Abstract
In this article, we demonstrate the method of participatory causal modeling to map the interdependencies of critical performance variables in a complex nonprofit health care provider with considerable financial and operational control challenges. Critical performance variables are output performance dimensions that are fundamental indicators of organizational success. Causal modeling provides an approach for nonprofit leaders to examine how critical performance variables dynamically and recursively affect each other and thereby offers a path to identify key points of leverage for organizational action. Using a case study, we show that participatory system dynamics modeling revealed assumptions, choices, and complexities and so helped a nonprofit health care organization recognize possible strategic opportunities. This study demonstrates an approach that other nonprofits may deploy in situations where they are experiencing competing objectives and constraints in managing critical performance variables.
Keywords: accounting in community health centers, critical performance variables, nonprofit performance measurement, system dynamics
Introduction
Leaders of nonprofits are frequently faced with multiple, complex, often-competing objectives. In particular, nonprofits aim to balance revenue-generating activities with fulfillment of service-delivery activities for beneficiaries. Other complexities include how best to deliver social value, manage stakeholder groups, govern itself, and measure performance, as well as how best to recruit and retain talent (Austin, Stevenson, & Wei-Skillern, 2006; Bagnoli & Megali, 2011; Carnochan, Samples, Myers, & Austin, 2014; Froelich, 1999; Gamble & Beer, 2015; Nicholls, 2009). These struggles are evident when nonprofit leaders attempt to select, measure, and manage their critical performance variables (CPVs). The act of expressing how their CPVs work together to achieve organizational goals can become frustrating if it is even undertaken.
The existing literature on CPVs spans many different domains, for example, management control systems (Hofstede, 1981; Kaplan, 2001; Kaplan & Norton, 2005; Simons, 1995a, 1995b), performance measurement (Bagnoli & Megali, 2011), and performance management (Otley, 1999). All embrace notions of critical variables that should be measured and managed. The importance of CPVs stems from their role in aligning organizational decision making (Malina & Selto, 2001; Shields, 2015), fostering innovative practices (Bisbe & Otley, 2004; Jørgensen & Messner, 2009; Widener, 2007), as well as providing a foundation for formal and informal reporting (Herremans & Nazari, 2016). As pressures mount for nonprofits to demonstrate accountability and effectiveness, CPVs can play an increasingly important role in organizational management.
Yet research remains equivocal regarding ways that nonprofit CPVs interact with each other to inform strategic choices. Interactions among nonprofit performance variables may be assumed, rather than explicitly analyzed, and interactions may be multilayered and recursive rather than linear and unidirectional. These complexities have direct and indirect consequences in theory and practice (Froelich, 1999). For example, nonprofit health care providers face tensions between revenue generation and mission effectiveness when considering their ideal patient mix. Compounding these considerable financial and operational tensions, managers feel constrained when facing pressures to increase salaries of doctors, dentists, and staff to recruit and retain high-quality personnel.
The motivation for this study stems from persistent pressures at a U.S. nonprofit federally qualified health center called Community Health Partners (CHP).1 It faces considerable financial and operational constraints, including relatively rural labor markets, shaped by the state’s low per-capita income and federal legislation governing health centers chartered to receive cost-based Medicaid and Medicare reimbursements. Together, these limit the degrees of freedom with which CHP leaders undertake decisions. At the outset of the research, executives at CHP were focused on a single leverage point of control—increasing salaries—to improve retention and recruitment of qualified staff, which they regarded as a CPV. While they believed salary increases were essential, they also felt that they were unachievable due to the nature of their revenues and organizational form.
Given that, like CHP, many nonprofits do not have a systematic process for managing multiple, complex, often-competing objectives, the purpose of this study was to explore how the CPVs chosen by nonprofit leaders may work together to clarify strategic challenges and opportunities. We used participatory system dynamics (Hovmand, 2014) as a method for understanding tensions in a complex nonprofit health care organization. We found that constructing a whole-system representation of CPVs expanded CHP leaders’ strategic opportunities (Simons, 1995b). When organizational leaders agreed on how CPVs influenced each other, some blind spots obscuring the larger organizational picture were removed. By describing how this approach expanded the set of strategic choices for these nonprofit leaders, we offer a useful and replicable method for identifying CPV interdependencies in other nonprofits.
Literature Informing the Study
CPVs are output variables representing varying performance elements (Simons, 1995b). Scholars also refer to CPVs using terms such as “critical success factors” (e.g., Tuomela, 2005), “key indicators” (e.g., Bagnoli & Megali, 2011), and “key performance indicators” (Inamdar, Kaplan, & Reynolds, 2002). In sum, managers monitor CPVs to inform strategic choice and action (Kaplan & Norton, 1996, 2005; Simons, 1995b). Prior work on CPVs has been used in different organizational forms including nonprofits (Chenhall, Hall, & Smith, 2013, 2017; LeRoux & Wright, 2010) and for-profits (Simons, 1995a, 1995b). Furthermore, CPVs have been used in different theoretical contexts such as performance measurement (Tuomela, 2005), performance management (A. Ferreira & Otley, 2009), and as a starting point for new control frameworks (Tessier & Otley, 2012).
