Abstract
Background
Heterotopic Ossification (HO) is a common condition referring to ectopic bone formation in soft tissues. It has two major etiologies, acquired (more common) and genetic. The acquired form is closely related to tissue trauma. The exact pathogenesis of this disease remains unclear; however, there is ongoing research in prophylactic and therapeutic treatments that is promising.
Conclusions
Due to HO potential to cause disability, it is so important to differentiate it from other causes in order to establish the best possible management.
Key words: heterotopic ossification, radiology, pathology
Introduction
Heterotopic Ossification (HO), also known as paraosteoarthopathy, myositis ossificans, and heterotopic calcification1 among others, is a commonly occurring condition that refers to ectopic bone formation in soft tissues. HO can be subdivided into two major types: acquired and genetic, with acquired being the most predominate. Acquired HO is closely related to tissue trauma and can be seen after joint surgery, musculoskeletal trauma, central nervous system injury, and even burns.2 HO develops in up to 44% of patients undergoing hip arthroscopy or replacement, 10-20% of those with CNS injury, and 4% of those with burns covering greater than 30% of body surface.3, 4, 5, 6, 7, 8, 9, 10 Many cases of HO lead an indolent course, however severe cases can cause inflammation, pain, immobility and functional impairment.11 Due to its potential to cause disability, it is imperative to be able to distinguish HO from other etiologies including tumoral calcinosis, osteosarcoma, or dystrophic calcification to provide adequate treatment.
Pathophysiology
Acquired HO can be broadly categorized in to three etiologic subtypes: neurogenic from central nervous system injury, orthopedic covering fractures, fixations, joint replacements, etc., and trauma related to burns and high velocity impacts.3 The formation of HO is tied to the underlying inflammatory process, which can even be demonstrated in genetic cases of HO where patients report pro-dromal symptoms of pain, swelling, and erythema prior to ectopic bone formation.12 Trauma-induced HO is also correlated with the severity of the trauma, infection, total burn coverage13 and cytokine concentration in affected tissues.3,14 As a result, the most frequently used prophylactic medications are nonsteroidal anti-inflammatory drugs.15 However, the underlying mechanisms for HO formation are still not clear. The Literature suggests multiple cellular origins for the formation of HO, pointing to muscle satellite cells16, smooth muscle cells17, and even endothelial cells.18 Although the exact cellular origin is debated, it is commonly accepted to be multipotent cells in the local tissue. The requirements necessary for HO formation include having an inducing agent, an osteogenic precursor, and a permissive environment for osteogenesis19,20 which when met leads to proliferation and formation of bone.21 Bidner et al. have proposed that failure to regulate the immune system or inflammatory response lead to the release of inciting agents that lead to HO.19,22 Further investigations by Salisbury et al. and Kan et al. have implicated bone morphogenic protein type 2 (BMP-2) as a pro-inflammatory agent by stimulating release of substance p and calcitonin gene-related peptide from sensory nerves.23,24 Further investigations could support BMP’s role in HO formation and lead to formulation of targeted therapies.3,21 Other suggested contributory factors include prostaglandin (specifically PGE-2), tissue hypoxia, and an imbalance between parathyroid hormone and calcitonin.25 A review performed by Cholok et al. showed multiple potential contributory cell lineages with likely varying signalling pathways, highlighting the current lack of understanding in HO formation.3 All in all, the precise mechanisms of HO formation remain vague and need further investigation.
Clinical presentation and diagnosis
Patients presenting with HO typically complain of inflammatory symptoms including pain, swelling, erythema, and warmth along with joint immobility, which appear anytime from 3 to 12 weeks after the precipitating event.11,25, 26, 27, 28 The most common sites of occurrence, in a decreasing order, are the hips, knees, shoulders, and elbows.25,27 The gold standard method for diagnosing HO is through imaging studies, mainly radiography and computerized tomography (CT).3 The downfall to these types of imaging is that they are not able to detect calcifications for at least 6 weeks after the inciting trauma.25,29 Three-phase bone scintigraphy is the most sensitive method for detecting HO, with the earliest detection being 2.5 weeks post trauma.25,30 It is also effective in monitoring HO progression and determining the appropriate time to stage surgical intervention.25,26,30 Activity on bone scans usually peaks a few months after the inciting event and returns to baseline by 12 months.25
Early screening methods used before imaging studies include serum alkaline phosphate levels and 24-hour urinary PGE2. Alkaline phosphate levels can increase two weeks after trauma, reaching 3.5 times baseline by 10 weeks, and then returning to baseline by 18 weeks. A rapid increase in 24-hour PGE2 urinary secretion has also been shown to suggest HO and would indicate further imaging studies.31,32
Upon suspicion of HO on imaging, it has been suggested to perform a biopsy to confirm the diagnosis; however, current recommendations are to follow up with imaging studies in four weeks, which together with the history of trauma can confirm the diagnosis.33
Imaging and classification
A soft tissue mass is the earliest finding of HO on imaging, it is often depicted as a peripheral zone of mineralization in acquired cases.33 With time, these outer regions can mature in to a peripheral cortex with a well-defined cancellous bone interior detectable by CT (Figures 1-2 and 3).29,33 Radiography (Figure 4) and CT scan remain the gold standard for diagnosis due to their ability to detect immature bone formation and the relatively cheap cost.3,29 In the acute phase of HO, there is increased tissue vascularization and density, which can be detected on Magnetic Resonance (MR).34 This region appears isointense or hyperintense to muscle on T1-weighted images and hyperintense on T2 weighted images with pronounced surrounding inflammation.34,35 As the rim of calcification forms, signal void begins to appear on the periphery on all sequences.35,36 During this maturing phase, MR imaging results in non-specific findings and heterogenous signal that mimics many other pathologic processes.29,37 Once mature, HO presents as cancellous fat that is hyperintense on T1 and T2 weighted images outlined by the hypointense cortical bone29 and this can be considered diagnostic. Therefore, when MR detects a mature HO, no further imaging is necessary. On the other hand, early MRI has a great advantage in excluding other differential diagnosis possibilities, as we can observe the “striate pattern” and “checkerboard-like pattern” appearance in T2-WI and contrast-enhanced MRI images38 or it can be detected by displacing the fascial planes, especially at the periphery of the lesion.39 Recognizing these MRI patterns in HO could be very beneficial in the early phases as the condition is commonly misdiagnosed for an osteomyelitis or even a malignancy, mostly sarcomas.40, 41, 42
Figure 1.
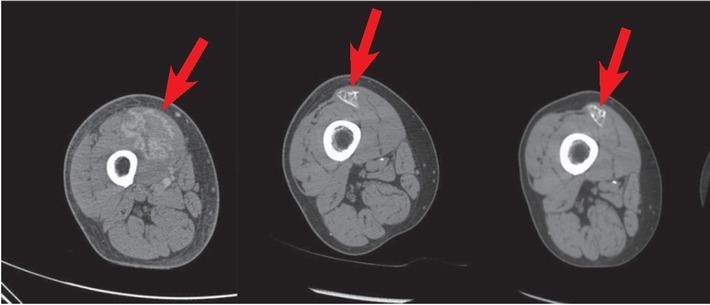
Progression of Heterotopic Ossification from presentation (left), 4 months (middle), and 8 months (right). Axial CT with contrast depicts initial hyperemia with increasing calcification at the site of injury with eventual outer cortical and inner cancellous bone formation.
Figure 2.
