Abstract
Social anxiety disorder (SAD) often involves difficulty developing relationships. Facial expressions are important in relationship formation, but data are limited regarding facial display production among persons with SAD during social interaction. The current study compared facial displays of individuals diagnosed with SAD (n=41) to control participants (n=24) as they interacted with a confederate; confederates and observers then rated their desire for future interaction with participants. Automated software used the Facial Action Coding System (FACS; Ekman & Friesen, 1978) to classify displays. During portions of the interaction that involved listening to partners, the SAD group smiled less frequently and less intensely than controls, and lower smiling was associated with others’ lower desire for future interaction with participants. Diminished positive facial affect in response to interaction partners may disrupt relationship formation in SAD and may serve as an effective treatment target.
Keywords: Social anxiety, Facial expressions, Emotion, Social processes, Social behavior
Social anxiety disorder (SAD) is characterized by difficulties in developing social relationships (see Alden & Taylor, 2004, 2010 for reviews). Individuals with SAD have significantly fewer friends, report having social relationships of lower quality, and are less likely to marry than are individuals without psychiatric diagnoses (Rodebaugh, 2009; Schneier et al., 1994). During laboratory-based conversation tasks with strangers, individuals high in social anxiety tend to receive lower overall ratings of socially effective verbal and nonverbal behavior, and are less liked by conversation partners (e.g., Meleshko & Alden, 1993; Voncken, Alden, Bogels, & Roelofs, 2008). If there are specific unhelpful behaviors associated with SAD that lead to negative interpersonal outcomes (e.g., negative impressions by others, eventual social exclusion) then these behaviors would be expected to cyclically strengthen unhelpful intrapersonal factors (e.g., negative expectations regarding social situations) and deprive individuals with SAD from developing positive connections with others (see Alden & Taylor, 2010). Identifying particular behaviors that tend to initiate these negative interpersonal cycles would both contribute to knowledge of mechanisms that underlie SAD’s maintenance and inform treatment strategies to optimize clinical outcomes.
Some emotion theorists have proposed that behaviors of emotional expression play an important role within social relationships and that deficits in this area may explain impairment in interpersonal processes across a wide range of psychological disorders (Keltner & Kring, 1998). While there is ongoing debate about whether viewing specific facial expressions leads to perception of certain emotion categories universally (Gendron, Lindquist, Barsalou, & Barrett, 2012; Kim & Sasaki, 2014; Kitayama & Uskul, 2011), considerable evidence supports the idea that affective facial displays have important interpersonal outcomes (aan het Rot, Enea, Dafinoiu, Iancu, & Tafta, 2017; Schrammel, Pannasch, Graupner, Mojzisch, & Velichkovsky, 2009; Williams, McGlone, Abbott, & Mattingley, 2008), and some propose that the function of facial displays can only be understood by assessing their role within social interactions (Crivelli & Fridlund, 2018). Evidence suggests that people rely heavily on strangers’ facial displays when making judgments regarding their stable traits, including the degree to which they are affiliative and warm (Knutson, 1996). Moreover, viewing others’ smiles has been linked to viewers’ subsequent approach behaviors (Furl, Gallagher, & Averbeck, 2012; Winkielman, Berridge, & Wilbarger, 2005), agreeable and dominant behaviors (aan het Rot et al., 2017), and desire for further contact with the person smiling (Palmer & Simmons, 1995). Research suggests that responsivity toward a partner per se, such as smiling in response to the partner’s disclosures, may be read as attentiveness and positive regard and has special significance for relationship building (Reis & Shaver, 1988). Accordingly, minimal smiling within positive social interactions may limit opportunities to build or strengthen a connection. In contrast, facial displays of fear are thought to convey that a stimulus is aversive (Blair, 2003), and observing displays of fear in others produces fear-related physiological responses in the onlooker (Olsson, Nearing & Phelps, 2007; Olsson & Phelps, 2004). Viewing fear displays in an interaction partner within an otherwise positive social context may signal to the viewer that the context actually is threatening and may thereby decrease the viewer’s desire for interaction with that partner in the future (Keltner & Kring, 1998). Gaining insight into smiling and fear displays in individuals with SAD may point to mechanisms that perpetuate problems in forming new social relationships.
Few studies, however, have examined facial expression production in individuals with elevated social anxiety symptoms during a social interaction (Baker & Edelmann, 2002; Heerey & Kring, 2007; for a review see Davies et al., 2016). Baker and Edelmann (2002) found no differences in lay (untrained) evaluations of smiling in SAD versus non-SAD participants during a conversation with a study confederate. Heerey and Kring (2007) used trained observers to classify both positive (smiling) and negative (frowning) facial displays during a getting acquainted social interaction in university students with high versus low levels of social anxiety. Social anxiety was not associated with differences in frequency of frowning; however, participants who were high in social anxiety less frequently matched the smiles of their partners than their low social anxiety counterparts did, suggesting diminished smile reciprocity. Further, conversation partners low in social anxiety tended not to experience a boost in positive affect if paired with a high social anxiety partner, and the positive affect that they did experience correlated with their high social anxiety partners’ displays of pleasant smiling (i.e., smiling that involved the eye region). The authors speculated that this blunted change in positive affect may have been linked in part to high social anxiety participants’ lower reciprocity of smiling; however, this hypothesis was not directly tested. Thus, one of two studies investigating facial displays of emotion in individuals with social anxiety found subtle differences in positive displays compared to control participants within an interpersonal context. Extant findings are limited, however, by small sample sizes, subjective measures of facial displays, relatively brief (up to 5-minute) and unstandardized interactions across participants, and use of non-clinical undergraduate samples.
The current study aimed to build upon this literature in several ways. First, prior studies did not use well-established methods for coding facial expressions. The current study used the Facial Action Coding System (FACS; Ekman & Friesen, 1978), which was designed to impartially categorize facial expressions by tracking individual muscle movements within the face, called action units (Ekman, Friesen & Ancoli, 1980). Although debate within emotion research has raised important questions about the universality of the basic emotion categories that subserve FACS (Gendron et al., 2012; Gendron, Roberson, van der Vyver, & Barrett, 2014), it is nonetheless still considered by many to be the optimal method of descriptively classifying facial displays, due to its precision and reliability (Fairbairn, Sayette, Aalen, & Frigessi, 2015; Girard, Cohn, Mahoor, Mavadati, & Rosenwald, 2013). Historically, it has been logistically challenging to measure production of facial displays with human coders via FACS, because both training to become expert in this system and engaging in manual coding is laborious and time consuming (e.g., three hours for a trained expert to code one minute of facial display video footage; Bartlett et al., 2014). These practical constraints limit the feasibility of manually FACS coding more than a few minutes of facial displays. The current study employed the Computer Expression Recognition Toolbox (CERT; Littlewort et al., 2011), an automated facial recognition software that classifies facial displays via FACS within each frame of video footage and estimates the intensity of each facial display. CERT has demonstrated excellent convergence with human expert FACS coders across multiple image corpuses, including ones that contain dynamic videos involving speech (Bartlett et al., 2010). Using this technology, the current study examined FACS coded facial displays across the entirety of a 25-minute relationship formation encounter, thereby both implementing a more precise method of facial coding and pooling a larger sample of observations per participant than has been possible to measure previously. The current study also standardized the content of the interactions across participants by using largely scripted verbal and nonverbal responses delivered by confederates, which afforded greater experimental control than in prior research.
We selected smiling and fear expressions as our primary outcomes, two facial displays that have been associated with interpersonal outcomes (aan het Rot et al., 2017; Schrammel et al., 2009; Williams et al., 2008) and that are relevant for individuals with SAD. The primary aim of the study was to characterize the frequency and intensity of these facial displays in individuals diagnosed with SAD versus a control group without clinical diagnoses within the context of a relationship formation encounter. As a second aim, the study sought to investigate the relationship between these facial expressions and others’ desire to affiliate further. More specifically, it aimed to test whether individual differences in smiling and fear displays during a relationship building opportunity are linked to others’ level of desire for future interaction (DFI) with the expresser, since it is possible that this may account for expected lower levels of partner DFI toward participants with SAD.