Yet several scholars have pointed out deficiencies with respect to nonprofit CPVs, due to the multidimensional and the socially constructed nature of nonprofit performance measurement (Hofstede, 1981; Packard, 2010). Speckbacher (2003) echoes this sentiment by asserting that cause-and-effect chains are typically multidirectional in nonprofits, rather than unidirectional as is assumed by CPV frameworks such as the Balanced Scorecard. These scholars proffer the Balanced Scorecard framework as a communication tool, but note that nonprofit control systems need to take into account both intrinsic and extrinsic motivations if they are to manage performance. Relatedly, Froelich (1999) describes complexities distinct to nonprofits, such as the constraints attached to government funding that can cause direct consequences, such as funding new services, and indirect consequences, such as goal and mission dilution, in the organization. Research also suggests that measurement models used by nonprofits miss important outcomes because “our understanding of what drives performance is incomplete” (Benjamin & Campbell, 2014, p. 988).
In light of this apparent gap in scholarship with respect to cause-and-effect relationships among nonprofit CPVs, and the subsequent difficulty nonprofit leaders may experience in understanding and communicating relationships among CPVs, we seek to develop a way to infer causal relationships. Once these relationships are made explicit, leaders can more easily have productive dialogues. Given multiple internal and external constituents at nonprofits, this is both a methodological and a practical matter. Without explicit causal chains, nonprofit managers may misuse CPVs for decision-making purposes. To date, the literature is silent on methods to ensure that CPVs work in concert to advance a nonprofit’s mission.
Therefore, this article addresses the gap in the literature by demonstrating a modeling method for nonprofit CPVs using system dynamics participatory modeling to examine CPV interdependencies. System dynamics (SD) is a method for representing complex systems and feedback dynamics in tractable ways (Sterman, 2000). Engaging multiple stakeholders in conceptualizing and modeling a shared complex problem has been a growing practice in system dynamics for nearly 40 years (Vennix, 1996, 1999).
SD is used to deal with cases where the overriding nature of the problem is “wicked” (Rittel & Webber, 1973). Wicked problems are characterized by intertwining social and technical aspects, so that interlocking constraints on resources, goals, and outcomes obscure clear entry points for engaging and addressing them (Ackoff, 1979; Black, 2013; Rittel & Webber, 1973). In situations like these, discerning activities to resolve “the problem,” which may not be consensually identified or named (Rittel & Webber, 1973; Vennix, 1999), is not intuitively obvious. Using participatory SD methods has the benefit of challenging assumptions, developing agreement on complex problems and, more importantly, identifying unexpected points of leverage to influence CPVs.
Method
Case Study of CHP
A clinical inquiry case study was the approach selected for investigating how nonprofit CPVs interact with each other to inform strategic choices. Clinical inquiry (Schein, 2007) privileges organizational leaders’ needs over academicians’ needs as the foundation for a research endeavor. It is based on the premise that client-driven inquiry reveals deeper and more valid information relevant to the research, which in turn strengthens research findings. Case study research is critical to the development of theory, while informing practice, because it examines dynamic phenomena and context-rich events (Bagnoli & Megali, 2011; Cooper & Morgan, 2008; Eisenhardt, 1989; Flyvbjerg, 2006). Case studies are a commonly used approach to investigate accounting controls, which include CPVs (Burns & Scapens, 2000; Charnes & Cooper, 1980; L. D. Ferreira & Merchant, 1992; Langfield-Smith, 1997; Simons, 1995b).
CHP was selected because it is a complex nonprofit facing considerable financial and operational challenges. CHP operates in southwestern Montana, chartered as a federally qualified health center, delivering health care to patients with limited access to alternatives. CHP’s leaders perceived themselves to be constrained in acting to influence isolated CPVs. Participatory modeling placed multiple CPVs in a broader system of variables and helped leaders become “unstuck,” freed from silo-thinking. Following three preliminary interviews of CHP’s CEO and dental director, we undertook a participatory modeling approach with key CHP personnel. We examined how CPVs were affected by interactions among organizational activities and subsequently constructed social agreements among multiple stakeholders in an effort to understand the complexities and uncertainties of management decision making.
The Process of Mapping CPVs
We used a participatory system dynamics causal-mapping method (Black & Andersen, 2012; Hovmand, 2014; Richardson & Andersen, 1995; Vennix, 1996) to engage CHP executives and staff in identifying CPVs that characterize the system of revenue generation and mission-related operational pressures experienced by employees at CHP. SD is a method by which researchers and participants recognize important patterns and the feedback structures driving them—or the “physics” of the current operating system (Sterman, 2000; Wolstenholme, 1994) to explore points of leverage for changing the system to achieve desired outcomes in sustainable ways with minimal unintended consequences. The goal of using participatory SD was to elicit a more systemic understanding of the CPVs from multiple perspectives in a structured group setting, including surfacing shared inferences and (dis-)agreements on CPVs and their relationships to one another.
Over multiple meetings (exceeding 50 hr) our research team interacted with CHP leaders, who included the CEO, dental director, a clinic director, the medical director, the administrative coordinator, the human resource director, a nurse, and a nurse practitioner. These leaders participated in each workshop session, and two researchers observed and took notes on leaders’ assertions and interactions (Geertz, 1973) while one or two researchers facilitated the conversation and created a shared visual representation of the variables described and the relationships among them (Black, 2013). The observer-researchers then met with the facilitator-researchers to debrief the sessions, review the observations, and document in sharable form the emerging causal map of variables (using Vensim software).
