeat angiography. Further expansion of septal haematoma, which was treated with coiling of the inflow and outflow of the culprit septal artery. |
| 12 h post-procedure | Echocardiogram with near obliteration of the right ventricle. Impella RP placed with immediate normalization of haemodynamics. |
| Day 4 post-procedure | Impella RP weaned and removed. |
| Day 8 post-procedure | Discharged from the hospital. |
| 2 weeks after discharge | Seen in follow-up clinic with no anginal symptoms or limitations. |
| 3 months after procedure | Cardiac magnetic resonance imaging scan with complete resolution of septal haematoma. |
Case presentation
A 63-year-old woman with hypertension and hyperlipidaemia developed typical angina with an inability to carry any physical activity (Canadian Cardiovascular Society Class IV) over a 6-month timeframe. Despite being on maximally tolerated doses of two anti-anginals (metoprolol succinate 100 milligrams daily and extended release isosorbide mononitrate 60 mg daily), in addition to aspirin 81 mg and atorvastatin 40 mg daily, she continued to have ongoing symptoms. She subsequently underwent a regadenoson nuclear stress demonstrating severe inferior wall ischaemia but with normal left ventricular function. The patient then underwent coronary angiography, which showed a right coronary artery (RCA) CTO with no other significant epicardial coronary artery disease. Due to her ongoing symptoms and single vessel disease, the decision was made to proceed with CTO PCI.
On the day of the procedure, the patient was found to have unremarkable vitals (heart rate 48 b.p.m., blood pressure 100/78 mmHg, and oxygen saturation of 100% on room air). Her physical examination demonstrated a normal cardiopulmonary exam with normal heart and lung sounds with no stigmata of heart failure. Her radial pulses were 2+, as well as her femoral pulses. Her initial electrocardiogram demonstrated normal sinus rhythm with no ST-T abnormalities or signs of a prior infarction. Due to patient preference to immediately ambulate post-procedure, a biradial approach was chosen for her CTO PCI.
The patient was pre-loaded with aspirin and clopidogrel, and underwent CTO PCI with a 7-Fr AL 0.75 guide and a 7-Fr EBU 3.5 guide. Dual angiography revealed a mid-RCA CTO, which was approximately 24 mm in length (Supplementary material online, Video S1). The plan was made to proceed with an antegrade approach using heparin with a target activated clotting time (ACT) of >300 s. An antegrade approach was initially attempted utilizing a TurnPike microcatheter (Teleflex, Wayne, PA, USA) and the following guidewires in serial succession: Fielder XT-A (Asahi Intecc, Aichi, Japan), Pilot 200 (Abbott Vascular, Santa Clara, CA, USA), and Gaia 2nd (Asahi Intecc). However, these wires kept going subintimal and there was also a wire exit with the Gaia 2nd wire. The CTO strategy was then switched to a retrograde approach utilizing a Turnpike 150 cm microcatheter. The ACT target was now increased to >350 s. A septal collateral to the right posterior descending artery was crossed with the use of a Sion wire (Asahi Intecc). A Gaia 2nd wire was then used retrograde to successfully cross the CTO from the distal true lumen to the proximal true lumen, which was then exchanged for a R350 externalizable wire (Teleflex). Percutaneous coronary intervention was then performed on the externalized wire via standard fashion with an excellent angiographic result.