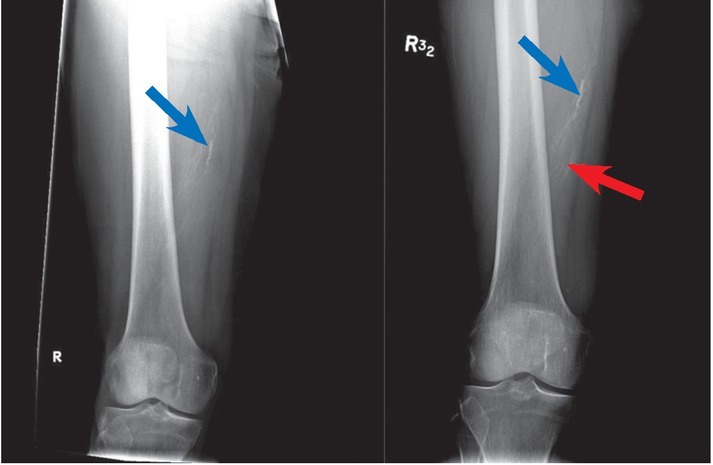
AP X-rays show previous vascular calcifications (Left-blue arrow) with no apparent masses at the site of injury at presentation. At 4 months follow up, there is increased calcifications noted (blue arrow) with expansion to the adjacent soft tissue area (red arrow) both are consistent with Heterotopic Ossification.
Figure 4.
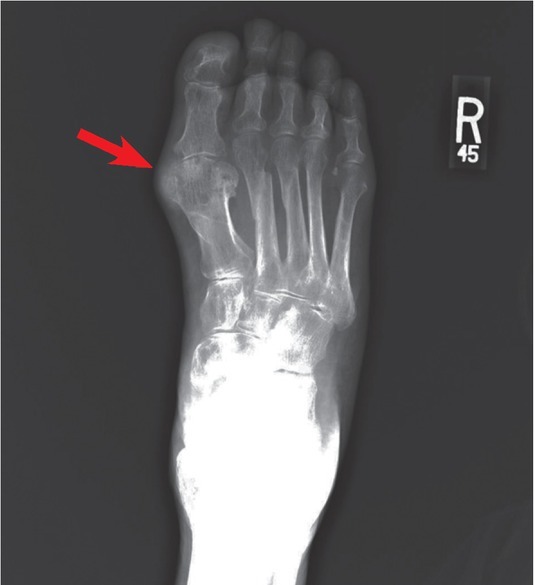
Severe gout presenting on the first metatarsophalangeal joint. AP X-ray of the right foot shows a medial pararticular calcified soft tissue mass at the level of the first metatarsophalangeal joint (red arrow), resulting in adjacent intraosseous erosions with sclerotic borders.
Figure 3.
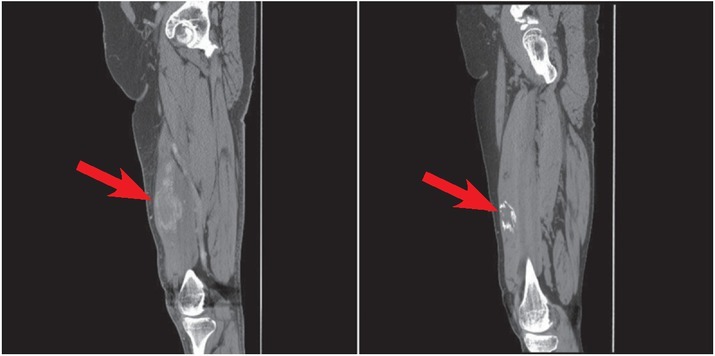
Heterotopic Ossification shown with initial hyperemia without calcification at presentation (left- red arrow) with increasing organized calcification seen after 4 months on Non-contrast CT (Right-red arrow).
Ultrasonography (US) is proved to be a sensitive imaging modality for soft tissues lesions and calcifications.43,44 It is also safe, of low-cost, and easy to perform and repeat.45 US has the great advantage of bedside application as well, which could be more feasible for bed-ridden patients.45,46 Qing Wang et al. discussed a new concept for monitoring the trauma-induced HO. The study gives a guidance to the orthopedist to modify the treatment and make an individualized rehabilitation program. They have shown that the grey-scale values are different during the different phases of HO maturation, and so US allows for a quantitative assessment during the rehabilitation of HO.47
Staging of HO is commonly done using the Brooker classification (Table 1), which was initially developed using anteroposterior radiographs of the hip.9 There has been some criticism of this classification as anteroposterior radiographs cannot distinguish between bridging or overlapping calcifications.48 To simplify and reduce variability, Della Valle et al. (Table 2) created a modified classification using only three distinct grades.49 However, a third and more comprehensive classification was established by Schmidt and Hackenbroch (Table 3) with the goal of classifying HO while considering ossification within the region of surgical approach.50 From these classifications, an important distinction for reporting and assessing severity is determining whether the space -between two opposing bone surfaces- is greater than or less than one centimeter.9,49,50
Table 1.
Brooker classification of heterotopic ossification9
| Class 1 | Islands of bone within the soft tissues over the hip |
| Class2 | Bone spurs from the pelvis or proximal end of the femur, leaving at least one centimeter between opposing bone surfaces. |
| Bone spurs from the pelvis or proximal end of the femur, reducing | |
| Class 3 | the space between opposing bone surfaces to less than one centimeter. |
| Class 4 | Apparent bone ankylosis of the hip |
Table 2.
Della Valle classification of heterotopic ossification49
| Class 1 | Absence of HO or islands measuring <1 cm in length |
| Class 2 | Islands >1 cm or spurs leaving at least 1 cm between femur and pelvis |
| Class 3 | Spurs leaving <1 cm between opposing surfaces or bony ankylosis |
Table 3.
Schmidt and Hackenbroch classification of heterotopic ossification50
| Region 1 | Heterotopic ossifications strictly below tip of greater trochanter |
| Region 2 | Heterotopic ossifications below and above tip of greater trochanter |
| Region 3 | Heterotopic ossifications strictly above tip of greater trochanter |
| Grade A | Single or multiple heterotopic ossifications < 10 mm in maximal extent without contact with pelvis or femur |
| Grade B | Heterotopic ossifications > 10 mm without contact with pelvis but with possible contact with femur; no bridging from femur to proximal part of greater trochanter, with no evidence of ankylosis |
| Grade C | Ankylosis by means of firm bridging from femur to pelvis |
Differential diagnosis
Many pathologies can imitate HO clinically or radiographically. It is vital to understand the similarities and differences of these mimetics when considering the diagnosis of HO. A few differentials that should be considered are briefly discussed below.
Dystrophic calcification
Dystrophic calcification (DC) is the calcification that occurs in soft tissue post inflammation and damage. The mechanism is thought to be either disruption of cell membranes during cellular stress allowing calcium to enter and subsequently be concentrated in the mitochondria or by creating an acidic environment in the tissue that lacks calcification inhibitors.51
It is well documented to occur in cases of collagen vascular diseases like dermatomyositis (Figure 5), systemic lupus erythematosus, and scleroderma52, but has also been identified in other disease processes.51 On plain film, DC appears as amorphous calcification with a hazy ill-defined appearance that can increase in density over time.53 CT will similarly show peripheral amorphous hyperdensities, with MRI showing hypointense signals in T1 and T2 weighted images (Figure 6).54
Figure 5.
