Abstract
Background
Bleeding is commonly seen during early pregnancy, and predicting the outcome of pregnancy in such cases is a difficult task. The aim of our study was to evaluate the predictive value of single serum progesterone level for finding the viability in threatened miscarriage and to determine the cut-off value for a viable ongoing pregnancy.
Methods
This was a prospective study in which patients attending the OPD with early pregnancy and bleeding were recruited. Inclusion criteria were period of amenorrhoea less than 12 weeks, complaints of bleeding per vaginum with or without lower abdominal pain and positive urine pregnancy test or serum beta HCG. Multiple pregnancies, inevitable miscarriage, ectopic pregnancy, molar pregnancy and pregnancy achieved by artificial reproductive techniques were excluded from this study. A detailed clinical examination was done, and routine investigations along with serum progesterone were done. Patients were followed up by serial ultrasound for viability, and their outcome was recorded.
Result
A total of 150 patients with early pregnancy threatened miscarriage were enrolled for this study. Of the patients studied, 105 (70%) had a viable pregnancy and 45 (30%) had non-viable pregnancies. The mean serum progesterone was higher in the viable pregnancy, 17.97 ± 7.75 ng/ml, compared to non-viable group, 6.21 ± 2.86 ng/ml. The area under curve was calculated, and a cut-off value of 10.08 ng/ml was obtained. 83.8% of viable pregnancies had serum progesterone more than or equal to 10.08 ng/ml which was statistically significant.
Conclusion
A single value of progesterone is useful in predicting the viability of the ongoing threatened pregnancy. Serum progesterone with a cut-off value of 10.8 ng/ml was found to have a positive predictive value of 95.7% and negative predictive value of 70.7% with an accuracy of 86%.
Keywords: Progesterone, Viability
Introduction
Early pregnancy loss is a common complication of pregnancy. 15–20% of all clinically recognized pregnancies end up as miscarriage [1]. Around 30% of all pregnancies have bleeding during early pregnancy [2].
Predicting the outcome in early pregnancy threatened miscarriage is a big challenge to the clinicians. Ultrasound is probably the single best diagnostic as well as prognostic tool in the management of early pregnancy loss. However, even with expert use, confirmation of ongoing pregnancy is not possible in 8–31% cases at the first visit [2]. Many bio-markers have been evaluated for this.
Serum beta HCG is very useful marker, but often more than one measurement is required to diagnose a viable pregnancy [3]. Serum progesterone is a highly sensitive marker and of great clinical value. It is has a good sensitivity, specificity, accuracy and is affordable. Studies have shown that it is a useful marker for distinguishing a viable from a non-viable pregnancy [1, 2]. Different cut-off values have been used by researchers as the values are dependent on the population under study. The aim of our study was to evaluate the predictive value of single serum progesterone level for finding the viability in threatened miscarriage. We studied the associated risk factors and tried to determine the serum progesterone cut-off value for a viable ongoing pregnancy.
Materials and Methods
A prospective study was conducted in the Department of Obstetrics and Gynaecology in Deen Dayal Upadhyay Hospital Hari Nagar, New Delhi, after obtaining prior approval from the ethical and scientific committee of the institution. The study period was 12 months. All patients attending the OPD with early pregnancy and bleeding were enrolled for the study. Inclusion criteria were period of amenorrhoea less than 12 weeks, complaints of bleeding per vaginum with or without lower abdominal pain and positive urine pregnancy test or serum beta HCG. Multiple pregnancies, inevitable miscarriage, ectopic pregnancy, molar pregnancy and pregnancy achieved by artificial reproductive techniques were excluded from this study. After a written informed consent from the patient, a detailed history was taken including socioeconomic status, previous obstetrics history and history of travel, trauma or intercourse. A detailed clinical examination was done, and routine investigations were done. Blood sample for serum progesterone was collected and analysed using competitive binding immunoenzymatic assay.
In all patients, an ultrasound to confirm the pregnancy, its location and viability was done. Based on ultrasound findings, pregnancy was labelled as viable and non-viable pregnancy. The criteria used were from the Society of Radiologists in Ultrasound Multispecialty Consensus Conference on Early First Trimester Diagnosis of Miscarriage and Exclusion of a Viable Intrauterine Pregnancy [4]. In patients with findings suspicious for, but not diagnostic of pregnancy failure, repeat ultrasound was performed again after two weeks, and according to this finding, they were reclassified into viable and non-viable pregnancies.
