Abstract
Anxiety is currently one of the main mood changes and can impair the quality of life of the individual when associated with other neurological or psychiatric disorders. Neuromodulation has been highlighted as a form of treatment of several pathologies, including those involving anxiety symptoms. Among the neuromodulatory options with the potential to improve mood changes, we highlight repetitive transcranial magnetic stimulation (rTMS). rTMS is a viable therapeutical option for neuropsychiatric dysfunctions of high prevalence and is important for the understanding of pathological and neuropsychological adaptation processes. Even with this potential, and high relevance of intervention, we observe the scarcity of literature that covers this subject. The objective of this study was to carry out a survey of the current literature, using scientific databases for the last five years. We found 32 studies reporting the effects of rTMS on anxiety, 7 on anxiety disorders and 25 on anxiety symptoms as comorbidities of neurological or psychiatric disorders. This survey suggests the need for further studies using TMS for anxiety in order to seek strategies that minimize these anxiety effects on the quality of life of the victims of this disorder.
Keywords: transcranial magnetic stimulation, anxiety disorders, review, treatment
Introduction
Individuals may experience anxiety as a warning sign in unknown situations, especially in response to fear and anticipation of danger.1 However, it is considered pathological when it directly affects the individual’s quality of life, affecting social relations, cognitive function, and the wake–sleep cycle.2–4 Anxiety disorders represent one of the major psychiatric disorders today that can impair the quality of life of adults.2–4
The Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition (DSM-5) defines the presence of an anxiety disorder when some criteria are met, for example: symptoms occurring more than six months, excessive anxiety and worry, panic attacks, restlessness or feeling nervous, fatigue, irritability, sleep and eating disorder. Based on the symptomatology, anxiety disorders can be classified in: Generalized Anxiety Disorder (GAD), Social Anxiety Disorder, Panic Disorder (PD), Agoraphobia, Separation Anxiety Disorder, Selective Mutism and Specific Phobias. In addition to anxiety disorders, anxiety can be a symptom or comorbidity in several other pathologies, such as Major Depression,5 Obsessive Compulsive Disorder,6 TBI,7 among others.
Neuromodulation minimizes the impact of mood changes8–11 and repetitive transcranial magnetic stimulation (rTMS) is receiving attention in the last decade.12,17 TMS is a non-invasive method of stimulating the motor cortex neurons through the scalp and skull based on the principle of electromagnetic induction.18,19 TMS was approved by the Food and Drug Administration (FDA) in 2008 as an alternative treatment for Major Depression Disorder,20 and has been shown to decrease the symptoms of Post Traumatic Stress Disorder (PTSD),21 Obsessive Compulsive Disorder (OCD),22 and Anxiety Disorders.14
Non-invasive brain stimulation techniques allow researchers to study in real-time the human brain activity, characterize the balance of excitation and cortical inhibition, and help guide plastic changes.8 With TMS, you can apply repetitive induced current pulses that can increase or decrease cortical excitability and stimulate the process of neuronal plasticity.9,23,24 A coil of wire is placed on the scalp generating an electric current that flows through the target area, inducing neuronal depolarization. Possible effects are depended on subject’s age, pharmacological treatment, number of technical parameters, including the intensity and number of stimulations (ie, frequency), coil orientation, focus, and depth of stimulation.9,25,26
Although TMS pulses (simple and repetitive) are considered safe, it is contraindicated for people who use a pacemaker or other implantable electronic devices.21,27 Patients with bone defects and craniotomy pose another concern, because the conductance of the structures would be modified.21,24 Some adverse effects might occur, such as headache and minor muscle spasms at the stimulation site.21,25,28,29
Recent literature reviews discussed the use of TMS as an intervention strategy for anxiety. Vicario et al's30 study addressed the use of TMS and transcranial direct current stimulation (tDCS) and other studies portray its efficacy for other psychiatric disorders, without major insights.14,30–32 However, there is a gap in the literature regarding rTMS efficacy in anxiety symptoms (primary and secondary outcomes) in clinical trials. Our study focused on the effectiveness of TMS for Anxiety Disorders and as an intervention for Anxiety Symptoms arising from other pathologies. We make the division between anxiety arising from Neurological Disorders and Psychiatric Disorders. Our hypothesis was that high-frequency rTMS on the dorsolateral prefrontal cortex (DLPFC) will decrease anxiety symptoms in patients with anxiety disorders, considering anxiety as the primary outcome.
Methods
We conducted a literature online search including Web of Science Medline/PubMed MEDLINE databases. We have included publications from any time until March 2019. We included clinical trial and open-label using the keywords: “TMS”, “transcranial magnetic stimulation”, “noninvasive brain stimulation”, and “anxiety”. The first exclusion was by title and followed by abstracts and full texts. Abstracts and full text, and studies were included if fulfilled, the inclusion criteria: (a) use of rTMS as intervention; (b) anxiety was assessed as primary or secondary outcome; (c) sample was adults; (d) published in peer-review journals; (e) full text written in English. The exclusion criteria: (a) animal studies; (b) case report; (c) systematic review or meta-analysis; (d) paper not written in English; (e) study with healthy; and (f) studies that did not report the use of rTMS in anxiety symptoms. Searching and data analysis were performed by Rodrigues PA and Zaninotto AL. This method follows PRISMA guidelines.
Results
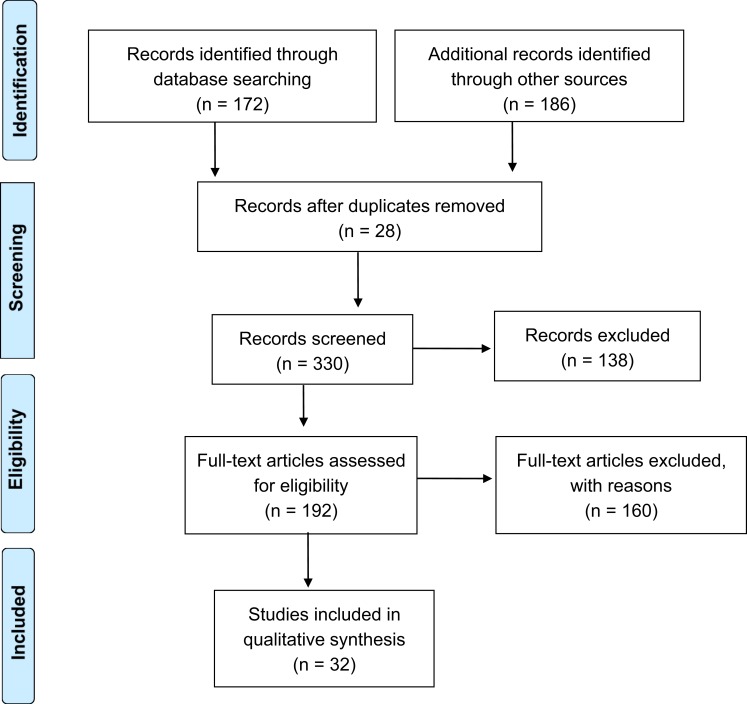
Figure 1 shows the systematic review that initially 358 papers were found (Pubmed =172; Web of Science =186). We found 32 studies that fulfilled our eligibility criteria.
Figure 1.
Flow diagram of the papers selected in our study, following PRISMA statement guidelines.