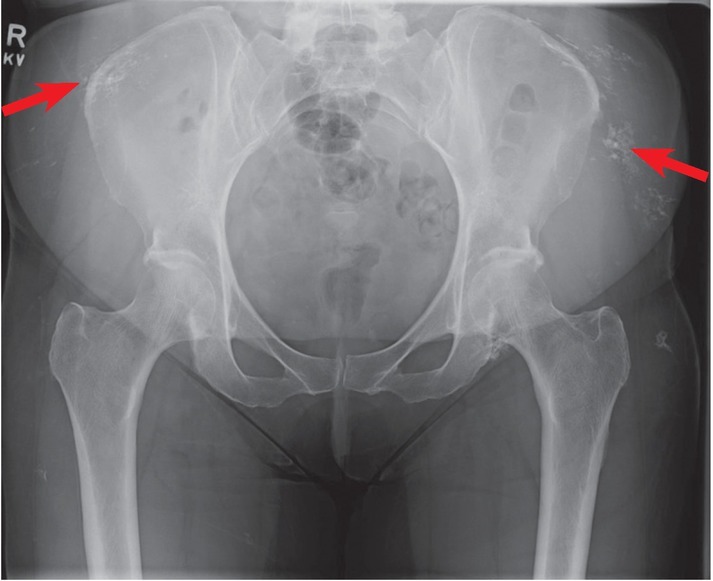
Dystrophic calcifications secondary to dermatomyositis are seen in the peripheral soft tissue (2 red arrows). They appear as hazy ill-defined opacities on plain film.
Figure 6.
T1 weighted non-contrast MRI (left-red arrow) of dystrophic calcifications show hypointense signal in patchy patterns. These appear as calicified hazy patches on CT (right-red arrow).
The distinguishing difference between DC and HO is organization. DC and HO are virtually indistinguishable on plain films, CT, or MRI early in the disease process as mineralization occurs. HO will begin to organize and ossify over the course of months into lamellar bone while DC will remain as amorphous, non-ossified calcifications.55
Chondrocalcinosis
Chondrocalcinosis is calcification within fibrous or cartilaginous structures and is frequently associated with calcium pyrophosphatase disease (CPPD).56 In cases of CPPD, there is usually acute, painful inflammation of a joint, often the knee, where calcium phosphate crystals are deposited.57 Microcrystals can then impregnate cartilage causing arthritic symptoms, which can range from mild to severe with joint destruction.57 On plain films, this appears as a dense line within hyaline cartilage that runs parallel to the articular surface.56 CT has excellent sensitivity and specificity for detecting chondrocalcinosis and can better visualize the linear hyperintense calcifications (Figure 7).56 There is often a concurrent degenerative joint disease with joint space narrowing and large osteophyte formation.58 The linear deposition contrasts with HO, which presents as a peripheral circumferential calcific mass on both plain films and CT with minimal intra-articular involvement. MRI has little utility in diagnosing Chondrocalcinosis, as the calcifications are not well visualized in tissues.56
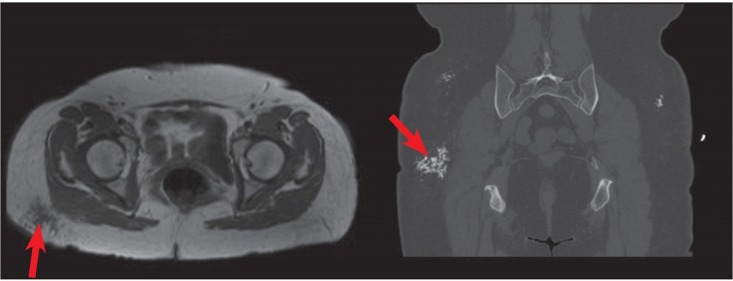
Figure 7.
Calcium Pyrophosphate Deposition disease can lead to calcification of intra-articular cartilage. There is opacification of the lateral joint space on plain film (left-red arrow) and a more clearly defined mineralization seen near the lateral condyle on CT (right-red arrow).
Tumoral calcinosis
Tumoral calcinosis (TC) refers to a syndrome characterized by calcium salt deposition in peri-articular soft tissue.59 A major component of TC is hyper-phosphatemia secondary to genetically acquired decrease in phosphate secretion59, 60, 61 or chronic renal failure and resulting hyperparathyroidism.59 Patients present with joint pain, swelling, or immobility most commonly in the hip, elbow, shoulder, foot, or wrist.59,62,63, 64 Unlike HO, TC lesions grow slowly over the course of several years.65 Plain radiographs, ultrasound and CT scan, all can be used for diagnosis and would show fluid filled, lobulated, cystic calcifications in peri-articular tissue.66
T1 and T2 weighted MRI show a hypointense lesion with septal enhancement (Figure 8). HO is not cystic in nature and lacks the lobulated pattern on both CT and MRI. HO also presents with hyperintense signal centrally with a hypointense cortical shell on MRI. Management of TC is clinically determined based on the symptoms and the size of calcinosis with surgical or needle decompression being most common interventions.66
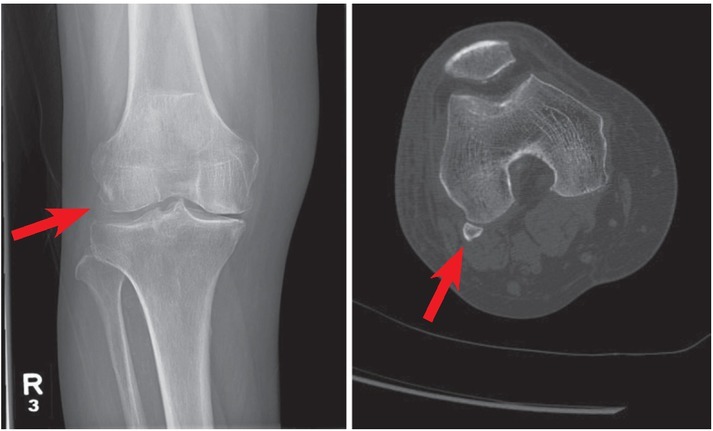
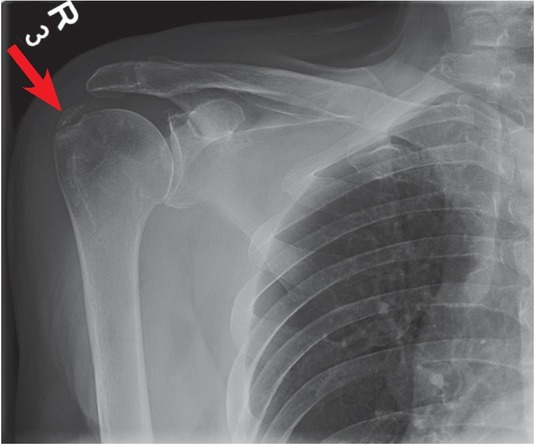
Figure 8.
X-ray of the (left- 2 red arrows) shoulder show opacified cystic, lobulated peri-articular lesions in Tumoral Calcinosis. Coronal MRI T2 sequencing (right-red arrow) reveals hypointense lesions with septal enhancement, hyperintense fluid filled cavities and fluid –fluid levels consistent with sedimentation.
Avulsion fracture
An avulsion fracture (AF) is the separation of a bone fragment at the site of tendon attachment, often occurring after a traumatic injury. Patients with this injury typically have a definite history of trauma accompanied by pain, swelling, and loss of joint function.67 Findings on imaging can be seen immediately post trauma, depicting sharply delineated bone fragments (Figure 9). Large avulsed fragments can appear identical to matured HO, therefore having a clinical history is important. In addition, HO will not be visible on a plain film until weeks after the inciting trauma and will not mature into cortical bone for many months.25 CT of avulsion fractures helps delineate fracture sites and show displaced hyperdense cortical bone.67 HO can be distinguished from AF on CT, showing a ring of hyperdense cortical bone with a hypodense interior.29,33 MRI may be useful in detecting local tissue damage seen in avulsion fragments; however, findings are consistent with inflammation and are non-specific.67
Figure 9.