Data were collected and statistically analysed to detect the relationship between serum progesterone levels and viability of the pregnancy during first trimester. Statistical analysis was performed by the SPSS program for windows, version 17.0. Continuous variables were presented as mean ± SD, and categorical variables were presented as absolute numbers and percentage. Data were checked for normality before statistical analysis. Normally distributed continuous variables were compared using the unpaired t test, whereas the Mann–Whitney U test was used for those variables that were not normally distributed. Categorical variables were analysed using either the Chi-square test or Fisher’s exact test. The sensitivity, specificity, positive predictive value and negative predictive value were calculated to analyse the diagnostic value of progesterone correlated with pregnancy outcome. For all statistical tests, a p value less than 0.05 was taken as significant difference.
Results
This was a prospective study carried out on 150 patients with early pregnancy threatened miscarriage. In this study, 66 (44%) patients were between the age group 21–25 yrs and the mean age was 25.62 yrs. 35 (23.33%) patients were primigravida, closely followed by 44 (29.34%) patients who were second gravida and 42 (28%) patients who were gravida three.
In our study, majority of patients (59.33%) were from low socioeconomic class and rest from middle (23.33%) and upper class (17.33%). Major presenting symptom was bleeding per vaginum which was seen in 80 patients. Seventy patients presented with both bleeding per vaginum and pain in abdomen.
Of the risk factor studied, it was seen that 56 (37.3%) patients had history of previous spontaneous miscarriage, 10 patients had history of thyroid disorder, and 1 patient had diabetes mellitus. Sixteen patients had history of intercourse, 22 patients had experienced trauma, 24 patients had history of travel, and 9 patients had history of heavy work.
Of the patients studied, 105 (70%) had a viable pregnancy and 45 (30%) had non-viable pregnancy. The mean gestational age at the time of progesterone assay was 8.42 ± 1.52 weeks with range of 6–11 weeks. It was seen that the mean serum progesterone was higher in the viable pregnancy, 17.97 ± 7.75 ng/ml, compared to non-viable group, 6.21 ± 2.86 ng/ml as shown in Table 1.
Table 1.
Relation between serum progesterone and viability of pregnancy
| Pregnancy outcome | Number | Serum progesterone (ng/ml) Mean ± SD | p value |
|---|---|---|---|
| Viable pregnancy | 105 | 17.97 ± 7.75 | < 0.001 |
| Non-viable pregnancy group | 45 | 6.21 ± 2.86 |
Relation between serum progesterone and maternal age was studied and was found to be insignificant. Other factors like history of previous spontaneous miscarriage, thyroid disorder, diabetes mellitus and history of intercourse, trauma, travel and heavy work were evaluated and found to be insignificant as shown in Table 2.
Table 2.
Relationship between serum progesterone and maternal age, gestational age, risk factors and presenting complaints
| Variables | Total no. (n = 150) | Serum progesterone (ng/ml) mean ± SD | p value | |
|---|---|---|---|---|
| Maternal age | < 25 yrs | 83 | 14.29 ± 8.80 | 0.662 |
| > 25yrs | 67 | 14.64 ± 8.36 | ||
| Past h/o of early miscarriage | Positive | 56 | 12.94 ± 7.74 | 0.098 |
| Negative | 94 | 15.34 ± 9.10 | ||
| Gestational age | < 8 weeks | 69 | 13.15 ± 7.80 | 0.090 |
| > 8 weeks | 81 | 15.54 ± 8.97 | ||
| H/o trauma | Positive | 22 | 11.67 ± 8.74 | 0.052 |
| Negative | 128 | 14.92 ± 8.49 | ||
| H/o travel | Positive | 24 | 12.64 ± 8.25 | 0.235 |
| Negative | 126 | 14.79 ± 8.63 | ||
| H/o heavy work | Positive | 9 | 16.82 ± 10.62 | 0.474 |
| Negative | 141 | 14.29 ± 8.46 | ||
| H/o intercourse | Positive | 16 | 16.85 ± 8.99 | 0.197 |
| Negative | 134 | 14.16 ± 8.52 | ||
| H/o diabetes | 1 | 21.07 ± 9 | 0.258 | |
| H/o thyroid disorders | 10 | 17.26 ± 9.00 | 0.374 | |
| Symptoms | Bleeding | 80 | 14.91 ± 8.71 | 0.485 |
| Bleeding and pain | 70 | 13.91 ± 8.46 | ||
The area under curve was calculated and was found to be 0.950 with 95% confidence interval (0.918–0.982) and with cut-off value of 10.08 ng/ml as shown in Table 3 and Fig. 1. The frequency distribution of patients as per pregnancy outcome and serum progesterone cut-off level is shown in Table 4. It was seen that 83.8% of viable pregnancies had serum progesterone more than or equal to 10.08 ng/ml while 91.9% of non-viable pregnancy had less than 10.08 ng/ml which was statistically significant. The cut-off value was found to be 83.8% sensitive and 91.1% specific to diagnose viable pregnancy. The positive predictive value was 95.7% and negative predictive value was 70.7% with an accuracy of 86%.