Participants took part in a laboratory-based, video recorded relationship formation task (Aron, Melinat, Aron, Vallone, & Bator, 1997; Taylor, Pearlstein, & Stein, 2017; Kashdan & Roberts, 2006 Study 1). Trained confederates served as interaction partners. Confederates as well as two observers who viewed the interaction recordings rated their DFI with participants following the task. CERT software used FACS to code participants’ recorded facial displays. Because individuals with SAD tend to experience and display both diminished positive affect and behaviors (Gilboa-Schechtman et al., 2014; Kashdan, Weeks, & Savostyanova, 2011) as well as heightened anxiety and anxious behaviors during social interactions (Alden & Taylor, 2010; Barlow, 2014), we predicted lower smiling and higher fear displays in the SAD group than in the control group. Moreover, we predicted that across all participants, lower smiling and higher fear displays each would be associated with conversation partners’ lower DFI.
Method
Participants
The total sample consisted of 76 volunteers, 50 of whom were treatment-seeking individuals with SAD, and 26 of whom were non-anxious control participants. Volunteers were recruited to participate in a larger treatment study via posted announcements in community settings (i.e., flyers) and online settings (e.g., ResearchMatch.org). To be considered eligible, those within the SAD group met criteria for principal SAD and had scores ≥ 50 on the clinician administered Liebowitz Social Anxiety Scale (LSAS; Liebowitz, 1987), and those within the control group had LSAS scores ≤ 20. Exclusion criteria were: (1) active suicidal ideation with intent or plan; (2) moderate to severe alcohol or marijuana use disorder within the past year; (3) all other mild substance use disorders within the past year; (4) bipolar I disorder; (5) psychotic disorders; (6) moderate to severe traumatic brain injury with evidence of neurological deficits or neurological disorders; (7) severe or unstable medical conditions that might leave the individual negatively impacted by participation in the study; (8) inability to speak or understand English; (9) concurrent psychotherapy (unless 12-week stability criteria had been met, for non-empirically supported therapies only); (10) concurrent psychotropic medication (e.g., SSRIs, benzodiazepines); and (11) characteristics that would compromise safety to complete an MRI scan (e.g., metal devices in body), due to aspects of the research unrelated and subsequent to the current investigation.
Participants within the SAD group met criteria for several comorbid diagnoses: major depressive disorder (current episode; 24.4%), generalized anxiety disorder (24.4%), agoraphobia (7.3%), obsessive compulsive disorder (2.4%), and mild alcohol use disorder (2.4%). Within the control group, any history of a psychiatric diagnosis was exclusionary.
Procedure
All procedures performed involving human participants were in accordance with the ethical standards of the University of California San Diego Human Research Protection Program and with the Code of Ethics of the World Medical Association (Declaration of Helsinki). The current study took place within the context of an overarching computer-based treatment study for SAD. Participants were informed during the consent process that the study would involve behavioral tasks prior to the start of treatment. After receiving information about the research, participants provided informed written consent to participate, including consent to be videotaped. They then completed a clinician administered diagnostic eligibility assessment and self-report symptom measures. During a subsequent visit, eligible participants completed the relationship formation task, which was video recorded. Facial action processing took place offline.
Measures
Symptom measures.
SAD diagnosis was assessed using the Structured Clinical Interview for the Diagnostic and Statistical Manual (4th ed.; DSM–IV-TR; American Psychiatric Association, 2000) Axis I Disorders (SCID-I; First, Spitzer, Gibbon, & Williams, 1995)1. The SCID-I SAD module is highly structured and has excellent inter-rater reliability (Lobbestael, Leurgans, & Antz, 2011). All participants were also administered the Mini International Neuropsychiatric Interview (MINI Version 5.0.0 or 7.0.02; Sheehan et al., 1998; 2015) to assess comorbid and exclusionary diagnoses and to determine that SAD was the principal diagnosis. Diagnostic assessments were conducted by a PhD-level clinician as well as a PhD student in clinical psychology and two post-baccalaureate clinical research coordinators under the supervision of the second author, all of whom received extensive training in the interview protocols. Diagnostic consensus was reached by reviewing completed interviews during team meetings with the second author.
Social anxiety symptom severity was measured using the clinician-rated Liebowitz Social Anxiety Scale (LSAS; Liebowitz, 1987). The LSAS is a 24-item scale that presents a wide range of social situations and asks individuals to rate on a four-point scale both their typical level of fear (ranging from “none” to “severe”) and their typical level of avoidance (ranging from “never” to “usually”) for each situation. Items are summed to create a total score reflecting social anxiety severity (current sample Cronbach’s α = .98). The clinician-administered LSAS has standard instructions that all assessors provided to participants verbatim, and it correlates highly with the self-report version of the scale (Fresco et al., 2001). The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) was used to assess depression symptom severity over the preceding two weeks. The BDI–II has high internal consistency among college samples (Cronbach’s α = .93) and psychiatric outpatients (Cronbach’s α =.92; current sample Cronbach’s α = .93) and has sound psychometric properties (Beck et al., 1996; Dozois, Dobson, & Ahnberg, 1998).
Facial displays of emotion.
Two facial actions were selected as dependent variables: smiling and fear displays. As an index of smiling, we selected facial action unit 12 combined with action unit 6, consistent with prior work (Ekman, Davidson, & Friesen, 1990; Fairbairn et al., 2015). Action unit 12 is produced via contraction of the zygomaticus major muscle, which is responsible for upward pull of the lip corners (Ekman & Friesen, 1978). Action unit 6 is produced via contraction of the orbicularis oculi muscle and is responsible for “crow’s feet” creases near the eyes (Ambadar, Cohn, & Reed, 2009; Ekman et al., 1990). Together they produce the “Duchenne smile,” associated with reward-related interpersonal outcomes during social interaction in prior work (Fairbairn et al., 2015; Heerey & Kring, 2007)3. To index fear displays we selected the “fear brow” facial action, which involves lifting and drawing together the brows. Fear brow results from a combination of action units 1, 2, and 4, together produced via contraction of the frontalis pars medialis, frontalis pars lateralis, depressor glabellae, and corrugator facial muscles (Bartlett et al., 2010; Gottman, Levinson, & Woodin, 2001). Fear brow previously was observed in participants while they discussed an anxiety provoking personal event (Harrigan & O’Connell, 1996). We examined both the frequency and intensity of these facial actions as they occurred over the course of the relationship formation task.
Desire for Future Interaction.
The Desire for Future Interaction scale (DFI; Coyne, 1976) was administered to confederate interaction partners as a measure of motivation to engage in further contact with the participant with whom they were paired during the relationship formation task. The DFI is a well-established measure used in studies investigating interpersonal dimensions of psychopathology (Segrin, 2001). The DFI consists of eight items rated on a 7- point scale with anchors of not at all and very much that assess the extent to which the rater would be willing to engage in a variety of social activities with their interaction partner in the future. Sample items include, “Would you invite a person like this to visit you?” and “Would you like to have this person as a friend?” The individual items of the DFI have been shown to reliably load on a single factor (e.g., Segrin, 1993). Higher scores reflect greater motivation to engage in further contact with one’s conversation partner. Prior studies support the reliability and validity of the DFI (Powers & Zuroff, 1988; Voncken & Dijk, 2013; current sample Cronbach’s α = .92). Two observers blind to study hypotheses and participant diagnostic status watched video footage of the interactions and independently rated their DFI. Confederates and observers were not trained to reliability on the DFI; however, inter-rater reliability was moderate (two-way random intraclass correlation coefficient [ICC] for absolute agreement of the average measure was .69 between different observers and .66 between observers and confederates, both p < .001), suggesting convergence in subjective observer reactions to participants. Others’ desire for further engagement with participants was indexed by mean DFI score, averaged across observers and confederates.4
Relationship formation task.
The relationship formation task used here was an abbreviated version of a previously validated social interaction task (Aron et al., 1997) and involved the participant and confederate alternating responses to a series of questions that gradually increased in the depth of self-disclosure they were designed to elicit (see Taylor & Amir, 2012; Taylor et al., 2017; Kashdan & Roberts, 2006 Study 1). Immediately before the task an experimenter informed a given participant that he or she would be getting to know an assistant who worked in the lab (i.e., a confederate) and, once the confederate was present, stated that the purpose of the task was to get to know one another by answering a series of questions about themselves. Interactions began with an open-ended ice-breaker question (“Tell your partner a bit about yourself”) followed by five relationship-building questions selected from the Aron et al. (1997) paradigm (see the questions in Supplemental Materials; also used in Taylor & Amir, 2012 and Taylor et al., 2017)5. They were asked to take turns acting as the “speaker” and the “listener” and to refrain from speaking during their listening turns. Both confederates and participants answered all six questions, and interactions typically took 25 minutes to complete. Confederates completed DFI ratings in relation to the participant with whom they had interacted immediately following the relationship formation task.