Prior to the SD workshops, we asked (via an anonymous survey) all CHP staff and executives to describe the variables that were perceived points of leverage (30% response rate). During the workshops the participants identified above transcribed onto cards the 80-plus variables generated by the survey. Then they placed the cards on the wall and silently sorted them into clusters based on similar themes, constructing an affinity diagram (Brassard, 1989). The facilitator coached them on naming each clustered theme with a header-card, which resulted in initial variables, including increasing wages, increasing resources, expanding recruitment, addressing workload, providing incentives, addressing training, increasing recognition, and improving work efficiency.
Then participants identified causal relationships among the variables. The facilitator elicited participants’ hypotheses about, for example, the role of scheduling efficiency on staff’s experienced workload. As conversation continued, participants freely expressed their operational understanding of relationships among the variables as well as named new operational variables (such as percent of patients whose services are reimbursed by private insurance or Medicaid/Medicare). Workshop participants instructed the facilitator on where to place variables in the diagram and how to draw and designate the causal relations among them.
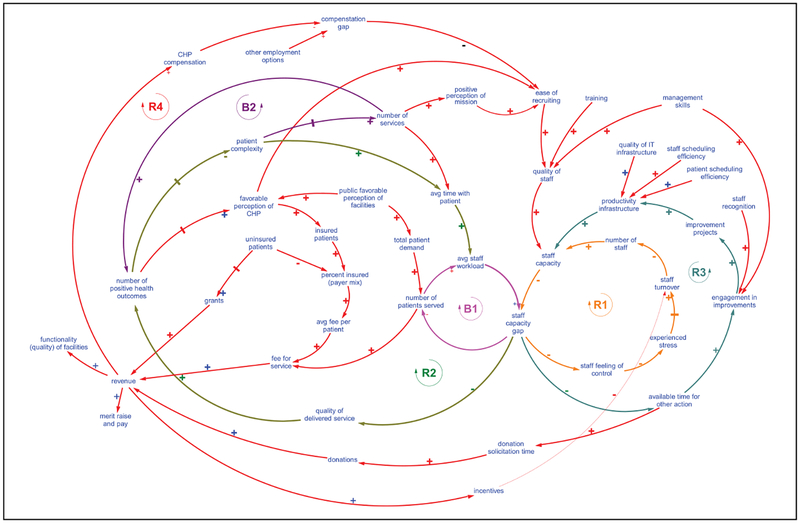
Finally, participants worked with the facilitator to further refine causal relations among the variables. Consequently, several more operational variables, such as staff capacity gap (the difference between workload demand and staff capacity), were added to complete a causal diagram (Figure 1) that included several closed feedback loops (summarized in the “Findings” section). The SD causal modeling workshops yielded an agreed-upon causal diagram showing relationships among variables salient to recruiting and retaining employees—but also relevant to managing and improving the clinic’s operations and monitoring and measuring patient and organizational outcomes.
Figure 1.
The final closed-looped causal diagram of critical variables at CHP.
Note. Identifying causal relations among the variables produced by the affinity diagram. As above, a + sign indicates positive polarity (i.e., positive partial derivative) of a causal relationship (a change in the cause variable creates a change in the same direction in the effect variable), all else being equal, and a − sign indicates a negative polarity (i.e., negative partial derivative) of the causal relationship (a change in the cause variable creates a change in the opposite direction in the effect variable), ceteris paribus. CHP = Community Health Partners.
Findings
Our findings emerged through the participatory causal mapping sessions, archival research, the preliminary interviews, and noted observations of CHP leaders’ conversations and interactions. We briefly present a summary of CHP’s underlying organizational tensions and CPVs based on our analyses of data from archives and interviews. We then describe in more detail the causal diagram constructed during the participatory modeling sessions, focusing our analysis on relationships among CPVs.
Organizational Tensions
The stated mission of CHP is to “enhance community health and well-being,” and the CHP vision statement is “100% Access, 0 Disparity for All” (CHP, 2016). The core values of the 120-person team at CHP are implicitly demonstrated by high commitment to patients’ well-being. On a daily basis, CHP staff members take extra steps to facilitate patients’ connections with appropriate providers of pharmaceutical, legal, and social services in a region with limited public transportation. However, this often leads to accumulating feelings of fatigue and frustration with the complexity of programs that the poorest, and often sickest, patients must navigate. For example, a majority of CHP patients lack the wherewithal and social support to manage complicated drug regimens or to apply for social-service aids, including transportation assistance and financial reimbursements.
Early dialogue with the CEO and dental director suggested that a prevailing tension was the difficulty in recruiting and retaining highly qualified, mission-driven employees. Like many community health centers in the United States, CHP was frequently on the edge of financial viability. Several financial CPVs at CHP are summarized as follows. Recent revenue figures (grants, subsidies, fee-for-service) were US$6.75 million (2013), US$7.68 million (2014), and US$7.68 million (2015). The biggest expense on the income statements of CHP is salaries, representing approximately 79% of revenue. In addition, annual employee turnover (the inverse of successful retention) at CHP is approximately 30%, a figure above average for health centers of similar size in the region. CHP’s leaders held little optimism for reducing this trend. This challenge is analogous to a nationwide problem at many community health centers in the United States (Glasser, Peters, & MacDowell, 2006; Rosenblatt, Andrilla, Curtin, & Hart, 2006). Accentuating the problem at CHP, however, is the market differential for medical professionals—the difference between salaries for positions at community health centers in neighboring states and those at CHP—which is as much as 30% annually. The typical private practice salary for comparable professionals is 2 to 3 times higher than salaries at CHP.