For a better understanding of the results, we divided the target population of the trials in two categories: Category 1) patients with Anxiety Disorders, according to DSM-5 (Table 1); Category 2) Anxiety symptoms, from neurological and psychiatric disorders that also evaluated anxiety symptoms as comorbidity (Table 2).
Table 1.
Patients with anxiety disorders, according to DSM 5
| Author/Year | Patient/Sham group | Diagnosis | Study design | Target | # of rTMS sessions | Frequency | Pulses per session | Stimulation intensity | NP tests | Relevant results following treatment | Tolerability and safety | Sustained effect of response |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Zhang, 201937 | 117 rTMS | Mood or Anxiety Disorders | RCT | Left DLPFC | 10 | 10 Hz | 2400 | 120% of RMT | HAMA | All the age groups showed significant improvements in clinical symptoms | No safety or tolerability concerns were identified | Yes for adolescents, but not in adults |
| Lu R, 201838 | 28 rTMS | GAD | Open-label | Right DLPFC + left DLPFC | 10 | 1 Hz | 750 | 80% of RMT | HRSA | In this study, low-frequency rTMS which was successively delivered to right and left DLPFC effectively alleviated anxiety symptoms in GAD patients | All patients tolerated rTMS well without any adverse effects | Yes |
| Dilkov D, 201733 | 9 rTMS/12 sham | GAD | RCT | Right DLPFC | 25 | 20 Hz | 3600 | 110% of RMT | HRSA | Participants receiving rTMS showed clinically significant decrease in reported anxiety symptoms. | One participant in the active group had seizure; transient dizziness was reported in three patients | Yes |
| Diefenbach GJ, 201635 | 13 rTMS/12 sham | GAD | RCT | Right DLPFC | 30 | 1 Hz | 900 | 90% of RMT | HRSA; DASS | ANOVA demonstrated significant group x time interaction for the primary and secondary outcomes with the gains maintained only in the rTMS group at follow-up. | No seizures occurred; mild adverse effects were reported and was similar in rTMS and sham groups | Yes |
| White D and Tavakoli S, 20155 | 13 rTMS | Comorbid MDD and GAD | Open-label, pilot study | Right DLPFC + left DLPFC | 2436 | 1Hz (right side)+10hz (left side) | 1000 | NR | GAD-7 | Paired T-test comparing baseline to final scores showed a markedly significant difference for both GAD-7 and the HDRS-21, suggesting a decrease of 65% and 75% in depression and anxiety, respectively. | NR | Not applicable |
| Mantovani A, 201334 | 12 rTMS/13 sham | PD and comorbid MDD | RCT. Two phases: Phase I 4-week double-blind followed by Phase II (optional) 4-week open-label | Right DLPFC | Phase I: 20; Phase II: 20 | 1Hz | 1800 | 110% of RMT | PDSS; HRSA-14 | Repeated-measures ANOVA revealed a significant time by group interaction with PDSS, with greater reduction in active group. | No seizures were reported. None of the patients reported significant side effects | Yes |
| Prasko J, 200736 | 7 rTMS/8 sham | PD or PD with agoraphobia | RCT | Right DLPFC | 10 | 1 Hz | 1800 | 110% of RMT | HRSA; BAI; PDSS | No statistical difference between groups were observed after treatment. | No seizures, headaches, neurological and cognitive decline occurred | Not applicable |
Abbreviations: BAI, Beck Anxiety Inventory; DASS, Depression Anxiety Stress Scales; DLPFC, Dorsolateral Prefrontal Cortex; GAD, Generalized Anxiety Disorder; GAD-7, Generalized Anxiety Disorder scale; HAMA, Hamilton Rating Scale for Anxiety; HRSA, Hamilton Rating Scale for Anxiety; MDD, major depressive disorder; NP, neuropsychological; NR, Not Reported; PD, Panic Disorder; PDSS, Panic Disorder Severity Scale; RCT, Randomized Controlled Trial; RMT, Resting Motor Threshold; rTMS, repetitive Transcranial Magnetic Stimulation.
Table 2.
Anxiety symptoms, from neurological and psychiatric disorders
| Author/Year | Patient/Sham group | Diagnosis | Study design | Target | # of rTMS sessions | Frequency | Pulses per session | Stimulation intensity | Anxiety questionnaire | Primary outcome | Relevant results following treatment | Tolerability and safety | Sustained effect of response |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kaur M, 201939 | 16 rTMS | Mood disorders | Open-label | Left DLPFC | 20 | 10 Hz | NR | 110% of RMT | Anxiety subscale of the HDRS | To determine whether sleep–wake disturbance, cognition or depression chronicity are associated with rTMS outcome in young depressed adults | Show reduced depressive and anxiety symptoms and no cognitive deterioration | NR | Yes |
| Lin H, 201840 | 7 rTMS | Thalamic pain | Open-label | Motor cortex | 10 | 10 Hz | 1000 | 90% of RMT | HAMA | To evaluate the analgesic lasting effect to treat thalamic pain | High-frequency rTMS can provide long-term pain relief in patients with thalamic pain |
All patients tolerated rTMS well with out any adverse effects | No |
| Reyes-Lopez. J, 201841 | 29 rTMS | Borderline | RCT | Right DLPFC + left DLPFC | 15 | 5 Hz or 1 Hz | 900 or 1500 | 100% of RMT | HRSA | To evaluate clinical improvement in patients with BPD after application of rTMS |
HAM-A scores reduced after rTMS treatment. Both protocols produced global improvement in severity and symptoms of BPD, particularly in impulsiveness, affective instability, and anger | NR | Yes |
| Durmaz O, 201742 | 36 rTMS | MDD | Open-label | Left DLPFC | 15 | 20 Hz | 1000 | 110% of RMT | HRSA | To evaluate the efficacy of rTMS in patients with treatment-resistant major depression | The findings suggested that comorbid anxiety symptoms, particularly somatic anxiety, could predict the response to rTMS in treatment-resistant major depressive disorder | Headache in eight patients, dizziness in four patients, and lacrimation in three patients. Only one patient dropped out of the study due to side effects or intolerance | Yes |
| Noh TS, 201743 | 17 rTMS | Tinnitus | RCT | Left auditory cortex (AC) and left DLPFC or only the left DLPFC | 4 | 1 Hz | 2000 or 3000 | 110% of RMT | STAI | We evaluated treatment outcomes following single-site rTMS in the DLPFC and dual-site rTMS in the AC and DLPFC |
Group 1 exhibited significant improvements in scores on the STAI for both state anxiety and trait anxiety at 12 weeks posttreatment. Group 2 showed an improvement in only the STAI-X2 score at 12 weeks posttreatment. |
NR | No |
| Tovar-Perdomo S, 201744 | 24 rTMS | MDD | Open-label, pilot study | Left DLPFC | 20 | 10 Hz | 3000 | 120% of RMT | BAI | To explore the effects of a course of accelerated high-frequency rTMS on two neurocognitive domains in patients with MDD | Depression and anxiety scores significantly improved from pre-post HF-rTMS treatment. | The absence of practice effects in our longitudinal design raises the possibility that rTMS may also have cognitive side effects which, like antidepressant effects, may recede and reveal cognitive improvements after treatment cessation and sustained recovery | No |
| Elbeh KAM, 20166 | 30 rTMS/15 sham | OCD | RCT | Right DLPFC + left DLPFC | 10 | 1 Hz or 10 Hz | 200 or 500 | 100% of RMT | HRSA | To evaluate the impact of different frequencies of rTMS in OCD | 1 Hz rTMS over the right DLPFC has medium-term effect on obsessive-compulsive symptoms and anxiety |
All patients tolerated rTMS well without any adverse effects except for two patients in the active stimulation group who experienced transient headache that disappeared with in a few hours | Yes |