Personnel.
Confederates were trained both to deliver standardized responses to maintain consistency across participants and to act warmly towards participants using a scripted set of verbal and nonverbal behaviors. Confederates were not informed about participants’ diagnostic status. Although there was no formal assessment of whether this blind was maintained, confidence that confederates remained uninformed was increased because the same social interaction procedures were concurrently implemented in different clinical populations as part of other research. Confederates were undergraduate and post-baccalaureate students (age 19–25; 16 women and 3 men) who were not matched to participants on any demographic characteristics. The majority of participants (89.2%) interacted with a female confederate, and this did not differ between the SAD (87.8%) and control groups (91.7 %; Fisher’s exact test = 1.00). Experimenters were undergraduate, post-baccalaureate, or graduate students who were thoroughly trained on the study protocol to deliver scripted instructions to participants.
Confederate Consistency Check.
To evaluate consistency of confederate performance, observers rated confederate behavior while viewing videotapes of the social interaction using five items written to reflect displays of warmth and friendliness (friendly, talkative, disinterested, distant, self-disclosive)6. Items were rated on a 7-point scale with anchors of not at all and very much and were summed to create an overall index of confederate warmth and friendliness (scale range = 5–35; current sample Cronbach’s α = .77). Examination of the observer ratings suggested that confederates adhered to expected levels of warmth and openness (M = 29.63, SD = 1.53)7.
Facial action data acquisition and CERT processing.
Videos were recorded at a rate of 15 frames per second using a Logitech C920 HD Pro webcam. This camera remained within plain sight throughout the relationship formation task and was mounted on top of a desktop computer monitor directly facing participants and immediately behind the left shoulder of confederates. Prior to CERT processing, videos were edited to ensure focus on a given participant’s face, placing a black background over all extraneous content. Given that participants and confederates alternated in the role of speaker and listener within the conversation, time stamps were noted reflecting when participants began and ended turns within each role, and conversational role was mapped to the facial display data.
CERT detects and records FACS action units for each video frame and outputs numeric weights that correspond to the estimated intensity of each action unit. A CERT output value of 0 or greater identifies when an action unit is more likely to be present than absent, with higher values reflecting the presence of more intense emotional expressions. Thus, frequency of smiling was defined as the percentage of total video frames during a specified part of the relationship formation task (either speaking role or listening role) in which CERT output values for both action units 12 and 6 were simultaneously 0 or greater. Frequency of fear displays was defined as percentage of total frames during the specified conversational role in which the single CERT output value for the fear brow action was 0 or greater. Intensity of smiling was defined as the mean output value for action unit 12 averaged across all video frames for a given participant in which both action units 12 and 6 had output values of 0 or greater. Intensity of fear displays was defined as mean output for fear brow across all video frames for a given participant in which fear brow was present at 0 or greater.
Prior to data analysis, eight videos were excluded due to concerns regarding obstacles to accurate facial coding. Selection of videos to exclude were based on visual inspection by an observer blind to diagnostic group and to the hypotheses of the current study, for the following reasons: camera framing errors, such as omitting part of the face (3 participants with SAD), gum chewing (2 participants with SAD; 1 control participant), highly visible tongue movements inside the mouth throughout the video (1 participant with SAD), and hair covering both eyebrows (1 participant with SAD). Of the remaining videos, we included data from all that yielded CERT output for at least 70% of frames over the course of the relationship formation task. Videos from which output was missing for more than 30% of frames were excluded prior to data analyses due to concerns that CERT was not properly registering faces for these videos as a result of unusual video characteristics. This resulted in the exclusion of data from an additional three participants (1 control participant with a brimmed cap casting shadows over the face throughout the video, 1 control participant who gestured with hands on and around the face throughout most of the video, and 1 participant with SAD whose head was turned in profile view throughout most of the video). The remaining 65 videos had substantially lower percentages of video frames for which CERT failed to yield facial expression output (While listening: M = 3.08% of frames with missing output, SD = 5.23; While speaking: M = 5.04% of frames with missing output, SD = 5.04).
Overview of Statistical Analyses.
Analyses were conducted using SPSS version 25. Our first research objective was to compare smiling and fear displays between SAD and control groups, within a relationship-building context. A key consideration in addressing this objective was the enforced turn taking nature of the relationship formation paradigm (described above), which delineates separate, alternating roles of speaker and listener within the conversation, each with different demands relevant to facial expressions. For this reason, and because facial affective displays during listening versus speaking may have different interpersonal impacts (e.g., potentially greater relevance of listening for interpersonal responsiveness; Reis & Shaver, 1988), we incorporated a separate factor to test for any differences related to conversational role. Thus, to address our first research objective, we conducted four analysis of variance (ANOVA) tests, each with one between-groups factor with two levels (Diagnostic status: SAD, control) and one within-groups factor with two levels (Conversational role: speaker, listener), with repeated measurement on the second factor. Frequency and intensity of smiling and fear displays respectively comprised the four dependent variables in these analyses. Arc-sin transformations were applied to frequency data prior to all statistical tests, in order to appropriately adjust the skewness inherent in proportional data (see Sokal & Rohlf, 1981). We confirmed that the data did not violate assumptions of ANOVA. We followed up significant interaction effects with between-group simple main effects tests comparing facial displays within the SAD group versus the control group across conditions of speaking and listening, as well as with paired sample t- tests comparing facial displays between the speaking and listening conditions within each diagnostic group.
Our second objective was to examine the extent to which individual differences in smiling and fear displays during a relationship formation interaction relate to others’ desire for further engagement with the expresser. To address this aim, we used a set of hierarchical regression analyses in the total sample of participants diagnosed with SAD and non-anxious controls to investigate (1) whether the facial displays identified in study aim 1, as differing between the two diagnostic groups, would account for significant variance in others’ desire for future engagement; (2) whether the predicted facial display-DFI relationship would hold when accounting for variance shared with social anxiety symptoms (i.e., LSAS scores entered in step 2 of the regression model); and (3) whether social anxiety severity moderated the facial display- DFI relationship (i.e., LSAS x facial display interaction entered in step 3).8 All continuous predictor variables included in interaction terms were mean centered prior to running the analyses. Checks were performed for violations of regression assumptions (e.g., non-normal distribution of residuals) prior to interpretation. The data did not violate these assumptions.
Results
Demographic and clinical characteristics
Demographic characteristics of the final sample are reported in Table 1. The SAD group was slightly but significantly younger than the control group, M = 23.20, SD = 5.13 and M = 25.75, SD = 4.07, respectively; t(63) = −2.08, p = .04; d = .559. The SAD and control groups did not significantly differ with respect to any other demographic characteristics (all p > .10). The SAD group exhibited elevated symptoms of social anxiety (LSAS, M = 82.78, SD = 15.30), comparable to treatment-seeking samples reported in prior research (e.g., Clark et al., 2006; Rodebaugh et al., 2011), whereas the control group exhibited minimal symptoms of social anxiety (LSAS, M = 9.70, SD = 7.26), and the two groups differed significantly, as expected, t(63) = 25.98, p < .001; d = 6.10. The SAD group exhibited moderate symptoms of depression (BDI-II, M = 17.68, SD = 10.17), the control group exhibited negligible symptoms of depression (BDI-II, M = 2.00, SD = 2.13), and the two groups differed significantly, t(63) = 9.52, p <.001; d = 2.13.
Table 1.
Demographic characteristics
| SAD (n = 41) | Control (n = 24) | |
|---|---|---|
| Mean age (SD) | 23.2 (5.1) | 25.8 (4.1) |
| Gender (% female) | 65.9 | 75.0 |
| Race (N per category)a | ||
| Asian | 13 | 8 |
| White | 19 | 13 |
| Black | 1 | 0 |
| Native American | 1 | 0 |
| More than one race | 4 | 3 |
| Unknown or declined to respond | 2 | 0 |
| Hispanic (N per category) | 13 | 6 |
Note.
For the chi square analysis comparing the racial makeup of the diagnostic groups, we dichotomized the variable of race into white versus other races, given the relatively low frequency of participants within each racial group.
Comparison of facial displays of emotion between SAD and control groups
Smiling.