Customer CPVs at CHP include the number of patients served annually and the total number of patient visits. The approximate number of yearly patients and patient visits are 12,300 and 45,000, respectively. Unfortunately demand often outpaces capacity, creating the undesired consequence of turning patients away. During the SD workshops, several executives commented with frustration that they are “turning patients away on a daily basis.” For example, the dental director stated that a week’s worth of 80 dental appointments are consistently booked within the first 2 hr on Monday mornings.
Mapping Relationships Among CPVs
Figure 1 shows the representation of interrelated CPVs, along with some other operational variables, constructed using participatory causal mapping with CHP executives and staff. Figure 1 contains many of the CPVs in terms of the overall system at CHP (i.e., payer mix, number of services offered, patient complexity) as well as several of the soft variables that were described as critical to the feedback loops in which CPVs were embedded (i.e., staff feeling of control, experienced stress, positive perception of mission). Figure 1 portrays participants’ understanding at the end of the SD workshop sessions of how variables are dynamically and systemically intertwined.
Figure 1 includes four reinforcing, or amplifying, feedback loops, which can work in either virtuous or vicious directions for the organization; a change in any variable in a reinforcing loop (indicated by an R in Figure 1) is amplified through its interaction with other variables. The diagram also includes two balancing feedback loops (indicated by a B in the diagram). In these feedback loops a change in any variable in the loop is “balanced,” or negated, through its interaction with other variables. Each of these feedback loops is briefly described below. The hash marks between variables in Figure 1 indicate lag effects.
R1: The staff capacity gap is the difference between staff capacity and the average staff workload; the gap increases when staff capacity falls below workload demands. As the gap increases, the staff feeling of control decreases, which in turn increases the level of experienced stress. Higher stress can increase staff turnover, reducing the number of staff, decreasing staff capacity, and reinforcing the staff capacity gap. Conversely, a decrease in the staff capacity gap can, through these relationships, further reinforce staff capacity.
R2: An increase in the staff capacity gap can decrease the quality of delivered service that patients experience, in turn decreasing the number of positive health outcomes. Decreasing positive health outcomes for patients, over time, increases patient complexity, as many CHP clients suffer from multiple chronic and interrelated health problems. Increased patient complexity requires that health care providers spend more time with each patient, thereby increasing average time with patient, which increases the overall average staff workload, which in turn further increases the staff capacity gap. Conversely, a decrease in staff capacity gap will, through these same relationships, create more positive health outcomes for patients, over time mitigating chronic health problems and reducing patient complexity, and further reducing the staff capacity gap, all else being equal.
R3: As the staff capacity gap decreases, staff members’ available time for other actions to benefit the organization increases, including increasing staff engagement in improvements, which increases the number of improvement projects completed. This in turn increases the robustness of productivity infrastructure at the clinics, thereby effectively increasing staff capacity and further reducing the staff capacity gap. Conversely, this same feedback loop can work in a vicious way, undermining staff capacity to engage in improvement efforts that could increase their effective capacity.
R4: Similarly, an increase in staff members’ available time for other actions to benefit the organization can increase donation solicitation time, which can lead to increased donations. More donations increase revenues for CHP, enabling higher CHP compensation for staff members and decreasing the compensation gap that CHP staff feel, relative to other employment options. Closing the compensation gap can increase the ease of recruiting and thereby increase the quality of staff that CHP can hire. Higher quality staff effectively increases staff capacity, reducing the staff capacity gap and increasing staff members’ available time for other actions to benefit CHP. Conversely, this feedback loop can work in a negatively amplifying direction as well.
B1: As the staff capacity gap increases, the number of patients served decreases, and so reduces the average staff workload, as CHP turns away patients needing care, thereby reducing the staff capacity gap, all else being equal.
B2: As CHP increases the number of services it offers, the number of positive health outcomes for patients increases. This in turn, over time, can decrease patient complexity, as patients’ chronic and interrelated health problems are mitigated. This would thereby reduce patients’ need for a large number of services.
While other feedback loops and combinations of loops can be identified, these were the feedback loops participants focused on most by the end of the SD workshops. After the sessions, the executive team at CHP and the research team had a more robust understanding of the causal relationships among critical variables and the strategic opportunities at CHP. Several variables dominating the conversations that emerged from the SD sessions included the following: patient complexity/mix, workload, and salary, all of which contributed to the recruitment and retention of highly qualified mission-driven employees. They also identified variables not previously considered part of the recruiting-and-retention challenge, such as the role that operational productivity improvements play in effective staff capacity, the importance of favorable public perceptions of the organization’s facilities, and the potential value in communicating more broadly and systematically patient success stories.
Relationships Among CPVs Suggest Expanding Strategic Opportunities
The process of expanding strategic opportunities involves stimulating seeking and learning, improving decision making, and generating momentum and commitment (Simons, 1995b). We offer evidence that the process of applying a participatory SD approach facilitated the expansion of strategic opportunities by revealing connections between consequences and causes separated by space and time; revealing potential conflicts among current CPVs related to funding, services provided, and the number and nature of patients served; and making explicit elements of operations and assumptions that were previously taken for granted, and therefore unexamined.
Connecting consequences and causes.