An avulsed piece of bone is seen on the posterior aspect of the calcaneus secondary to trauma (red arrow).
Primary osteosarcoma
Osteosarcomas (OS) are the most common primary bone tumor, developing from uninhibited osteoid production by malignant mesenchymal cells.68 Patients present with localized pain and swelling, which then proceeds to joint immobility. This type of tumor is commonly seen in the metaphysis of long bones, most commonly the distal femur, proximal tibia, and proximal humerus; in a descending fashion.68,69 On plain radiographs, it can present as osteoblastic, osteolytic, or with mixed appearances, and have patchy calcifications from the newly developing bone in the surrounding soft tissue.68 The imaging appearance is commonly described as a “sunburst” appearance or as having cloudlike density (Figure 10).70 CT scan is highly sensitive to calcification and is useful in showing the amorphous osteoid formation in OS, which can help distinguish it from organized circumferential osteoid formation in HO. MRI of OS shows heterogenous signal intensities on T1- and T2-weighted images due to a mixture of amorphous osteoid, hemorrhage, and necrosis.70,71 Radiographs can be correlated with a low signal intensity on T1-wieghted imaging and hyperintensity on STIR imaging indicating mineralized matrix deposition with small periosteal reaction. Other findings include cortical bone destruction and marrow invasion not typically seen with HO.71
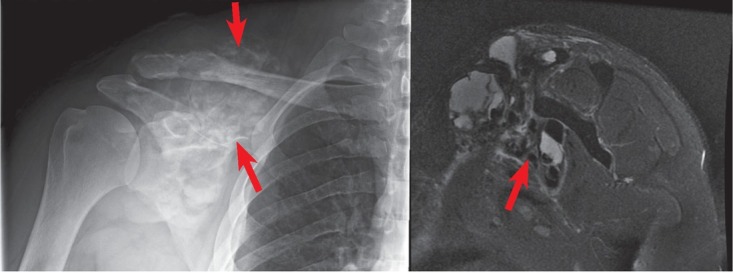
Figure 10.
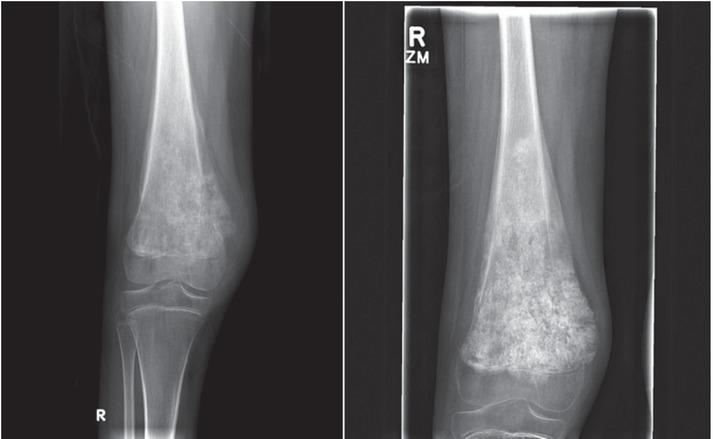
The “sunburst” appearance with cloudlike density of untreated Osteosarcoma is observed in the distal femur (left-red arrow). After chemotherapy, the lesion ossifies and becomes increasingly opaque on plain film (right-red arrow), consistent with positive therapeutic response).
Tophaceous gout
Gout is a type of inflammatory arthritis caused by the deposition of monosodium urate crystals in joints and surrounding tissue.72 Clinically, this condition presents with an acute onset pain and swelling at the site of deposition, typically the feet and knees but can also be seen elsewhere.72 Early radiographic studies can often be negative, however in chronic gout patients, punched erosions with well-defined sclerotic borders can form extra marginally, articularly, or para-articularly with preservation of the joint space.72,73 In severe cases, extreme bone destruction can occur with large periarticular lesions, joint space widening, and concurring osteoarthritis.72, 73, 74 Tophi on CT are seen as discrete masses with a higher intensity than adjacent soft tissue.75 CT is also useful in defining well-demarcated erosions with overhanging osteophytes seen in gout.75 MRI is only beneficial in identifying soft tissue abnormalities around affected joints rather than tophi themselves, leading to low specificity and utility.75 When seen, tophi appear with decreased signal intensity on T1 weighted images and heterogeneous signal on T2.75 HO can be distinguished from tophaceous gout on x-ray and CT by lack of intraosseous erosions, peripheral calcifications in the soft tissue, and formation of cortical bone. MRI is not useful in distinguishing between the two unless the HO is mature, when complete lamellar bone is seen.
Calcific tendonitis
Calcific Tendonitis refers to the condition of calcium deposition in tendons.76 This is clinically depicted by chronic pain with activity, tenderness, swelling, and joint immobility that is commonly localized to the rotator cuff tendons.76,77 The etiology remains unknown; however, severity has been associated with endocrine diseases.78 Pathology can be noted by standard AP radiograph with internal and external rotation views showing dense homogenous calcification typically noted proximal to the greater tubercle (Figure 11).79 Ultrasound, used to evaluate a rotator cuff injury, can show a hyperechoic lesions with reproducible pain in palpation during the procedure.80 Calcific tendonitis can also be viewed with susceptibility-weighted imaging, which presents as a hyperintense lesion at tendon insertion site with occasional central hypointensity. It lacks the well-defined shape of HO and the hyperintense core seen on T1 weighted images.81
Figure 11.
Opaque linear coarse calcification along the expected location of the supraspinatus tendon insertion onto the greater tubercle of the humerus (red arrow), consistent with Calcific Tendonitis.
Fibrodysplasia Ossificans Progressiva
Fibrodysplasia Ossificans Progessiva is an extremely rare genetic form of HO in which patients repair mechanism ossifies the fibrous tissue at the trauma site, leaving the patient permanently frozen secondary to minor trauma.82 Patients initially present with characteristic malformations of the large toes at birth with painful soft tissue swelling and ectopic bone formation within the first decade of life.82, 83, 84 Laboratory changes include increased serum alkaline phosphatase and urinary basic fibroblast growth factor during acute episodes. Radiographic imaging shows extensive heterotopic bone formation diffusely with no specific pattern and ankylosis of adjacent joints with heterotopic bone formation.82 MRI can show heterotopic bone formation with underlying edema and subtle soft tissue changes indicating pre-osseous lesions, noted as hyperintense lesion on fat suppressed T2 imaging.85 CT imaging can be used for volumetric analysis of ossification that is unattainable via radiographs or MRI, showing the extent of joint ankylosis with 3D rendering and assessment of severity via Lederson grading scale. 85 This condition can be distinguished from traumatic HO by early onset and severe disseminated ossification.