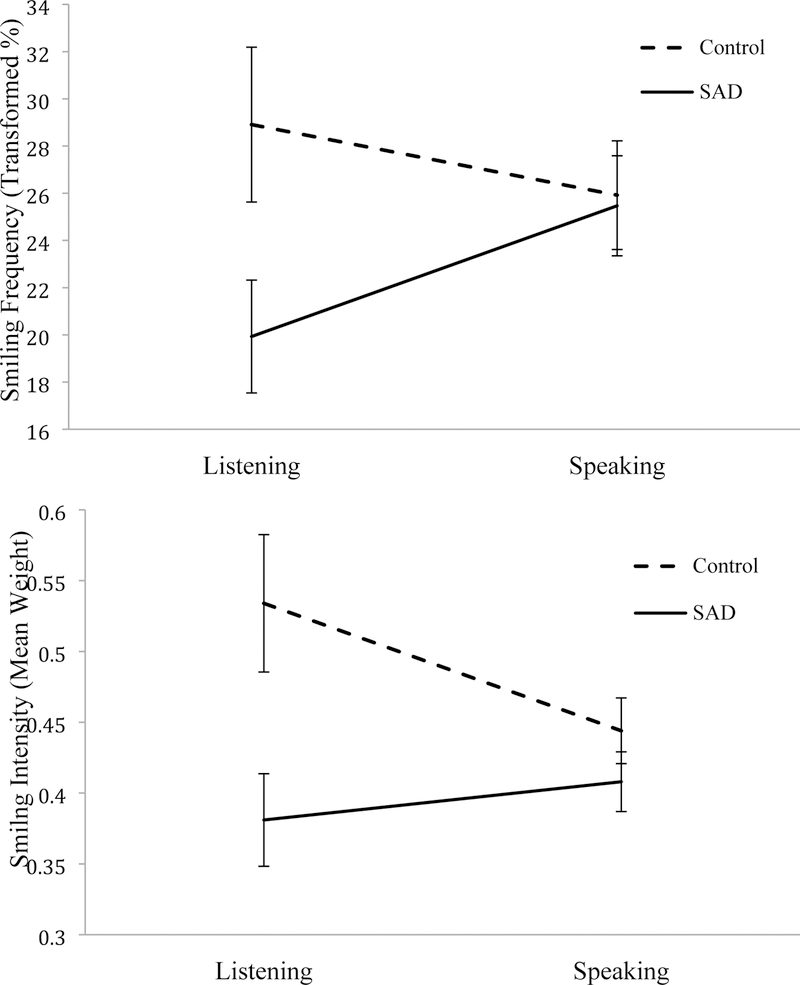
Results revealed significant 2 (Diagnostic status: SAD, control) X 2 (Conversational role: speaker, listener) interactions for both frequency and intensity of smiling, F(1, 63) = 9.41, p = .003, ηp 2 = .13 and F(1, 63) = 8.84, p = .004, ηp 2 = .12, respectively (see Figure 1). Simple main effects tests within the listening role alone revealed that those in the SAD group displayed less frequent smiling, t(63) = −2.24, p = .03; d = .57 and lower intensity smiling, t(63) = −2.87, p = .006; d =.72 than those in the control group. No significant group differences were found within the speaking role for either frequency, t(63) = −.14, p = .89, d = .04 or intensity, t(63) = −1.03, p = .31, d = .27.
Figure 1.
Interaction between diagnostic status (SAD vs. control) and conversational role (listening vs. speaking) as related to frequency of smiling (top) and intensity of smiling (bottom).
Within the SAD group, participants smiled less frequently while listening than while speaking, t(1, 40) = −3.46, p = .001. The intensity of their smiling did not differ across these two conversational roles, t(1, 40) = −1.07, p = .29. Within the control group, participants smiled more intensely while listening than while speaking t(1, 23) = 2.80, p = .01. The frequency of their smiling did not differ by conversational role, t(1, 23) = 1.25, p = .22.
It is possible that depression has an impact on facial displays by blunting positive affect. In the current sample, social anxiety and depression were highly correlated, making it impossible to fully disentangle the effects of social anxiety and depression on outcomes of interest.10 However, we conducted a sensitivity analysis to test whether depression symptoms moderated the relationship between diagnostic group and smiling. Social anxiety (diagnostic group), depression (BDI-II total score), and the interaction between social anxiety and depression were tested as predictors of smiling frequency and intensity using repeated measures general linear models, where speaking condition was a within-subjects factor. No significant effects of depression were found. Specifically, there was no main effect of depression on smile frequency, F(1, 61) = .12, p = .74, ηp 2 = .002 or intensity F(1, 61) = .15, p = .70, ηp 2 = .002, and nor were there 2-way interaction effects between depression and speaking condition on smiling (smile frequency: F(1, 61) = .34, p = .56, ηp 2 = .006; smile intensity: F(1, 61) = .033, p = .86, ηp 2 = .001), nor 3-way interaction effects between depression, social anxiety, and speaking condition (smile frequency: F(1, 61) < .001, p = .99, ηp 2 < .001; smile intensity, F(1, 61) = .200, p = .66, ηp 2 = .003).11
We also conducted a sensitivity analysis to test whether participant gender moderated the diagnostic group-by-role relationship. The 2 (Diagnostic status: SAD, control) X 2 (Conversational role: speaker, listener) X 2 (Participant gender: male, female) ANOVA revealed no significant effects of participant gender. There was no main effect of gender on smile frequency, F(1, 61) = 3.13, p = .082, ηp2 = .049 or intensity F(1, 61) = .024, p = .88, ηp2 < .001, and nor were there 2-way interaction effects between gender and speaking condition on smiling (smile frequency: F(1, 61) = .074, p = .79, ηp 2 = .001; smile intensity: F(1, 61) = 1.62, p = .21, ηp 2 = .026), nor 3-way interaction effects between gender, diagnostic status, and speaking condition (smile frequency: F(1, 61) = .16, p = .70, ηp2 = .003; smile intensity, F(1, 61) = .76, p = .39, ηp 2 = .012).11,12
Fear displays.
Counter to predictions, there were no instances of fear displays that occurred above threshold levels for any participant within either the SAD group or the control group. Thus, no further analyses were conducted related to fear displays.
Relationships between smiling while listening and others’ DFI
Results of the regression analyses revealed that lower participant smiling while listening was associated with lower DFI, for both smile frequency, β = .33, t(63) = 2.74, p = .008 and intensity, β = .36, t(62) = 3.02, p = .004. When controlling for social anxiety severity, low intensity of smiling while listening continued to be significantly associated with low DFI, β = .25, t(62) = 2.06, p = .044. The relationship between DFI and smile frequency was at a trend level, β = .23, t(62) = 1.96, p = .054. The interaction between smiling and LSAS was not related to DFI for smile frequency, β = .024, t(61) = .21, p = .83 or intensity, β = .053, t(61) = .47, p = .64, suggesting that social anxiety severity did not moderate the relationship between smiling and DFI.13,14
Discussion
While no fear displays were observed in either the SAD or control group, the SAD group displayed both lower frequency and intensity of smiling during a relationship formation encounter. These group differences emerged specifically during the listening portions of the interaction, and lower smile frequency and intensity while listening were associated with others’lower desire for future interaction. The current findings both add to a body of research supporting an important role of facial displays in relationship building and suggest that atypical patterns of positive displays may be implicated in relational impairments experienced by those with SAD.
There are several possible explanations for low smiling in SAD. One possibility is that lower expressed positive affect may reflect lower felt emotional experience. This hypothesis is consistent with findings that individuals with SAD tend to experience low positive affect within social situations and often report chronically low positive affect more broadly compared with non-clinical populations (see Gilboa-Schechtman, et al., 2014 for a review). However, facial displays do not always serve as a window into felt emotion (Crivelli & Fridlund, 2018; Lanteigne, Eastabrook, & Hollenstein, 2014; Mauss, Levenson, McCarter, Wilhelm, & Gross, 2005). Another possibility is that differences in expression could be driven by physiological processes (as has been investigated in other clinical populations, e.g. flat affect in schizophrenia; Gur et al., 2007) or by expressive suppression, a common emotion regulation strategy used by individuals with SAD (Kivity & Huppert, 2018; Spokas, Luterek, & Heimberg, 2009). Future research could test the influence of expressive suppression on smiling in SAD by experimentally reducing use of this emotion regulation strategy and assessing resulting facial displays.