The visual representation portrayed a series of causal links from CHP’s focus on underinsured patients through patients’ complex health conditions resulting from chronic, undiagnosed, and untreated illness, to increased workload and subsequently staff burnout—which, combined with low compensation, could contribute significantly to turnover (the center of the diagram in Figure 1). “It is so nice to see the breakdown [of the variables and how they relate to each other].” The medical director commented, “So this is more complicated than we thought [followed by all participants laughing].” At the end of the sessions, a participant thanked one of the researchers: “I liked that … seeing the cascading effect [of variables and causal relationships].” “When you see them [the variables] up there [on the white-board], you start to see how interrelated they are.” The process of creating the diagram also revealed conflicting beliefs about the effect on staff recruitment and retention from “patient complexity” (patients experiencing multiple complications from undertreated chronic disease); while leaders agreed that patient complexity could contribute to staff fatigue and staff turnover, some participants asserted the same patient complexity made work interesting and challenging for staff members. One CHP leader, during a SD session, commented, “I was surprised on the recruitment comment … that challenging patients [were part of the recruiting problem].” Recognizing that the CPV of successful staff retention and recruiting may be adversely affected by the mission focus on under-insured patients created opportunity, in light of the workshop conversations, for CHP leaders to consider changes to recruiting processes to ensure staff are not only mission-committed but also people who relish challenges of addressing complex health conditions. They also discussed possibilities for balancing patient workload, scheduling, and staff empowerment resources to reduce burnout.
Potential conflict among CPVs.
Constructing the causal model generated conversations related to introducing new services, often tied to specific grants. While grants obtained and the number of services offered are CPVs that leaders hope to increase, in reflecting on the causal diagram, they also wondered if expanding the number of services could dilute focus on core medical services for the targeted clientele. “We are good at adding services to the budget but we are not really good at saying no,” “I am actually concerned that we cannot say no [to adding services],” “Should we spend our dollars on the core of what we do, or should we spread them out on other things?” and “This is about making choices. We can slow down.” The notion of deliberately limiting CHP’s number of services had not been recognized as a possibility, one that relates to its strategy and mission.
Making implicit variables explicit.
The representation also showed causal relations depicting that serving more patients with adequate insurance could increase revenue, decreasing CHP’s dependence on grants and possibly leading to increased compensation for health care providers (the lower left of the causal diagram). We heard conversations in which executives and staff acknowledged limitations of the existing CHP boundary. “This [our current business model] is not a sustainable business model. We try to solve everything but not get paid for it,” “Our current model is hopeless when we look at the causal loops,” “We will always have less than we want [referencing revenue availability].” Another said, “Increasing pay [for example] may put pressure on these other things.”
Despite their focus on the shared visual representation, participants’ conversations consistently omitted references to revenues from insured patients, and they referred to fund-raising as an unending organizational priority. The researchers observed that, even though variables named insured patients and percent insured (payer mix) appeared in the causal diagram, CHP leaders nevertheless perceived a boundary: The organization would serve primarily or solely patients whose resources (insurance and otherwise) could not cover the cost of care. The conversations also affirmed the belief that the patient population would always remain larger than CHP could address. A logical inference is that the organization’s vision for 100% access and 0 disparity would remain unachievable.
Discussion
This case study has potential to speak to a broader audience because it demonstrates a method for articulating explicitly how strategic and operational variables affect each other and for revealing ways to move CPVs in desirable directions. Specifically, this approach holistically explores interconnectedness of CPVs in nonprofits, and we describe its application at a community health center. A causal modeling method shows how CPVs can dynamically and recursively affect each other, and facilitated participatory modeling aids in constructing social agreements about opportunities to improve performance. This study contributes to scholarship about CPVs as well as informs possibilities for practice.
Implications for Scholarship
Literature on CPVs is long-standing. CPVs are frequently used to measure and manage elements of organizations and are intended to inform strategic decisions and tradeoffs (Bagnoli & Megali, 2011; Simons, 1995b). Chenhall (2003) and Malmi and Brown (2008) suggest that such controls should be viewed in a comprehensive and integrated way. However, relationships among CPVs are often underspecified. This article offers one approach, namely participatory SD, for specifying them. The method allows for explicit specifications of causal relationships among activities affecting CPVs.
Before this study, the CPVs used by the CHP team did not provide a comprehensive or integrated description of the overall system. Placing CPVs in relationship to each other and to operational variables helped leaders see unexpected influences among variables (e.g., introducing new services could possibly dilute core services for targeted clientele). The process also revealed that certain operational variables could play more strategic roles than previously imagined (e.g., operational improvements in scheduling efficiency could reduce personnel burnout and subsequent turnover; increased publicity about the clinic’s work could help employees take pride in what they do).
The SD method can reveal feedback loops and recursive interdependencies about these activities that can identify powerful points of leverage for moving CPVs in desirable directions. An especially valuable aspect of this method relates to its depiction of reinforcing and balancing feedback dynamics, whose virtuous or vicious effects can be influenced by leaders’ decisions. Recognizing that CPVs may interact with each other—not just directly but through multiple intermediate variables over time—provides specific steps to understand the complexity of organizational actions and their consequences. We contrast the reinforcing and balancing loops revealed by this approach, which places CPVs in the causal context of multiple organizational activities, with characterizations of strategic performance controls as positive or enabling and operational performance controls as negative or constraining (Tessier & Otley, 2012). Each feedback loop’s dynamics may work to the advantage or harm of the organization, so feedback loops connecting multiple variables reveal increased options for influencing strategic activities and their measurements. Examining CPVs in a causal map of the organization’s understanding of “how it works” can lead to different conclusions about which activities and resultant CPVs are enabling and which constraining organizational goals. The use of this method is relevant to a broad audience of nonprofits in that it facilitates opportunities to increase explanatory power of CPVs and their role in nonprofit performance.
