Abstract
Viral bronchiolitis is a common clinical syndrome affecting infants and young children. Concern about its associated morbidity and cost has led to a large body of research that has been summarised in systematic reviews and integrated into clinical practice guidelines in several countries. The evidence and guideline recommendations consistently support a clinical diagnosis with the limited role for diagnostic testing for children presenting with the typical clinical syndrome of viral upper respiratory infection progressing to the lower respiratory tract. Management is largely supportive, focusing on maintaining oxygenation and hydration of the patient. Evidence suggests no benefit from bronchodilator or corticosteroid use in infants with a first episode of bronchiolitis. Evidence for other treatments such as hypertonic saline is evolving but not clearly defined yet. For infants with severe disease, the insufficient available data suggest a role for high-flow nasal cannula and continuous positive airway pressure use in a monitored setting to prevent respiratory failure.
Introduction
Acute bronchiolitis, a viral infection of the lower respiratory tract, is one of the most substantial health burdens for infants and young children worldwide.1 Respiratory syncytial virus is the most prevalent viral cause of bronchiolitis in infants. Estimates suggest that about 34 million new cases of lower respiratory infection due to respiratory syncytial virus occur globally in children younger than 5 years, with 3·4 million admissions to hospitals and about 199 000 deaths per year, predominantly in the developing world.2 In developed countries such as the USA, bronchiolitis is the most common reason for admission to hospital in the first 12 months of life,3 accounting for approximately 100 000 infant admissions annually. Although admissions to hospital have declined from 2000 to 2010, emergency department visits have increased, in addition to increased use of mechanical ventilation and hospital charges.4, 5
The clinical management remains challenging despite the frequency, global reach, economic cost, and morbidity and mortality associated with bronchiolitis. Several treatment strategies (including bronchodilators and corticosteroids) showed no effect in pooled meta-analyses, making supportive care the hallmark of current therapy. In this Seminar, we aim to summarise the current evidence for the epidemiology, pathophysiology, diagnostic approach, and management of acute viral bronchiolitis.
Epidemiology
Bronchiolitis is a seasonal infection, with the season typically beginning in late October in the temperate northern hemisphere, peaking in January or February, and ending in April.6 Globally, independent of region, respiratory syncytial virus infection peaks consistently during annual or biannual epidemics. Although the peak and duration of these epidemics vary worldwide, they are consistent year-to-year within a country.7 Some data suggest that climate might also be associated with prevalence of respiratory syncytial virus infection, with global surveillance suggesting that infection peaks during wet months in areas with high precipitation and during cooler months in hot regions.7 Indoor crowding in population-dense areas during rainy seasons or cooler months might be one factor that facilitates viral transmission.8 Additionally, weather-related factors, such as inhalation of cold and dry air that might impair ciliary function, the airway mucosa, and inhibition of temperature-dependent antiviral responses, might influence both disease transmission and severity.9, 10
Altitude, climate, and meteorological conditions (such as wind speed and dew point) have been shown to have a modest association with bronchiolitis.11, 12 Furthermore, air pollutants, such as ozone and traffic pollutants, have been associated with exacerbations of respiratory infections in children younger than 5 years.13, 14, 15 Environmental tobacco smoke has been associated with increased risk for respiratory syncytial virus-attributable admission to hospital and disease severity in those admitted.16, 17
As with other respiratory viral infections, the risk of severe respiratory syncytial virus bronchiolitis might be greater in boys than in girls.18, 19 This difference might be due to differences in lung and airway development, and by genetic factors.8, 20
Pathophysiology
Bronchiolitis is characterised by extensive inflammation and oedema of the airways, increased mucus production, and necrosis of airway epithelial cells.21 Respiratory syncytial virus binds to epithelial cells and replicates, resulting in epithelial necrosis and ciliary destruction.21, 22 The cell destruction triggers an inflammatory response with proliferation of polymorphonuclear cells and lymphocytes. The submucosa and adventitial tissues become oedematous with increased mucus secretion.22 Plugs composed of cellular debris and mucus form in the bronchiole lumens leading to bronchiolar obstruction, air trapping, and different degrees of lobar collapse.21
Microbiology
Molecular testing has led to an improved understanding of the viruses associated with bronchiolitis. Respiratory syncytial virus remains the most commonly identified virus, detected in 41–83% of patients.23, 24, 25, 26, 27, 28 Other viruses associated with bronchiolitis include rhinovirus, metapneumovirus, coronavirus, human bocavirus, influenza virus, adenovirus, and parainfluenza virus.24, 25, 27, 29, 30
Studies have investigated whether severity of illness, as measured by need for hospital admission, length of hospital stay, intensive care unit admission, repeated emergency department visits, and apnoea, is associated with specific viral infections or co-infections, but the evidence is conflicting. Data from some studies have shown that in infections involving a single virus, respiratory syncytial virus is associated with a more severe course compared with other viruses.31, 32 Up to 30% of children with bronchiolitis are found to have co-infections with two other viruses,29 with the combination of respiratory syncytial virus and rhinovirus being the most commonly reported.29 Some evidence suggests that co-infection in bronchiolitis, particularly respiratory syncytial virus in combination with rhinovirus or metapneumovirus, could be associated with a more severe disease course compared with infection by a single virus.25, 30, 31, 33, 34 However, other studies do not confirm this association.24, 26
Furthermore, although use of nucleic acid amplification tests has greatly improved our ability to detect viruses present in respiratory infections, studies using these technologies have also found at least one respiratory virus in up to 30% of children younger than 6 years with no respiratory symptoms.35, 36, 37 These viruses might be detected because of asymptomatic colonisation, incubation before clinical infection, or prolonged viral shedding post-infection. The conflicting evidence and high prevalence of respiratory viruses in asymptomatic children suggest no indication at this time that management should vary based on presumed viral cause and presence, or absence of viral co-infections.
Clinical presentation and differential diagnosis
The diagnosis of bronchiolitis is clinical and thus requires a clinician to recognise signs and symptoms of viral lower respiratory tract infection in young children. Peak incidence occurs between 3 months and 6 months of age.38 Since the early clinical definition by Court, and as noted in recent practice guidelines, the most specific definition is in infants.38, 39, 40 Although the same physiology can occur in toddlers older than 12 months, many clinical trials have excluded these children or have included them as a small subgroup of patients. Bronchiolitis in toddlers can overlap with other conditions such as viral-induced wheezing and asthma, and application of evidence from trials predominantly assessing infants might not be appropriate. Further efforts to focus the definition might assist efforts to standardise care.
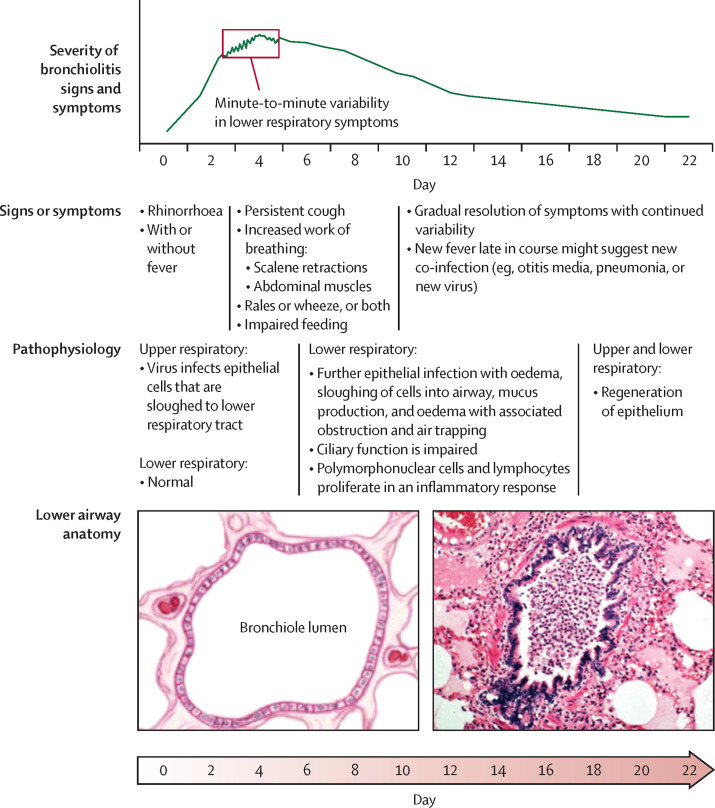
The classic clinical presentation of bronchiolitis starts with symptoms of a viral upper respiratory infection, such as nasal discharge, that progress to the lower respiratory tract over several days (figure 1 ). Timing of symptom progression can vary, and young infants can present with apnoea. Lower respiratory tract symptoms of bronchiolitis include persistent cough, tachypnoea, and increased work of breathing, as shown by intercostal or supraclavicular retractions, use of abdominal muscles, grunting, or nasal flaring. Auscultatory findings include crackles and wheeze. A hallmark characteristic of bronchiolitis is the minute-to-minute variation in clinical findings, as mucus and debris in the airways are cleared by coughing or as the child's state changes from sleep to agitation. This variation can confound assessment, and often requires several examinations over a period of observation. Nasal congestion can also confound the clinical assessment. Nasal suctioning might help to ascertain which findings are truly from the lower airways. Fever can be present in about a third of infants with bronchiolitis, but it is usually present early in the illness with a temperature less than 39°C.38 The median duration of symptoms is about 2 weeks, with 10–20% of infants still having symptoms at 3 weeks after onset.38, 41 Various clinical scores have been shown in studies and clinical protocols to correlate with disease severity and improvement.42, 43 Although documentation of a score can be useful as an objective measure, individual scores are not highly predictive, and they should be repeated and combined with other measures of severity for a universal assessment to guide decision making.
Figure 1.
Typical clinical course and pathophysiology of viral bronchiolitis
The differential diagnosis for bronchiolitis includes considerations of various infectious and non-infectious causes. Absence of upper respiratory symptoms should raise suspicion of other causes of respiratory distress in young infants, including cardiac disease, congenital airway abnormalities such as a vascular ring, or foreign body aspiration. Other infections can resemble or complicate bronchiolitis. Pertussis should be considered in infants with severe or paroxysmal cough, or with known exposure. Bacterial infections complicating viral bronchiolitis, including otitis media or pneumonia, might present as a new fever or worsening status later in the course of illness.