Smiling behavior was lower in participants with SAD specifically during their listening turns. This finding could suggest that individuals with SAD experience lower positive affect during these portions of social interactions, potentially due to greater opportunity to focus attention on feared social outcomes. Alternatively, differences in smiling behavior may be driven by a tendency among non-anxious individuals to volitionally increase their level of smiling during listening turns in order to convey interpersonal responsiveness to their partners. Those with SAD may not intentionally increase smiling behavior to the same extent either due to differences in social skill, attentional resources, self-monitoring tendencies, and/or engagement in self-protective (safety) behaviors. Future research could investigate these hypotheses, for example by experimentally manipulating engagement in safety behaviors during a social interaction and testing the impact on facial displays.
The link between others’ motivation to affiliate with participants and participant smiling in the listening condition per se is consistent with existing evidence that interpersonally responsive behaviors are particularly important for relationship building (Davis & Perkowitz, 1979; Fehr, 2008; Reis & Shaver, 1988). Previous literature also suggests that smiling promotes the formation of positive impressions more broadly (Knutson, 1996; Otta, Abrosio, & Hoshino, 1996; Reis et al., 1990). In contrast, repeated missed opportunities to engage in smiling and other responsive behaviors may lead to less positive partner perceptions and may signal low interest in or regard for the interaction partner, who then may be less willing to sustain the interaction or to initiate future contact. The current findings suggest this may be one candidate pathway to relational impairment in SAD. Reduced breadth and depth of social relationships in turn may limit the opportunities of those diagnosed with SAD to use interpersonal emotion regulation strategies adaptively (e.g., to seek out the company and/or desired responses of supportive others; see Hofmann, 2014 for a review). Impairments in social relationship functioning in conjunction with potential narrowing of the emotion regulation strategy repertoire may be a factor implicated in the maintenance of SAD.
Counter to study predictions, the SAD group did not differ from the control group in facial expressions of fear; rather, neither group displayed above-threshold fear displays during the conversation. One interpretation of this finding is that, in spite of experiencing negative affect within social contexts, those diagnosed with SAD may not tend to express this negative affect in detectible facial displays (and perhaps express it in other ways instead, e.g. via postural cues; Aviezer, Trope, & Todorov, 2012). It is also possible that the relationship formation task employed in this study, which was designed to elicit social connectedness and positive affect (Aron et al., 1997), may be an atypically positive social encounter and thus may not induce negative affect at high enough intensities to result in fear displays. Although fear brow was previously observed while participants verbally recounted an anxiety-provoking past event (Harrigan & O’Connell, 1996), it may be less likely to arise in response to the mild levels of fear aroused during positive, low risk social contexts.
The current findings may inform treatment strategies to enhance interpersonal outcomes for those with SAD. It may be beneficial if treatment procedures discussed how interaction partners tend to interpret nonverbal feedback (including facial expressions) they receive, and then encourage ways for patients to experiment with sending more positive interpersonal messages (e.g., safety behavior reduction). Consistent with this proposal, increasing evidence suggests that incorporating such relational treatment strategies into contemporary treatment regimens may be valuable (Alden, Buhr, Robichaud, Trew, & Plasencia, 2018; Alden & Taylor, 2011). Alternatively, treatments may achieve positive relational outcomes by increasing internally experienced positive affect (e.g., Alden & Trew, 2013; Layous, Chancellor, & Lyubomirsky, 2014; Taylor, Lyubomirsky, & Stein, 2017). By shifting focus toward positive aspects of social experiences and approach goals (Gable, 2006), perhaps facial displays of emotion would also spontaneously shift closer to patterns displayed by non-anxious populations. In addition to investigating how facial displays may inform intervention strategies, future studies could also examine whether changes in facial displays may serve as a sensitive behavioral marker of treatment response.
Several limitations of the current study remain to be addressed by future research. The structured nature of the task required participants to take turns answering questions with clearly delineated roles of listener versus speaker and with affiliation ratings provided by confederates. Although this afforded increased internal validity by standardizing the social context across participants, it may be beneficial for future research to characterize facial affect in individuals with SAD within more naturalistic interpersonal interactions. It would also be useful to extend the research to other cultural contexts, since research suggests that facial display rules and interpretations may differ depending on culture (Gendron et al., 2013) and gender (e.g., Wilhelm et al., 2017), and to extend it to other types of interactions, such as interactions with individuals who have a wider variety of interpersonal styles (e.g., lower warmth and friendliness), or interactions that may be more fear-provoking (e.g., conflict-based interactions). Future research could also measure additional negative affect displays (e.g., sadness, anger), could compare their incidence within different clinical populations, and could investigate the relationship between facial displays and internally experienced affect and affiliation processes.
The current research was intended to model processes relevant to new friendship development; interactions between pre-existing social relationship partners may involve different processes and outcomes (Rodebaugh et al., 2014; Rodebaugh, Lim, Shumaker, Levinson, & Thompson, 2015). In addition, since the current research did not assess confederates’ facial displays, it was not possible to distinguish whether associations between participant facial displays and others’ desire for future interaction were related to smiling while listening in general or to reciprocity of smiling in particular (as suggested by Heerey & Kring, 2007); this will be an important area for future work. Additionally, facial expressions were not experimentally manipulated in the current study; thus, although a statistical relationship was found between positive facial displays and subsequent confederate reactions, causal relationships cannot be inferred based on these findings alone. Experimental manipulations intended to induce differential facial displays would offer stronger evidence to support positive facial displays as a causal process underlying social relationship impairments characteristic of SAD. Finally, while the high rate of depression symptoms within the SAD group was representative of the SAD- diagnosed population at large (Schneier, Johnson, Hornig, Liebowitz, & Weissman, 1992; Magee, Eaton, Wittchen, McGonagle, & Kessler, 1996), and while depression symptoms did not appear to impact facial expressions within the current sample, future research could aid in disentangling unique effects of SAD versus depression by testing comparison groups of individuals who meet criteria for SAD alone and major depressive disorder alone.
The above limitations notwithstanding, the current findings are the outcome of important methodological advancements, building upon prior work by incorporating a standardized, face- to-face interpersonal task, by testing facial displays during listening and speaking separately, by testing within a clinically diagnosed sample, and by applying a validated approach to the study of facial displays of emotion. The findings support the notion that facial displays of emotion are an important area for further research. Investigating them may not only aid in understanding the interpersonal ecology that maintains SAD, but also may inform intervention targets and strategies across a wide range of psychopathology characterized by interpersonal impairment, thus promoting transdiagnostic enhancement of social connection.
Supplementary Material
Acknowledgements
We would like to thank the many individuals who helped make this research possible: Marni Bartlett, Gwen Littlewort, Crane Huang, and Abraham Bae for their invaluable assistance with CERT and facial expression processing; Taylor Smith and Sarah Dowling for conducting diagnostic interviews and overseeing project management; Karalani Cross for overseeing project management; as well as Jennifer Alcalde, Gabby Arellano, Nora Asi, Ethan Averbukh, Gina Belli, Carl Bolano, Maya Bunyan, Kevin Carlis, Michelle Chang, Joanna Chen, Melody Chen, Lina Choi, Christina Cui, Vivi Dang, Teji Dulai, Allison Endo, Brooke Engel, Angelica Estrada, Jessica Foster, Ari Goodman, Tina Hua, Ira Hyun, Alyson Johnson, Sanskruti Kakaria, Sarah Knapp, Sarah Kouzi, Stephanie Lee, Mercy Lopez, Deborah May, Natasha Nowicka, Katherine Padilla, Marisa Padilla, Gregory Pak, Alisha Patel, Melissa Perez-Ruan, Katherine Price, Shayna Quach, Jasmine Rai, Atiyeh Samadi, Katherine Socha, Rachel Storer, Aaron Tay, Sarah Tran, Charles Vigilia, and Stephanie Zepeda for their help with recruitment, screening, data collection, and data management.
Funding: This work was supported by a grant awarded to Charles T. Taylor from the National Institute of Mental Health R00MH090243.
Footnotes
Conflict of Interest: Sarah L. Pearlstein declares no conflicts of interest. Charles T. Taylor declares that in the past three years he has been a paid consultant for Homewood Health and receives payment for editorial work for UpToDate. Murray B. Stein declares that he has in the past three years been a consultant for Actelion, Aptinyx, Bionomics, Dart Neuroscience, Healthcare Management Technologies, Janssen, Neurocrine Biosciences, Oxeia Biopharmaceuticals, Pfizer, and Resilience Therapeutics; he also receives payment for editorial work for UpToDate and the journals Biological Psychiatry and Depression and Anxiety.
Footnotes
Enrollment began prior to the release of the SCID for DSM-5. Interview questions were subsequently scored to reflect DSM-5 criteria for SAD.