| Malavera A, 201645 | 27 rTMS/27 sham | Pain | RCT | Primary Motor Cortex contralateral to the amputated leg | 10 | 10 Hz | 1200 | 90% of RMT | Zung Self-Rating Anxiety Scale | The score change in the Visual Analogue Scale for pain | No statistically significant between-group difference was found when comparing the absolute scores of the depression and anxiety scales at day 15 or day 30 |
Some patients experienced minor adverse effects such as headache, neck pain, and sleepiness without significant differences between groups | Yes |
| Bilici S, 201546 | 45 rTMS/30 sham | Tinnitus | RCT | Left temporoparietal region | 10 | 1 Hz or 10 Hz | 600 or 900 | 110% of RMT | BAS | To compare the effects of rTMS and paroxetine on tinnitus in terms of effectiveness and medium-term results | The positive effects that were observed might reflect a relationship between tinnitus and auditory cortex areas related to emotions | In the 10 Hz TMS treatment group, two patients complained of neck and shoulder stiffness, which disappeared in 2 days without any medical treatment; two patients had jaw fasciculation, which continued for 1 hr; and one patient had a headache for 1 day. One patient in the 1 Hz rTMS group had mild jaw pain for 2 days. All patients in the paroxetine-treated group were asked to report possible side effects of the drug. Among those, three had cephalalgia, two had gastrointestinal disorders, and one had sexual dysfunction; all these side effects were mild-to-moderate in intensity and did not delay the therapy | Yes |
| Lin YC, 201547 | 14 rTMS | RLS | Open-label | Motor cortex area of the frontal lobe | 14 | 15 Hz | 600 | 100% of RMT | HRSA | To investigate whether rTMS could have any beneficial effects in restless legs syndrome | rTMS can markedly alleviate the motor system symptoms, sleep disturbances, and anxiety in RLS patients | No adverse effects were observed during stimulation or after treatment, and all patients showed good compliance | Yes |
| Oznur T, 201448 | 20 rTMS | PTSD | Open-label | Right DLPFC | 20 | 1 Hz | NR | 80% of RMT | BAI | To examine the effectiveness of rTMS in patients with treatment-resistant posttraumatic stress disorder | The effectiveness of rTMS on the anxiety and depression scores in the patients was not determined in this study | NR | No |
| Diefenbach GJ, 201349 | 32 rTMS | MDD | Open-label | Left DLPFC | 31 | 10 Hz | 3000–5000 | 80 at 130% of RMT | Anxiety/somatization subscale of the HDRS | To determine if anxious depression is associated with attenuated response to rTMS | Both depression and anxiety symptoms improved from pre- to post-treatment with moderate to large treatment effects | NR | Yes |
| Pretalli JB, 201250 | 75 rTMS | MDD | RCT | Left DLPFC | 10 | 10 Hz | NR | 95% of RMT | HAMD anxiety subscale (items 9, 10, 11, and 15); Tyrer scale for anxiety; STAI | To investigate whether or not RMT changes during the treatment of resistant depression | These RMT changes influenced the outcome of the 10 sessions concerning the severity of depressive and anxiety symptoms | Only mild side-effects were reported (pain at the site of the coil placement or headache) | Yes |
| Sun W, 201251 | 60 rTMS | Focal epilepsy | RCT | Epileptogenic focus | 10 | 0.5 Hz | 1500 | 90% or 20% of RMT | SCL-90 | To evaluate the therapeutic effect of low-frequency rTMS on patients with refractory partial epilepsy | All the subscale scores of somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, paranoid ideation and psychoticism in group 1 was lower than that of group 2 when evaluated at the end of follow-up period | The most common adverse events were mild or moderate headache and tinnitus. Adverse events occurred more often in group one patients who received “90% rMT” rTMS | Yes |
| Watts BV, 201221 | 10 rTMS/10 sham | PTSD | RCT | Right DLPFC | 10 | 1 Hz | NR | 90% of RMT | STAI | This study seeks to examine the efficacy of rTMS for PTSD | Anxiety symptoms showed improvement with rTMS, but those improvements were not statistically significant compared with sham | NR | Yes |
| Berlim MT, 201152 | 15 rTMS | MDD | Open-label | Left DLPFC | 20 | 10 Hz | 3000 | 120% of RMT | HRSA; BAI | To address an augmenting strategy in subjects with chronic, severely treatment-resistant MDD | Clinically meaningful improvements in anxious and depressive symptoms | Only one of the 15 participants withdrew from the study at week 1 because of lack of tolerability (ie, severe scalp pain) | Yes |
| Boggio PS, 201053 | 20 rTMS/10 sham | PTSD | RCT | Right DLPFC or left DLPFC | 10 | 20 Hz | 1600 | 80% of RMT | HRSA | To investigate the efficacy of rTMS for the relief of posttraumatic stress disorder (PTSD)-associated symptoms | Right rTMS generated a significant improvement in the measure of anxiety at days 5 and 10 while left rTMS did not | There were no seizures and only mild adverse effects, such as mild headache, neck pain, sleepiness, and dizziness were reported similarly in the 3 groups of treatment | Yes |
| Epstein CM, 200754 | 14 rTMS | Parkinson disease | Open-label | Left DLPFC | 10 | 10 Hz | 1000 | 110% of RMT | HRSA | To investigate about rTMS as a potential treatment for depression in PD and for the movement disorder of PD | Open rTMS treatment of PD patients with treatment-resistant depression was followed by highly significant improvement in mood scores and anxiety ratings | There were no seizures and no complaints of headache or neurological deterioration | Yes |
| Passard A, 200755 | 15 rTMS/15 sham | Fibromyalgia | RCT | Left primary motor cortex | 10 | 10 Hz | 2000 | 80% of RMT | Hospital Anxiety Scale | To assess the effects of unilateral rTMS of the motor cortex on chronic widespread pain in patients with fibromyalgia | The analgesic effects were observed from the fifth stimulation onwards and were not related to changes in mood or anxiety. | Minor and transient side effects were reported during the stimulation period only. Nine patients reported headaches: four in the active-stimulation group and five in the sham stimulation group. These headaches, reported after only 1 of the 10 daily sessions, were mild and transient in all cases. Other side effects included nausea after the fifth session in one patient in the active-treatment group. Two patients reported transient tinnitus and one patient reported mild dizziness after one sham-stimulation session | Yes |
| Rossi S, 200756 | 14 rTMS | Tinnitus | Open-label | Left temporoparietal region | 5 | 1 Hz | 1200 | 120% of RMT | HRSA | To assess about rTMS on chronic tinnitus in which also eventual mood changes are monitored | In patients with chronic tinnitus, psychiatric comorbidity as mood or anxiety disorders are relevant and may partly found their functional counterpart in the activation of higher-order processing | The majority of patients did not complain of side effects due to rTMS, a part a slight transient headache on the stimulation site, which however did not require pharmacological treatment. About 30% of patients complained of tongue paraesthesia occurring during the active rTMS. Most of patients reported a transient worsening of their tinnitus in the first two–three days of active rTMS. Two male patients, one receiving active rTMS and one sham rTMS as first intervention, dropped ut from the study for this reason | Yes |