Various risk factors have been associated with progression to severe bronchiolitis. Those supported by the strongest evidence include presence of chronic lung disease of prematurity and haemodynamically important congenital heart disease, with immunodeficiency and neuromuscular disorders also considered as high risk in practice guidelines.38, 39 Young infants (aged <2–3 months) and those with a history of premature birth (especially <32 weeks' gestation) are also at high risk for progression and can present with apnoea without other clinical findings. Studies assessing the risk for further apnoea in hospital have found it to be limited to infants less than 1 month for full-term infants, 48 weeks postconceptional age for preterm infants, or those with apnoea observed before admission.44
Diagnostic investigations
Pulse oximetry
Bronchiolitis is a clinical diagnosis based on history and physical examination, according to consensus across national guidelines. For infants with a typical presentation of bronchiolitis, routine imaging or laboratory testing is not recommended, as they increase costs without evidence for benefit (table ).
Table.
National clinical practice guidelines for bronchiolitis
| NICE (UK), 201538 | AAP (USA), 201439 | CPS (Canada), 201445 | SIGN (Scotland), 200646 | Italy, 201447 | Spain, 201048 | Australia, 200849 | France, 201350 | |
|---|---|---|---|---|---|---|---|---|
| Diagnostic testing | ||||||||
| Pulse oximetry | No mention about continuous use; intermittent checks should be performed in all children | Not recommended if supplemental oxygen is not required, or if oxyhaemoglobin saturation >90% | Not recommended unless high-risk patients in acute phase of disease; intermittent checks appropriate | Intermittent pulse oximetry should be performed on every child who presents to hospital | No mention | Intermittent pulse oximetry; no clear recommendation for continuous monitoring | No mention | No mention |
| Chest radiography | Not routinely recommended; consider when intensive care is proposed | Not routinely recommended; consider in severe disease requiring intensive care unit care or signs of airway complication (eg, pneumothorax) | Not routinely recommended; consider when diagnosis is unclear, rate of improvement not as expected, or disease severity indicates other diagnoses | Not routinely recommended; consider with diagnostic uncertainty or atypical disease course | Not routinely recommended | Not routinely recommended; consider if diagnostic uncertainty, atypical presentation, severe disease, or progressive disease course | Not routinely recommended; might be warranted if diagnostic uncertainty, severe respiratory distress, or high risk for severe illness | Not routinely recommended; consider if asymmetrical breath sounds are heard, diagnostic uncertainty, cardiac disease, chronic lung disease, and immunodeficiency |
| Viral testing | No mention | Not routinely recommended | Not routinely recommended | Rapid respiratory syncytial virus testing recommended for admitted infants to guide cohorting | Respiratory syncytial virus antigen recommended in hospital setting for cohorting and potentially decreasing antibiotic use | Not routinely recommended; respiratory syncytial virus testing might assist with cohorting | Not routinely recommended; consider if diagnostic uncertainty or young febrile infants | Not routinely recommended |
| Complete blood count | Not routinely recommended | Not recommended | Not recommended | Not recommended | Not routinely recommended | Not recommended | No mention | Obtain if undergoing septic work-up |
| Blood gas | Not routinely recommended; only if concern for severe worsening respiratory distress or impending respiratory failure | No mention | Not routinely recommended; only if concern for respiratory failure | Not routinely recommended; consider in severe distress or impending respiratory failure | Not routinely recommended | Not routinely recommended; might be useful for severe distress or impending respiratory failure | Not routinely recommended; obtain in severe disease or consider in moderate disease | No mention |
| Bacterial cultures | Not routinely recommended | No mention | Not routinely recommended | Not routinely recommended | Not routinely recommended | Not routinely recommended | Not routinely recommended | Not routinely recommended; recommended for infants <1 month as part of full septic work-up; not needed for infants 1–3 months unless presenting with signs of severe sepsis |
| Treatments | ||||||||
| β-agonist bronchodilators | Not recommended | Not recommended | Not recommended | Not recommended | Not routinely recommended; carefully monitored trial might be appropriate | Not routinely recommended; if used, must undergo carefully monitored trial | Not routinely recommended; carefully monitored trial might be considered in infants >9 months, especially with recurrent wheeze | Not recommended in first episode of wheezing; consider trial in child with recurrent wheeze depending on atopic history, case history, and clinical features |
| Epinephrine | Not recommended | Not recommended | Not routinely recommended; carefully monitored trial might be appropriate | Not recommended | Not recommended | Not recommended | Not routinely recommended | Not routinely recommended |
| Corticosteroids | Not recommended | Not recommended | Not recommended | Not recommended | Not recommended | Not recommended | Not routinely recommended | Not recommended |
| Hypertonic saline (nebulised) | Not recommended | Not recommended in emergency department; weak recommendation for inpatients in hospitals with average inpatient length of stay >72 h | Not recommended in emergency department or outpatient setting; might be beneficial in inpatients with long length of stay | No mention | Recommended | Recommended for inpatients | No mention | Recommended for inpatients who are moderate to severe |
| Suctioning | Do not routinely perform; consider upper airway suctioning in those with respiratory distress or feeding difficulties due to upper airway sections; use if apnoea present | Insufficient data; routine use of deep suctioning might not be beneficial | Superficial nasal suctioning at frequent intervals; avoid deep suctioning and long intervals between suctioning | Use nasal suction to clear secretions if respiratory distress due to nasal blockage | Superficial suctioning recommended; deep suctioning not recommended | Superficial nasal suctioning recommended before feeding, sleeping, and assessment | Might be trialled | Superficial nasal suctioning recommended if nasal congestion |
| Supplemental oxygen | Use if oxygen saturation is persistently <92% | Not recommended if oxyhaemoglobin saturation >90% without acidosis | Use if oxyhaemoglobin saturation <90% to maintain saturations ≥90% | Use of oxygen saturation ≤92% or severe respiratory distress | Use if oxygen saturation is persistently <90–92% | Use if severe respiratory distress or oxygen saturation <92% | Consider if infant <3 months, increased work of breathing, decreased oxygenation during feeds, oxygen saturation <90–92% | Use if oxygen saturation is <92%, or <95% and if signs of severe respiratory distress |
| Chest physiotherapy | Not routinely recommended unless relevant comorbidities present (eg, spinal muscular atrophy) | Not recommended | Not recommended | Not recommended in infants not admitted to intensive care | Not recommended | Not recommended | Not routinely recommended | Not recommended unless relevant comorbidities (eg, muscular dystrophy or cystic fibrosis), or profound difficulty ventilating |
| Antibiotic therapy | Not recommended | Not recommended unless strong suspicion or definite concomitant bacterial infection | Not recommended unless clear and documented evidence of secondary bacterial infection | Not recommended | Not recommended unless clear and documented evidence of secondary bacterial infection | Not recommended unless clear bacterial infection | Not routinely recommended; consider with signs of secondary bacterial infection | Not recommended; consider with signs of secondary bacterial infection or severe difficulty with ventilation |
| Antiviral therapy (ie, ribavirin) | No mention | No mention | Not recommended | Not recommended | Not recommended | Not recommended; might be a role for ribavirin in severely immunocompromised patients | Not routinely recommended | No mention |
| Cool mist or saline aerosol | No mention | No mention | Not recommended | No mention | Insufficient evidence | Not recommended | Not routinely recommended | No mention |
| Nutrition or hydration | Nasogastric or orogastric fluids first in infants who cannot maintain oral hydration; isotonic intravenous fluids in those who cannot tolerate nasogastric or orogastric, or impending respiratory failure | Nasogastric or intravenous fluids for infants who cannot maintain hydration | Nasogastric or intravenous fluids for infants who cannot maintain hydration | Consider nasogastric hydration (over intravenous) if difficulty maintaining hydration | Nasogastric or intravenous fluids for infants who cannot maintain hydration | Nasogastric or intravenous fluids for infants who cannot maintain hydration | Nasogastric or intravenous fluids for infants who cannot maintain hydration | Nasogastric or intravenous fluids for infants who cannot maintain hydration; consider restricting fluid intake to 66% of normal maintenance in severe bronchiolitis for risk of SiADH |
AAP=American Academy of Pediatrics. CPS=Canadian Pediatric Society. NICE=National Institute for Health and Care Excellence. SIGN=Scottish Intercollegiate Guidelines Network. SiADH=syndrome of inappropriate antidiuretic hormone excretion.
Appropriate use of pulse oximetry monitoring and initiation of oxygen for bronchiolitis have received increasing attention in studies and practice guidelines. Findings suggest that arbitrary thresholds for oxygen administration might drive hospital admissions and prolong hospital length of stay. These outcomes represent only part of the morbidity of bronchiolitis, but developing evidence suggests that intermittent hypoxaemia might occur commonly in otherwise stable infants with bronchiolitis and raises questions as to whether this factor should be used as a sole indication for admission to hospitals. A Canadian randomised trial found reduced admissions to hospital from the emergency department without any increase in revisits when pulse oximeters displayed values 3% higher than the actual value, suggesting that arbitrary pulse oximetry thresholds result in unnecessary admissions.51 A similar trial in the UK in the hospital setting found that reduction of the oxygen threshold from 94% to 90% resulted in earlier discharge from the hospital without any evidence of adverse outcomes.52 A US trial comparing intermittent versus continuous pulse oximetry in non-hypoxaemic infants in hospitals found similar outcomes between the groups.53 This US trial and other evidence supports recommendations in US practice guidelines that clinicians use a threshold of 90% for initiation of oxygen, whereas UK guidelines recommend 92%.38, 39 As the child improves, reduction in intensity of monitoring to intermittent checks is appropriate. A recent study using blinded oximetry at home showed that a substantial proportion of infants with bronchiolitis who are otherwise doing well have oxygen desaturations less than 90%, particularly during sleep, further calling into question arbitrary thresholds for hospital admissions and initiation of oxygen.54 This evidence will probably lead to efforts to reduce continuous monitoring in children without other indications for monitoring.