Because enrollment began prior to the release of MINI Version 7.0.0 for DSM-5, 30 participants were administered MINI Version 5.0.0 for DSM-IV (SAD group: 18, control group: 12) and 35 participants were administered the MINI 7.0.0 for DSM-5 (SAD group: 23, control group: 12) to assess comorbid diagnoses.
We conducted a sensitivity analysis wherein we repeated the main analyses using only AU12 as our marker of smiling (without concurrent activation of AU6). Results revealed an identical pattern of significant findings to those reported in the main text.
We ran sensitivity analyses using DFI ratings provided by confederates alone. The pattern of findings was the same as those reported in the main text using the mean observer DFI index. Lower participant smiling while listening was associated with lower confederate DFI, for both smile frequency, β = .31, t(63) = 2.54, p = .013 and intensity, β = .32, t(63) = 2.67, p = .010. However, the strength of the relationships was attenuated when LSAS was also included in the model (smile frequency: β = .20, t(62) = 1.72, p = .090; smile intensity: β = .20, t(62) = 1.65, p = .10).
Due to the design of the larger treatment study of which this research was a part, participants were randomized to use one of two parallel question sets, A and B. Within the SAD group 22 participants used Set A and 19 participants used Set B; within the control group 13 participants used Set A and 11 participants used Set B. Use of question set A versus B did not differ between the SAD and control groups (Fisher’s exact test = 1.00).
Confederate behavior from one interaction with a control participant was not rated due to technical difficulties with the videotape that muted the sound.
Confederates who interacted with control participants scored slightly but significantly higher on this metric than those who interacted with participants with SAD, t(63) = −3.04, p = .003 (SAD group: M = 29.21, SD = 1.46; control group: M = 30.33, SD = 1.40). However, confederate behavior was not significantly related to any participant facial display outcome (all p > .10), and the pattern of findings remained the same for all main analyses when including confederate behavior as a covariate (i.e., all significant facial display related findings remained significant).
We thank the anonymous reviewer who suggested this analytic approach.
We conducted a sensitivity analysis for our main outcome variables in which participant age was included as a covariate. Results revealed that participant age did not account for group differences observed across the main outcome indices, and thus this variable was subsequently dropped from analyses.
The point-biserial correlation between diagnostic group and BDI-II scores was rpb(65) = .69, p < .001. Results of the sensitivity analysis including BDI-II scores should therefore be interpreted with caution.
These analyses were conducted following feedback received from reviewers in response to an earlier draft of this article.
At the request of an anonymous reviewer, we conducted a sensitivity analysis to test whether the match between participant and confederate gender moderated the relationship between diagnostic group and conversational role in predicting smile frequency and intensity. The 3-way interaction including gender match within the dyad was not significant for smile frequency, F(1, 61) = .21, p = .65, ηp2 = .003 or intensity, F(1, 61) = 1.63, p = .21, ηp2 = .03).
We re-ran the regression analyses using diagnostic status (SAD diagnosis versus non-anxious control) as the indicator of social anxiety rather than continuous LSAS score, first dummy coding the diagnostic status variable (+1/2 and −1/2) and ensuring there were no violations of regression assumptions. The same pattern of findings emerged, except that the relationship between smile frequency and DFI remained significant when controlling for social anxiety status. That is, when controlling for diagnostic status, both intensity, β = .27, t(62) = 2.19, p = and frequency, β = .25, t(62) = 2.09, p = .041 of smiling while listening continued to be associated with DFI. The interaction between smiling and diagnostic status was not related to DFI for smile frequency, β = −.006, t(61) = −.049, p = .96 or intensity β = .046, t(61) = .40, p = .69.
At the request of an anonymous reviewer, we conducted exploratory analyses to investigate the temporal dynamics of smiling. To investigate whether changes in smiling over time were different between diagnostic groups and whether this was associated with partner DFI, we calculated the slopes of smiling during the listening condition over the course of the interaction. These slopes did not differ between groups for either smiling frequency, t(61) = −.67, p = .51 or intensity, t(61) = −.98, p = .33, and did not correlate with partner DFI for smile frequency, r(63) = −.07, p =.57 or intensity, r(63) = .14, p =.28.
References
- aan het Rot M, Enea V, Dafinoiu I, Iancu S, Taftă SA, & Bărbuşelu M (2017). Behavioural responses to facial and postural expressions of emotion: An interpersonal circumplex approach. British Journal of Psychology, 108(4), 797–811. doi: 10.1111/bjop.12247 [DOI] [PubMed] [Google Scholar]
- Alden LE, Buhr K, Robichaud M, Trew JL, & Plasencia ML (2018). Treatment of social approach processes in adults with social anxiety disorder. Journal of Consulting and Clinical Psychology, 86(6), 505–517. doi:/ 10.1037/ccp0000306 [DOI] [PubMed] [Google Scholar]
- Alden LE, & Taylor CT (2004). Interpersonal processes in social phobia. Clinical Psychology Review, 24(7), 857–882. doi: 10.1016/j.cpr.2004.07.006 [DOI] [PubMed] [Google Scholar]
- Alden LE, & Taylor CT (2010). Interpersonal processes in social anxiety disorder. In Beck J (Ed.), Interpersonal processes in the anxiety disorders: Implications for understanding psychopathology and treatment (pp. 125–152). Washington, DC: American Psychological Association. [Google Scholar]
- Alden LE, & Taylor CT (2011). Relational treatment strategies increase social approach behaviors in patients with generalized social anxiety disorder. Journal of Anxiety Disorders, 25(3), 309–318. doi: 10.1016/j.janxdis.2010.10.003 [DOI] [PubMed] [Google Scholar]
- Alden LE, & Trew JL (2013). If it makes you happy: Engaging in kind acts increases positive affect in socially anxious individuals. Emotion, 13(1), 64–75. [DOI] [PubMed] [Google Scholar]
- Ambadar Z, Cohn JF, & Reed LI (2009). All smiles are not created equal: Morphology and timing of smiles perceived as amused, polite, and embarrassed/nervous. Journal of Nonverbal Behavior, 33(1), 17–34. doi: 10.1007/s10919-008-0059-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR Washington, DC: American Psychiatric Association. [Google Scholar]
- Aron A, Melinat E, Aron EN, Vallone RD, & Bator RJ (1997). The experimental generation of interpersonal closeness: A procedure and some preliminary findings. Personality and Social Psychology Bulletin, 23(4), 363–377. doi: 10.1177/0146167297234003 [DOI] [Google Scholar]
- Aviezer H, Trope Y, & Todorov A (2012). Body cues, not facial expressions, discriminate between intense positive and negative emotions. Science, 338(6111), 1225–1229. doi: 10.1126/science.1224313. [DOI] [PubMed] [Google Scholar]
- Baker SR, & Edelmann RJ (2002). Is social phobia related to lack of social skills? Duration of skill-related behaviours and ratings of behavioural adequacy. British Journal of Clinical Psychology, 41(3), 243–257. doi: 10.1348/014466502760379118 [DOI] [PubMed] [Google Scholar]
- Barlow DH (Ed.). (2014). Clinical handbook of psychological disorders: A step-by-step treatment manual New York, NY: Guilford Publications. [Google Scholar]
- Bartlett MS, Littlewort GC, Frank MG, & Lee K (2014). Automatic decoding of facial movements reveals deceptive pain expressions. Current Biology, 24(7), 738–743. doi: 10.1016/j.cub.2014.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett M, Littlewort G, Vural E, Whitehill J, Wu T, Lee K, & Movellan J (2010). Insights on spontaneous facial expressions from automatic expression measurement. In Curio C, Bülthoff HH, & Giese MA (Eds.), Dynamic faces: Insights from experiments and computation (pp. 211–238). Cambridge, MA: MIT Press. doi: 10.7551/mitpress/9780262014533.003.0015 [DOI] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for Beck Depression Inventory-II San Antonio, TX: Psychological Corporation. [Google Scholar]