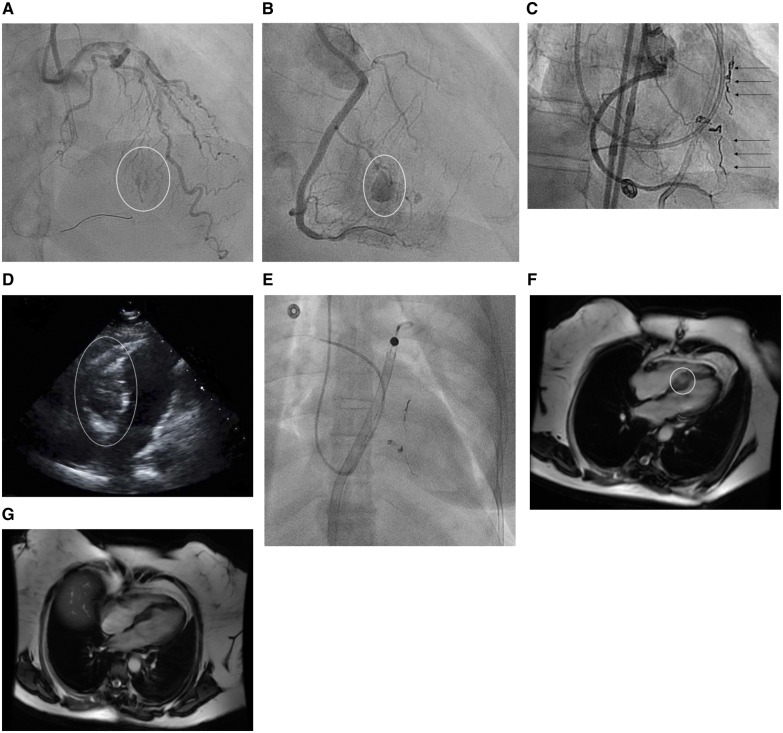
After completion of the PCI, the retrograde hardware was removed. However, an injection in the retrograde donor artery demonstrated septal artery laceration with subsequent haematoma formation (Figure 1A, Supplementary material online, Video S2). A conservative management strategy was initially chosen, where she was observed on the cath lab table for approximately 2 h. No additional fluid or anticoagulation was given. Reversal of her anticoagulation was not performed because her ACT fell to sub-therapeutic levels quickly post-procedure. She fared well without any haemodynamic stability or arrhythmias initially in the post-procedural area. However, the patient developed a sudden onset 8 of 10 chest pain. The heart rate at the time was 94 b.p.m., blood pressure of 100/60 mmHg, and 98% oxygen saturation on room air. Her electrocardiogram demonstrated only sinus tachycardia. However, she was brought back to the cath lab due to her ongoing pain where a repeat angiogram demonstrated expansion of the septal haematoma (Figure 1B, Supplementary material online, Video S3). Due to the enlarging size of the haematoma, she underwent coiling of the inflow and outflow of the culprit septal collateral (Figure 1C) (Of note, the patient did receive heparin for the coiling procedure, to prevent clotting of the required catheters and devices.). The patient was then transferred to the cardiac care unit.
Figure 1.
Fluoroscopic images of the septal haematoma. (A) Initial septal perforation and haematoma formation (circle shows the perforation). (B) Haematoma expansion in the intraventricular septum (circle shows the enlarging haematoma). (C) Coiling of the inflow and outflow of the perforated septal collateral (arrows show the coils). (D) Transthoracic apical four chamber view of the septal haematoma compressing the right ventricle and obliterating the right ventricular cavity (circle shows the haematoma). (E) Fluoroscopic image of an Impella RP device in place with a Swan-Ganz catheter. (F) Baseline cardiac magnetic resonance imaging at discharge showing the septal haematoma (circle shows the haematoma). (G) Repeat magnetic resonance imaging 3 months later with resolution of the septal haematoma.
While initially stable post-procedure, the patient became hypotensive to 70/48 mmHg and failed to improve with over 3 L of fluid resuscitation and inotropes (dopamine and norepinephrine) over the next two hours. A transthoracic echocardiogram demonstrated almost complete obliteration of the entire right ventricle (RV) from the haematoma (Figure 1D, Supplementary material online, Video S4), but with normal left ventricular function. The septal haematoma measured 4.2 cm in certain views, and a trivial pericardial effusion was noted. Due to severe right-sided failure, the patient underwent placement of a percutaneous RV assist device, Impella RP (Abiomed, Danvers, MA, USA) via a right femoral approach (Figure 1E). The Impella was placed at P-9, which was the maximal performance level of the device. Her haemodynamics normalized immediately and over the next few days, the septal haematoma steadily decreased in size. The Impella RP was weaned steadily to P2 and removed. During the process, the patient was maintained on dual-antiplatelet therapy with aspirin and clopidogrel.