Table 3.
Area under curve with 95% confidence interval
| Area under the curve | ||||
|---|---|---|---|---|
| Area | Std. error | Asymptotic sig | Asymptotic 95% confidence interval | |
| Lower bound | Upper bound | |||
| 0.950 | 0.021 | < 0.001 | 0.918 | 0.982 |
Fig. 1.
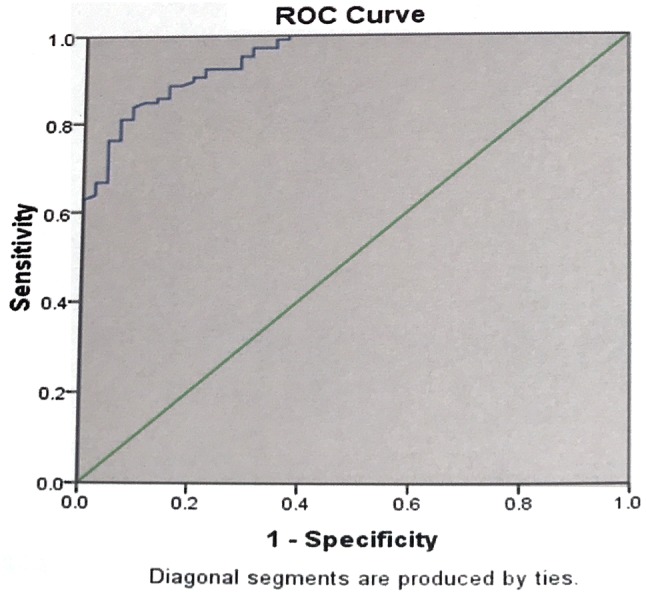
Receiver operator characteristic (ROC) of progesterone as diagnostic test for non-viable pregnancy
Table 4.
Frequency distribution of patients as per pregnancy outcome and serum progesterone cut-off level
| Non-viable | Viable | p value | |||
|---|---|---|---|---|---|
| Frequency | % | Frequency | % | ||
| No of cases with serum progesterone < 10.8 ng/ml | 41 | 91.1 | 17 | 16.2 | < 0.001 |
| No of cases with serum progesterone > 10.8 ng/ml | 4 | 8.9 | 88 | 83.8 | |
| Total | 45 | 100 | 105 | 100 | |
Discussion
Bleeding in early pregnancy is very common in the first trimester of pregnancy. Less than half proceed to complete miscarriage. Eighty percentage of all miscarriages occur in the first trimester of pregnancy.
The progesterone hormone which is secreted by the granulosa cells of the ovary is required for the maintenance of pregnancy. It induces secretary changes in the lining of the uterus and is essential for a successful implantation of the embryo. When fertilization occurs, the progesterone secreted by the corpus luteum has the important function of maintaining the early pregnancy till the placenta takes over its function at 7–9th week of gestation. Moreover, progesterone also modulates the immune response of the mother to prevent rejection of the embryo and enhances uterine quiescence and suppresses uterine contractions. Hence, measurement of serum progesterone levels in early pregnancy has been regarded as one of the most powerful predictors of pregnancy outcome in natural conception. We have evaluated the correlation of single value serum progesterone in predicting the viability of threatened miscarriage and its risk factors.