Imaging
The majority of children with bronchiolitis have either normal radiographs or radiographic findings consistent with simple bronchiolitis,55, 56, 57, 58 including peribronchial thickening, hyperinflation, and atelectasis. One prospective study58 of routine radiographs as part of the assessment for bronchiolitis in the emergency department reported airspace disease in 17 (7%) of 246 patients. Despite the low prevalence of radiographic pneumonia, this and other studies have reported an increase in antibiotic prescription after radiographs are performed, because of non-specific findings that influence clinicians' decisions.58, 59 Factors that have been associated with definite focal infiltrates consistent with pneumonia include hypoxia (oxygen saturation <92%),56, 57, 58, 60 grunting, persistently focal crackles, and fever (especially >39°C).38 Chest radiographs should only be considered in patients when the presentation is not classic for bronchiolitis. These situations include when another diagnosis (such as foreign body aspiration) is high on the differential diagnosis, when a child is severely ill and respiratory failure is imminent, and when symptoms are progressing or not resolving according to the typical disease course expected for bronchiolitis.
Lung ultrasound is increasingly used to assess cardiopulmonary conditions in adults and children. Several studies have investigated the use of lung ultrasound in the diagnosis of bronchiolitis. Two small studies found that ultrasound findings in infants with bronchiolitis correlate with clinical findings, and might be more specific than chest radiography,61, 62 but further studies are needed to establish whether there is a role for ultrasound in diagnosis or assessment of severity.
Viral testing
With the development of PCR to detect respiratory viruses in the nasopharynx, interest in the use of viral testing for causative diagnosis in bronchiolitis has increased. Virological testing, however, does not generally assist in management and is insufficient to predict outcomes.30, 63 Many national guidelines therefore recommend against routine virological testing in bronchiolitis (table). Recent studies suggest that higher respiratory syncytial virus genomic load, measured using quantitative PCR, might be associated with increased length of stay, use of respiratory support, and need for intensive care, in addition to recurrent wheezing, compared with lower viral loads.28, 31, 32, 64 Further study is warranted to confirm this association and clarify whether viral load measurement improves understanding of disease pathophysiology and severity. Several guidelines recommend using respiratory syncytial virus testing to guide cohorting of patients; however, the viruses most likely to cause bronchiolitis are all transmitted in a similar fashion (close contact with large-particle aerosols or direct contact with contaminated fomites).65, 66, 67 Thus, infection control might not be dependent on the identification of specific viruses, but rather on following strict precautions including hand hygiene, separating infants in shared hospital rooms by more than 1 m, and other infection control procedures.65 Additionally, given the sensitivity of PCR testing, results should be interpreted with caution. Certain viruses, such as rhinovirus, might be detected because of viral shedding from an unrelated illness or colonisation; whereas certain other viruses, such as respiratory syncytial virus and metapneumovirus, are almost always associated with an acute infection.
Blood and urine testing
Blood and urine testing is not routinely recommended as part of standard practice in the diagnostic work-up of bronchiolitis (table). A blood gas measurement should not be routinely obtained in infants with bronchiolitis, unless there are signs of impending respiratory failure or severe distress. Proportions of serious bacterial infections, especially bacteraemia and meningitis, are very low in infants with bronchiolitis.68 Abnormal white blood cell count is rarely useful in predicting serious bacterial infections in children infected with respiratory syncytial virus.69 Guidelines universally do not recommend complete blood counts in infants with bronchiolitis unless blood count is part of assessment for a fever in infants younger than 1–2 months. Similarly, given that bacteraemia is exceedingly rare (with cited proportions of <0·1% in the post-pneumococcal vaccine era), blood cultures should not be routinely performed, except in the septic work-up of infants younger than 1–2 months,70, 71 or in those with severe illness and signs of sepsis. Hydration status is an important consideration in infants with bronchiolitis and should be determined by clinical examination. Routine measurement of serum electrolytes is of little value in the majority of infants.
Urinary tract infections in infants with bronchiolitis occur with greater frequency than do bacteraemia and meningitis, with proportions ranging from 1% to 7%.68, 71, 72 It is reasonable to obtain a urinalysis and urine culture for infants aged less than 60 days with fever and for older febrile infants who have risk factors for urinary tract infections,73 but urine should not be routinely obtained in all infants with bronchiolitis.
Management
Bronchodilators
Current recommendations for management of bronchiolitis focus on agents to treat the pathophysiological effects of viral lower respiratory infection (eg, bronchodilators and hypertonic saline). Specific antivirals such as ribavirin to treat respiratory syncytial virus infection are not recommended in practice guidelines for typical cases of bronchiolitis because of challenging delivery methods, high cost, and potential health risks to caregivers. Multiple new agents for prevention and treatment are under investigation and might become available in the future, including immunoglobulins, small interfering RNA interference, fusion inhibitors, and small molecules.74
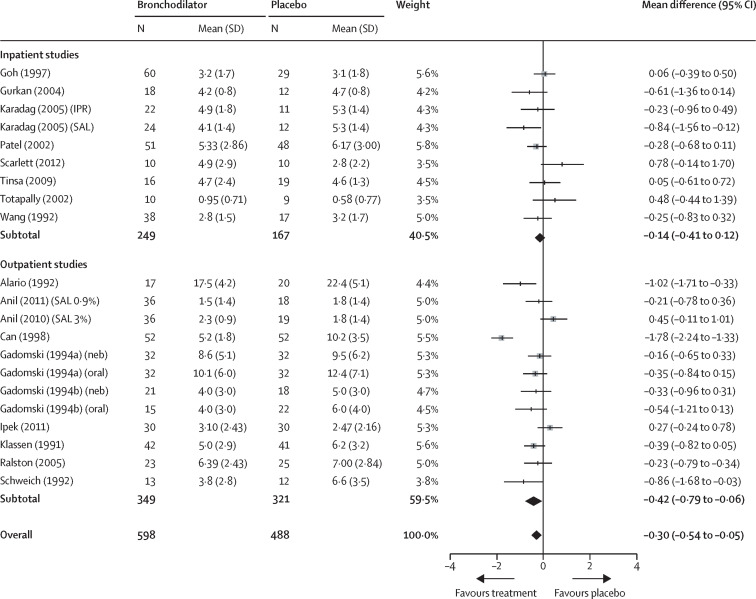
Numerous studies have assessed the role of bronchodilators for the treatment of bronchiolitis, and systematic reviews have found no consistent benefit. A 2014 Cochrane Collaboration systematic review identified 30 studies assessing bronchodilators, predominantly salbutamol and excluding epinephrine, and 21 studies that looked specifially at clinical scores found no evidence of benefit in any outcomes for infants admitted to hospitals.75 In outpatients, oxygen saturation, admission to hospital, or time to resolution of symptoms did not improve with bronchodilator usage compared with placebo. For outpatient studies assessing short-term change in pooled clinical scores, the reviewers found a small significant difference in mean score (Z=2·26; p=0·024) that was of small effect with minimal clinical importance (figure 2 ). Outpatient studies were heterogeneous (I 2=81%; p<0·00001), and those showing benefit in scores tended to include older children and children with recurrent wheezing.
Figure 2.
Meta-analysis of studies assessing average clinical score after treatment in patients with bronchiolitis receiving bronchodilators versus placebo
Test for heterogeneity in the inpatient studies demonstrated low inconsistency between the nine studies (I2=36%; p=0·13) and the summary effect was not significant (Z=1·06; p=0·29), the outpatient studies demonstrated very high inconsistency between the 12 studies (I2=81%; p<0·00001) and the summary effect was significant (Z=2·26; p=0·024), and the overall heterogeneity of the meta-analysis demonstrated high inconsistency between the 21 studies (I2=73%; p<0·00001) and the overall summary effect was significant (Z=2·4; p=0·016). IPR=ipratropium. SAL=salbutamol. neb=nebulised. Reproduced from Gadomski and Scribani,75 by permission of John Wiley and Sons.
Nebulised epinephrine was assessed in another Cochrane Collaboration systematic review.76 This review found no benefit for epinephrine compared with placebo for inpatients in hospital length of stay or other outcomes. A multicentre Scandinavian study published after this Cochrane review found that inpatients receiving standing doses of epinephrine had longer length of stay compared with inpatients receiving as-needed epinephrine or placebo.77 For outpatients, the Cochrane review found a difference in the numbers of admissions associated with epinephrine treatment during the time of an emergency department visit, but not during the overall course of illness when assessed at 1 week. Clinical practice guidelines including those from the USA, UK, and Canada do not recommend treatment with bronchodilators for bronchiolitis because of this evidence (table).38, 39, 45
Nebulised hypertonic saline
Nebulised hypertonic saline is thought to reduce airway oedema, decrease mucus plugging, improve mucociliary clearance, and rehydrate the airway surface liquid in infants with bronchiolitis.78 These physiological changes are extrapolated from the cystic fibrosis literature,79, 80 and the pathophysiological processes in acute bronchiolitis are different. Therefore, the theoretical benefits of hypertonic saline seen in cystic fibrosis might not be present in infants with acute viral bronchiolitis. Although initial trials demonstrated some ability of hypertonic saline to decrease hospital length of stay and transiently improve clinical severity score,81, 82, 83 more recent trials demonstrated conflicting results.84, 85, 86, 87, 88, 89, 90 The trials that showed the largest benefit were done in hospitals with lengths of stay more than 72 h; thus, hypertonic saline for infants in countries and institutions in which the length of stay approaches or exceeds 72 h might be beneficial at reducing length of stay. The conflicting results are reflected in the differences in recommendations across national guidelines (table), with some countries not recommending hypertonic saline, some recommending use for all inpatients, and some recommending use only in moderate to severe illness.