The patient was discharged after a baseline cardiac magnetic resonance imaging (MRI) (Figure 1F) was performed. A follow-up MRI scan 3 months post-procedure demonstrated resolution of the haematoma (Figure 1G). The patient was seen 4 months post-procedure in follow-up clinic and found to be symptom free with no limitations.
Discussion
One of the most well-known complications of CTO PCI is perforation of a collateral artery. Recent studies demonstrate that it occurs from 3% to 7% of cases of CTO PCI.10,11 While most septal artery perforations are benign and can be managed conservatively, some can progress to become septal haematomas, which in turn, can cause haemodynamic compromise through outflow obstruction (as demonstrated in this case). While this is a rarely described phenomenon, all prior reports of septal haematomas have all been due to either isolated left-sided or biventricular outflow obstruction.4–6 Our case is unique in that there was isolated right ventricular outflow obstruction.
Previously described strategies to manage enlarging septal haematomas include conservative treatment (if the patient is haemodynamically stable),12 aspiration with a microcatheter,9 and occlusion of the septal perforator with coils.9 In our case, we obviated the haemodynamic sequalae of outflow obstruction with use of a right-sided ventricular support device and allowing for regression of the haematoma. Another strategy considered, but not ultimately needed, would have been to create a controlled fenestration of the haematoma into the right or left ventricular cavity with a stiff wire followed by dilatation with a small balloon.
Conclusions
Septal haematomas causing outflow obstruction are rare complications of CTO PCI and can be life-threatening. This is the first report of isolated RV compression and the use of a right-sided haemodynamic support device was life-saving.
Lead author biography

Dr Darshan Doshi is an interventional cardiologist who specializes in complex and high-risk coronary interventions. He received his BA from Columbia University’s Columbia College and his MD from Columbia University’s College of Physicians and Surgeons. He completed his internal medicine residency, and his cardiovascular medicine and interventional cardiology fellowships at the Columbia University Medical Center. He also underwent additional dedicated training at Columbia in complex and high-risk interventional procedures. Then, he joined the faculty in the Division of Cardiology at the Massachusetts General Hospital and Harvard Medical School in 2018. He also holds a MS in patient-oriented research from Columbia University’s Mailman School of Public Health with a research interest focused on clinical trials evaluating novel cardiovascular devices and therapeutics in interventional cardiology. He has authored several original manuscripts in translational and clinical cardiovascular medicine, and has published in the New England Journal of Medicine, Journal of the American College of Cardiology, and Circulation, among many others.
Supplementary Material
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: D.K. is on the speaker’s bureau of Boston Scientific and Abbott Vascular. The other authors have no conflict of interest to declare.