- Blair RJR (2003). Facial expressions, their communicatory functions and neuro–cognitive substrates. Philosophical Transactions of the Royal Society B: Biological Sciences, 358(1431), 561–572. doi: 10.1098/rstb.2002.1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DM, Ehlers A, Hackmann A, McManus F, Fennell M, Grey N, … Wild J (2006). Cognitive therapy versus exposure and applied relaxation in social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 74(3), 568–578. doi: 10.1037/0022-006X.74.3.568 [DOI] [PubMed] [Google Scholar]
- Coyne JC (1976). Depression and the response of others. Journal of Abnormal Psychology, 85(2), 186–193. doi: 10.1037/0021-843X.85.2.186 [DOI] [PubMed] [Google Scholar]
- Crivelli C, & Fridlund AJ (2018). Facial displays are tools for social influence. Trends in Cognitive Sciences, 22(5), 388–399. doi: 10.1016/j.tics.2018.02.006 [DOI] [PubMed] [Google Scholar]
- Davies H, Wolz I, Leppanen J, Fernandez-Aranda F, Schmidt U, & Tchanturia K (2016). Facial expression to emotional stimuli in non-psychotic disorders: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 64, 252–271. doi: 10.1016/j.neubiorev.2016.02.015 [DOI] [PubMed] [Google Scholar]
- Davis D, & Perkowitz WT (1979). Consequences of responsiveness in dyadic interaction: Effects of probability of response and proportion of content-related responses on interpersonal attraction. Journal of Personality and Social Psychology, 37(4), 534–550. doi: 10.1037/0022-3514.37.4.534 [DOI] [Google Scholar]
- Dozois DJ, Dobson KS, & Ahnberg JL (1998). A psychometric evaluation of the Beck Depression Inventory–II. Psychological Assessment, 10(2), 83–89. [Google Scholar]
- Ekman P, Davidson RJ, & Friesen WV (1990). The Duchenne smile: Emotional expression and brain physiology: II. Journal of Personality and Social Psychology, 58(2), 342–353. [PubMed] [Google Scholar]
- Ekman P, & Friesen WV (1978). Manual for the facial action coding system Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Ekman P, Freisen WV, & Ancoli S (1980). Facial signs of emotional experience. Journal of Personality and Social Psychology, 39(6), 1125–1134. doi: 10.1037/h0077722 [DOI] [Google Scholar]
- Fairbairn CE, Sayette MA, Aalen OO, & Frigessi A (2015). Alcohol and emotional contagion: An examination of the spreading of smiles in male and female drinking groups. Clinical Psychological Science, 3(5), 686–701. doi: 10.1177/2167702614548892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehr B (2008). Friendship formation. In Sprecher S, Wenzel A, & Harvey J (Eds.), Handbook of relationship initiation (pp. 29–54). New York, NY: Psychology Press, Taylor & Francis Group [Google Scholar]
- First MB, Spitzer RL, Gibbon MWJB, & Williams JB (1995). Structured Clinical Interview for DSM-IV Axis I disorders New York: New York State Psychiatric Institute. [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, & Goetz D (2001). The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine, 31(6), 1025–1035. doi: 10.1017/S0033291701004056 [DOI] [PubMed] [Google Scholar]
- Furl N, Gallagher S, & Averbeck BB (2012). A selective emotional decision-making bias elicited by facial expressions. PLoS ONE, 7(3): e33461. doi: 10.1371/journal.pone.0033461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gable SL (2006). Approach and avoidance social motives and goals. Journal of Personality, 74(1), 175–222. doi: 10.1111/j.1467-6494.2005.00373.x [DOI] [PubMed] [Google Scholar]
- Gendron M, Lindquist KA, Barsalou L, & Barrett LF (2012). Emotion words shape emotion percepts. Emotion, 12(2), 314–325. doi: 10.1037/a0026007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gendron M, Roberson D, van der Vyver JM, & Barrett LF (2014). Perceptions of emotion from facial expressions are not culturally universal: Evidence from a remote culture. Emotion, 14(2), 251–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilboa-Schechtman E, Shachar I, & Sahar Y (2014). Positivity impairment as a broad-based feature of social anxiety. In Weeks JW (Ed.), The Wiley Blackwell Handbook of Social Anxiety Disorder (409–432). John Wiley & Sons, Ltd. doi: 10.1002/9781118653920.ch19/summary [DOI] [Google Scholar]
- Girard JM, Cohn JF, Mahoor MH, Mavadati S, & Rosenwald DP (2013, April). Social risk and depression: Evidence from manual and automatic facial expression analysis. In Automatic Face and Gesture Recognition (FG), 2013 10th IEEE International Conference and Workshops on (1–8) IEEE. doi: 10.1109/FG.2013.6553748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottman J, Levenson R, & Woodin E (2001). Facial expressions during marital conflict. Journal of Family Communication, 1(1), 37–57. doi: 10.1207/S15327698JFC0101_06 [DOI] [Google Scholar]
- Gur RE, Loughead J, Kohler CG, Elliott MA, Lesko K, Ruparel K,& Gur RC (2007). Limbic activation associated with misidentification of fearful faces and flat affect in schizophrenia. Archives of General Psychiatry, 64(12), 1356–1366. doi: 10.1001/archpsyc.64.12.1356 [DOI] [PubMed] [Google Scholar]
- Harrigan JA, & O’Connell DM (1996). How do you look when feeling anxious? Facial displays of anxiety. Personality and Individual Differences, 21(2), 205–212. doi: 10.1016/0191-8869(96)00050-5 [DOI] [Google Scholar]
- Heerey EA, & Kring AM (2007). Interpersonal consequences of social anxiety. Journal of Abnormal Psychology, 116(1), 125–134. doi: 10.1037/0021-843X.116.1.125 [DOI] [PubMed] [Google Scholar]
- Hofmann SG (2014). Interpersonal emotion regulation model of mood and anxiety disorders. Cognitive Therapy and Research, 38(5), 483–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, & Roberts JE (2006). Affective outcomes in superficial and intimate interactions: Roles of social anxiety and curiosity. Journal of Research in Personality, 40(2), 140–167. doi: 10.1016/j.jrp.2004.10.005 [DOI] [Google Scholar]
- Kashdan TB, Weeks JW, & Savostyanova AA (2011). Whether, how, and when social anxiety shapes positive experiences and events: A self-regulatory framework and treatment implications. Clinical Psychology Review, 31(5), 786–799. doi: 10.1016/j.cpr.2011.03.012 [DOI] [PubMed] [Google Scholar]
- Keltner D, & Kring AM (1998). Emotion, social function, and psychopathology. Review of General Psychology, 2(3), 320–342. [Google Scholar]
- Kim HS, & Sasaki JY (2014). Cultural neuroscience: Biology of the mind in cultural contexts. Annual Review of Psychology, 65(1), 487–514. doi: 10.1146/annurev-psych-010213-115040 [DOI] [PubMed] [Google Scholar]
- Kivity Y, & Huppert JD (2018). Are individuals diagnosed with social anxiety disorder successful in regulating their emotions? A mixed-method investigation using self-report, subjective, and event-related potentials measures. Journal of Affective Disorders, 236, 298–305. doi: 10.1016/j.jad.2018.02.029 [DOI] [PubMed] [Google Scholar]
- Kitayama S, & Uskul AK (2011). Culture, mind, and the brain: Current evidence and future directions. Annual Review of Psychology, 62(1), 419–449. doi: 10.1146/annurev-psych-120709-145357 [DOI] [PubMed] [Google Scholar]
- Knutson B (1996). Facial expressions of emotion influence interpersonal trait inferences. Journal of Nonverbal Behavior, 20(3), 165–182. doi: 10.1007/BF02281954 [DOI] [Google Scholar]
- Lanteigne DM, Flynn JJ, Eastabrook JM, & Hollenstein T (2014). Discordant patterns among emotional experience, arousal, and expression in adolescence: Relations with emotion regulation and internalizing problems. Canadian Journal of Behavioural Science, 46(1), 29–39. doi: 10.1037/a0029968 [DOI] [Google Scholar]
- Layous K, Chancellor J, & Lyubomirsky S (2014). Positive activities as protective factors against mental health conditions. Journal of Abnormal Psychology, 123(1), 3–12. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR (1987). Social phobia. Modern Problems in Pharmacopsychiatry, 22, 141–173. [DOI] [PubMed] [Google Scholar]