In our case study, the modeling sessions challenged participants from this nonprofit clinic to examine the dynamic nature of their system through CPVs seen in relation to each other. Given the CPVs that were described as prevailing tensions in the SD workshops—balancing mission-related service delivery and successful recruiting and retention, both of which are influenced (in different ways) by workload, salaries, and overtime—one can appreciate how executive and staff frustration may manifest in a mind-set of “helplessness” (Noonan, 2007). Helplessness is a defensive routine (Argyris, 1990; Noonan, 2007) in which people reason they cannot take action because there is no feasible way to address the problem; yet “helplessness enshrines the defensive routine [of inaction] in a place of permanence” (Noonan, 2007, p. 99). The “stuck” feeling expressed by leaders of CHP may have resulted in part from overfocus on salaries as the only point of leverage affecting the recruiting and retention CPV and in part from defensive reasoning. Defensive reasoning relies on keeping causal reasoning and inferences tacit (Argyris, 1993). Therefore, a method (such as the one used here) that elicits causal relations among CPVs in a facilitated participatory setting can shift an organizational team to productive reasoning, which is characterized by making data and causal reasoning explicit in ways that permit others to challenge them (Argyris, 1993). Productive reasoning is central to learning at individual and organizational levels (Argyris, 1993; Argyris & Schön, 1992) and therefore is valuable to increasing clarity on managing CPVs. This aligns with Simons’s (1995b) assertion that active management of CPVs is related to stimulating organization learning.
Implications for Practice
Viewing the complex and intertwined CPVs of a nonprofit from a holistic perspective brings to light several insights for practitioners. First, these findings serve as a cautionary warning against employing CPVs in a naive manner. Control mechanisms in nonprofits are neither simple nor unconflicted, and they may actively undermine each other if not considered in concert and in causal context. This method suggests that it makes little sense (and can do damage) to push or pull on singular performance variables without catalyzing more robust understanding of the larger system within the organization.
Second, client-driven clinical inquiry, in which researchers work together with an organization’s leaders, yields more valid information relevant to the research, which in turn can yield more useful insights for organization leaders. In particular, making explicit causal influences among CPVs helps leaders agree on and communicate to others opportunities for action. For example, participants in the SD sessions afterward commented, “This helps us talk about solutions,” “This helps us identify links and loops that are clear,” and “We have already started working elements of it [the causal loop model] into our budget.” More to the point, the use of CPVs in this nonprofit setting facilitated strategic planning: “This [SD diagram] is a tool that we can use in the future as fodder for real time strategic planning; it has become a tool for communication” and “It will guide the way we prioritize investments.” We believe that a clinical-inquiry approach is valuable to explore and substantiate the intertwined nature of various CPVs. Guided by a field site’s leaders’ perception of “the problem,” researchers can elicit multiple variables, as well as nuances in beliefs and causal reasoning, related to the organization’s diagnostic control system, which can suggest new opportunities for achieving desired organizational metrics and outcomes.
Third, because at their founding nonprofits are situated regionally and socially to offer solutions to specific problems, a clinical-inquiry approach that uses participatory causal-mapping provides a clear method for making explicit a particular nonprofit’s tailored causal chains for operationally addressing and fulfilling its mission. This can prevent inadvertent misuse of CPVs that may be appropriate for one organization but not for another. Moreover, the jointly constructed shared visual representations integral to the approach give nonprofit leaders opportunities and tools to engage internal and external stakeholders iteratively as they communicate, listen, and make decisions.
Fourth, a participatory causal-mapping approach to CPVs gives nonprofit leaders opportunity to consider together how they may cope with exogenous shocks. In the case of a community health center, this could be health care reform, which would affect variables in Figure 1 such as percent insured (payer mix) and average fee per service. By examining the effects of those variables and others on CPVs, leaders may recognize options for proactive, rather than reactive, strategic moves.
Limitations
A primary limitation of the article lies in its focus on a single case study. Nevertheless, as one of hundreds of the federally chartered community health centers that collectively served 25 million people in 2016, CHP faces ongoing challenges in successfully retaining and recruiting qualified staff, a challenge shared by other community health centers (Rosenblatt et al., 2006). More broadly, however, the particular CPV of staff recruiting and retention and CHP leaders’ frustration in addressing it represent a broader class of issues related to focusing on CPVs in isolation, rather than in the context of causal relations among multiple organizational variables and activities. The method used with leaders at this health center to elicit key variables and causally map interdependencies offers an approach that could be deployed by other nonprofits experiencing financial and operational challenges.
Conclusion
Previous scholarship highlights the importance of understanding the complex and intertwined nature of organizations. This is especially true for nonprofits chronically on the precipice of viability. Rather than simply acknowledge the importance of complexity and interdependencies, however, scholarship can inform more specifically how to explore causal relationships and make explicit dependencies among an organization’s CPVs. Co-creating a visual representation of interdependencies, leaders can discuss and decide with more insight how to make strategic trade-offs in the face of internal and external complexity. This case study demonstrates a generalizable method for executives and staff in nonprofits to make sense of their own interconnected and interdependent CPVs. It portrays that making explicit connections among management controls can promote strategic decision making to address financial sustainability and operational challenges. We hope the study presents a compelling glimpse of the challenges and potential benefits of advancing research in this domain.