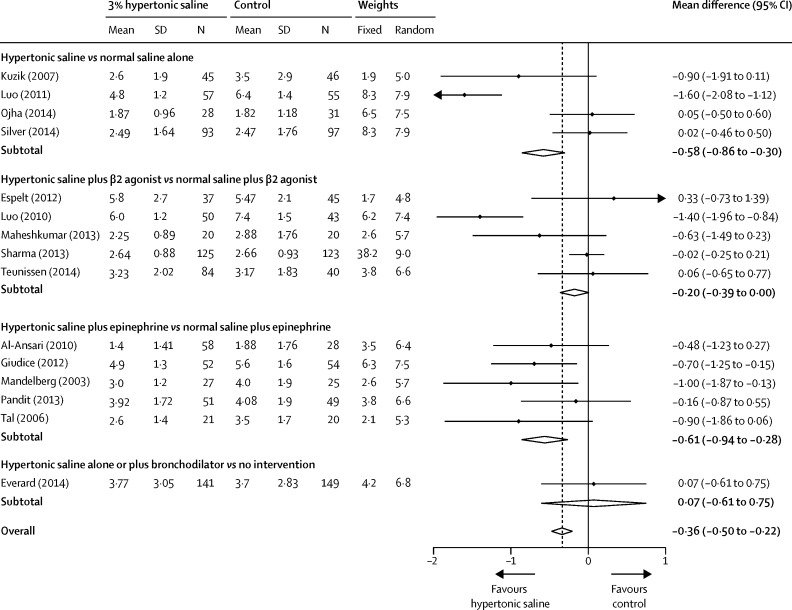
The largest systematic review and meta-analysis, published in 2015, examined 24 trials and 3209 patients.91 Infants receiving hypertonic saline had a significant difference in hospital length of stay of −0·45 days (95% CI −0·82 to −0·08; p=0·01) compared with those receiving 0·9% saline or standard care. In seven trials, hypertonic saline reduced the risk of admission to hospital by 20% (risk ratio 0·8; 95% CI 0·67–0·96) compared with 0·9% saline. No substantial adverse effects of hypertonic saline were noted in this systematic review. Although the results of this meta-analysis were significant, attention should be paid to the outer limits of the confidence intervals, which approach no difference, and to the clinical relevance of these differences. A second 2015 meta-analysis of 15 trials and 1922 patients found a smaller, but significant, decrease in length of stay by −0·36 days (95% CI −0·5 to −0·22; p<0·001) in those who received hypertonic saline (figure 3 ).92 This study found a discrepancy between the overall combined effect of all studies on length of stay and the negative results from the largest trials, allowing the authors to conclude that neither individual trials nor pooled estimates provide a strong evidence-based foundation for the use of hypertonic saline. Both meta-analyses showed substantial heterogeneity across studies (I 2=82·1%, p<0·001;91 and I 2=77·8%, p=0·02992). A recent reanalysis of the first 2015 meta-analysis removed two outlying Chinese studies and accounted for imbalances in day of illness at presentation.93 These analyses resolved the heterogeneity and found that hypertonic saline does not reduce length of stay in infants admitted to hospitals with bronchiolitis (mean difference in length of stay removing outliers −0·21 days; 95% CI −0·43 to 0·02; mean difference in length of stay accounting for day of illness imbalance 0·02 days; 95% CI −0·14 to 0·17). Large trials have not demonstrated benefit for hypertonic saline and this meta-analysis found no effect of hypertonic saline on length of stay after adjustment for outliers and imbalances. The decision to undertake future trials is controversial given the positive results of some meta-analyses and negative results of others.
Figure 3.
Meta-analysis of studies assessing hospital length of stay in patients with bronchiolitis receiving nebulised 3% hypertonic saline versus control
Significant difference in length of hospital stay was found in those receiving hypertonic saline compared with control; however, the largest trials had negative results, making it challenging to provide definitive conclusions regarding use of hypertonic saline in bronchiolitis. Reproduced from Maguire and colleagues,92 under the CC BY 4.0 Creative Commons license: http://creativecommons.org/licenses/by/4.0/.
Corticosteroids
Multiple studies have examined the role of corticosteroids in the management of children with bronchiolitis. Data from two large multicentre trials have shown no benefit to corticosteroids alone in reducing admissions to hospital,94, 95 and a 2013 Cochrane Collaboration review supports the results of these studies.96 This review included only studies that enrolled children younger than 24 months with a first episode of wheezing and signs of a viral illness. Among the included eight outpatient studies (1824 participants) comparing corticosteroids with placebo there was no reduction in admission at day 1 (Z=1·05; p=0·3) or day 7 (Z=1·38; p=0·17) after enrolment (figure 4 ), clinical scores, length of stay in the emergency department, or length of time to resolution of symptoms. Among the nine inpatient studies (772 participants), length of hospital stay was not reduced.96 On the basis of this evidence, multiple clinical practice guidelines recommend against the use of corticosteroids for infants with bronchiolitis (table). Although clinicians report considering a family or personal history of atopy when deciding whether to treat infants with bronchiolitis with corticosteroids,41 there is no evidence that such infants receive any benefit from corticosteroid treatment.94, 95, 96 Evidence for the presence or absence of respiratory syncytial virus infection in these infants being associated with a response to corticosteroids is also unavailable.94, 95 Authors from a large study with a factorial design have suggested, in an unadjusted analysis, that high-dose corticosteroids in combination with nebulised epinephrine might reduce admissions for outpatients with bronchiolitis by day 7,95 but these results are considered exploratory.39, 45
Figure 4.
Meta-analysis of studies assessing admission to hospital on day 1 and day 7 in patients with bronchiolitis receiving corticosteroids versus placebo
Test for heterogeneity in studies assessing admission at day 1 demonstrated very low inconsistency between the ten studies (I2=0%; p=0·55) and the summary effect was not significant (Z=1·05; p=0·30), and studies assessing admission at day 7 demonstrated low inconsistency between the six studies (I2=32%; p=0·21) and the summary effect was not significant (Z=1·38; p=0·17). G=glucocorticoid. P=placebo. S=salbutamol. E=epinephrine. Reproduced from Fernandes and colleagues,96 by permission of John Wiley and Sons.
High-flow oxygen and respiratory support
Non-invasive technologies to improve oxygenation and ventilation for bronchiolitis include humidified high-flow nasal cannula oxygen and continuous positive airway pressure.97 High-flow nasal cannula allows delivery of high flows (usually 1–2 L/kg per min) with humidification and a cannula designed to improve patient tolerance. It has been used widely in premature infants, but the mechanisms of action are unclear, in particular whether it might deliver positive end-expiratory pressure in some conditions. Evidence for efficacy of high-flow nasal cannula is predominantly observational, with studies documenting improved respiratory parameters and reduced intubation rates after implementation.97 One small randomised trial compared high-flow nasal cannula with hypertonic saline and found no difference in change in respiratory score.98 Concerns about high-flow nasal cannula include the potential for rapid deterioration if the infant is not closely monitored and costs associated with overuse.
Continuous positive airway pressure has been studied in intensive care settings in observational studies and several small trials, with some evidence of improved respiratory parameters.97 The UK guidelines recommend considering continuous positive airway pressure in children with impending respiratory failure from bronchiolitis.
Antibiotics
Antibiotic overuse in children with bronchiolitis probably occurs because of concerns about the presence of fever, the young age of affected patients, difficulty differentiating atelectasis from infectious consolidation on chest radiograph, and concern for undetected secondary bacterial infection. Bronchiolitis, however, has a clear viral cause and the occurrence of secondary bacterial infections is low, with a risk of bacteraemia or meningitis of less than 1%.99 A detailed review of randomised clinical trials found that routine use of antibiotics did not improve duration of symptoms, length of hospital stay, need for oxygen therapy, or hospital admission.38 Overuse of antibiotics is known to result in unnecessary adverse effects on the patient, and the development of antimicrobial resistance. Routine use should be avoided unless there is clear evidence of a secondary bacterial infection (table). Acute otitis media has been documented in up to 60% of infants with bronchiolitis.100, 101 Antibiotic use for acute otitis media in bronchiolitis should follow established evidence and guidelines for acute otitis media.102
Macrolide antibiotics have anti-inflammatory properties that might have potential benefit in mitigating the inflammation present in bronchiolitis. Two randomised trials found that there was no difference between azithromycin and placebo in hospital length of stay, need for oxygen, or hospital re-admission.103, 104 Another randomised trial found that azithromycin lowered nasal interleukin-8 concentrations, prolonged time to subsequent wheezing episodes, and resulted in fewer days with respiratory symptoms in the year following the bronchiolitis episode compared with placebo.105 Finally, a US multicentre study found that in children aged 12–72 months with a history of recurrent severe lower respiratory tract infections, early administration of azithromycin during a lower respiratory tract infection reduced the likelihood of progression to a severe infection, but it is not clear whether the underlying disease in these children was bronchiolitis or some other disease process.106 Given the current evidence, routine use of macrolides is not recommended in bronchiolitis and more research is needed to clarify any potential role it might have in the future.