References
- 1. Galassi AR, Sianos G, Werner GS, Escaned J, Tomasello SD, Boukhris M, Castaing M, Büttner JH, Bufe A, Kalnins A, Spratt JC, Garbo R, Hildick-Smith D, Elhadad S, Gagnor A, Lauer B, Bryniarski L, Christiansen EH, Thuesen L, Meyer-Geßner M, Goktekin O, Carlino M, Louvard Y, Lefèvre T, Lismanis A, Gelev VL, Serra A, Marzà F, Di Mario C, Reifart N.. Retrograde recanalization of chronic total occlusions in Europe: procedural, in-hospital, and long-term outcomes from the Multicenter ERCTO Registry. J Am Coll Cardiol 2015;65:2388–2400. [DOI] [PubMed] [Google Scholar]
- 2. Karmpaliotis D, Karatasakis A, Alaswad K, Jaffer FA, Yeh RW, Wyman RM, Lombardi WL, Grantham JA, Kandzari DE, Lembo NJ, Doing A, Patel M, Bahadorani JN, Moses JW, Kirtane AJ, Parikh M, Ali ZA, Kalra S, Nguyen-Trong PK, Danek BA, Karacsonyi J, Rangan BV, Roesle MK, Thompson CA, Banerjee S, Brilakis ES. Outcomes with the use of the retrograde approach for coronary chronic total occlusion interventions in a contemporary multicenter US registry. Circ Cardiovasc Interv 2016;9. pii: e003434. doi: 10.1161/CIRCINTERVENTIONS.115.003434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Riley RF, Sapontis J, Kirtane AJ, Karmpaliotis D, Kalra S, Jones PG, Lombardi WL, Grantham JA, McCabe JM.. Prevalence, predictors, and health status implications of periprocedural complications during coronary chronic total occlusion angioplasty. EuroIntervention 2018;14:e1199–e2206. [DOI] [PubMed] [Google Scholar]
- 4. Fairley SL, Donnelly PM, Hanratty CG, Walsh SJ.. Images in cardiovascular medicine. Interventricular septal hematoma and ventricular septal defect after retrograde intervention for a chronic total occlusion of a left anterior descending coronary artery. Circulation 2010;122:e518–e521. [DOI] [PubMed] [Google Scholar]
- 5. Araki M, Murai T, Kanaji Y, Matsuda J, Usui E, Niida T, Ichijo S, Hamaya R, Kakuta T.. Interventricular septal hematoma after retrograde intervention for a chronic total occlusion of a right coronary artery: echocardiographic and magnetic resonance imaging-diagnosis and follow-up. Case Rep Med 2016;2016:1.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Frisoli TM, Afana M, Mawri S, Hadid M, Sayed L, O’Neill WW, Wang DD, Parikh S, Khandelwal A, Alaswad K.. Respect the septal perforator: septal artery perforation during CTO PCI resulting in massive interventricular septal hematoma and biventricular cardiac obstructive shock. JACC Cardiovasc Interv 2017;10:e91–e92. [DOI] [PubMed] [Google Scholar]
- 7. Jackson MWP, Lee D, Egred M.. Septal hematoma: a rare but potentially serious complication of retrograde CTO-PCI. J Invasive Cardiol 2019;31:E47–E48. [PubMed] [Google Scholar]
- 8. Matsumi J, Adachi K, Saito S.. A unique complication of the retrograde approach in angioplasty for chronic total occlusion of the coronary artery. Catheter Cardiovasc Intervent 2008;72:371–378. [DOI] [PubMed] [Google Scholar]
- 9. Abdel-Karim AR, Vo M, Main ML, Grantham JA.. Interventricular septal hematoma and coronary-ventricular fistula: a complication of retrograde chronic total occlusion intervention. Case Rep Cardiol 2016;2016:8750603.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Danek BA, Karatasakis A, Tajti P, Sandoval Y, Karmpaliotis D, Alaswad K, Jaffer F, Yeh RW, Kandzari DE, Lembo NJ, Patel MP, Mahmud E, Choi JW, Doing AH, Lombardi WL, Wyman RM, Toma C, Garcia S, Moses JW, Kirtane AJ, Hatem R, Ali ZA, Parikh M, Karacsonyi J, Rangan BV, Khalili H, Burke MN, Banerjee S, Brilakis ES.. Incidence, treatment, and outcomes of coronary perforation during chronic total occlusion percutaneous coronary intervention. Am J Cardiol 2017;120:1285–1292. [DOI] [PubMed] [Google Scholar]
- 11. Patel VG, Brayton KM, Tamayo A, Mogabgab O, Michael TT, Lo N, Alomar M, Shorrock D, Cipher D, Abdullah S, Banerjee S, Brilakis ES.. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv 2013;6:128–136. [DOI] [PubMed] [Google Scholar]
- 12. Lorca R, Pascual I, Suarez-Cuervo A, Martín M, Calvo J, Corros C, Cigarrán H, Avanzas P, Hernández-Vaquero D, Morís C.. Severe intramyocardial hematoma as a complication of retrograde approach in chronic total occlusion. JACC Cardiovasc Interv 2017;10:1591–1592. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.