Treatment
Treatment for HO is divided into prophylaxis for high-risk patients and management of already formed HO. Due to the large variability in etiology and underlying mechanisms for HO and individualized patient risk factors, there is little agreement on appropriate treatment regimens. Commonly used prophylaxis includes NSAIDs, localized low dose radiation, or a combination there-of with the most popular being NSAID alone.86,87 Prophylactic NSAIDs have shown to reduce the occurrence of ectopic bone formation when given peri-operatively compared to placebo, but at the expense of medication side effects such as gastrointestinal ulcers, bleeding, and delayed bone healing.88,89 Although there is a decrease in HO formation, NSAIDs had no effect on pain or physical function compared to placebo.88,90,91 NSAIDs target pro-inflammatory prostaglandins, which have been shown to be integral to osteogenesis and are thought to have some effect by suppressing the migration and proliferation of mesenchymal cells.21,92,93 The NSAID of choice is the non-selective cox inhibitor indomethacin.94 Cox-2 specific inhibitors have been suggested to reduce side effects associated with nonselective cox inhibitors; however, their cardiovascular side effects and lack of safety with routine use limit their use.15
Coventry et al. first established radiation therapy (RT) as an effective treatment in 1981, and further studies by Childs et al. and Chao et al. confirmed its benefits.95, 96, 97 In the retrospective cohort study by Childs et al. covering 263 patients whom experienced traumatic acetabular fractures, 5.3% of patients receiving RT also developed ectopic bone formation compared to 60% of patients without any treatment. The drawbacks to RT include potential side effects such as carcinogenesis, bone disunion, and oligospermia as well as the higher cost.15 Strauss et al. determined that the total cost of RT was approximately 45 times higher than that of NSAIDs.98 The high cost of RT limits its utility, especially considering it has not been shown to be more effective than NSAID therapy.99 Other therapies currently under development and clinical testing include BMP antagonists, selective ALK receptor inhibitors, Noggin protein delivery, and retinoic acid.21
Surgical management currently remains the only effective treatment for a preformed ectopic bone. Indications for surgery include symptomatic disabilities and radiographic evidence showing the cessation of bone growth.3 Surgery should not be performed until 12 to 18 months after HO formation to allow maturation of the lesion and patient’s tissue has had time to recover to decrease intraoperative complications and HO reoccurrence.28,100 Although efficacious, surgery inherently causes tissue trauma, which can simulate the same inflammatory conditions for HO formation and is therefore complicated by high reoccurrence rates.101
Conclusions
Heterotopic ossification is a commonly seen condition occurring secondary to trauma and may cause mild to severe disability. The exact pathogenesis of this disease remains unclear; however, there is an ongoing promising research to develop prophylactic and therapeutic treatments that is promising. Distinguishing HO from other mimics help clinicians better manage the disease and improve patient care.
Disclosure
No potential conflicts of interest were disclosed.
References
- 1.Naraghi FF, DeCoster TA, Moneim MS, Miller RA, Rivero D. Heterotopic ossification. Orthopedics. 1996;19:145–51. doi: 10.3928/0147-7447-19960201-10. [DOI] [PubMed] [Google Scholar]
- 2.Kornhaber R, Foster N, Edgar D, Visentin D, Ofir E, Haik J. The development and impact of heterotopic ossification in burns: a review of four decades of research. Scars Burn Heal. 2017;3:2059513117695659. doi: 10.1177/2059513117695659. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cholok D, Chung MT, Ranganathan K, Ucer S, Day D, Davis TA. Heterotopic ossification and the elucidation of pathologic differentiation. Bone. 2018;109:12–21. doi: 10.1016/j.bone.2017.09.019. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bedi A, Zbeda RM, Bueno VF, Downie B, Dolan M, Kelly BT. The incidence of heterotopic ossification after hip arthroscopy. Am J Sports Med. 2012;40:854–63. doi: 10.1177/0363546511434285. [DOI] [PubMed] [Google Scholar]
- 5.Cipriano CA, Pill SG, Keenan MA. Heterotopic ossification following traumatic brain injury and spinal cord injury. J Am Acad Orthop Surg. 2009;17:689–97. doi: 10.5435/00124635-200911000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Medina A, Shankowsky H, Savaryn B, Shukalak B, Tredget EE. Characterization of heterotopic ossification in burn patients. J Burn Care Res. 2014;35:251–6. doi: 10.1097/BCR.0b013e3182957768. [DOI] [PubMed] [Google Scholar]
- 7.Forsberg JA, Pepek JM, Wagner S, Wilson K, Flint J, Andersen RC. Heterotopic ossification in high-energy wartime extremity injuries: prevalence and risk factors. J Bone Joint Surg Am. 2009;91:1084–91. doi: 10.2106/JBJS.H.00792. et al. [DOI] [PubMed] [Google Scholar]
- 8.Potter BK, Forsberg JA, Davis TA, Evans KN, Hawksworth JS, Tadaki D. Heterotopic ossification following combat-related trauma. J Bone Joint Surg Am. 2010;92(Suppl 2):74–89. doi: 10.2106/JBJS.J.00776. et al. [DOI] [PubMed] [Google Scholar]
- 9.Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–32. [PubMed] [Google Scholar]
- 10.Shin JJ, de Sa DL, Burnham JM, Mauro CS. Refractory pain following hip arthroscopy: evaluation and management. J Hip Preserv Surg. 2018;5:3–14. doi: 10.1093/jhps/hnx047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Popovic M, Agarwal A, Zhang L, Yip C, Kreder HJ, Nousiainen MT. Radiotherapy for the prophylaxis of heterotopic ossification: A systematic review and meta-analysis of published data. Radiother Oncol. 2014;113:10–7. doi: 10.1016/j.radonc.2014.08.025. et al. [DOI] [PubMed] [Google Scholar]
- 12.Pignolo RJ, Bedford-Gay C, Liljesthrom M, Durbin-Johnson BP, Shore EM, Rocke DM. The natural history of flare-ups in fibrodysplasia ossificans progressiva (FOP): A comprehensive global assessment. J Bone Miner Res. 2016;31:650–6. doi: 10.1002/jbmr.2728. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orchard GR, Paratz JD, Blot S, Roberts JA. Risk factors in hospitalized patients with burn injuries for developing heterotopic ossification- A retrospective analysis. J Burn Care Res. 2015;36:465–70. doi: 10.1097/BCR.0000000000000123. [DOI] [PubMed] [Google Scholar]