Acknowledgments
We would like to thank Don Greer for facilitating the participatory modeling workshops. We also thank the staff of CHP for their participation.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The first author acknowledges research support from the Initiative for Regulation and Applied Economic Analysis (IRAEA) at Montana State University. The second author would like to acknowledge the support of the National Institute of General Medical Sciences (NIGMS) of the National Institutes of Health under award number 5P20GM104417 during the revision process in preparing this article for publication.
Author Biographies
Edward Gamble is an accounting professor at Montana State University. His research focuses on accounting approaches that reduce social, environmental, and economic inequality.
Andreas Thorsen is an assistant professor of management in the Jake Jabs College of Business & Entrepreneurship at Montana State University. His research interests include health service operations and optimization under uncertainty.
Laura Black is a management professor at Montana State University. Her research focuses on collaborative practices, particularly in the context of new product development and innovation, using participatory modeling with system dynamics.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The CEO of Community Health Partners (CHP) has given permission for this material to be published and their name to be used.
References
- Ackoff RL (1979). The future of operational research is past. Journal of the Operational Research Society, 30, 93–104. [Google Scholar]
- Argyris C (1990). Overcoming organizational defenses. New York, NY: Allyn & Bacon. [Google Scholar]
- Argyris C (1993). Knowledge for action: A guide to overcoming barriers to organizational change. San Francisco, CA: Jossey-Bass. [Google Scholar]
- Argyris C, & Schön DA (1992). On organizational learning. Cambridge, MA: Blackwell. [Google Scholar]
- Austin J, Stevenson H, & Wei-Skillern J (2006). Social and commercial entrepreneurship: Same, different, or both? Entrepreneurship, Theory and Practice, 30, 1–22. [Google Scholar]
- Bagnoli L, & Megali C (2011). Measuring performance in social enterprises. Nonprofit and Voluntary Sector Quarterly, 40, 149–165. [Google Scholar]
- Benjamin L, & Campbell D (2014). Nonprofit Performance: Accounting for the Agency of Clients. Nonprofit and Voluntary Sector Quarterly, 44, 988–1006. [Google Scholar]
- Bisbe J, & Otley D (2004). The effects of the interactive use of management control systems on product innovation. Accounting, Organizations and Society, 29, 709–737. [Google Scholar]
- Black LJ (2013). When visuals are boundary objects in system dynamics work. System Dynamics Review, 29, 70–86. [Google Scholar]
- Black LJ, & Andersen DF (2012). Using visual representations as boundary objects to resolve conflict in collaborative model-building approaches. Systems Research and Behavioral Science, 29, 194–208. [Google Scholar]
- Brassard M (1989). The memory jogger plus. Methuen, MA: GOAL/QPC. [Google Scholar]
- Burns J, & Scapens RW (2000). Conceptualizing management accounting change: An institutional framework. Management Accounting Research, 11, 3–25. [Google Scholar]
- Carnochan S, Samples M, Myers M, & Austin MJ (2014). Performance measurement challenges in nonprofit human service organizations. Nonprofit and Voluntary Sector Quarterly, 43, 1014–1032. [Google Scholar]
- Charnes A, & Cooper WW (1980). Auditing and accounting for program efficiency and management efficiency in not-for-profit entities. Accounting, Organizations and Society, 5, 87–107. [Google Scholar]
- Chenhall RH (2003). Management control systems design within its organizational context: Findings from contingency-based research and directions for the future. Accounting, Organizations and Society, 28, 127–168. [Google Scholar]
- Chenhall RH, Hall M, & Smith D (2013). Performance measurement, modes of evaluation and the development of compromising accounts. Accounting, Organizations and Society, 38, 268–287. [Google Scholar]
- Chenhall RH, Hall M, & Smith D (2017). The expressive role of performance measurement systems: A field study of a mental health development project. Accounting, Organizations and Society, 63, 60–75. [Google Scholar]
- Community Health Partners. (2016, January 5). Available from http://chphealthmt.org/
- Cooper DJ, & Morgan W (2008). Case study research in accounting. Accounting Horizons, 22, 159–178. [Google Scholar]
- Eisenhardt KM (1989). Making fast strategic decisions in high-velocity environments. Academy of Management Journal, 32, 543–576. [Google Scholar]
- Ferreira A, & Otley D (2009). The design and use of performance management systems: An extended framework for analysis. Management Accounting Research, 20, 263–282. [Google Scholar]
- Ferreira LD, & Merchant KA (1992). Field research in management accounting and control: A review and evaluation. Accounting, Auditing & Accountability Journal, 5(4). doi: 10.1108/09513579210019503 [DOI] [Google Scholar]
- Flyvbjerg B (2006). Five misunderstandings about case-study research. Qualitative Inquiry, 12, 219–245. [Google Scholar]
- Froelich KA (1999). Diversification of revenue strategies: Evolving resource dependence in nonprofit organizations. Nonprofit and Voluntary Sector Quarterly, 28, 246–268. [Google Scholar]
- Gamble EN, & Beer HA (2015). Spiritually informed not-for-profit performance measurement. Journal of Business Ethics, 141, 451–468. [Google Scholar]