| Cohen H, 200457 | 18 rTMS/6 sham | PTSD | RCT | Right DLPFC | 10 | 1 Hz or 10 Hz | NR | 80% of RMT | HRSA | To evaluate the therapeutic effects of two different frequencies of active rTMS of PTSD patients | Active 10-Hz rTMS, relative to 1-Hz treatment and sham, significantly reduced Hamilton anxiety scale scores but not Hamilton depression scale scores | Headache was the main side effect reported, regardless of stimulation group. It was reported by 14 patients: eight patients reported headache after one rTMS treatment, five patients reported it after two sessions, and one (receiving sham treatment) reported it after three sessions. In most cases, this side effect was reported several hours after the stimulation or on the following morning. Only four patients reported headache immediately after the stimulation. In three cases, headache was a symptom before the study. However, the total number of headaches after treatment was 21. Two patients receiving high-frequency rTMS reported neck pain and muscular contraction in the area. Another patient receiving high-frequency treatment reported an exacerbation of previously existing dizziness. One patient in the group receiving slow-frequency rTMS and one patient from the high-frequency group developed a manic episode; in both cases, this occurred after the third session of rTMS. One patient reported a mild rage attack, probably related to the stimulation. Although we did not use earplugs, only two patients reported ear discomfort, which lasted less than 1 min | Yes |
| Loo CK, 200358 | 18 rTMS | MDD | RCT | Left DLPFC | NR | 15 Hz or 1 Hz | NR | 90% of RMT | 7-item scale | To understand further the mechanisms of action of high- and low-frequency rTMS by examining their acute effects on regional cerebral blood flow (rCBF) in depressed patients | Anxiety scores did not differ between the 15 Hz and 1 Hz groups. rTMS can produce functional changes in areas of the brain involved in mood control, including changes tending toward correction of deficits associated with depression | NR | Yes |
| Münchau A, 200259 | 12 rTMS | GTS | Open-label | Left premotor | 6 | 1 Hz | 1200 | 80% of RMT | Hospital Anxiety Scale | To study whether rTMS targeted to left motor and premotor cortex can improve tics in GTS | There was no significant improvement of symptoms after any of the rTMS conditions as assessed | One patient reported mild headache after premotor rTMS. Two patients reported excessive tiredness after both premotor and motor rTMS lasting for about 1 day | Yes |
| George MS, 200060 | 20 rTMS/10 sham | MDD | RCT | Left prefrontal cortex | 10 | 5 Hz or 20 Hz | NR | 100% of RMT | HRSA | To conduct a study to address whether 2 weeks of daily TMS over the left prefrontal cortex has antidepressant activity greater than sham | Expressed as a percent change from baseline, active TMS subjects had significantly greater improvement on the BDI as well as the HARS than did those who received sham | Two subjects with average MTs (60% and 70% of machine output) elected to stop the study because of the pain of stimulation. One subject tried for 2 consecutive days, whereas the other decided to stop after only 2 mins of the first session. Ten subjects reported mild headaches following at least one session (beginning immediately after to 3 hrs after rTMS), which were relieved by acetaminophen | Yes |
| Rollnik JD, 200061 | 6 rTMS/6 sham | Schizophrenia | RCT | Left DLPFC | 10 | 20 Hz | 800 | 80% of RMT | STAI | To investigate the therapeutic efficacy of rTMS in schizophrenic patients with acute exacerbation of their psychosis | STAI, BDI, and NCT scores tended to improve during active rTMS and to worsen during sham stimulation, but the observed changes were not significant. | NR | Yes |
Abbreviations: STAI, State-Trait Anxiety Inventory; HRSA, Hamilton Rating Scale for Anxiety; BAI, Beck Anxiety Inventory; HAMA, Hamilton Rating Scale for Anxiety; RMT, Resting Motor Threshold; rTMS, repetitive Transcranial Magnetic Stimulation; DLPFC, dorsolateral prefrontal cortex; MDD, major depressive disorder; PTSD, Post Traumatic Stress Disorder; RLS, Restless Legs Syndrome; OCD, Obsessive Compulsive Disorder.
Treatment for anxiety disorders
In our search, five studies were randomized double-blind clinical trial (RCT) and two studies were open-label. Seven papers described Anxiety Disorders as the main outcome for rTMS,5,33–38 one was related to Anxiety Disorders, two were Panic Disorder (PD), and the other four were GAD (Table 1). The sample size of these studies ranged from 13 to 25 patients.
The right dorsolateral prefrontal cortex (DLPFC) was the most frequent stimulation region and in one study they stimulated the left region of the DLPFC. The predominant frequency used was 1 Hz, although one study compared the use of 1 hz and 10 hz and another used only 20 Hz.
The number of sessions ranged between 10 and 30 and the number of pulses per stimulation ranged from 750 to 3600. Most papers used an intensity of 110% of the rest motor threshold (RMT), one used 80% and other used 90% of RMT and one study did not specify.
Treatment for other psychiatric neurological diseases
We found 23 studies reporting rTMS as an alternative for the treatment of neurological or psychiatric disorders and as secondary intervention to anxiety symptoms (Table 2).6,21,39–61
Papers that cited symptoms of anxiety as comorbidity were grouped in Neurological Disorders (Table 3)40,45,47,51,54,55,59 and Psychiatric Disorders (Table 4).6,21,39,41–44,46,48–50,52,53,56–58,60,61 We found that MDD is the psychiatric disorder with the highest occurrence appearing in seven papers while pain is the highest Neurological Disorders occurrence appearing in three papers.
Table 3.
Symptoms of anxiety present in neurological disorders
Table 4.
Symptoms of anxiety present in psychiatric disorders
| Primary pathology | Number of studies |
|---|---|
| Borderline | 1 (Reyes-Lopez. J et al,201841) |
| MDD | 8 (Kaur et al, 201939 Durmaz et al, 201742 Tovar-Perdomo et al, 201744 Diefenbach et al, 201349 Pretalli et al, 201250 Berlim et al, 201152 Loo et al, 200358 George et al, 200060) |
| Tinnitus | 3 (Noh et al, 201743 Bilici et al, 201546 Rossi et al, 200756) |
| Obsessive Compulsive Disorder | 1 (Elbeh et al, 20166) |
| Post Traumatic Stress Disorder | 4 (Oznur et al, 201448 Watts et al, 201221 Boggio et al, 201053 Cohen et al, 200457) |
| Schizophrenia | 1 (Rollnik et al, 200061) |
Abbreviation: MDD, major depressive disorder.
Fourteen papers reported the stimulation in the left DLPFC, three papers both left and right DLPFC and in one study the left auditory cortex was stimulated. Two papers focused the stimulation in the left temporoparietal region and left primary motor cortex. The stimulation target of right DLPFC appeared in three papers, in addition to those already mentioned. These regions were stimulated in one paper each: primary motor cortex contralateral to the amputated leg, motor cortex area of the frontal lobe, and the epileptogenic focus. Two studies described stimulation in the left temporoparietal region and left primary motor cortex.