In our study, the age of presentation of patients ranged from 18 to 35 yrs with a mean age of 25.62 yrs. This was comparable with study of Khosho et al. [5] in which the mean age was 27.2 yrs. However, this was in contrast to studies done by Hanita et al. (30 yrs) [6] and Abdelazaim et al. [7] (32.7 ± 5.1 yrs). This may be due to delaying of conception in these patients. Relationship of gestation age with serum progesterone has been evaluated by few studies. Studies done by Hanita [6] and Khosho et al. [5] have found no correlation between gestational age and progesterone level. They observed that serum progesterone changes very little during early pregnancy.
Primary presenting complaint was bleeding which was seen in 80 patients. Seventy patients had both pain and bleeding. Newbatt et al. [8] stated that the most common symptom of miscarriage is bleeding during pregnancy. Symptoms other than that are not statistically related to miscarriage.
In our study, we also evaluated few risk factors for threatened miscarriage. The most common risk factor for first trimester miscarriage was a history of previous loss. 56 patients out of 150 had history of previous loss. In the study done by Abdelazim et al. [7], 18.4% patients had history of earlier miscarriage. Arck et al. [9] in their study said that previous pregnancy loss is associated with increased risk of miscarriage in subsequent pregnancy. Thyroid disorders and diabetes were associated with increased risk of miscarriage, but were not significant, this may be because of the small sample size.
The mean serum progesterone in our study was significantly high in viable pregnancy (17.97 ± 7.75 ng/ml) compared to non-viable pregnancy (6.21 ± 2.86 ng/ml) in early pregnancy with threatened miscarriage. Khosho et al. [5] stated that serum progesterone levels vary between 8.7 and 41.3 ng/ml in viable pregnancy while with miscarriage it is in the range of 0.81–20.1 ng/ml (6.7 ± 4.8). This was statistically significant. Hanita et al. [6] compared serum progesterone in viable and non-viable pregnancy and found it to be 45.9 ng/ml versus 10.7 ng/ml, respectively, which was statistically significant. Progesterone levels were also found to be lower in threatened abortion patients with non-viable pregnancy (23.3 ± 12.0 ng/ml) compared to viable pregnancies (89.7 ± 33.2 ng/ml).
The ROC curve analysis demonstrated a significant ability of serum progesterone to differentiate between viable and non-viable pregnancies. The area under curve for progesterone was 0.95 (95% confidence interval, 0.918–0.982) with the parameters calculated from the ROC curve. The cut-off value of serum progesterone in our study was 10.08 ng/ml which was comparable to the study of Abdelazim et al. In our study, 83.8% of viable pregnancies had serum progesterone more than or equal to 10.08 ng/ml, while 91.9% of non-viable pregnancy had less than 10.08 ng/ml which was statistically significant. Abdelazim et al. [7] in their study observed that the serum progesterone cut-off level at 10 ng/ml was 79.3% sensitive to diagnose non-viable pregnancy and was 93.3% specific to diagnose viable pregnancy. Elewa et al. [10] in their study said that the serum progesterone cut-off level of 15.5 ng/ml had 70.6% sensitivity and 87.5% in predicting the continuation of pregnancy.
Lek et al. [11] suggested 35 nmol/L as a cut-off value for serum progesterone to predict spontaneous miscarriage in patients with early threatened pregnancy. Hanita et al. [6] evaluated serum progesterone as a marker for early pregnancy failure. They said that at a cut-off value of 32.7 ng/ml, progesterone had 90% sensitivity with 75% negative predictive value and 92% specificity with 97% positive predictive value to diagnose early pregnancy failure. They also observed that the discriminatory efficacy of a single progesterone determination was not increased by serial estimation of progesterone level [6]. Hence, repeated value is usually not done. The difference in the cut-off value may due to the difference in the studied population and methods used to estimate serum progesterone levels.