Supportive therapies
Hydration, suctioning, and chest physiotherapy have been suggested as supportive therapies. Infants with bronchiolitis might have difficulty feeding because of nasal congestion and increased work of breathing; thus, hydration remains a cornerstone of therapy. A multicentre study of 759 infants younger than 12 months admitted to hospital with bronchiolitis showed no benefit of intravenous fluids compared with administration of fluids by nasogastric tube in mean length of stay, admission to the intensive care unit, need for ventilatory support, and adverse events. This trial also found that a nasogastric tube might be easier to place than an intravenous line in these infants.107 Most guidelines recommend either nasogastric or intravenous fluids to maintain hydration, with the UK and Scottish guidelines preferring nasogastric or orogastric hydration in those that can tolerate it compared with intravenous hydration (table). If intravenous fluids are used, isotonic fluids are preferred to avoid risk of hyponatraemia.38
Because infants are obligate nasal breathers, nasal suctioning has been suggested to help with clearing of the nares, improve the work of breathing, and improve feeding; however, suctioning might irritate the nasal mucosa and result in oedema. No randomised controlled trials have examined the role of nasal suctioning in bronchiolitis. The insufficient available evidence includes a retrospective cohort study of 740 infants108 and a small observational study of 40 infants.109 These studies suggest that deep suctioning might increase length of stay for inpatients,108 infrequent suctioning is associated with an increased length of stay,108 and oxygen saturation might increase after suctioning.109 To draw conclusions about causality from these observational studies is difficult, because the potential for confouding by indication exists (eg, sicker children might be more likely to receive deep suctioning). Evidence suggests that oxygen saturation increases after nasal irrigation even without suctioning.110 Current guidelines give differing recommendations with regard to suctioning; those that support its use recommend only superficial suctioning rather than deep suctioning (table).38, 39, 45
Chest physiotherapy use in bronchiolitis appears to vary by country.111, 112 A recent Cochrane Collaboration review of 12 studies (1249 participants) demonstrated no evidence of benefit to any type of chest physiotherapy among inpatients in length of stay, oxygen saturation, or respiratory parameters.113 No published guidelines routinely recommend chest physiotherapy for the management of uncomplicated bronchiolitis in otherwise healthy children without respiratory comorbidities (table).38, 39, 45
Prognosis
Much work has been published about the risk of developing recurrent wheezing and asthma following bronchiolitis in infancy.114, 115, 116 Studies have followed birth cohorts to determine the risk of subsequent wheezing after lower respiratory tract infection in young childhood, and cohorts of children admitted to hospital with bronchiolitis.114, 115, 116, 117 Overall, admission to hospital with bronchiolitis at a young age is associated with an increased risk of recurrent wheezing. Studies report that 17–60% of children with bronchiolitis might develop recurrent wheezing in the years following their initial admission to hospital. A large study from Taiwan that followed up 1981 children admitted with bronchiolitis before age 3 years found that by age 10 years, 351 (17·7%) of 1981 children with bronchiolitis had a diagnosis of asthma compared with 2159 (11·7%) of 18 527 controls (hazard ratio 1·58; 95% CI 1·41–1·71).118 One small cohort study of 138 patients has suggested that 18 (39%) of 46 children admitted with bronchiolitis before 12 months have asthma by 18 years compared with eight (9%) of 92 controls.115 However, another study that followed a birth cohort of 1246 children found that although lower respiratory tract infection in childhood was associated with an increased risk of recurrent wheezing, this association decreased with age and was not significant by age 13 years.116 Most children in this cohort had mild illness not requiring hospital admission, and severity of illness might be associated with the increased risk of asthma.119 The question remains whether respiratory infection at a young age itself predisposes children to asthma through damage or alteration of lung function, or whether children with severe bronchiolitis might have individual risk factors (such as altered immune response or airway function) that predisposes them to both severe bronchiolitis and recurrent wheezing.8
Knowledge gaps and controversies
Substantial knowledge gaps and controversies exist in the management of acute bronchiolitis. The role of nebulised hypertonic saline in acute management is not clear, resulting in conflicting recommendations across clinical guidelines (table). Although meta-analyses suggest a small reduction of length of stay, these analyses are limited by heterogeneity, not accounting for duration of illness, and not considering the role of outlying study populations.91 Two large multicentre trials do not support a clinically significant difference in length of stay for inpatients and there is no clear evidence of cost benefit.4, 89, 90, 91, 120 While the same meta-analysis suggests a possible reduction in admissions for outpatients, the confidence intervals were wide and the studies were also heterogeneous.91 No multicentre studies of nebulised hypertonic saline have been completed in outpatients. Although the evidence is increasing that hypertonic saline has little role in meaningfully reducing the length of stay, its role in outpatients is less clear. A large outpatient multicentre study could clarify whether there is any benefit.
Evidence also suggests that combined therapy with nebulised epinephrine and corticosteroids might reduce admissions to hospital.95 Synergy between corticosteroids and β2 agonists is well documented in clinical trials of asthma management.121, 122, 123, 124 Basic science literature also shows that β2 agonists and corticosteroids enhance each other's effectiveness, particularly with regard to anti-inflammatory gene expression.125, 126 Because of the economic burden of bronchiolitis and the plausible basic and clinical evidence for synergy, a large and multicentre trial is needed to ascertain whether combined therapy with epinephrine and corticosteroids is beneficial.
Oxygen saturation and the use of pulse oximetry play an important role in the decision to admit infants with bronchiolitis to hospital and in the length of their hospital stay.51, 52, 53, 54, 55, 56, 57, 58, 59 Clinical practice guidelines also give conflicting guidance on the level of oxygen saturation at which admission should be considered. Furthermore, a substantial proportion of discharged infants have episodes of transient desaturation.54 Again, in view of the large health-care costs associated with hospital admission in bronchiolitis, further research is needed to clarify the level of oxygen saturation requiring admission, the role of continuous and spot measurements of oxygen saturation, and the clinical importance of transient desaturations in otherwise stable young infants.
Search strategy and selection criteria
We searched the Cochrane Collaboration Library for systematic reviews and PubMed for scientific articles in English only from Jan 1, 2005, to Jan 31, 2016, using the search terms “bronchiolitis” and “respiratory syncytial virus”. We added the following appropriate search terms: “epidemiology”, “microbiology”, “pathophysiology”, “diagnosis OR severity”, “interventions” (including “oxygen”, “bronchodilators”, “hypertonic saline”, “corticosteroids”, “respiratory therapies”, “antimicrobials”, “chest physiotherapy”, “suctioning”, and “hydration”), and “prognosis”. In addition, we reviewed references and available technical reports from recent national guidelines from the USA, UK, and Canada, which conducted systematic reviews of the literature; as well as guidelines from Scotland, Italy, Spain, Australia, and France. We tabulated recommendations from these guidelines into a table.
Acknowledgments
Acknowledgments
TAF receives funding from the National Institutes of Health—National Institute of Allergy and Infectious Diseases (grant 1K23AI121325-01). The NIH had no role in the writing of this manuscript, and in the decision to submit the paper for publication. We would like to thank Kerry Aicholtz for her administrative support.
Contributors
TAF contributed to the design and coordinated the writing of this manuscript. All authors contributed to the literature search and writing of this manuscript.
Declarations of interest
We declare no competing interests. TAF, ACP, and JJZ have participated in trials of bronchiolitis funded by unrestricted public or academic institutional funding sources that had no influence on the conception and writing of this manuscript.
References
- 1.Kyu HH, Pinho C, Wagner JA. Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: findings from the Global Burden of Disease 2013 Study. JAMA Pediatr. 2016;170:267–287. doi: 10.1001/jamapediatrics.2015.4276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nair H, Nokes DJ, Gessner BD. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375:1545–1555. doi: 10.1016/S0140-6736(10)60206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pfuntner A, Wier L, Stocks C. Most frequent conditions in US hospitals, 2010. HCUP Statistical Brief #148. 2013. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb148.pdf (accessed March 30, 2016). [PubMed]
- 4.Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA., Jr Temporal trends in emergency department visits for bronchiolitis in the United States, 2006 to 2010. Pediatr Infect Dis J. 2014;33:11–18. doi: 10.1097/INF.0b013e3182a5f324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA., Jr Trends in bronchiolitis hospitalizations in the United States, 2000–2009. Pediatrics. 2013;132:28–36. doi: 10.1542/peds.2012-3877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haynes AK, Prill MM, Iwane MK, Gerber SI. Respiratory syncytial virus—United States, July 2012–June 2014. MMWR Morb Mortal Wkly Rep. 2014;63:1133–1136. [PMC free article] [PubMed] [Google Scholar]