High pulse frequency (>5 Hz) used in rTMS protocols can have an excitatory effect while a low frequency (1 Hz) has an inhibitory effect. These effects are not limited to the target of stimulation, favoring the improvement of mood symptoms since there is complex connectivity of the cerebral cortex with other deep brain regions, favoring, ultimately, the improvement of mood symptoms. Most studies analyzed in this review used 10 stimulation sessions and half used excitatory stimulation for all subjects with rTMS frequency range between 5 Hz and 20 Hz. In the treatment of anxious symptoms, studies reported using between 4 and 31 sessions with 200–5000 pulses per stimulation and an intensity of 20–130% of the RMT.
Measures of anxiety symptoms
One of the criteria used to include the paper in our systematic review was to contain measures to assess the symptoms of anxiety pre and post rTMS sessions. The Hamilton Rating Scale for Anxiety (HRSA) was the main scale found in this review; overall, this scale appeared in 14 papers; secondly the Beck Anxiety Inventory (BAI) and the State-Trait Anxiety Inventory (STAI), both appearing in four papers. In Table 5, we observe the other scales of assessment of the symptoms of anxiety found and their frequency in the papers.
Table 5.
Anxiety scales found in papers
| Anxiety questionnaire papers | Number of citations |
|---|---|
| HRSA | 15 |
| BAI | 4 |
| STAI | 4 |
| Hospital Anxiety Scale | 2 |
| PDSS | 2 |
| Anxiety/somatization subscale of the HDRS | 2 |
| HAMA | 2 |
| 7-item scale | 1 |
| BAS | 1 |
| DASS | 1 |
| GAD-7 | 1 |
| HAMD anxiety subscale (items 9, 10, 11 and 15) | 1 |
| SCL-90 | 1 |
| Tyrer scale for anxiety | 1 |
| Zung Self-Rating Anxiety Scale | 1 |
Abbreviations: HRSA, Hamilton Rating Scale for Anxiety; BAI, Beck Anxiety Inventory; STAI, State-Trait Anxiety Inventory; PDSS, Panic Disorder Severity Scale; HAMA, Hamilton Rating Scale for Anxiety; DASS, Depression Anxiety Stress Scales; GAD, Generalized Anxiety Disorder.
Clinical findings
We observed, in general, that most of the studies found satisfactory results with the use of rTMS in Anxiety Disorders and Anxiety as comorbidity.
In the studies on Anxiety Disorders, it was observed that three papers reported a sustained effect of response on the improvement of anxious symptoms, one paper reported improvement of symptoms, although this response did not sustain in the long term and one paper reported that there was no significant improvement.
The papers on Anxious Symptoms showed that most of the studies obtained the sustained effect of response on the anxiety symptoms observed in 21 studies. Two studies showed improvement but not sustained over time and one of them did not find a positive response to the improvement in anxiety symptoms.
Tolerability and safety
Adverse effects were minimal, showing that there is safety in the application of rTMS in anxious symptoms independent of the primary outcome.
In the papers on Anxiety Disorders, only one study reported that one participant in the active group had seizures and three participants reported transient dizziness; in the other papers, no adverse effects were reported.
In the papers on Anxious Symptoms, mild side effects were observed. The most frequent effect was a headache that appeared in 12 studies. In two studies, some patients were withdrawn because of side effects or treatment intolerance. Table 6 has the description and frequency of other side effects found in the papers on Anxious Symptoms.
Table 6.
Side effects of rTMS found in papers
| Side effects | Frequency in papers |
|---|---|
| Dizziness | 4 |
| Pain and stiffness in the neck and shoulder | 2 |
| Ringing in the ear | 3 |
| Drowsiness | 2 |
| Tearing | 1 |
| Regression in cognitive improvement during treatment | 1 |
| Neck pain | 1 |
| Fasciculation and mandibular pain | 1 |
| Gastrointestinal disorders | 1 |
| Sexual dysfunction | 1 |
| Muscle contraction | 1 |
| Rage attack | 1 |
| Ear discomfort | 1 |
| Excessive fatigue | 1 |
Discussion
The rTMS is already established as a non-invasive valid alternative to measure plastic alterations of the cerebral cortex for the treatment of depression,2 borderlines,41 OCD,6 among other pathologies. We observed in this review that anxiety is one of the main symptoms related to current mood disorders, with a direct impact on individuals’ quality of life.7
TMS have a direct correlation between the parameters associated with cortical excitability and plasticity, suggesting the existence of mechanisms that partially overlap and probably act in the same neurophysiological framework.62
Pennisi et al suggest that lesion in the ischemic subcortical and prefrontal region might have implications in cognition and mood and may result in functional changes of the intracortical system, in addition to associating an increase in global cortical excitability, together with a significant worsening of frontal lobe abilities, but without substantial functional impairment.62
Cortical plasticity plays a clear and fundamental role in patients with depression, while this still seems to be firmly established in anxiety disorders.63
Studies observed that impaired brain plasticity may be one of the pathophysiological mechanisms underlying cognitive decline and major depression.63 Some degree of cognitive impairment is often observed across the clinical spectrum of mood disorders, and between depression and cognition often bidirectional.63 Depressed patients have significant differences between the brain hemispheres, the intracortical neurochemical circuit (inhibitory or excitatory) might be unbalanced, the excitability of the motor cortex and TMS may indicate a disruption of plasticity.63 The data suggest that the motor cortex is more refractory to modulatory inputs from other non-motor areas within the CNS in depressed individuals.63 In addition, several studies have shown that functional abnormalities in cortical connections may play crucial roles in patients with depression and other mood disorders.63
Studies with depressive disorder usually predict anxiety symptoms as a secondary outcome. It is possible to observe how this mechanism occurs in cases of anxiety disorders, since it is directly related to the functioning of neurotransmitters and to the cerebral circuits. TMS may interfere directly in this functioning and may influence the regulation of anxiety as a symptom arising from another psychopathology or as an anxiety disorder.63
Other studies14,30,32 have found that TMS have promising results as a treatment for anxiety disorders; we observed comparable results, showing TMS intervention having positive effects on anxiety symptoms. However, there is still no standard intervention protocol for the use of TMS, neither for anxiety or depression disorders, as a comorbidity of psychiatric and neurological disorders.14,30,32
A few studies describe protocols for TMS application on anxiety disorders, Dilkov et al33 evidenced the effects of rTMS on participants with GAD. Most participants who received treatment from 25 rTMS sessions had a clinically significant decrease in anxiety symptoms as identified by the efficacy symptom scale.33
Another study also observed positive results in subjects with GAD after 30 rTMS sessions according to pre- and post-treatment comparative assessment scales.35 However, the Sham coil group also had reduced anxiety symptoms; they had a limited sample size and further assessment is necessary.35
The authors used 2 sessions of rTMS in the prefrontal ventromedial cortex region for the treatment of Acrophobia and fear of irrational stature.64 Their study used virtual reality technology to assist in the therapy and they observed a better response for fear and symptoms.64
There is no clear pattern for using high or low frequencies of TMS stimulation in which regions of the brain. One review study cited the use of both high- and low-frequency TMS stimulation under the right and left stimulation target DLPFC.30 Iannone et al14 cited papers that used both high and low frequencies of TMS on anxiety disorders. Another review study found that the right and left DLPFC were targets for TMS stimulation in most papers.31 However, when searching for anxiety as a secondary outcome, the stimulation region was dependable on the primary outcome of the TMS intervention. TMS stimulation for pathologies involving motor aspects poses another difficulty.65 In these cases, the stimulation target was primarily in specific regions of the motor cortex.65
Patients with Restless Legs Syndrome (RLS) who receive TMS intervention had improvements on anxiety symptoms with the improvement of the RLS symptoms.47 A similar study found that using TMS to stimulate the motor cortex area alleviated motor sensory complaints of RLS patients. TMS excitation and inhibition rates indicate intracortical injury and corticospinal imbalance, involving GABAergic and glutamatergic circuits, as well as impairment of the short-term mechanisms of plasticity.65 The activation induced by rTMS with the consequent increase in dopamine release may have contributed to the clinical and neurophysiological outcome in those patients.65 The occurrence of anxiety in patients with RLS is related to an abnormal sensorimotor integration, suggesting an interrupted connectivity in the RLS.66 Using TMS in the sensory cortex motor region may promote improvements of physical symptoms and therefore reduction in anxiety.66
TMS has also been shown to be effective as a sustained response effect compared to drug intervention. It is observed that drug-resistant patients on MDD treatment achieved improvement of symptoms with the use of TMS after a period of six months post-intervention, while this period is reduced when only medication is used.67
Although there is no consensus in the TMS intervention parameters for anxiety disorders and symptoms due to neurological or psychiatric disorders, we observed that the DLPFC region is preferred among researcher’s stimulation target. TMS have promising results in high frequency, promoting excitatory stimulation, and low frequency, promoting inhibitory stimulation. The number of sessions should range from 10 to 20 sessions so that the sustained response effect is possible. The stimulation of the motor cortex, especially in the sensorimotor region, also shows promising results in the stimulation of anxiety symptoms due to neurological disorders, mainly focusing on motor aspects.