- Littlewort G, Whitehill J, Wu T, Fasel I, Frank M, Movellan J, & Bartlett M (2011). The Computer Expression Recognition Toolbox (CERT). Face and Gesture 2011, 298–305. doi: 10.1109/FG.2011.5771414 [DOI] [Google Scholar]
- Lobbestael J, Leurgans M, & Arntz A (2011). Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I disorders (SCID I) and Axis II disorders (SCID II). Clinical Psychology & Psychotherapy, 18(1), 75–79. doi: 10.1002/cpp.693 [DOI] [PubMed] [Google Scholar]
- Magee W, Eaton W, Wittchen HU, McGonagle KA, & Kessler RC (1996). Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Archives of General Psychiatry, 53(2), 159–168. doi: 10.1001/archpsyc.1996.01830020077009 [DOI] [PubMed] [Google Scholar]
- Mauss IB, Levenson RW, McCarter L, Wilhelm FH, & Gross JJ (2005). The tie that binds? Coherence among emotion experience, behavior, and physiology. Emotion, 5(2), 175–190. doi: 10.1037/1528-3542.5.2.175 [DOI] [PubMed] [Google Scholar]
- Meleshko KG, & Alden LE (1993). Anxiety and self-disclosure: Toward a motivational model. Journal of Personality and Social Psychology, 64(6), 1000–1009. [DOI] [PubMed] [Google Scholar]
- Otta E, Abrosio FFE, & Hoshino RL (1996). Reading a smiling face: Messages conveyed by various forms of smiling. Perceptual and Motor Skills, 82(3), 1111–1121. doi: 10.2466/pms.1996.82.3c.1111 [DOI] [PubMed] [Google Scholar]
- Olsson A, Nearing KI, & Phelps EA (2007). Learning fears by observing others: The neural systems of social fear transmission. Social Cognitive and Affective Neuroscience, 2(1), 3–11. doi: 10.1093/scan/nsm005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsson A, & Phelps EA (2004). Learned fear of “unseen” faces after Pavlovian, observational, and instructed fear. Psychological Science, 15(12), 822–828. doi: 10.1111/j.0956-7976.2004.00762.x [DOI] [PubMed] [Google Scholar]
- Palmer MT, & Simmons KB (1995). Communicating intentions through nonverbal behaviors conscious and nonconscious encoding of liking. Human Communication Research, 22(1), 128–160. doi: 10.1111/j.1468-2958.1995.tb00364.x [DOI] [Google Scholar]
- Powers TA, & Zuroff DC (1988). Interpersonal consequences of overt self-criticism: A comparison with neutral and self-enhancing presentations of self. Journal of Personality and Social Psychology, 54(6), 1054–1062. doi: 10.1037/0022-3514.54.6.1054 [DOI] [Google Scholar]
- Reis HT & Shaver P (1988). Intimacy as an interpersonal process. In Duck SW (Ed.), Handbook of Personal Relationships, 24(3), 367–389. Retrieved from: http://depts.washington.edu/uwcssc/sites/default/files/Reis%20%26%20Shaver,%201988.pdf [Google Scholar]
- Reis HT, Wilson IM, Monestere C, Bernstein S, Clark K, Seidl E, … Radoane K (1990). What is smiling is beautiful and good. European Journal of Social Psychology, 20(3), 259–267. doi: 10.1002/ejsp.2420200307 [DOI] [Google Scholar]
- Rodebaugh TL (2009). Social phobia and perceived friendship quality. Journal of Anxiety Disorders, 23(7), 872–878. doi: 10.1016/j.janxdis.2009.05.001 [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Heimberg RG, Brown PJ, Fernandez KC, Blanco C, Schneier FR, & Liebowitz MR (2011). More reasons to be straightforward: Findings and norms for two scales relevant to social anxiety. Journal of Anxiety Disorders, 25(5), 623–630. doi: 10.1016/j.janxdis.2011.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodebaugh TL, Lim MH, Fernandez KC, Langer JK, Weisman JS, Tonge N,& Shumaker EA (2014). Self and friend’s differing views of social anxiety disorder’s effects on friendships. Journal of Abnormal Psychology, 123(4), 715–724. doi: 10.1037/abn0000015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodebaugh TL, Lim MH, Shumaker EA, Levinson CA, & Thompson T (2015). Social anxiety and friendship quality over time. Cognitive Behaviour Therapy, 44(6), 502–511. doi: 10.1080/16506073.2015.1062043 [DOI] [PubMed] [Google Scholar]
- Schneier FR, Heckelman LR, Garfinkel R, Campeas R, A, B., Gitow A, … R, M. (1994). Functional impairment in social phobia. Journal of Clinical Psychiatry, 55(8), 322–331. [PubMed] [Google Scholar]
- Schneier FR, Johnson J, Hornig CD, Liebowitz MR, & Weissman MM (1992). Social phobia: Comorbidity and morbidity in an epidemiologic sample. Archives of General Psychiatry, 49(4), 282–288. doi: 10.1001/archpsyc.1992.01820040034004 [DOI] [PubMed] [Google Scholar]
- Schrammel F, Pannasch S, Graupner S-T, Mojzisch A, & Velichkovsky BM (2009). Virtual friend or threat? The effects of facial expression and gaze interaction on psychophysiological responses and emotional experience. Psychophysiology, 46(5), 922–931. doi: 10.1111/j.1469-8986.2009.00831.x [DOI] [PubMed] [Google Scholar]
- Segrin C (1993). Interpersonal reactions to dysphoria: The role of relationship with partner and perceptions of rejection. Journal of Social and Personal Relationships, 10(1), 83–97. doi: 10.1177/0265407593101006 [DOI] [Google Scholar]
- Segrin C (2001). Interpersonal processes in psychological problems New York, NY: Guilford Press. [Google Scholar]
- Sheehan D, Janavs J, Baker R, Sheehan KH, Knapp E, & Sheehan M (2015). Mini International Neuropsychiatric Interview–Version 7.0.0 DSM-5
- Sheehan DV, Lecrubie Y, Sheehan KH, Amorim P, Janavs J, Weiller MS, Hergueta T, … & Dunbar GC (1998). The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. Journal of Clinical Psychiatry, 59, 22–33. [PubMed] [Google Scholar]
- Sokal RR, & Rohlf FJ (1981). Biometry San Francisco, CA: WH Freeman and Company. [Google Scholar]
- Spokas M, Luterek JA, & Heimberg RG (2009). Social anxiety and emotional suppression: The mediating role of beliefs. Journal of Behavior Therapy and Experimental Psychiatry, 40(2), 283–291. doi: 10.1016/j.jbtep.2008.12.004 [DOI] [PubMed] [Google Scholar]
- Taylor CT, & Amir N (2012). Modifying automatic approach action tendencies in individuals with elevated social anxiety symptoms. Behaviour Research and Therapy, 50(9), 529–536. doi: 10.1016/j.brat.2012.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CT, Lyubomirsky S, & Stein MB (2017). Upregulating the positive affect system in anxiety and depression: Outcomes of a positive activity intervention. Depression and Anxiety, 34(3), 267–280. doi: 10.1002/da.22593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CT, Pearlstein SL, & Stein MB (2017). The affective tie that binds: Examining the contribution of positive emotions and anxiety to relationship formation in social anxiety disorder. Journal of Anxiety Disorders, 49, 21–30. doi: 10.1016/j.janxdis.2017.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voncken MJ, Alden LE, Bögels SM, & Roelofs J (2008). Social rejection in social anxiety disorder: The role of performance deficits, evoked negative emotions and dissimilarity. British Journal of Clinical Psychology, 47(4), 439–450. doi: 10.1016/j.brat.2005.11.005 [DOI] [PubMed] [Google Scholar]
- Voncken MJ, & Dijk KFL (2013). Socially anxious individuals get a second chance after being disliked at first sight: The role of self-disclosure in the development of likeability in sequential social contact. Cognitive Therapy and Research, 37(1), 7–17. doi: 10.1007/s10608-012-9449-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelm FH, Rattel JA, Wegerer M, Liedlgruber M, Schweighofer S, Kreibig SD,& Blechert J (2017). Attend or defend? Sex differences in behavioral, autonomic, and respiratory response patterns to emotion–eliciting films. Biological Psychology, 130, 30–40. doi: 10.1016/j.biopsycho.2017.11.001 [DOI] [PubMed] [Google Scholar]
- Williams MA, McGlone F, Abbott DF, & Mattingley JB (2008). Stimulus-driven and strategic neural responses to fearful and happy facial expressions in humans. European Journal of Neuroscience, 27(11), 3074–3082. doi: 10.1111/j.1460-9568.2008.06264.x [DOI] [PubMed] [Google Scholar]
- Winkielman P, Berridge KC, & Wilbarger JL (2005). Unconscious affective reactions to masked happy versus angry faces influence consumption behavior and judgments of value. Personality and Social Psychology Bulletin, 31(1), 121–135. doi: 10.1177/0146167204271309 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.