- 7.Haynes AK, Manangan AP, Iwane MK. Respiratory syncytial virus circulation in seven countries with Global Disease Detection Regional Centers. J Infect Dis. 2013;208(suppl 3):S246–S254. doi: 10.1093/infdis/jit515. [DOI] [PubMed] [Google Scholar]
- 8.Meissner HC. Viral bronchiolitis in children. N Engl J Med. 2016;374:62–72. doi: 10.1056/NEJMra1413456. [DOI] [PubMed] [Google Scholar]
- 9.Foxman EF, Storer JA, Fitzgerald ME. Temperature-dependent innate defense against the common cold virus limits viral replication at warm temperature in mouse airway cells. Proc Natl Acad Sci USA. 2015;112:827–832. doi: 10.1073/pnas.1411030112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salah B, Dinh Xuan AT, Fouilladieu JL, Lockhart A, Regnard J. Nasal mucociliary transport in healthy subjects is slower when breathing dry air. Eur Respir J. 1988;1:852–855. [PubMed] [Google Scholar]
- 11.Wang VJ, Cavagnaro CS, Clark S, Camargo CA, Jr, Mansbach JM. Altitude and environmental climate effects on bronchiolitis severity among children presenting to the emergency department. J Environ Health. 2012;75:8–15. [PubMed] [Google Scholar]
- 12.Yusuf S, Piedimonte G, Auais A. The relationship of meteorological conditions to the epidemic activity of respiratory syncytial virus. Epidemiol Infect. 2007;135:1077–1090. doi: 10.1017/S095026880600776X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Darrow LA, Klein M, Flanders WD, Mulholland JA, Tolbert PE, Strickland MJ. Air pollution and acute respiratory infections among children 0–4 years of age: a 1–8 year time-series study. Am J Epidemiol. 2014;180:968–977. doi: 10.1093/aje/kwu234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim BJ, Seo JH, Jung YH. Air pollution interacts with past episodes of bronchiolitis in the development of asthma. Allergy. 2013;68:517–523. doi: 10.1111/all.12104. [DOI] [PubMed] [Google Scholar]
- 15.Rice MB, Rifas-Shiman SL, Oken E. Exposure to traffic and early life respiratory infection: a cohort study. Pediatr Pulmonol. 2014 doi: 10.1002/ppul.23029. published online March 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DiFranza JR, Masaquel A, Barrett AM, Colosia AD, Mahadevia PJ. Systematic literature review assessing tobacco smoke exposure as a risk factor for serious respiratory syncytial virus disease among infants and young children. BMC Pediatr. 2012;12:81. doi: 10.1186/1471-2431-12-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bradley JP, Bacharier LB, Bonfiglio J. Severity of respiratory syncytial virus bronchiolitis is affected by cigarette smoke exposure and atopy. Pediatrics. 2005;115:e7–14. doi: 10.1542/peds.2004-0059. [DOI] [PubMed] [Google Scholar]
- 18.Stockman LJ, Curns AT, Anderson LJ, Fischer-Langley G. Respiratory syncytial virus-associated hospitalizations among infants and young children in the United States, 1997–2006. Pediatr Infect Dis J. 2012;31:5–9. doi: 10.1097/INF.0b013e31822e68e6. [DOI] [PubMed] [Google Scholar]
- 19.Hall CB, Weinberg GA, Blumkin AK. Respiratory syncytial virus-associated hospitalizations among children less than 24 months of age. Pediatrics. 2013;132:e341–e348. doi: 10.1542/peds.2013-0303. [DOI] [PubMed] [Google Scholar]
- 20.Schuurhof A, Bont L, Siezen CL. Interleukin-9 polymorphism in infants with respiratory syncytial virus infection: an opposite effect in boys and girls. Pediatr Pulmonol. 2010;45:608–613. doi: 10.1002/ppul.21229. [DOI] [PubMed] [Google Scholar]
- 21.Ali S, Plint AC, Klassen TP. Bronchiolitis. In: Wilmott RW, Kendig EL, Boat TF, Bush A, Chernick V, editors. Kendig and Chernick's disorders of the respiratory tract in children. 8th edn. Elsevier Saunders; Philadelphia: 2012. pp. 443–452. [Google Scholar]
- 22.Aherne W, Bird T, Court SD, Gardner PS, McQuillin J. Pathological changes in virus infections of the lower respiratory tract in children. J Clin Pathol. 1970;23:7–18. doi: 10.1136/jcp.23.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mansbach JM, Camargo CA., Jr Bronchiolitis: lingering questions about its definition and the potential role of vitamin D. Pediatrics. 2008;122:177–179. doi: 10.1542/peds.2007-3323. [DOI] [PubMed] [Google Scholar]
- 24.Calvo C, Pozo F, Garcia-Garcia ML. Detection of new respiratory viruses in hospitalized infants with bronchiolitis: a three-year prospective study. Acta Paediatr. 2010;99:883–887. doi: 10.1111/j.1651-2227.2010.01714.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Midulla F, Scagnolari C, Bonci E. Respiratory syncytial virus, human bocavirus and rhinovirus bronchiolitis in infants. Arch Dis Child. 2010;95:35–41. doi: 10.1136/adc.2008.153361. [DOI] [PubMed] [Google Scholar]
- 26.Marguet C, Lubrano M, Gueudin M. In very young infants severity of acute bronchiolitis depends on carried viruses. PLoS One. 2009;4:e4596. doi: 10.1371/journal.pone.0004596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller EK, Gebretsadik T, Carroll KN. Viral etiologies of infant bronchiolitis, croup and upper respiratory illness during 4 consecutive years. Pediatr Infect Dis J. 2013;32:950–955. doi: 10.1097/INF.0b013e31829b7e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Skjerven HO, Megremis S, Papadopoulos NG, Mowinckel P, Carlsen KH, Lodrup Carlsen KC. Virus type and genomic load in acute bronchiolitis: severity and treatment response with inhaled adrenaline. J Infect Dis. 2016;213:915–921. doi: 10.1093/infdis/jiv513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mansbach JM, McAdam AJ, Clark S. Prospective multicenter study of the viral etiology of bronchiolitis in the emergency department. Acad Emerg Med. 2008;15:111–118. doi: 10.1111/j.1553-2712.2007.00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mansbach JM, Piedra PA, Teach SJ. Prospective multicenter study of viral etiology and hospital length of stay in children with severe bronchiolitis. Arch Pediatr Adolesc Med. 2012;166:700–706. doi: 10.1001/archpediatrics.2011.1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hasegawa K, Jartti T, Mansbach JM. Respiratory syncytial virus genomic load and disease severity among children hospitalized with bronchiolitis: multicenter cohort studies in the United States and Finland. J Infect Dis. 2015;211:1550–1559. doi: 10.1093/infdis/jiu658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scagnolari C, Midulla F, Selvaggi C. Evaluation of viral load in infants hospitalized with bronchiolitis caused by respiratory syncytial virus. Med Microbiol Immunol. 2012;201:311–317. doi: 10.1007/s00430-012-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Papadopoulos NG, Moustaki M, Tsolia M. Association of rhinovirus infection with increased disease severity in acute bronchiolitis. Am J Respir Crit Care Med. 2002;165:1285–1289. doi: 10.1164/rccm.200112-118BC. [DOI] [PubMed] [Google Scholar]
- 34.Semple MG, Cowell A, Dove W. Dual infection of infants by human metapneumovirus and human respiratory syncytial virus is strongly associated with severe bronchiolitis. J Infect Dis. 2005;191:382–386. doi: 10.1086/426457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jansen RR, Wieringa J, Koekkoek SM. Frequent detection of respiratory viruses without symptoms: toward defining clinically relevant cutoff values. J Clin Microbiol. 2011;49:2631–2636. doi: 10.1128/JCM.02094-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hasegawa K, Linnemann RW, Avadhanula V. Detection of respiratory syncytial virus and rhinovirus in healthy infants. BMC Res Notes. 2015;8:718. doi: 10.1186/s13104-015-1695-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Self WH, Williams DJ, Zhu Y. Respiratory viral detection in children and adults: comparing asymptomatic controls and patients with community-acquired pneumonia. J Infect Dis. 2016;213:584–591. doi: 10.1093/infdis/jiv323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bronchiolitis in children: diagnosis and management NICE guideline. 2015. https://www.nice.org.uk/Guidance/NG9 (accessed March 30, 2016). [PubMed]
- 39.Ralston SL, Lieberthal AS, Meissner HC. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134:e1474–e1502. doi: 10.1542/peds.2014-2742. [DOI] [PubMed] [Google Scholar]
- 40.Court SD. The definition of acute respiratory illnesses in children. Postgrad Med J. 1973;49:771–776. doi: 10.1136/pgmj.49.577.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Plint AC, Grenon R, Klassen TP, Johnson DW. Bronchodilator and steroid use for the management of bronchiolitis in Canadian pediatric emergency departments. CJEM. 2015;17:46–53. doi: 10.2310/8000.2013.131325. [DOI] [PubMed] [Google Scholar]
- 42.Fernandes RM, Plint AC, Terwee CB. Validity of bronchiolitis outcome measures. Pediatrics. 2015;135:e1399–e1408. doi: 10.1542/peds.2014-3557. [DOI] [PubMed] [Google Scholar]
- 43.McCallum GB, Morris PS, Wilson CC. Severity scoring systems: are they internally valid, reliable and predictive of oxygen use in children with acute bronchiolitis? Pediatr Pulmonol. 2013;48:797–803. doi: 10.1002/ppul.22627. [DOI] [PubMed] [Google Scholar]
- 44.Willwerth BM, Harper MB, Greenes DS. Identifying hospitalized infants who have bronchiolitis and are at high risk for apnea. Ann Emerg Med. 2006;48:441–447. doi: 10.1016/j.annemergmed.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 45.Friedman JN, Rieder MJ, Walton JM. Bronchiolitis: recommendations for diagnosis, monitoring and management of children one to 24 months of age. Paediatr Child Health. 2014;19:485–498. doi: 10.1093/pch/19.9.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Scottish Intercollegiate Guidelines Network (SIGN) Bronchiolitis in children: a national clinical guideline. 2006. http://sign.ac.uk/guidelines/fulltext/91/index.html (accessed March 30, 2016).
- 47.Baraldi E, Lanari M, Manzoni P. Inter-society consensus document on treatment and prevention of bronchiolitis in newborns and infants. Ital J Pediatr. 2014;40:65. doi: 10.1186/1824-7288-40-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Working Group of the Clinical Practice Guideline on Acute Bronchiolitis. Quality plan for the Spanish national healthcare system of the Spanish Ministry for Health and Social Policy; Catalan Agency for Health Technology Assessment, 2010. Clinical Practice Guidelines in the Spanish National Healthcare System: CAHTA no. 2007/05.