- 14.Jackson WM, Aragon AB, Onodera J, Koehler SM, Ji Y, Bulken-Hoover JD. Cytokine expression in muscle following traumatic injury. J Orthop Res. 2011;29:1613–20. doi: 10.1002/jor.21354. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baird EO, Kang QK. Prophylaxis of heterotopic ossification - an updated review. J Orthop Surg Res. 2009;4:12. doi: 10.1186/1749-799X-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wosczyna MN, Biswas AA, Cogswell CA, Goldhamer DJ. Multipotent progenitors resident in the skeletal muscle interstitium exhibit robust BMP-dependent osteogenic activity and mediate heterotopic ossification. J Bone Miner Res. 2012;27:1004–17. doi: 10.1002/jbmr.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cairns DM, Liu R, Sen M, Canner JP, Schindeler A, Little DG. Interplay of Nkx3.2, Sox9 and Pax3 regulates chondrogenic differentiation of muscle progenitor cells. PloS one. 2012;7:e39642–e. doi: 10.1371/journal.pone.0039642. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lounev VY, Ramachandran R, Wosczyna MN, Yamamoto M, Maidment AD, Shore EM. Identification of progenitor cells that contribute to heterotopic skeletogenesis. J Bone Joint Surg Am. 2009;91:652–63. doi: 10.2106/JBJS.H.01177. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang X, Jie S, Liu T, Zhang X. Acquired heterotopic ossification in hips and knees following encephalitis: case report and literature review. BMC Surg. 2014;14:74. doi: 10.1186/1471-2482-14-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chalmers J, Gray DH, Rush J. Observations on the induction of bone in soft tissues. J Bone Joint Surg Br. 1975;57:36–45. [PubMed] [Google Scholar]
- 21.Shimono K, Uchibe K, Kuboki T, Iwamoto M. The pathophysiology of heterotopic ossification: current treatment considerations in dentistry. Jpn Dent Sci Rev. 2014;50:1–8. doi: 10.1016/j.jdsr.2013.07.003. [DOI] [Google Scholar]
- 22.Bidner SM, Rubins IM, Desjardins JV, Zukor DJ, Goltzman D. Evidence for a humoral mechanism for enhanced osteogenesis after head injury. J Bone Joint Surg Am. 1990;72:1144–9. [PubMed] [Google Scholar]
- 23.Salisbury E, Rodenberg E, Sonnet C, Hipp J, Gannon FH, Vadakkan TJ. Sensory nerve induced inflammation contributes to heterotopic ossification. J Cell Biochem. 2011;112:2748–58. doi: 10.1002/jcb.23225. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kan L, Kitterman JA, Procissi D, Chakkalakal S, Peng C-Y, McGuire TL. CNS demyelination in fibrodysplasia ossificans progressiva. J Neurol. 2012;259:2644–55. doi: 10.1007/s00415-012-6563-x. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shehab D, Elgazzar AH, Collier BD. Heterotopic ossification. J Nucl Med. 2002;43:346–53. [PubMed] [Google Scholar]
- 26.Rossier AB, Bussat P, Infante F, Zender R, Courvoisier B, Muhelm G. Current facts of para-osteo-arthropathy (POA) Paraplegia. 1973;11:38–78. doi: 10.1038/sc.1973.5. et al. [DOI] [PubMed] [Google Scholar]
- 27.Wharton GW, Morgan TH. Ankylosis in the paralyzed patient. J Bone Joint Surg Am. 1970;52:105–12. [PubMed] [Google Scholar]
- 28.Freed JH, Hahn H, Menter R, Dillon T. The use of the three-phase bone scan in the early diagnosis of heterotopic ossification (HO) and in the evaluation of Didronel therapy. Paraplegia. 1982;20:208–16. doi: 10.1038/sc.1982.39. [DOI] [PubMed] [Google Scholar]
- 29.Zagarella A, Impellizzeri E, Maiolino R, Attolini R, Castoldi MC. Pelvic heterotopic ossification: when CT comes to the aid of MR imaging. Insights Imaging. 2013;4:595–603. doi: 10.1007/s13244-013-0265-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Svircev JN, Wallbom AS. False-negative triple-phase bone scans in spinal cord injury to detect clinically suspect heterotopic ossification: a case series. J Spinal Cord Med. 2008;31:194–6. doi: 10.1080/10790268.2008.11760711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schurch B, Capaul M, Vallotton MB, Rossier AB. Prostaglandin E2 measurements: their value in the early diagnosis of heterotopic ossification in spinal cord injury patients. Arch Phys Med Rehabil. 1997;78:687–91. doi: 10.1016/S0003-9993(97)90074-5. [DOI] [PubMed] [Google Scholar]
- 32.Orzel JA, Rudd TG. Heterotopic bone formation: clinical, laboratory, and imaging correlation. J Nucl Med. 1985;26:125–32. [PubMed] [Google Scholar]
- 33.Daniel Shawn Moore MCEFSC, MD, MBA. Heterotopic Ossification Imaging: Medscape. 2015. https://emedicine.medscape.com/article/390416-overview [updated Nov 01, 2015] Available from.
- 34.Lacout A, Jarraya M, Marcy P-Y, Thariat J, Carlier RY. Myositis ossificans imaging: keys to successful diagnosis. Indian J Radiol Imaging. 2012;22:35–9. doi: 10.4103/0971-3026.95402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kransdorf MJ, Meis JM, Jelinek JS. Myositis ossificans: MR appearance with radiologic-pathologic correlation. AJR Am J Roentgenol. 1991;157:1243–8. doi: 10.2214/ajr.157.6.1950874. [DOI] [PubMed] [Google Scholar]
- 36.De Smet AA, Norris MA, Fisher DR. Magnetic resonance imaging of myositis ossificans: analysis of seven cases. Skeletal Radiol. 1992;21:503–7. doi: 10.1007/BF00195231. [DOI] [PubMed] [Google Scholar]
- 37.Shirkhoda A, Armin AR, Bis KG, Makris J, Irwin RB, Shetty AN. MR imaging of myositis ossificans: variable patterns at different stages. J Magn Reson Imaging. 1995;5:287–92. doi: 10.1002/jmri.1880050312. [DOI] [PubMed] [Google Scholar]
- 38.Parikh J, Hyare H, Saifuddin A. The imaging features of post-traumatic myositis ossificans, with emphasis on MRI. Clin Radiol. 2002;57:1058–66. doi: 10.1053/crad.2002.1120. [DOI] [PubMed] [Google Scholar]
- 39.Ledermann HP, Schweitzer ME, Morrison WB. Pelvic heterotopic ossification: MR imaging characteristics. Radiology. 2002;222:189–95. doi: 10.1148/radiol.2221010552. [DOI] [PubMed] [Google Scholar]
- 40.Choi YH, Kim KE, Lim SH, Lim JY. Early presentation of heterotopic ossification mimicking pyomyositis - two case reports. Ann Rehabil Med. 2012;36:713–8. doi: 10.5535/arm.2012.36.5.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Siegel MJ. Magnetic resonance imaging of musculoskeletal soft tissue masses. Radiol Clin North Am. 2001;39:701–20. doi: 10.1016/S0033-8389(05)70306-7. [DOI] [PubMed] [Google Scholar]
- 42.Chan WP. Magnetic resonance imaging of soft-tissue tumors of the extremities: A practical approach. World J Radiol. 2013;5:455–9. doi: 10.4329/wjr.v5.i12.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Falsetti P, Acciai C, Lenzi L, Frediani B. Ultrasound of enthesopathy in rheumatic diseases. Mod Rheumatol. 2009;19:103–13. doi: 10.1007/s10165-008-0129-x. [DOI] [PubMed] [Google Scholar]
- 44.Frediani B, Filippou G, Falsetti P, Lorenzini S, Baldi F, Acciai C. Diagnosis of calcium pyrophosphate dihydrate crystal deposition disease: ultrasonographic criteria proposed. Ann Rheum Dis. 2005;64:638–40. doi: 10.1136/ard.2004.024109. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Falsetti P, Acciai C, Palilla R, Carpinteri F, Patrizio C, Lenzi L. Bedside ultrasound in early diagnosis of neurogenic heterotopic ossification in patients with acquired brain injury. Clin Neurol Neurosurg. 2011;113:22–7. doi: 10.1016/j.clineuro.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 46.Stefanidis K, Brindley P, Ramnarine R, Blaivas M, Daneshi M, Sidhu PS. Bedside ultrasound to facilitate early diagnosis and ease of follow-up in neurogenic heterotopic ossification: A pilot study from the intensive care unit. J Head Trauma Rehabil. 2017;32:E54–e8. doi: 10.1097/HTR.0000000000000293. et al. [DOI] [PubMed] [Google Scholar]