Conclusion
A single value of progesterone helps to guide us regarding the viability of the ongoing threatened pregnancy. It prevents unnecessary inconvenience to patients and identifies the one requiring increased surveillance. It is a sensitive and specific test that reliably guides the prognosis of pregnancy. Our study found that serum progesterone cut-off value of 10.8 ng/ml is a reasonably good predictor of a viable early threatened pregnancy.
Funding
No financial aid provided for the study.
Dr. Vijay Kumar Kadam
is Head of the Department of Obstetrics and Gynaecology at Deen Dayal Upadhyay Hospital. He has done his MBBS and MD in Obstetrics and gynaecology from All India Institute of Medical Sciences, New Delhi. He is a good clinician and a meticulous surgeon. He has a keen interest in academics. His field of interest is laparoscopy and infertility.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Permission was obtained from the scientific and ethical committee of the institution for the study.
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Footnotes
Dr. Vijay K. Kadam, MS (Obstetrics and Gynaecology), MBBS, is a Consultant in Obstetrician and Gynaecology at DDU Hospital. Dr. Shivani Agrawal, DNB (obstetrics and Gynaecology), MBBS, is a DNB Resident in Obstetrician and Gynaecology at DDU Hospital. Dr. Pinkee Saxena MD (obstetrics and Gynaecology), MBBS, is a Specialist in Obstetrician and Gynaecology at DDU Hospital. Dr. Poonam Laul MD (obstetrics and Gynaecology), MBBS, is a Specialist in Obstetrician and Gynaecology at DDU Hospital.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ahmed Salah, Alsammani Mohamed, AlSheeha Muneera, Aitallah Abdou, Khan Farhat. Pregnancy Outcome in Women with Threatened Miscarriage: a Year Study. Materia Socio Medica. 2012;24(1):26. doi: 10.5455/msm.2012.24.26-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verhaegen J, Gallos ID, van Mello NM, et al. Accuracy of single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies. BMJ. 2012;27(345):e6077. doi: 10.1136/bmj.e6077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seeber BE. What serial hCG can tell you, and cannot tell you, about an early pregnancy. Fertil Steril. 2012;98(5):1074–1077. doi: 10.1016/j.fertnstert.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Peter MD, Carol BB, Tom B, et al. Diagnostic criteria for nonviable pregnancy early in the first trimester. Society of radiologists in ultrasound multispeciality panel on early first trimester diagnosis of miscarriage and exclusion of a viable Intrauterine pregnancy. N Engl J Med. 2013;369:1443–1451. doi: 10.1056/NEJMra1302417. [DOI] [PubMed] [Google Scholar]
- 5.Khosho EZ, Aiub MM, Adnan S. The value of early pregnancy single serum progesterone measurement in relation to first trimester viability. Thi-Qar Med J. 2011;5(2):133–141. [Google Scholar]
- 6.Hanita O, Hanisah AH. Potential use of single measurement of serum progesterone in detecting early pregnancy failure. Malays J Pathol. 2012;34:41–46. [PubMed] [Google Scholar]
- 7.Abdelazim IA, Elezz AA, Elsherbiny M. Relation between single serum progesterone assay and viability of the first trimester pregnancy. Springerplus. 2012;1(1):80. doi: 10.1186/2193-1801-1-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newbatt E, Beckles Z, Ullman R, et al. Ectopic pregnancy and miscarriage: summary of NICE guidance. BMJ. 2012;12(345):e8136. doi: 10.1136/bmj.e8136. [DOI] [PubMed] [Google Scholar]
- 9.Arck PC, Rücke M, Rose M, et al. Early risk factors for miscarriage: a prospective cohort study in pregnant women. Reprod Biomed Online. 2008;17(1):101–113. doi: 10.1016/S1472-6483(10)60300-8. [DOI] [PubMed] [Google Scholar]
- 10.Elewa AM, Mansour AEA, Sharaf El-Deen AA, et al. The role of a single serum progesterone measurement in relation to early pregnancy failure and fetal viability. Med J Cairo Univ. 2016;84(2):169–175. [Google Scholar]
- 11.Lek SM, Ku CW, Allen JC, Jr, et al. Validation of serum progesterone < 35 nmol/L as a predictor of miscarriage among women with threatened miscarriage. BMC Pregnancy Childbirth. 2017;17(1):78. doi: 10.1186/s12884-017-1261-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