- 49.Turner T, Wilkinson F, Harris C, Mazza D. Evidence based guidelines for the management of bronchiolitis. Aust Fam Physician. 2008;37:6–13. [PubMed] [Google Scholar]
- 50.Verstraete M, Cros P, Gouin M. Prise en charge de la bronchiolite aiguë du nourrisson de moins 1 an: actualization et consensus medical au sein des hôpitaux universitaires du Grand Ouest (HUGO) Arch Pediatr. 2014;21:53–62. doi: 10.1016/j.arcped.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 51.Schuh S, Freedman S, Coates A. Effect of oximetry on hospitalization in bronchiolitis: a randomized clinical trial. JAMA. 2014;312:712–718. doi: 10.1001/jama.2014.8637. [DOI] [PubMed] [Google Scholar]
- 52.Cunningham S, Rodriguez A, Adams T. Oxygen saturation targets in infants with bronchiolitis (BIDS): a double-blind, randomised, equivalence trial. Lancet. 2015;386:1041–1048. doi: 10.1016/S0140-6736(15)00163-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McCulloh R, Koster M, Ralston S. Use of intermittent vs continuous pulse oximetry for non-hypoxemic infants and young children hospitalized for bronchiolitis: a randomized clinical trial. JAMA Pediatr. 2015;169:898–904. doi: 10.1001/jamapediatrics.2015.1746. [DOI] [PubMed] [Google Scholar]
- 54.Principi T, Coates AL, Parkin PC, Stephens D, DaSilva Z, Schuh S. Effect of oxygen desaturations on subsequent medical visits in infants discharged from the emergency department with bronchiolitis. JAMA Pediatr. 2016;170:602–608. doi: 10.1001/jamapediatrics.2016.0114. [DOI] [PubMed] [Google Scholar]
- 55.Mahabee-Gittens EM, Bachman DT, Shapiro ED, Dowd MD. Chest radiographs in the pediatric emergency department for children < or = 18 months of age with wheezing. Clin Pediatr (Phila) 1999;38:395–399. doi: 10.1177/000992289903800703. [DOI] [PubMed] [Google Scholar]
- 56.Mathews B, Shah S, Cleveland RH, Lee EY, Bachur RG, Neuman MI. Clinical predictors of pneumonia among children with wheezing. Pediatrics. 2009;124:e29–e36. doi: 10.1542/peds.2008-2062. [DOI] [PubMed] [Google Scholar]
- 57.Ecochard-Dugelay E, Beliah M, Perreaux F. Clinical predictors of radiographic abnormalities among infants with bronchiolitis in a paediatric emergency department. BMC Pediatr. 2014;14:143. doi: 10.1186/1471-2431-14-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schuh S, Lalani A, Allen U. Evaluation of the utility of radiography in acute bronchiolitis. J Pediatr. 2007;150:429–433. doi: 10.1016/j.jpeds.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ecochard-Dugelay E, Beliah M, Boisson C. Impact of chest radiography for children with lower respiratory tract infection: a propensity score approach. PLoS One. 2014;9:e96189. doi: 10.1371/journal.pone.0096189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mahabee-Gittens EM, Dowd MD, Beck JA, Smith SZ. Clinical factors associated with focal infiltrates in wheezing infants and toddlers. Clin Pediatr (Phila) 2000;39:387–393. doi: 10.1177/000992280003900702. [DOI] [PubMed] [Google Scholar]
- 61.Caiulo VA, Gargani L, Caiulo S. Lung ultrasound in bronchiolitis: comparison with chest X-ray. Eur J Pediatr. 2011;170:1427–1433. doi: 10.1007/s00431-011-1461-2. [DOI] [PubMed] [Google Scholar]
- 62.Basile V, Di Mauro A, Scalini E. Lung ultrasound: a useful tool in diagnosis and management of bronchiolitis. BMC Pediatr. 2015;15:63. doi: 10.1186/s12887-015-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stollar F, Alcoba G, Gervaix A, Argiroffo CB. Virologic testing in bronchiolitis: does it change management decisions and predict outcomes? Eur J Pediatr. 2014;173:1429–1435. doi: 10.1007/s00431-014-2334-2. [DOI] [PubMed] [Google Scholar]
- 64.Nenna R, Ferrara M, Nicolai A. Viral load in infants hospitalized for respiratory syncytial virus bronchiolitis correlates with recurrent wheezing at thirty-six-month follow-up. Pediatr Infect Dis J. 2015;34:1131–1132. doi: 10.1097/INF.0000000000000825. [DOI] [PubMed] [Google Scholar]
- 65.Hall CB. The spread of influenza and other respiratory viruses: complexities and conjectures. Clin Infect Dis. 2007;45:353–359. doi: 10.1086/519433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fabian M, McDevitt J, Milton D. Modes of transmission of respiratory viral infections. In: Johnston SL, O'Byrne P, eds. Exacerbations of asthma. Boston: exposure, epidemiology risk program. Department of Environmental Health Harvard School of Public Health, 2005: 2007: 1–2.
- 67.Brankston G, Gitterman L, Hirji Z, Lemieux C, Gardam M. Transmission of influenza A in human beings. Lancet Infect Dis. 2007;7:257–265. doi: 10.1016/S1473-3099(07)70029-4. [DOI] [PubMed] [Google Scholar]
- 68.Levine DA, Platt SL, Dayan PS. Risk of serious bacterial infection in young febrile infants with respiratory syncytial virus infections. Pediatrics. 2004;113:1728–1734. doi: 10.1542/peds.113.6.1728. [DOI] [PubMed] [Google Scholar]
- 69.Purcell K, Fergie J. Lack of usefulness of an abnormal white blood cell count for predicting a concurrent serious bacterial infection in infants and young children hospitalized with respiratory syncytial virus lower respiratory tract infection. Pediatr Infect Dis J. 2007;26:311–315. doi: 10.1097/01.inf.0000258627.23337.00. [DOI] [PubMed] [Google Scholar]
- 70.Librizzi J, McCulloh R, Koehn K, Alverson B. Appropriateness of testing for serious bacterial infection in children hospitalized with bronchiolitis. Hosp Pediatr. 2014;4:33–38. doi: 10.1542/hpeds.2013-0073. [DOI] [PubMed] [Google Scholar]
- 71.Ralston S, Hill V, Waters A. Occult serious bacterial infection in infants younger than 60 to 90 days with bronchiolitis a systematic review. Arch Pediat Adol Med. 2011;165:951–956. doi: 10.1001/archpediatrics.2011.155. [DOI] [PubMed] [Google Scholar]
- 72.Elkhunovich MA, Wang VJ. Assessing the utility of urine testing in febrile infants aged 2 to 12 months with bronchiolitis. Pediatr Emerg Care. 2015;31:616–620. doi: 10.1097/PEC.0000000000000359. [DOI] [PubMed] [Google Scholar]
- 73.Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128:595–610. doi: 10.1542/peds.2011-1330. [DOI] [PubMed] [Google Scholar]
- 74.Mazur NI, Martinón-Torres F, Baraldi E. Lower respiratory tract infection caused by respiratory syncytial virus: current management and new therapeutics. Lancet Respir Med. 2015;3:888–900. doi: 10.1016/S2213-2600(15)00255-6. [DOI] [PubMed] [Google Scholar]
- 75.Gadomski AM, Scribani MB. Bronchodilators for bronchiolitis. Cochrane Database Syst Rev. 2014;6 doi: 10.1002/14651858.CD001266.pub4. CD001266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hartling L, Bialy LM, Vandermeer B. Epinephrine for bronchiolitis. Cochrane Database Syst Rev. 2011;6 doi: 10.1002/14651858.CD003123.pub3. CD003123. [DOI] [PubMed] [Google Scholar]
- 77.Skjerven HO, Hunderi JO, Brugmann-Pieper SK. Racemic adrenaline and inhalation strategies in acute bronchiolitis. N Engl J Med. 2013;368:2286–2293. doi: 10.1056/NEJMoa1301839. [DOI] [PubMed] [Google Scholar]
- 78.Mandelberg A, Amirav I. Hypertonic saline or high volume normal saline for viral bronchiolitis: mechanisms and rationale. Pediatr Pulmonol. 2010;45:36–40. doi: 10.1002/ppul.21185. [DOI] [PubMed] [Google Scholar]
- 79.Wills PJ, Hall RL, Chan W, Cole PJ. Sodium chloride increases the ciliary transportability of cystic fibrosis and bronchiectasis sputum on the mucus-depleted bovine trachea. J Clin Invest. 1997;99:9–13. doi: 10.1172/JCI119138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Donaldson SH. Hydrator therapies for cystic fibrosis lung disease. Pediatric Pulmonology. 2008;43:S18–S23. [Google Scholar]
- 81.Mandelberg A, Tal G, Witzling M. Nebulized 3% hypertonic saline solution treatment in hospitalized infants with viral bronchiolitis. Chest. 2003;123:481–487. doi: 10.1378/chest.123.2.481. [DOI] [PubMed] [Google Scholar]
- 82.Kuzik BA, Al-Qadhi SA, Kent S. Nebulized hypertonic saline in the treatment of viral bronchiolitis in infants. J Pediatr. 2007;151:266–270. doi: 10.1016/j.jpeds.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 83.Luo Z, Liu E, Luo J. Nebulized hypertonic saline/salbutamol solution treatment in hospitalized children with mild to moderate bronchiolitis. Pediatr Int. 2010;52:199–202. doi: 10.1111/j.1442-200X.2009.02941.x. [DOI] [PubMed] [Google Scholar]
- 84.Wu S, Baker C, Lang ME. Nebulized hypertonic saline for bronchiolitis: a randomized clinical trial. JAMA Pediatr. 2014;168:657–663. doi: 10.1001/jamapediatrics.2014.301. [DOI] [PubMed] [Google Scholar]
- 85.Florin TA, Shaw KN, Kittick M, Yakscoe S, Zorc JJ. Nebulized hypertonic saline for bronchiolitis in the emergency department: a randomized clinical trial. JAMA Pediatr. 2014;168:664–670. doi: 10.1001/jamapediatrics.2013.5306. [DOI] [PubMed] [Google Scholar]
- 86.Grewal S, Klassen TP. The tale of 2 trials: disentangling contradictory evidence on hypertonic saline for acute bronchiolitis. JAMA Pediatr. 2014;168:607–609. doi: 10.1001/jamapediatrics.2014.423. [DOI] [PubMed] [Google Scholar]
- 87.Silver AH, Esteban-Cruciani N, Azzarone G. 3% hypertonic saline versus normal saline in inpatient bronchiolitis: a randomized controlled trial. Pediatrics. 2015;136:1036–1043. doi: 10.1542/peds.2015-1037. [DOI] [PubMed] [Google Scholar]
- 88.Flores P, Mendes AL, Neto AS. A randomized trial of nebulized 3% hypertonic saline with salbutamol in the treatment of acute bronchiolitis in hospitalized infants. Pediatr Pulmonol. 2016;51:418–425. doi: 10.1002/ppul.23306. [DOI] [PubMed] [Google Scholar]