- 47.Wang Q, Zhang P, Li P, Song X, Hu H, Li X. Ultrasonography monitoring of trauma-induced heterotopic ossification: guidance for rehabilitation procedures. Front Neurol. 2018;9:771. doi: 10.3389/fneur.2018.00771. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Amar E, Sharfman ZT, Rath E. Heterotopic ossification after hip arthroscopy. J Hip Preserv Surg. 2015;2:355–63. doi: 10.1093/jhps/hnv052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Della Valle AG, Ruzo PS, Pavone V, Tolo E, Mintz DN, Salvati EA. Heterotopic ossification after total hip arthroplasty: a critical analysis of the Brooker classification and proposal of a simplified rating system. J Arthroplasty. 2002;17:870–5. doi: 10.1054/arth.2002.34819. [DOI] [PubMed] [Google Scholar]
- 50.Schmidt J, Hackenbroch MH. A new classification for heterotopic ossifications in total hip arthroplasty considering the surgical approach. Arch Orthop Trauma Surg. 1996;115:339–43. doi: 10.1007/BF00420328. [DOI] [PubMed] [Google Scholar]
- 51.Jeon SW, Park YK, Chang SG. Dystrophic calcification and stone formation on the entire bladder neck after potassium-titanyl phosphate laser vaporization for the prostate: a case report. J Korean Med Sci. 2009;24:741–3. doi: 10.3346/jkms.2009.24.4.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tristano AG, Villarroel JL, Rodriguez MA, Millan A. Calcinosis cutis universalis in a patient with systemic lupus erythematosus. Clin Rheumatol. 2006;25:70–4. doi: 10.1007/s10067-005-1134-5. [DOI] [PubMed] [Google Scholar]
- 53.Hwang Z-A, Suh KJ, Chen D, Chan WP, Wu JS. Imaging features of soft-tissue calcifications and related diseases: a systematic approach. Korean J Radiol. 2018;19:1147–60. doi: 10.3348/kjr.2018.19.6.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Freire V, Moser TP, Lepage-Saucier M. Radiological identification and analysis of soft tissue musculoskeletal calcifications. Insights Imaging. 2018;9:477–92. doi: 10.1007/s13244-018-0619-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ragsdale BD, Madewell JE, Sweet DE. Radiologic and pathologic analysis of solitary bone lesions. Part II: periosteal reactions. Radiol Clin North Am. 1981;19:749–83. [PubMed] [Google Scholar]
- 56.Miksanek J, Rosenthal AK. Imaging of calcium pyrophosphate deposition disease. Curr Rheumatol Rep. 2015;17:20. doi: 10.1007/s11926-015-0496-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Villiaumey J, Avouac B. [Role of radiology in the diagnosis of joint chondro-calcinosis]. [Fench] The so-called atypical symptomatic aspects. J Radiol. 1994;75:339–61. [PubMed] [Google Scholar]
- 58.Helms C. Fundamentals of Skeletal Radiology. Amsterdam: Elsevier; 2014. 4th Edition. [Google Scholar]
- 59.Fathi I, Sakr M. Review of tumoral calcinosis: a rare clinico-pathological entity. World J Clin Cases. 2014;2:409–14. doi: 10.12998/wjcc.v2.i9.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Topaz O, Shurman DL, Bergman R, Indelman M, Ratajczak P, Mizrachi M. Mutations in GALNT3, encoding a protein involved in O-linked glycosylation, cause familial tumoral calcinosis. Nat Genet. 2004;36:579–81. doi: 10.1038/ng1358. et al. [DOI] [PubMed] [Google Scholar]
- 61.Benet-Pages A, Orlik P, Strom TM, Lorenz-Depiereux B. An FGF23 missense mutation causes familial tumoral calcinosis with hyperphosphatemia. Hum Mol Genet. 2005;14:385–90. doi: 10.1093/hmg/ddi034. [DOI] [PubMed] [Google Scholar]
- 62.Kim H-S, Suh JS, Kim YH, Park S-H. Tumoral calcinosis of the hand: Three unusual cases with painful swelling of small joints. Arch Pathol Lab Med 2006. 2006;130:548–51. doi: 10.1043/1543-2165. 130[548:TCOTHT]2.0. CO;2. [DOI] [PubMed] [Google Scholar]
- 63.Asuncion GF, Tzarnas CD. Uremic tumoral calcinosis: acute hand presentations mimicking infection. J Hand Surg Am. 1994;19:809–12. doi: 10.1016/0363-5023(94)90190-2. [DOI] [PubMed] [Google Scholar]
- 64.Pakasa NM, Kalengayi RM. Tumoral calcinosis: a clinicopathological study of 111 cases with emphasis on the earliest changes. Histopathology. 1997;31:18–24. doi: 10.1046/j.1365-2559.1997.6050831.x. [DOI] [PubMed] [Google Scholar]
- 65.Meltzer CC, Fishman EK, Scott WW Jr.. Tumoral calcinosis causing bone erosion in a renal dialysis patient. Clin Imaging. 1992;16:49–51. doi: 10.1016/0899-7071(92)90091-M. [DOI] [PubMed] [Google Scholar]
- 66.Olsen KM, Chew FS. Tumoral calcinosis: Pearls, polemics, and alternative possibilities. Radiographics. 2006;26:871–85. doi: 10.1148/rg.263055099. [DOI] [PubMed] [Google Scholar]
- 67.Stevens MA, El-Khoury GY, Kathol MH, Brandser EA, Chow S. Imaging features of avulsion injuries. Radiographics. 1999;19:655–72. doi: 10.1148/radiographics.19.3.g99ma05655. [DOI] [PubMed] [Google Scholar]
- 68.Ritter J, Bielack SS. Osteosarcoma. Ann Oncol. 2010;21(Suppl 7):vii320–5. doi: 10.1093/annonc/mdq276. [DOI] [PubMed] [Google Scholar]
- 69.Bielack S, Jurgens H, Jundt G, Kevric M, Kuhne T, Reichardt P. Osteosarcoma: the COSS experience. Cancer Treat Res. 2009;152:289–308. doi: 10.1007/978-1-4419-0284-9_15. et al. [DOI] [PubMed] [Google Scholar]
- 70.Park SK, Lee IS, Cho KH, Lee YH, Yi JH, Choi KU. Osteosarcoma of pelvic bones: imaging features. Clin Imaging. 2017;41:59–64. doi: 10.1016/j.clinimag.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 71.Dosda R, Marti-Bonmati L, Menor F, Aparisi F, Rodrigo C, Ricart V. Comparison of plain radiographs and magnetic resonance images in the evaluation of periosteal reaction and osteoid matrix in osteosarcomas. MAGMA. 1999;9:72–80. doi: 10.1007/BF02634595. [DOI] [PubMed] [Google Scholar]
- 72.McQueen FM, Doyle A, Dalbeth N. Imaging in gout--what can we learn from MRI, CT, DECT and US? Arthritis Res Ther. 2011;13:246. doi: 10.1186/ar34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barthelemy CR, Nakayama DA. Carrera GF, Lightfoot RWJr., Wortmann RL. Gouty arthritis: a prospective radiographic evaluation of sixty patients. Skeletal Radiol. 1984;11:1–8. doi: 10.1007/BF00361124. 89. [DOI] [PubMed] [Google Scholar]
- 74.Dalbeth N, Clark B, McQueen F, Doyle A, Taylor W. Validation of a radiographic damage index in chronic gout. Arthritis Rheum. 2007;57:1067–73. doi: 10.1002/art.22891. [DOI] [PubMed] [Google Scholar]
- 75.Girish G, Glazebrook KN, Jacobson JA. Advanced imaging in gout. AJR Am J Roentgenol. 2013;201:515–25. doi: 10.2214/AJR.13.10776. [DOI] [PubMed] [Google Scholar]