- Geertz C (1973). The interpretation of cultures. Chicago, IL: Basic Books. [Google Scholar]
- Glasser M, Peters K, & MacDowell M (2006). Rural Illinois hospital chief executive officers’ perceptions of provider shortages and issues in rural recruitment and retention. The Journal of Rural Health, 22, 59–62. [DOI] [PubMed] [Google Scholar]
- Herremans IM, & Nazari JA (2016). Sustainability reporting driving forces and management control systems. Journal of Management Accounting Research, 28, 103–124. [Google Scholar]
- Hofstede G (1981). Management control of public and not-for-profit activities. Accounting, Organizations and Society, 6, 193–211. [Google Scholar]
- Hovmand PS (2014). Community based system dynamics. New York, NY: Springer Science Business Media. [Google Scholar]
- Inamdar N, Kaplan R, & Reynolds K (2002). Applying the balanced scorecard in health-care provider organizations/practitioner’s response. Journal of Healthcare Management, 47, 179–196. [PubMed] [Google Scholar]
- Jørgensen B, & Messner M (2009). Management control in new product development: The dynamics of managing flexibility and efficiency. Journal of Management Accounting Research, 21, 99–124. [Google Scholar]
- Kaplan RS (2001). Strategic performance measurement and management in nonprofit organizations. Nonprofit Management and Leadership, 11, 353–370. [Google Scholar]
- Kaplan RS, & Norton DP (1996). Linking the balanced scorecard to strategy. California Management Review, 39, 53–79. [Google Scholar]
- Kaplan RS, & Norton DP (2005). The balanced scorecard. Harvard Business Review, 84, 100–109. [PubMed] [Google Scholar]
- Langfield-Smith K (1997). Management control systems and strategy: A critical review. Accounting, Organizations and Society, 22, 207–232. [Google Scholar]
- LeRoux K, & Wright N (2010). Does performance measurement improve strategic decision making? Findings from a national survey of nonprofit social service agencies. Nonprofit and Voluntary Sector Quarterly, 39, 571–587. [Google Scholar]
- Malina MA, & Selto FH (2001). Communicating and controlling strategy: An empirical study of the effectiveness of the balanced scorecard. Journal of Management Accounting Research, 13, 47–90. [Google Scholar]
- Malmi T, & Brown DA (2008). Management control systems as a package—Opportunities, challenges and research directions. Management Accounting Research, 19, 287–300. [Google Scholar]
- Nicholls A (2009). “We do good things, don’t we?” Blended value accounting in social entrepreneurship. Accounting, Organizations and Society, 34, 755–769. [Google Scholar]
- Noonan WR (2007). Discussing the undiscussable: A guide to overcoming defensive routines in the workplace. San Francisco, CA: Jossey-Bass. [Google Scholar]
- Otley D (1999). Performance management: A framework for management control systems research. Management Accounting Research, 10, 363–382. [Google Scholar]
- Packard T (2010). Staff perceptions of variables affecting performance in human service organizations. Nonprofit and Voluntary Sector Quarterly, 39, 971–990. [Google Scholar]
- Richardson GP, & Andersen DF (1995). Teamwork in group model building. System Dynamics Review, 11, 113–137. [Google Scholar]
- Rittel HWJ, & Webber MM (1973). Dilemmas in a general theory of planning. Policy Sciences, 4, 155–169. [Google Scholar]
- Rosenblatt RA, Andrilla CH, Curtin T, & Hart LG (2006). Shortages of medical personnel at community health centers: Implications for planned expansion. Journal of the American Medical Association, 295, 1042–1049. [DOI] [PubMed] [Google Scholar]
- Schein EH (2007). Clinical inquiry / research In Reason P & Bradbury H (Eds.), Handbook of action research (pp. 266–279). Thousand Oaks, CA: SAGE. [Google Scholar]
- Shields MD (2015). Established management accounting knowledge. Journal of Management Accounting Research, 27, 123–132. [Google Scholar]
- Simons R (1995a). Control in an age of empowerment. Harvard Business Review, 73(2), 80–88. [Google Scholar]
- Simons R (1995b). Control levers: How managers use innovative control systems to drive strategic renewal. Cambridge, MA: Harvard Business Press. [Google Scholar]
- Speckbacher G (2003). The economics of performance management in nonprofit organizations. Nonprofit Management & Leadership, 13, 267–281. [Google Scholar]
- Sterman JD (2000). Business dynamics: Systems thinking and modeling for a complex world. Boston, MA: Irwin/McGraw-Hill. [Google Scholar]
- Tessier S, & Otley D (2012). A conceptual development of Simons’ Levers of Control framework. Management Accounting Research, 23, 171–185. [Google Scholar]
- Tuomela TS (2005). The interplay of different levers of control: A case study of introducing a new performance measurement system. Management Accounting Research, 16, 293–320. [Google Scholar]
- Vennix JAM (1996). Group model building: Facilitating team learning using system dynamics. Chichester, UK: John Wiley. [Google Scholar]
- Vennix JAM (1999). Group model-building: Tackling messy problems. System Dynamics Review, 15, 379–401. [Google Scholar]
- Widener SK (2007). An empirical analysis of the levers of control framework. Accounting, Organizations and Society, 32, 757–788. [Google Scholar]
- Wolstenholme E (1994). A systematic approach to model creation In Morecroft JDW & Sterman JD (Eds.), Modeling for learning organizations (pp. 175–194). Portland, OR: Productivity Press. [Google Scholar]