- 89.Everard ML, Hind D, Ugonna K. SABRE: a multicentre randomised control trial of nebulised hypertonic saline in infants hospitalised with acute bronchiolitis. Thorax. 2014;69:1105–1112. doi: 10.1136/thoraxjnl-2014-205953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Teunissen J, Hochs AH, Vaessen-Verberne A. The effect of 3% and 6% hypertonic saline in viral bronchiolitis: a randomised controlled trial. Eur Respir J. 2014;44:913–921. doi: 10.1183/09031936.00159613. [DOI] [PubMed] [Google Scholar]
- 91.Zhang L, Mendoza-Sassi RA, Klassen TP, Wainwright C. Nebulized hypertonic saline for acute bronchiolitis: a systematic review. Pediatrics. 2015;136:687–701. doi: 10.1542/peds.2015-1914. [DOI] [PubMed] [Google Scholar]
- 92.Maguire C, Cantrill H, Hind D, Bradburn M, Everard ML. Hypertonic saline (HS) for acute bronchiolitis: systematic review and meta-analysis. BMC Pulm Med. 2015;15:148. doi: 10.1186/s12890-015-0140-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Brooks CG, Harrison WN, Ralston SL. Association between hypertonic saline and hospital length of stay in acute viral bronchiolitis: a reanalysis of 2 meta-analyses. JAMA Pediatr. 2016;170:577–584. doi: 10.1001/jamapediatrics.2016.0079. [DOI] [PubMed] [Google Scholar]
- 94.Corneli HM, Zorc JJ, Mahajan P. A multicenter, randomized, controlled trial of dexamethasone for bronchiolitis. N Engl J Med. 2007;357:331–339. doi: 10.1056/NEJMoa071255. [DOI] [PubMed] [Google Scholar]
- 95.Plint AC, Johnson DW, Patel H. Epinephrine and dexamethasone in children with bronchiolitis. N Engl J Med. 2009;360:2079–2089. doi: 10.1056/NEJMoa0900544. [DOI] [PubMed] [Google Scholar]
- 96.Fernandes RM, Bialy LM, Vandermeer B. Glucocorticoids for acute viral bronchiolitis in infants and young children. Cochrane Database Syst Rev. 2013;6 doi: 10.1002/14651858.CD004878.pub4. CD004878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sinha IP, McBride AK, Smith R, Fernandes RM. CPAP and high-flow nasal cannula oxygen in bronchiolitis. Chest. 2015;148:810–823. doi: 10.1378/chest.14-1589. [DOI] [PubMed] [Google Scholar]
- 98.Bueno Campana M, Olivares Ortiz J, Notario Munoz C. High flow therapy versus hypertonic saline in bronchiolitis: randomised controlled trial. Arch Dis Child. 2014;99:511–515. doi: 10.1136/archdischild-2013-305443. [DOI] [PubMed] [Google Scholar]
- 99.Farley R, Spurling GK, Eriksson L, Del Mar CB. Antibiotics for bronchiolitis in children under two years of age. Cochrane Database Syst Rev. 2014;10 doi: 10.1002/14651858.CD005189.pub4. CD005189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Andrade MA, Hoberman A, Glustein J, Paradise JL, Wald ER. Acute otitis media in children with bronchiolitis. Pediatrics. 1998;101:617–619. doi: 10.1542/peds.101.4.617. [DOI] [PubMed] [Google Scholar]
- 101.Shazberg G, Revel-Vilk S, Shoseyov D, Ben-Ami A, Klar A, Hurvitz H. The clinical course of bronchiolitis associated with acute otitis media. Arch Dis Child. 2000;83:317–319. doi: 10.1136/adc.83.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lieberthal AS, Carroll AE, Chonmaitree T. The diagnosis and management of acute otitis media. Pediatrics. 2013;131:e964–e999. doi: 10.1542/peds.2012-3488. [DOI] [PubMed] [Google Scholar]
- 103.McCallum GB, Morris PS, Chatfield MD. A single dose of azithromycin does not improve clinical outcomes of children hospitalised with bronchiolitis: a randomised, placebo-controlled trial. PLoS One. 2013;8:e74316. doi: 10.1371/journal.pone.0074316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pinto LA, Pitrez PM, Luisi F. Azithromycin therapy in hospitalized infants with acute bronchiolitis is not associated with better clinical outcomes: a randomized, double-blinded, and placebo-controlled clinical trial. J Pediatr. 2012;161:1104–1108. doi: 10.1016/j.jpeds.2012.05.053. [DOI] [PubMed] [Google Scholar]
- 105.Beigelman A, Isaacson-Schmid M, Sajol G. Randomized trial to evaluate azithromycin's effects on serum and upper airway IL-8 levels and recurrent wheezing in infants with respiratory syncytial virus bronchiolitis. J Allergy Clin Immunol. 2015;135:1171–1178. doi: 10.1016/j.jaci.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bacharier LB, Guilbert TW, Mauger DT. Early administration of azithromycin and prevention of severe lower respiratory tract illnesses in preschool children with a history of such illnesses: a randomized clinical trial. JAMA. 2015;314:2034–2044. doi: 10.1001/jama.2015.13896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Oakley E, Borland M, Neutze J, for the Paediatric Research in Emergency Departments International Collaborative (PREDICT) Nasogastric hydration versus intravenous hydration for infants with bronchiolitis: a randomised trial. Lancet Respir Med. 2013;1:113–120. doi: 10.1016/S2213-2600(12)70053-X. [DOI] [PubMed] [Google Scholar]
- 108.Mussman GM, Parker MW, Statile A, Sucharew H, Brady PW. Suctioning and length of stay in infants hospitalized with bronchiolitis. JAMA Pediatr. 2013;167:414–421. doi: 10.1001/jamapediatrics.2013.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Moschino L, Mario F, Carraro S, Visentin F, Zanconato S, Baraldi E. Is nasal suctioning warranted before measuring O2 saturation in infants with bronchiolitis? Arch Dis Child. 2016;101:114–115. doi: 10.1136/archdischild-2015-309587. [DOI] [PubMed] [Google Scholar]
- 110.Schreiber S, Ronfani L, Ghirardo S. Nasal irrigation with saline solution significantly improves oxygen saturation in infants with bronchiolitis. Acta Paediatr. 2016;105:292–296. doi: 10.1111/apa.13282. [DOI] [PubMed] [Google Scholar]
- 111.Ralston S, Garber M, Narang S. Decreasing unnecessary utilization in acute bronchiolitis care: results from the value in inpatient pediatrics network. J Hosp Med. 2013;8:25–30. doi: 10.1002/jhm.1982. [DOI] [PubMed] [Google Scholar]
- 112.Gajdos V, Katsahian S, Beydon N. Effectiveness of chest physiotherapy in infants hospitalized with acute bronchiolitis: a multicenter, randomized, controlled trial. PLoS Med. 2010;7:e1000345. doi: 10.1371/journal.pmed.1000345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Roqué i Figuls M, Giné-Garriga M, Granados Rugeles C, Perrotta C, Vilaró J. Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database Syst Rev. 2016;2 doi: 10.1002/14651858.CD004873.pub5. CD004873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Carlsen KH, Larsen S, Bjerve O, Leegaard J. Acute bronchiolitis: predisposing factors and characterization of infants at risk. Pediatr Pulmonol. 1987;3:153–160. doi: 10.1002/ppul.1950030308. [DOI] [PubMed] [Google Scholar]
- 115.Sigurs N, Aljassim F, Kjellman B. Asthma and allergy patterns over 18 years after severe RSV bronchiolitis in the first year of life. Thorax. 2010;65:1045–1052. doi: 10.1136/thx.2009.121582. [DOI] [PubMed] [Google Scholar]
- 116.Stein RT, Sherrill D, Morgan WJ. Respiratory syncytial virus in early life and risk of wheeze and allergy by age 13 years. Lancet. 1999;354:541–545. doi: 10.1016/S0140-6736(98)10321-5. [DOI] [PubMed] [Google Scholar]
- 117.Fjaerli HO, Farstad T, Rod G, Ufert GK, Gulbrandsen P, Nakstad B. Acute bronchiolitis in infancy as risk factor for wheezing and reduced pulmonary function by seven years in Akershus County, Norway. BMC Pediatr. 2005;5:31. doi: 10.1186/1471-2431-5-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Jeng MJ, Lee YS, Tsao PC, Yang CF, Soong WJ. A longitudinal study on early hospitalized airway infections and subsequent childhood asthma. PLoS One. 2014;10:e0121906. doi: 10.1371/journal.pone.0121906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Carroll KN, Wu P, Gebretsadik T. The severity-dependent relationship of infant bronchiolitis on the risk and morbidity of early childhood asthma. J Allergy Clin Immunol. 2009;123:1055. doi: 10.1016/j.jaci.2009.02.021. 61.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Everard ML, Hind D, Ugonna K. Saline in acute bronchiolitis RCT and economic evaluation: hypertonic saline in acute bronchiolitis—randomised controlled trial and systematic review. Health Technol Assess. 2015;19:1–130. doi: 10.3310/hta19660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Greening AP, Ind PW, Northfield M, Shaw G. Added salmeterol versus higher-dose corticosteroid in asthma patients with symptoms on existing inhaled corticosteroid. Allen & Hanburys Limited UK Study Group. Lancet. 1994;344:219–224. doi: 10.1016/s0140-6736(94)92996-3. [DOI] [PubMed] [Google Scholar]
- 122.Pauwels RA, Lofdahl CG, Postma DS. Effect of inhaled formoterol and budesonide on exacerbations of asthma. Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. N Engl J Med. 1997;337:1405–1411. doi: 10.1056/NEJM199711133372001. [DOI] [PubMed] [Google Scholar]
- 123.Barnes PJ. Scientific rationale for using a single inhaler for asthma control. Eur Respir J. 2007;29:587–595. doi: 10.1183/09031936.00080306. [DOI] [PubMed] [Google Scholar]
- 124.Giembycz MA, Kaur M, Leigh R, Newton R. A holy grail of asthma management: toward understanding how long-acting beta(2)-adrenoceptor agonists enhance the clinical efficacy of inhaled corticosteroids. Br J Pharmacol. 2008;153:1090–1104. doi: 10.1038/sj.bjp.0707627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kaur M, Chivers JE, Giembycz MA, Newton R. Long-acting beta 2-adrenoceptor agonists synergistically enhance glucocorticoid-dependent transcription in human airway epithelial and smooth muscle cells. Mol Pharmacol. 2008;73:203–214. doi: 10.1124/mol.107.040121. [DOI] [PubMed] [Google Scholar]
- 126.Holden NS, Bell MJ, Rider CF. Beta 2-adrenoceptor agonist-induced RGS2 expression is a genomic mechanism of bronchoprotection that is enhanced by glucocorticoids. Proc Natl Acad Sci USA. 2011;108:19713–19718. doi: 10.1073/pnas.1110226108. [DOI] [PMC free article] [PubMed] [Google Scholar]