Conclusion
We observed in this review that TMS might be a satisfactory intervention measure to improve anxiety, although there are a limited number of reports on the use of this intervention. In addition, satisfactory results have also noted that TMS is a safe treatment strategy with low side effect. Further studies using TMS could direct the treatment with psychological or psychiatric intervention.
Disclosure
Miss Cintya Yukie Hayashi reports grant from Coordination for the Improvement of Higher Education Personnel (CAPES) – Brazil, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Cabrera CC, Sponholz Júnior A. Ansiedade e insônia In: Prática Psiquiátrica No Hospital Geral: Interconsulta E Emergência. Porto Alegre, Brazil: Artmed Editora;2005:283–304. [Google Scholar]
- 2.Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58(1):55–61. doi: 10.1001/archpsyc.58.1.55 [DOI] [PubMed] [Google Scholar]
- 3.Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. J Consult Clin Psychol. 2002;70(2):288. doi: 10.1037/0022-006X.70.2.288 [DOI] [PubMed] [Google Scholar]
- 4.Balconi M, Ferrari C. Left DLPFC rTMS stimulation reduced the anxiety bias effect or how to restore the positive memory processing in high-anxiety subjects. Psychiatry Res. 2013;209:554–559. doi: 10.1016/j.psychres.2013.03.032 [DOI] [PubMed] [Google Scholar]
- 5.White D, Tavakoli S. Repetitive transcranial magnetic stimulation for treatment of major depressive disorder with comorbid generalized anxiety disorder. Ann Clin Psychiatry. 2015;27(3):192–196. [PubMed] [Google Scholar]
- 6.Elbeh KAM, Elserogy YMB, Khalifa HE, Ahmed MA, Hafez MH, Khedr EM. Repetitive transcranial magnetic stimulation in the treatment of obsessive-compulsive disorders: double blind randomized clinical trial. Psychiatry Res. 2016;238:264–269. doi: 10.1016/j.psychres.2016.02.031 [DOI] [PubMed] [Google Scholar]
- 7.Gould KR, Ponsford JL, Spitz G. Association between cognitive impairments and anxiety disorders following traumatic brain injury. J Clin Exp Neuropsychol. 2014;36(1):1–14. doi: 10.1080/13803395.2013.863832 [DOI] [PubMed] [Google Scholar]
- 8.Bashir S, Mizrahi I, Weaver K, Fregni F, Pascual-Leone A. Assessment and modulation of neural plasticity in rehabilitation with transcranial magnetic stimulation. PM&R. 2010;2(12):S253–S268. doi: 10.1016/j.pmrj.2010.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kobayashi M, Pascual-Leone A. Transcranial magnetic stimulation in neurology. Lancet Neurol. 2003;2(3):145–156. [DOI] [PubMed] [Google Scholar]
- 10.Barker AT. An introduction to the basic principles of magnetic nerve stimulation. J Clin Neurophysiol. 1991;8(1):26–37. [DOI] [PubMed] [Google Scholar]
- 11.Hallett M. Transcranial magnetic stimulation and the human brain. Nature. 2000;406(6792):147–150. doi: 10.1038/35018000 [DOI] [PubMed] [Google Scholar]
- 12.Kim YI, Kim SM, Kim H, Han DH. The effect of high-frequency repetitive transcranial magnetic stimulation on occupational stress among health care workers: a pilot study. Psychiatry Investig. 2016;13(6):622–629. doi: 10.4306/pi.2016.13.6.622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sagliano L, D’Olimpio F, Panico F, Gagliardi S, Trojano L. The role of the dorsolateral prefrontal cortex in early threat processing: a TMS study. Soc Cogn Affect Neurosci. 2016;11(12):1992–1998. doi: 10.1093/scan/nsw105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iannone A, Cruz APM, Brasil-Neto JP, Boechat-Barros R. Transcranial magnetic stimulation and transcranial direct current stimulation appear to be safe neuromodulatory techniques useful in the treatment of anxiety disorders and other neuropsychiatric disorders. Arq Neuropsiquiatr. 2016;74(10):829–835. doi: 10.1590/0004-282X20160115 [DOI] [PubMed] [Google Scholar]
- 15.Luber BM, Davis S, Bernhardt E, et al. Using neuroimaging to individualize TMS treatment for depression: toward a new paradigm for imaging-guided intervention. NeuroImage. 2017;148:1–7. doi: 10.1016/j.neuroimage.2016.12.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vidor LP, Torres ILS, Medeiros LF, et al. Association of anxiety with intracortical inhibition and descending pain modulation in chronic myofascial pain syndrome. BMC Neurosci. 2014;15:42. doi: 10.1186/1471-2202-15-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mak ADP, Chan SSM, Lam LCW, et al. Preliminary results from a randomized sham-controlled trial of augmentative neuro-navigated right-dorsolateral prefrontal cortex low-frequency repetitive transcranial magnetic stimulation for antidepressant non-responding bipolar depression. Brain Stimul. 2017;10(2):378. doi: 10.1016/j.brs.2017.01.121 [DOI] [Google Scholar]
- 18.Bashir S, Vernet M, Yoo WK, Mizrahi I, Theoret H, Pascual-Leone A. Changes in cortical plasticity after mild traumatic brain injury. Restor Neurol Neurosci. 2012;30(4):277–282. doi: 10.3233/RNN-2012-110207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li SS, Zaninotto AL, Neville IS, Paiva WS, Nunn D, Fregni F. Clinical utility of brain stimulation modalities following traumatic brain injury: current evidence. Neuropsychiatr Dis Treat. 2015;11:1573–1586. doi: 10.2147/NDT.S65816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weir K, Gray S. Can magnets cure depression. Transcranial magnetic stimulation is gaining ground as a therapy for treatment-resistant depression. APA. 2015;46(2):50. [Google Scholar]
- 21.Watts BV, Landon B, Groft A, Young-Xu Y. A sham controlled study of repetitive transcranial magnetic stimulation for posttraumatic stress disorder. Brain Stimul. 2012;5(1):38–43. doi: 10.1016/j.brs.2011.02.002 [DOI] [PubMed] [Google Scholar]
- 22.Ma X, Huang Y, Liao L, Jin Y. A randomized double-blinded sham-controlled trial of a electroencephalogram-guided transcranial magnetic stimulation for obsessive-compulsive disorder. Chin Med J. 2014;127(4):601–606. [PubMed] [Google Scholar]