- 76.Oliva F, Via AG, Maffulli N. Physiopathology of intratendinous calcific deposition. BMC Med. 2012;10:95. doi: 10.1186/1741-7015-10-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Siegal DS, Wu JS, Newman JS, Del Cura JL, Hochman MG. Calcific tendinitis: a pictorial review. Can Assoc Radiol J. 2009;60:263–72. doi: 10.1016/j.carj.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 78.Harvie P, Pollard TC, Carr AJ. Calcific tendinitis: natural history and association with endocrine disorders. J Shoulder Elbow Surg. 2007;16:169–73. doi: 10.1016/j.jse.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 79.Uhthoff HK, Loehr JW. Calcific tendinopathy of the rotator cuff: Pathogenesis, diagnosis, and management. J Am Acad Orthop Surg. 1997;5:183–91. doi: 10.5435/00124635-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 80.Bazzocchi A, Pelotti P, Serraino S, Battaglia M, Bettelli G, Fusaro I. Ultrasound imaging-guided percutaneous treatment of rotator cuff calcific tendinitis: success in short-term outcome. Br J Radiol. 2016;89:20150407. doi: 10.1259/bjr.20150407. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Norenberg D, Ebersberger HU, Walter T, Ockert B, Knobloch G, Diederichs G. Diagnosis of calcific tendonitis of the rotator Cuff by Using Susceptibility-weighted MR Imaging. Radiology. 2016;278:475–84. doi: 10.1148/radiol.2015150034. et al. [DOI] [PubMed] [Google Scholar]
- 82.Kaplan FS, Le Merrer M, Glaser DL, Pignolo RJ, Goldsby RE, Kitterman JA. Fibrodysplasia ossificans progressiva. Best Pract Res Clin Rheumatol. 2008;22:191–205. doi: 10.1016/j.berh.2007.11.007. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shore EM, Xu M, Feldman GJ, Fenstermacher DA, Cho TJ, Choi IH. A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nat Genet. 2006;38:525–7. doi: 10.1038/ng1783. et al. [DOI] [PubMed] [Google Scholar]
- 84.Cohen RB, Hahn GV, Tabas JA, Peeper J, Levitz CL, Sando A. The natural history of heterotopic ossification in patients who have fibrodysplasia ossificans progressiva. A study of forty-four patients. J Bone Joint Surg Am. 1993;75:215–9. doi: 10.2106/00004623-199302000-00008. et al. [DOI] [PubMed] [Google Scholar]
- 85.Klang A, Kneissl S, Glanzel R, Fuchs-Baumgartinger A. Imaging diagnosis: fibrodysplasia ossificans progressiva in a cat. Vet Radiol Ultrasound. 2013;54:532–5. doi: 10.1111/vru.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Karunakar MA, Sen A, Bosse MJ, Sims SH, Goulet JA, Kellam JF. Indometacin as prophylaxis for heterotopic ossification after the operative treatment of fractures of the acetabulum. J Bone Joint Surg Br. 2006;88:1613–7. doi: 10.1302/0301-620X.88B12.18151. [DOI] [PubMed] [Google Scholar]
- 87.Pavlou G, Kyrkos M, Tsialogiannis E, Korres N, Tsiridis E. Pharmacological treatment of heterotopic ossification following hip surgery: an update. Expert Opin Pharmacother. 2012;13:619–22. doi: 10.1517/14656566.2012.662342. [DOI] [PubMed] [Google Scholar]
- 88.Fransen M, Anderson C, Douglas J, MacMahon S, Neal B, Norton R. Safety and efficacy of routine postoperative ibuprofen for pain and disability related to ectopic bone formation after hip replacement surgery (HIPAID): randomised controlled trial. BMJ. 2006;333:519. doi: 10.1136/bmj.38925.471146.4F. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fransen M, Neal B. Non-steroidal anti-inflammatory drugs for preventing heterotopic bone formation after hip arthroplasty. Cochrane Database Syst Rev. 2004 doi: 10.1002/14651858.CD001160.pub2. Cd001160. [DOI] [PubMed] [Google Scholar]
- 90.Barbato M, D’Angelo E, Di Loreto G, Menna A, Di Francesco A, Salini V. Adherence to routine use of pharmacological prophylaxis of heterotopic ossification after total hip arthroplasty: results from an Italian multicenter, prospective, observational survey. J Orthop Traumatol. 2012;13:63–7. doi: 10.1007/s10195-012-0180-4. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vuolteenaho K, Moilanen T, Moilanen E. Non-steroidal anti-inflammatory drugs, cyclooxygenase-2 and the bone healing process. Basic Clin Pharmacol Toxicol. 2008;102:10–4. doi: 10.1111/j.1742-7843.2007.00149.x. [DOI] [PubMed] [Google Scholar]
- 92.Chang JK, Li CJ, Wu SC, Yeh CH, Chen CH, Fu YC. Effects of anti-inflammatory drugs on proliferation, cytotoxicity and osteogenesis in bone marrow mesenchymal stem cells. Biochem Pharmacol. 2007;74:1371–82. doi: 10.1016/j.bcp.2007.06.047. et al. [DOI] [PubMed] [Google Scholar]
- 93.Sell S, Willms R, Jany R, Esenwein S, Gaissmaier C, Martini F. The suppression of heterotopic ossifications: radiation versus NSAID therapy--a prospective study. J Arthroplasty. 1998;13:854–9. doi: 10.1016/S0883-5403(98)90189-9. et al. [DOI] [PubMed] [Google Scholar]
- 94.Macfarlane RJ, Ng BH, Gamie Z, El Masry MA, Velonis S, Schizas C. Pharmacological treatment of heterotopic ossification following hip and acetabular surgery. Expert Opin Pharmacother. 2008;9:767–86. doi: 10.1517/14656566.9.5.767. et al. [DOI] [PubMed] [Google Scholar]
- 95.Coventry MB, Scanlon PW. The use of radiation to discourage ectopic bone. A nine-year study in surgery about the hip. J Bone Joint Surg Am. 1981;63:201–8. doi: 10.2106/00004623-198163020-00004. [DOI] [PubMed] [Google Scholar]
- 96.Childs HA. Cole T, Falkenberg E, Smith JT, Alonso JE, Stannard JP. A prospective evaluation of the timing of postoperative radiotherapy for preventing heterotopic ossification following traumatic acetabular fractures. Int J Radiat Oncol Biol Phy. 2000;47:1347–52. doi: 10.1016/S0360-3016(00)00582-4. 3rd. et al. [DOI] [PubMed] [Google Scholar]
- 97.Chao ST, Lee SY, Borden LS, Joyce MJ, Krebs VE, Suh JH. External beam radiation helps prevent heterotopic bone formation in patients with a history of heterotopic ossification. J Arthroplasty. 2006;21:731–6. doi: 10.1016/j.arth.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 98.Strauss JB, Chen SS, Shah AP, Coon AB, Dickler A. Cost of radiotherapy versus NSAID administration for prevention of heterotopic ossification after total hip arthroplasty. Int J Radiat Oncol Biol Phy. 2008;71:1460–4. doi: 10.1016/j.ijrobp.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 99.Vavken P, Castellani L, Sculco TP. Prophylaxis of heterotopic ossification of the hip: systematic review and meta-analysis. Clin Orthop Relat Res. 2009;467:3283–9. doi: 10.1007/s11999-009-0924-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mavrogenis AF, Soucacos PN, Papagelopoulos PJ. Heterotopic ossification revisited. Orthopedics. 2011;34:177. doi: 10.3928/01477447-20110124-08. [DOI] [PubMed] [Google Scholar]
- 101.Agarwal S, Loder S, Cholok D, Li J, Breuler C, Drake J. Surgical excision of heterotopic ossification leads to re-emergence of mesenchymal stem cell populations responsible for recurrence. Stem Cells Transl Med. 2017;6:799–806. doi: 10.5966/sctm.2015-0365. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]