- 23.Hegde S. Music-based cognitive remediation therapy for patients with traumatic brain injury. Front Neurol. 2014;5. doi: 10.3389/fneur.2014.00034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nielson DM, McKnight CA, Patel RN, Kalnin AJ, Mysiw WJ. Preliminary guidelines for safe and effective use of repetitive transcranial magnetic stimulation in moderate to severe traumatic brain injury. Arch Phys Med Rehabil. 2015;96(4):S138–S144. doi: 10.1016/j.apmr.2014.09.010 [DOI] [PubMed] [Google Scholar]
- 25.Araújo HA, Iglesio RF, de Camargo Correia GS, et al. Estimulação magnética transcraniana e aplicabilidade clínica: perspectivas na conduta terapêutica neuropsiquiátrica. Rev Med. 2011;90(1):3–14. doi: 10.11606/issn.1679-9836.v90i1p3-14 [DOI] [Google Scholar]
- 26.Barker A, Freeston I, Jalinous R, Jarratt J. Magnetic stimulation of the human brain and peripheral nervous system: an introduction and the results of an initial clinical evaluation. Neurosurgery. 1987;20(1):100–109. doi: 10.1097/00006123-198701000-00024 [DOI] [PubMed] [Google Scholar]
- 27.Lefaucheur JP. Stroke recovery can be enhanced by using repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2006;36(3):105–115. doi: 10.1016/j.neucli.2006.08.011 [DOI] [PubMed] [Google Scholar]
- 28.Miniussi C, Rossini PM. Transcranial magnetic stimulation in cognitive rehabilitation. Neuropsychol Rehabil. 2011;21(5):579–601. doi: 10.1080/09602011.2011.562689 [DOI] [PubMed] [Google Scholar]
- 29.Ricci R, Ramsey D, Johnson K, et al. A pilot feasibility study of daily rTMS to modify corticospinal excitability during lower limb immobilization. Ther Clin Risk Manag. 2008;4(5):1127–1134. doi: 10.2147/tcrm.s2719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vicario CM, Salehinejad MA, Felmingham K, Martino G, Nitsche MA. A systematic review on the therapeutic effectiveness of non-invasive brain stimulation for the treatment of anxiety disorders. Neurosci Biobehav Rev. 2018;96:219–231. [DOI] [PubMed] [Google Scholar]
- 31.Paes F, Machado S, Arias-Carrion O, et al. The value of repetitive transcranial magnetic stimulation (rTMS) for the treatment of anxiety disorders: an integrative review. CNS Neurol Disord Drug Targets. 2011;10(5):610–620. [DOI] [PubMed] [Google Scholar]
- 32.Lefaucheur JP, André-Obadia N, Antal A, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125(11):2150–2206. doi: 10.1016/j.clinph.2014.05.021 [DOI] [PubMed] [Google Scholar]
- 33.Dilkov D, Hawken ER, Kaludiev E, Milev R. Repetitive transcranial magnetic stimulation of the right dorsal lateral prefrontal cortex in the treatment of generalized anxiety disorder: a randomized, double-blind sham controlled clinical trial. Prog Neuro-Psychopharmacol Biol Psychiatry. 2017;78:61–65. doi: 10.1016/j.pnpbp.2017.05.018 [DOI] [PubMed] [Google Scholar]
- 34.Mantovani A, Aly M, Dagan Y, Allart A, Lisanby SH. Randomized sham controlled trial of repetitive transcranial magnetic stimulation to the dorsolateral prefrontal cortex for the treatment of panic disorder with comorbid major depression. J Affect Disord. 2013;144(1–2):153–159. doi: 10.1016/j.jad.2012.05.038 [DOI] [PubMed] [Google Scholar]
- 35.Diefenbach GJ, Bragdon LB, Zertuche L, et al. Repetitive transcranial magnetic stimulation for generalised anxiety disorder: a pilot randomised, double-blind, sham-controlled trial. Br J Psychiatry. 2016;209(3):222–228. doi: 10.1192/bjp.bp.115.168203 [DOI] [PubMed] [Google Scholar]
- 36.Prasko J, Zalesky R, Bares M, et al. The effect of repetitive transcranial magnetic stimulation (rTMS) add on serotonin reuptake inhibitors in patients with panic disorder: a randomized, double blind sham controlled study. Neuroendocrinol Lett. 2007;28(1):33–38. [PubMed] [Google Scholar]
- 37.Zhang T, Zhu J, Xu L, et al. Add-on rTMS for the acute treatment of depressive symptoms is probably more effective in adolescents than in adults: evidence from real-world clinical practice. Brain Stimul. 2019;12(1):103–109. doi: 10.1016/j.brs.2018.09.007 [DOI] [PubMed] [Google Scholar]
- 38.Lu R, Zhang C, Liu Y, Wang L, Chen X, Zhou X. The effect of bilateral low-frequency rTMS over dorsolateral prefrontal cortex on serum brain-derived neurotropic factor and serotonin in patients with generalized anxiety disorder. Neurosci Lett. 2018;684:67–71. doi: 10.1016/j.neulet.2018.07.008 [DOI] [PubMed] [Google Scholar]
- 39.Kaur M, Naismith SL, Lagopoulos J, et al. Sleep-wake, cognitive and clinical correlates of treatment outcome with repetitive transcranial magnetic stimulation for young adults with depression. Psychiatry Res. 2019;271:335–342. doi: 10.1016/j.psychres.2018.12.002 [DOI] [PubMed] [Google Scholar]
- 40.Lin H, Li W, Ni J, Wang Y. Clinical study of repetitive transcranial magnetic stimulation of the motor cortex for thalamic pain. Medicine. 2018;97(27):e11235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reyes-López J, Ricardo-Garcell J, Armas-Castañeda G, et al. Clinical improvement in patients with borderline personality disorder after treatment with repetitive transcranial magnetic stimulation: preliminary results. Rev Bras Psiquiatr. 2018;40(1):97–104. doi: 10.1590/1516-4446-2016-2112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Durmaz O, Ebrinc S, Ates MA, Algul A. Evaluation of repetitive transcranial magnetic stimulation for treatment resistant major depression and the impact of anxiety symptoms on outcome. Psychiatry Clin Psychopharmacol. 2017;27(1):14–18. doi: 10.1080/24750573.2017.1293239 [DOI] [Google Scholar]
- 43.Noh TS, Kyong JS, Chang MY, et al. Comparison of treatment outcomes following either prefrontal cortical-only or dual-site repetitive transcranial magnetic stimulation in chronic tinnitus patients: a double-blind randomized study. Otol Neurotol. 2017;38(2):296–303. doi: 10.1097/MAO.0000000000001266 [DOI] [PubMed] [Google Scholar]
- 44.Tovar-Perdomo S, McGirr A, Van Den Eynde F, Dos Santos NR, Berlim MT. High frequency repetitive transcranial magnetic stimulation treatment for major depression: dissociated effects on psychopathology and neurocognition. J Affect Disord. 2017;217:112–117. doi: 10.1016/j.jad.2017.03.075 [DOI] [PubMed] [Google Scholar]
- 45.Malavera A, Silva FA, Fregni F, Carrillo S, Garcia RG. Repetitive transcranial magnetic stimulation for phantom limb pain in land mine victims: a double-blinded, randomized, sham-controlled trial. J Pain. 2016;17(8):911–918. doi: 10.1016/j.jpain.2016.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bilici S, Yigit O, Taskin U, Gor AP, Yilmaz ED. Medium-term results of combined treatment with transcranial magnetic stimulation and antidepressant drug for chronic tinnitus. Eur Archiv Oto-Rhino-Laryngol. 2015;272(2):337–343. doi: 10.1007/s00405-013-2851-z [DOI] [PubMed] [Google Scholar]
- 47.Lin YC, Feng Y, Zhan SQ, et al. Repetitive transcranial magnetic stimulation for the treatment of restless legs syndrome. Chin Med J. 2015;128(13):1728. doi: 10.4103/0366-6999.159344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oznur T, Akarsu S, Celik C, et al. Is transcranial magnetic stimulation effective in treatment-resistant combat related posttraumatic stress disorder? Neurosciences (Riyadh). 2014;19(1):29–32. [PubMed] [Google Scholar]
- 49.Diefenbach GJ, Bragdon L, Goethe JW. Treating anxious depression using repetitive transcranial magnetic stimulation. J Affect Disord. 2013;151(1):365–368. doi: 10.1016/j.jad.2013.05.094 [DOI] [PubMed] [Google Scholar]
- 50.Pretalli JB, Nicolier M, Chopard G, et al. Resting motor threshold changes and clinical response to prefrontal repetitive transcranial magnetic stimulation in depressed patients. Psychiatry Clin Neurosci. 2012;66(4):344–352. doi: 10.1111/j.1440-1819.2012.02341.x [DOI] [PubMed] [Google Scholar]
- 51.Sun W, Mao W, Meng X, et al. Low‐frequency repetitive transcranial magnetic stimulation for the treatment of refractory partial epilepsy: a controlled clinical study. Epilepsia. 2012;53(10):1782–1789. doi: 10.1111/j.1528-1167.2012.03626.x [DOI] [PubMed] [Google Scholar]
- 52.Berlim MT, McGirr A, Beaulieu MM, Turecki G. High frequency repetitive transcranial magnetic stimulation as an augmenting strategy in severe treatment-resistant major depression: a prospective 4-week naturalistic trial. J Affect Disord. 2011;130(1–2):312–317. doi: 10.1016/j.jad.2010.10.011 [DOI] [PubMed] [Google Scholar]
- 53.Boggio PS, Rocha M, Oliveira MO, et al. Noninvasive brain stimulation with high-frequency and low-intensity repetitive transcranial magnetic stimulation treatment for posttraumatic stress disorder. J Clin Psychiatry. 2010;71(8):992. doi: 10.4088/JCP.08m04638blu [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Epstein CM, Evatt ML, Funk A, et al. An open study of repetitive transcranial magnetic stimulation in treatment-resistant depression with Parkinson’s disease. Clin Neurophysiol. 2007;118(10):2189–2194. doi: 10.1016/j.clinph.2007.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Passard A, Attal N, Benadhira R, et al. Effects of unilateral repetitive transcranial magnetic stimulation of the motor cortex on chronic widespread pain in fibromyalgia. Brain. 2007;130(10):2661–2670. doi: 10.1093/brain/awm189 [DOI] [PubMed] [Google Scholar]
- 56.Rossi S, De Capua A, Ulivelli M, et al. Effects of repetitive transcranial magnetic stimulation on chronic tinnitus. A randomised, cross over, double blind, placebo-controlled study. Journal of Neurology, Neurosurgery & Psychiatry. 2007. doi: 10.1136/jnnp.2006.105007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cohen H, Kaplan Z, Kotler M, Kouperman I, Moisa R, Grisaru N. Repetitive transcranial magnetic stimulation of the right dorsolateral prefrontal cortex in posttraumatic stress disorder: a double-blind, placebo-controlled study. Am J Psychiatry. 2004;161(3):515–524. doi: 10.1176/appi.ajp.161.3.515 [DOI] [PubMed] [Google Scholar]
- 58.Loo CK, Sachdev PS, Haindl W, et al. High (15 Hz) and low (1 Hz) frequency transcranial magnetic stimulation have different acute effects on regional cerebral blood flow in depressed patients. Psychol Med. 2003;33(6):997–1006. [DOI] [PubMed] [Google Scholar]
- 59.Münchau A, Bloem BR, Thilo KV, Trimble MR, Rothwell JC, Robertson MM. Repetitive transcranial magnetic stimulation for Tourette syndrome. Neurology. 2002;59(11):1789–1791. doi: 10.1212/01.wnl.0000036615.25044.50 [DOI] [PubMed] [Google Scholar]
- 60.George MS, Nahas Z, Molloy M, et al. A controlled trial of daily left prefrontal cortex TMS for treating depression. Biol Psychiatry. 2000;48(10):962–970. doi: 10.1016/s0006-3223(00)01048-9 [DOI] [PubMed] [Google Scholar]
- 61.Rollnik JD, Huber TJ, Mogk H, et al. High frequency repetitive transcranial magnetic stimulation (rTMS) of the dorsolateral prefrontal cortex in schizophrenic patients. Neuroreport. 2000;11(18):4013–4015. doi: 10.1097/00001756-200012180-00022 [DOI] [PubMed] [Google Scholar]
- 62.Pennisi G, Bella R, Lanza G. Motor cortex plasticity in subcortical ischemic vascular dementia: what can TMS say? Clin Neurophysiol. 2015;126(5):851–852. doi: 10.1016/j.clinph.2014.09.001 [DOI] [PubMed] [Google Scholar]
- 63.Cantone M, Bramanti A, Lanza G, et al. Cortical plasticity in depression: a neurochemical perspective from transcranial magnetic stimulation. ASN Neuro. 2017;9(3):1759091417711512. doi: 10.1177/1759091417711512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Herrman MJ, Katzorke A, Busch Y, et al. Medial prefrontal cortex stimulation accelerates therapy response of exposure therapy in acrophobia. Brain Stimul. 2017;10(2):291. doi: 10.1016/j.brs.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 65.Lanza G, Cantone M, Aricò D, et al. Clinical and electrophysiological impact of repetitive low-frequency transcranial magnetic stimulation on the sensory–motor network in patients with restless legs syndrome. Ther Adv Neurol Disord. 2018;11:1756286418759973. doi: 10.1177/1756286418759973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lanza G, Bachmann CG, Ghorayeb I, Wang Y, Ferri R, Paulus W. Central and peripheral nervous system excitability in restless legs syndrome. Sleep Med. 2017;31:49–60. doi: 10.1016/j.sleep.2016.05.010 [DOI] [PubMed] [Google Scholar]
- 67.Concerto C, Lanza G, Cantone M, et al. Repetitive transcranial magnetic stimulation in patients with drug-resistant major depression: a six-month clinical follow-up study. Int J Psychiatry Clin Pract. 2015;19(4):252–258. doi: 10.3109/13651501.2015.1084329 [DOI] [PubMed] [Google Scholar]